Intracoronary Streptokinase after Primary Percutaneous Coronary Intervention Murat



- Slides: 21
Intracoronary Streptokinase after Primary Percutaneous Coronary Intervention Murat Sezer, Hüseyin Oflaz, Taner Gören, Irem Okcular, Berrin Umman, Yılmaz Nişancı, Ahmet Kaya Bilge, Yasemin Şanlı, Mehmet Meriç, Sabahattin Umman Istanbul University, Istanbul Faculty of Medicine, Department of Cardiology
Rational of the study From Epicardial Coronaries… • Primary percutaneous coronary intervention (PCI) is the most effective reperfusion method in the treatment of STEMI. • Nevertheless, processes causing myocardial damage are not immediately terminated despite elimination of epicardial occlusion with successful primary PCI. • It has been presumed that reperfusion injury mechanisms including embolization of epicardial thrombus and plaque content to microvasculature, are responsible for this ongoing damage. • Unfortunately almost all of the studies based on these hypothesis and aiming to stop this injury have not been succeeded.

… to the Microvasculature • There is a growing evidence pointing concordance between myocardial and microvascular damage in STEMI patients. • Microvascular damage might not be only an accompanying prosess to the myocardial damage. Also there might be a causal relationship in between. • If one focused to microvasculature during peri PCI procedure, it can easily realized that another and important contributor might have a role in this process. insitu microvascular thrombus!
Virchow’s Triad and Autochthonous Thrombus • All three components of Virchow’s triad (blood constituent, endothelial damage and stasis) exist at extreme levels in the microvasculature of infarcted myocardium. • Therefore, in situ (de novo) formed fraction may constitute the main part of the thrombus located in infarct site’s microvasculature. Virchow RR. Cellular Pathology. London, Churchill, 1860.
Coronary Vascular Resistance • If epicardial and microvascular vessels are considered as serially connected resistances, elimination of the proximal epicardial occlusion and retrieval of whole epicardial thrombus would not be enough to normalize total coronary resistance and perfusion at affected segments.
Hypothesis • Complementary intracoronary streptokinase (ICSK) infusion immediately following primary PCI may further improve tissue level perfusion by dissolving thrombus (either in situ formed or embolized from the proximal origin) at microvascular level. • To this end, the effect of low dose (250 k. U) ICSK, administered immediately after primary PCI, on myocardial perfusion was investigated prospectively.
Inclusion / Exclusion Criteria • Inclusion criteria: – Ongoing chest pain, – ST segment elevation on electrocardiogram, – Occlusion of the infarct related artery at angiography (Thrombolysis in Myocardial Infarction [TIMI] 0 I flow) • Exclusion criteria: – – – Culprit lesion in a saphenous vein graft, Additional narrowing >50% distal to the culprit lesion, Left bundle branch block, History of prior myocardial infarction, and Contraindications to streptokinase, tirofiban, aspirin, clopidogrel or heparin.
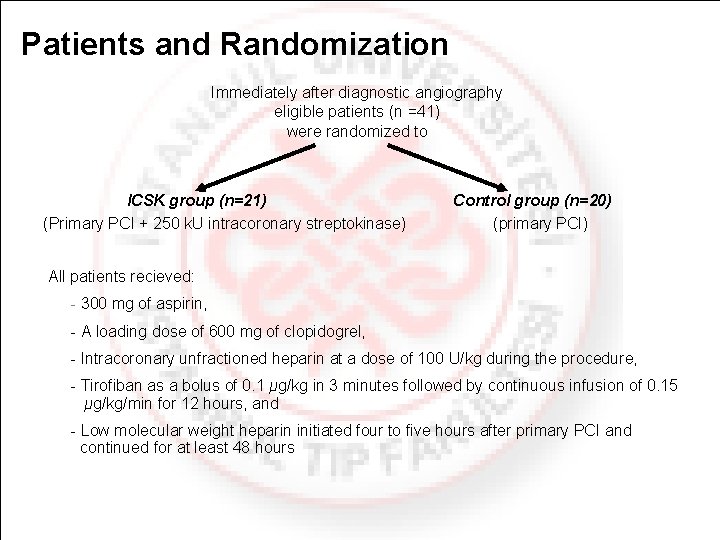
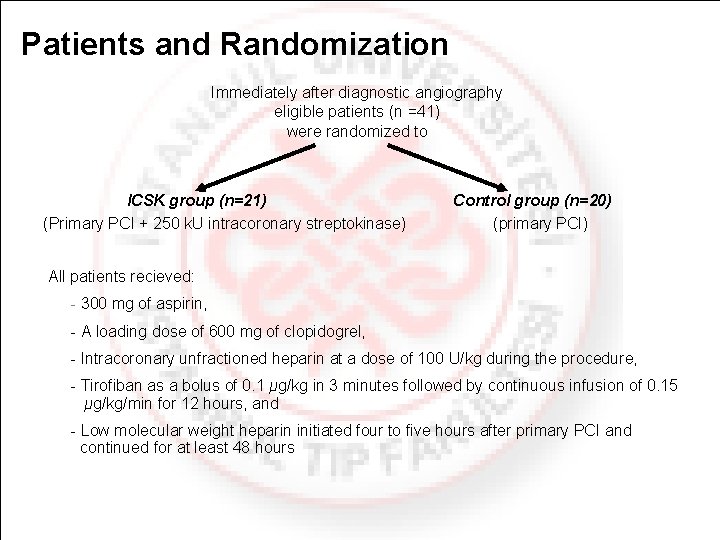
Patients and Randomization Immediately after diagnostic angiography eligible patients (n =41) were randomized to ICSK group (n=21) (Primary PCI + 250 k. U intracoronary streptokinase) Control group (n=20) (primary PCI) All patients recieved: 300 mg of aspirin, A loading dose of 600 mg of clopidogrel, Intracoronary unfractioned heparin at a dose of 100 U/kg during the procedure, Tirofiban as a bolus of 0. 1 μg/kg in 3 minutes followed by continuous infusion of 0. 15 μg/kg/min for 12 hours, and Low molecular weight heparin initiated four to five hours after primary PCI and continued for at least 48 hours

Study Design All patients underwent intracoronary hemodynamic measurement and angiographic analysis two days after primary PCI to evaluate microvascular function Long term Assesing microvascular perfusion assesments and LV volumes in early phase of (at 6 months) STEMI ST segment resolution Diastolic deceleration time Echocardiographic assessment of left ventricular volumes and function Coronary flow reserve Index of microvascular resistance Coronary wedge pressure (mean ad systolic) Pressure derived collateral flow index Myocardial blush grades Corrected TIMI frame count Pre/post PCI ECG Transthoracic echocardiography, 2 days after AMI Second angiography and intracoronary hemodynamic measurements 2 days after AMI. Control angiography (TIMI frame count, Myocardial blush grade) Infarct size measurement (SPECT), Echocardiographic assessment of left ventricular volumes and function
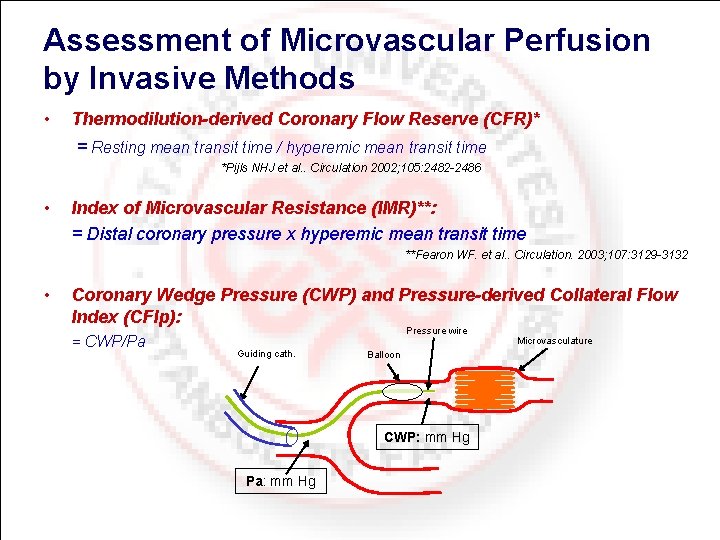
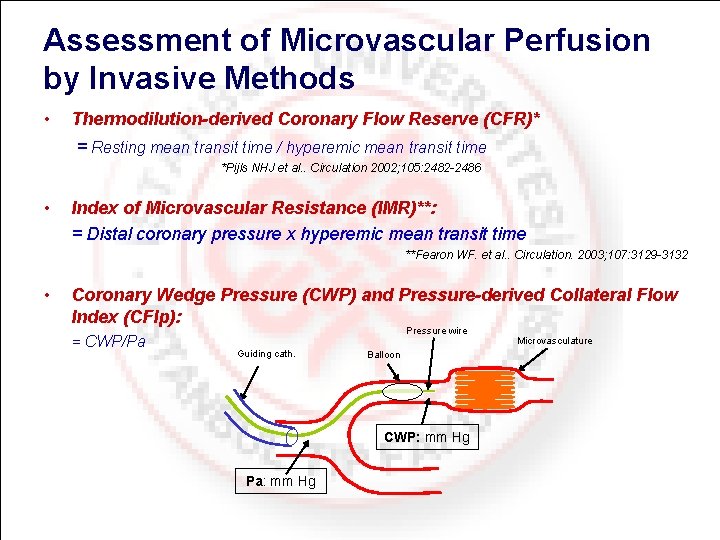
Assessment of Microvascular Perfusion by Invasive Methods • Thermodilution-derived Coronary Flow Reserve (CFR)* = Resting mean transit time / hyperemic mean transit time *Pijls NHJ et al. . Circulation 2002; 105: 2482 -2486 • Index of Microvascular Resistance (IMR)**: = Distal coronary pressure x hyperemic mean transit time **Fearon WF. et al. . Circulation. 2003; 107: 3129 -3132 • Coronary Wedge Pressure (CWP) and Pressure-derived Collateral Flow Index (CFIp): = CWP/Pa Pressure wire Guiding cath. Balloon CWP: mm Hg Pa: mm Hg Microvasculature
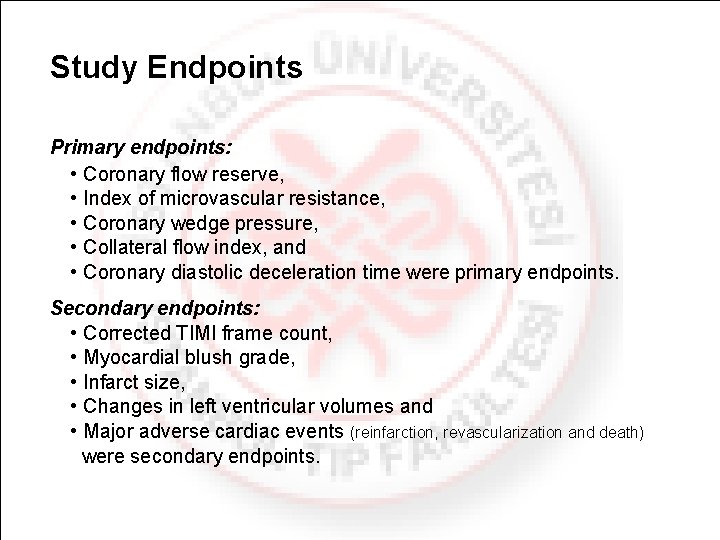
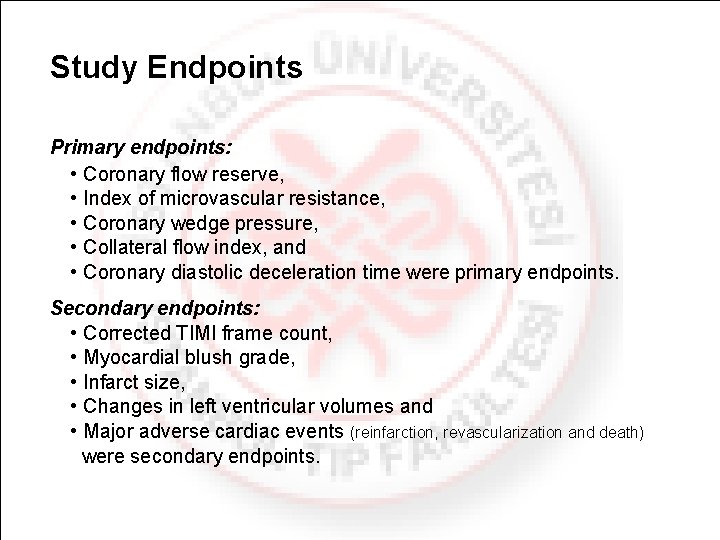
Study Endpoints Primary endpoints: • Coronary flow reserve, • Index of microvascular resistance, • Coronary wedge pressure, • Collateral flow index, and • Coronary diastolic deceleration time were primary endpoints. Secondary endpoints: • Corrected TIMI frame count, • Myocardial blush grade, • Infarct size, • Changes in left ventricular volumes and • Major adverse cardiac events (reinfarction, revascularization and death) were secondary endpoints.
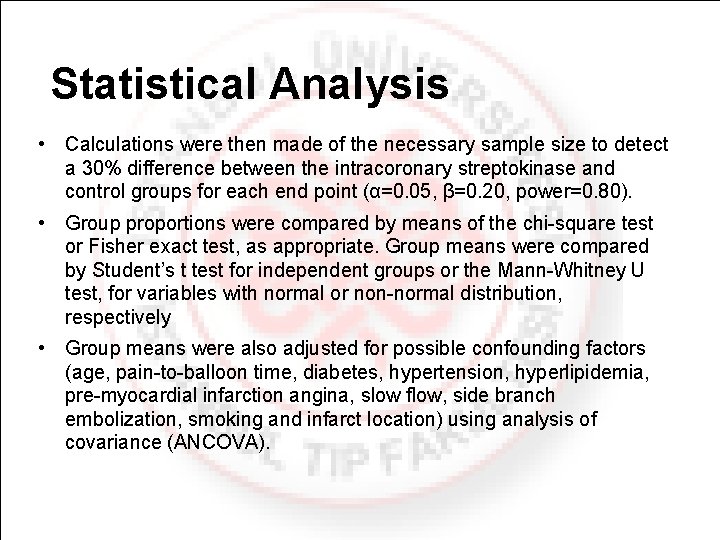
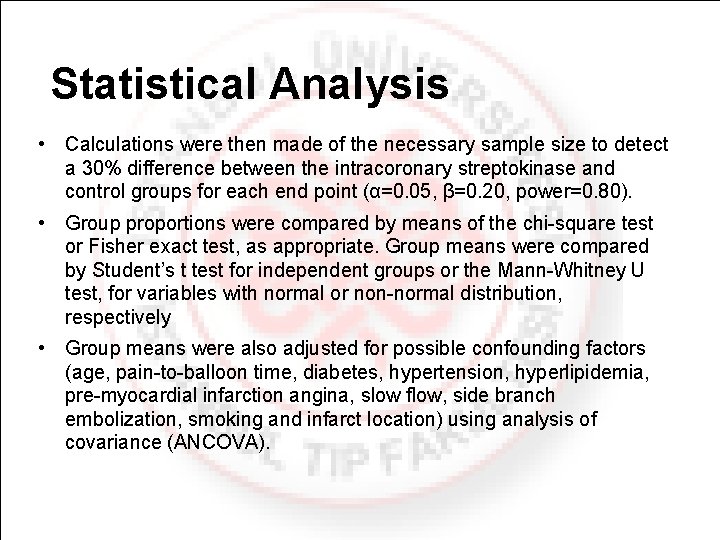
Statistical Analysis • Calculations were then made of the necessary sample size to detect a 30% difference between the intracoronary streptokinase and control groups for each end point (α=0. 05, β=0. 20, power=0. 80). • Group proportions were compared by means of the chi square test or Fisher exact test, as appropriate. Group means were compared by Student’s t test for independent groups or the Mann Whitney U test, for variables with normal or non normal distribution, respectively • Group means were also adjusted for possible confounding factors (age, pain to balloon time, diabetes, hypertension, hyperlipidemia, pre myocardial infarction angina, slow flow, side branch embolization, smoking and infarct location) using analysis of covariance (ANCOVA).
Results

Baseline Demographic and Clinical Characteristics. Intracoronary Streptokinase Group n: 21 Control Group n: 20 p (two tailed) 51. 4± 5. 7 52. 2± 10. 9 0. 79 21 19 0, 98 Smoking 17 (81%) 14 (70%) 0. 65 Diabetes Mellitus 2 (10%) 3 (16%) 0. 65 Hypertension 4 (19%) 7 (37%) 0. 20 Dyslipidemia 12 (57%) 14 (74%) 0. 27 History of preinfarction angina 5 (24%) 5 (26%) 0. 85 Anterior 14 (67%) 16 (80%) Non anterior 7 (33%) 4 (20%) 9. 1 ± 6. 5 10. 4 ± 7. 6 0, 61 15. 6 ± 10. 5 19 ± 9. 7 0. 18 Main characteristics Age (mean, yrs) Sex (male) Infarct localization Peak troponin T Initial ST elevation (mean, mm) 0. 54 Concomitant medications during PCI and in the Coronary Care Unit Aspirin 21 (100%) 20 (100%) 1 Beta Blocker 19 (90%) 18 (90%) 0. 96 LMWH 21 (100%) 20 (100%) 1 GP IIb/IIIa inhibitor 21 (100%) 20 (100%) 1 Clopidogrel 21 (100%) 20 (100%) 1 Statins 19 (90%) 18 (90%) 0. 96 Intravenous nitroglycerin 16 (76%) 12 (60%) 0. 44 ACE inhibitor 19 (90%) 16 (80%) 0. 61
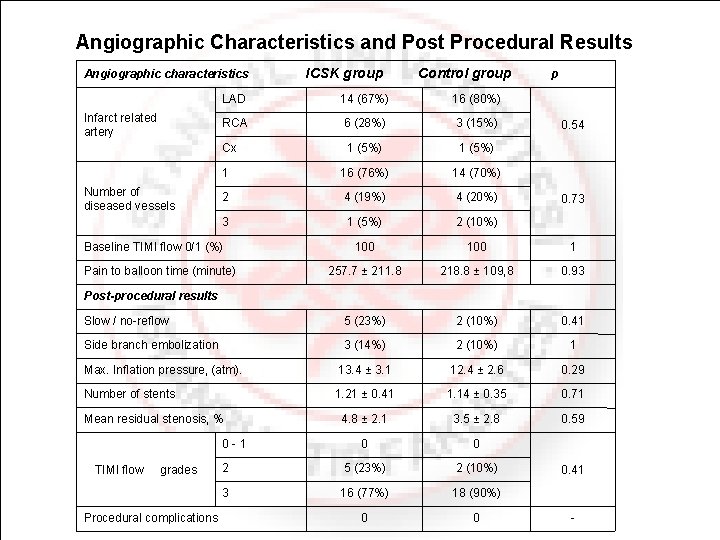
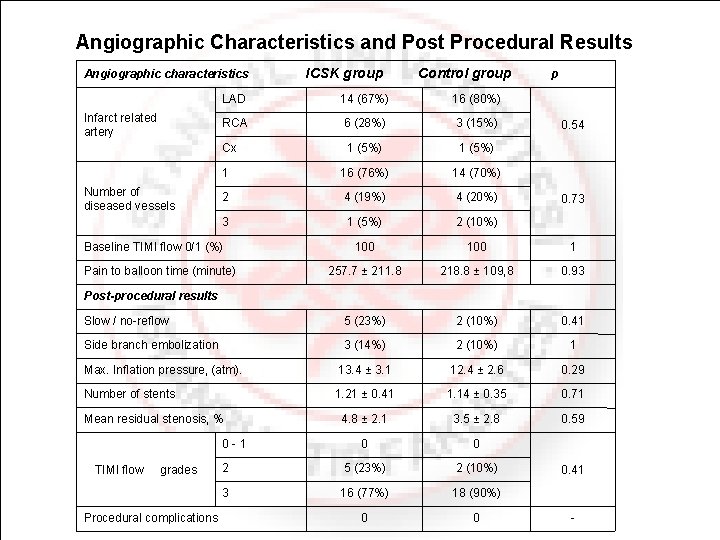
Angiographic Characteristics and Post Procedural Results Angiographic characteristics ICSK group Control group p LAD 14 (67%) 16 (80%) RCA 6 (28%) 3 (15%) Cx 1 (5%) 1 16 (76%) 14 (70%) 2 4 (19%) 4 (20%) 3 1 (5%) 2 (10%) 100 1 257. 7 ± 211. 8 218. 8 ± 109, 8 0. 93 Slow / no reflow 5 (23%) 2 (10%) 0. 41 Side branch embolization 3 (14%) 2 (10%) 1 Max. Inflation pressure, (atm). 13. 4 ± 3. 1 12. 4 ± 2. 6 0. 29 Number of stents 1. 21 ± 0. 41 1. 14 ± 0. 35 0. 71 4. 8 ± 2. 1 3. 5 ± 2. 8 0. 59 0 0 2 5 (23%) 2 (10%) 3 16 (77%) 18 (90%) 0 0 Infarct related artery Number of diseased vessels Baseline TIMI flow 0/1 (%) Pain to balloon time (minute) 0. 54 0. 73 Post-procedural results Mean residual stenosis, % 0 1 TIMI flow grades Procedural complications 0. 41
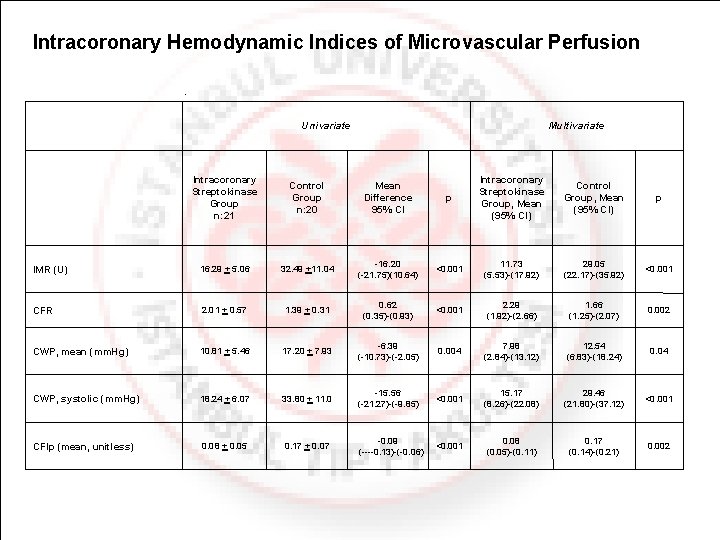
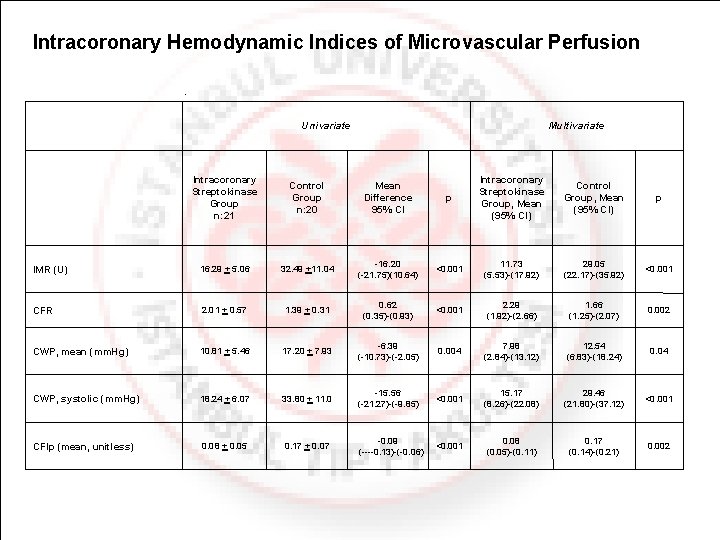
Intracoronary Hemodynamic Indices of Microvascular Perfusion Univariate Multivariate Intracoronary Streptokinase Group n: 21 Control Group n: 20 Mean Difference 95% CI p Intracoronary Streptokinase Group, Mean (95% CI) Control Group, Mean (95% CI) p IMR (U) 16. 29 + 5. 06 32. 49 +11. 04 16. 20 ( 21. 75)(10. 64) <0. 001 11. 73 (5. 53) (17. 92) 29. 05 (22. 17) (35. 92) <0. 001 CFR 2. 01 + 0. 57 1. 39 + 0. 31 0. 62 (0. 35) (0. 93) <0. 001 2. 29 (1. 92) (2. 66) 1. 66 (1. 25) (2. 07) 0. 002 CWP, mean (mm. Hg) 10. 81 + 5. 46 17. 20 + 7. 93 6. 39 ( 10. 73) ( 2. 05) 0. 004 7. 98 (2. 84) (13. 12) 12. 54 (6. 83) (18. 24) 0. 04 CWP, systolic (mm. Hg) 18. 24 + 6. 07 33. 80 + 11. 0 15. 56 ( 21. 27) ( 9. 85) <0. 001 15. 17 (8. 26) (22. 08) 29. 46 (21. 80) (37. 12) <0. 001 CFIp (mean, unitless) 0. 08 + 0. 05 0. 17 + 0. 07 0. 09 ( 0. 13) ( 0. 06) <0. 001 0. 08 (0. 05) (0. 11) 0. 17 (0. 14) (0. 21) 0. 002
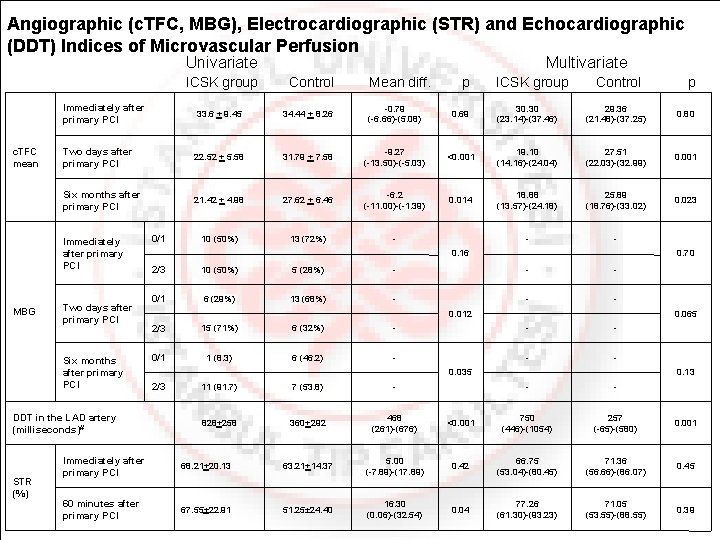
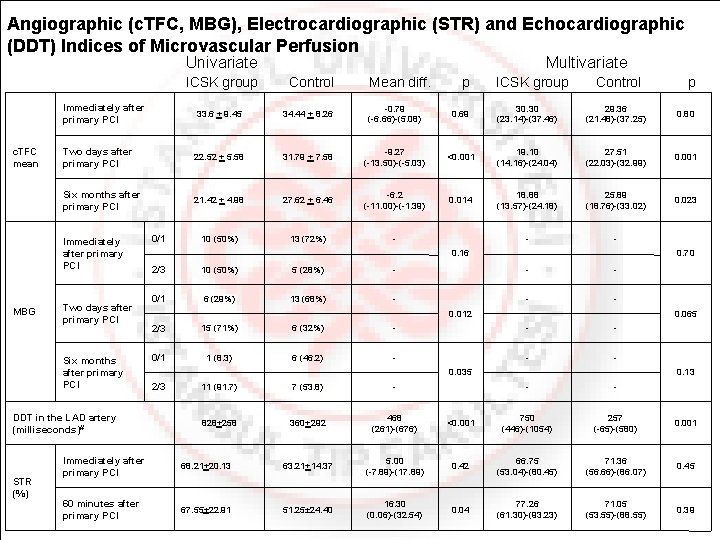
Angiographic (c. TFC, MBG), Electrocardiographic (STR) and Echocardiographic (DDT) Indices of Microvascular Perfusion Univariate ICSK group c. TFC mean Mean diff. p ICSK group Control p 33. 6 + 9. 45 34. 44 + 8. 26 0. 79 ( 6. 66) (5. 08) 0. 69 30. 30 (23. 14) (37. 46) 29. 36 (21. 48) (37. 25) 0. 80 Two days after primary PCI 22. 52 + 5. 58 31. 79 + 7. 58 9. 27 ( 13. 50) ( 5. 03) <0. 001 19. 10 (14. 16) (24. 04) 27. 51 (22. 03) (32. 99) 0. 001 Six months after primary PCI 21. 42 + 4. 98 27. 62 + 6. 46 6. 2 ( 11. 00) ( 1. 39) 0. 014 18. 88 (13. 57) (24. 18) 25. 89 (18. 76) (33. 02) 0. 023 10 (50%) 13 (72%) Two days after primary PCI Six months after primary PCI DDT in the LAD artery (milliseconds)# STR (%) Control Immediately after primary PCI MBG Multivariate 0/1 0. 16 0. 70 2/3 10 (50%) 5 (28%) 0/1 6 (29%) 13 (68%) 2/3 15 (71%) 6 (32%) 0/1 1 (8. 3) 6 (46. 2) 0. 012 0. 065 0. 035 2/3 11 (91. 7) 7 (53. 8) 828+258 360+292 468 (261) (676) 0. 13 <0. 001 750 (446) (1054) 257 ( 65) (580) 0. 001 Immediately after primary PCI 68. 21+20. 13 63. 21+14. 37 5. 00 ( 7. 89) (17. 89) 0. 42 66. 75 (53. 04) (80. 45) 71. 36 (56. 66) (86. 07) 0. 45 60 minutes after primary PCI 67. 55+22. 91 51. 25± 24. 40 16. 30 (0. 06) (32. 54) 0. 04 77. 26 (61. 30) (93. 23) 71. 05 (53. 55) (88. 55) 0. 39
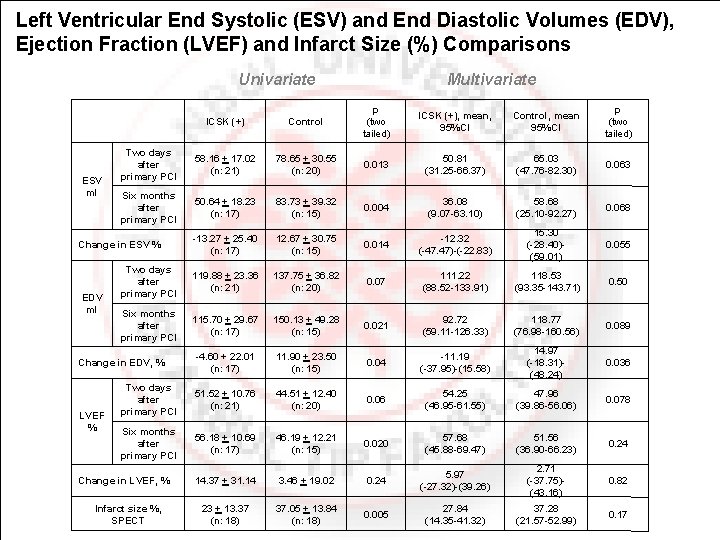
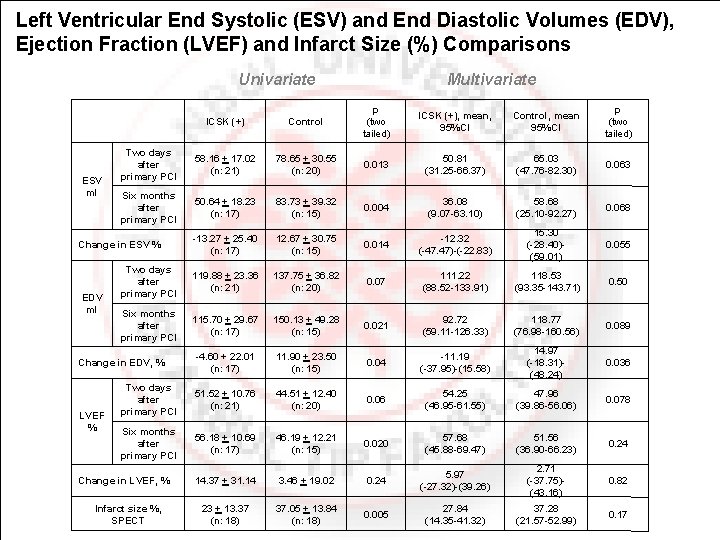
Left Ventricular End Systolic (ESV) and End Diastolic Volumes (EDV), Ejection Fraction (LVEF) and Infarct Size (%) Comparisons Univariate ESV ml ICSK (+) Control p (two tailed) ICSK (+), mean, 95%CI Control, mean 95%CI p (two tailed) Two days after primary PCI 58. 16 + 17. 02 (n: 21) 78. 65 + 30. 55 (n: 20) 0. 013 50. 81 (31. 25 66. 37) 65. 03 (47. 76 82. 30) 0. 063 Six months after primary PCI 50. 64 + 18. 23 (n: 17) 83. 73 + 39. 32 (n: 15) 0. 004 36. 08 (9. 07 63. 10) 58. 68 (25. 10 92. 27) 0. 068 13. 27 + 25. 40 (n: 17) 12. 67 + 30. 75 (n: 15) 0. 014 12. 32 ( 47. 47) ( 22. 83) 15. 30 ( 28. 40) (59. 01) 0. 055 Two days after primary PCI 119. 88 + 23. 36 (n: 21) 137. 75 + 36. 82 (n: 20) 0. 07 111. 22 (88. 52 133. 91) 118. 53 (93. 35 143. 71) 0. 50 Six months after primary PCI 115. 70 + 29. 67 (n: 17) 150. 13 + 49. 28 (n: 15) 0. 021 92. 72 (59. 11 126. 33) 118. 77 (76. 98 160. 56) 0. 089 4. 60 + 22. 01 (n: 17) 11. 90 + 23. 50 (n: 15) 0. 04 11. 19 ( 37. 95) (15. 58) 14. 97 ( 18. 31) (48. 24) 0. 036 Two days after primary PCI 51. 52 + 10. 76 (n: 21) 44. 51 + 12. 40 (n: 20) 0. 06 54. 25 (46. 95 61. 55) 47. 96 (39. 86 56. 06) 0. 078 Six months after primary PCI 56. 18 + 10. 69 (n: 17) 46. 19 + 12. 21 (n: 15) 0. 020 57. 68 (45. 88 69. 47) 51. 56 (36. 90 66. 23) 0. 24 14. 37 + 31. 14 3. 46 + 19. 02 0. 24 5. 97 ( 27. 32) (39. 26) 2. 71 ( 37. 75) (43. 16) 0. 82 23 + 13. 37 (n: 18) 37. 05 + 13. 84 (n: 18) 0. 005 27. 84 (14. 35 41. 32) 37. 28 (21. 57 52. 99) 0. 17 Change in ESV % EDV ml Change in EDV, % LVEF % Multivariate Change in LVEF, % Infarct size %, SPECT
Comments and Conclusions Early phase results: • In this pilot trial, low dose intracoronary streptokinase administration immediately following primary PCI was compared with standard primary PCI without use of intracoronary streptokinase. • Almost all indices of microvascular perfusion concordantly pointed out that use of intracoronary streptokinase immediately after primary PCI yields better perfusion at the microvascular level.
Comments and Conclusions 2 Late term results • At six months, there was no significant difference between the two study groups with regards to left ventricular size or function and infarct size, although there were some trends favoring the streptokinase group. • The trial was not originally planned to be large enough to detect differences in long term outcome, and indeed enrollment was terminated early based on the midterm data on microvascular perfusion. • Since trends in favor of the intracoronary streptokinase group were detected, it is possible that the study was underpowered for these analyses.
Comments and Conclusions 3 • The finding of the current study supports the in situ formed (autochthonous) microvascular thrombus hypothesis and pointed out that this thrombus should be taken into consideration for achieving more efficient reperfusion at microvascular level during primary PCI. • The results of the study should be confirmed by a larger randomized study before applying this treatment modality in daily cardiology practice.
 Thrombolytic agents list
Thrombolytic agents list Wirchow trias
Wirchow trias Streptokinase mechanism of action
Streptokinase mechanism of action After me after me after me
After me after me after me If any man come after me
If any man come after me Percutaneous balloon pericardiotomy
Percutaneous balloon pericardiotomy Pleural effusion ellis curve
Pleural effusion ellis curve Indication for cholecystectomy
Indication for cholecystectomy Percutaneous umbilical blood sampling
Percutaneous umbilical blood sampling Percutaneous image-guided lumbar decompression
Percutaneous image-guided lumbar decompression Common bile duct diameter
Common bile duct diameter Andicator
Andicator Classification of antianginal drugs
Classification of antianginal drugs Coronary artery disease
Coronary artery disease Mesa coronary calcium score
Mesa coronary calcium score Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Unlocking of knee joint
Unlocking of knee joint Course of right coronary artery
Course of right coronary artery Sinus of venae cavae
Sinus of venae cavae Lig hepatoduodenal
Lig hepatoduodenal Qfr coronary
Qfr coronary Coronary personality
Coronary personality