Lower genital tract Infection Mervat Elsersy Assistant professor
![n n Diagnosis : 1] Inspection: - Vulval soreness - Vaginal discharge on separation n n Diagnosis : 1] Inspection: - Vulval soreness - Vaginal discharge on separation](https://slidetodoc.com/presentation_image_h2/48c45978360ae0fba53ef40d2a1e8fe1/image-14.jpg)


![Regimens: 1] Cefoxitin 2 gm I. V. / 6 hr + Doxycycline l 00 Regimens: 1] Cefoxitin 2 gm I. V. / 6 hr + Doxycycline l 00](https://slidetodoc.com/presentation_image_h2/48c45978360ae0fba53ef40d2a1e8fe1/image-53.jpg)
- Slides: 60
Lower genital tract Infection Mervat Elsersy Assistant professor of Obs & Gyn. Faculty of medicine Alexandria university Egypt
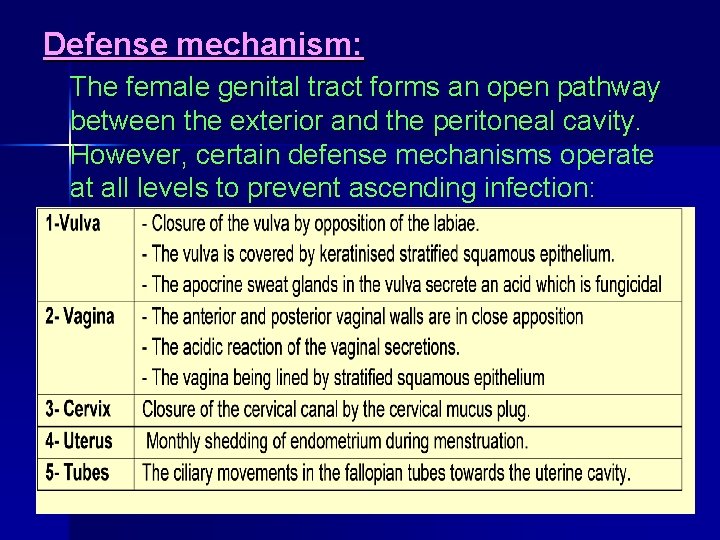
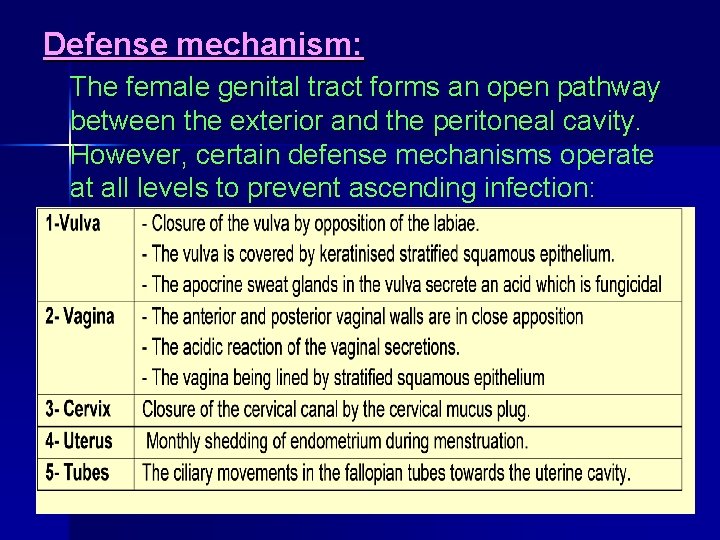
Defense mechanism: The female genital tract forms an open pathway between the exterior and the peritoneal cavity. However, certain defense mechanisms operate at all levels to prevent ascending infection:
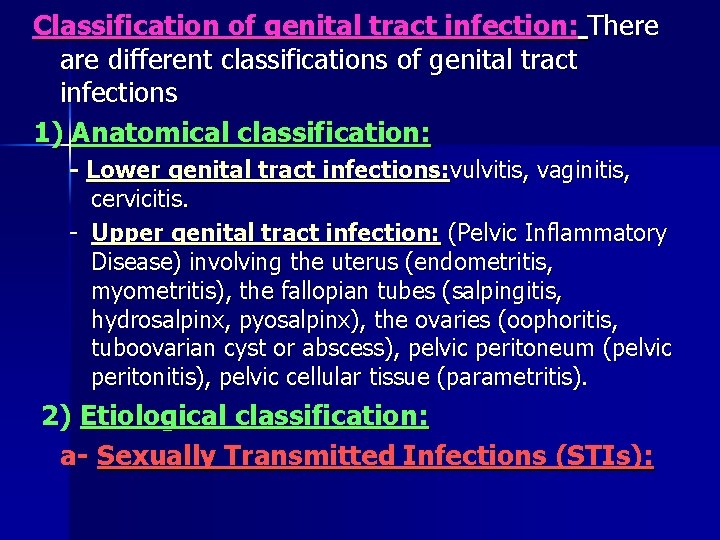
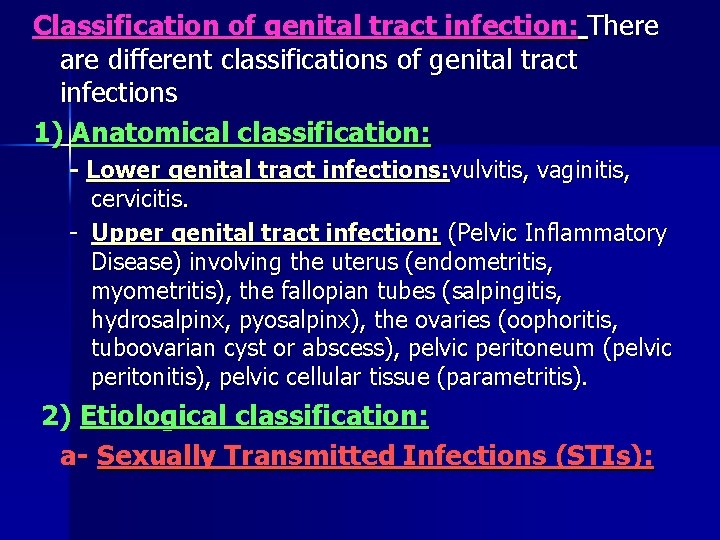
Classification of genital tract infection: There are different classifications of genital tract infections 1) Anatomical classification: - Lower genital tract infections: vulvitis, vaginitis, cervicitis. - Upper genital tract infection: (Pelvic Inflammatory Disease) involving the uterus (endometritis, myometritis), the fallopian tubes (salpingitis, hydrosalpinx, pyosalpinx), the ovaries (oophoritis, tuboovarian cyst or abscess), pelvic peritoneum (pelvic peritonitis), pelvic cellular tissue (parametritis). 2) Etiological classification: a- Sexually Transmitted Infections (STIs):
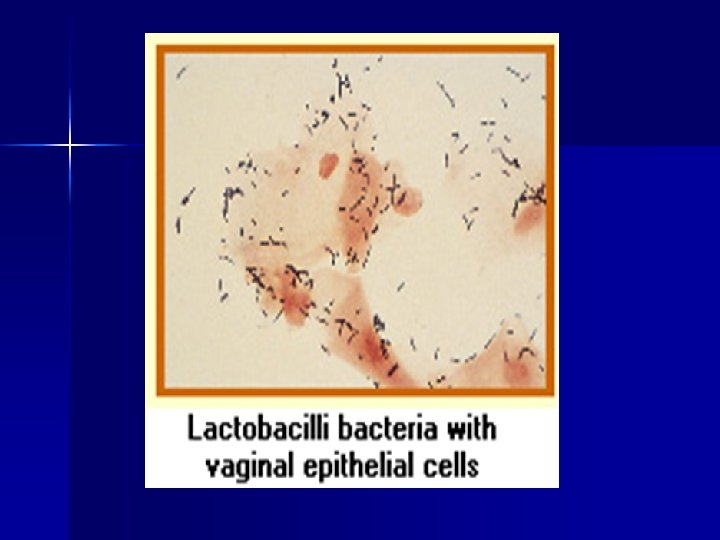
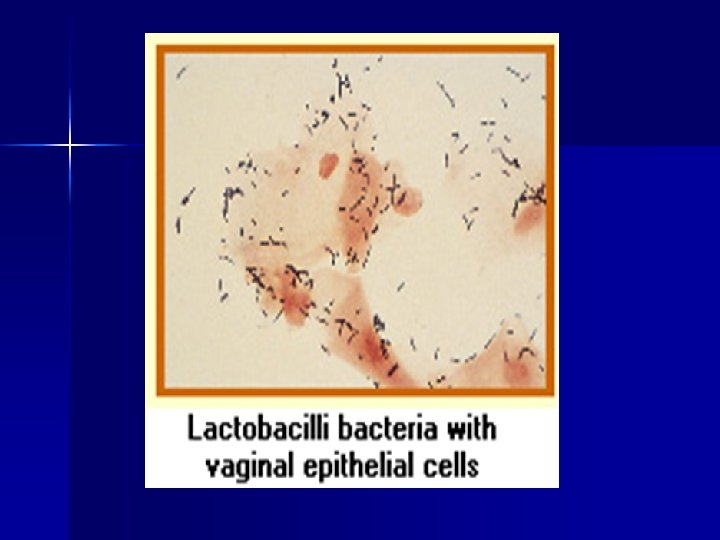
2) Etiological classification(cotn. ): b- Non-specific infections: (mostly caused by lack of appropriate infection prevention measures): -Puerperal (after labour or abortion). - Pelvic examination. - Traditional practices as female genital cutting/ vaginal tampons, etc. c- Blood born infection: mostly T. B d- Endogenous infections: caused by overgrowth of microbal agents that are normal inhabitants: Candida albicans, Normal vaginal organisms: Facultative: • - Lactobacilli Group B. streptococci • Gardenerella vaginalis -listeria monocytogens • - Staph epidermidis - E coli
Anaerobes: - Anaerobic lactobacillus - Bacteroides species - Peptostreptococcus n Yeast: candida albicans · Mycoplasma: - Mycoplasma hominis - Ureaplasma urealyticu
Vulvitis vulvitis is inflammation of the external female genitalia (vulva). Classification: According to clinical presentation: 1 - Acute vulvitis: most cases are secondary to septic discharges from above 2 - Chronic vulvitis: It is seen as a result of long standing infected vaginal discharges and primary infections by tuberculosis, bilharziasis, viruses, and actinomycosis According to the cause: 1 - Non-infectious 30%: due to irritation or hypersensitivity. It is more common in premenarchal and post-menopausal women. 2 - Infectious: common in reproductive years, vulvovaginitis most often due to infection - Bacterial vaginosis - Candidal vaginitis - Trichomonas - Mixed infections - Chlamydia/gonorrhea
According to the mode of infection: 1. Sexually transmitted diseases: 2. Non-sexually transmitted: TB. , Bilharziasis. , Symptoms: - Erythema, edema of vulva and perineum - Itching - Burning, stinging - Pain, dypareunia (painful intercourse) - Discharge - Malodor Signs: n Redness and swelling of the vulvar skin n Thickening of the vulvar skin n Possible vaginal discharge n Possible small cracks or skin lesions on the vulvar skin
Vulvitis Investigation: see pruritus vulva Treatment: n Discontinue the use of any potential irritants n If discharge from a vaginal infection is the cause of vulvitis, the source of the vaginal infection should be treated and concurrent topical cortisone cream may be used to decrease vulvar itching. n If treatment of vulvitis is not very effective, further evaluation may include biopsy of the skin to rule out the potential of vulvar dystrophy (a chronic vulvar skin condition) or vulvar dysplasia, (a precancerous condition). A biopsy may also be necessary if any skin lesions are present.
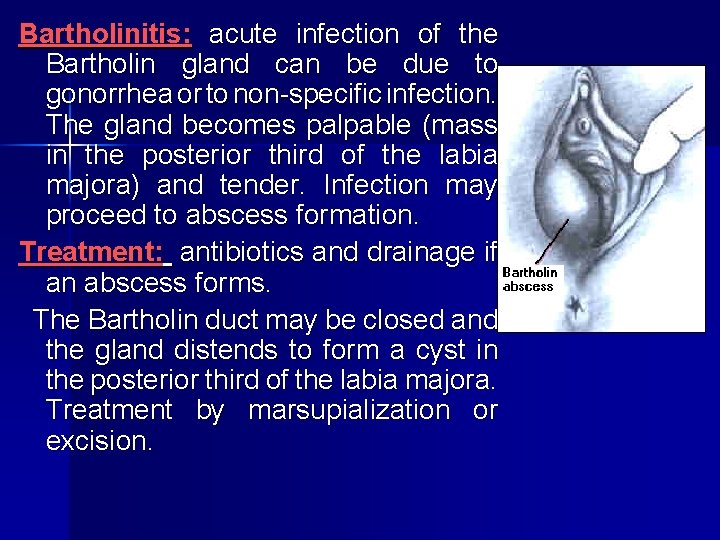
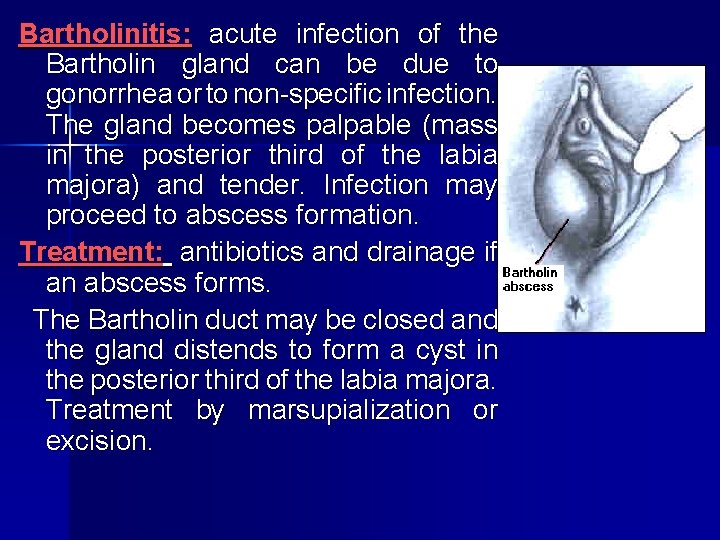
Bartholinitis: acute infection of the Bartholin gland can be due to gonorrhea or to non specific infection. The gland becomes palpable (mass in the posterior third of the labia majora) and tender. Infection may proceed to abscess formation. Treatment: antibiotics and drainage if an abscess forms. The Bartholin duct may be closed and the gland distends to form a cyst in the posterior third of the labia majora. Treatment by marsupialization or excision.
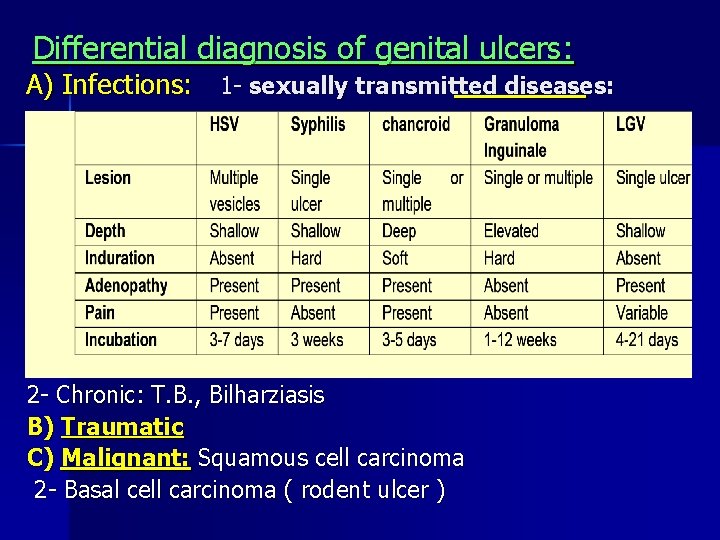
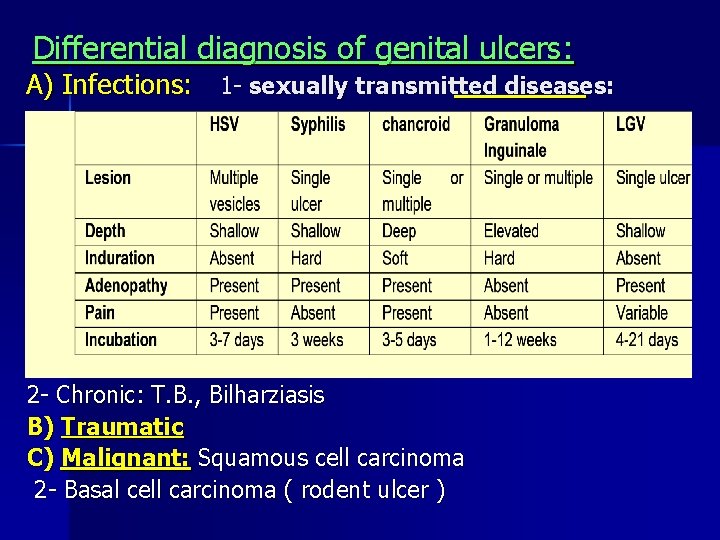
Differential diagnosis of genital ulcers: A) Infections: 1 - sexually transmitted diseases: 2 - Chronic: T. B. , Bilharziasis B) Traumatic C) Malignant: Squamous cell carcinoma 2 - Basal cell carcinoma ( rodent ulcer )
Vaginitis Classification: A) Primary vaginitis: *During infancy and childhood : Vulvovaginitis of children *During reproductive years : 1] Bacterial : - Gonococcal( see STD) - Bacterial vaginosis 2] Viral : - Genital herpes ( see STD) - Genital warts ( see STD) 3] Chlamydia : ( see STD) 4] Fungal : Candidal infection 5] Parasitic : Trichomonas vaginitis *During postmenopause : Atrophic or senile vaginitis B) Secondary vaginitis: to 1 - Urinary conditions: e. g. vesicovaginal fistula 2 - Rectal conditions: e. g. rectovaginal fistula 3 - Infected cervical discharge 4 - Mechanical irritatione. g. by neglected pessary 5 - Chemical irritation e. g. by drugs and douches
Vulvovaginitis of children: common in the 1 st 5 years n Predisposing factors: Thin vaginal mucosa, low glycogen content and higher PH n Etiology: - Non specific infection (staphylococci, streptococci. , E coli) - Rarely specific organisms (candida , gonorrhea) - Forigen body (F. B. ) - Oxyuris n Clinical picture: - Profuse purulent discharge - Soreness and irritation → continuous scratching - Vulva edematous and reddened.
![n n Diagnosis 1 Inspection Vulval soreness Vaginal discharge on separation n n Diagnosis : 1] Inspection: - Vulval soreness - Vaginal discharge on separation](https://slidetodoc.com/presentation_image_h2/48c45978360ae0fba53ef40d2a1e8fe1/image-14.jpg)
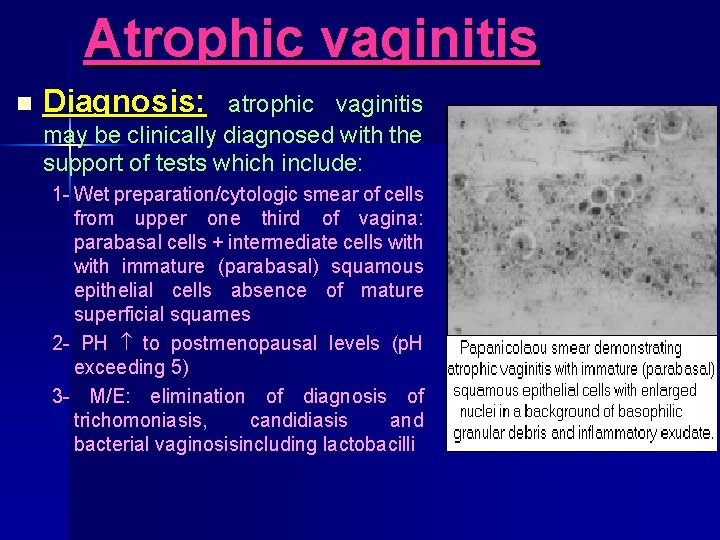
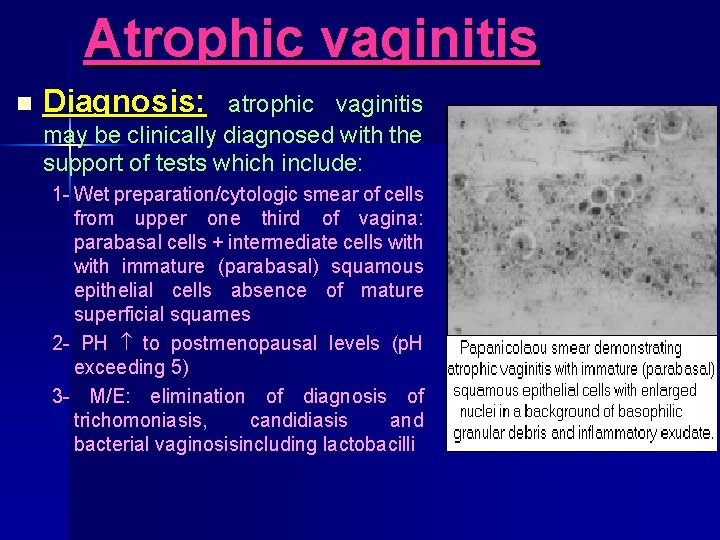
n n Diagnosis : 1] Inspection: - Vulval soreness - Vaginal discharge on separation of the labia (may foul smell) 2] P. R. with the little finger: - To detect any F. B. - To milk any discharge down 3] Platinum loop: used to take a drop of discharge for direct staining and direct examination 4] Pipette: used to take small amount of discharge & culture on Staurt medium for culture. 5] X-ray or ultrasound: to detect F. B. Treatment: - Perineal hygiene ( by the mother ) - Local estrogen to the vulva each night for 2 weeks to relief soreness and increase natural vaginal resistance. - If an organism is identified by CST , give short course of antibiotic - If candida , give 100 mg ketoconazole twice daily for 7 days - If oxyuris , give piperazine citrate for all family members - If gonorrhea , IM or oral penicillin for 4 days and the child is isolated from other children to prevent cross infection.
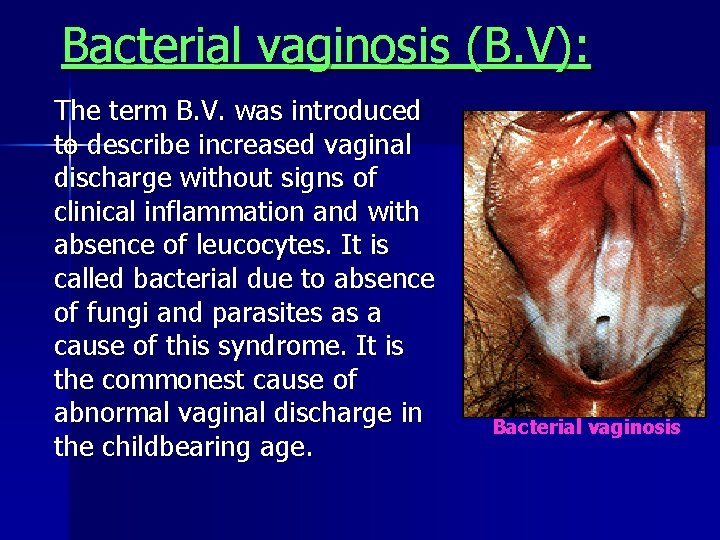
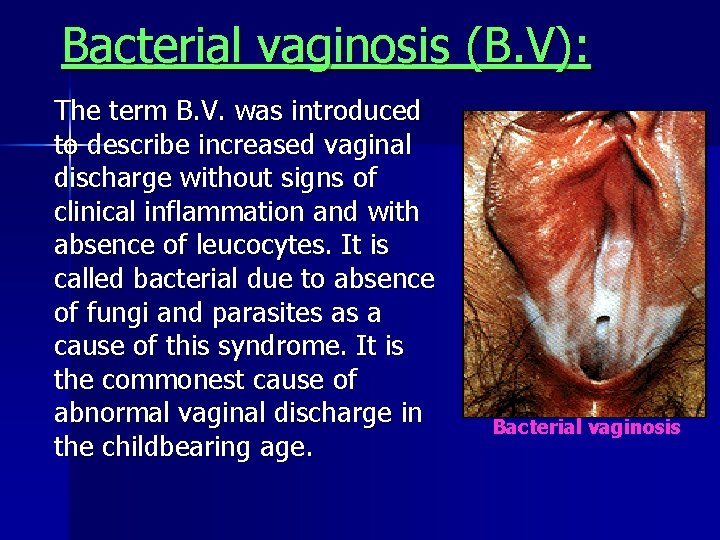
Bacterial vaginosis (B. V): The term B. V. was introduced to describe increased vaginal discharge without signs of clinical inflammation and with absence of leucocytes. It is called bacterial due to absence of fungi and parasites as a cause of this syndrome. It is the commonest cause of abnormal vaginal discharge in the childbearing age. Bacterial vaginosis
n n Etiology: (B. V) The exact etiology is unknown. However, it is suggested to occur due to a change of the vaginal flora from being predominantly lactobacilli to a polymicrobal flora dominated by Gardnerella vaginalis and other anaerobic organisms, all of which can be found in low numbers in healthy vagina. Decreased vaginal acidity is accompanied by increased concentration of these organisms 100 fold or more at the expense of the protective lactobacilli. Symptoms: about 50% of women with BV do not have symptoms 1 Vaginal discharge rather than pruritus. The discharge is characterized by a thin , watery , homogenous , gray and adherent but easily whipped. 2 May be mild valvular itching or burning. 3 Bad smell (fishy odour) especially after coitus and during menstruation due to increased PH which liberates certain amines.
n Signs: (B. V) 1 Discharge: copious, thin, greyish white, homogenous, but not sticky 2 No inflammation reaction (No epithelial edema or erythema) n Diagnosis: 1 Characters of vaginal discharge. 2 Vaginal PH: Vaginal fluid can be tested by dipping PH paper. PH is usually > 4. 7. 3 Amine test or Whiff test : addition of KOH to a sample of vaginal secretion → characteristic fishy odour. 4 Clue cells: Detected when the vaginal fluid is mixed with normal saline and examined under the microscope. Clue cells are nothing but vaginal epithelial cells obscured by B. V. organisms in absence of lactobacilli ( is diagnostic).
(B. V) n Complications: 1 PID 2 Post hysterectomy infection 3 Obstetric complications: PROM, chorioamnionitis, preterm labour, postpartum endometritis, post C S endometritis and post CS wound infection n Treatment : 1. Systemic therapy (oral) (80% cure) 1) Metronidazole: 500 mg, 2 3 times a day for 7 days 2) Clindamycin: 300 mg, twice a day for 7 days 2. Topical therapy (80% cure) 1) Metronidazole 0. 5 gm per night for 5 nights
Fungal vaginitis (candidal vaginitis): n n Organism: the etiologic agent is candida. Candida albicans is responsible for 80 90% of vulvovaginal candidiasis. It is gm +ve with hyphae and spores Incidence: A) About 1/3 of vaginitis cases are caused by fungal infection. b) About 75% of women develop candidiasis at least once in life most commonly following antibiotic or pregnancy. n Predisposing factors: 1] Pregnancy: attributed to higher glycogen content with increased vaginal acidity 2] Oral contraceptives: higher glycogen content with increased vaginal acidity 3] Diabetes mellitus: higher glycogen content and decreased immunity 4] Antibiotics : thought to eliminate the normal protective vaginal bacterial flora. 5] Prolonged therapy with corticosteroids or other immunosuppressive: decrease immunity 6] Other factors: which create a suitable environment for this opportunistic pathogen. Use of tight restricting poorly ventilated underwear leads to increase of the perineal moisture and increase temperature Lack of proper female hygiene
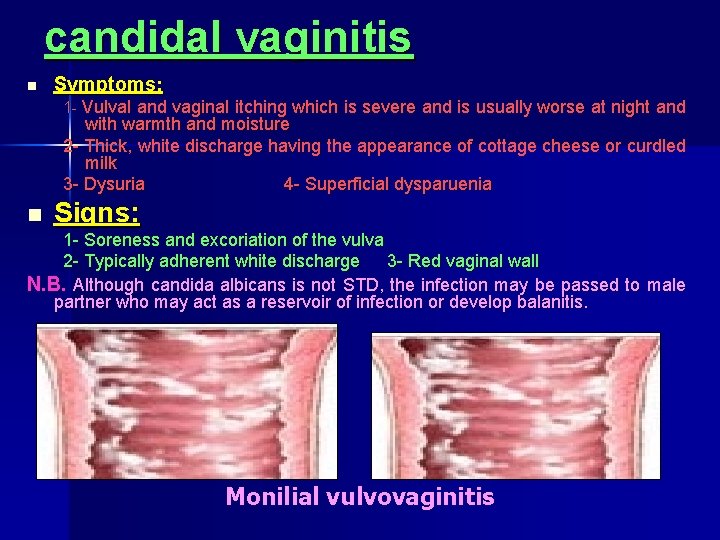
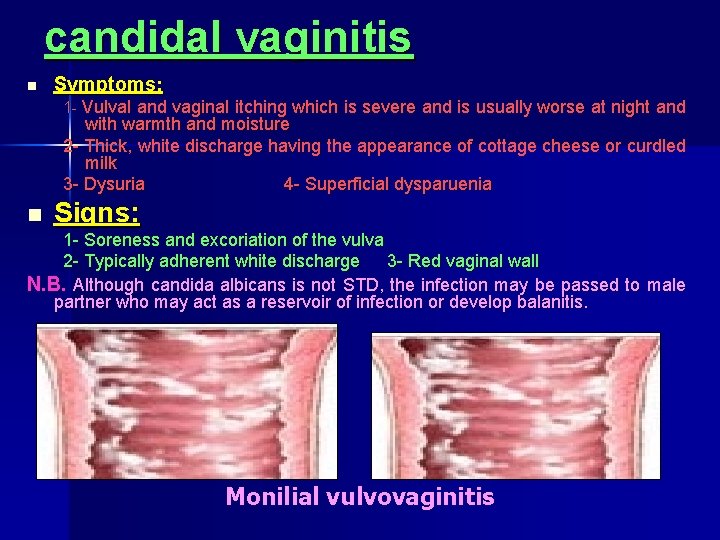
candidal vaginitis n Symptoms: 1 Vulval and vaginal itching which is severe and is usually worse at night and with warmth and moisture 2 Thick, white discharge having the appearance of cottage cheese or curdled milk 3 Dysuria 4 Superficial dysparuenia n Signs: 1 Soreness and excoriation of the vulva 2 Typically adherent white discharge 3 Red vaginal wall N. B. Although candida albicans is not STD, the infection may be passed to male partner who may act as a reservoir of infection or develop balanitis. Monilial vulvovaginitis
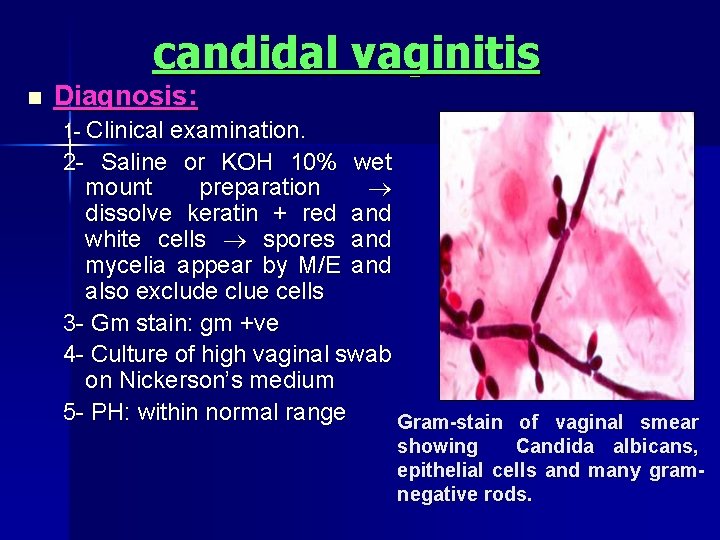
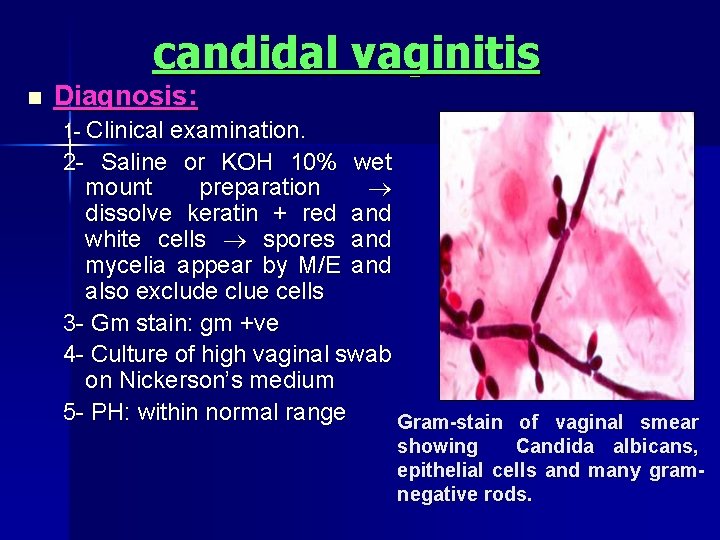
candidal vaginitis n Diagnosis: 1 Clinical examination. 2 Saline or KOH 10% wet mount preparation dissolve keratin + red and white cells spores and mycelia appear by M/E and also exclude clue cells 3 Gm stain: gm +ve 4 Culture of high vaginal swab on Nickerson’s medium 5 PH: within normal range Gram-stain of vaginal smear showing Candida albicans, epithelial cells and many gramnegative rods.
candidal vaginitis n – – Treatment: Elimination of predisposing factors: as control of diabetes Topical application of antifungal agents: 1) Miconazole: 2) Clotrimazole: a) b) c) a) 200 mg/day for 7 days b) 400 mg/day for 3 days 100/day for 7 days 100 MG, twice a day for 3 days 500 mg single dose 3) Nystatin n 1. 2. 3. Systemic medication: oral agents are used only for cases that can not be treated with topical application of antifungal drugs. Fluconazole: 150 mg, single use. Itraconazole: a) 200 mg/day for 3 -5 days b) 400 mg for 1 day divided in two doses Ketoconazole: 200 mg, once or twice/day until culture result is negative.
candidal vaginitis n Causes of failure: may be due to: 1 Failure to properly take the medication (poor compliance) 2 Drug resistance 3 Unusual fungal infection (other than C. albicans) 4 Sexual transmission from male partner 5 Recurrent infection from GIT 6 Immunocompromised patient
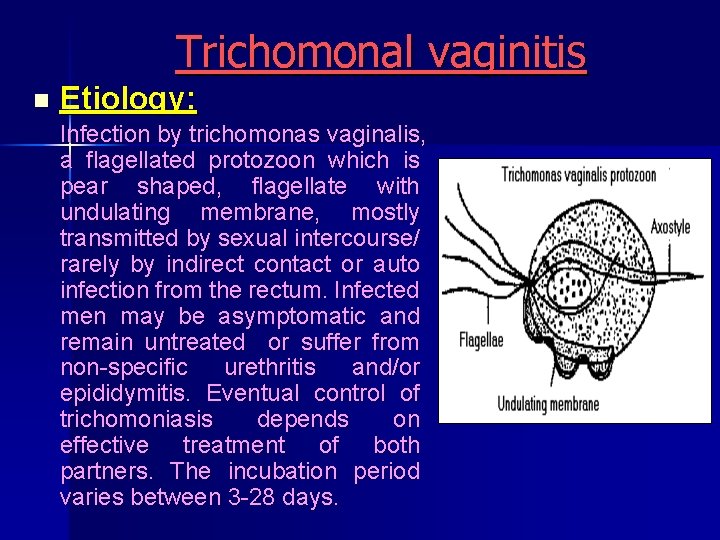
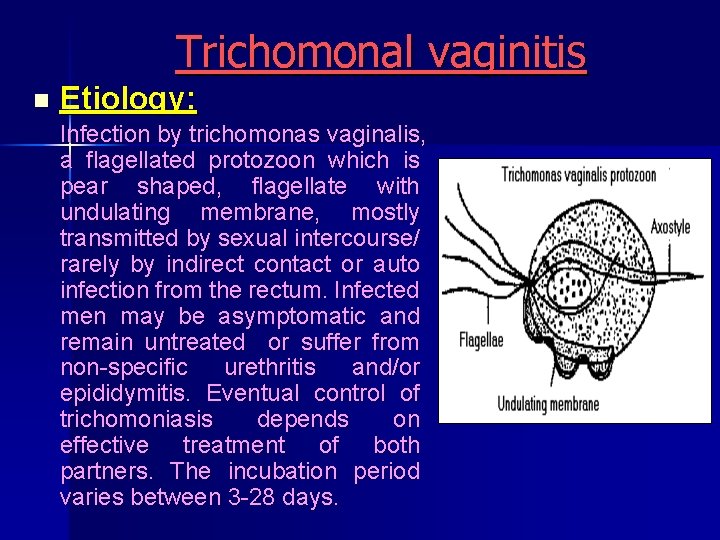
Trichomonal vaginitis n Etiology: Infection by trichomonas vaginalis, a flagellated protozoon which is pear shaped, flagellate with undulating membrane, mostly transmitted by sexual intercourse/ rarely by indirect contact or auto infection from the rectum. Infected men may be asymptomatic and remain untreated or suffer from non specific urethritis and/or epididymitis. Eventual control of trichomoniasis depends on effective treatment of both partners. The incubation period varies between 3 28 days.
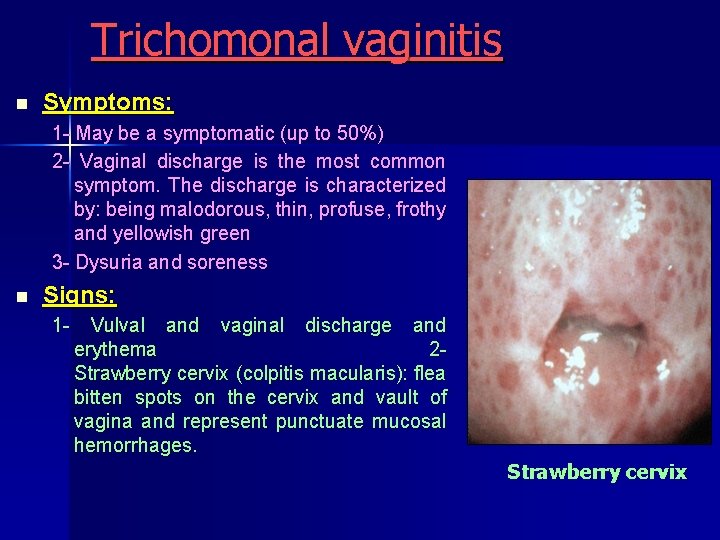
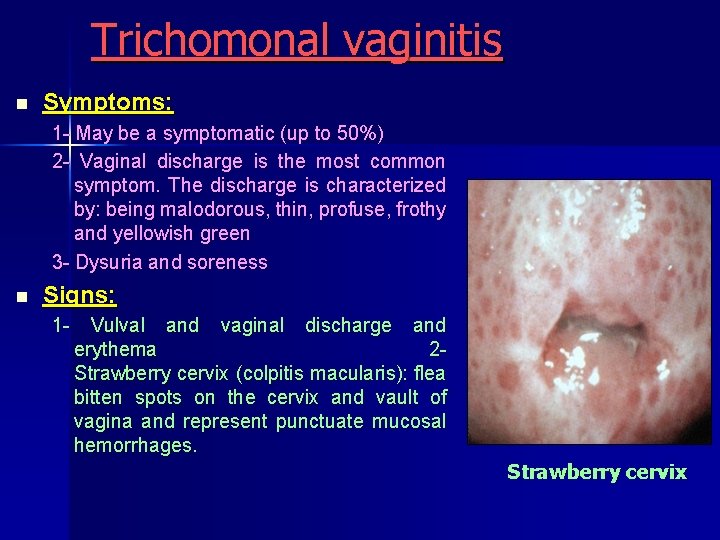
Trichomonal vaginitis n Symptoms: 1 May be a symptomatic (up to 50%) 2 Vaginal discharge is the most common symptom. The discharge is characterized by: being malodorous, thin, profuse, frothy and yellowish green 3 Dysuria and soreness n Signs: 1 Vulval and vaginal discharge and erythema 2 Strawberry cervix (colpitis macularis): flea bitten spots on the cervix and vault of vagina and represent punctuate mucosal hemorrhages. Strawberry cervix
Trichomonal vaginitis n Diagnosis: 1 Clinical features: but unreliable guide and even those features classically associated with trichomoniasis do not occur in all cases 2 PH: of vaginal discharge is elevated above normal 3 Addition of KOH 10% to the discharge elicits an amine like odour in about 75% These findings however are more strongly associated with B. V. than with trichomoniasis 4 Wet mount preparation: for identification of the organism. 5 Culture: on kupferberg medium or Frienberg medium. these media contain antibiotics (streptomycin, penicillin) so, all organisms except trichomonas and monilia will die. n Treatment: by metronidazole by mouth or intravaginally 1. Systemic therapy: (First choice), oral metronidazole a) 2 g single dose b) 500 mg, twice or 3 times a day, for 7 days. 2. Topical application: a) Metronidazole gel b) Acidification of vagina with 1% lactic acid or 0. 5% acetic acid
Trichomonal vaginitis N. B. Male partner should receive treatment at the same time. n Causes of treatment failure: Compliance Reexposure to infected partner Drug resistance In this case, large dose is indicated 1 gm twice daily 17 – 14 days in combination with 500 mg twice daily 17 – 14 days vaginally Treatment during pregnancy: Metronidazole is best avoided during pregnancy in the 1 st trimester but can be given in severe cases in 2 nd and 3 rd trimesters. Clotrimazole is reserved for 1 st trimester but is far less effective.
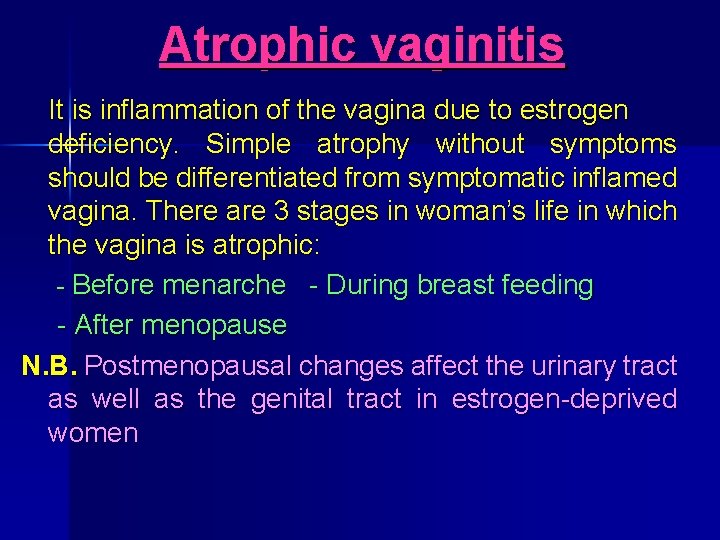
Atrophic vaginitis It is inflammation of the vagina due to estrogen deficiency. Simple atrophy without symptoms should be differentiated from symptomatic inflamed vagina. There are 3 stages in woman’s life in which the vagina is atrophic: Before menarche During breast feeding After menopause N. B. Postmenopausal changes affect the urinary tract as well as the genital tract in estrogen deprived women
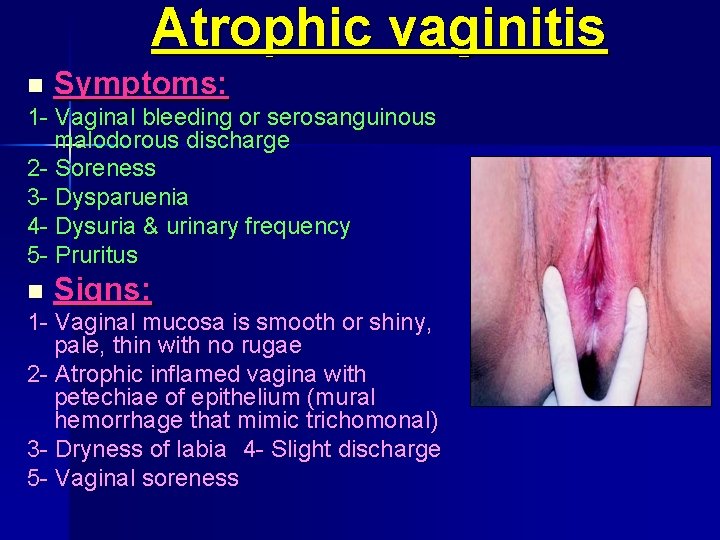
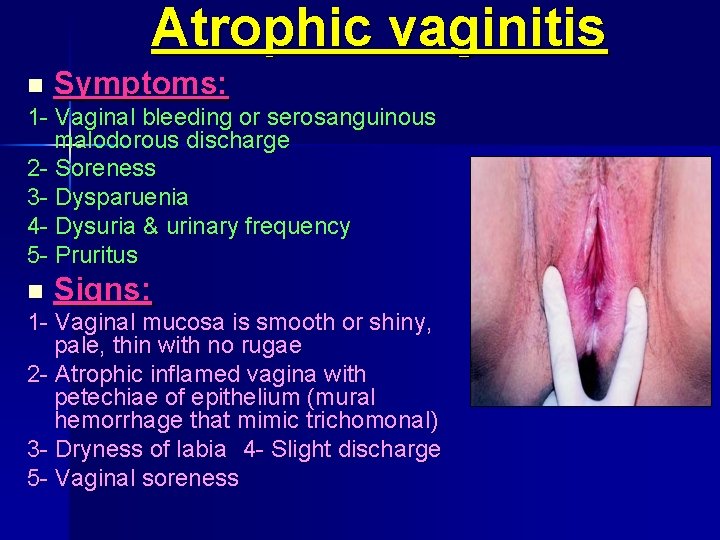
Atrophic vaginitis n Symptoms: 1 Vaginal bleeding or serosanguinous malodorous discharge 2 Soreness 3 Dysparuenia 4 Dysuria & urinary frequency 5 Pruritus n Signs: 1 Vaginal mucosa is smooth or shiny, pale, thin with no rugae 2 Atrophic inflamed vagina with petechiae of epithelium (mural hemorrhage that mimic trichomonal) 3 Dryness of labia 4 Slight discharge 5 Vaginal soreness
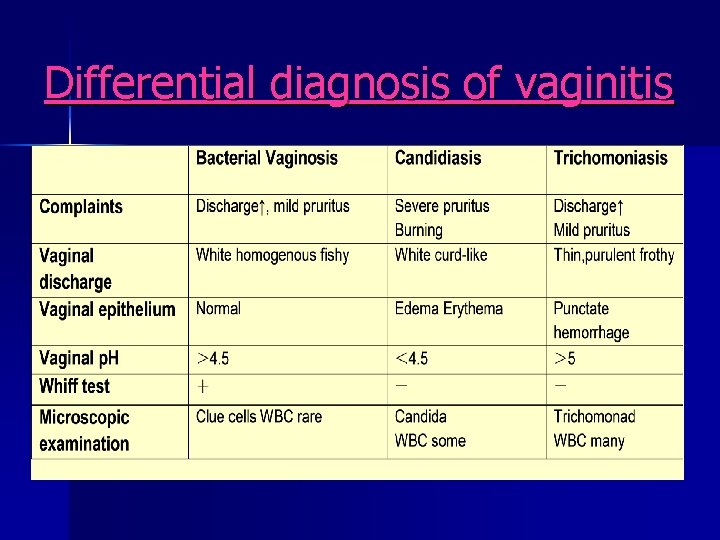
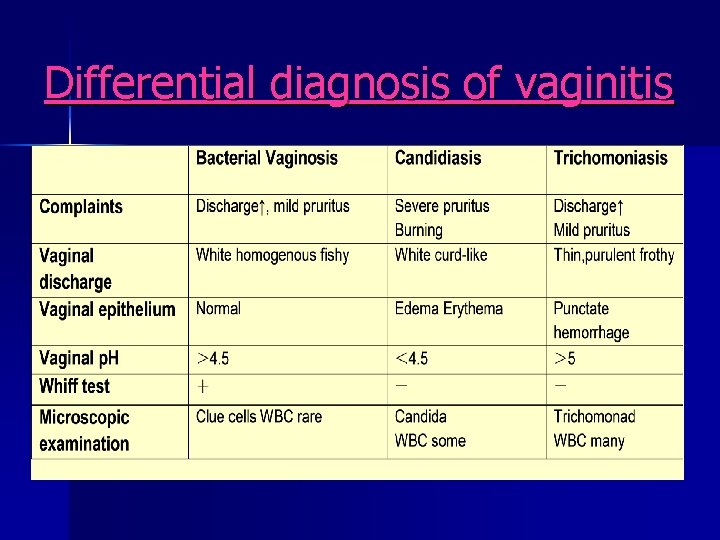
Atrophic vaginitis n Diagnosis: atrophic vaginitis may be clinically diagnosed with the support of tests which include: 1 Wet preparation/cytologic smear of cells from upper one third of vagina: parabasal cells + intermediate cells with immature (parabasal) squamous epithelial cells absence of mature superficial squames 2 PH to postmenopausal levels (p. H exceeding 5) 3 M/E: elimination of diagnosis of trichomoniasis, candidiasis and bacterial vaginosisincluding lactobacilli
Atrophic vaginitis N. B. you should exclude neoplasm, F. B. and other infection n Treatment: § Topical estrogen: once daily for 2 weeks and not > 4 weeks. § Systemic estrogen: appropriate only if the patient has menopausal symptoms in addition to vaginal symptoms.
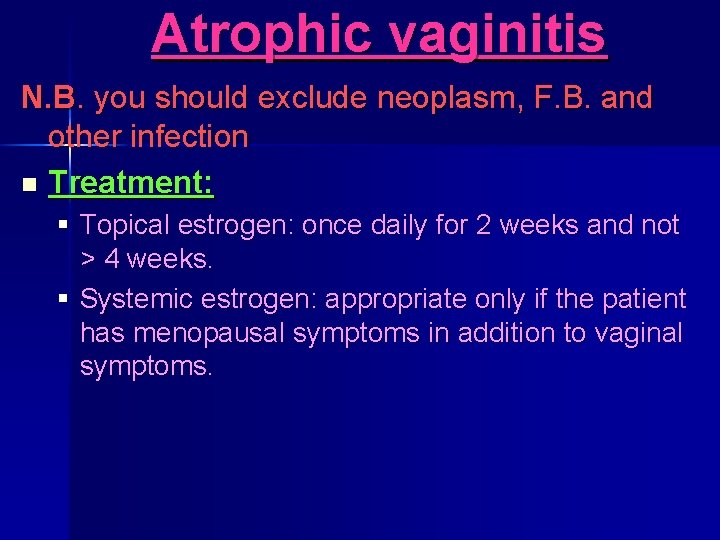
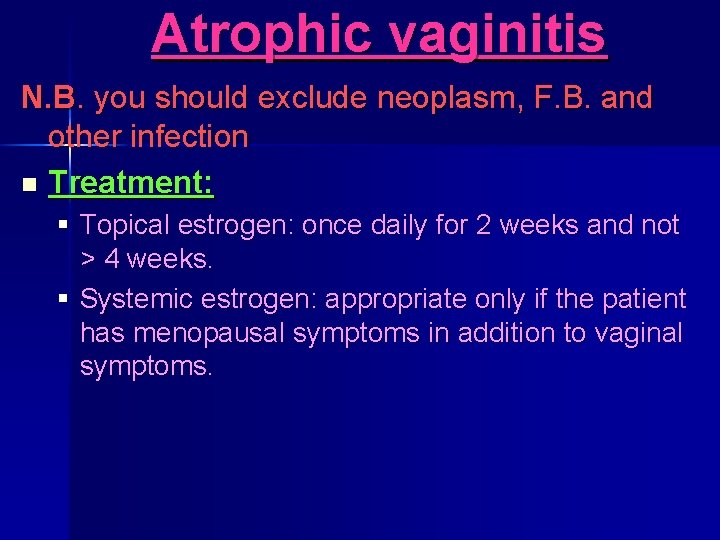
Differential diagnosis of vaginitis
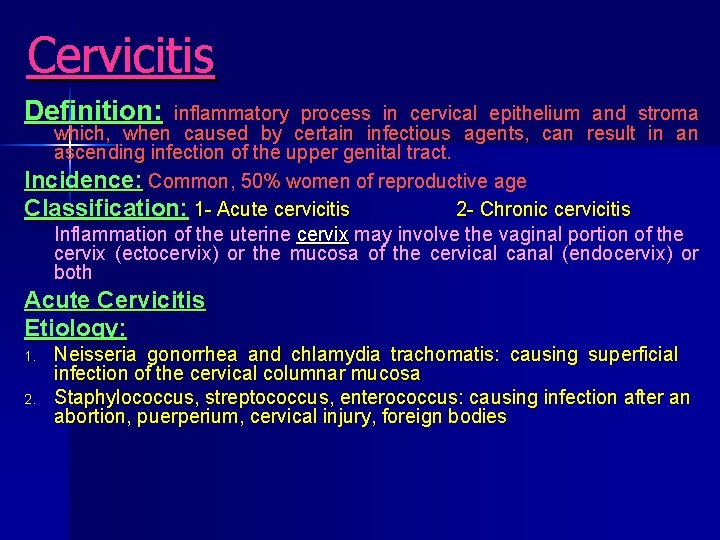
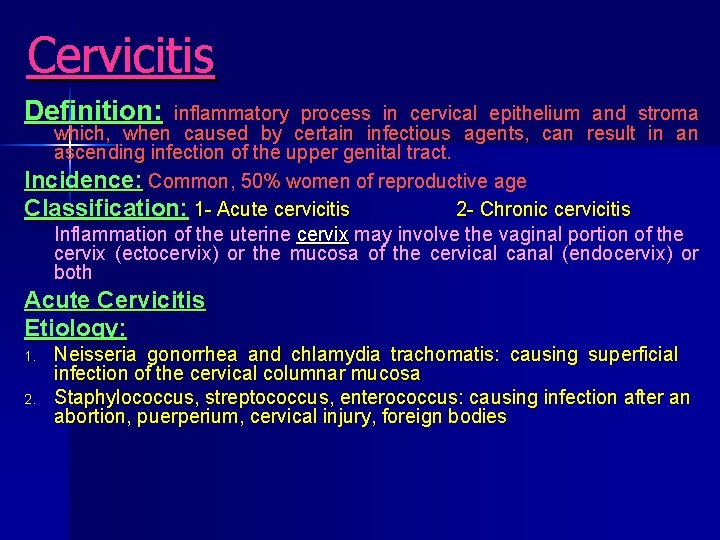
Cervicitis Definition: inflammatory process in cervical epithelium and stroma which, when caused by certain infectious agents, can result in an ascending infection of the upper genital tract. Incidence: Common, 50% women of reproductive age Classification: 1 Acute cervicitis 2 Chronic cervicitis Inflammation of the uterine cervix may involve the vaginal portion of the cervix (ectocervix) or the mucosa of the cervical canal (endocervix) or both Acute Cervicitis Etiology: 1. 2. Neisseria gonorrhea and chlamydia trachomatis: causing superficial infection of the cervical columnar mucosa Staphylococcus, streptococcus, enterococcus: causing infection after an abortion, puerperium, cervical injury, foreign bodies
Cervicitis Symptoms: there may be no symptoms. § § § Mucopurulent vaginal discharge: persistent, gray, white or yellow color and may be profuse Vaginal irritation symptoms: pruritus, burning sensation Back ache Intermenstrual bleeding or postcoital bleeding Dysparuenia Symptoms of the lower urinary tract infection may be present Signs: § Swelling and redness of the cervix § Purulent endocervical discharge, gen erally yellow or green in color and referred to as “mucopus”. § It may also reveal inflammation of the vaginal walls caused by the infected discharge. Investigations: 1. Gram’s stain of the cervical discharge for leukocyte ≥ 30/HP 2. Tests for gonococcus and chlamydia
Complications: Cervicitis Chronicity: due to racemose branching cervical glands Spread of infection to the upper genital tract (PID) Secondary vaginitis Treatment : systemic broad spectrum antibiotic, choice of drug depends on the pathogens. Chronic cervicitis: It is a common sequel of acute cervicitis Incidence: commonest gynecological lesion Predisposing factors: Racemose glands (branched) Repeated trauma No menstrual shedding Clinical Features: Symptoms: 1. Persistent leukohrrea usually mucopurulent 2. Slight postcoital bleeding or staining 3. Pains: lower abdominal discomfort, lumbosacral backache, dysmenorrhea, dyspareunia 4. Infertility 5. Urinary symptoms: frequency, urgency, dysuria due to subvesical lymphangitis not to cystitis
Cervicitis Signs (pathological types): 1 - Chronic endocervicitis: limited inflammation of the cervical canal but external os appears normal; pus is seen coming from external os 2 - Cervical mucus polyp: due to hyperplastic endocervical epithelium, projecting polyp (single, small, soft, smooth and pedunculated) 3 - Chronic hypertrophic cervicitis: swollen hypertrophic muscle layer of the cervix. It appears barrel shaped 4 - Nabothian follicle: small bluish or yellowish cysts projecting on the portiovaginalis, It is due to duct obstruction of the cervical glands 5 - Ectropion: everted anterior & posterior lip of the cervix, exposing the lower part of endocervix, it is due to bilateral cervical tears
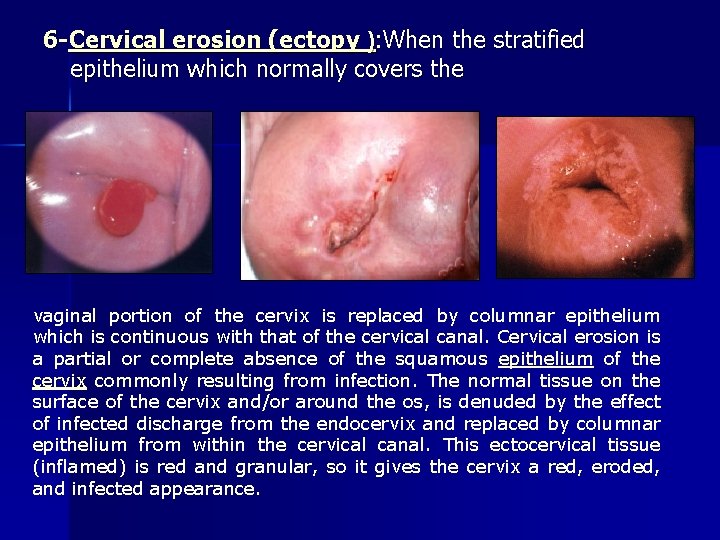
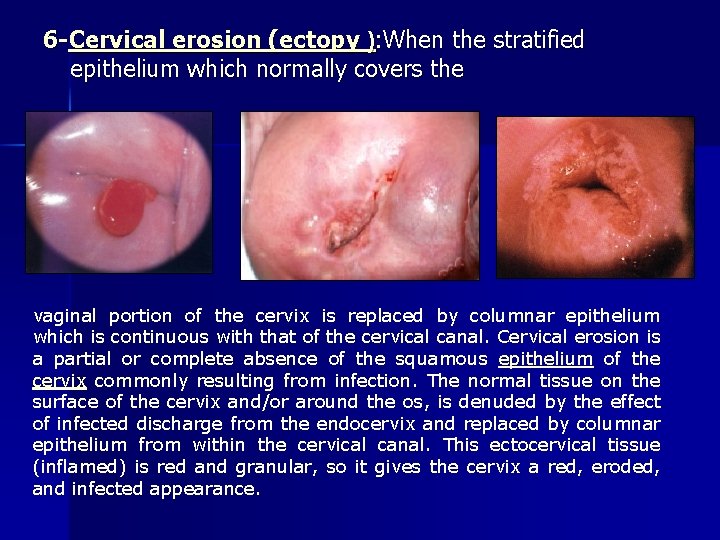
6 -Cervical erosion (ectopy ): When the stratified epithelium which normally covers the vaginal portion of the cervix is replaced by columnar epithelium which is continuous with that of the cervical canal. Cervical erosion is a partial or complete absence of the squamous epithelium of the cervix commonly resulting from infection. The normal tissue on the surface of the cervix and/or around the os, is denuded by the effect of infected discharge from the endocervix and replaced by columnar epithelium from within the cervical canal. This ectocervical tissue (inflamed) is red and granular, so it gives the cervix a red, eroded, and infected appearance.
Cervical erosion Causes: Cervical erosion may be caused by: 1) Congenital: due to arrest of squamous metaplasia 2) Hormonal: during pregnancy or due to COCs 3) Infection: Types: Simple flat Papillary Follicular Symptoms: there may be no symptoms. 1 Abnormal vaginal bleeding (not associated with a menstrual period): § After sexual intercourse (postcoital) § Between menstrual periods 2 Discharge (clear or yellowish mucus) may have an odor if associated with a vaginal infection 3 Back ache Signs: Pelvic examination reveals velvety sensation and speculum show an area on the cervix that looks raw, red, and inflamed. Investigations: n A Pap smear may show atypical cells n Culture of discharge may reveal organisms, such as E. coli n Colposcopic examination reveals an area of raw, stripped, squamous epithelium n Cervical biopsy may be necessary
Treatment of chronic cervicitis: n n A. B. 1. 2. 3. Prophylaxis: STIs & avoid trauma to the cervix Active: Medical: (systemic antibiotic) Cauterization: Chemical: by silver nitrate or zinc chloride (not used now) Cryocautery: nitrous oxide or carbon dioxide (prolonged discharge is a disadvantage) Electrocautery: (diathermy) * Time: post menstrual * It coagulates unhealthy tissue by strokes of 3 mm depth. No cauterization at (3 & 9) 0 ‘clock to avoid cervical branches of uterine artery. *After cauterization: give systemic antibiotic * Side effects: Stenosis, 2 ry hemorrhage, spread of infection Laser cautery (best) C- Surgical: 1 - Conization 2 - Trachelorraphy for ectropion

Pelvic Inflammatory Disease (PID) Dr. Hossam El Sokkary Lecturer of Ob. & Gyn. Faculty of medicine Alexandria university Egypt
PID Definition: PID is defined as acute upper genital tract infection that involve the endometrium (endometritis), parametrium parametritis), fallopian tubes (salpingitis), ovaries (oophritis) and pelvic peritoneum (peritonitis) associated with ascending spread of microorganism from the vagina or endocervix. Incidence : The highest incidence is among sexually active women in their
PID Risk factors: A -Sexually transmitted infections: 1) Age : 2) 3) 4) 5) 6) 7) 8) with young age (15 ‑ 20 y. ) due to increase sexual activity in young age Race : in black due to low socioeconomic status Douching : pressure in the vagina forcing material up through the cervix. Cigarette smoking : risk due to damage of immune system Previous episodes of acute salpingitis : damaged tube is susceptible to altered defense mechanism Sexual intercourse: pressure gradient between lower and upper genital tract leading cervical barrier compromisation Multiple sexual partners : risk of meeting male with STD. Use of IUD : among women with increased risk of STI B -Postpartum C -Postoperative
PID Microbiology : many cases are polymicrobial in etiology. Pure gonococcal or chlamydial PID is possible. Infective organisms are: • Sexually transmitted: - Chlamydia trachomatis Neisseria gonorrhea • Endogenous aerobic: - - Streptococci staphylococci E. coli - Bacterial vaginosis • Anaerobes: Bacteroides, peptostreptococcus • Mycobacterium tuberculosis & bovis
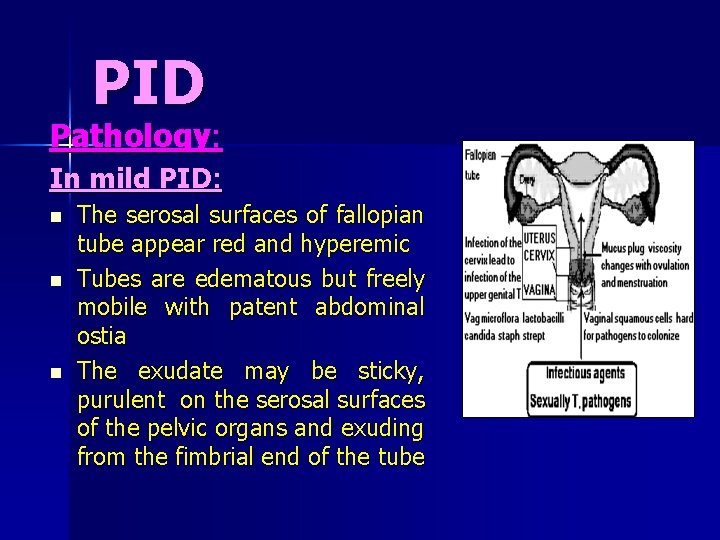
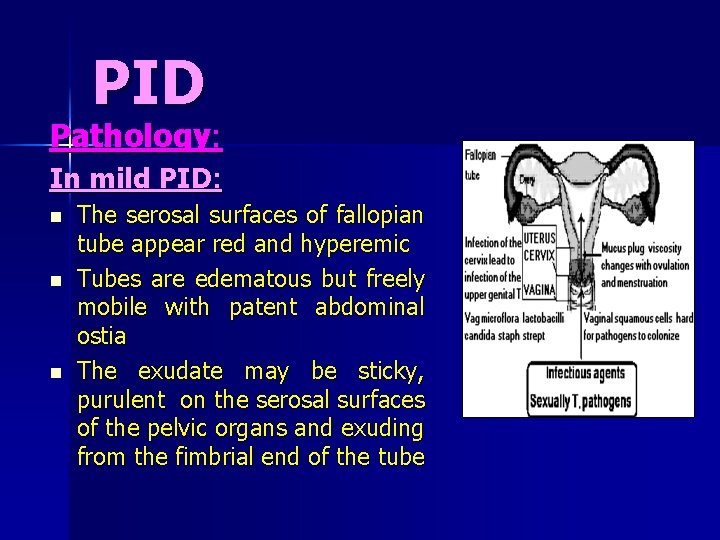
PID Pathology: In mild PID: n n n The serosal surfaces of fallopian tube appear red and hyperemic Tubes are edematous but freely mobile with patent abdominal ostia The exudate may be sticky, purulent on the serosal surfaces of the pelvic organs and exuding from the fimbrial end of the tube
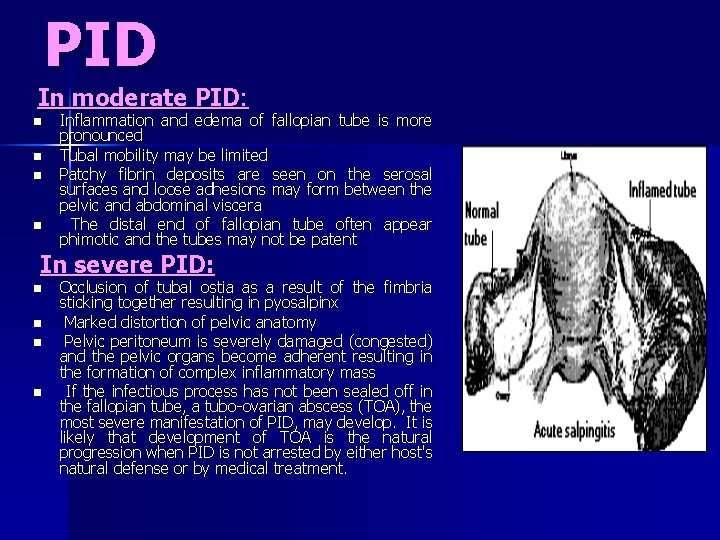
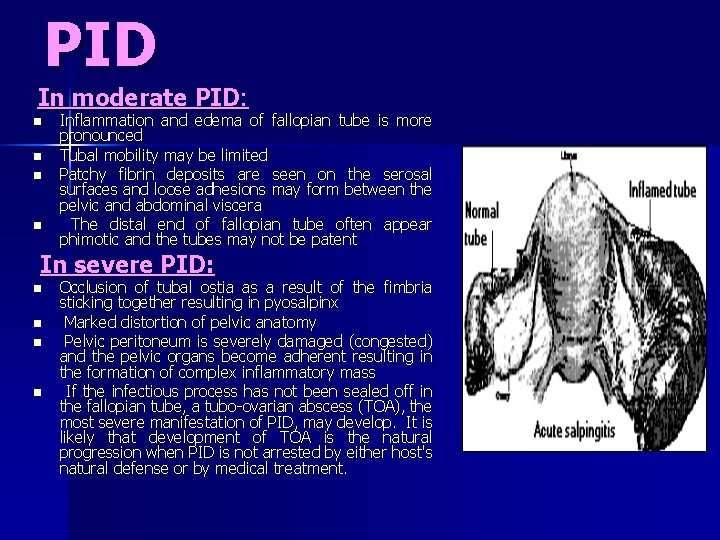
PID In moderate PID: n n Inflammation and edema of fallopian tube is more pronounced Tubal mobility may be limited Patchy fibrin deposits are seen on the serosal surfaces and loose adhesions may form between the pelvic and abdominal viscera The distal end of fallopian tube often appear phimotic and the tubes may not be patent In severe PID: n n Occlusion of tubal ostia as a result of the fimbria sticking together resulting in pyosalpinx Marked distortion of pelvic anatomy Pelvic peritoneum is severely damaged (congested) and the pelvic organs become adherent resulting in the formation of complex inflammatory mass If the infectious process has not been sealed off in the fallopian tube, a tubo-ovarian abscess (TOA), the most severe manifestation of PID, may develop. It is likely that development of TOA is the natural progression when PID is not arrested by either host's natural defense or by medical treatment.
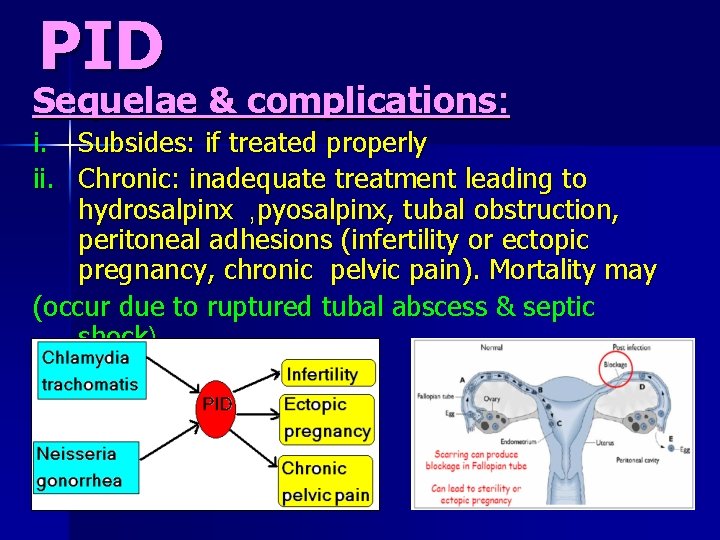
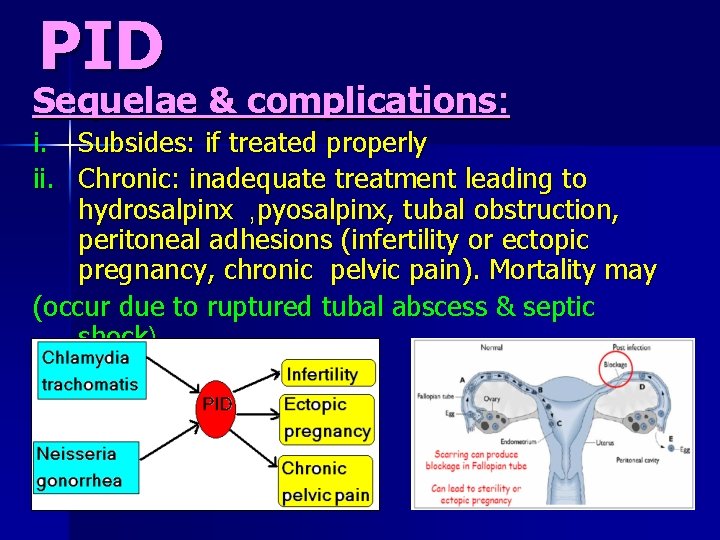
PID Sequelae & complications: i. Subsides: if treated properly ii. Chronic: inadequate treatment leading to hydrosalpinx , pyosalpinx, tubal obstruction, peritoneal adhesions (infertility or ectopic pregnancy, chronic pelvic pain). Mortality may (occur due to ruptured tubal abscess & septic shock).

PID Clinical picture: § Severe pain & tenderness lower abdomen § § § Fever, Malaise, vomiting, tachycardia Offensive vaginal discharge Bilateral adnexal tenderness Cervical mobility tenderness Tubo-ovarian mass
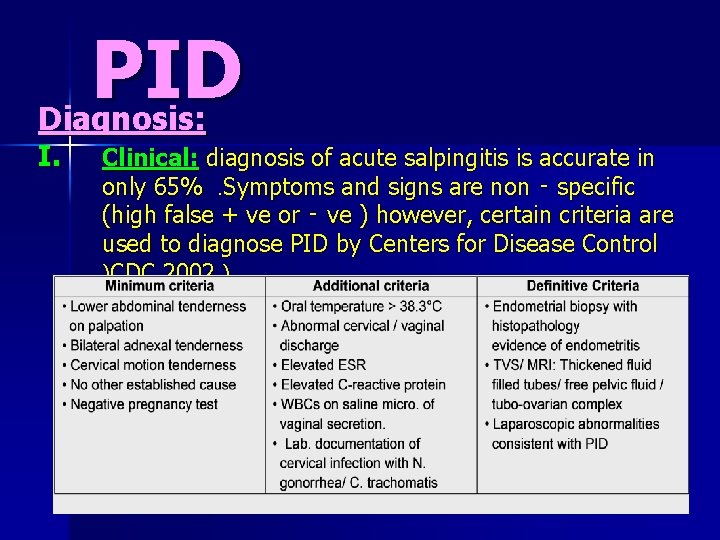
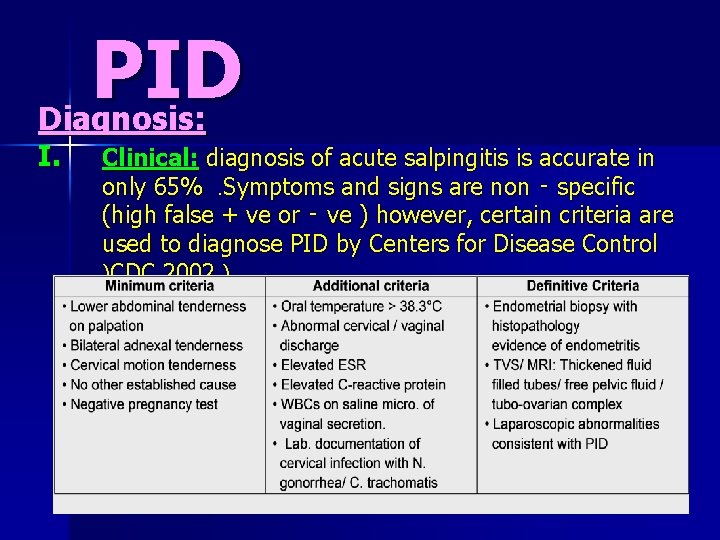
PID Diagnosis: I. Clinical: diagnosis of acute salpingitis is accurate in only 65%. Symptoms and signs are non ‑ specific (high false + ve or ‑ ve ) however, certain criteria are used to diagnose PID by Centers for Disease Control )CDC 2002 )
II )Laboratory investigations : to detect organisms or evidence of their antibodies 1. Gm stain and cervical culture for gonococci 2. High vaginal swab for WBC 3. Gm stain for (B. V) 4. ELISA or culture from the cervix for chlamydia 5. Urethral, rectal or oral cultures for gonococci 6. Serologic test for syphilis, hepatitis B and C, HIV as the patient with one STD is at risk for other infection III) Laparoscopic diagnosis : gold standard (definitive) – – – Pronounced hyperemia of tubal surface Edema of tubal wall A sticky exudate on tubal surface and from tubal ends when patent Differential Diagnosis: Gynecologic: ectopic (tubal), Torsion/ ruptured ovarian cyst and endometriosis GIT: appendicitis, diverticulitis. UTI: Cystits/ pyelonephritis
PID Treatment of PID Principles: n n The goal of therapy in uncomplicated acute salpingitis is: 1. 2. 3. Prevention of infertility Prevention of ectopic pregnancy Prevention of tubo‑ovarian abscess The goal of therapy in salpingitis complicated by abscess is : 1. Preservation of life 2. Prevention of septic complications General: - Rest in Fowler's position - Light diet with free fluid - Sedatives Antibiotics: n As PID is polymicrobial, antibiotic coverage should include: 1 - Chlamydia 2 - N. G 3 -Anaerobes 4‑Gm +ve and gm‑ve aerobes
Regimens : according to severity, it may be outpatient or inpatient regimens A )Outpatient regimen : if symptoms and signs are mild *Cefoxitin 2 gm I. M or Amoxycillin 3 gm IM or Ampicillin 3. 5 gm IM or Aqueous procaine penicillin G 4. 8 million U I. M. + l gm probencid + Doxycycline l 00 mg twice daily for 10 ‑ 14 days * Another regimen: Metronidazole + Tetracycline orally B )Inpatient regimen : Criteria for hospitalization 1 - Diagnosis is uncertain 2 - Suspected pelvic abscess 3 - Pregnancy 4 - IUD 5 - Temperature > 38°c 6 - Adolescent 7 - Nausea and vomiting 8 - Failure to respond to oral antibiotics within 48 hr
![Regimens 1 Cefoxitin 2 gm I V 6 hr Doxycycline l 00 Regimens: 1] Cefoxitin 2 gm I. V. / 6 hr + Doxycycline l 00](https://slidetodoc.com/presentation_image_h2/48c45978360ae0fba53ef40d2a1e8fe1/image-53.jpg)
Regimens: 1] Cefoxitin 2 gm I. V. / 6 hr + Doxycycline l 00 mg I. V. / 12 hr for at least 4 days or 2 days after patient is a febrile then doxycycline l 00 mg orally to complete 2 weeks. This regimen covers all pathogens 2] Cefotaxime lgm / 6 hr + Metronidazole lgm / 12 hr. rectal suppository. NB: If no improvement, laparoscope is indicated
Pelvic abscess Tubo-ovarian abscess: communication between pyosalpinx and ovarian abscess n Pelvic abscess: pelvic peritonitis → pus collection in Douglas pouch→ roofed by adherent intestine and omentum. Pelvic abscess can be divided according to mode of infection into: 1 - Primary : due to ascending infection without predisposing factor i. e. without surgery , trauma or pregnancy 2 - Secondary : a‑ Following pregnancy : l‑ Postabortive infection 2 - Puerpeural infection 3 - Infected chomplicated ectopic pregnancy. b‑ Direct extension e. g. following appendicitis or diverticulitis c‑ Following surgery e. g. cuff abscess n
Pelvic abscess Clinical presentation: A) Uncomplicated tuboovarian abscess: The same clinical picture of uncomplicated salpingitis. Differentiation requires determination of an inflammatory adnexal mass. On examination: n n n Patient appears ill with temperature elevated She walks slowly with the hand on lower abdomen Abdominal distention and direct and rebound tenderness in the lower abdominal quadrant Pelvic examination is extremely painful with tender cervical mobility An irregular, tender, fixed inflammatory mass may be felt on one or both sides of the pelvis. B) Ruptured tuboovarian abscess: • Symptoms: Acute progressive pelvic pain which is so severe
Pelvic abscess • Examination: - Patient appear ill, dehydrated - Abdominal distention - Absent intestinal sound ‑ Pelvic mass is felt in 50% of cases - Fever, tachycardia, leucocytosis. ‑ Culdecentesis reveal purulent material - Signs of generalized peritonitis with shifting dullness. Management of pelvic abscess : whatever the etiological factor involved in the pathogenesis of pelvic abscess, the initial approach to the problem is the same. Once diagnosis has been made, the patient is admitted to hospital for drainage of the pus by posterior
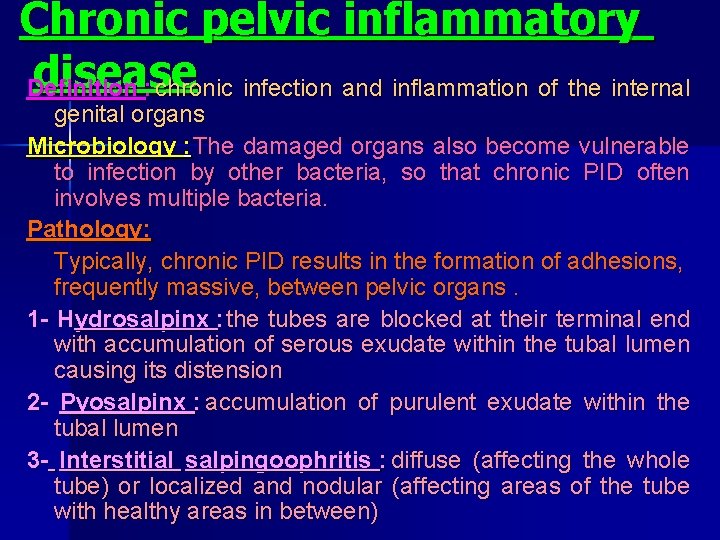
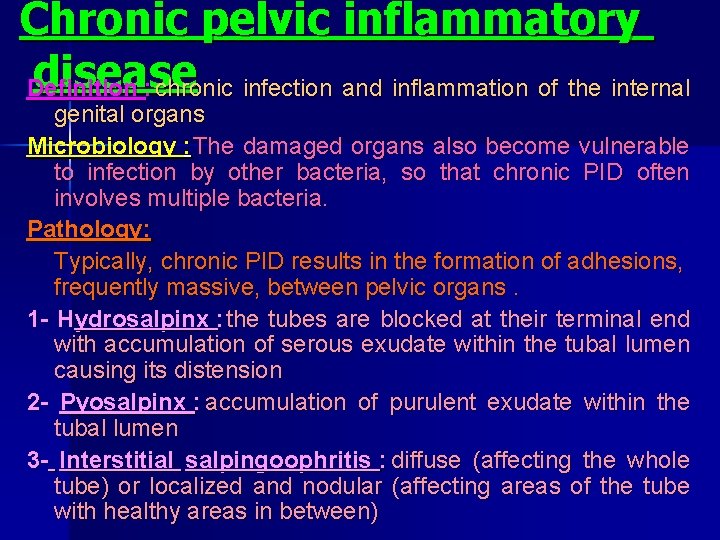
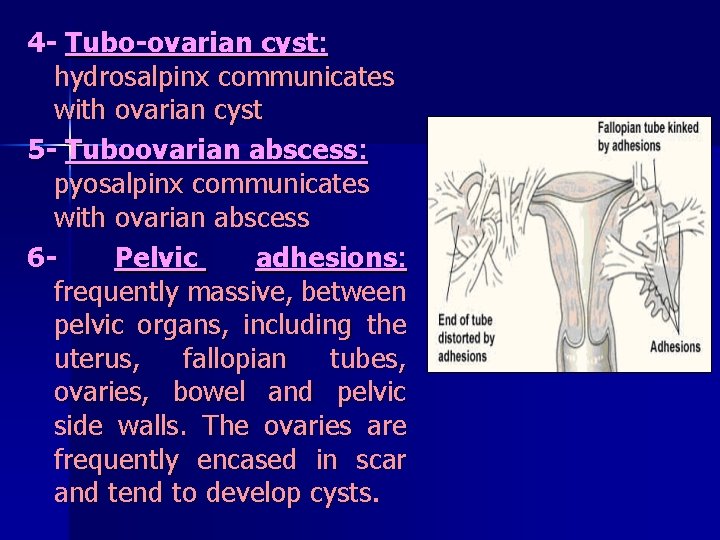
Chronic pelvic inflammatory disease Definition : chronic infection and inflammation of the internal genital organs Microbiology : The damaged organs also become vulnerable to infection by other bacteria, so that chronic PID often involves multiple bacteria. Pathology: Typically, chronic PID results in the formation of adhesions, frequently massive, between pelvic organs. 1 - Hydrosalpinx : the tubes are blocked at their terminal end with accumulation of serous exudate within the tubal lumen causing its distension 2 - Pyosalpinx : accumulation of purulent exudate within the tubal lumen 3 - Interstitial salpingoophritis : diffuse (affecting the whole tube) or localized and nodular (affecting areas of the tube with healthy areas in between)
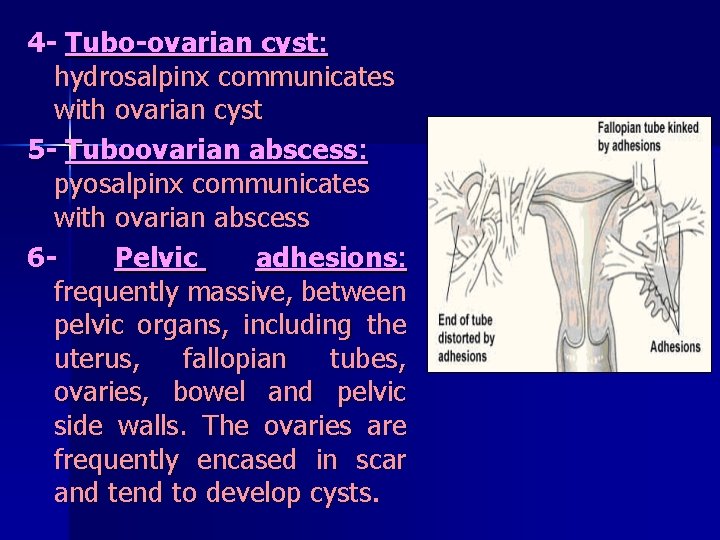
4 - Tubo-ovarian cyst: hydrosalpinx communicates with ovarian cyst 5 - Tuboovarian abscess: pyosalpinx communicates with ovarian abscess 6 Pelvic adhesions: frequently massive, between pelvic organs, including the uterus, fallopian tubes, ovaries, bowel and pelvic side walls. The ovaries are frequently encased in scar and tend to develop cysts.
Clinical picture of chronic PID: – – – – – General malaise & fatigue Chronic lower abdominal pain, Backache Deep dyspareunia, dysmennorhea Intermittent vaginal discharge Heavy periods or intermenstrual irregular bleeding Infertility Bowel symptoms such as abdominal cramps and constipation Lower abdominal/ pelvic tenderness Bulky, tender uterus Intermittently, the chronic infection is complicated by acute episodes characterized by fever and severe pain Differential Diagnosis: Uterine fibroid Chronic disturbed ectopic pregnancy Ovarian tumour T. B. of pelvic organs Pelvic endometriosis Chronic appendicitis Broad ligament tumour
Treatment: *Medical: Rest, proper diet and vitamins Pelvic heat e. g. short wave therapy Long course (6 -8 weeks) of antibiotics Anti-inflammatory steroids (prednisone) *Surgical: A )Conservative : especially if future pregnancy is an issue , the great majority of patients with chronic pelvic inflammatory disease can be successfully treated without a hysterectomy Salpingolysis Salpingostomy Unilateral salpingoophrectomy Cervical dilation and antibiotics in cases of pyometra B) Radical : if childbearing is not an issue , this condition is commonly treated by surgical removal of both ovaries and fallopian tubes, with or without hysterectomy.