Iliac Lesions Covered Versus Uncovered Stents John Fritz






- Slides: 26
Iliac Lesions Covered Versus Uncovered Stents John Fritz Angle, M. D. University of Virginia Charlottesville, VA
John Angle, M. D. Consultant: Medtronic Cook W. L. Gore Research Funding: Siemens Medical
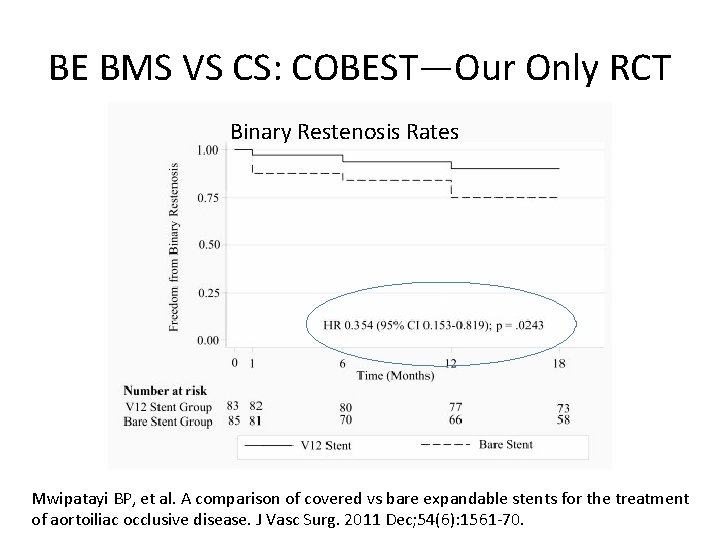
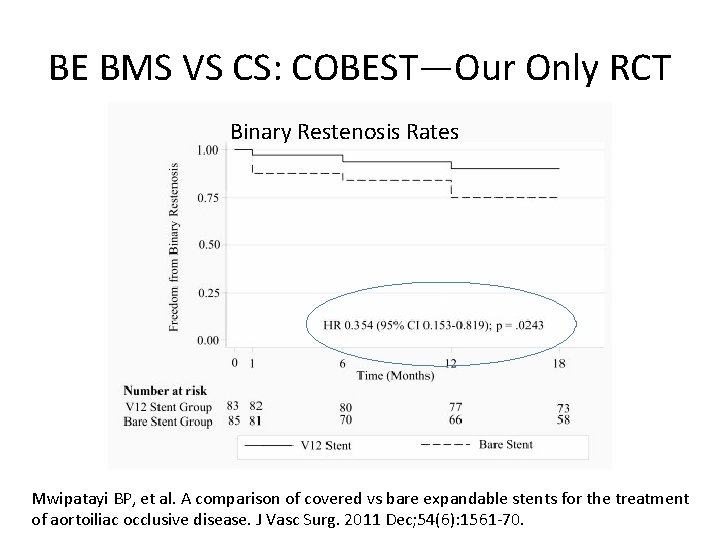
BE BMS VS CS: COBEST—Our Only RCT Binary Restenosis Rates Mwipatayi BP, et al. A comparison of covered vs bare expandable stents for the treatment of aortoiliac occlusive disease. J Vasc Surg. 2011 Dec; 54(6): 1561 -70.
Questions That Remain Unanswered • Significant difference in freedom from binary restenosis for BE CS in TASC C and D lesions compared with BE BMS (hazard ratio, 0. 13; 95% CI: 0. 042 -0. 442) but no difference for TASC B lesions (hazard ratio, 0. 74; 95% CI, 0. 23 -2. 38) • TASC does not differentiate aorta/CIA versus EIA (only 14/168 patients had EIA treated) or occlusion length (shortcoming of TASC) • Only 18 months of follow-up Mwipatayi BP, et al. A comparison of covered vs bare expandable stents for the treatment of aortoiliac occlusive disease. J Vasc Surg. 2011 Dec; 54(6): 1561 -70.
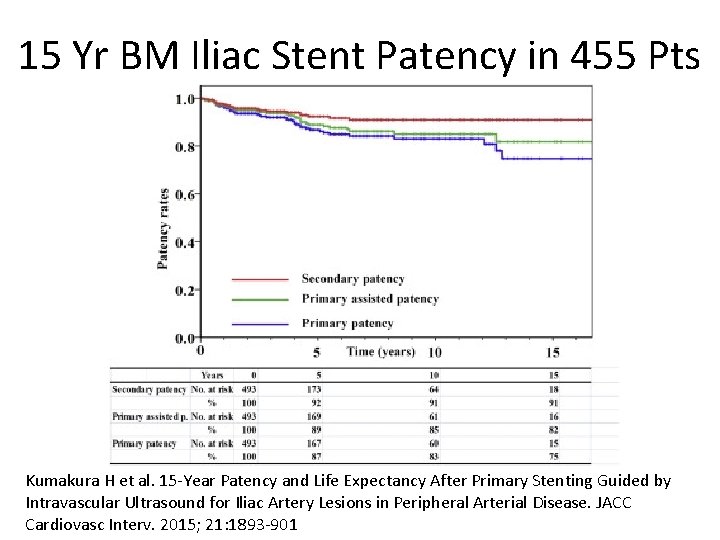
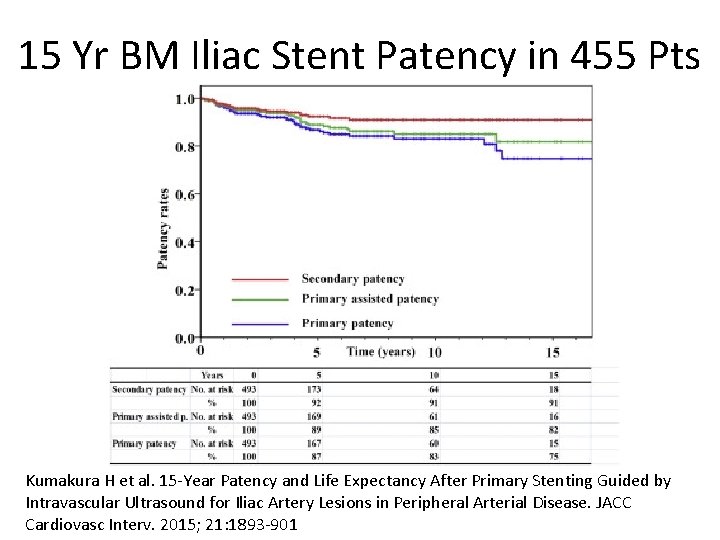
15 Yr BM Iliac Stent Patency in 455 Pts Kumakura H et al. 15 -Year Patency and Life Expectancy After Primary Stenting Guided by Intravascular Ultrasound for Iliac Artery Lesions in Peripheral Arterial Disease. JACC Cardiovasc Interv. 2015; 21: 1893 -901
Assisted Stent Patency • Variety of BM stents • Median observation was 63 months (range 1 to 246 months) • 5, 10, and 15 years, primary patencies were 87%, 83%, and 75% • 5, 10, and 15 years, primary-assisted patencies were 89%, 85%, and 82% Kumakura H et al. 15 -Year Patency and Life Expectancy After Primary Stenting Guided by Intravascular Ultrasound for Iliac Artery Lesions in Peripheral Arterial Disease. JACC Cardiovasc Interv. 2015; 21: 1893 -901
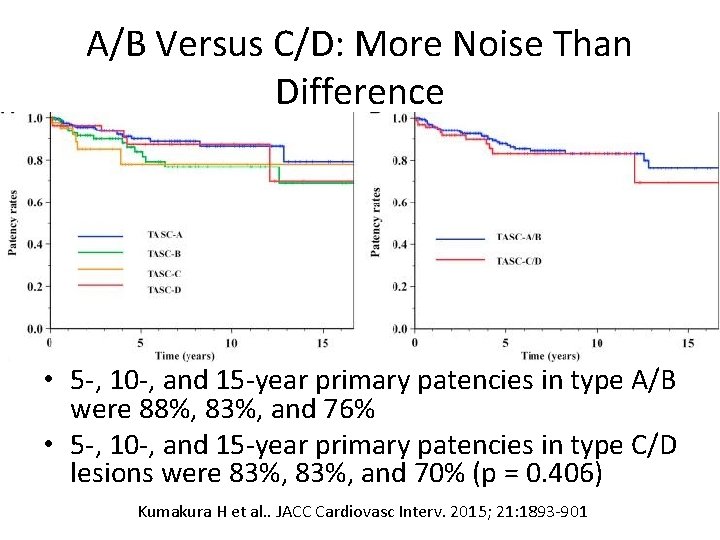
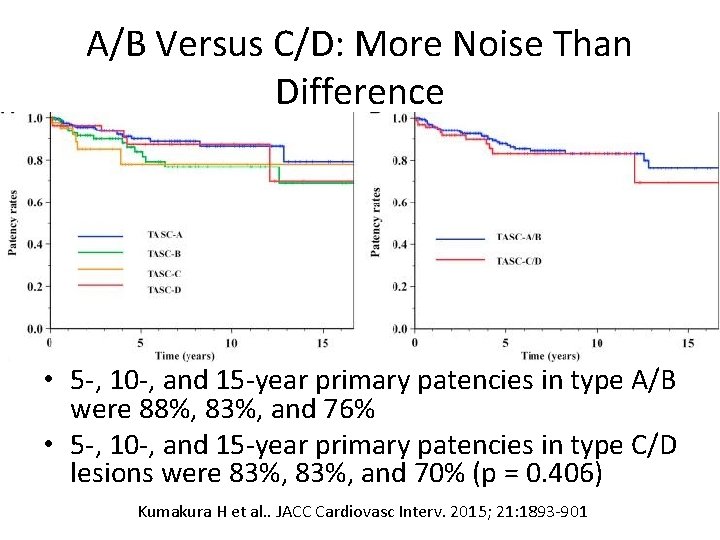
A/B Versus C/D: More Noise Than Difference • 5 -, 10 -, and 15 -year primary patencies in type A/B were 88%, 83%, and 76% • 5 -, 10 -, and 15 -year primary patencies in type C/D lesions were 83%, and 70% (p = 0. 406) Kumakura H et al. . JACC Cardiovasc Interv. 2015; 21: 1893 -901
Cox Multi-variate Analysis of Factors Associated with Restenosis Lesion length Pre-procedure stenosis severity Calcified lesions Post-procedural angiographic stenosis rates, Pre- and post-procedural IVUS minimum lesion area • SE versus BE was NOT significant (covered not analyzed) • • • Kumakura H et al. 15 -Year Patency and Life Expectancy After Primary Stenting Guided by Intravascular Ultrasound for Iliac Artery Lesions in Peripheral Arterial Disease. JACC Cardiovasc Interv. 2015; 21: 1893 -901
Long Lesions and Runoff Important • 62 iliacs (87 stents) in 54 patients • Primary stent patency at 1 and 2 years was 83. 0% and 79. 9% • Primary patency rates at 1 and 2 years by length: – stents ≤ 61 mm were 90. 6% and 86. 6% – stents >61 mm were 67. 7% and 60. 2% (P=0. 016) • Multivariate Cox regression analysis of patency: – stent in both the CIA and the EIA (HR: 3. 3; 95% CI: 1. 19. 5; P=0. 021) – poor runoff (HR: 3. 2; 95%, CI 1. 0 -10. 0; P=0. 047) Kavaliauskienė Z, et al. Factors affecting primary patency of stenting for Trans. Atlantic Inter. Society (TASC II) type B, C, and D iliac occlusive disease. Medicina (Kaunas) 2014; 50(5): 287 -94.
Self-Expanding: CS Versus BMS • 128 patients (mean age of 70 years)--167 iliac arteries TASC II C in 86 (51%) and D in 81 (49%) • Technical success 99% in both groups (P = 1. 0) • 30 -day cumulative complications rate (CS vs BMS) (7. 3% vs 4. 7%; P =. 53) are nearly equal • Mortality (1. 8% vs 0%; P =. 45) and Morbidity (1. 8% vs 1. 4%; P =. 99) are similar Piazza M, et al. Outcomes of polytetrafluoroethylene-covered stent versus bare-metal stent in the primary treatment of severe iliac artery obstructive lesions. J Vasc Surg. 2015 Nov; 62(5): 1210 -1218.
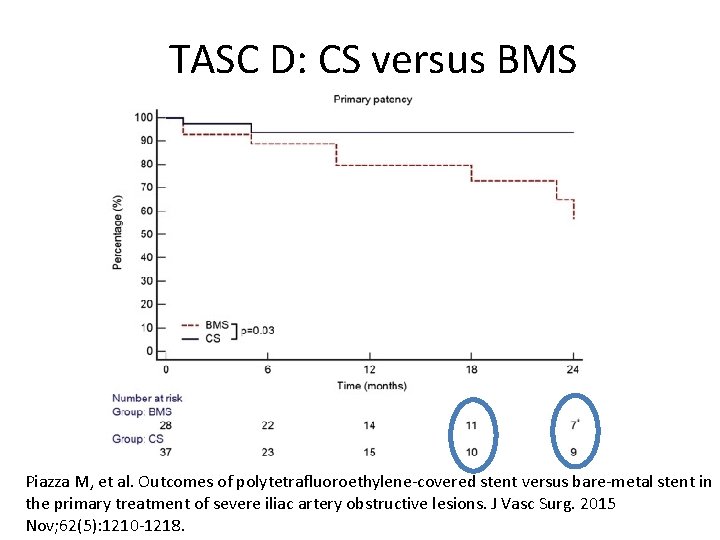
SE stent: Analysis by Lesion Length • Primary patency of CS vs BMS (93% vs 80%; P =. 14 at 24 months (average 22 m; 30 days-56 mo) • TASC D, primary patency at 24 mo was significantly higher for CS than BMS (88% vs 57%; P =. 03) • Limb salvage was 99% and 95% (P =. 35) • Multivariate analysis indicated BMS in longsegment stenoses involving the common and external iliac arteries was a negative predictor of patency (odds ratio, 0. 16; 95% confidence interval, 0. 04 -0. 62; P =. 007 Piazza M, et al. Outcomes of polytetrafluoroethylene-covered stent versus bare-metal stent in the primary treatment of severe iliac artery obstructive lesions. J Vasc Surg. 2015 Nov; 62(5): 1210 -1218.
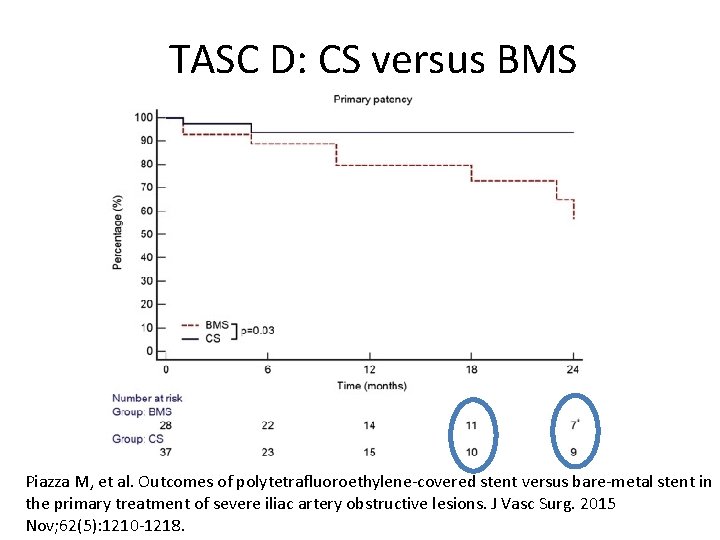
TASC D: CS versus BMS Piazza M, et al. Outcomes of polytetrafluoroethylene-covered stent versus bare-metal stent in the primary treatment of severe iliac artery obstructive lesions. J Vasc Surg. 2015 Nov; 62(5): 1210 -1218.
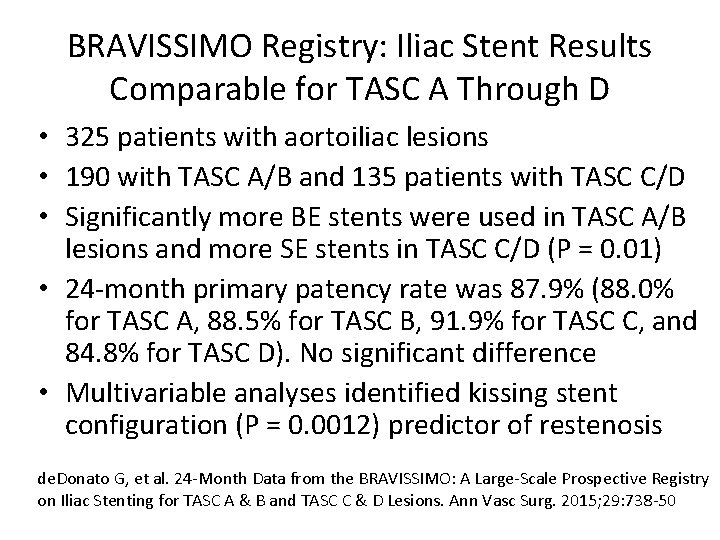
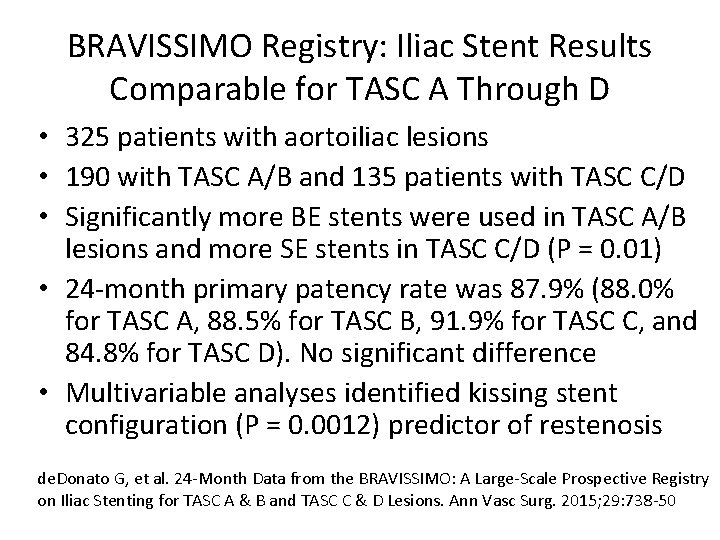
BRAVISSIMO Registry: Iliac Stent Results Comparable for TASC A Through D • 325 patients with aortoiliac lesions • 190 with TASC A/B and 135 patients with TASC C/D • Significantly more BE stents were used in TASC A/B lesions and more SE stents in TASC C/D (P = 0. 01) • 24 -month primary patency rate was 87. 9% (88. 0% for TASC A, 88. 5% for TASC B, 91. 9% for TASC C, and 84. 8% for TASC D). No significant difference • Multivariable analyses identified kissing stent configuration (P = 0. 0012) predictor of restenosis de. Donato G, et al. 24 -Month Data from the BRAVISSIMO: A Large-Scale Prospective Registry on Iliac Stenting for TASC A & B and TASC C & D Lesions. Ann Vasc Surg. 2015; 29: 738 -50
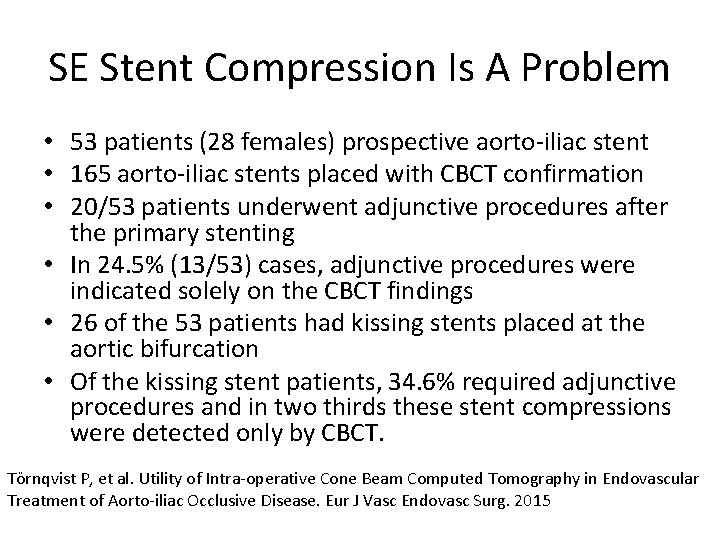
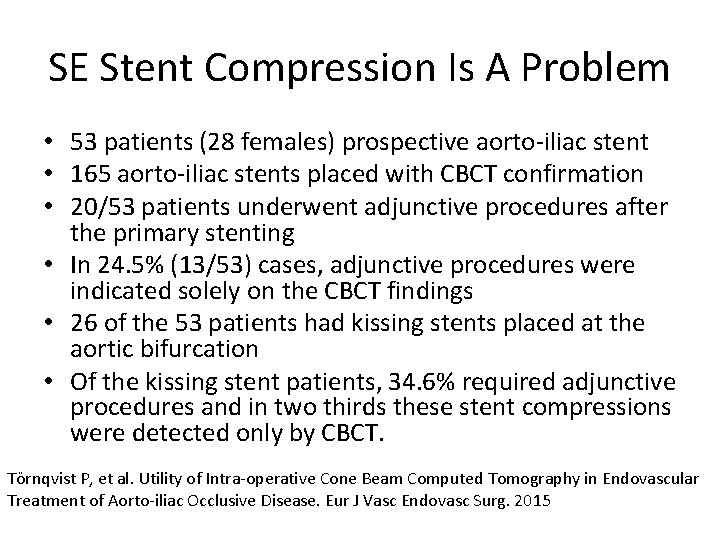
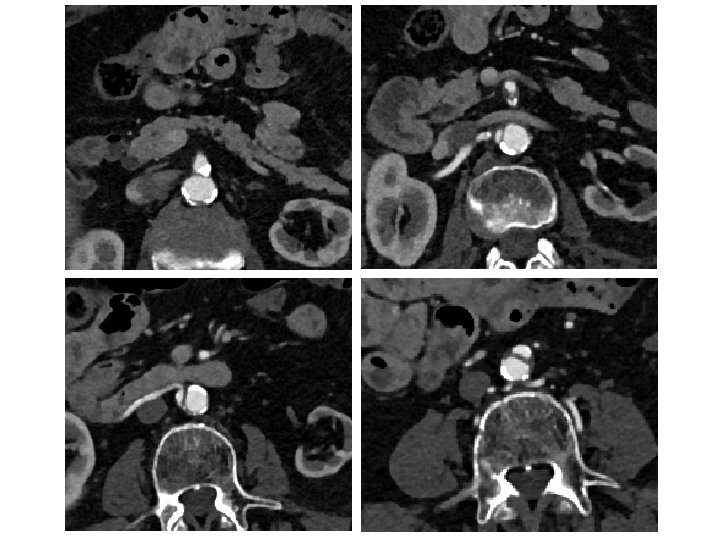
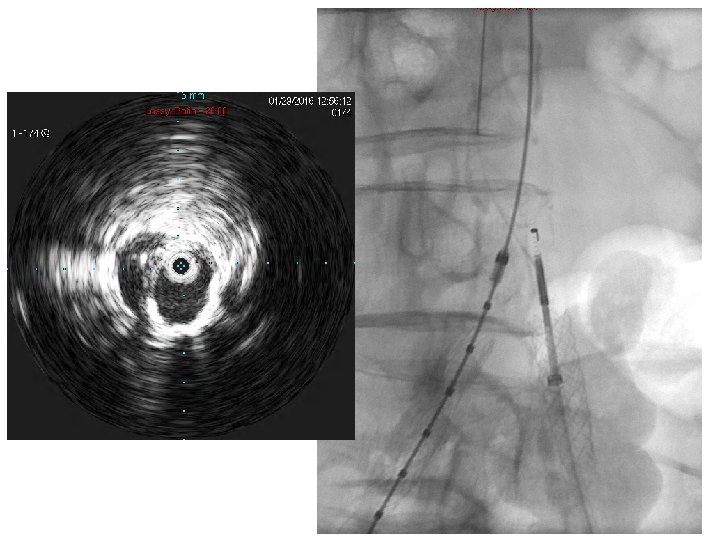
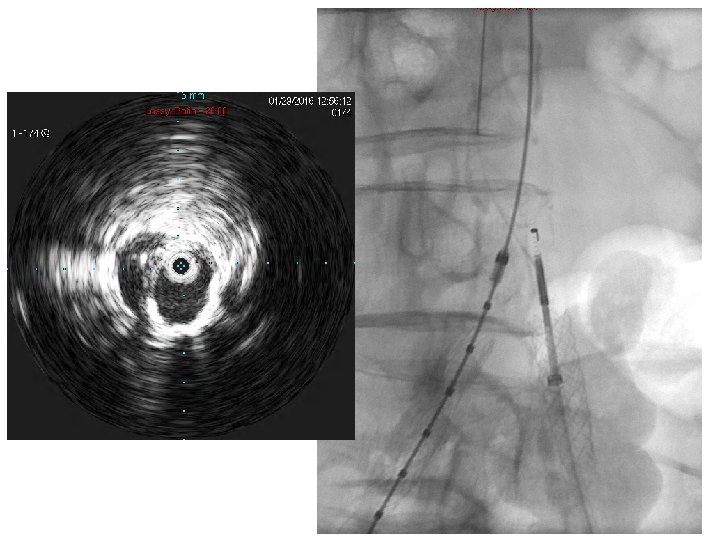
SE Stent Compression Is A Problem • 53 patients (28 females) prospective aorto-iliac stent • 165 aorto-iliac stents placed with CBCT confirmation • 20/53 patients underwent adjunctive procedures after the primary stenting • In 24. 5% (13/53) cases, adjunctive procedures were indicated solely on the CBCT findings • 26 of the 53 patients had kissing stents placed at the aortic bifurcation • Of the kissing stent patients, 34. 6% required adjunctive procedures and in two thirds these stent compressions were detected only by CBCT. Törnqvist P, et al. Utility of Intra-operative Cone Beam Computed Tomography in Endovascular Treatment of Aorto-iliac Occlusive Disease. Eur J Vasc Endovasc Surg. 2015
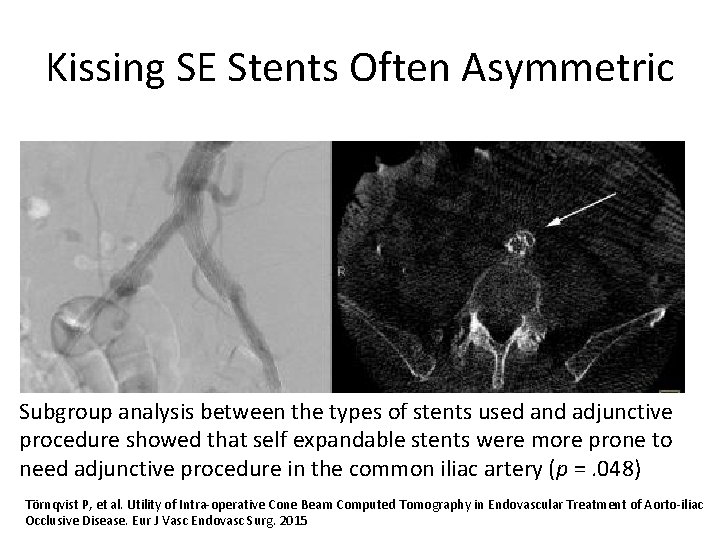
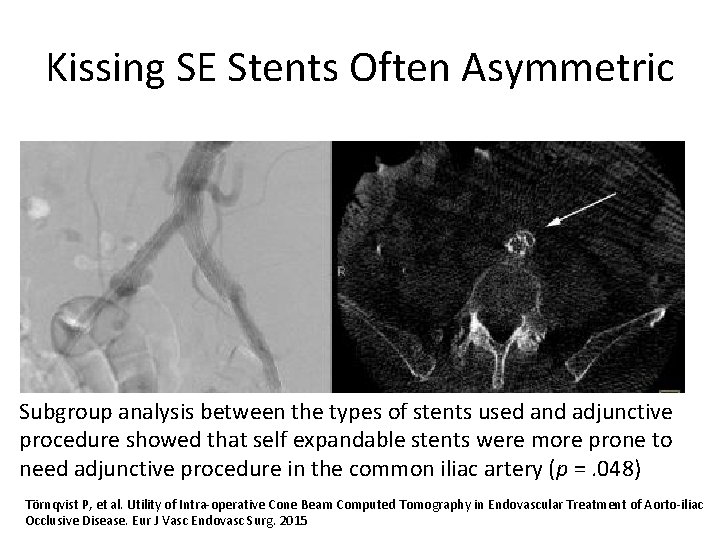
Kissing SE Stents Often Asymmetric Subgroup analysis between the types of stents used and adjunctive procedure showed that self expandable stents were more prone to need adjunctive procedure in the common iliac artery (p =. 048) Törnqvist P, et al. Utility of Intra-operative Cone Beam Computed Tomography in Endovascular Treatment of Aorto-iliac Occlusive Disease. Eur J Vasc Endovasc Surg. 2015






Kissing CBE Stents Still Essential With Distal Aorta Disease • In cases of aortic reentry—kissing stents insure both CIA have adequate flow • The farther the stents extend into the aorta (more that just touching) the more likely they are to narrow/occlude • Kissing Iliac stents should be BE CS (CS>>BMS) Sabri SS, et al. Outcomes of covered kissing stent placement compared with bare metal stent placement in the treatment of atherosclerotic occlusive disease at the aortic bifurcation. J Vasc Interv Radiol. 2010 Jul; 21(7): 995 -1003.
Single Versus Kissing Stents for Unilateral Proximal CIA Disease • Unilateral >50% CIA and 30%-50% in the contralateral CIA • 80 patients (69 males, 66. 6 years) treated with a single stent and 30 (26 males, 67. 1 years) treated with kissing stents • Two patients in the single-stent group (3%) required bailout kissing stents because of plaque shift to the contralateral side • Major complication rates: 8% in single-stent vs 13% in the kissing -stent group (P =. 399) • At 3 years, the single-stent and kissing-stents group had similar primary patency (89% vs 87%; P =. 916) and target lesion revascularization-free survival (93% vs 87%; P =. 462) Suh Y et al. Outcomes of the single-stent versus kissing-stents technique in asymmetric complex aortoiliac bifurcation lesions. J Vasc Surg. 2015; 62: 68 -74
Summary • Residual stenosis is important—get multiple views and consider IVUS and/or CBCT • Kissing stents probably not needed in every proximal CIA lesion, but CBE stents still first choice for bifurcation • Runoff quality, lesion length and calcification are best predictors of poor outcome > stent type
 Uncovered interest rate parity formula
Uncovered interest rate parity formula Covered interest arbitrage takes place when
Covered interest arbitrage takes place when Nibbling of uncovered skin
Nibbling of uncovered skin General structure of news item
General structure of news item Cooking term fold
Cooking term fold Cooking food uncovered without liquid or fat.
Cooking food uncovered without liquid or fat. Importance of choosing the right cooking technique
Importance of choosing the right cooking technique Iliac region
Iliac region Inferior gastric artery
Inferior gastric artery Internal iliac branches mnemonic
Internal iliac branches mnemonic Posterior inferior iliac spine
Posterior inferior iliac spine Iliac regions
Iliac regions Puddle sign
Puddle sign Iliac stent complications
Iliac stent complications Ileolumbar
Ileolumbar Anterior superior iliac spine
Anterior superior iliac spine M
M Aortic nodes
Aortic nodes Right iliac fossa
Right iliac fossa Sonja bone
Sonja bone Pelvic girdle
Pelvic girdle Foot vascular anatomy
Foot vascular anatomy Anastemosis
Anastemosis Iliac crest
Iliac crest Ischiofemoral ligament
Ischiofemoral ligament Aourta
Aourta Falciform fascia
Falciform fascia