Interesting case conference Xuan Wang 12102015 Case scenario





- Slides: 23
Interesting case conference Xuan Wang 12/10/2015
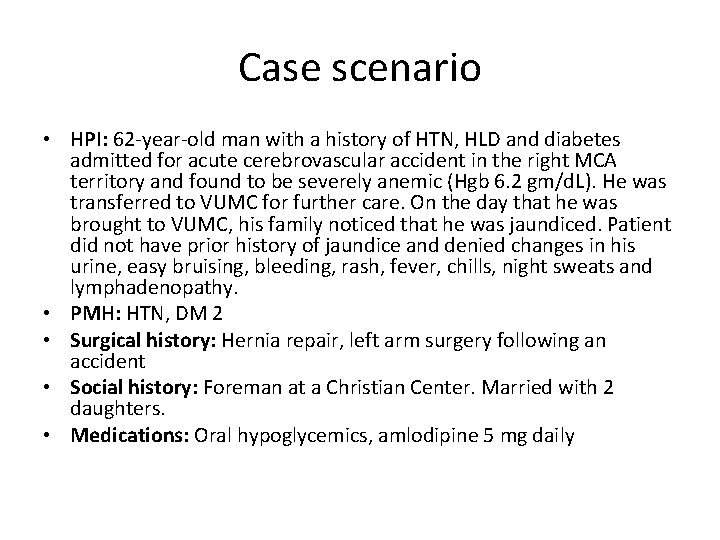
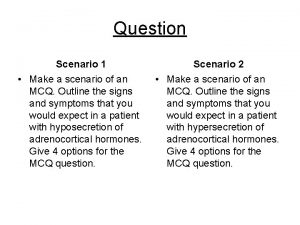
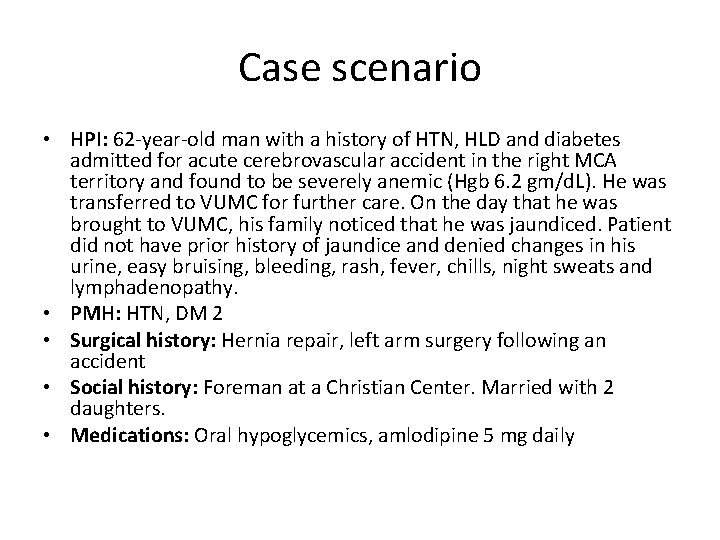
Case scenario • HPI: 62 -year-old man with a history of HTN, HLD and diabetes admitted for acute cerebrovascular accident in the right MCA territory and found to be severely anemic (Hgb 6. 2 gm/d. L). He was transferred to VUMC for further care. On the day that he was brought to VUMC, his family noticed that he was jaundiced. Patient did not have prior history of jaundice and denied changes in his urine, easy bruising, bleeding, rash, fever, chills, night sweats and lymphadenopathy. • PMH: HTN, DM 2 • Surgical history: Hernia repair, left arm surgery following an accident • Social history: Foreman at a Christian Center. Married with 2 daughters. • Medications: Oral hypoglycemics, amlodipine 5 mg daily
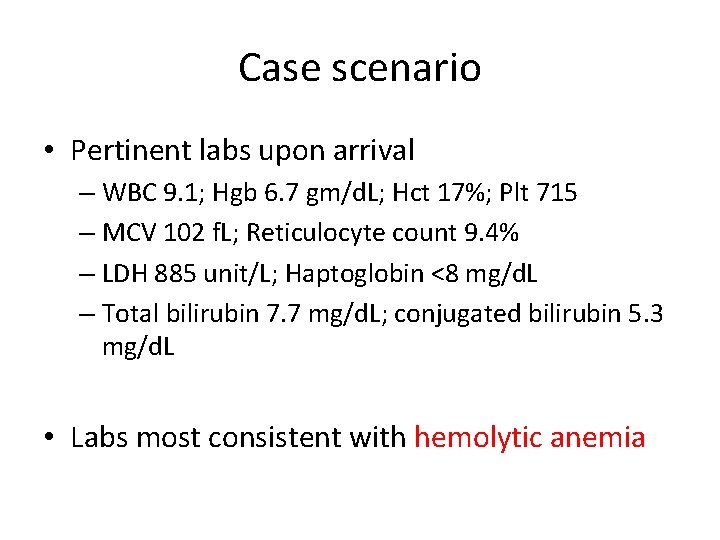
Case scenario • Pertinent labs upon arrival – WBC 9. 1; Hgb 6. 7 gm/d. L; Hct 17%; Plt 715 – MCV 102 f. L; Reticulocyte count 9. 4% – LDH 885 unit/L; Haptoglobin <8 mg/d. L – Total bilirubin 7. 7 mg/d. L; conjugated bilirubin 5. 3 mg/d. L • Labs most consistent with hemolytic anemia
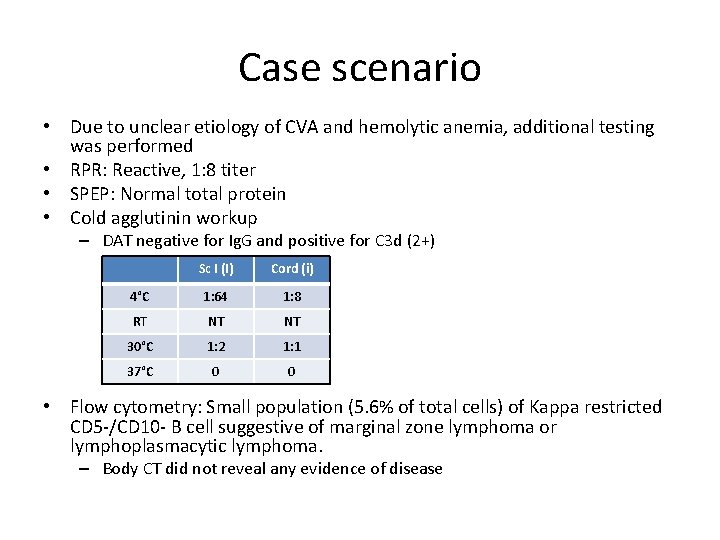
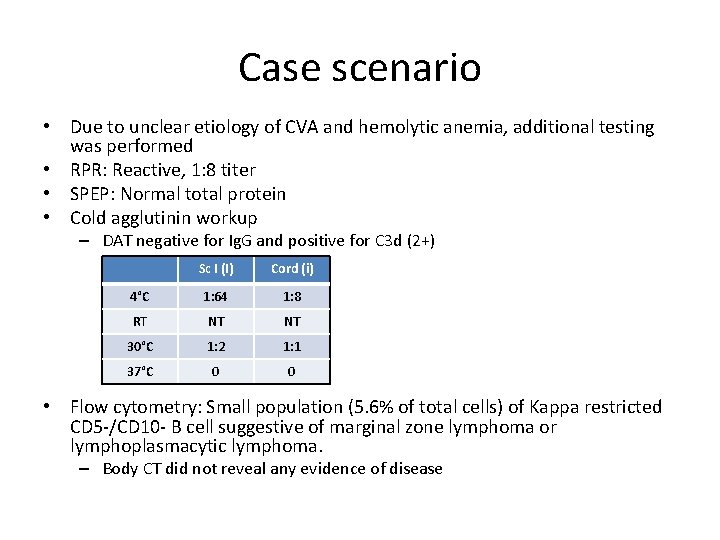
Case scenario • Due to unclear etiology of CVA and hemolytic anemia, additional testing was performed • RPR: Reactive, 1: 8 titer • SPEP: Normal total protein • Cold agglutinin workup – DAT negative for Ig. G and positive for C 3 d (2+) Sc I (I) Cord (i) 4°C 1: 64 1: 8 RT NT NT 30°C 1: 2 1: 1 37°C 0 0 • Flow cytometry: Small population (5. 6% of total cells) of Kappa restricted CD 5 -/CD 10 - B cell suggestive of marginal zone lymphoma or lymphoplasmacytic lymphoma. – Body CT did not reveal any evidence of disease
Additional pending tests • Hematologic tests – JAK 2 (V 617 F) Mutation Analysis – BCR/ABL Mutation • Confirmatory syphilis tests: – FTA-ABS (Fluorescent treponemal antibody absorption) – MHA-TP (Microhemagglutination assay)
Blood Bank page • Given the patient’s reactive RPR and hemolytic anemia, Blood Bank was asked about performing a Donath-Landsteiner test for patient • How is syphilis and Donath-Landsteiner test related? • What is appropriateness of performing the D-L test? • And how would test result influence clinical management?
Syphilis • Chronic infection caused by the bacterium Treponema pallidum • Primary syphilis – chancre at the site of inoculation • Secondary syphilis – systemic disease in 25% of untreated individuals – – – A rash (most characteristic finding) Fever Headache Malaise Anorexia Diffuse lymphadenopathy • Tertiary (late) syphilis – symptomatic manifestations of the disease involving the CNS, the cardiovascular system, or the skin and subcutaneous tissues (gummas). – CNS syphilis may occur early as one year after initial infection to 25 years later – CNS manifestations: meningitis ( infectious arteritis), cranial neuropathy (optic, facial, or auditory nerves), general paresis, tabes dorsalis
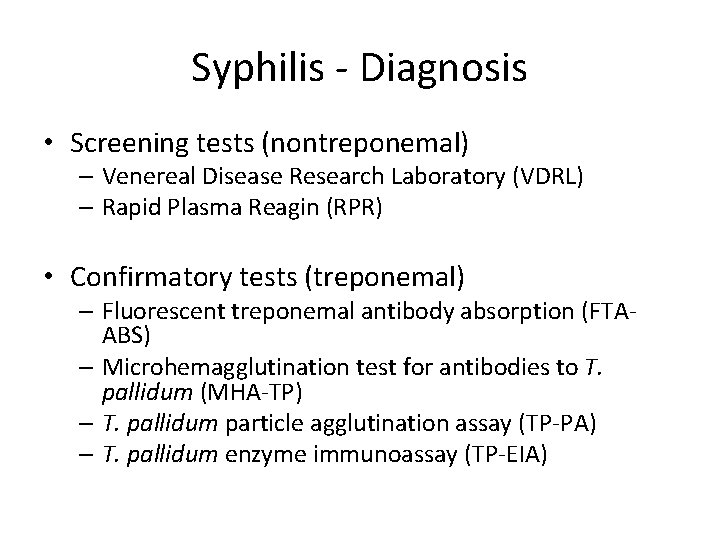
Syphilis - Diagnosis • Screening tests (nontreponemal) – Venereal Disease Research Laboratory (VDRL) – Rapid Plasma Reagin (RPR) • Confirmatory tests (treponemal) – Fluorescent treponemal antibody absorption (FTAABS) – Microhemagglutination test for antibodies to T. pallidum (MHA-TP) – T. pallidum particle agglutination assay (TP-PA) – T. pallidum enzyme immunoassay (TP-EIA)

Donath-Landsteiner antibody • Seen in paroxysmal cold hemoglobinuria (PCH) • The term PCH was named for a recurrent complication in late-stage or congenital syphilis: sudden attacks of constitutional symptoms and hemoglobinuria precipitated by exposure to cold temperatures • With the advent of antibiotics and the almost complete eradication of late syphilis, this chronic relapsing form of PCH is now extremely rare • PCH now tends to be an acute non-recurring illness affecting the pediatric population.
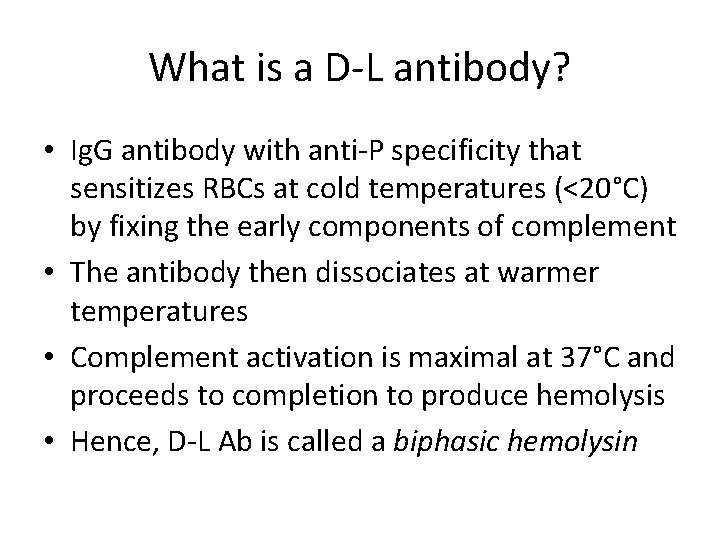
What is a D-L antibody? • Ig. G antibody with anti-P specificity that sensitizes RBCs at cold temperatures (<20°C) by fixing the early components of complement • The antibody then dissociates at warmer temperatures • Complement activation is maximal at 37°C and proceeds to completion to produce hemolysis • Hence, D-L Ab is called a biphasic hemolysin

History • 1904 – Julius Donath and Karl Landsteiner were the first to attribute the temperature-dependent hemolysis in PCH to a cold-reacting autohemolysin and warm-reacting lytic factor (Eder, 2005) • Early 1900 s, 90% of cases were secondary to syphilis, particularly congenital syphilis (Heddle, 1989; Gottsche et al, 1990) • Now seen almost exclusively in children following infection – 30 -40% of AIHA in young children – 0. 4/100, 000 in children <5 yrs (Sokol et al, 1999) – Slight male predominance • Rare examples of D-L antibodies in adults with other immunologic disorders (lymphoproliferative, collagen disease, delayed hemolytic transfusion rxn)

Eder AF. Immunohematology. 2005.
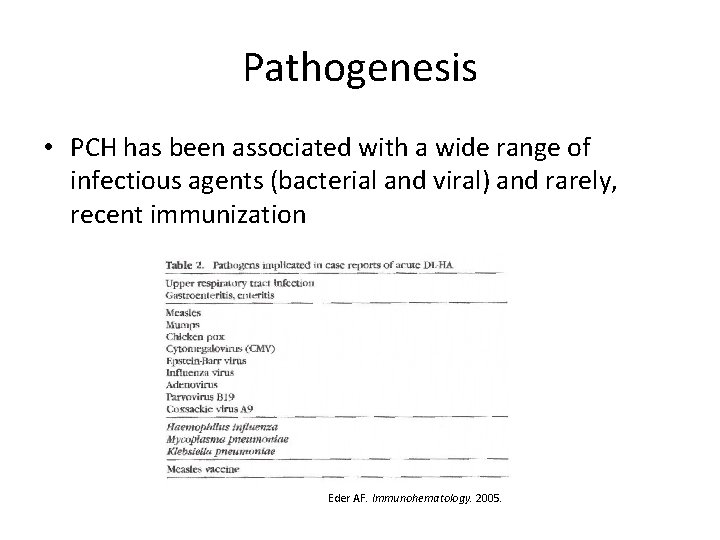
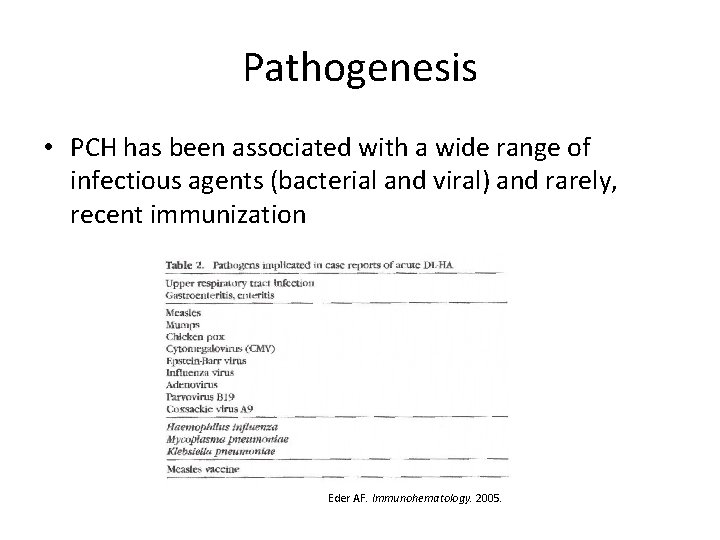
Pathogenesis • PCH has been associated with a wide range of infectious agents (bacterial and viral) and rarely, recent immunization Eder AF. Immunohematology. 2005.

Pathogenesis II • Inciting stimulus for autoantibody formation is unknown but a few hypotheses: – P antigen may be altered by an infectious agent so as to stimulate auto. Ab formation – Molecular mimicry: Infectious agent may possess antigens similar to P antigen and the resultant antibodies will cross-react – Increased production of autoantibodies due to increased lymphocyte activation
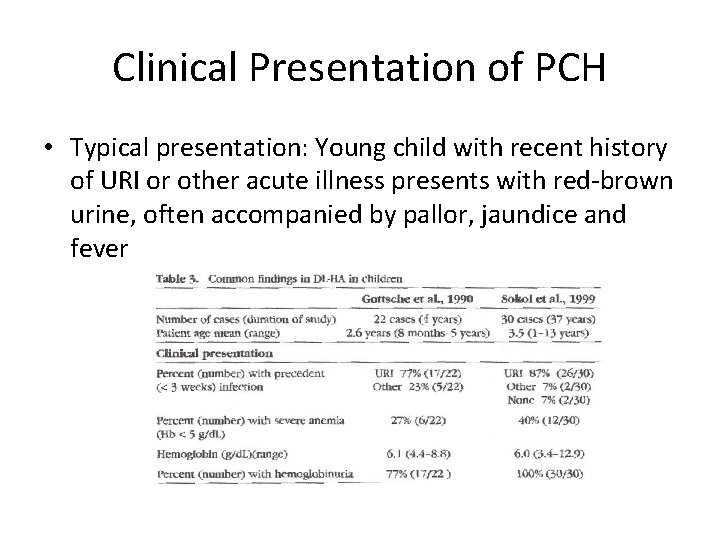
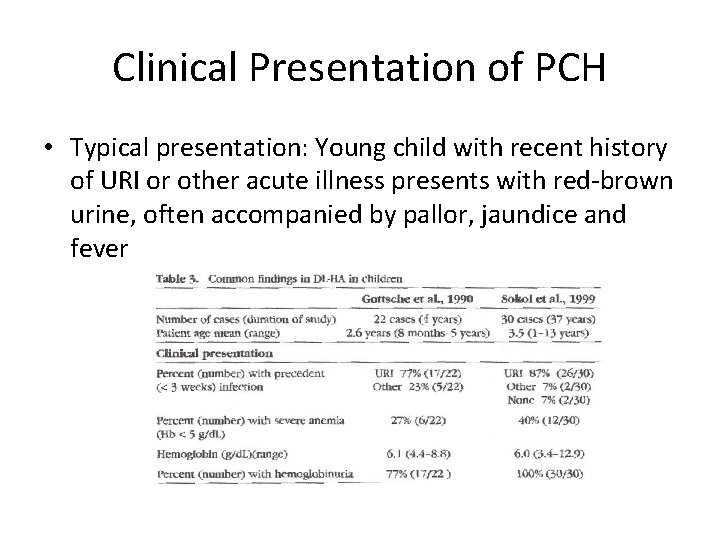
Clinical Presentation of PCH • Typical presentation: Young child with recent history of URI or other acute illness presents with red-brown urine, often accompanied by pallor, jaundice and fever
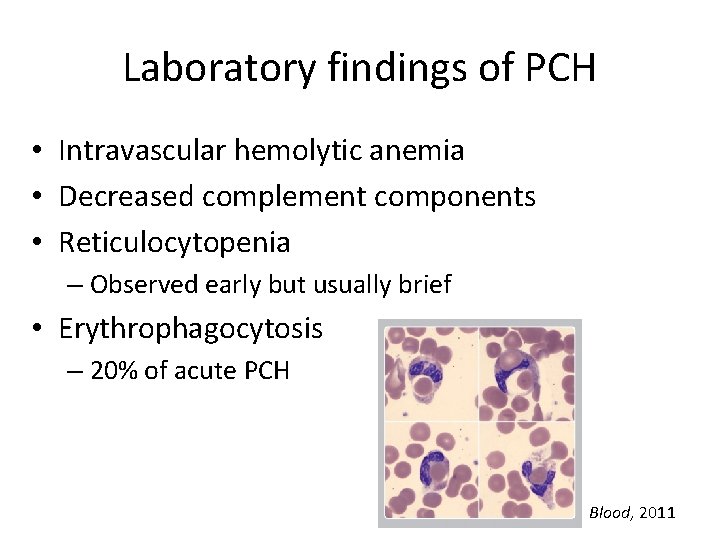
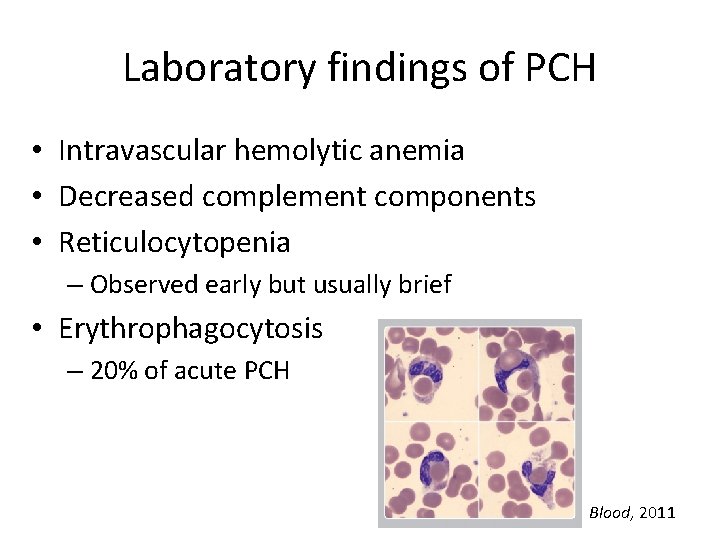
Laboratory findings of PCH • Intravascular hemolytic anemia • Decreased complement components • Reticulocytopenia – Observed early but usually brief • Erythrophagocytosis – 20% of acute PCH Blood, 2011
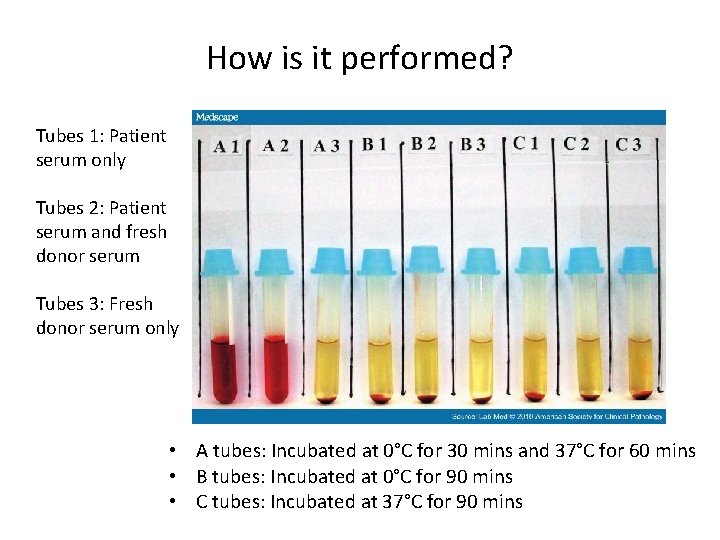
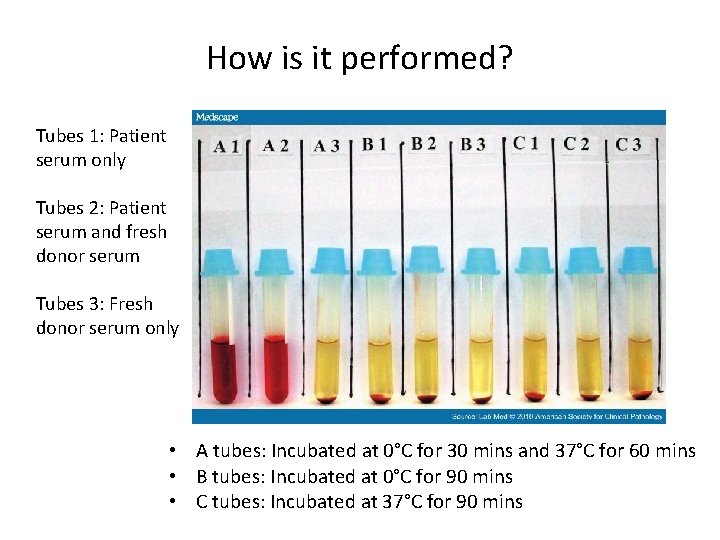
How is it performed? Tubes 1: Patient serum only Tubes 2: Patient serum and fresh donor serum Tubes 3: Fresh donor serum only • A tubes: Incubated at 0°C for 30 mins and 37°C for 60 mins • B tubes: Incubated at 0°C for 90 mins • C tubes: Incubated at 37°C for 90 mins
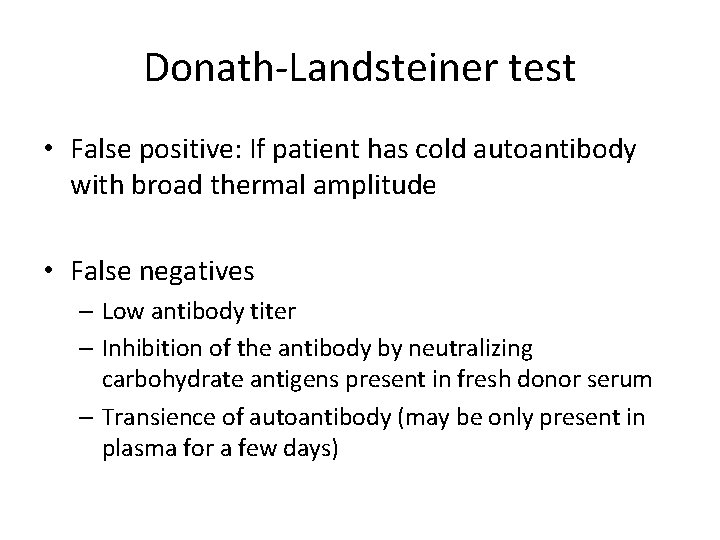
Donath-Landsteiner test • False positive: If patient has cold autoantibody with broad thermal amplitude • False negatives – Low antibody titer – Inhibition of the antibody by neutralizing carbohydrate antigens present in fresh donor serum – Transience of autoantibody (may be only present in plasma for a few days)
Differential diagnosis • Cold agglutinin syndrome – Typically Ig. M with specificity of anti-I or anti-i – Thermal amplitude >30°C and titer>1: 500

Management • Acute DL-HA usually resolves spontaneously and completely within several weeks • Usually does not recur • Treatment is supportive – Patient should be kept warm – Transfusion if severe anemia; use blood warmer • Steroids have been given in cases, but effectiveness of therapy may be difficult to evaluate • In rare cases of life-threatening anemia, plasmapheresis has been used to acutely remove Ig. G antibodies
Back to the patient • The Blood Bank team convinced the clinical team of the low utility of performing the D-L test.
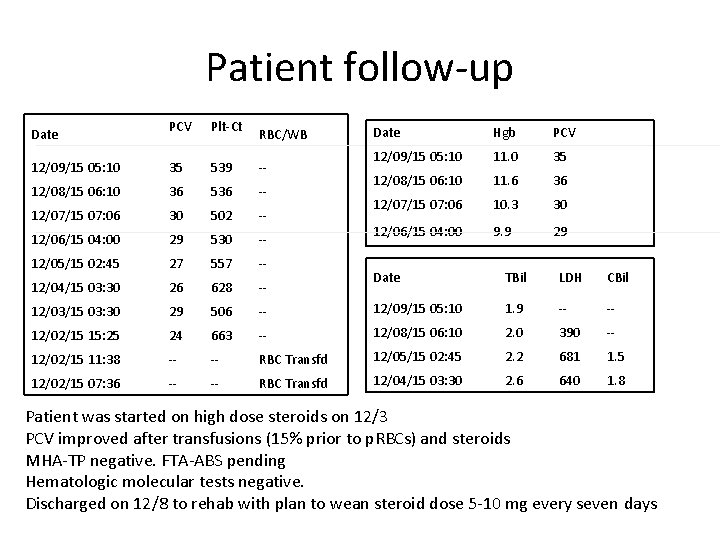
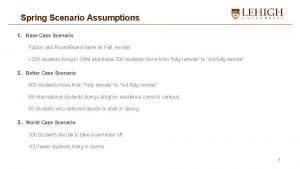
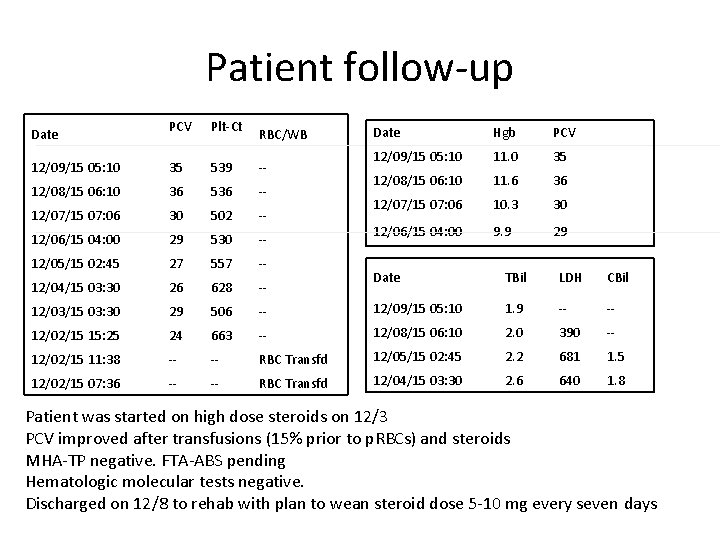
Patient follow-up Date PCV Plt-Ct RBC/WB 12/09/15 05: 10 35 539 -- 12/08/15 06: 10 36 536 -- 12/07/15 07: 06 30 502 -- 12/06/15 04: 00 29 530 -- 12/05/15 02: 45 27 557 -- 12/04/15 03: 30 26 628 -- 12/03/15 03: 30 29 506 12/02/15 15: 25 24 12/02/15 11: 38 12/02/15 07: 36 Date Hgb PCV 12/09/15 05: 10 11. 0 35 12/08/15 06: 10 11. 6 36 12/07/15 07: 06 10. 3 30 12/06/15 04: 00 9. 9 29 Date TBil LDH CBil -- 12/09/15 05: 10 1. 9 -- 663 -- 12/08/15 06: 10 2. 0 390 -- -- RBC Transfd 12/05/15 02: 45 2. 2 681 1. 5 -- RBC Transfd 12/04/15 03: 30 2. 6 640 1. 8 Patient was started on high dose steroids on 12/3 PCV improved after transfusions (15% prior to p. RBCs) and steroids MHA-TP negative. FTA-ABS pending Hematologic molecular tests negative. Discharged on 12/8 to rehab with plan to wean steroid dose 5 -10 mg every seven days
References • Eder AF. Review: acute Donath-Landsteiner hemolytic anemia. Immunohematology. 2005; 21(2): 56 -62. • Rausen AR, Le. Vine R, Hsu TC, Rosenfield RE. Compatible transfusion therapy for paroxysmal cold hemoglobinuria. Pediatrics. 1975 Feb; 55(2): 275 -8. • Sokol RH, Hewitt S, Stamps BK, et al. Autoimmune haemolysis in childhood and adolescence. Acta Haematol. 1984; 72: 245– 257. • Sokol RJ, Booker DJ, Stamps R. Erythropoiesis: Paroxysmal Cold Haemoglobinuria: A Clinico-Pathological Study of Patients with a Positive Donath-Landsteiner Test. Hematology. 1999; 4(2): 137 -164. • Heddle NM. Acute paroxysmal cold hemoglobinuria. Transfus Med Rev. 1989; 3: 219– 229.
 Interesting more interesting the most interesting
Interesting more interesting the most interesting Xuan wang md
Xuan wang md Case scenario
Case scenario Contoh use case scenario
Contoh use case scenario Hypertensive crisis classification
Hypertensive crisis classification Use case description
Use case description Use case scenario contoh
Use case scenario contoh Ciria
Ciria Define use case
Define use case Use case scenario example
Use case scenario example Tension pneumothorax case scenario
Tension pneumothorax case scenario Contoh diagram use case
Contoh diagram use case Nursing care plan case scenario
Nursing care plan case scenario Xuan long
Xuan long Những cây nào sau đây thuộc cây ngắn ngày
Những cây nào sau đây thuộc cây ngắn ngày Thúy vân chợt tỉnh giấc xuân
Thúy vân chợt tỉnh giấc xuân Xuan mei
Xuan mei Xuan cao md
Xuan cao md Vua nào thần tốc quân hành
Vua nào thần tốc quân hành Luna_xuany
Luna_xuany Xuan vs peacock
Xuan vs peacock Xuan kong si
Xuan kong si Angel x chang
Angel x chang Xuân 1975
Xuân 1975