Comparative Effectiveness of Percutaneous Coronary Interventions and Coronary















- Slides: 66

Comparative Effectiveness of Percutaneous Coronary Interventions and Coronary Artery Bypass Grafting for Coronary Artery Disease January 31, 2006 Dena Bravata, MD, MS and Mark Hlatky, MD

Today’s Talk Background on the procedures Methodological issues Results Conclusions and next steps

What is coronary artery disease? A narrowing of the coronary arteries that prevents adequate blood supply to the heart muscle. Usually caused by atherosclerosis, it may progress to the point where the heart muscle is damaged due to lack of blood supply. Such damage may result in infarction, arrhythmias, and heart failure.
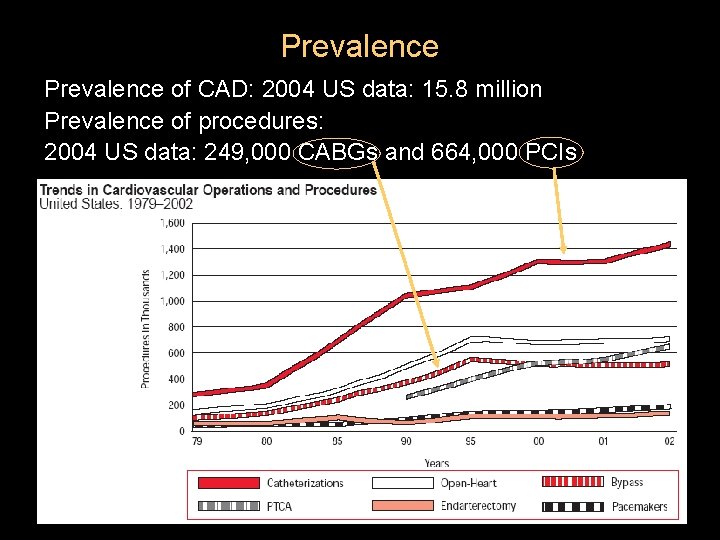
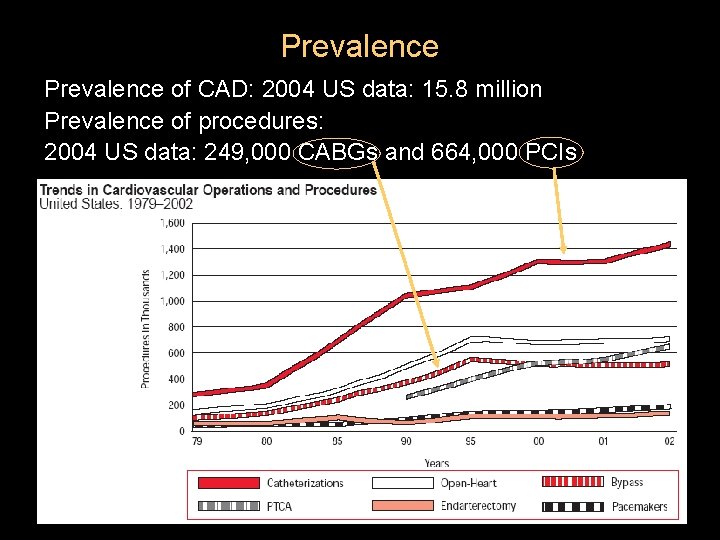
Prevalence of CAD: 2004 US data: 15. 8 million Prevalence of procedures: 2004 US data: 249, 000 CABGs and 664, 000 PCIs
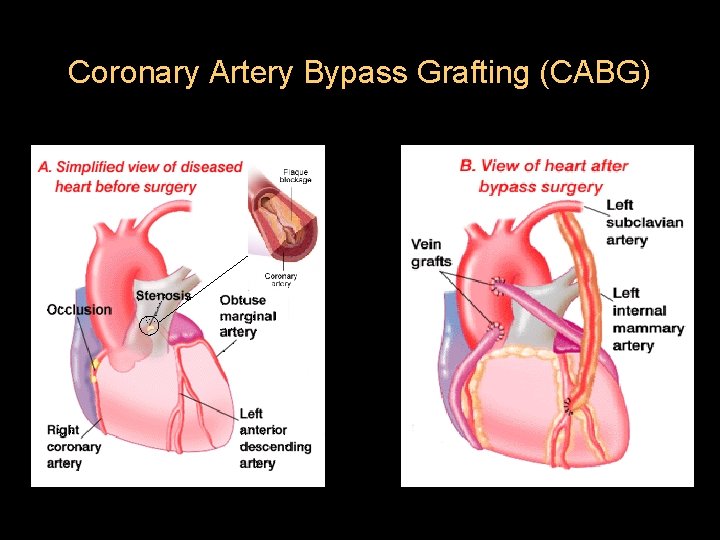
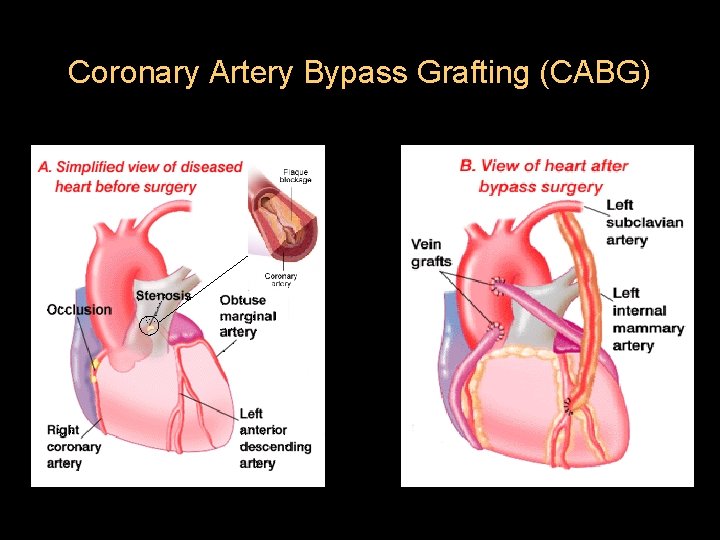
Coronary Artery Bypass Grafting (CABG)
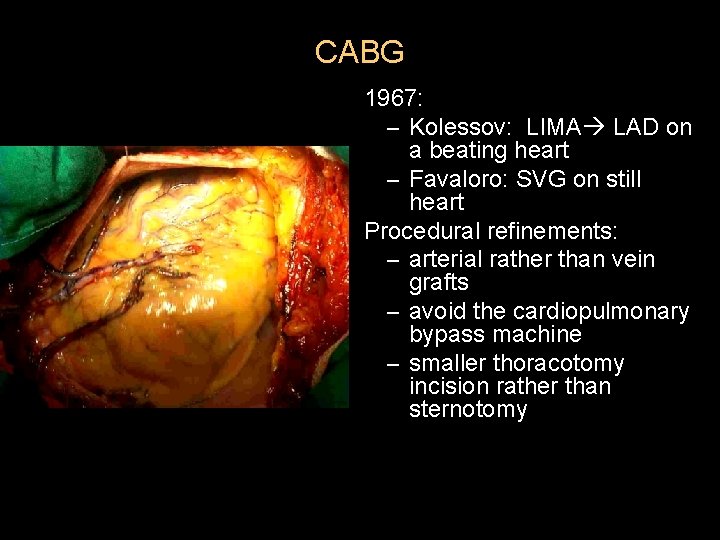
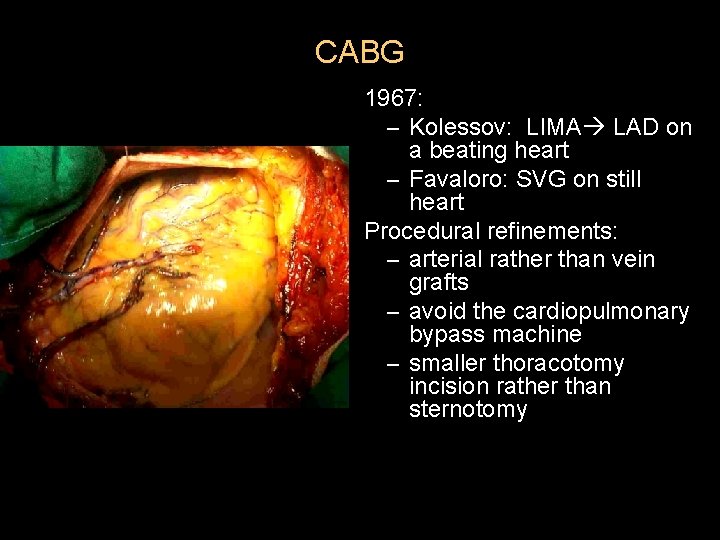
CABG 1967: – Kolessov: LIMA LAD on a beating heart – Favaloro: SVG on still heart Procedural refinements: – arterial rather than vein grafts – avoid the cardiopulmonary bypass machine – smaller thoracotomy incision rather than sternotomy
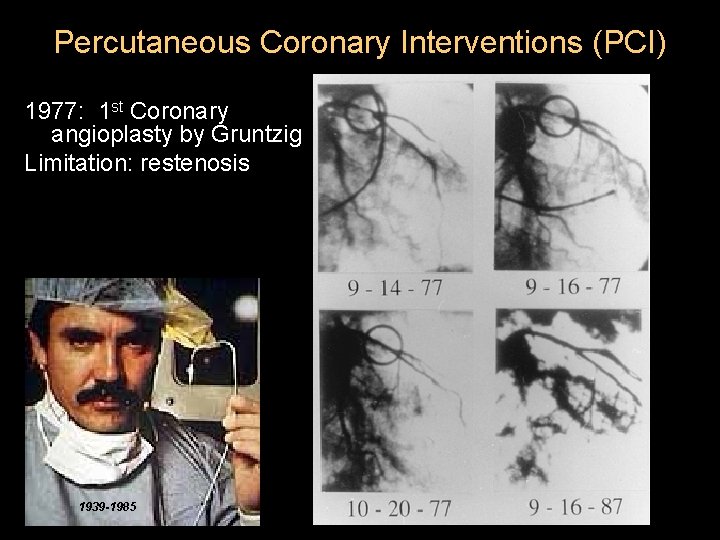
Percutaneous Coronary Interventions (PCI) 1977: 1 st Coronary angioplasty by Gruntzig Limitation: restenosis 1939 -1985
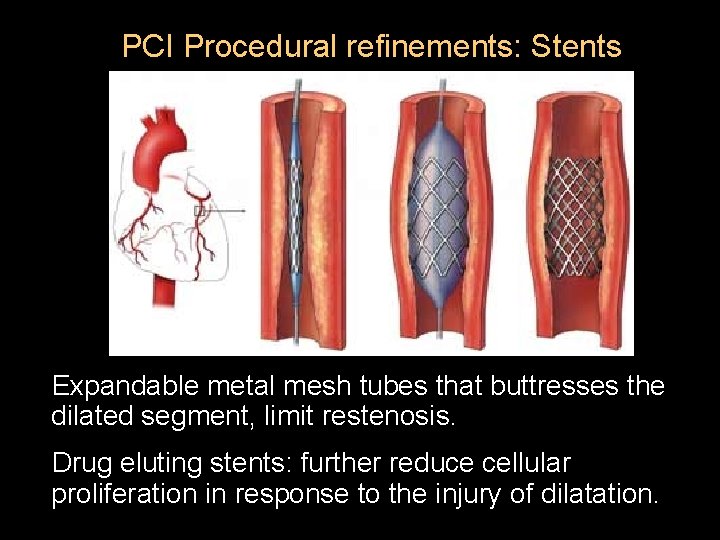
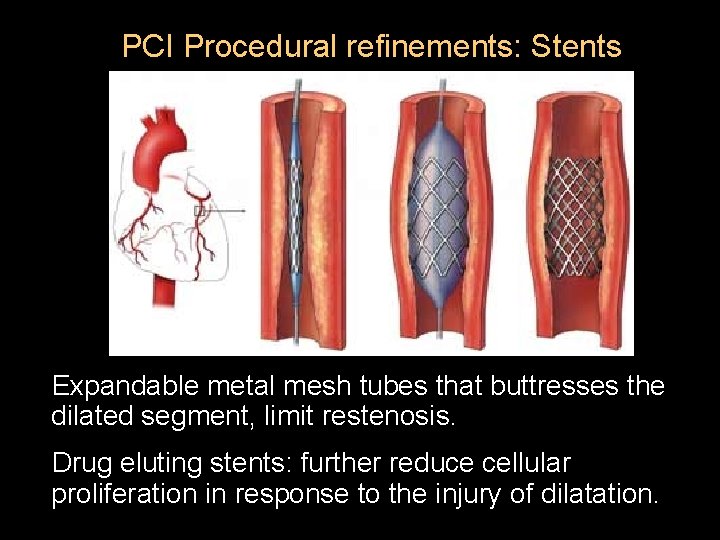
PCI Procedural refinements: Stents Expandable metal mesh tubes that buttresses the dilated segment, limit restenosis. Drug eluting stents: further reduce cellular proliferation in response to the injury of dilatation.
Which procedure is best?
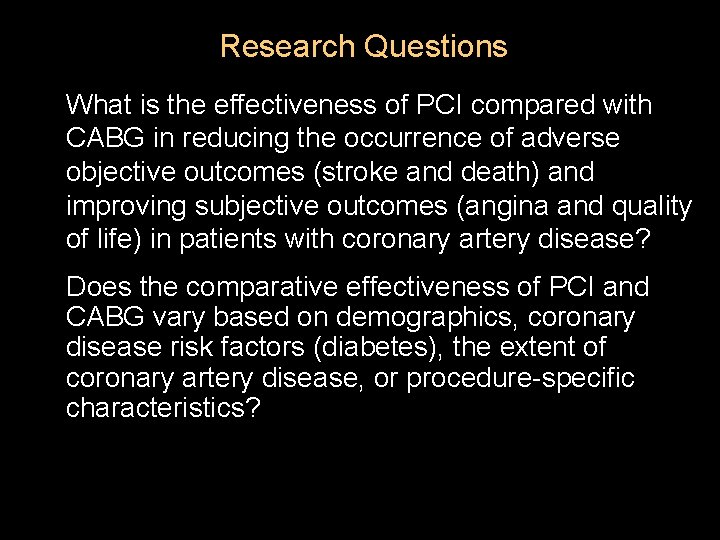
Research Questions What is the effectiveness of PCI compared with CABG in reducing the occurrence of adverse objective outcomes (stroke and death) and improving subjective outcomes (angina and quality of life) in patients with coronary artery disease? Does the comparative effectiveness of PCI and CABG vary based on demographics, coronary disease risk factors (diabetes), the extent of coronary artery disease, or procedure-specific characteristics?
Max is a 79 yo man with well controlled HTN, hypercholesterolemia, afib, and diet controlled-DM who had a vfib arrest in the setting of an MI. His angiogram showed proximal vessel LAD and 3 -vessel CAD. He was stabilized, did well, and given the option of PCI or CABG. His UCSF and Stanford doctors reviewed the evidence with him and his family…
Today’s Talk Background on the procedures Methodological issues Results Conclusions and next steps
Overview of Methodologic Approach l l l l Our 1 st MMA project: slight procedural differences from other EPC work Develop a REALLY (no kidding) expert team* Systematic literature search for RCTs Limited/selected searches for observational studies for generalizability Quality evaluations of primary literature Data extraction: which time points? Data synthesis: which outcome metric?

Literature Search for RCTs l l l Literature searches – 1/1966 to 8/2006 – Strategy for each source developed through clinician/librarian collaboration MEDLINE: 1576 citations Cochrane: 54 citations Embase: 65 citations Additional searches (experts): 7 citations
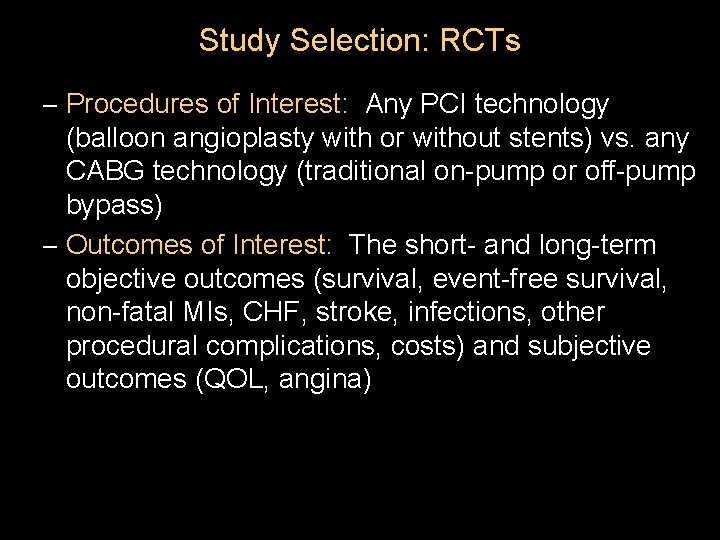
Study Selection: RCTs – Procedures of Interest: Any PCI technology (balloon angioplasty with or without stents) vs. any CABG technology (traditional on-pump or off-pump bypass) – Outcomes of Interest: The short- and long-term objective outcomes (survival, event-free survival, non-fatal MIs, CHF, stroke, infections, other procedural complications, costs) and subjective outcomes (QOL, angina)

Synthesizing Survival Curves Digitize. It Software
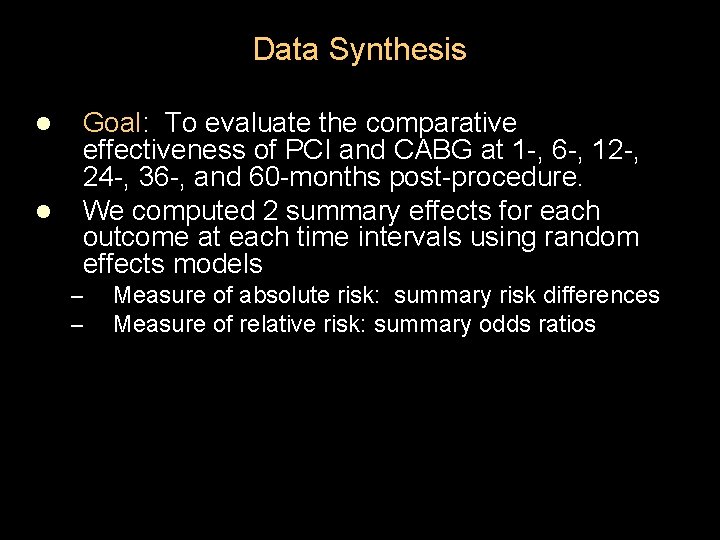
Data Synthesis l l Goal: To evaluate the comparative effectiveness of PCI and CABG at 1 -, 6 -, 12 -, 24 -, 36 -, and 60 -months post-procedure. We computed 2 summary effects for each outcome at each time intervals using random effects models – – Measure of absolute risk: summary risk differences Measure of relative risk: summary odds ratios
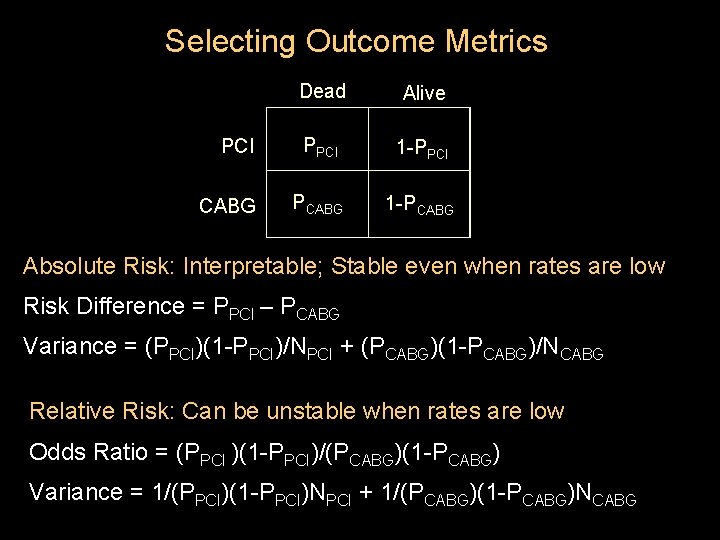
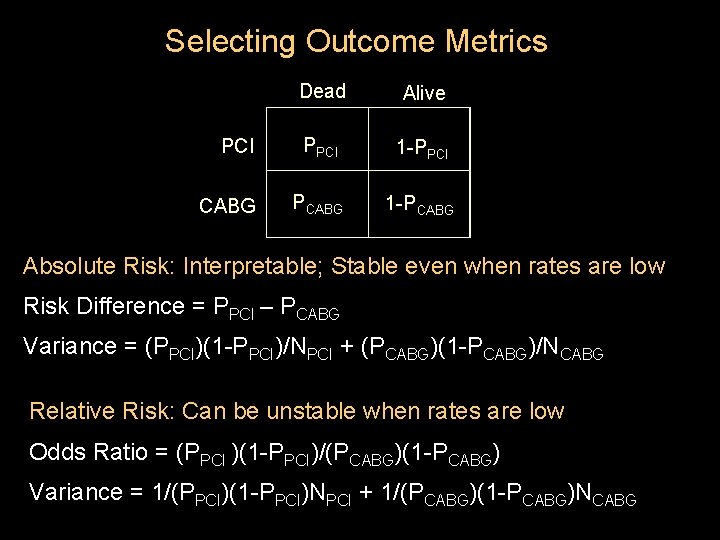
Selecting Outcome Metrics Dead Alive PCI PPCI 1 -PPCI CABG PCABG 1 -PCABG Absolute Risk: Interpretable; Stable even when rates are low Risk Difference = PPCI – PCABG Variance = (PPCI)(1 -PPCI)/NPCI + (PCABG)(1 -PCABG)/NCABG Relative Risk: Can be unstable when rates are low Odds Ratio = (PPCI )(1 -PPCI)/(PCABG)(1 -PCABG) Variance = 1/(PPCI)(1 -PPCI)NPCI + 1/(PCABG)(1 -PCABG)NCABG
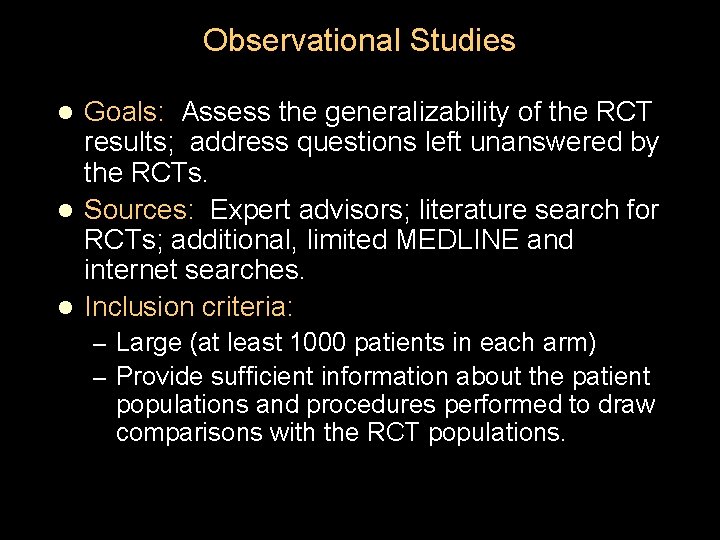
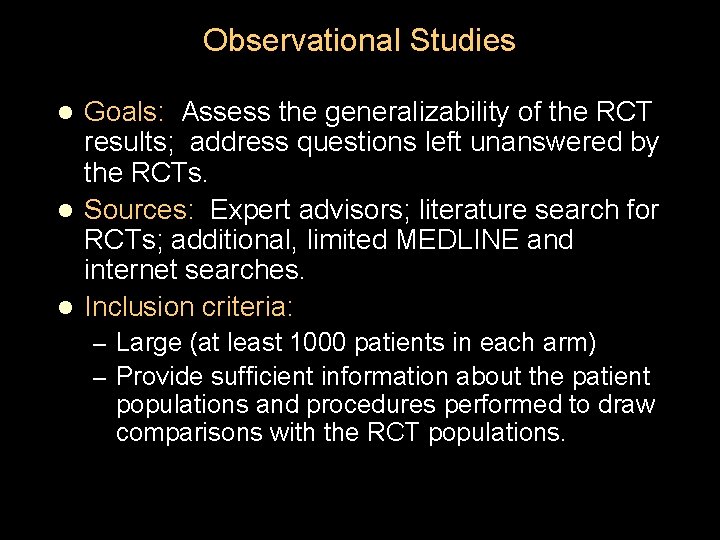
Observational Studies Goals: Assess the generalizability of the RCT results; address questions left unanswered by the RCTs. l Sources: Expert advisors; literature search for RCTs; additional, limited MEDLINE and internet searches. l Inclusion criteria: l – Large (at least 1000 patients in each arm) – Provide sufficient information about the patient populations and procedures performed to draw comparisons with the RCT populations.
Today’s Talk Background on the procedures Methodological issues Results Conclusions and next steps
General Description of the Included Studies RCTs: 113 included articles, 22 unique RCTs (See handout) 9, 640 patients: 4969 PCI, 4894 CABG Most were conducted in Europe/UK Only 3 trials performed in the US High quality trials except for Seoul (? randomized) Observational Studies: 94 included articles, 10 registries Generally similar populations to the RCT populations (fewer women, more unstable angina patients than in the RCTs)
RCTs: Patient Characteristics Age: Mean 61 years Gender: 27% women Race/Ethnicity: Overwhelmingly European ancestry Typical CAD patients who can receive either intervention (not entire CAD spectrum): 20% diabetes, 50% hypertension, 50% chol Among multi-vessel disease (MVD) studies: most patients had 2 -vessel rather than 3 -vessel disease 40% prior MI, low rates of CHF, good LV function Very few patients with left main or SVD
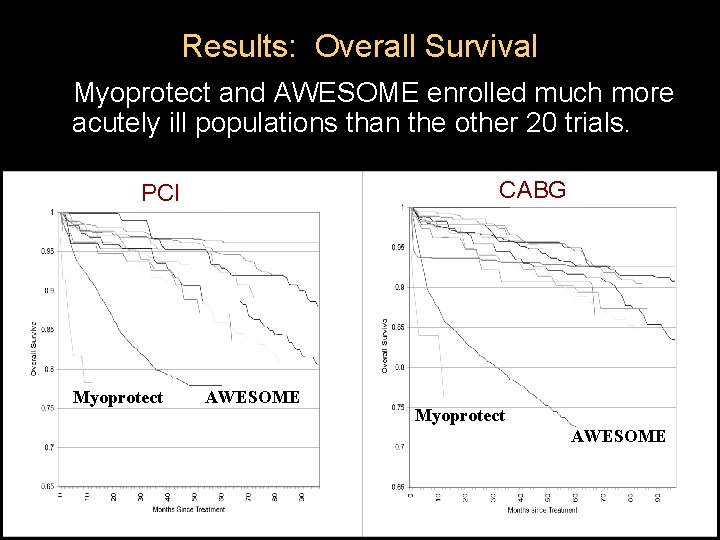
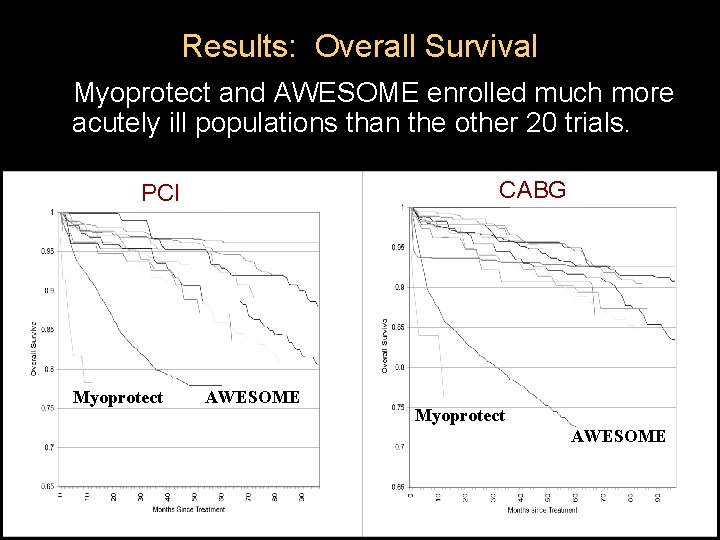
Results: Overall Survival Myoprotect and AWESOME enrolled much more acutely ill populations than the other 20 trials. CABG PCI Myoprotect AWESOME
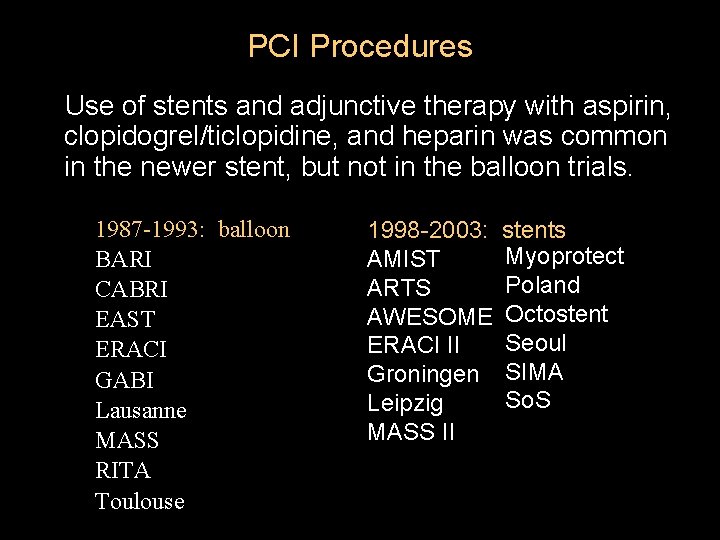
PCI Procedures Use of stents and adjunctive therapy with aspirin, clopidogrel/ticlopidine, and heparin was common in the newer stent, but not in the balloon trials. 1987 -1993: balloon BARI CABRI EAST ERACI GABI Lausanne MASS RITA Toulouse 1998 -2003: AMIST ARTS AWESOME ERACI II Groningen Leipzig MASS II stents Myoprotect Poland Octostent Seoul SIMA So. S

CABG Procedures LIMA was frequently employed, especially in more recent trials. Few CABGs were performed off-pump, although a few studies used minimally invasive direct coronary artery bypass (MIDCAB) incisions and beating heart operations in patients with singlevessel LAD disease. In patients with MVD, surgeons generally bypassed more vessels than angioplasty operators dilated.
Comparative Effectiveness Results Procedural outcomes l Long-term outcomes l Subgroup analyses l

Procedural Survival (Risk Difference) Heterogeneity Statistics: Q-value 20. 3, P-value 0. 5; I-squared 0. 000. Procedural mortality rare for both procedures; no significant difference between them.
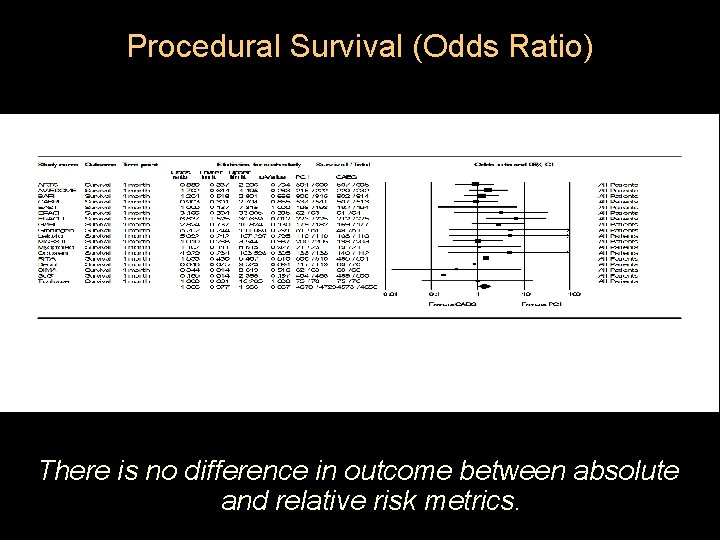
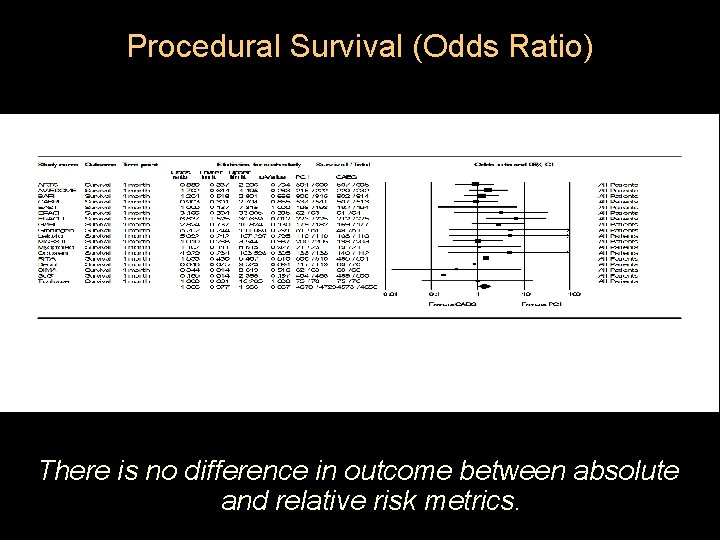
Procedural Survival (Odds Ratio) There is no difference in outcome between absolute and relative risk metrics.
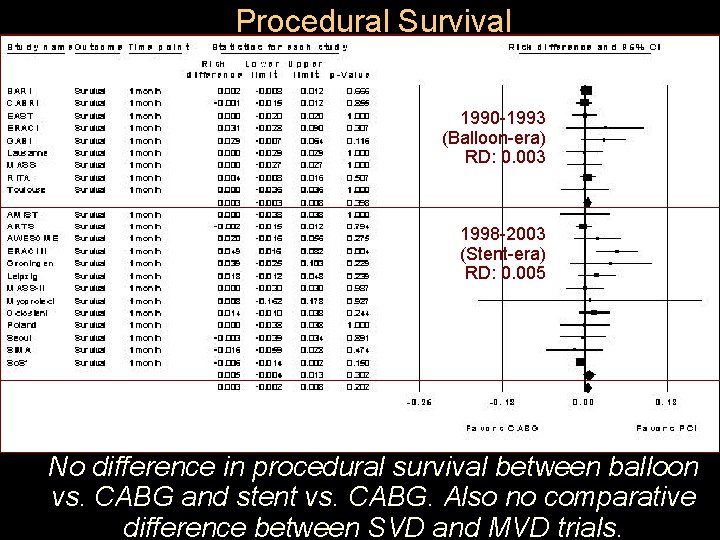
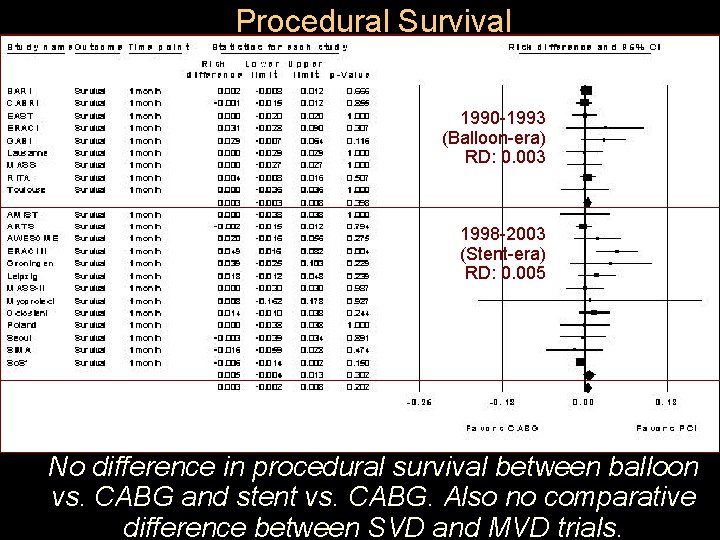
Procedural Survival 1990 -1993 (Balloon-era) RD: 0. 003 1998 -2003 (Stent-era) RD: 0. 005 No difference in procedural survival between balloon vs. CABG and stent vs. CABG. Also no comparative difference between SVD and MVD trials.
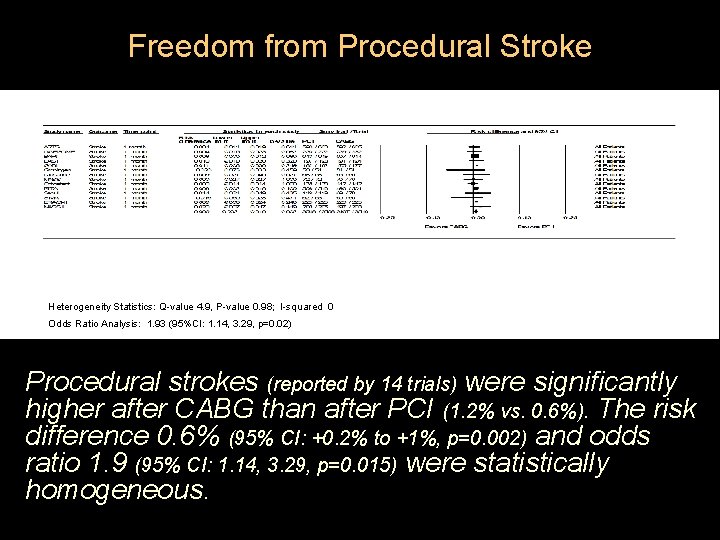
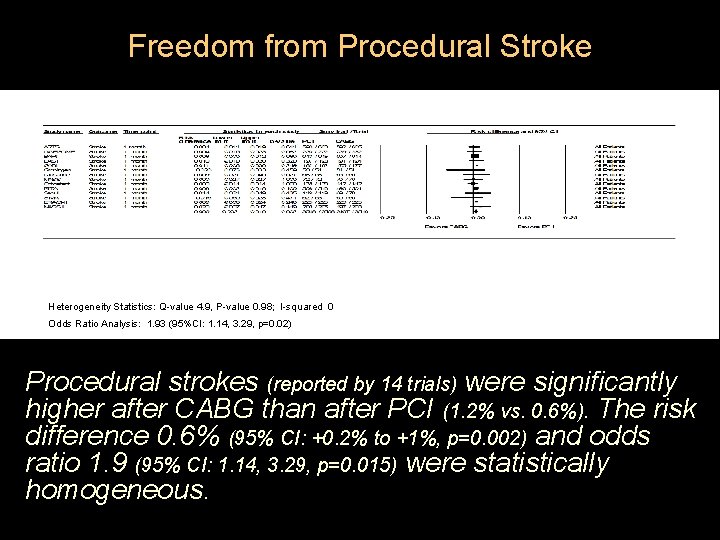
Freedom from Procedural Stroke Heterogeneity Statistics: Q-value 4. 9, P-value 0. 98; I-squared 0 Odds Ratio Analysis: 1. 93 (95%CI: 1. 14, 3. 29, p=0. 02) Procedural strokes (reported by 14 trials) were significantly higher after CABG than after PCI (1. 2% vs. 0. 6%). The risk difference 0. 6% (95% CI: +0. 2% to +1%, p=0. 002) and odds ratio 1. 9 (95% CI: 1. 14, 3. 29, p=0. 015) were statistically homogeneous.
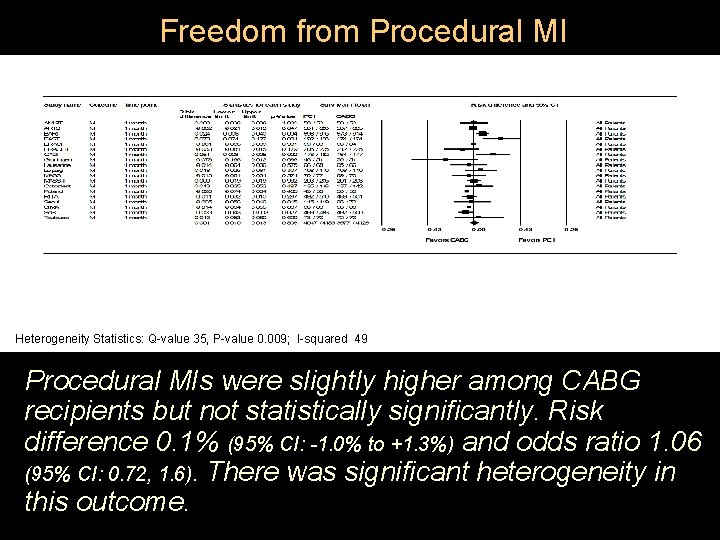
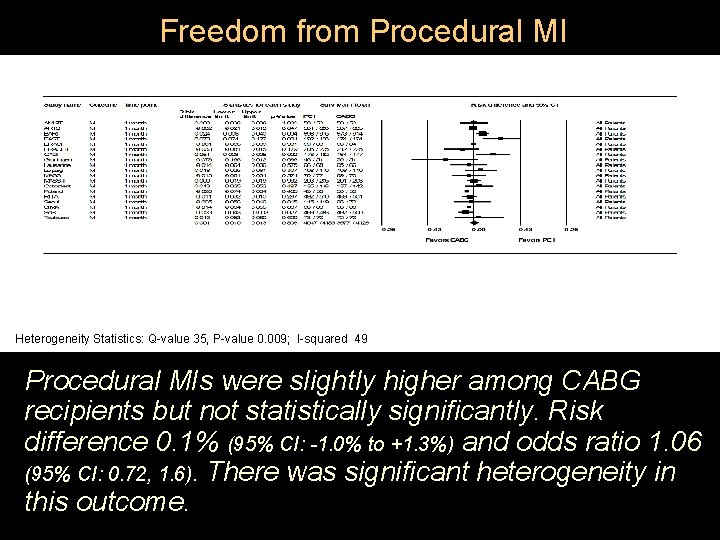
Freedom from Procedural MI Heterogeneity Statistics: Q-value 35, P-value 0. 009; I-squared 49 Procedural MIs were slightly higher among CABG recipients but not statistically significantly. Risk difference 0. 1% (95% CI: -1. 0% to +1. 3%) and odds ratio 1. 06 (95% CI: 0. 72, 1. 6). There was significant heterogeneity in this outcome.
Generalizability of the Procedural Outcomes: Observational Studies l Procedural risk in RCTs was lower overall than in the large registries. – Society of Thoracic Surgeons: operative mortality 3. 2% 2. 2% (1995 2005) despite patients of higher risk profiles – Hospital Corp. of America (1999 -2002): procedural mortality was 1. 25% for PCI vs 2. 63% for CABG and that mortality fell for both over the interval studied. l Potential explanation: rigorous RCT selection of patient, institutions, and operators

Comparative Effectiveness Results Procedural outcomes l Long-term outcomes l Subgroup analyses l
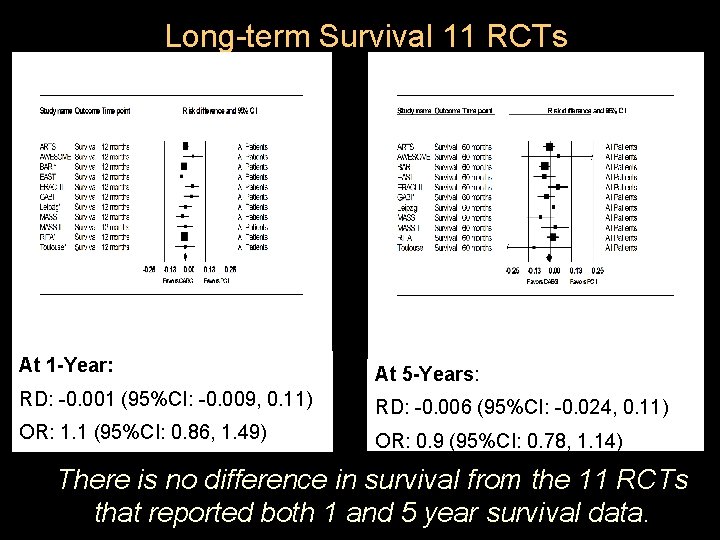
Long Term Survival l Overall survival across all randomized trials did not differ significantly between CABG and PCI between one and five years of follow-up: Risk difference at each time point was less than 1%. (See handout. ) l Risk difference between PCI and CABG was smaller in the more recent stent trials. Caveat: recent trials included more patients with singlevessel LAD disease and had shorter follow-up.
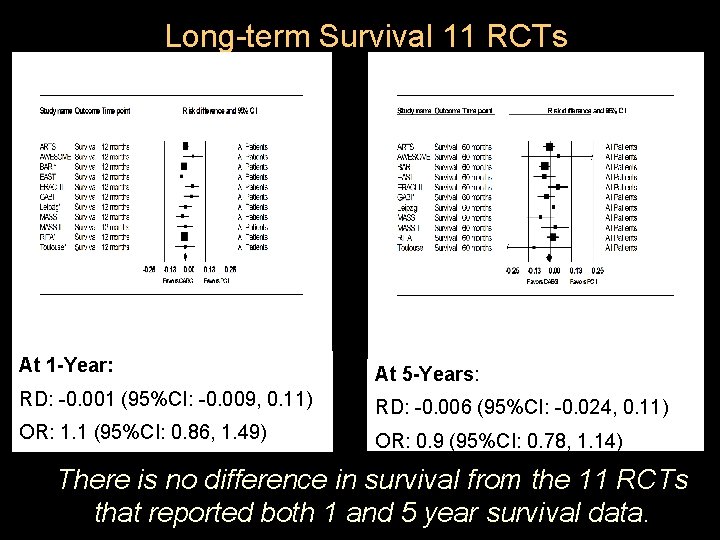
Long-term Survival 11 RCTs At 1 -Year: At 5 -Years: RD: -0. 001 (95%CI: -0. 009, 0. 11) RD: -0. 006 (95%CI: -0. 024, 0. 11) OR: 1. 1 (95%CI: 0. 86, 1. 49) OR: 0. 9 (95%CI: 0. 78, 1. 14) There is no difference in survival from the 11 RCTs that reported both 1 and 5 year survival data.

Single-vessel vs. Multi-vessel Disease l 7 trials proximal LAD, 15 trials MVD l No statistically significant differences in comparative survival at any time post-procedure between SVD and MVD trials; however: – SVD-LAD trials: survival was 1% greater for CABG recipients (95%CI: -5% to +2%) among balloon trials and was 0. 1% greater for PCI recipients (95%CI: -4% to +4%) among stent trials. – MVD trials: survival 0. 6% greater for CABG recipients (95%CI: -1. 5% to +0. 4%) for balloon trials but was 1. 4% greater for PCI recipients (95% CI: -1% to +3. 8%) for the stent trials.
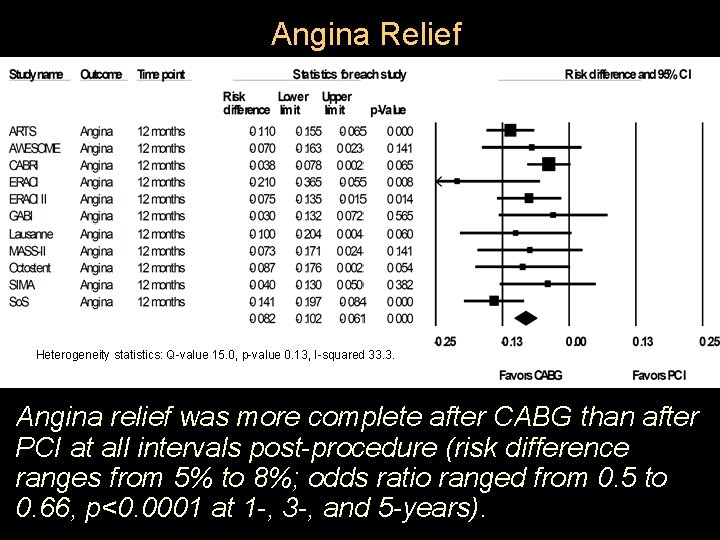
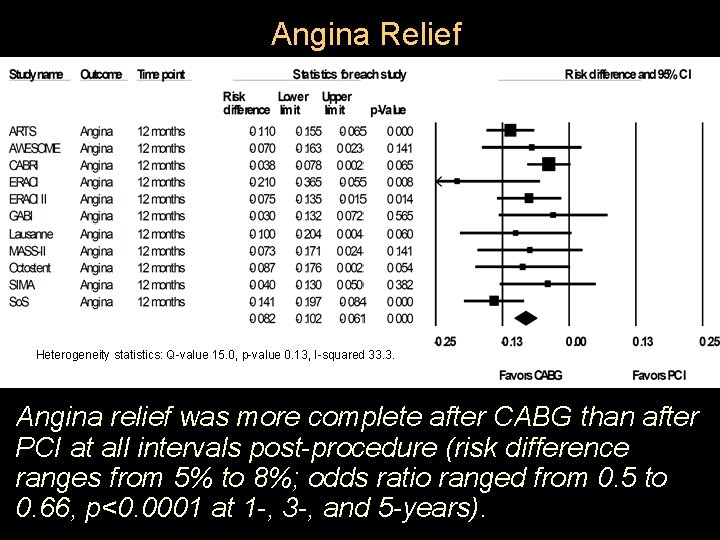
Angina Relief Heterogeneity statistics: Q-value 15. 0, p-value 0. 13, I-squared 33. 3. Angina relief was more complete after CABG than after PCI at all intervals post-procedure (risk difference ranges from 5% to 8%; odds ratio ranged from 0. 5 to 0. 66, p<0. 0001 at 1 -, 3 -, and 5 -years).
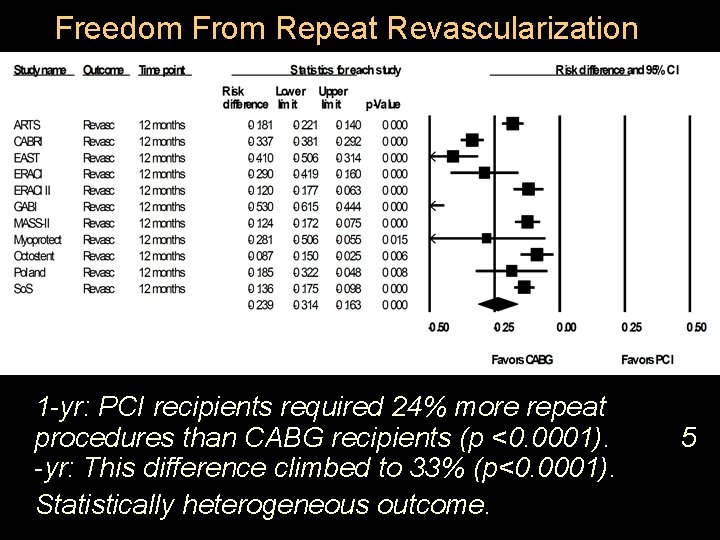
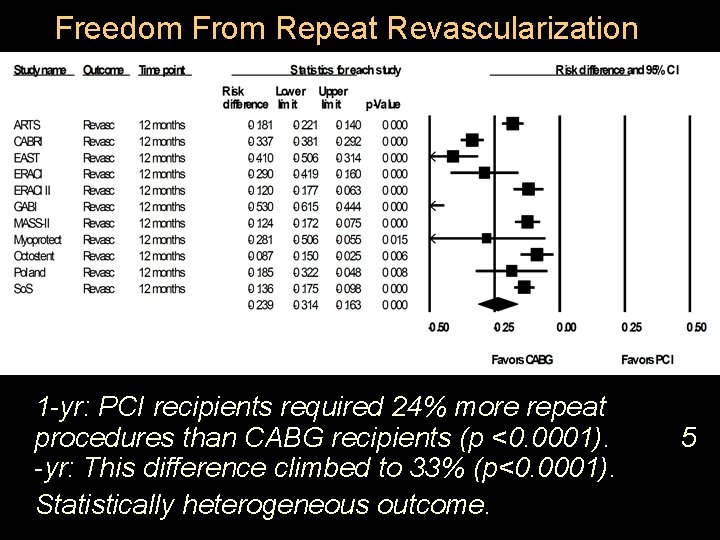
Freedom From Repeat Revascularization 1 -yr: PCI recipients required 24% more repeat procedures than CABG recipients (p <0. 0001). -yr: This difference climbed to 33% (p<0. 0001). Statistically heterogeneous outcome. 5
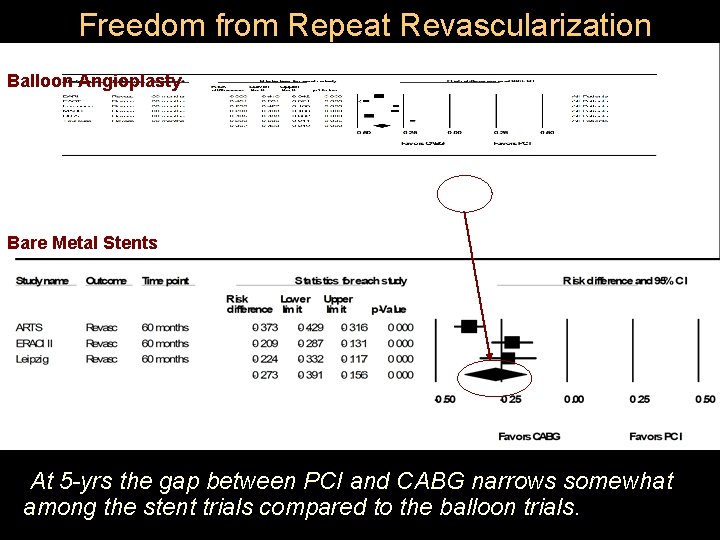
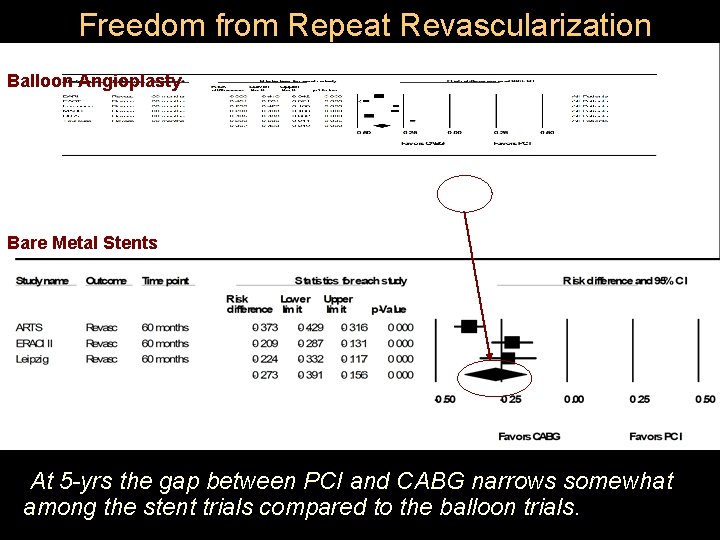
Freedom from Repeat Revascularization Balloon Angioplasty Bare Metal Stents At 5 -yrs the gap between PCI and CABG narrows somewhat among the stent trials compared to the balloon trials.

Post-procedure MI 10 studies reported MIs during follow-up l Between 1 and 5 yrs post-procedure, the MI rate increased among all patients, but at a somewhat higher rate for PCI recipients. l However, the risk differences were small (less than 1%) (odds ratio ranged from 0. 87 to 0. 92) and did not achieve statistical significance. l
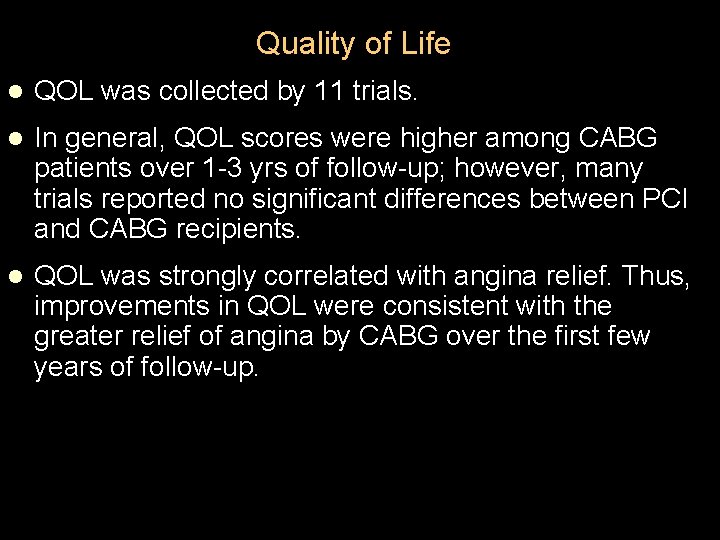
Quality of Life l QOL was collected by 11 trials. l In general, QOL scores were higher among CABG patients over 1 -3 yrs of follow-up; however, many trials reported no significant differences between PCI and CABG recipients. l QOL was strongly correlated with angina relief. Thus, improvements in QOL were consistent with the greater relief of angina by CABG over the first few years of follow-up.
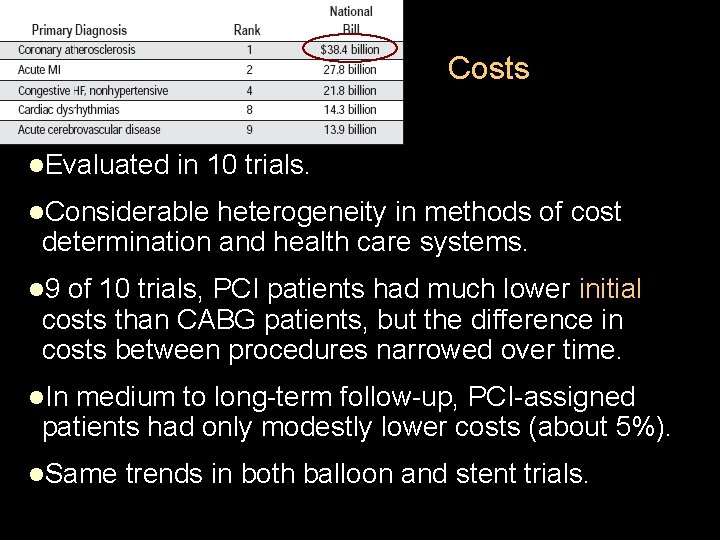
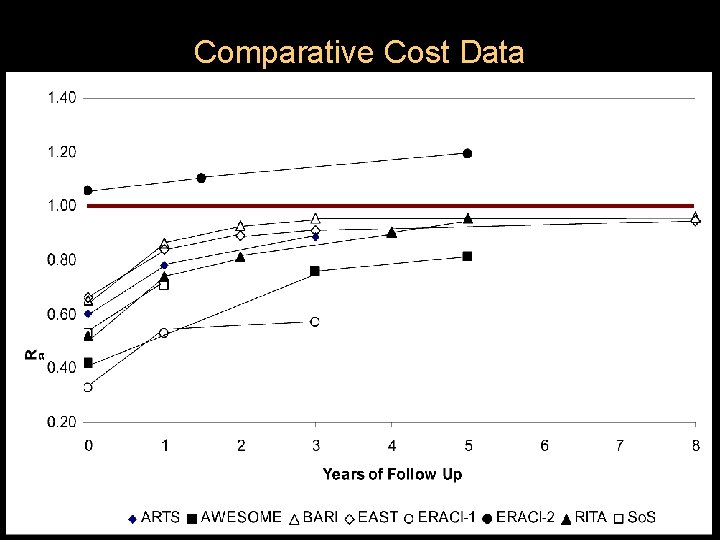
Costs l. Evaluated in 10 trials. l. Considerable heterogeneity in methods of cost determination and health care systems. l 9 of 10 trials, PCI patients had much lower initial costs than CABG patients, but the difference in costs between procedures narrowed over time. l. In medium to long-term follow-up, PCI-assigned patients had only modestly lower costs (about 5%). l. Same trends in both balloon and stent trials.
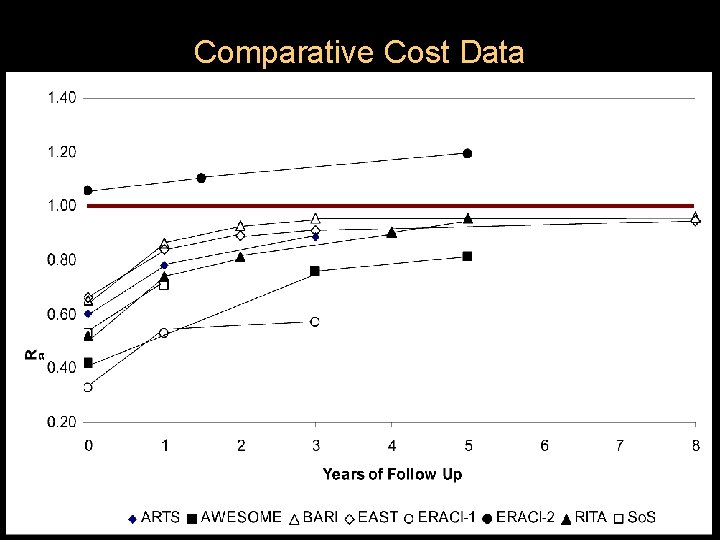
Comparative Cost Data
Comparative Effectiveness Results Procedural outcomes l Long-term outcomes l Subgroup analyses l
Max is a 79 yo man with well controlled HTN, hypercholesterolemia, afib, and diet controlled-DM…knowing about the comparative effectiveness of PCI and CABG by key subgroups would help his decision making…
Issues in Subgroup Analyses Few studies reported key outcomes for subgroups of interest l Heterogeneity in the outcome metric reported (relative risk reduction vs absolute risk differences) l Lower power statistic: the common test strategy of treatment by interaction p-values l

Outcomes in Key Subgroups: Age l All RCTs -Very few patients 75 yrs+ were enrolled. -There were more procedural complications in the older patients, especially stroke. l Outcomes by age evaluated in BARI, AWESOME, and pooled stent trials (ARTS, ERACI-II, MASS-II, So. S) -BARI: patients aged 65 yrs+ had lower overall survival than younger patients. Risk difference at 7 yrs was larger in the older patients (4. 7% risk difference; CABG survival 78. 7% vs. PCI 74. 0%) than younger patients (2. 8% risk difference; CABG 88. 1% vs. PCI 85. 3%).

Outcomes in Key Subgroups: Age Pooled stent trials: higher 1 -yr incidence of death, MI and stroke among patients aged 65 yrs+ compared with younger patients. Mortality was lower after CABG in the younger patients, and was lower after PCI in the older patients, although there was no statistically significant evidence of a differential treatment effect by age (age by treatment covariate interaction test).

Outcomes in Key Subgroups: Gender outcomes reported for BARI, So. S, pooled stent trials BARI: Women had lower overall survival, but only at 7 years. The risk difference between PCI and CABG was similar in women (3. 4% risk difference: 82. 6% CABG vs. 79. 2% PCI) and in men (3. 5% risk difference: 85. 1% CABG vs. 81. 6% PCI). So. S trial: Women had lower QOL at baseline, but improved after revascularization. In men, QOL improved more with CABG than with PCI, whereas in women the improvements were similar with CABG and PCI.
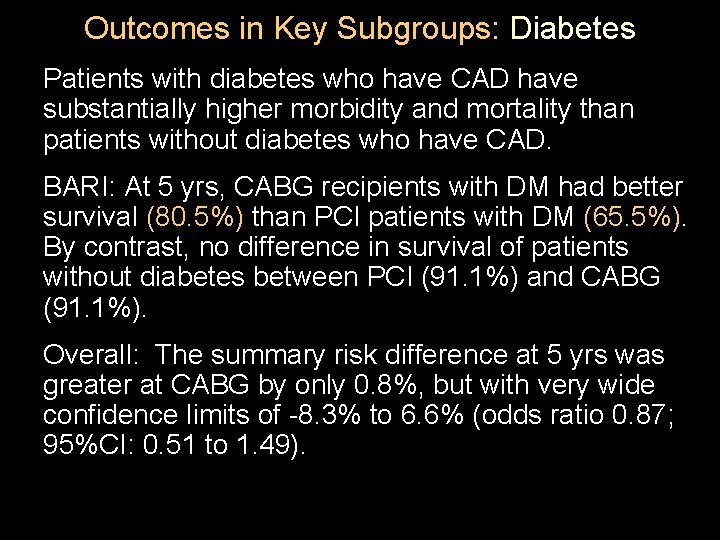
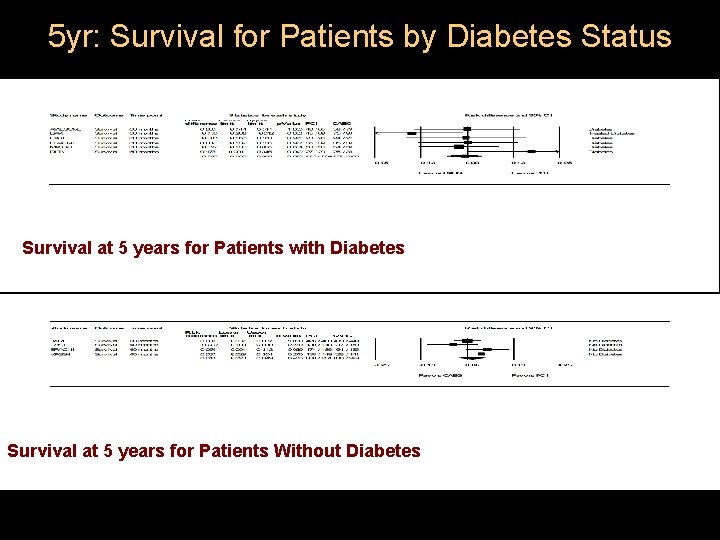
Outcomes in Key Subgroups: Diabetes Patients with diabetes who have CAD have substantially higher morbidity and mortality than patients without diabetes who have CAD. BARI: At 5 yrs, CABG recipients with DM had better survival (80. 5%) than PCI patients with DM (65. 5%). By contrast, no difference in survival of patients without diabetes between PCI (91. 1%) and CABG (91. 1%). Overall: The summary risk difference at 5 yrs was greater at CABG by only 0. 8%, but with very wide confidence limits of -8. 3% to 6. 6% (odds ratio 0. 87; 95%CI: 0. 51 to 1. 49).
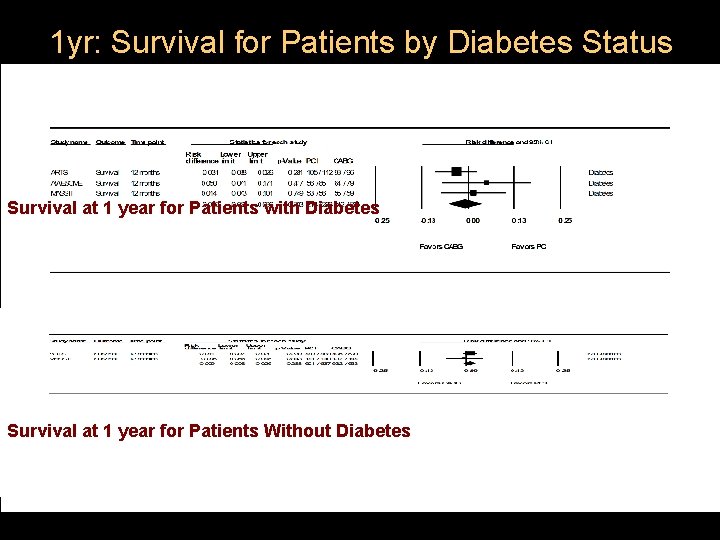
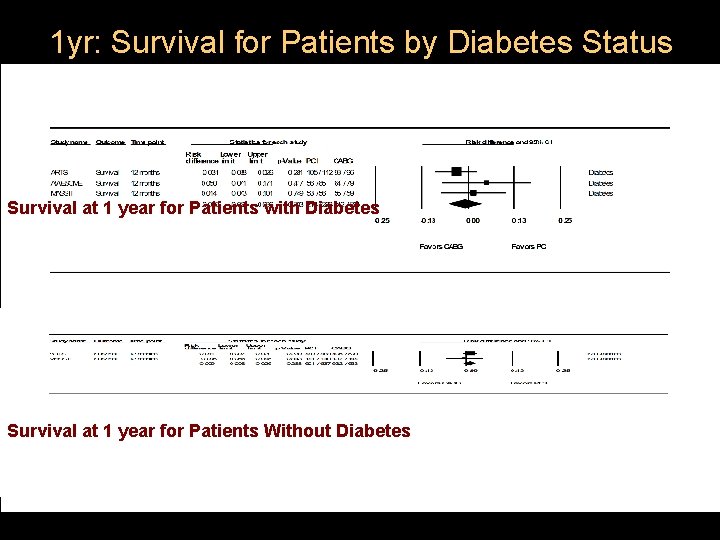
1 yr: Survival for Patients by Diabetes Status Survival at 1 year for Patients with Diabetes Survival at 1 year for Patients Without Diabetes
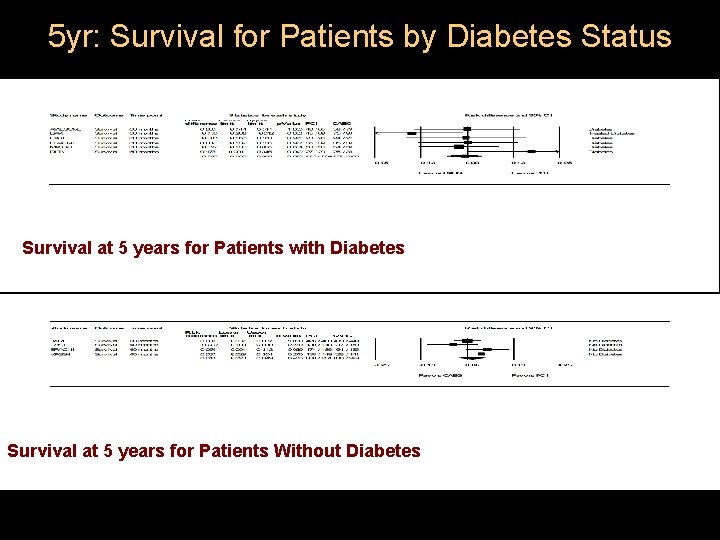
5 yr: Survival for Patients by Diabetes Status Survival at 5 years for Patients with Diabetes Survival at 5 years for Patients Without Diabetes
Outcomes by Other Risk Factors There was no evidence that hypertension, tobacco use, renal dysfunction, vascular disease, or obesity increased risk differentially in PCI-assigned and CABG-assigned patients.

Comparative Effectiveness by Extent of CAD l. BARI: Better survival for patients with 2 -vsl rather than 3 -vsl disease. Risk difference between PCI and CABG at 5 -yrs was greater in patients with 3 -vsl disease (3. 9% risk difference: 84. 7% PCI vs. 88. 6% CABG) than in patients with 2 -vsl disease (2. 1% risk difference; 87. 6% PCI vs. 89. 7% CABG). l. Similar trend reported in the EAST trial and the pooled stent-era trials. l. By contrast, RITA-I found very little difference in mortality between patients with SVD and MVD (mostly 2 -vessel) and similar PCI-CABG risk differences. l. Overall, these data suggest that mortality in patients with 3 -vsl disease may be reduced somewhat more by CABG than by PCI, and that in SVD there is little mortality difference between PCI and CABG.
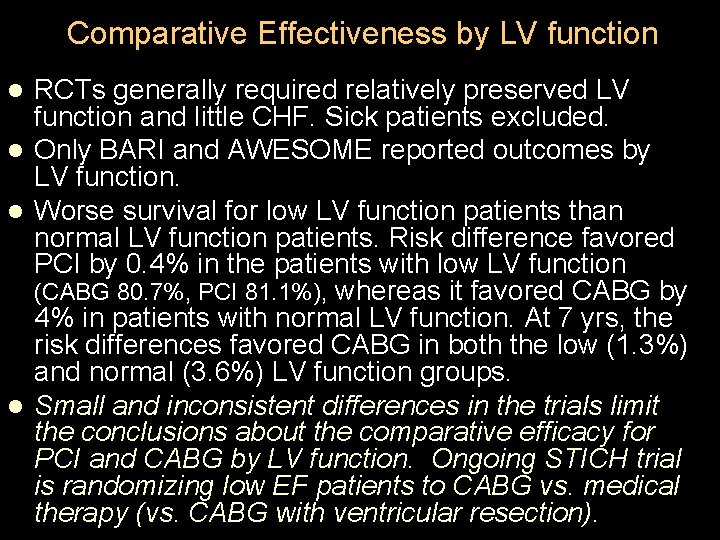
Comparative Effectiveness by LV function RCTs generally required relatively preserved LV function and little CHF. Sick patients excluded. l Only BARI and AWESOME reported outcomes by LV function. l Worse survival for low LV function patients than normal LV function patients. Risk difference favored PCI by 0. 4% in the patients with low LV function (CABG 80. 7%, PCI 81. 1%), whereas it favored CABG by 4% in patients with normal LV function. At 7 yrs, the risk differences favored CABG in both the low (1. 3%) and normal (3. 6%) LV function groups. l Small and inconsistent differences in the trials limit the conclusions about the comparative efficacy for PCI and CABG by LV function. Ongoing STICH trial is randomizing low EF patients to CABG vs. medical therapy (vs. CABG with ventricular resection). l

CABG-specific Factors “Minimally invasive” surgery (MIDCAB): – small throracotomy incision on a beating heart – Compared with PCI in 7 small trials l l SVD proximal LAD PCI with stents as the comparator These trials showed similar outcomes over a relatively short follow-up period. l There are only a few early trials of balloon angioplasty and standard CABG (Lausanne, MASS-I) in patients with single-vessel disease whose results can be compared with these trials. l In general, the risk differences over one to two years of follow-up are comparable. l
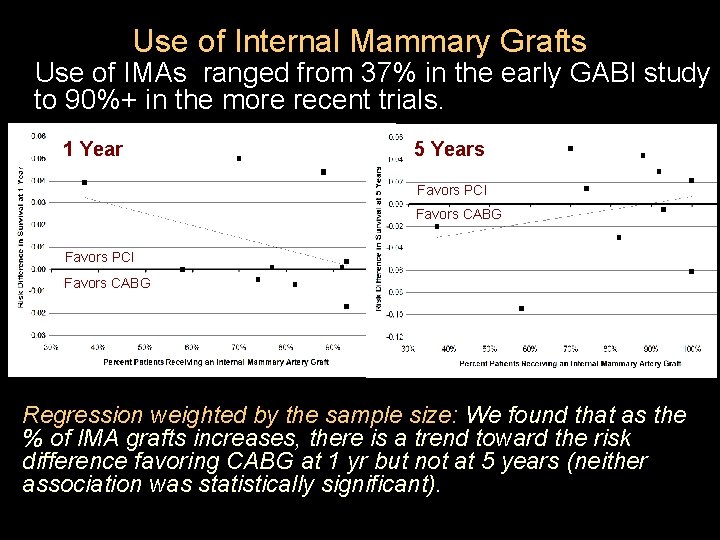
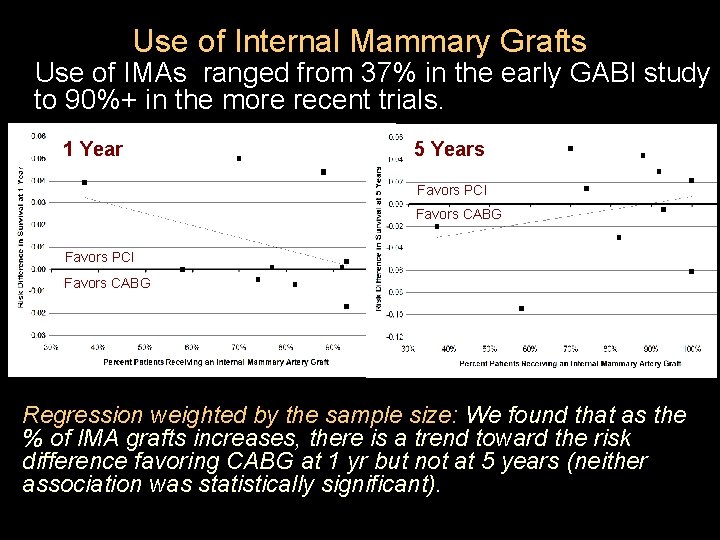
Use of Internal Mammary Grafts Use of IMAs ranged from 37% in the early GABI study to 90%+ in the more recent trials. 1 Year 5 Years Favors PCI Favors CABG Regression weighted by the sample size: We found that as the % of IMA grafts increases, there is a trend toward the risk difference favoring CABG at 1 yr but not at 5 years (neither association was statistically significant).
Prior Procedures Most RCTs excluded patients with prior CABG, but 1 RCT and several registries compared PCI with re-do CABG in patients with a prior CABG. l AWESOME trial (142 with prior CABG): l – Procedural mortality was higher in the patients assigned to re-CABG (8% vs 0%), three-year mortality was only slightly higher (27% vs 22%) and not significantly different. l A similar pattern has been reported by large clinical registry studies from Cleveland, Emory, and Kansas City: procedural mortality was higher for re-do CABG than for PCI, but survival at five to six years of follow-up did not differ significantly.
Volume-Outcome Relationships Randomized trials have not directly tested for differences in clinical outcomes of PCI and CABG on the basis of process characteristics. l There is considerable evidence from observational studies that procedural risk of both procedures increases significantly in low volume hospitals and with low volume operators. This relationship remains significant for PCI, even as procedural risk has been reduced by the availability of coronary stents and adjunctive therapy. l
Max Based on the best available evidence, Max chose CABG. He chose to have it at a high-volume academic center by a highly experienced surgeon. His surgery was complicated by a stroke and prolonged ICU stay. He was discharged to a skilled nursing facility and died 3 months after his bypass.
Today’s Talk Background on the procedures Methodological issues Results Conclusions and next steps
Conclusions: Survival • Procedural mortality is low for both PCI and CABG and does not differ significantly (RD: 0. 1%). • Long-term mortality was not substantially different between PCI and CABG up to 5 yrs after the initial procedure (RDs favor CABG over PCI between six months and five years by less than 1%). • 5 -yr survival in the “balloon-era” trials among patients with MVD favored CABG, whereas survival in the “stent-era” trials favored PCI, although this finding was not statistically significant.
Conclusions Freedom from angina and repeat revascularization strongly favored CABG over PCI. l The overall survival advantage of CABG over PCI among patients with DM was not statistically significant, averaging 0. 8% in absolute terms at 5 yrs. l Only a few trials specifically reported outcomes by number of diseased vessels—these suggest that CABG reduces mortality compared with PCI to a greater extent in patients with 3 -vsl disease than in patients with 2 -vsl disease. l
Limitations Most RCTs included low prevalence of heart failure and LV function was generally well preserved, limiting our analyses by LF function. • Many outcomes, including cognitive function, cost, and quality of life outcomes were reported by very few studies. • Most clinical trials have not reported outcomes in key subgroups. • Extended follow-up for the most recent trials was not available. •
Future Research Individual patient-level data pooling Clinical trials of drug-eluting stents Explore minimally invasive approaches to CABG with respect to procedure volume and outcomes l Presently, volume-outcomes studies focus exclusively on mortality. Procedural myocardial infarction, graft patency, relief of angina, and longterm outcomes are also pertinent to decision making and should be explored in relation to volume levels. l l l
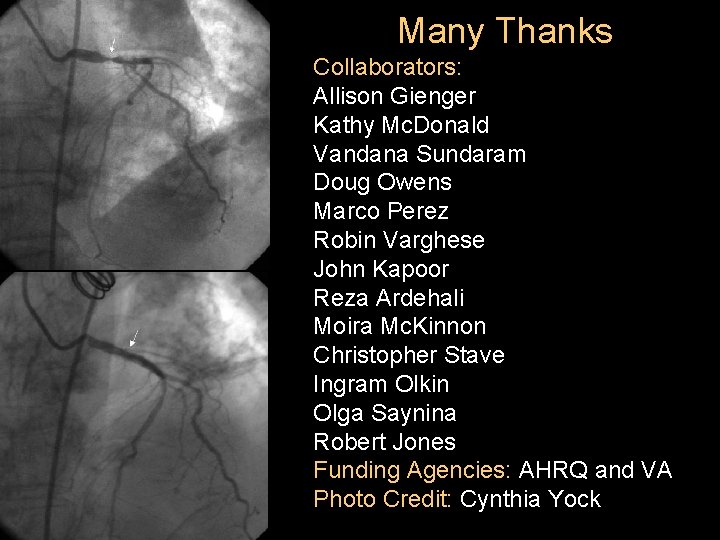
Many Thanks Collaborators: Allison Gienger Kathy Mc. Donald Vandana Sundaram Doug Owens Marco Perez Robin Varghese John Kapoor Reza Ardehali Moira Mc. Kinnon Christopher Stave Ingram Olkin Olga Saynina Robert Jones Funding Agencies: AHRQ and VA Photo Credit: Cynthia Yock
 Common bile duct diameter
Common bile duct diameter Percutaneous image-guided lumbar decompression
Percutaneous image-guided lumbar decompression Terminal testicular cancer
Terminal testicular cancer Intraoperative cholangiogram
Intraoperative cholangiogram Amnio vs cvs
Amnio vs cvs Pleural effusion ellis curve
Pleural effusion ellis curve Fossa ovalis
Fossa ovalis Heart wall
Heart wall Coronary personality
Coronary personality Aortic semi lunar valve
Aortic semi lunar valve Coronary sinusoids
Coronary sinusoids Cardiac plexus
Cardiac plexus Coronary artery disease
Coronary artery disease Cpr routine
Cpr routine Venae cordis minimi
Venae cordis minimi Coronary steal syndrome
Coronary steal syndrome Aortic sinus
Aortic sinus Right and left aortic sinus
Right and left aortic sinus Global registry of acute coronary events
Global registry of acute coronary events Chronic coronary syndrome
Chronic coronary syndrome Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Flow
Flow Acute coronary syndrome
Acute coronary syndrome Coronary ligament
Coronary ligament Coronary blood flow
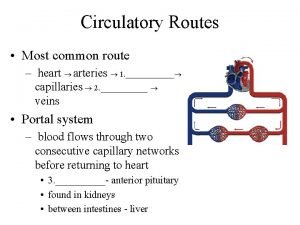
Coronary blood flow Coronary circulatory routes
Coronary circulatory routes Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Mesa coronary calcium score
Mesa coronary calcium score Superadded changes in coronary atherosclerosis
Superadded changes in coronary atherosclerosis Crash course heart
Crash course heart Coronary circulation animation
Coronary circulation animation Coronary circulation of heart
Coronary circulation of heart Function of coronary artery
Function of coronary artery Mesa coronary calcium score
Mesa coronary calcium score Coronary heart disease
Coronary heart disease Shepherd crook rca
Shepherd crook rca Coronary calcium score guidelines
Coronary calcium score guidelines Qfr coronary
Qfr coronary Vein
Vein Stent papyrus
Stent papyrus Ligamentum venosum
Ligamentum venosum Dr eter
Dr eter The effectiveness of online and blended learning
The effectiveness of online and blended learning Arrangement of people
Arrangement of people Efficiency and effectiveness examples
Efficiency and effectiveness examples Volumetric efficiency formula
Volumetric efficiency formula Efficiency and effectiveness in higher education
Efficiency and effectiveness in higher education Strategic profitability analysis
Strategic profitability analysis Managerial behavior and effectiveness
Managerial behavior and effectiveness Superlative form adjectives
Superlative form adjectives Jones and bartlett ekg strips 2012
Jones and bartlett ekg strips 2012 Positive behavioral interventions and supports
Positive behavioral interventions and supports Positive behavioral interventions and supports
Positive behavioral interventions and supports Developing and evaluating complex interventions
Developing and evaluating complex interventions Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Examples of internal forms of social control
Examples of internal forms of social control Steiner's model of group effectiveness in sport
Steiner's model of group effectiveness in sport This is making use of all the personal resources
This is making use of all the personal resources Effectiveness ntu method
Effectiveness ntu method Cath lab cost effectiveness
Cath lab cost effectiveness Liberal reforms essay
Liberal reforms essay Cooling equipment heat exchanger
Cooling equipment heat exchanger Enhancing personal effectiveness
Enhancing personal effectiveness Slip slop slap seek slide campaign effectiveness
Slip slop slap seek slide campaign effectiveness Team effectiveness model robbins
Team effectiveness model robbins It means making use of all the personal resources
It means making use of all the personal resources Cope certificate
Cope certificate