Introduction to Physical Examination Dr Gwen Hollaar Dr






- Slides: 38
Introduction to Physical Examination Dr. Gwen Hollaar Dr. Lanice Jones Dr. Robert Lee September 2006 Lao Project
Outline General Observations Vital Signs General Approach to physical examination General surface anatomy Examination of Head and Neck Examination of Lymph nodes
Physical Examination begins with observing the patient Many observations can be made while the patient walks into the examination room or as you approach the patient Level of Consciousness Alert or decreased level of consciousness Apparent State of Health: Acutely ill or chronically ill (i. e. emaciated) Signs of Distress Sweating / Diaphoresis Dyspnea / Wheeze / Cough Pain Posture, gait, or motor activity Anxiety or Depression Skin Pale Jaundice Dress or hygiene
Preparation / Draping Prior to beginning formal physical examination: Explain to patient what you will be doing Make sure patient feels comfortable and provide privacy Ask patient to remove clothing so that you can do proper physical examination Give patient sheet/gown to cover herself Uncover only the area that you are presently examining to keep patient comfortable In general, examine from head to toe During examination make as few position changes as possible
Vital Signs Height and Weight Temperature Usually oral or rectal thermometer Respiratory Rate Have student count for 30 seconds Have student also observe character of respirations Pulse Can be done on any pulse, but radial pulse is usually used Need to teach how to assess rate AND quality of pulse Blood pressure Need to teach students the steps involved in taking BP
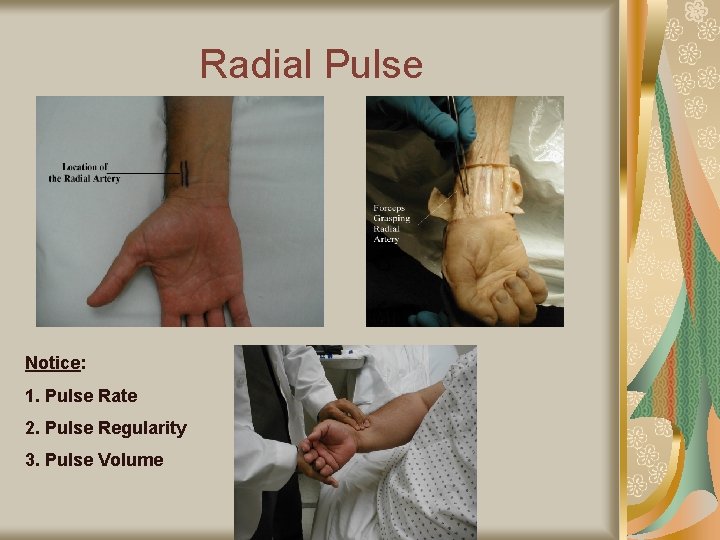
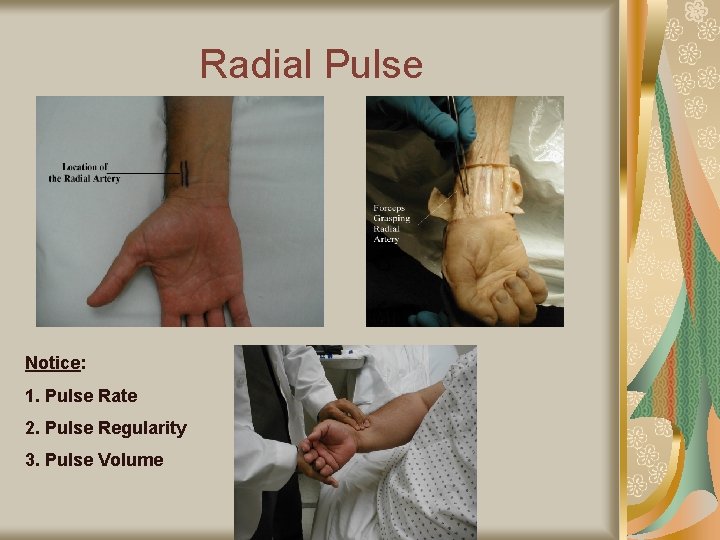
Radial Pulse Notice: 1. Pulse Rate 2. Pulse Regularity 3. Pulse Volume

Blood Pressure Measurement 3 Cuff Sizes: 1. Pediatric 2. Adult Regular to 32 – 35 cm arm circumference 3. Adult Large TOO SMALL A CUFF ARTIFICIALLY ELEVATES BP! Brachial artery on ulnar side of biceps tendon Place BP cuff marker over brachial artery
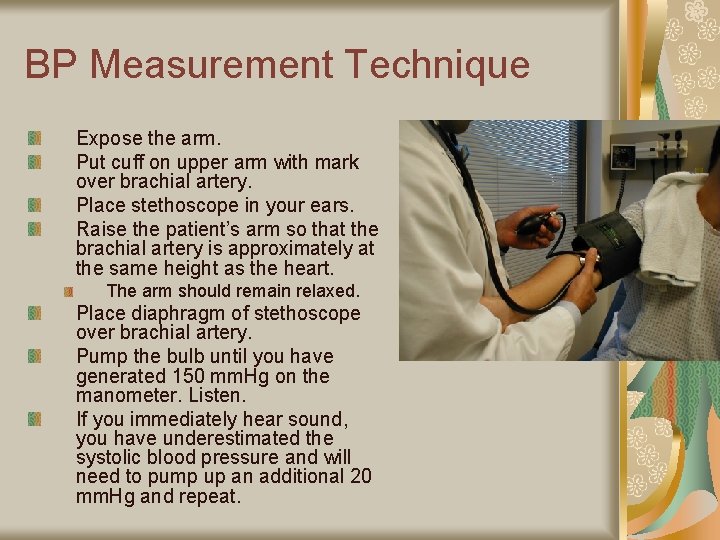
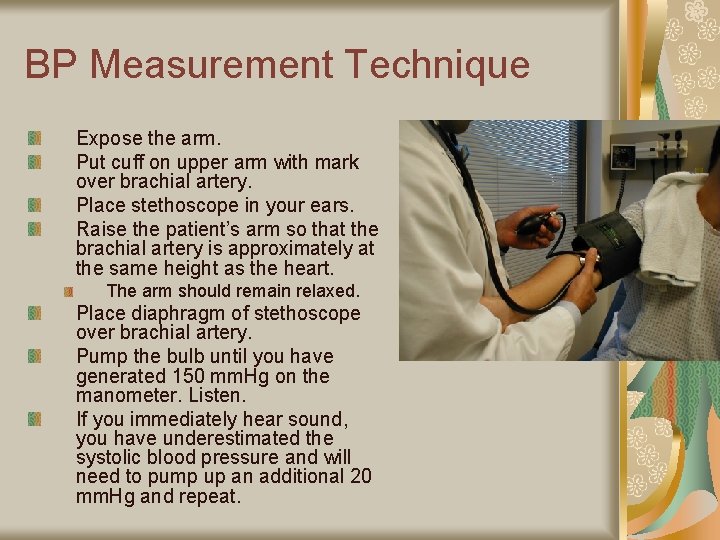
BP Measurement Technique Expose the arm. Put cuff on upper arm with mark over brachial artery. Place stethoscope in your ears. Raise the patient’s arm so that the brachial artery is approximately at the same height as the heart. The arm should remain relaxed. Place diaphragm of stethoscope over brachial artery. Pump the bulb until you have generated 150 mm. Hg on the manometer. Listen. If you immediately hear sound, you have underestimated the systolic blood pressure and will need to pump up an additional 20 mm. Hg and repeat.
BP Measurement Technique Now slowly deflate the blood pressure cuff. The first sound that you hear is systolic blood pressure. You are hearing blood that has started to flow through the artery as you release pressure of the cuff. The diastolic blood pressure is measured when the sound completely disappears. This is the point when the pressure within the vessel is greater then that supplied by the cuff, allowing the free flow of blood without turbulence and thus no audible sound. The sound between the systolic and diastolic pressure are known as the ‘sounds of Korotkov’
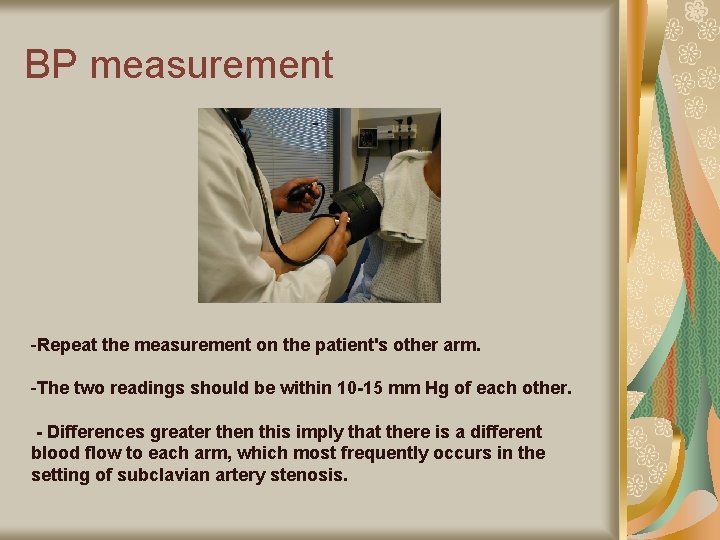
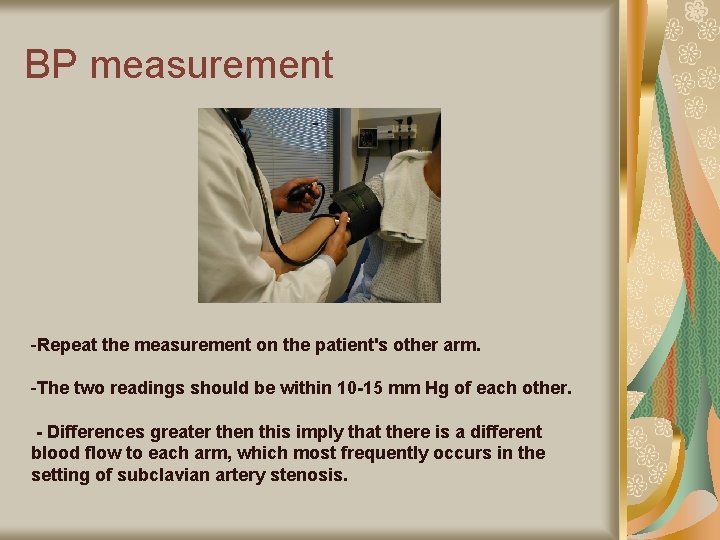
BP measurement - -Repeat the measurement on the patient's other arm. -The two readings should be within 10 -15 mm Hg of each other. - Differences greater then this imply that there is a different blood flow to each arm, which most frequently occurs in the setting of subclavian artery stenosis.
General approach to a physical examination Patient sitting – Physician stands in front of patient Vital signs include observation of the hands Head Examination Examine the eyes & mouth Examine ears, sinus, scalp as needed Neck Examination Central (thyroid), anterior triangle, posterior triangle Patient sitting – Physician stands behind patient Examine posterior chest (Respiratory) Patient sitting – Physician stands in front of patient Exam anterior chest (Respiratory and Cardiac) Patient Lying down Finish cardiac examination Do abdominal Examination Genitourinary exam and rectal exam as indicated MSK as indicated (lying, sitting, and standing)
Surface Anatomy Why do we have students study surface anatomy? Students need to make practical their knowledge of anatomy Students need to understand body landmarks in order to describe their observations You should teach surface anatomy for every body system We will now cover some examples
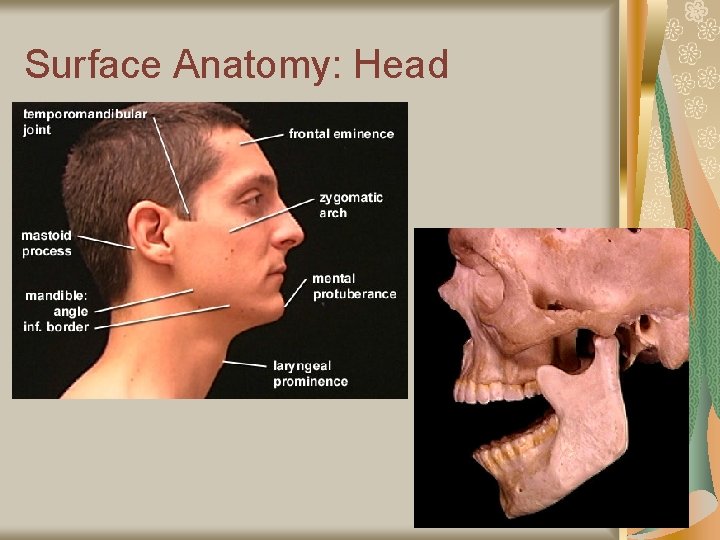
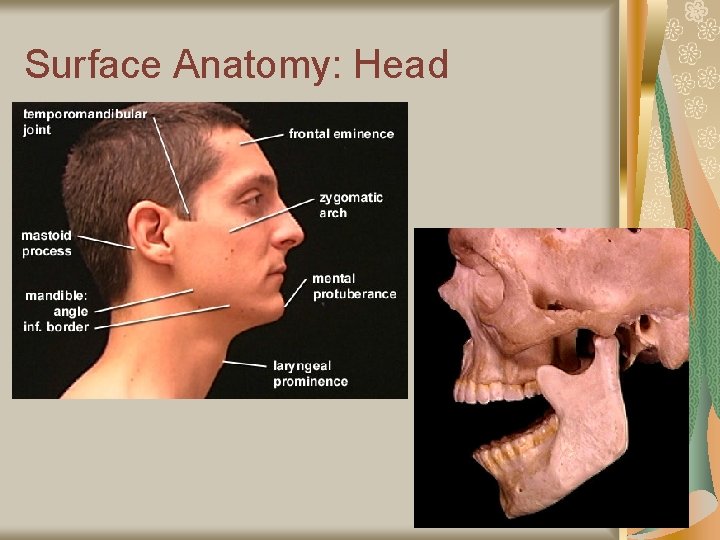
Surface Anatomy: Head
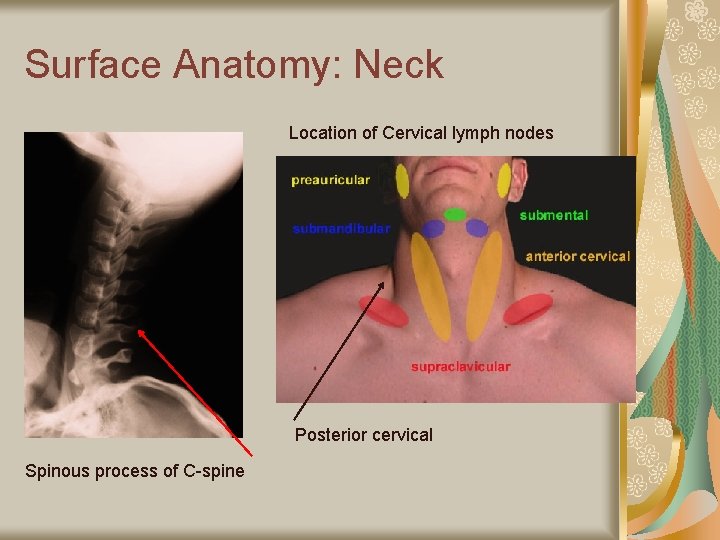
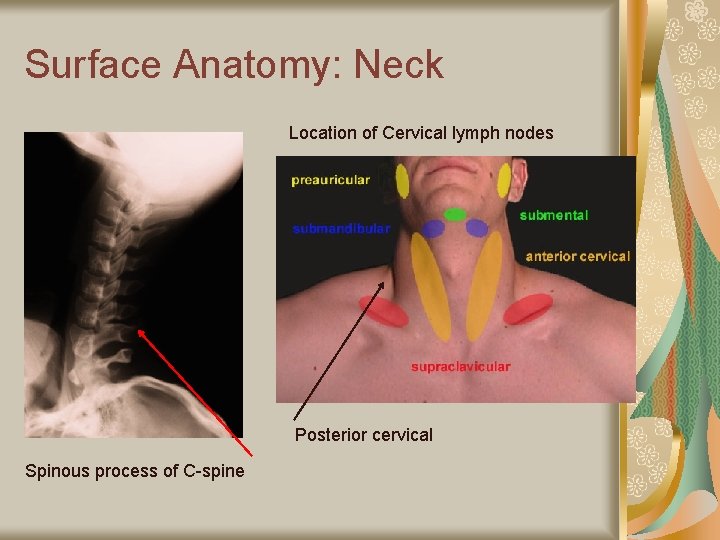
Surface Anatomy: Neck Location of Cervical lymph nodes Posterior cervical Spinous process of C-spine
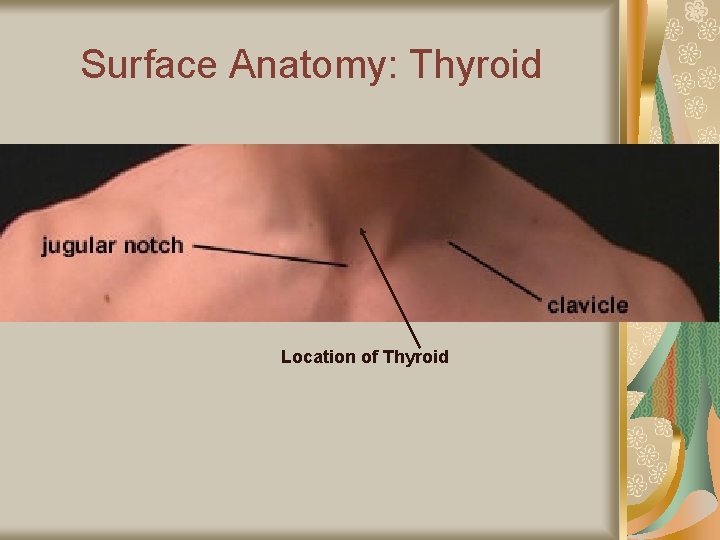
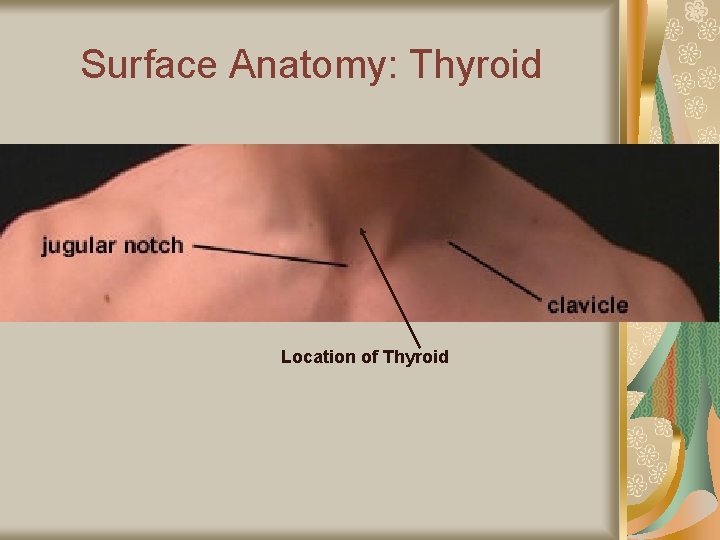
Surface Anatomy: Thyroid Location of Thyroid
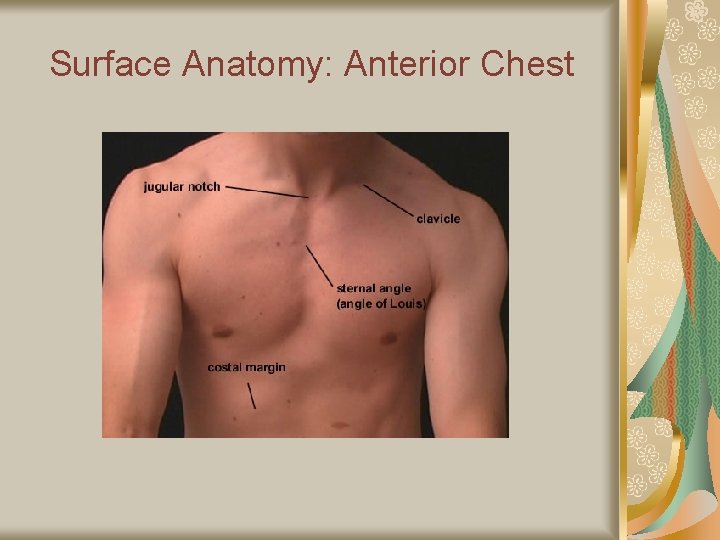
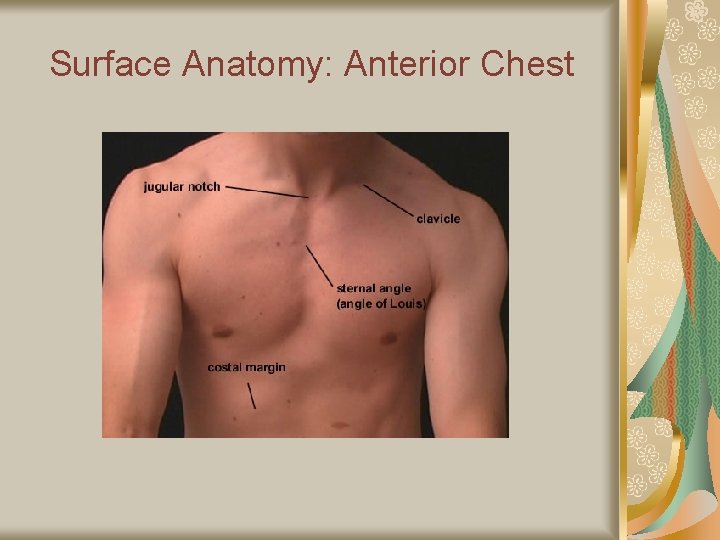
Surface Anatomy: Anterior Chest

Surface Anatomy: Anterior Chest
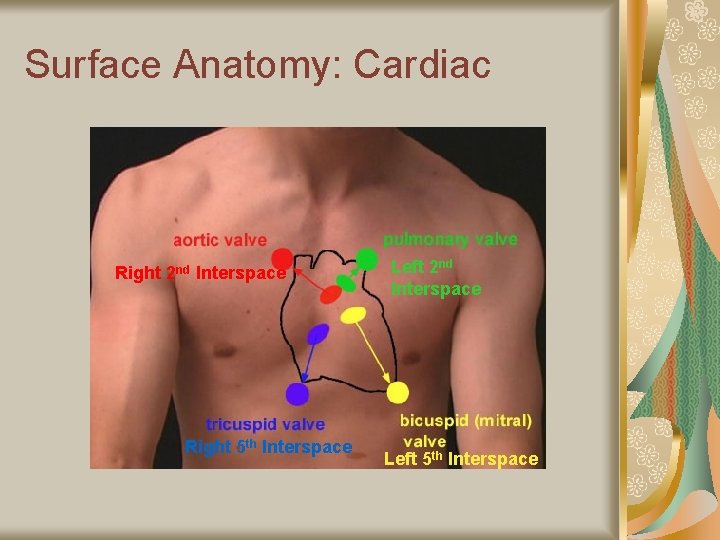
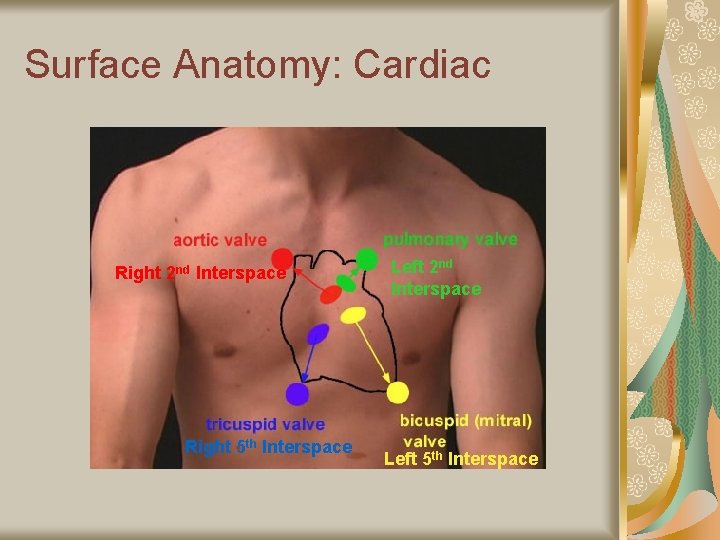
Surface Anatomy: Cardiac Right 2 nd Interspace Right 5 th Interspace Left 2 nd Interspace Left 5 th Interspace
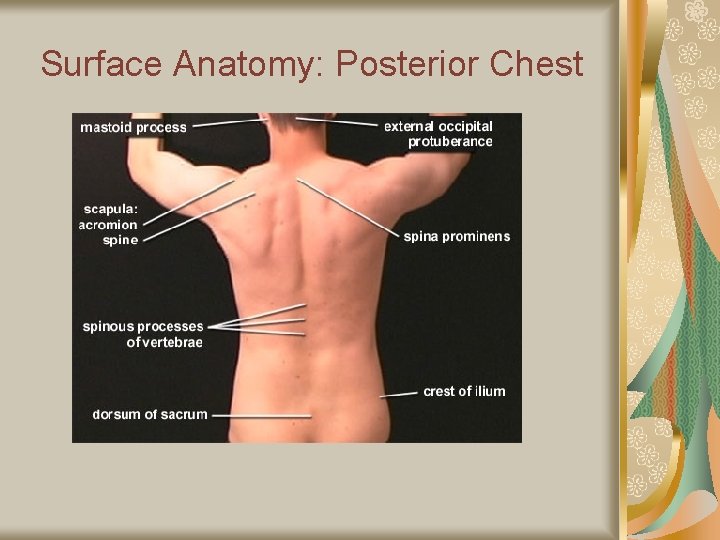
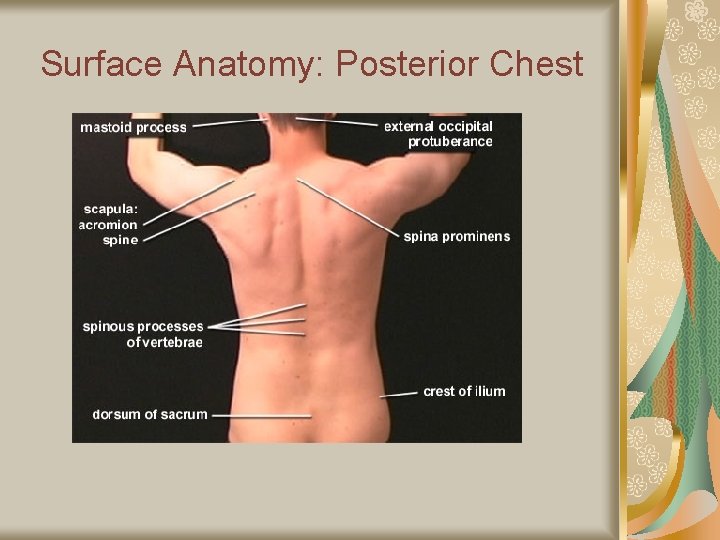
Surface Anatomy: Posterior Chest
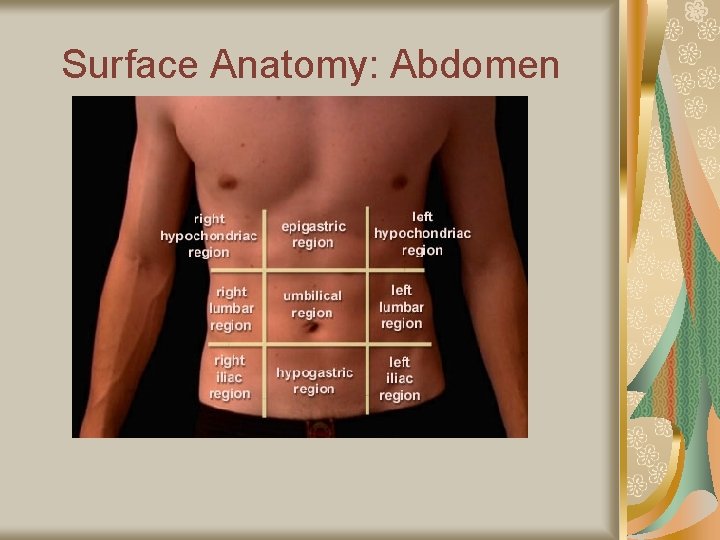
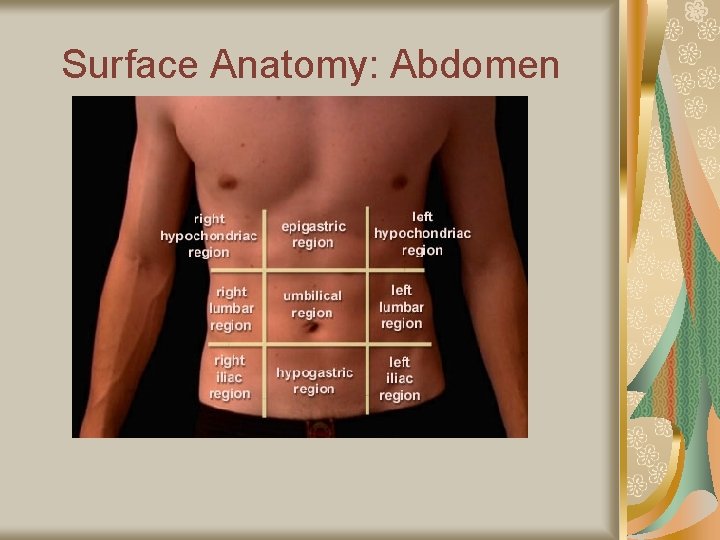
Surface Anatomy: Abdomen
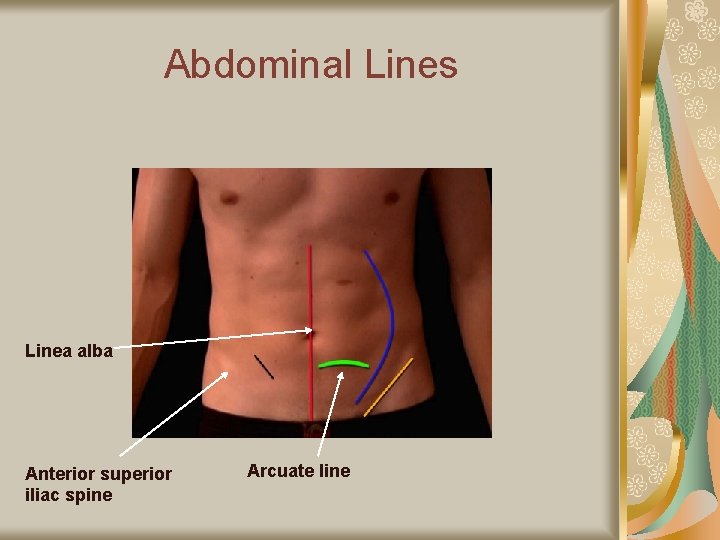
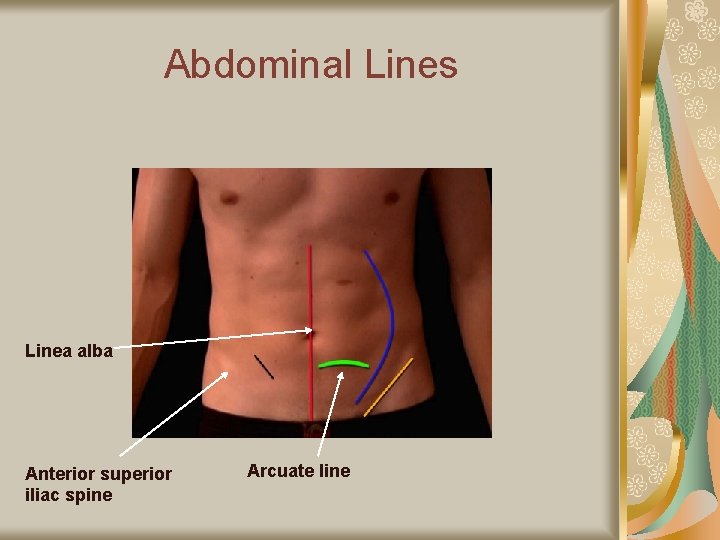
Abdominal Lines Linea alba Anterior superior iliac spine Arcuate line
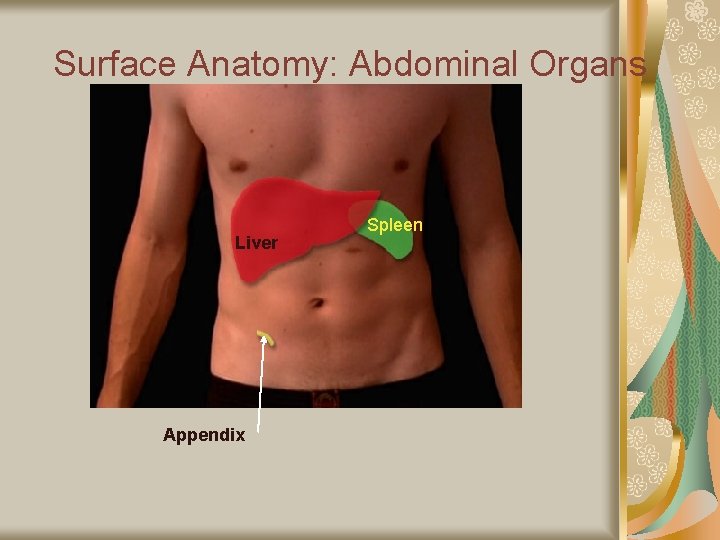
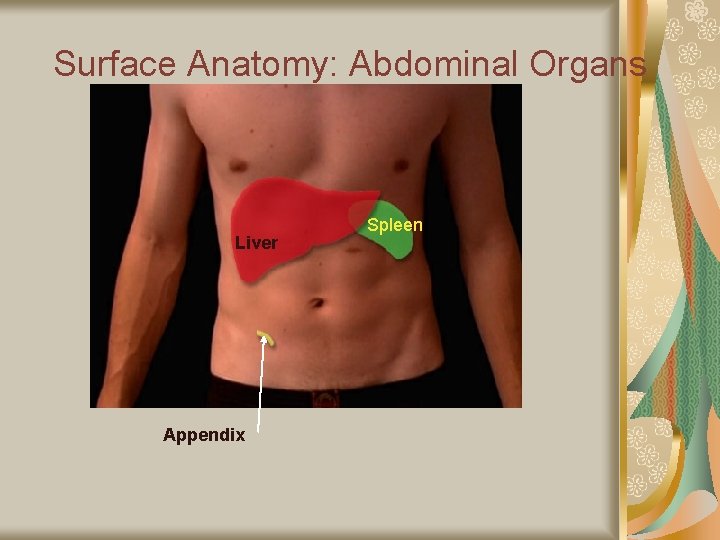
Surface Anatomy: Abdominal Organs Liver Appendix Spleen
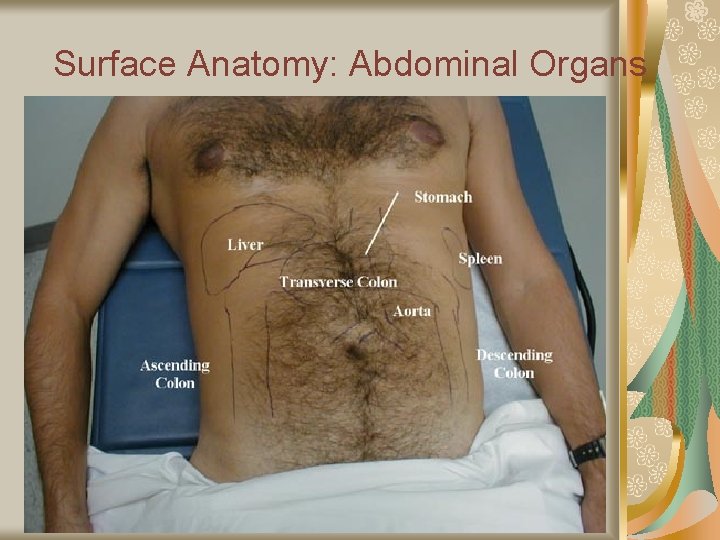
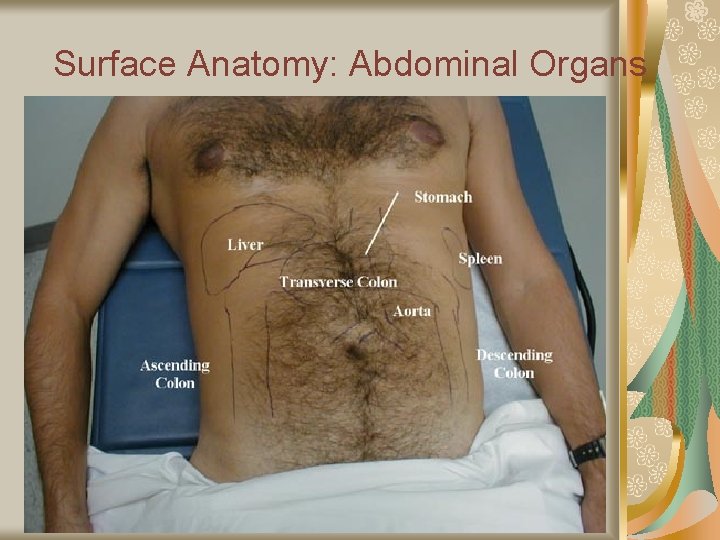
Surface Anatomy: Abdominal Organs

Musculo-Skeletal Surface Anatomy: Knee (as one example)
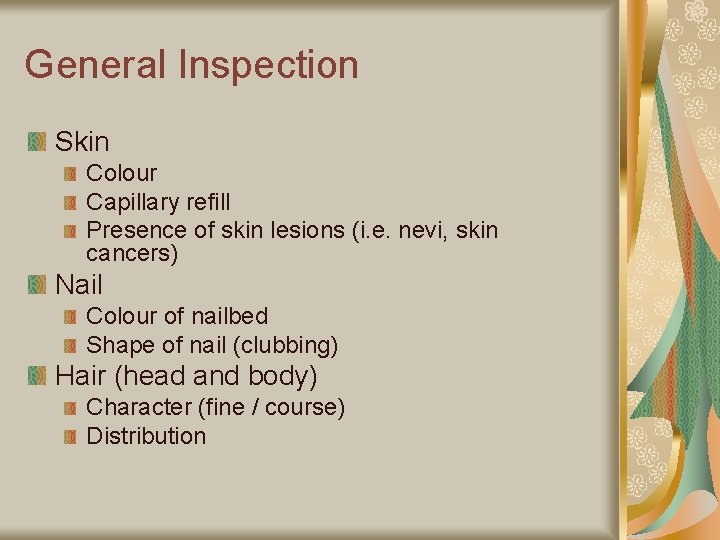
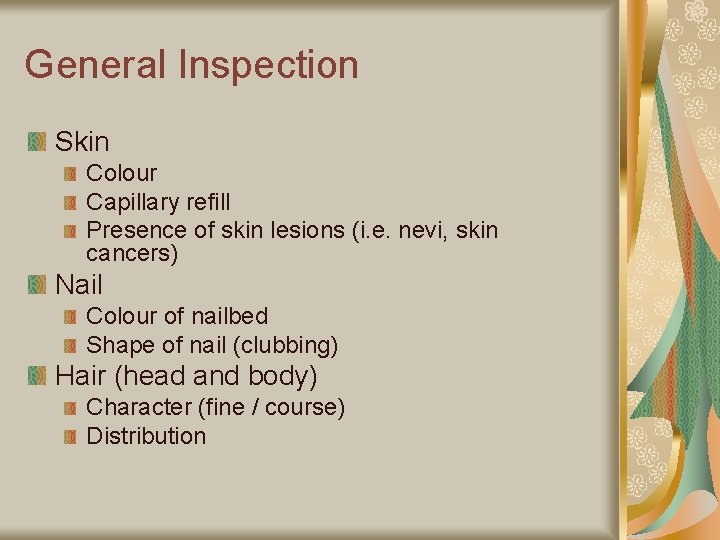
General Inspection Skin Colour Capillary refill Presence of skin lesions (i. e. nevi, skin cancers) Nail Colour of nailbed Shape of nail (clubbing) Hair (head and body) Character (fine / course) Distribution
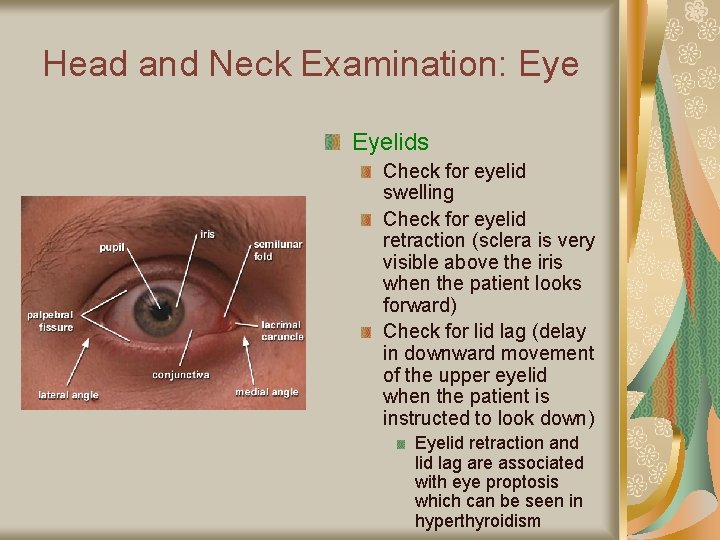
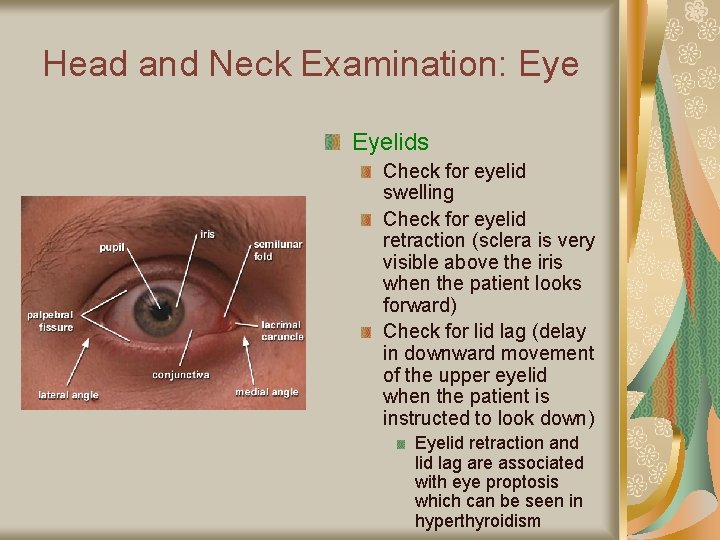
Head and Neck Examination: Eyelids Check for eyelid swelling Check for eyelid retraction (sclera is very visible above the iris when the patient looks forward) Check for lid lag (delay in downward movement of the upper eyelid when the patient is instructed to look down) Eyelid retraction and lid lag are associated with eye proptosis which can be seen in hyperthyroidism
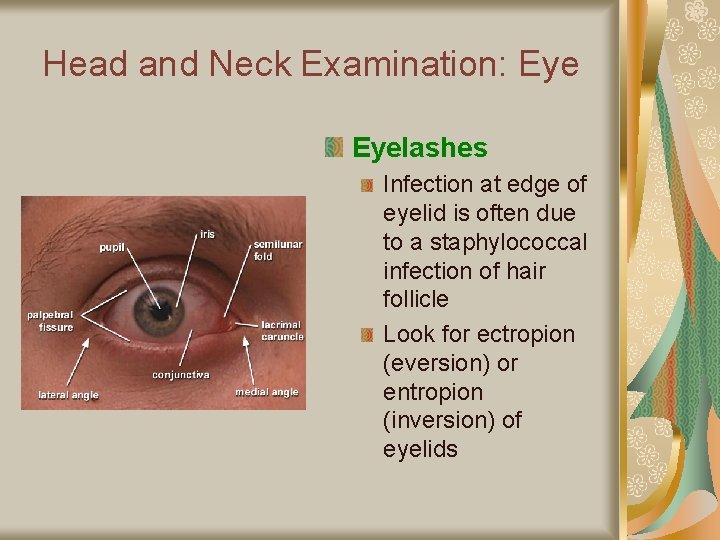
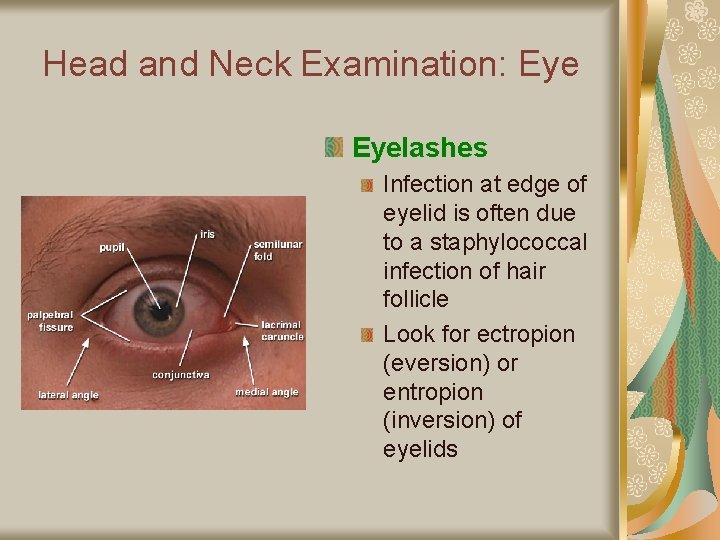
Head and Neck Examination: Eyelashes Infection at edge of eyelid is often due to a staphylococcal infection of hair follicle Look for ectropion (eversion) or entropion (inversion) of eyelids
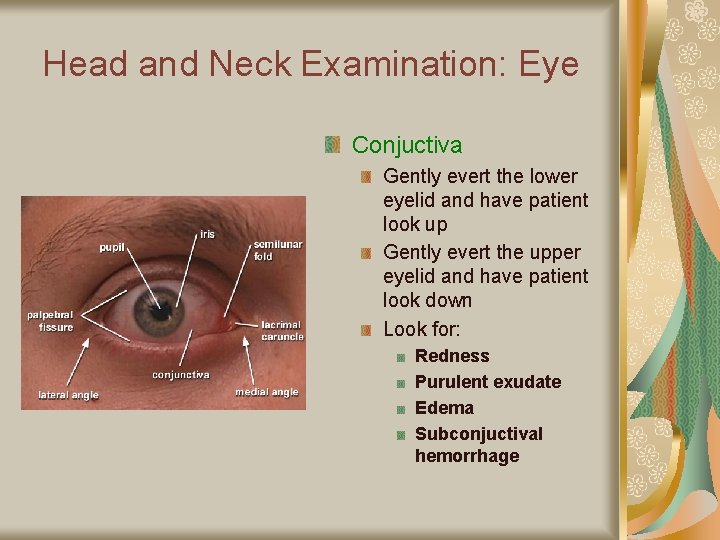
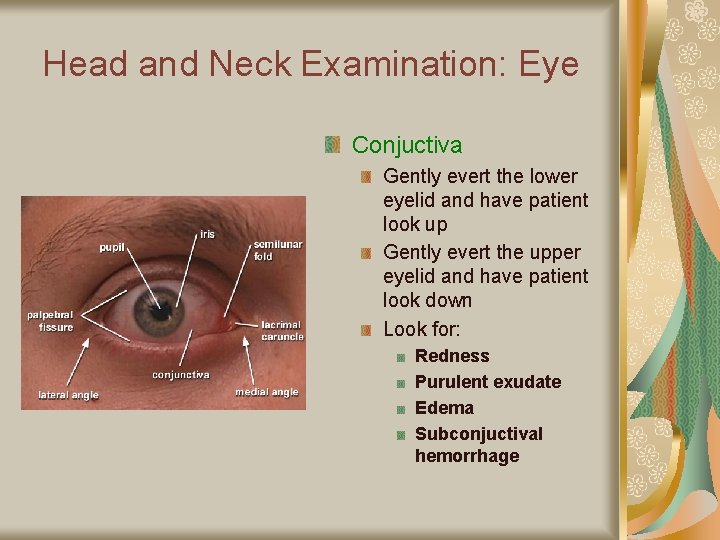
Head and Neck Examination: Eye Conjuctiva Gently evert the lower eyelid and have patient look up Gently evert the upper eyelid and have patient look down Look for: Redness Purulent exudate Edema Subconjuctival hemorrhage
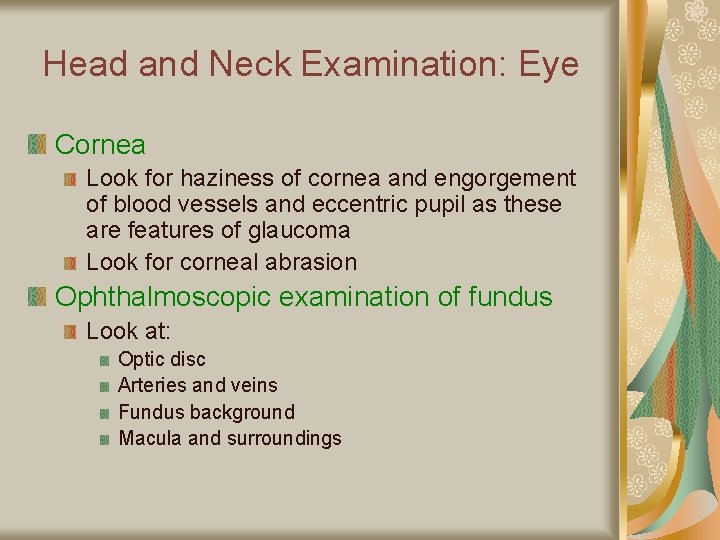
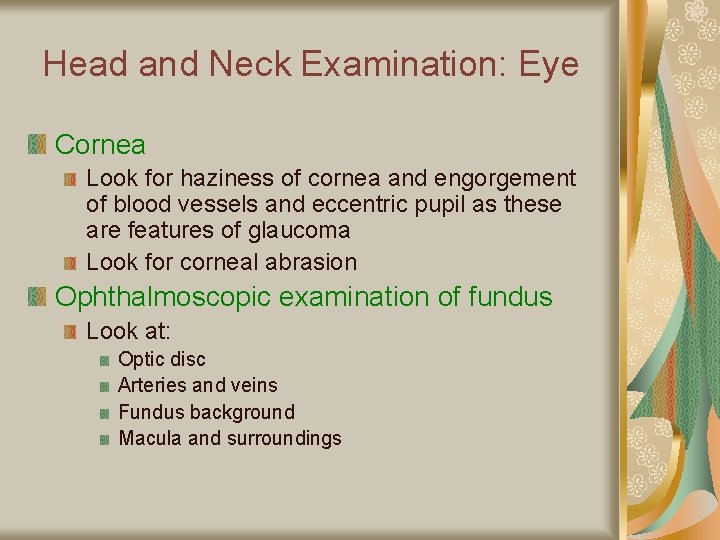
Head and Neck Examination: Eye Cornea Look for haziness of cornea and engorgement of blood vessels and eccentric pupil as these are features of glaucoma Look for corneal abrasion Ophthalmoscopic examination of fundus Look at: Optic disc Arteries and veins Fundus background Macula and surroundings
Head and Neck Examination: Ears Look at external ear Do auriscopic examination Pull the outside ear up and slightly lateral and look at: External meatus Tympanum – The ear drum is normally grey in colour
Head and Neck Examination: Nose and Sinuses Test patency of each nostril by closing one nostril with your finger and asking patient to breathe through their other nostril with their mouth closed Look up each nostril with nasal speculum to see appearance of mucosa and inferior nasal turbinates Can tap over frontal and maxillary sinuses to test for tenderness
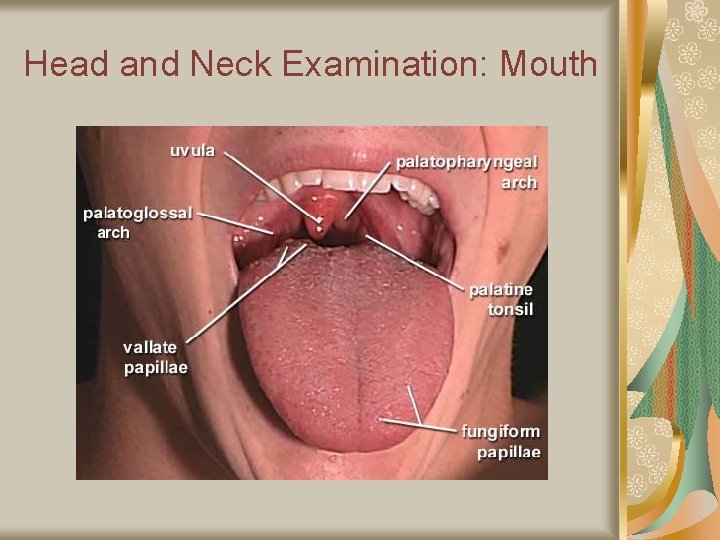
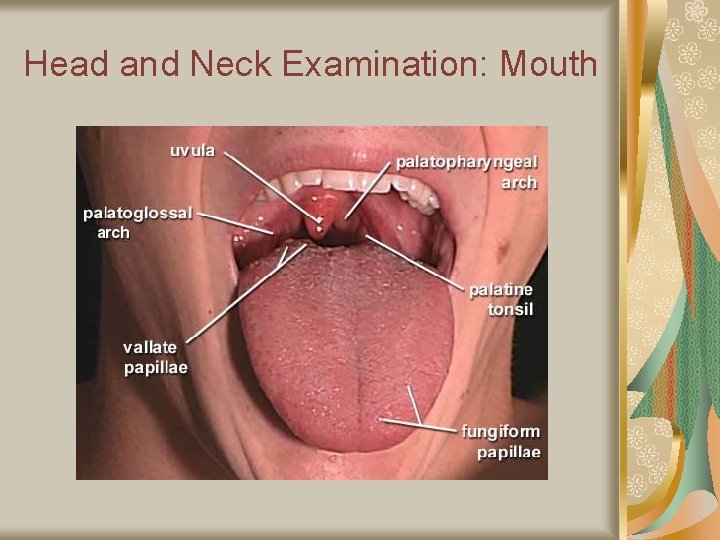
Head and Neck Examination: Mouth
Head and Neck Examination: Mouth Lips Look at colour (i. e. cyanosis) Look for cracking of the lips or non-healing lesions Look for painful cracks at the corners of the mouth Teeth Look at dental hygiene Gums Look for areas where gums may be swollen or infected Tongue Look at tongue size and movement Look at tongue mucosa (top and bottom of tongue) Colour Atrophy or smooth mucosa (i. e. associated with iron or vitamin B 12 deficiency) Look for tongue lesions or non-healing ulcers (i. e. tongue cancer)
Head and Neck Examination: Mouth Palate Look at mucosa and make sure there is no mucosal lesion or deformity Tonsils and pharynx Have patient protrude tongue, say ‘ah’, and place tongue depressor over tongue Look for swollen gland or red mucosa or exudate Salivary glands Palpate over parotid and submandibular salivary glands feeling for masses or tenderness (i. e. parotid gland may be enlarged from mumps, plugged salivary duct from stone, or tumor) Look at ductal openings in mouth Parotid duct openings are located opposite the second upper molars Submandibular duct openings are located near the midline in the sublingual region

Head and Neck Examination: Cervical Lymph Nodes Inspect and palpate all the cervical lymph node areas: Preauricular Submental Submandibular Anterior cervical chain Posterior cervical chain Supraclavicular Posterior cervical

Head and Neck Examination: Thyroid Inspect from the front Can palpate from the front or the back (often easier from the back) Place fingers over each lobe of the thyroid (below the thyroid cartilage and above the jugular notch) Stabilize one side while examining the opposite lobe Feel for firmness, tenderness, nodules, or enlargement Ask patient to swallow as you palpate each lobe Auscultate over the thyroid gland May hear a bruit in conditions of hyperthyroidism
Examination of Lymph Nodes Need to examine all major areas of lymph nodes Cervical lymph nodes (Discussed already on neck examination) Epitrochlear lymph nodes Palpate on medial aspect of elbow) Axillary lymph nodes Slightly abduct arm, have patient keep arm relaxed, and slide your hand up into the axilla and palpate along the chest wall Femoral lymph nodes Palpate over the area of the femoral artery and vein in the groins

Questions?
 Physical examination introduction
Physical examination introduction Van nuffelen marc
Van nuffelen marc Gwen nuttall
Gwen nuttall Gwen nuttall
Gwen nuttall Gwen blumberg
Gwen blumberg Mr ames is dragging a box
Mr ames is dragging a box Gwen graphs
Gwen graphs Veiligheidsgevoel en burgerparticipatie
Veiligheidsgevoel en burgerparticipatie Gwen araujo
Gwen araujo Gwen hansen
Gwen hansen Suburban sonnet gwen harwood
Suburban sonnet gwen harwood What frightened the fair gwen
What frightened the fair gwen Gwen nuttall
Gwen nuttall Physical examination tray
Physical examination tray Physical exam equipment
Physical exam equipment Nutrition focused physical examination
Nutrition focused physical examination Focused gastrointestinal assessment
Focused gastrointestinal assessment Bates guide to physical examination
Bates guide to physical examination Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Office-based pre-participation physical examination
Office-based pre-participation physical examination Ballottement spleen
Ballottement spleen Integumentary system physical examination
Integumentary system physical examination Pediatric history and physical examination
Pediatric history and physical examination Physical examination of a patient
Physical examination of a patient Speciality certificate examination in respiratory medicine
Speciality certificate examination in respiratory medicine Principles of history taking
Principles of history taking What is tactile fremitus
What is tactile fremitus Positioning and draping for physical examinations
Positioning and draping for physical examinations Principles of physical examination
Principles of physical examination Inspection and palpation
Inspection and palpation Myotomes ll
Myotomes ll Neonatal jaundice physical examination
Neonatal jaundice physical examination Pulastion
Pulastion Wolters kluwer
Wolters kluwer Principles of physical examination
Principles of physical examination Principles of physical examination
Principles of physical examination Conclusion of physical examination
Conclusion of physical examination Skin erosion
Skin erosion Painad scale
Painad scale