Interesting Case Rounds Nadim Lalani R 5 08



![Case o Physical? • • General [growth chart] Abdo [distended bladder, stool in rectum] Case o Physical? • • General [growth chart] Abdo [distended bladder, stool in rectum]](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-6.jpg)

![Pathophysiology o Genetics: • Risk: 43% [one parent with NE] 77% [both parents with Pathophysiology o Genetics: • Risk: 43% [one parent with NE] 77% [both parents with](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-10.jpg)


![Pharmacotherapy o TCA • • Imipramine best studied Mechanism unclear. Anticholnergic? Side effects [mood/weight/OD/Cardiac/Sz] Pharmacotherapy o TCA • • Imipramine best studied Mechanism unclear. Anticholnergic? Side effects [mood/weight/OD/Cardiac/Sz]](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-19.jpg)
![Cochrane Review 2004 o 17 studies > 700 kids [380 got behaviour training] Results: Cochrane Review 2004 o 17 studies > 700 kids [380 got behaviour training] Results:](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-22.jpg)



- Slides: 31

Interesting Case Rounds Nadim Lalani R 5 08. 21. 08

Which of the following are/were “Famous Bedwetters”?

“Fergie Wets Pants!” “I was late. . . I didn’t go to the restroom before I went onstage. It was horrible. But, whatever. It happened. . . everyone knows I wet my pants on-stage and had a crystal-meth addiction. That sucks. You have to laugh. ”
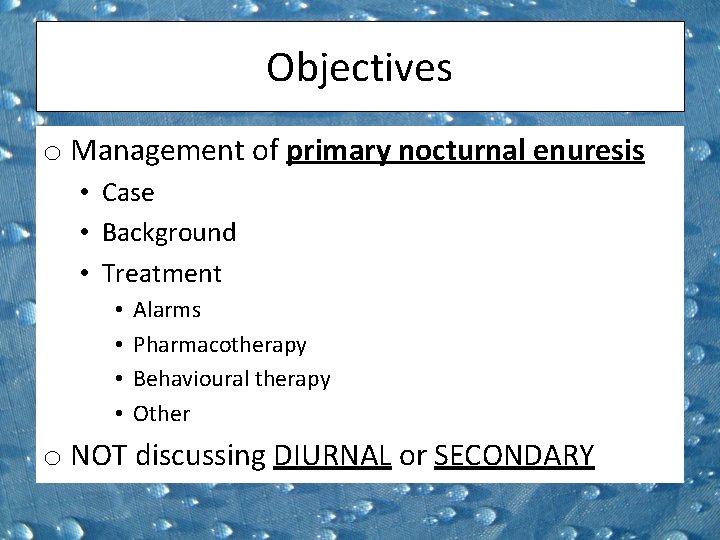
Objectives o Management of primary nocturnal enuresis • Case • Background • Treatment • • Alarms Pharmacotherapy Behavioural therapy Other o NOT discussing DIURNAL or SECONDARY
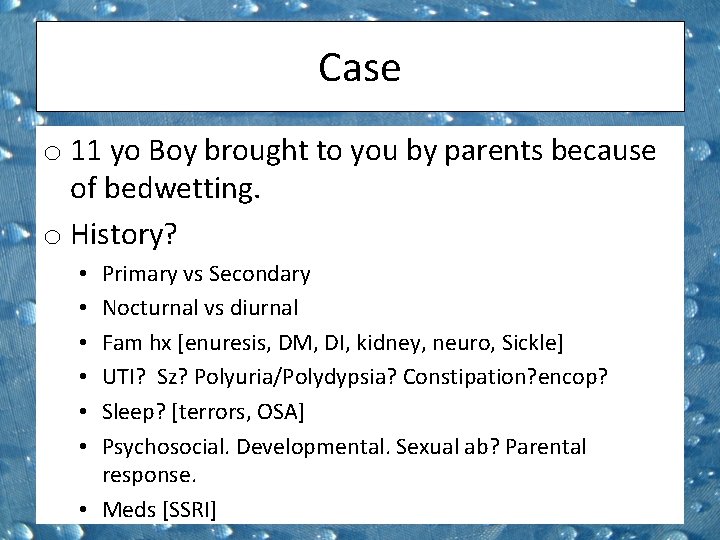
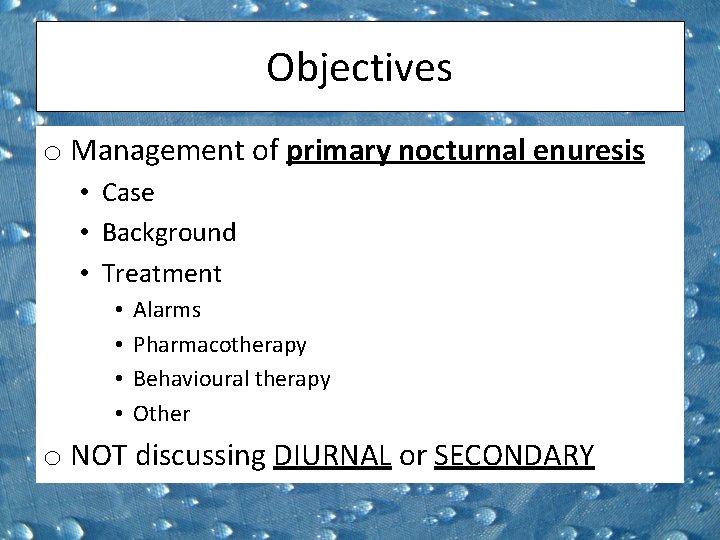
Case o 11 yo Boy brought to you by parents because of bedwetting. o History? Primary vs Secondary Nocturnal vs diurnal Fam hx [enuresis, DM, DI, kidney, neuro, Sickle] UTI? Sz? Polyuria/Polydypsia? Constipation? encop? Sleep? [terrors, OSA] Psychosocial. Developmental. Sexual ab? Parental response. • Meds [SSRI] • • •
![Case o Physical General growth chart Abdo distended bladder stool in rectum Case o Physical? • • General [growth chart] Abdo [distended bladder, stool in rectum]](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-6.jpg)
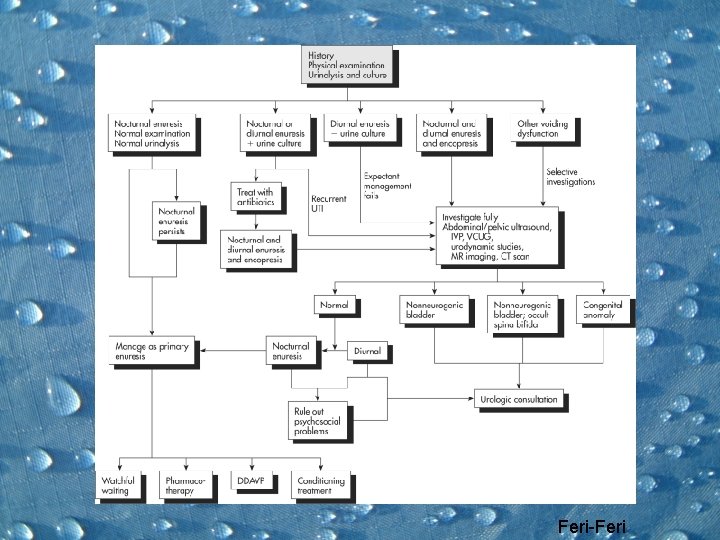
Case o Physical? • • General [growth chart] Abdo [distended bladder, stool in rectum] GU [ectopic ureter, labial adhesions, Sexual ab] Neuro exam[ Sacral dimples or tufts of hair] o Diagnostics? • Urinalysis. First void SG • Unless secondary or treatment failure [see algorithm]
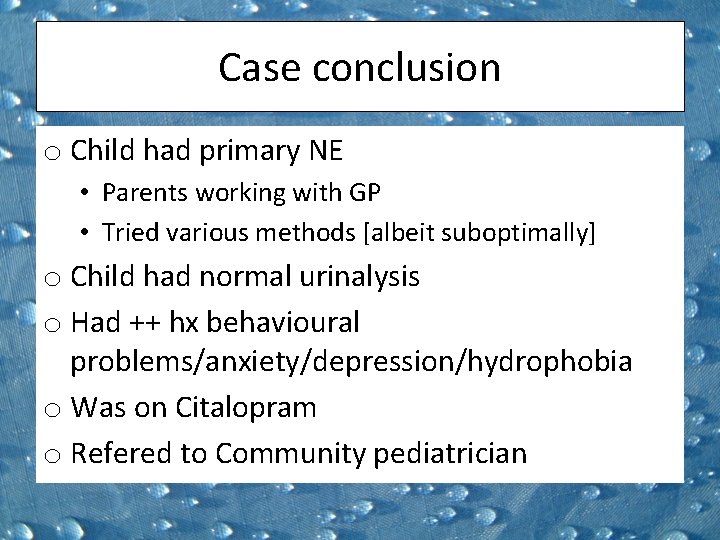
Case conclusion o Child had primary NE • Parents working with GP • Tried various methods [albeit suboptimally] o Child had normal urinalysis o Had ++ hx behavioural problems/anxiety/depression/hydrophobia o Was on Citalopram o Refered to Community pediatrician

Background: o Definition: Involuntary discharge of urine at night. Beyond age of bladder control. > Twice per week for 3 months Uncomplicated [85%] vs Complicated* [10%] o Epidemiology: • Boys >> girls [2: 1] • 15% of 5 yo [8% of 8 yo] 1% 15 yo • 5% are due to organic pathology * Have other symptoms [const/encop]
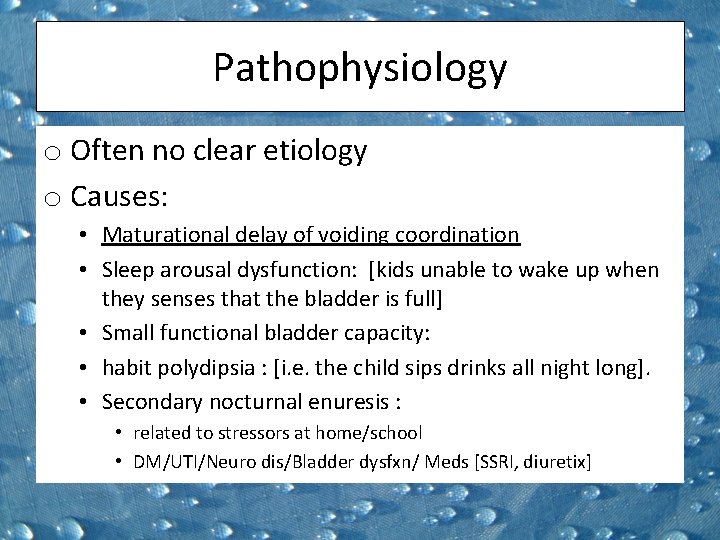
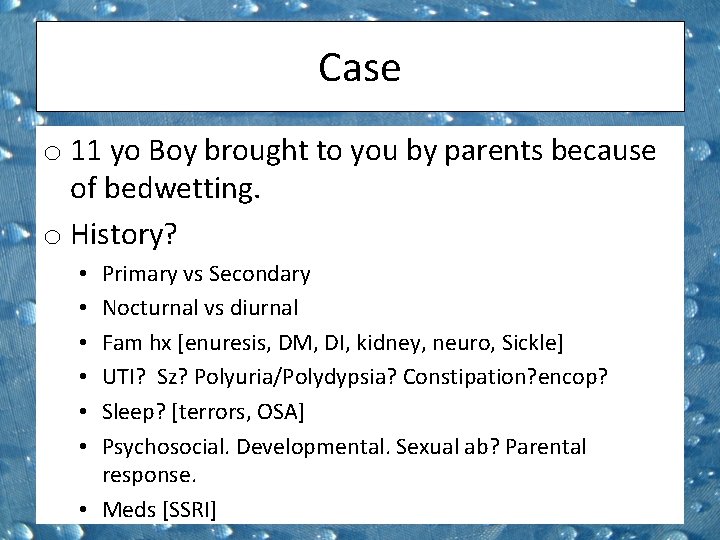
Pathophysiology o Often no clear etiology o Causes: • Maturational delay of voiding coordination • Sleep arousal dysfunction: [kids unable to wake up when they senses that the bladder is full] • Small functional bladder capacity: • habit polydipsia : [i. e. the child sips drinks all night long]. • Secondary nocturnal enuresis : • related to stressors at home/school • DM/UTI/Neuro dis/Bladder dysfxn/ Meds [SSRI, diuretix]
![Pathophysiology o Genetics Risk 43 one parent with NE 77 both parents with Pathophysiology o Genetics: • Risk: 43% [one parent with NE] 77% [both parents with](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-10.jpg)
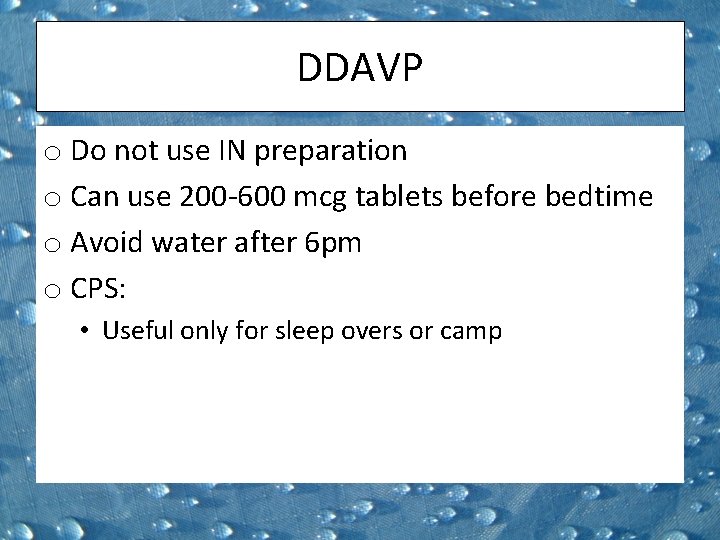
Pathophysiology o Genetics: • Risk: 43% [one parent with NE] 77% [both parents with NE] • 75% of kids with NE have a first-degree relative who had enuresis • Linkage studies have shown associated genetic loci on chromosomes 8 q, 12 q, 13 q, and 22 q 11
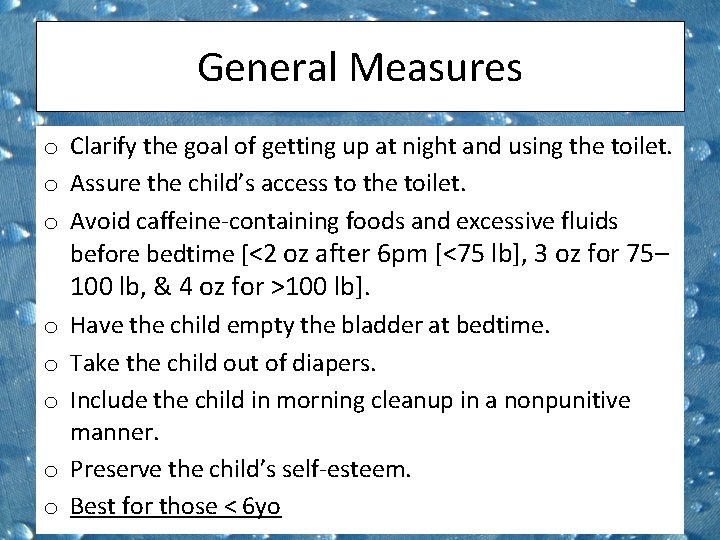
General Measures o Clarify the goal of getting up at night and using the toilet. o Assure the child’s access to the toilet. o Avoid caffeine-containing foods and excessive fluids before bedtime [<2 oz after 6 pm [<75 lb], 3 oz for 75– 100 lb, & 4 oz for >100 lb]. o Have the child empty the bladder at bedtime. o Take the child out of diapers. o Include the child in morning cleanup in a nonpunitive manner. o Preserve the child’s self-esteem. o Best for those < 6 yo
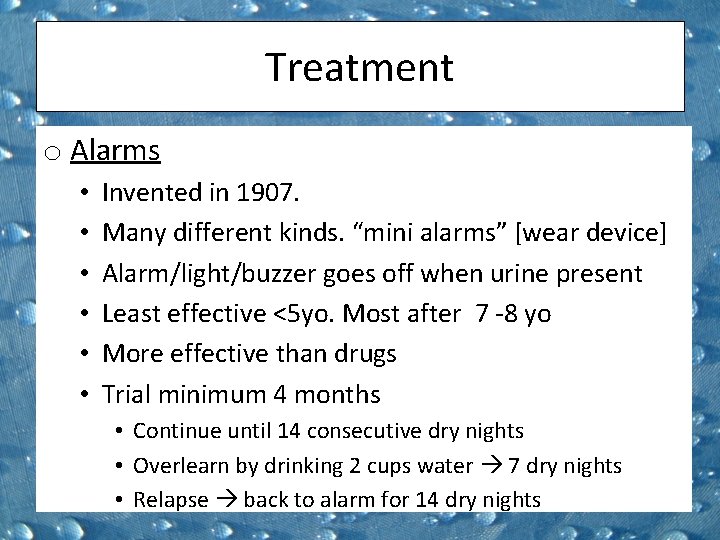
Treatment o Alarms • • • Invented in 1907. Many different kinds. “mini alarms” [wear device] Alarm/light/buzzer goes off when urine present Least effective <5 yo. Most after 7 -8 yo More effective than drugs Trial minimum 4 months • Continue until 14 consecutive dry nights • Overlearn by drinking 2 cups water 7 dry nights • Relapse back to alarm for 14 dry nights
Cochrane review 2005 o 56 studies. Over 3200 children o. RCT’s & quasi-RCT’s involving alarms [2400 pts] o. Excluded diurnal Results: o. Alarm 60% effective at stopping bedwetting o 50% relapse. Less relapse with overlearning and dry bed training. o. No difference in alarm types [but kids prefer wearable ones] o. DDAVP faster than alarm but not sustainable o. TCA no different, but also not sustainable
Alarms o Overall cure rate of 50% o Requires buy in from whole family as it’s disruptive o Impractical for ‘sleepovers’ and camp o No need to go high-end, kids like mini o Don’t buy second-hand [don’t work well after 2 -3 pts]


Treatment o Pharmacotherapy : DDAVP • Studied since 1970 s • Enuretic kids have decreased nighttime ADH secretion produce more urine. • Side effects water intoxication • Expensive • IN preparation pulled by FDA/health Canada • HYponatremia • 5 cases /10 million doses IN vs 1/10 million PO
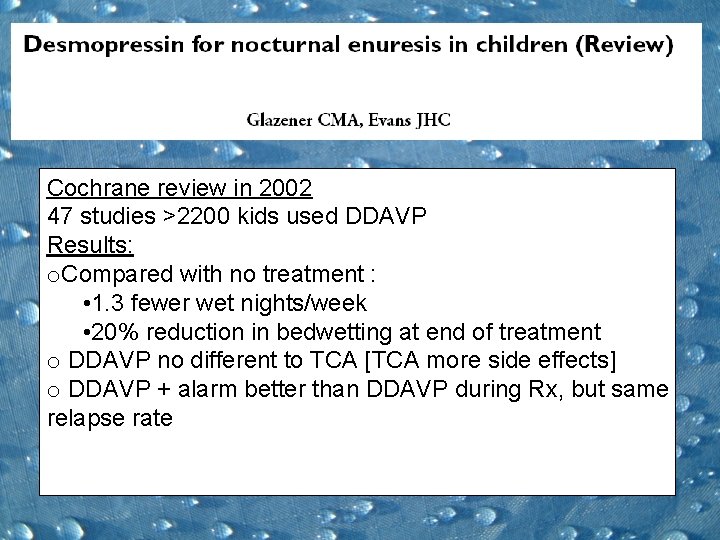
Cochrane review in 2002 47 studies >2200 kids used DDAVP Results: o. Compared with no treatment : • 1. 3 fewer wet nights/week • 20% reduction in bedwetting at end of treatment o DDAVP no different to TCA [TCA more side effects] o DDAVP + alarm better than DDAVP during Rx, but same relapse rate
DDAVP o Do not use IN preparation o Can use 200 -600 mcg tablets before bedtime o Avoid water after 6 pm o CPS: • Useful only for sleep overs or camp
![Pharmacotherapy o TCA Imipramine best studied Mechanism unclear Anticholnergic Side effects moodweightODCardiacSz Pharmacotherapy o TCA • • Imipramine best studied Mechanism unclear. Anticholnergic? Side effects [mood/weight/OD/Cardiac/Sz]](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-19.jpg)
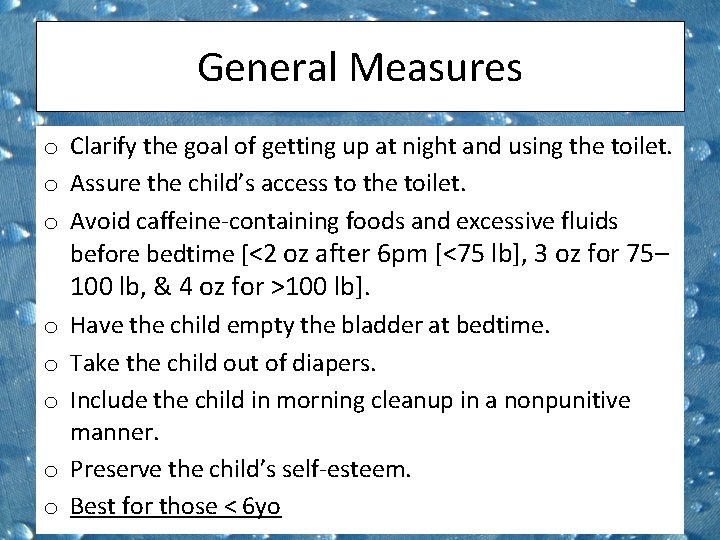
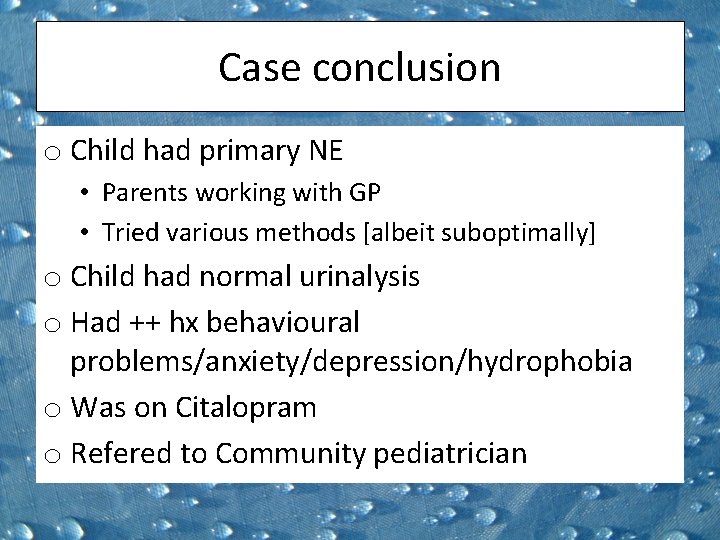
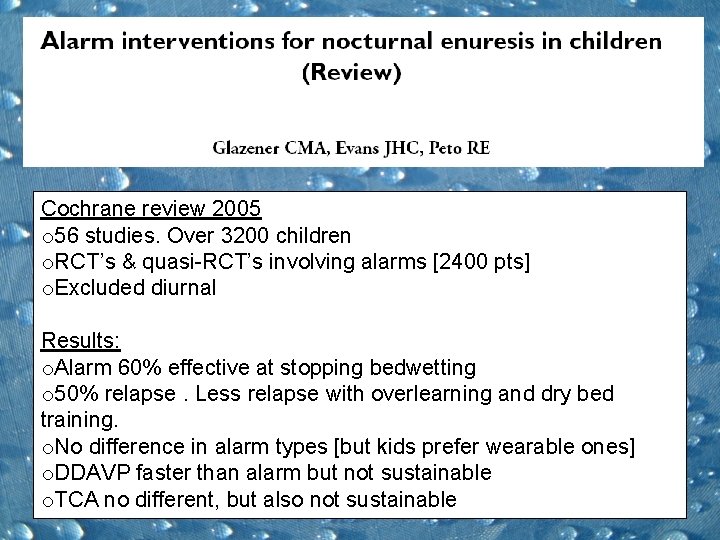
Pharmacotherapy o TCA • • Imipramine best studied Mechanism unclear. Anticholnergic? Side effects [mood/weight/OD/Cardiac/Sz] CPS Position Statement: • Short-term • Distressed, Older kids • Reliable parents
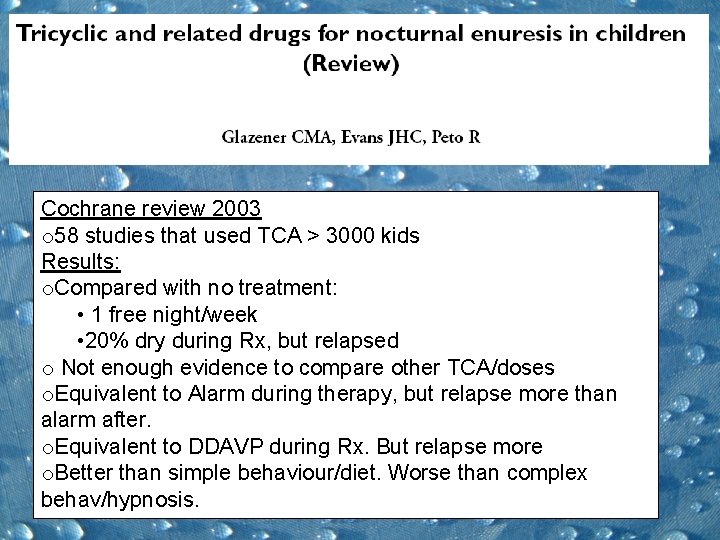
Cochrane review 2003 o 58 studies that used TCA > 3000 kids Results: o. Compared with no treatment: • 1 free night/week • 20% dry during Rx, but relapsed o Not enough evidence to compare other TCA/doses o. Equivalent to Alarm during therapy, but relapse more than alarm after. o. Equivalent to DDAVP during Rx. But relapse more o. Better than simple behaviour/diet. Worse than complex behav/hypnosis.
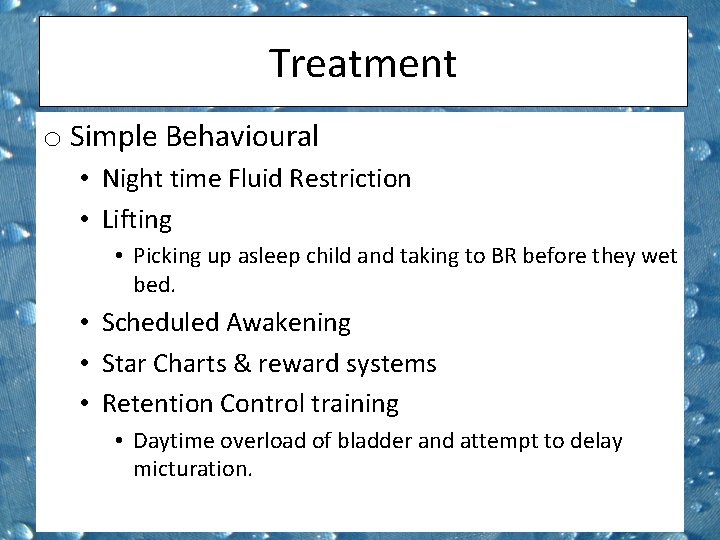
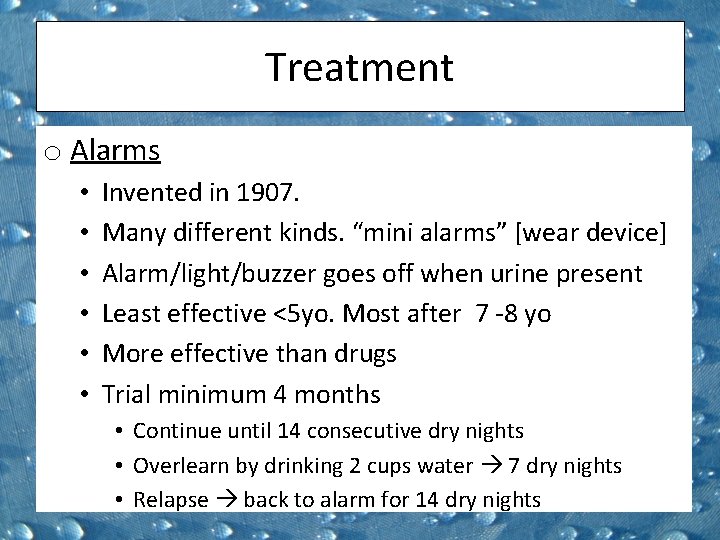
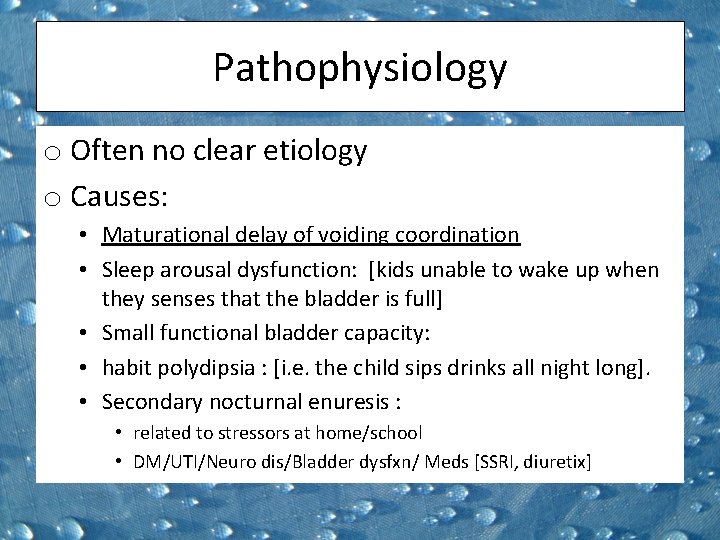
Treatment o Simple Behavioural • Night time Fluid Restriction • Lifting • Picking up asleep child and taking to BR before they wet bed. • Scheduled Awakening • Star Charts & reward systems • Retention Control training • Daytime overload of bladder and attempt to delay micturation.
![Cochrane Review 2004 o 17 studies 700 kids 380 got behaviour training Results Cochrane Review 2004 o 17 studies > 700 kids [380 got behaviour training] Results:](https://slidetodoc.com/presentation_image/99910260531f8c6e7575a351a095579b/image-22.jpg)
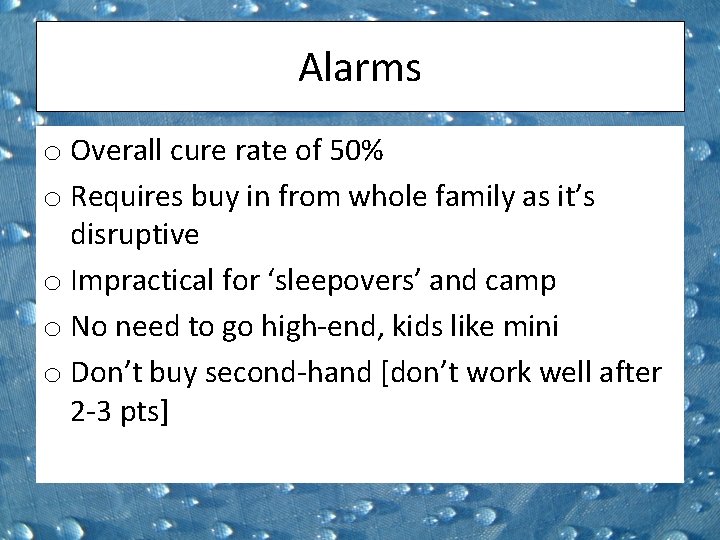
Cochrane Review 2004 o 17 studies > 700 kids [380 got behaviour training] Results: • Star charts, Lifting and Waking better than nothing • Might be worth initiating 1 st • Drop out associated with frustration and family strife.

Treatment o Complex behavioural Dry Bed Training: • Intensive 1 st night woken Q 1 h • If bed wet clean bed [cleanliness] & practice going to BR • Subsequent nights awoken once/night [getting earlier and earlier] Full spectrum Home Training: o Alarm + cleanliness + retention control + overlearning
Cochrane Review 2004 o 18 trials >1000 kids o. Results: o. Complex training better than nothing o. No better than alarm alone
Behavioural Therapy o CPS Position: • Insufficient evidence • Labor intensive and can contribute to frustration and conflict • Might do more harm than good • Shouldn’t be recommended without careful consideration
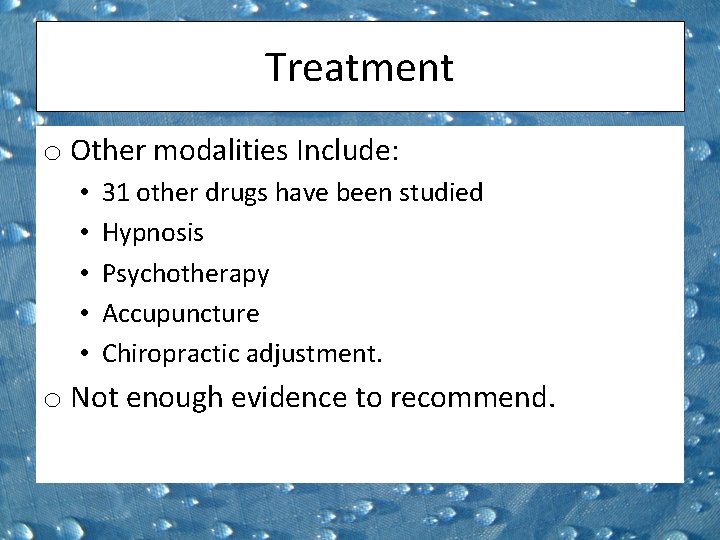
Treatment o Other modalities Include: • • • 31 other drugs have been studied Hypnosis Psychotherapy Accupuncture Chiropractic adjustment. o Not enough evidence to recommend.

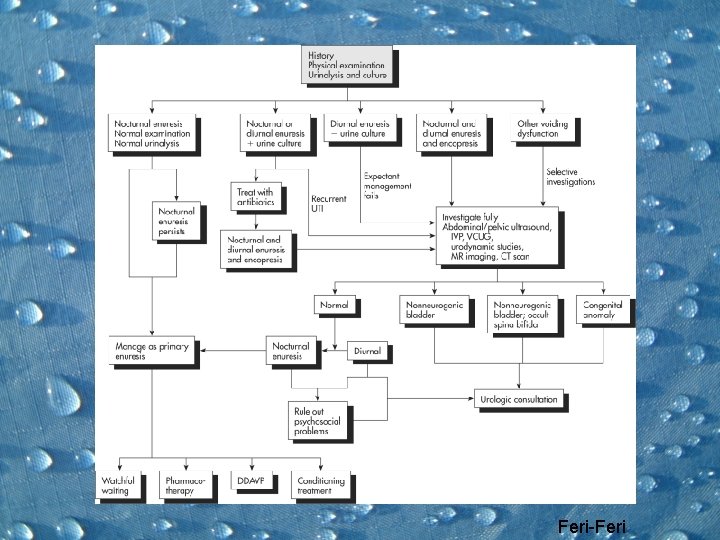
Summary o Distinguish NE from Diurnal and secondary o Most important to have supportive environment & minimise impact o Conditioning using alarm most efficacious o Special situations can use DDAVP o Difficult circumstances imipramine o Judicious use of behavioural therapy o Should be handled by paediatrician o Persistence urology referral
Feri-Feri

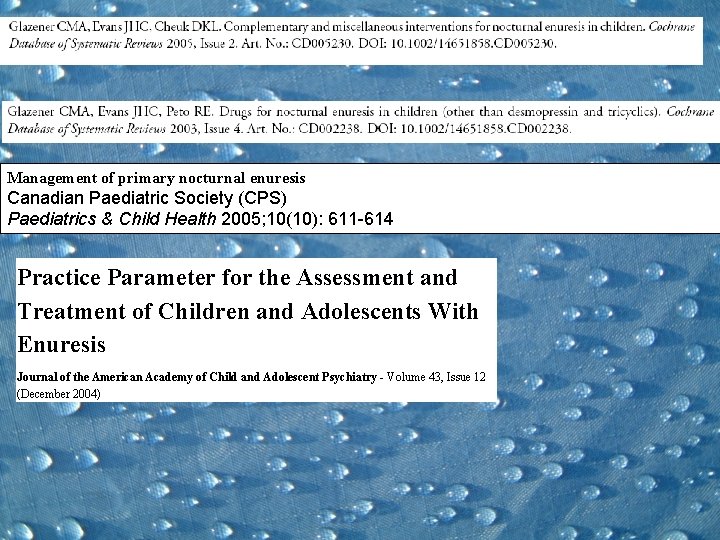
Management of primary nocturnal enuresis Canadian Paediatric Society (CPS) Paediatrics & Child Health 2005; 10(10): 611 -614 Practice Parameter for the Assessment and Treatment of Children and Adolescents With Enuresis Journal of the American Academy of Child and Adolescent Psychiatry - Volume 43, Issue 12 (December 2004)
Parent Handout http: //www. caringforkids. cps. ca/growing&learn ing/Bedwetting. htm
 Nadim lalani
Nadim lalani Interesting more interesting the most interesting
Interesting more interesting the most interesting Majla custo
Majla custo Dr christopher jernigan
Dr christopher jernigan Nadim elhage
Nadim elhage Best case worst case average case
Best case worst case average case Maths quiz rounds names
Maths quiz rounds names Duke family medicine and community health
Duke family medicine and community health Maintenance rounds
Maintenance rounds Readiness rounds
Readiness rounds Rounds and fillets are usually dimensioned using
Rounds and fillets are usually dimensioned using Nursing grand rounds presentation example
Nursing grand rounds presentation example Schwartz rounds facilitator training
Schwartz rounds facilitator training Utmb grand rounds
Utmb grand rounds Breech marks
Breech marks Layers of neurosis gestalt
Layers of neurosis gestalt Quality teaching rounds coding sheet
Quality teaching rounds coding sheet Sam rounds
Sam rounds What is 475 rounded to the nearest ten
What is 475 rounded to the nearest ten Harvard instructional rounds
Harvard instructional rounds A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Red white and blue tortilla chips
Red white and blue tortilla chips Bubble sort best case and worst case
Bubble sort best case and worst case Case western reserve university case school of engineering
Case western reserve university case school of engineering Bubble sort best case and worst case
Bubble sort best case and worst case Bubble sort best case and worst case
Bubble sort best case and worst case Triangle ambiguous case
Triangle ambiguous case Short case vs long case
Short case vs long case Hershey's erp failure
Hershey's erp failure Average case of binary search
Average case of binary search The five principles of design
The five principles of design Interesting facts about change management
Interesting facts about change management