Injury to the Collateral Cartilage and Collateral Ligament
- Slides: 37
Injury to the Collateral Cartilage and Collateral Ligament of the Distal Interphalangeal Joint Intern: Laura A. Axiak, DVM* Mentor: Natasha M. Werpy, DVM, Dipl. ACVR** University of Florida Large Animal Clinical Sciences* Diagnostic Imaging Department**
Signalment & History • 11 year old Warmblood gelding • Event horse with long history of good performance • Problem: right forelimb lameness of 3 months duration • Previous treatment: routine coffin joint injections of both forelimbs
Lameness Examination • Straight trot on hard ground – Grade 2. 5/5 right forelimb • Circling on hard ground – Right forelimb lameness is exacerbated circling to the right • Palpation – No significant sensitivities identified • Flexion Test – Negative to proximal and distal limb flexion • Hoof Testers – No response
Lameness Video
Circling Left
Circling Right
Diagnostic Analgesia • RF Palmar Digital Nerve Block – 90% improvement • RF Abaxial Sesamoid Nerve Block – no additional improvement • Lameness did not switch to left forelimb
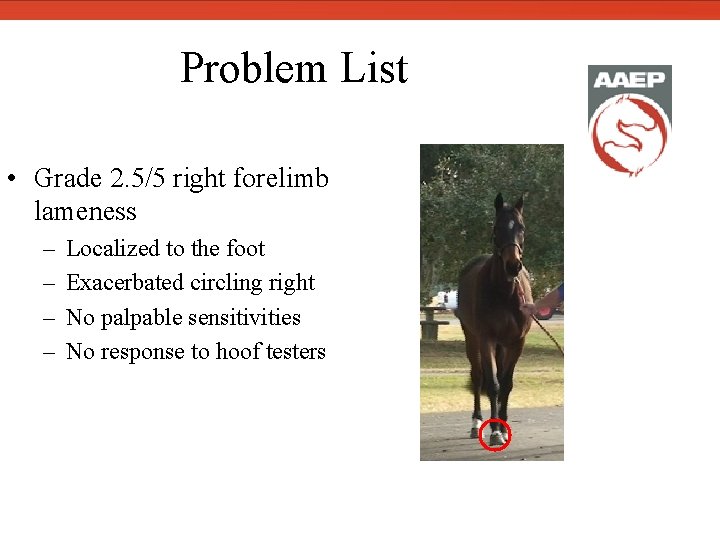
Problem List • Grade 2. 5/5 right forelimb lameness – – Localized to the foot Exacerbated circling right No palpable sensitivities No response to hoof testers
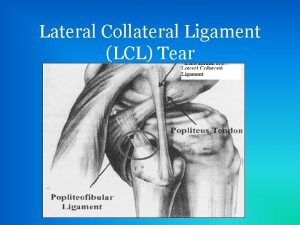
Differential Diagnoses • Lesions causing foot lameness are primarily caused by degenerative or traumatic injury localized to these structures: 1 – Bones: navicular bone, middle phalanx, distal phalanx – Tendons: deep digital flexor tendon, common digital extensor tendon – Ligaments: collateral sesamoidean ligament, impar ligament, collateral ligaments of the distal interphalangeal joint, distal digital annular ligament, chondrocoronal ligaments – Synovial structures: distal interphalangeal joint, navicular bursa, distal aspect of the digital tendon sheath • Other differentials may include foot pain, laminitis, keratoma, space occupying lesions, abscess or infection
Diagnostic Plan • Radiographs of the Foot – Lateral Projection • Survey view of the distal phalanx, middle phalanx, navicular bone and articular surfaces – Horizontal DP Projection • Used to evaluate the distal interphalangeal joint space – 65 -degree Dorsoproximal-Palmarodistal Oblique • Aids in evaluation of the distal margin of the navicular bone – Palmaroproximal-Palmarodistal Oblique (Skyline) • Used to evaluate the navicular bone flexor surface and corticomedullary distinction in the navicular bone, as well as the palmar processes of the distal phalanx • Ultrasound • Advanced Imaging (MRI or CT)
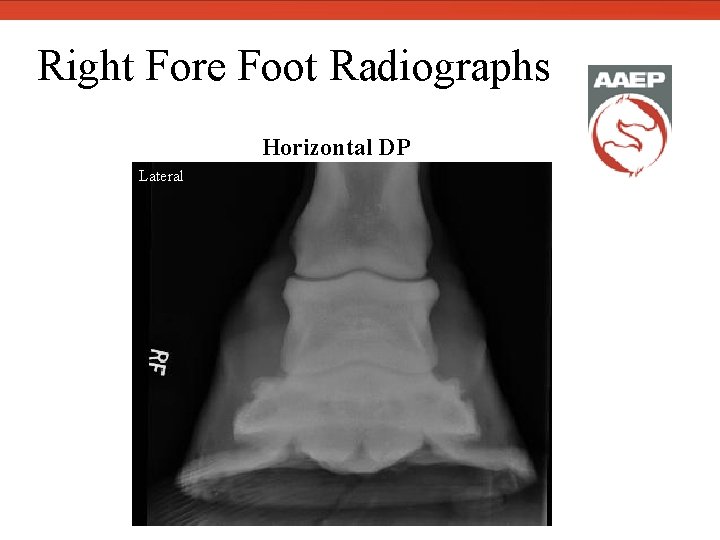
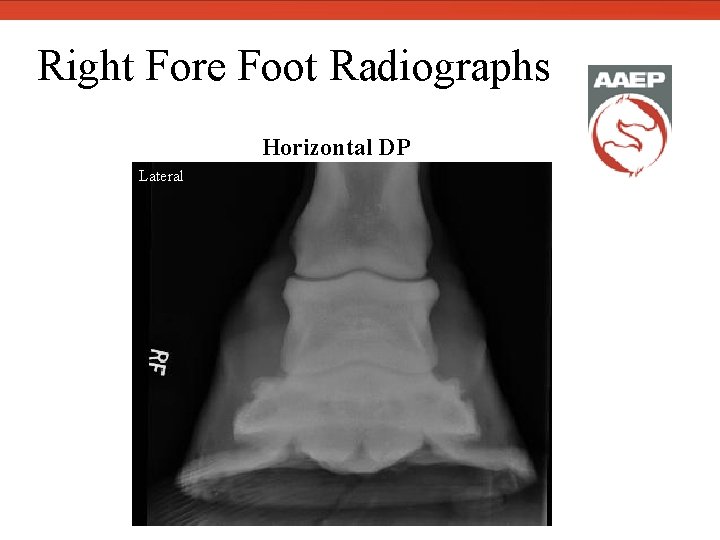
Right Fore Foot Radiographs Lateral Horizontal DP
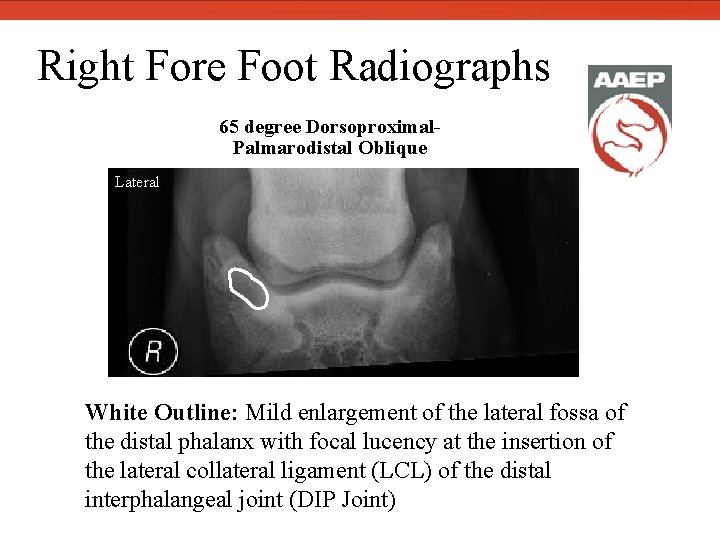
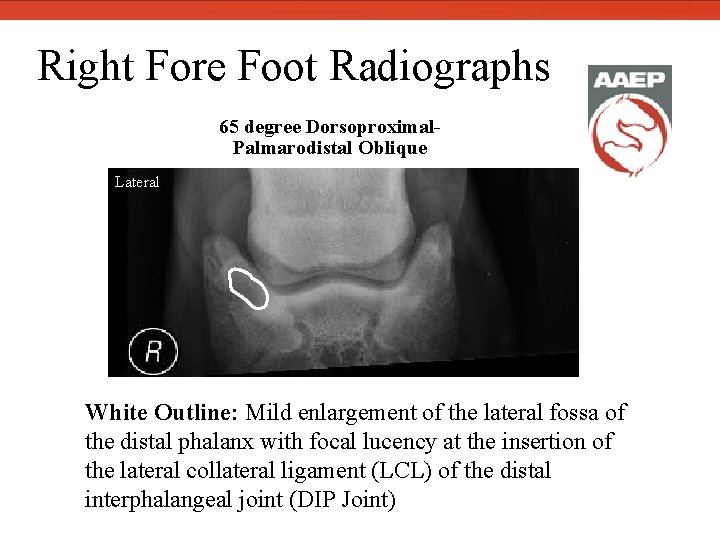
Right Fore Foot Radiographs 65 degree Dorsoproximal. Palmarodistal Oblique Lateral White Outline: Mild enlargement of the lateral fossa of the distal phalanx with focal lucency at the insertion of the lateral collateral ligament (LCL) of the distal interphalangeal joint (DIP Joint)
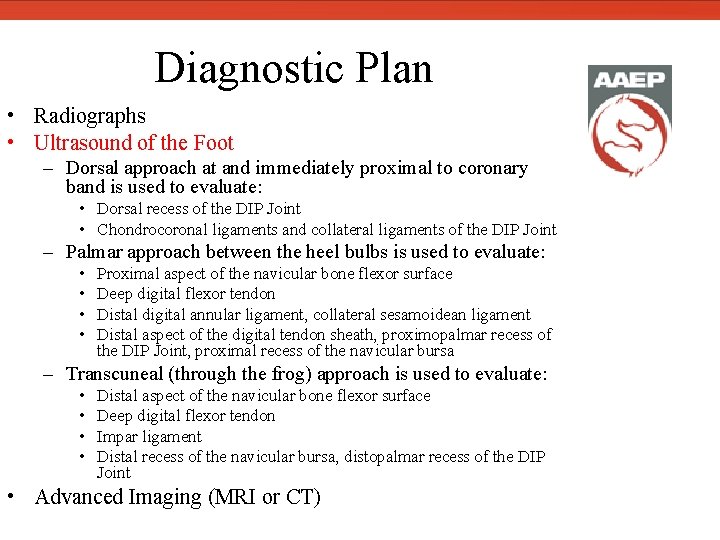
Diagnostic Plan • Radiographs • Ultrasound of the Foot – Dorsal approach at and immediately proximal to coronary band is used to evaluate: • Dorsal recess of the DIP Joint • Chondrocoronal ligaments and collateral ligaments of the DIP Joint – Palmar approach between the heel bulbs is used to evaluate: • • Proximal aspect of the navicular bone flexor surface Deep digital flexor tendon Distal digital annular ligament, collateral sesamoidean ligament Distal aspect of the digital tendon sheath, proximopalmar recess of the DIP Joint, proximal recess of the navicular bursa – Transcuneal (through the frog) approach is used to evaluate: • • Distal aspect of the navicular bone flexor surface Deep digital flexor tendon Impar ligament Distal recess of the navicular bursa, distopalmar recess of the DIP Joint • Advanced Imaging (MRI or CT)
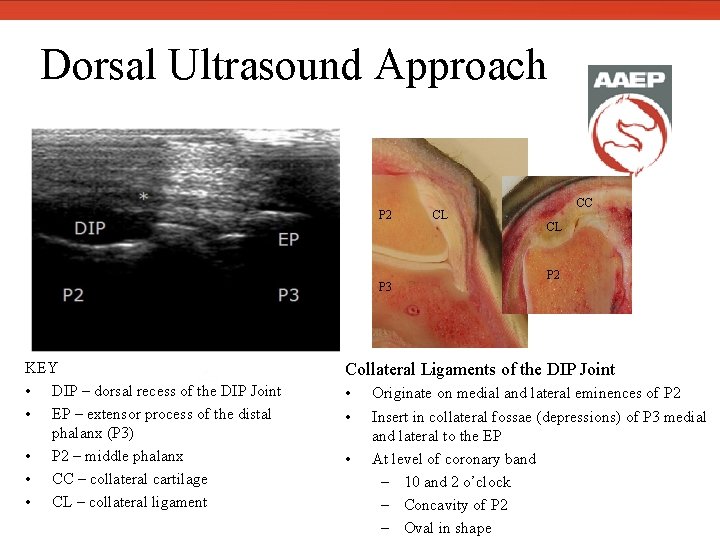
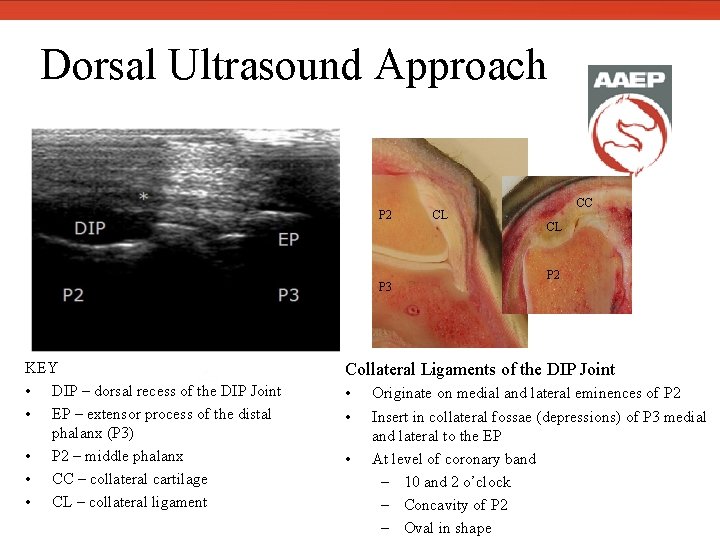
Dorsal Ultrasound Approach P 2 P 3 KEY • DIP – dorsal recess of the DIP Joint • EP – extensor process of the distal phalanx (P 3) • P 2 – middle phalanx • CC – collateral cartilage • CL – collateral ligament CL CC CL P 2 Collateral Ligaments of the DIP Joint • • • Originate on medial and lateral eminences of P 2 Insert in collateral fossae (depressions) of P 3 medial and lateral to the EP At level of coronary band – 10 and 2 o’clock – Concavity of P 2 – Oval in shape
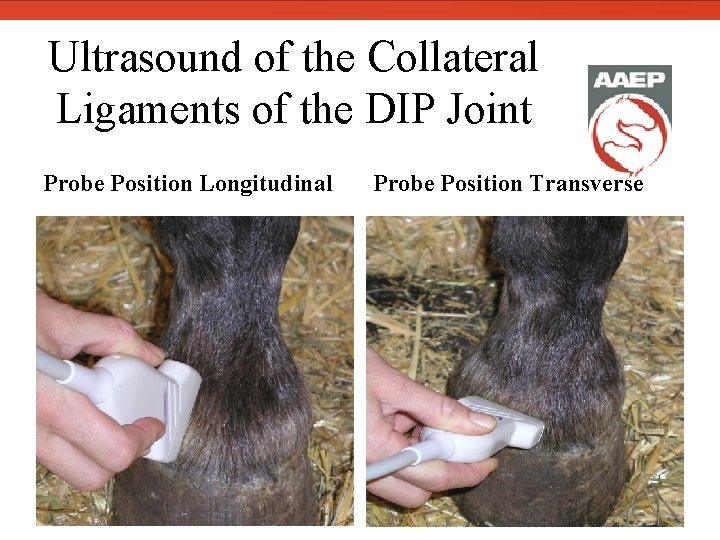
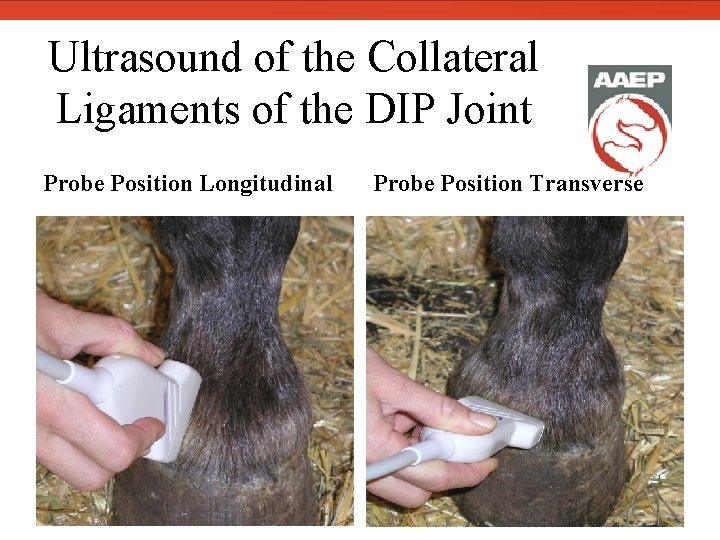
Ultrasound of the Collateral Ligaments of the DIP Joint Probe Position Longitudinal Dorsal recess of DIP Joint Probe Position Transverse
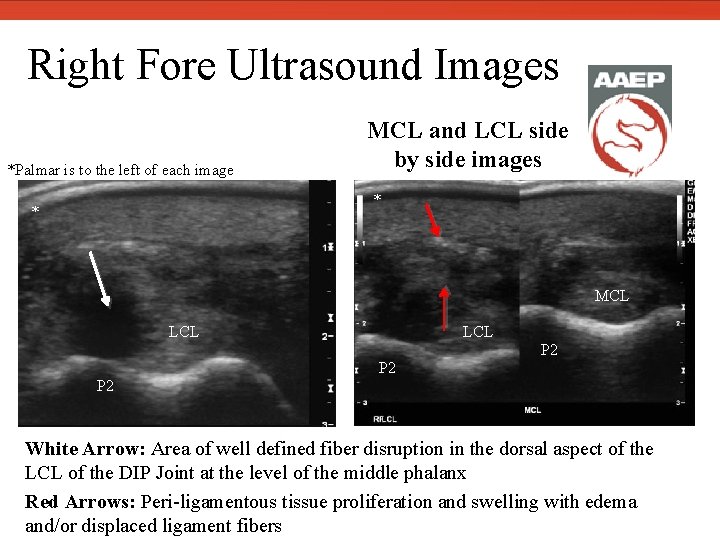
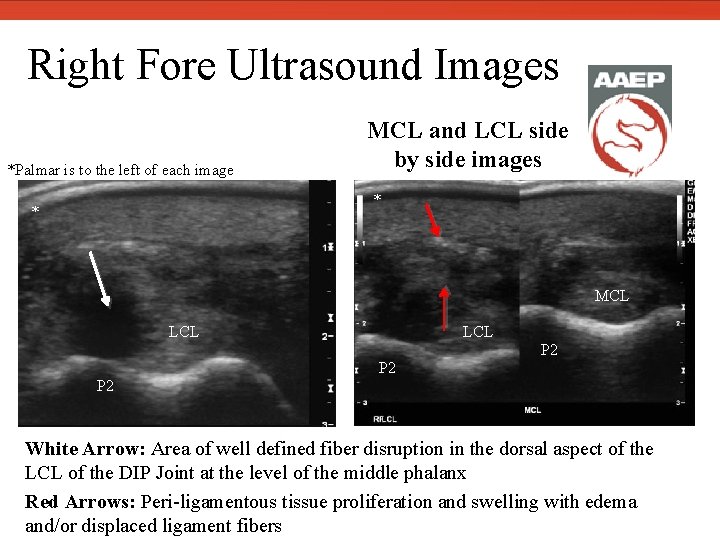
Right Fore Ultrasound Images *Palmar is to the left of each image MCL and LCL side by side images * * MCL LCL P 2 P 2 White Arrow: Area of well defined fiber disruption in the dorsal aspect of the LCL of the DIP Joint at the level of the middle phalanx Red Arrows: Peri-ligamentous tissue proliferation and swelling with edema and/or displaced ligament fibers
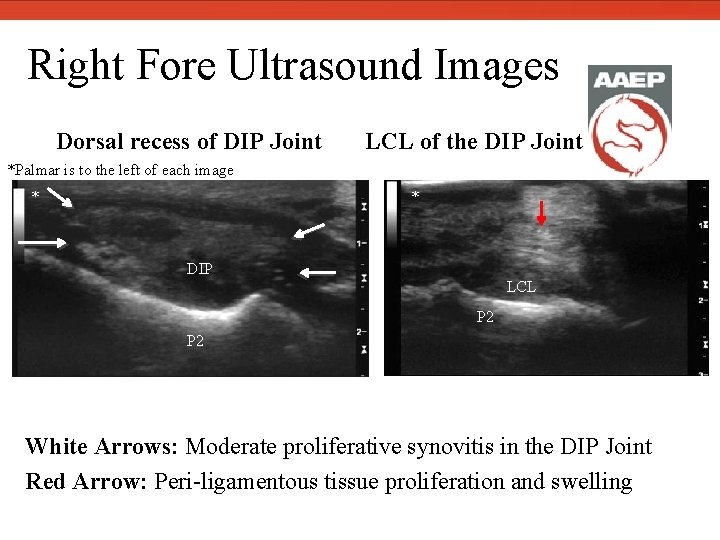
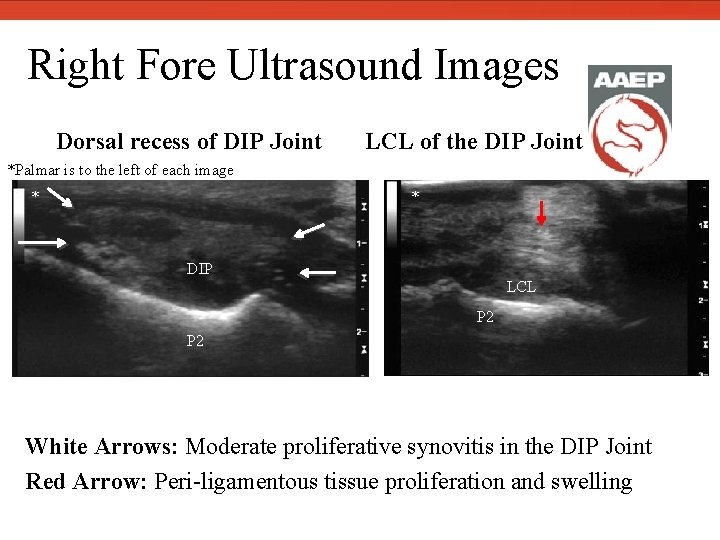
Right Fore Ultrasound Images Dorsal recess of DIP Joint LCL of the DIP Joint *Palmar is to the left of each image * * DIP LCL P 2 Dorsal recess of DIP Joint White Arrows: Moderate proliferative synovitis in the DIP Joint Red Arrow: Peri-ligamentous tissue proliferation and swelling
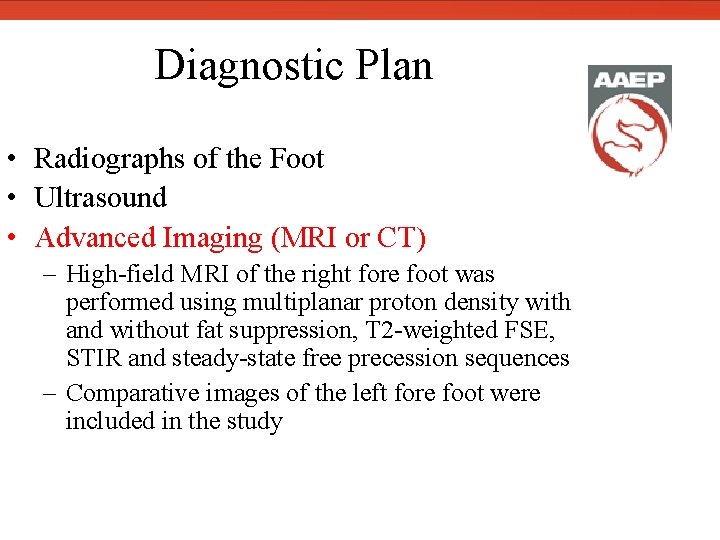
Diagnostic Plan • Radiographs of the Foot • Ultrasound • Advanced Imaging (MRI or CT) – High-field MRI of the right fore foot was performed using multiplanar proton density with and without fat suppression, T 2 -weighted FSE, STIR and steady-state free precession sequences – Comparative images of the left fore foot were included in the study
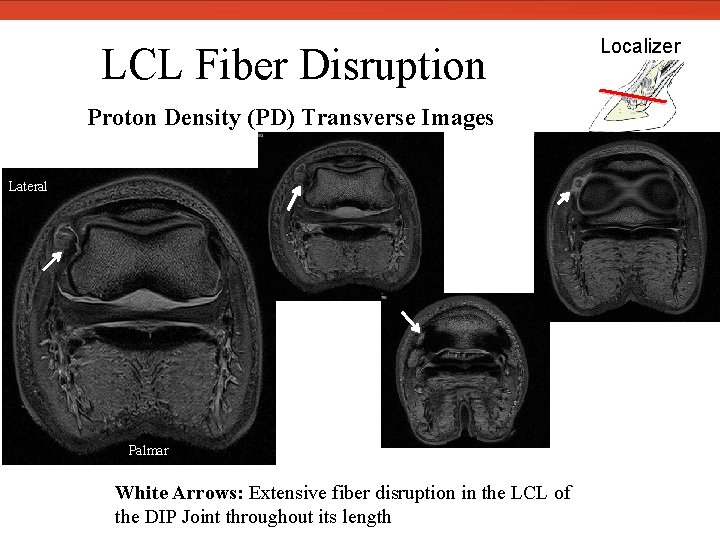
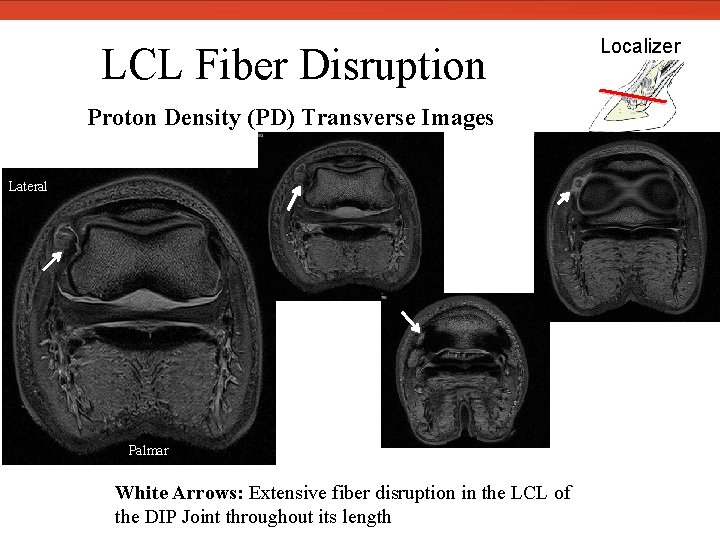
LCL Fiber Disruption Proton Density (PD) Transverse Images Lateral Palmar White Arrows: Extensive fiber disruption in the LCL of the DIP Joint throughout its length Localizer
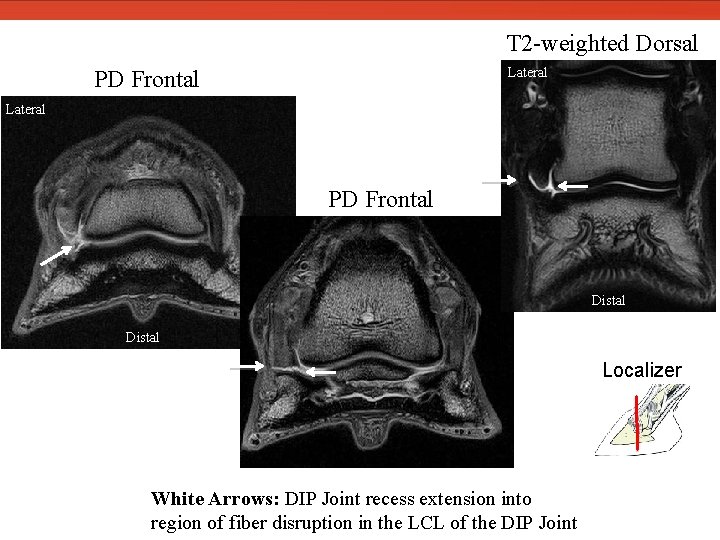
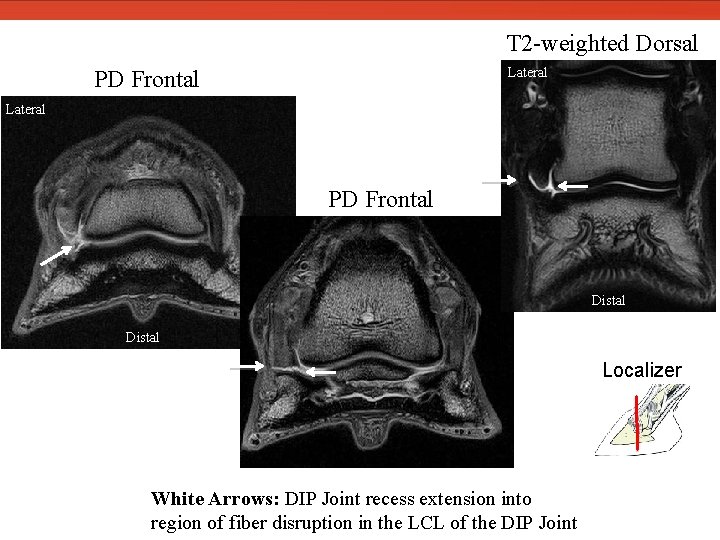
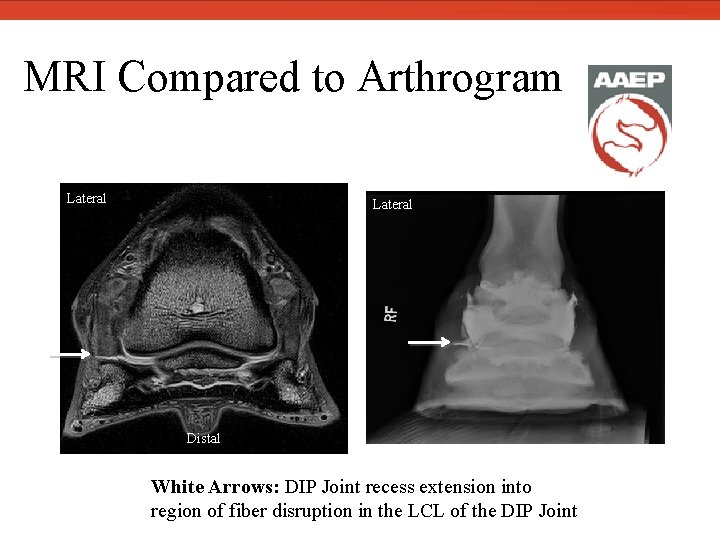
T 2 -weighted Dorsal Lateral PD Frontal Distal Localizer White Arrows: DIP Joint recess extension into region of fiber disruption in the LCL of the DIP Joint
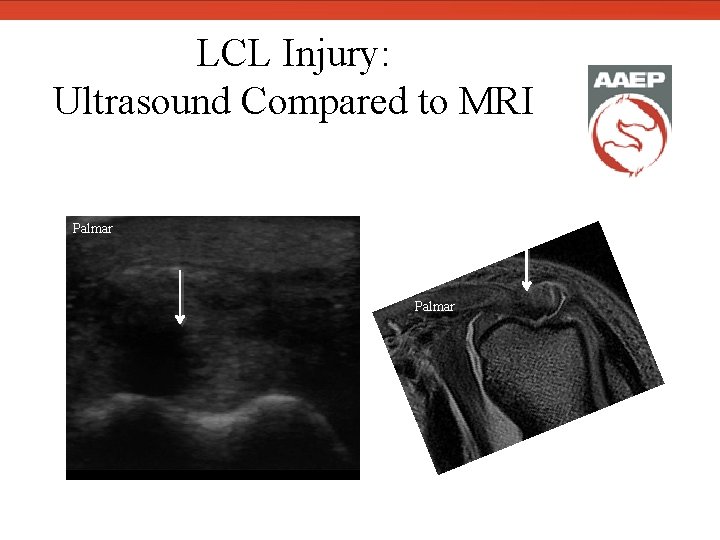
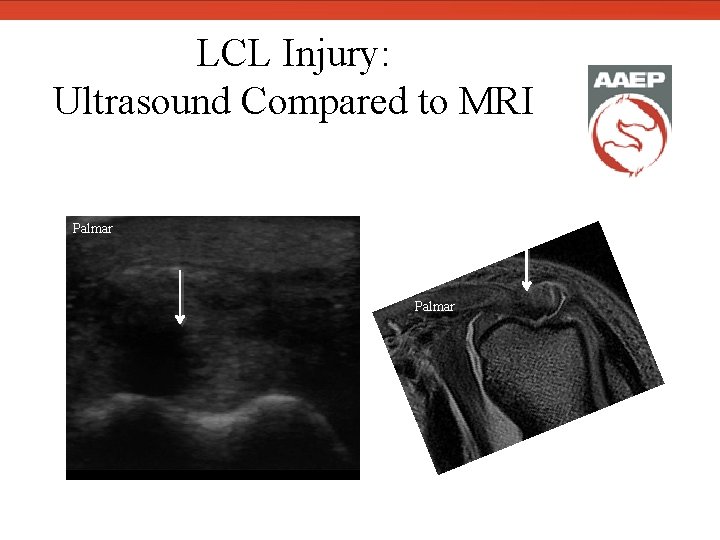
LCL Injury: Ultrasound Compared to MRI Palmar
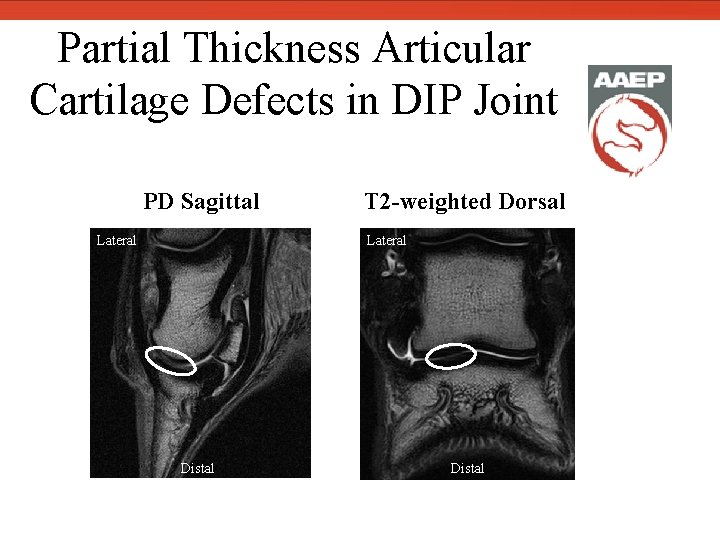
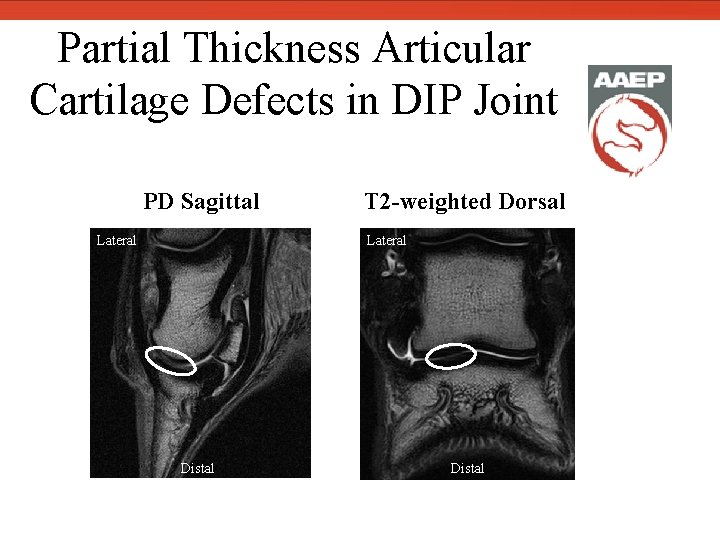
Partial Thickness Articular Cartilage Defects in DIP Joint PD Sagittal Lateral T 2 -weighted Dorsal Lateral Distal
MRI Diagnosis • Extensive fiber disruption in the LCL of the DIP Joint throughout its length • Separation of the lateral collateral cartilage (LCC) from the lateral palmar process of the distal phalanx • DIP Joint recess extends into region of fiber disruption in the LCL of the DIP Joint in the area where the LCC is separated from the distal phalanx • Mild to moderate resorption of the lateral fossa of the distal phalanx
Additional MRI Findings • Moderate proliferative synovitis in the DIP Joint • Mild to moderate multifocal partial thickness articular cartilage defects in the DIP Joint with moderate proliferative synovitis
Comments • The alterations in the fluid distribution and the appearance of fiber disruption are likely explained by the differences between weight bearing US images and non-weight bearing MRI images
Positive Contrast Arthrogram (PCA) of the DIP Joint • PCA performed post-MRI as a possible method for monitoring healing, to aid in determining the best time frame for a recheck MRI and to confirm communication with DIP Joint
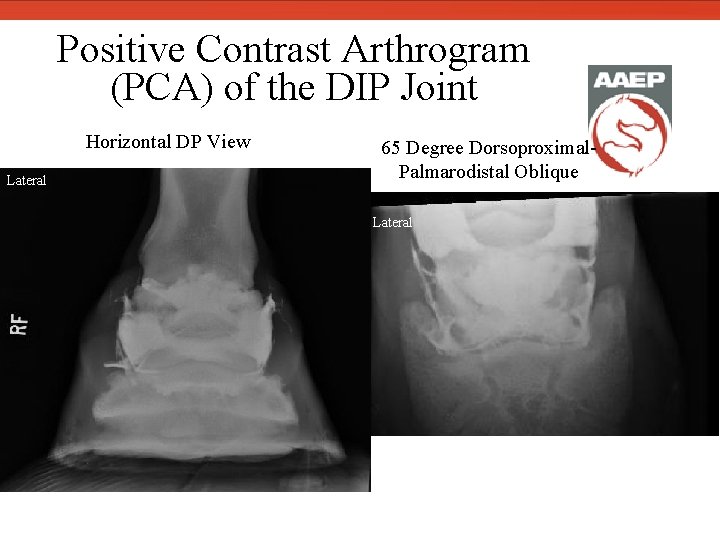
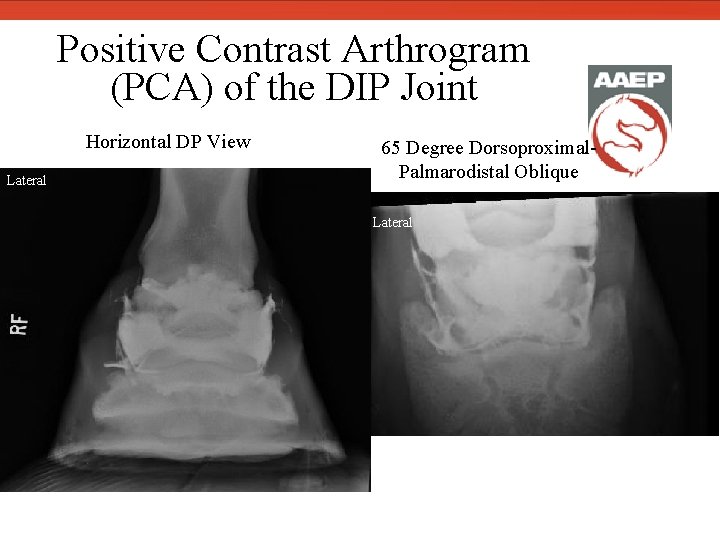
Positive Contrast Arthrogram (PCA) of the DIP Joint Horizontal DP View Lateral 65 Degree Dorsoproximal. Palmarodistal Oblique Lateral
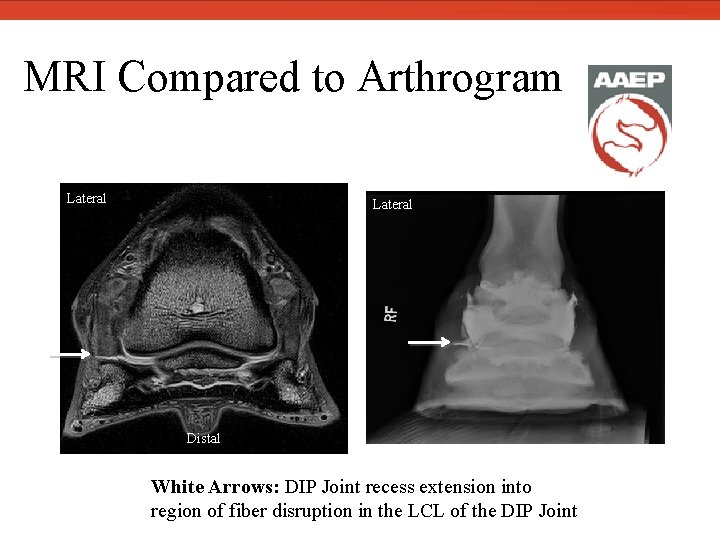
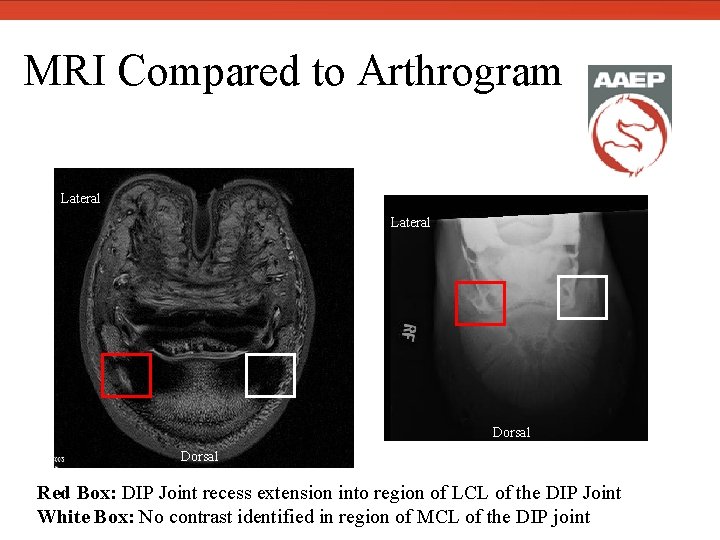
MRI Compared to Arthrogram Lateral Distal White Arrows: DIP Joint recess extension into region of fiber disruption in the LCL of the DIP Joint
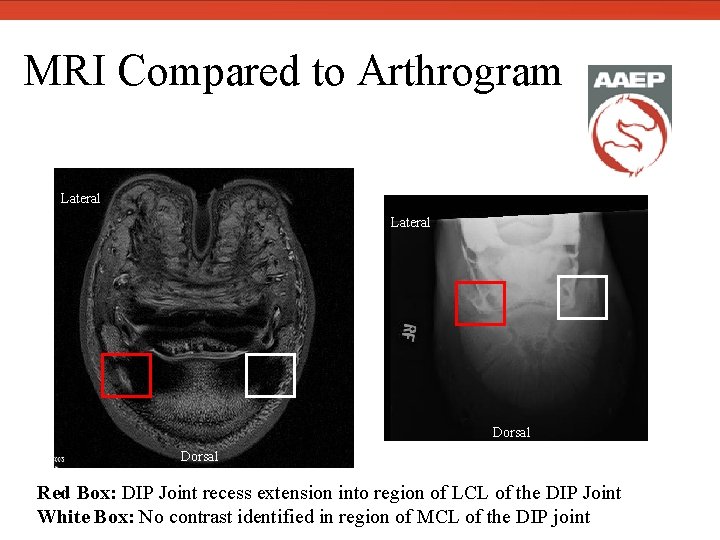
MRI Compared to Arthrogram Lateral Dorsal Red Box: DIP Joint recess extension into region of LCL of the DIP Joint White Box: No contrast identified in region of MCL of the DIP joint
Therapeutic Plan • Treatment: Ultrasound-guided intralesional injection of lateral collateral ligament of the DIP joint with regenerative therapies (stem cells or PRP) • Rehabilitation Program: Rest and hand walking for 4 -6 months with recheck diagnostic imaging before any increase in exercise
Prognosis • LCL and LCC injury is severe representing permanent structural injury • Extensive fiber disruption in LCL with dorsal DIP joint extension into lesion will have a prolonged healing time • Prognosis for return to previous level of exercise is fair to poor
Discussion • Injuries to the collateral ligament of the DIP Joint occur frequently in the axial margin towards the palmar aspect of the ligament at the insertion on the distal phalanx. 2, 3 • Associated osseous abnormalities may include enthesophyte formation, bone fluid, bone loss or the development of an osseous cyst-like lesion. 4
• Osseous injuries are reported to have a higher incidence in the distal phalanx immediately distal and palmar to the insertion of the collateral ligament rather 3, 5 than at the origin on the middle phalanx. • Infrequently, it may be possible to see these changes radiographically, but the majority of these injuries are diagnosed using MRI. 4
• In our experience, collateral ligament tears are frequently occupied by the DIP Joint recesses, especially when located at the level of the DIP Joint or the distal phalanx. • A PCA could be a consideration in cases with an osseous cyst-like lesion on radiographs and ultrasound abnormalities that are not able to have a MRI study. • In addition, this case demonstrates injury to the collateral cartilage in conjunction with collateral ligament injury.
Outcome • We have seen several cases. However, only two cases have had a recheck MRI study. – On a 7 month post-injury recheck MRI the collateral ligament had improved, but still had significant abnormalities. – However, the collateral cartilages remained fully separated from the distal phalanx and this space was occupied by the DIP Joint recess.
Acknowledgements • The authors would like to acknowledge Dr. Christiana Ober and Dr. Lisa Casinella for referring this interesting case.
Further Reading & References 1. 2. 3. 4. 5. Vallance SA, Bell RJ, Spriet M, et al. Comparisons of computed tomography, contrast-enhanced computed tomography and standing low-field magnetic resonance imaging in horses with lameness localised to the foot. Part 2: Lesion identification. Equine Vet J. 2012; 44: 149 -56. Gutierrez-Nibeyro SD, White NA, Werpy NM, et al. Magnetic resonance imaging findings of desmopathy of the collateral ligaments of the equine distal interphalangeal joint. Vet Rad & Ultrasound. 2009; 50: 21 -31. Dyson S, Blunden T, Murray R. The collateral ligaments of the distal interphalangeal joint: Magnetic resonance imaging and post mortem observations in 25 lame and 12 control horses. Equine Vet J. 2008; 40: 538 -544. Dakin SG, Dyson SJ, Murray RC, et al. Osseous abnormalities associated with collateral desmopathy of the distal interphalangeal joint: Part 1. Equine Vet J. 2009; 41: 786 -793. Dyson SJ, Murray R, Schramme M, et al. Collateral desmitis of the distal interphalangeal joint in 18 horses (2001 -2002). Equine Vet J. 2004; 36: 160 -166.
 Biomechanics of throwing a football
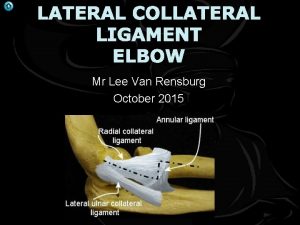
Biomechanics of throwing a football Ligament collateral radial
Ligament collateral radial Radial collateral ligament
Radial collateral ligament Radial collateral ligament
Radial collateral ligament Intentional and unintentional injury
Intentional and unintentional injury Xborder funding mc
Xborder funding mc Cricoid cartilage and suprasternal notch
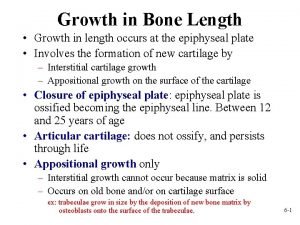
Cricoid cartilage and suprasternal notch Epiphyseal plate
Epiphyseal plate Periosteum and endosteum of bone
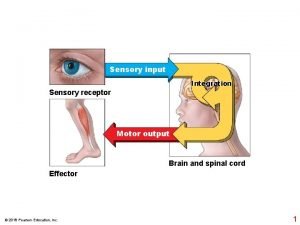
Periosteum and endosteum of bone Depolarization
Depolarization Definition of collateral beauty
Definition of collateral beauty Collateral estoppel definition
Collateral estoppel definition Condition is a stipulation that is
Condition is a stipulation that is Chapter 21 hemodynamics
Chapter 21 hemodynamics Collateral estoppel definition
Collateral estoppel definition Dorsal scapular artery
Dorsal scapular artery Collateral superficial veins definition
Collateral superficial veins definition What is triparty collateral management
What is triparty collateral management E4 evaluation examples
E4 evaluation examples Character capacity collateral
Character capacity collateral Collateral management framework
Collateral management framework European collateral management system
European collateral management system Sample of collateral reading
Sample of collateral reading Leveraged loan monthly
Leveraged loan monthly Collateral sulcus
Collateral sulcus Collateral management
Collateral management Pericardiophrenic artery
Pericardiophrenic artery Collateral evaluation
Collateral evaluation Thyrohyoid membrane
Thyrohyoid membrane Salivary gland
Salivary gland Lobar bronchus
Lobar bronchus Hyaline cartilage in nose
Hyaline cartilage in nose Conus elasticus larynx
Conus elasticus larynx Meckel's cartilage
Meckel's cartilage Cricoid cartilage
Cricoid cartilage What type of joint is the intervertebral joint
What type of joint is the intervertebral joint Perichondrium
Perichondrium Mcq cartilage
Mcq cartilage