Infection of lower genital Tract PID Lateefa Al


- Slides: 16
Infection of lower genital Tract & PID Lateefa Al Dakhyel FRCSC, FACOG Assistant professor & consultant Obstetric & gynecology department Collage of medicine King Saud University

Bacterial Vaginosis (BV) • Most common cause of vaginitis in premenopausal women • It is caused by alteration of the normal flora, with over-growth of anaerobic bacteria • It is triggered by ↑ PH of the vagina (intercourse, douches) • Recurrences are common • 50% are asymptomatic • Itching and inflammation are uncommon • It is not a STD Complications • Increases risk for: – – – Preterm labor in pregnant women Endometritis and postpartum fever Post-hysterectomy vaginal-cuff cellulitis Postabortal infection Acquiring other STDs, especially HIV
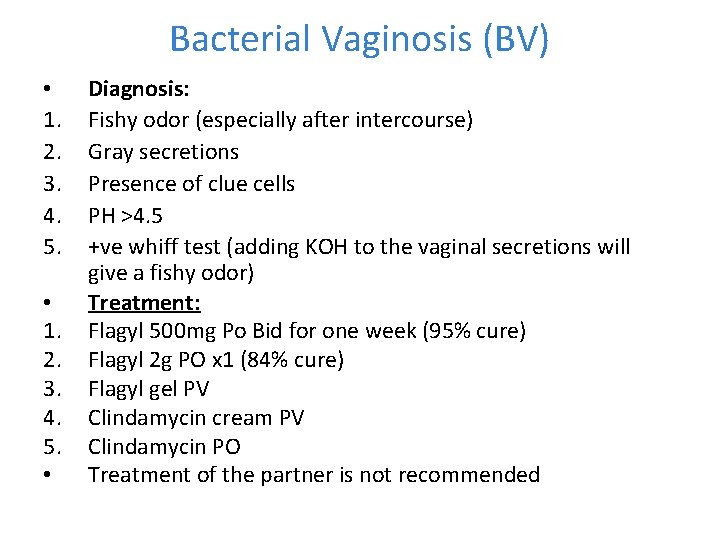
Bacterial Vaginosis (BV) • 1. 2. 3. 4. 5. • Diagnosis: Fishy odor (especially after intercourse) Gray secretions Presence of clue cells PH >4. 5 +ve whiff test (adding KOH to the vaginal secretions will give a fishy odor) Treatment: Flagyl 500 mg Po Bid for one week (95% cure) Flagyl 2 g PO x 1 (84% cure) Flagyl gel PV Clindamycin cream PV Clindamycin PO Treatment of the partner is not recommended
Candidiasis • • 75% of women will have at least once during their life 45% of women will have two or more episodes/year 15% have chronic infection Rare before menarche, but 50% will have it by age 25 Less common in postmenopausal women, unless taking estrogen It is not a. STD 90% of yeast infections are secondary to Candida Albican Other species (glabrata, tropicalis) tend to be resistant to treatment Predisposing factors: 1. Antibiotics: disrupting the normal flora by ↓ lactobacilli 2. Pregnancy (↓ cell-mediated immunity) 3. Diabetes 4. OCP 5. Disinfecting the vagina
Candidiasis “diagnosis” 1. 2. 3. 4. 5. 6. 7. 8. Vulvar pruritis and burning The discharge vary from watery to thick cottage cheese discharge Vaginal soreness and dysparunea Splash dysuria O/E: erythema and edema of the labia and vulva The vagina may be erythematous with adherent whitish discharge Cervix is normal PH< 4. 5 budding yeast or mycelia on microscopy Treatment: 1. 2. 3. 4. Topical Azole drugs (80 -90% effective) Fluconazole is equally effective (Diflucan 150 mg PO x 1), but symptoms will not disappear for 2 -3 days 1% hydrocortisone cream may be used as an adjuvant treatment for vulvar irritation Chronic infections may need long-term treatment (6 months) with weekly Fluconazole Trichomonas Vaginalis • • • It is an anaerobic parasite, that exists only in trophozite form 3 rd most common vaginitis 60% of patients also have BV 70% of males will contract the disease with single exposure Virtually always sexually transmitted Patients should be tested for other STDs (HIV, Syphilis, hepatitis)
Trichomonas Vaginalis Diagnosis: 1. Profuse, purulent malodorous discharge 2. It may be accompanied by vulvar pruritis 3. Secretions may exudate from the vagina 4. If severe → patchy vaginal edema and strawberry cervix 5. PH >5 6. Microscopy: motile trichomands and ↑ leukocytes 7. Clue cells may if BV is present 8. Whiff test may be +ve Treatment: 1. Falgyl PO (single or multi dose) 2. Flagyl gel is not effective 3. The partner should be treated 4. If refractory to treatment Other Causes of Vaginitis • Atrophic vaginitis (in post menopausal women) • Atypical manifestations: HSV, HPV • Noninfectious vulvovaginitis
Herpes Simplex Virus • The “silent epidemic” • > 45 million in the US • > 1 million newly diagnosed annually • The most common STD in US, and likely the world • Almost 25% of Americans have HSV 2 antibodies by the age of 30 • HSV – 1 • HSV – 2 Primary Herpes – Classic Symptoms • Systemic – fever, myalgia, malaise • Can have meningitis, encephalitis, or hepatitis Local – clusters of small, painful blisters that ulcerate and crust outside of mucous membranes Itching, dysuria, vaginal discharge, inguinal adenopathy, bleeding from cervicitis New lesions form for about 10 days after initial infection, but can last up to 3 weeks • Shedding of virus lasts 2 – 10 days Recurrent Herpes • Reactivation of virus • Mild, self-limited • Localized, lasting 6 -7 days • Shedding: 4 -5 days • Prodrome: 1 -2 days •
Diagnosis • Viral isolation (culture) • Direct detection of virus (Tzcank smears, PCR) • Serology Management Goals • Relieve symptoms • Heal lesions • Reduce frequency of recurrent episodes • Reduce viral transmission • Patient support and counseling Oral Antiviral Therapy • Valacyclovir (Valtrex) • Famciclovir (Famvir) • Acyclovir (Zovirax) Cervicitis • My cause abnormal vaginal discharge , postcoital bleeding or irregular bleeding • Neisseria Gonorrhea and Chlamydia Trachomatis infect only the glandular epithelium and are responsible for mucopurulent endocervisitis (MPC) • Ectocx epithelium is continuous with the vaginal epithelium, so Trichomonas, HSV and Candida may cause ectocx inflammation
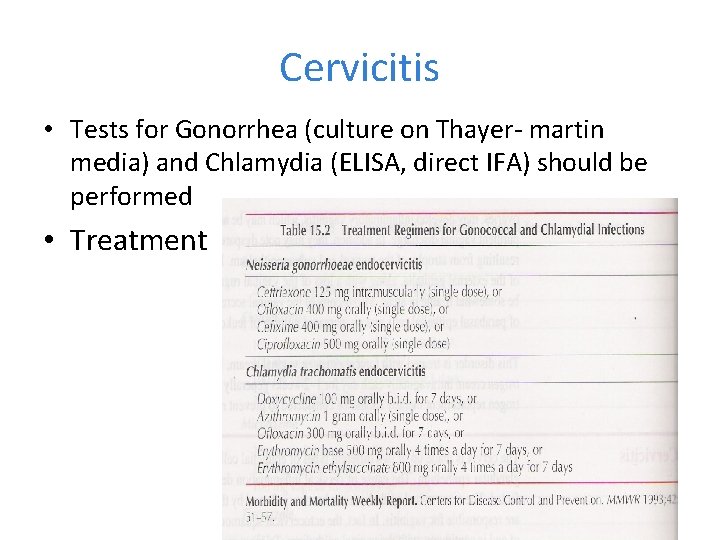
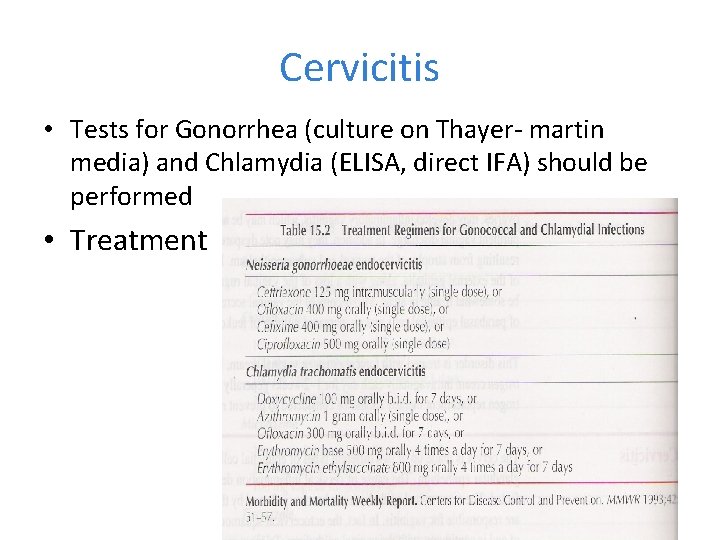
Cervicitis • Tests for Gonorrhea (culture on Thayer- martin media) and Chlamydia (ELISA, direct IFA) should be performed • Treatment
Pelvic Inflammatory Disease (PID) • • • Ascending infection, ? Up to the peritoneal cavity Organisms: Chlamydia, N Gonorrhea Less often: H Influenza, group A Strept, Pneumococci, E-coli acute PID 1 -2% of young sexually active women each year 85% because of STD- 15% occur after procedures that break cervical mucous barrier PID • Diagnosis: difficult because of wide variation of signs and symptoms • Clinical triad: pelvic pain (90%) , cervical motin & adnexal tenderness • fever • Cervical motion tenderness indicate peritoneal inflammation • Patients may or may not have mucopurulent discharge • leukocytosis • • 75% asso. endocervical infection & coexist purulent vaginal d/c Fitz-Hugh-Curtis syndrome : Differential Diagnosis • acute appendicitis • Endometriosis • torsion/rupture adx mass • ectopic preg • lower genital tract infection

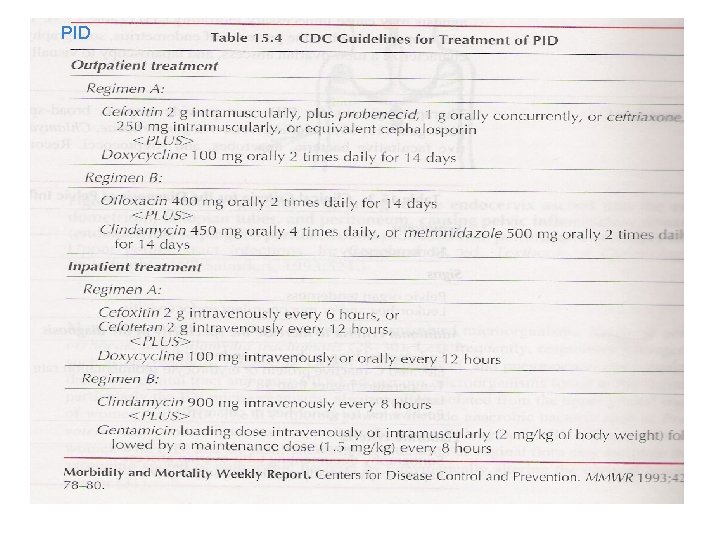
Risk factors Sexual behavior others – IUD user (multifilament string – surgical procedure – previous acute PID • Reinfection untreated male partners 80% • Decrease risk - barrier method - OC Sequelae • Infertility~20% • Ectopic pregnancy ~6 fold increase • Chronic pelvic pain • TOA~ 10% • Mortality -acute 1% -after rupture TOA ~10% Medication • Empirical ABx cover wide range of bacteria • Treatment start as soon as culture & diagnosis is confirmed/suspected - failure rate, OPD oral ATB 10 -20% - failure rate, IPD iv ATB 5 -10% • reevaluate 48 -72 hrs of initial OPD therapy • •
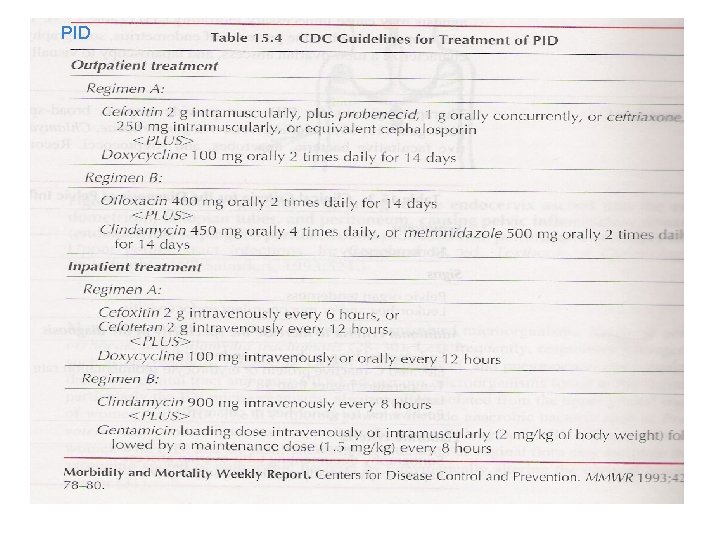
PID
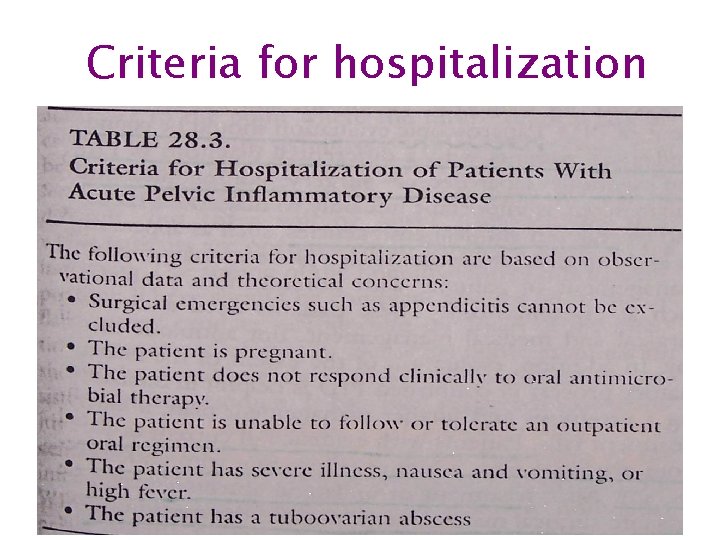
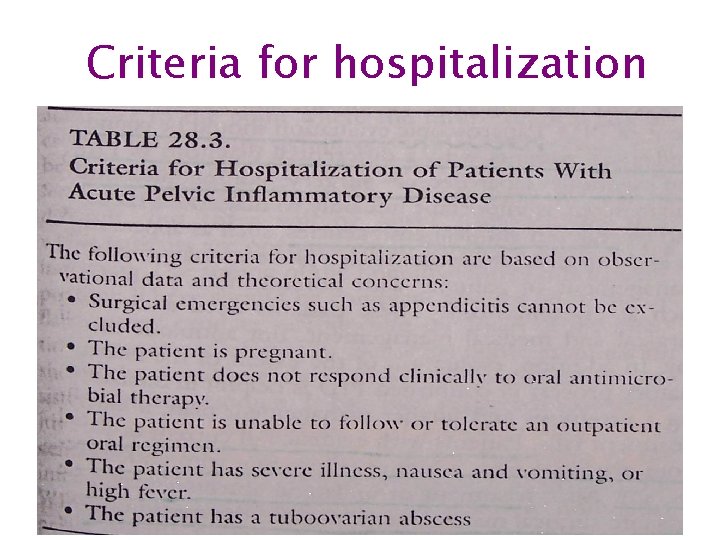
Criteria for hospitalization
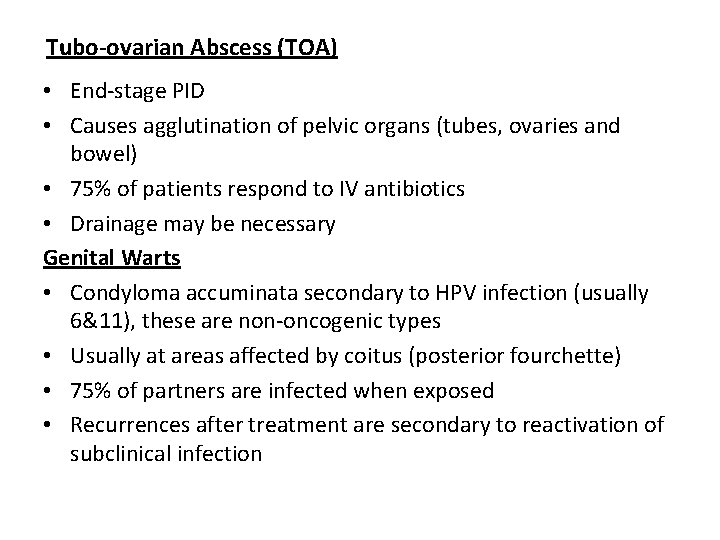
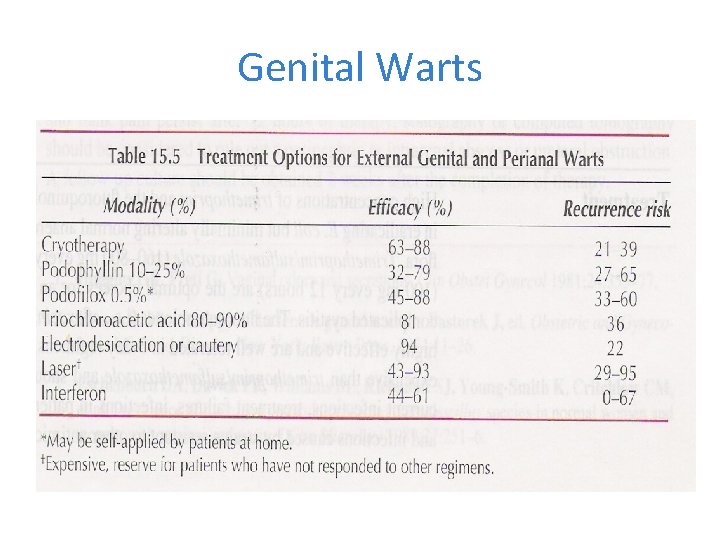
Tubo-ovarian Abscess (TOA) • End-stage PID • Causes agglutination of pelvic organs (tubes, ovaries and bowel) • 75% of patients respond to IV antibiotics • Drainage may be necessary Genital Warts • Condyloma accuminata secondary to HPV infection (usually 6&11), these are non-oncogenic types • Usually at areas affected by coitus (posterior fourchette) • 75% of partners are infected when exposed • Recurrences after treatment are secondary to reactivation of subclinical infection
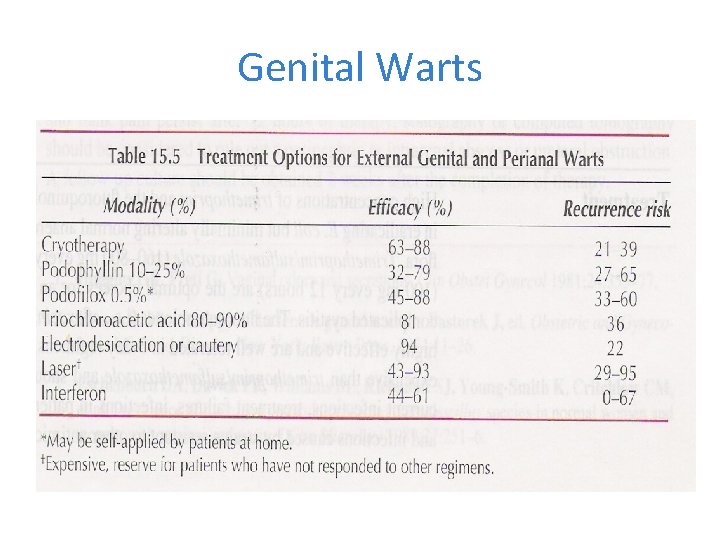
Genital Warts
 Multi loop pid controller regolatore pid multi loop
Multi loop pid controller regolatore pid multi loop Cervical ectropion
Cervical ectropion Female external genitalia
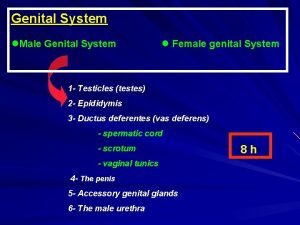
Female external genitalia Male genital tract
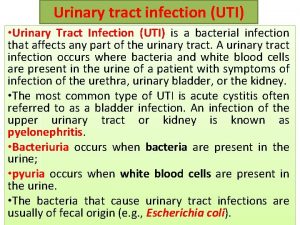
Male genital tract Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Sexually transmitted diseases
Sexually transmitted diseases Complicated uti symptoms
Complicated uti symptoms Nursing management for urinary tract infection
Nursing management for urinary tract infection Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Conclusion of respiratory tract infection
Conclusion of respiratory tract infection Complicated urinary tract infection
Complicated urinary tract infection Uti causes
Uti causes Extrapyramidal tract names
Extrapyramidal tract names Olivospinal tract vs tectospinal tract
Olivospinal tract vs tectospinal tract Anatomical structures of the upper respiratory tract
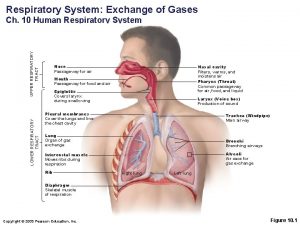
Anatomical structures of the upper respiratory tract Classification of pneumonia
Classification of pneumonia Upper and lower respiratory tract
Upper and lower respiratory tract