Covered Versus Uncovered Iliac Artery Stents J Fritz






























- Slides: 40
Covered Versus Uncovered Iliac Artery Stents J. Fritz Angle, M. D. University of Virginia Charlottesville, VA
Disclosures Research Support: Proteon Siemens Medical
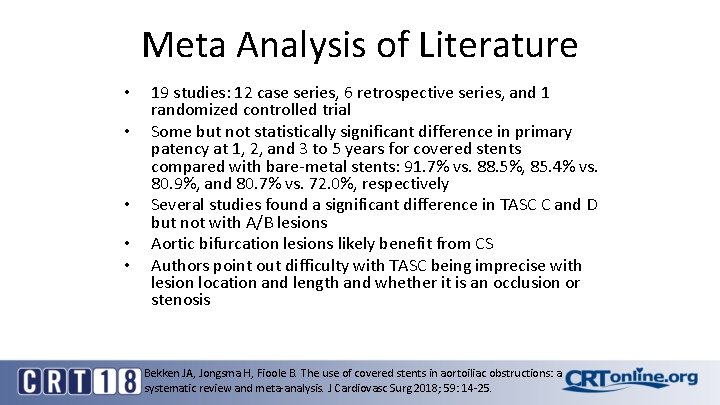
Meta Analysis of Literature • • • 19 studies: 12 case series, 6 retrospective series, and 1 randomized controlled trial Some but not statistically significant difference in primary patency at 1, 2, and 3 to 5 years for covered stents compared with bare-metal stents: 91. 7% vs. 88. 5%, 85. 4% vs. 80. 9%, and 80. 7% vs. 72. 0%, respectively Several studies found a significant difference in TASC C and D but not with A/B lesions Aortic bifurcation lesions likely benefit from CS Authors point out difficulty with TASC being imprecise with lesion location and length and whether it is an occlusion or stenosis Bekken JA, Jongsma H, Fioole B. The use of covered stents in aortoiliac obstructions: a systematic review and meta-analysis. J Cardiovasc Surg 2018; 59: 14 -25.
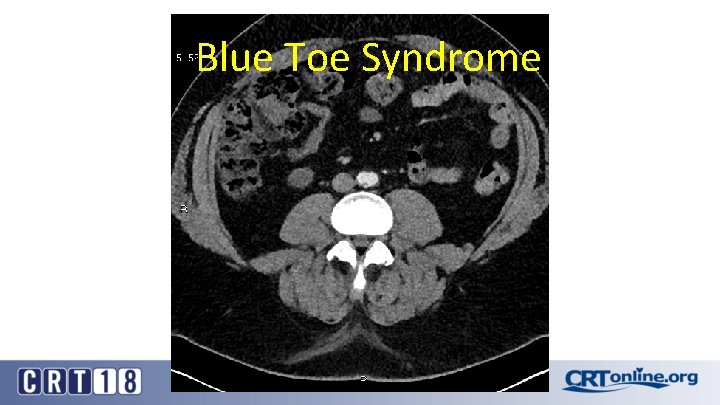
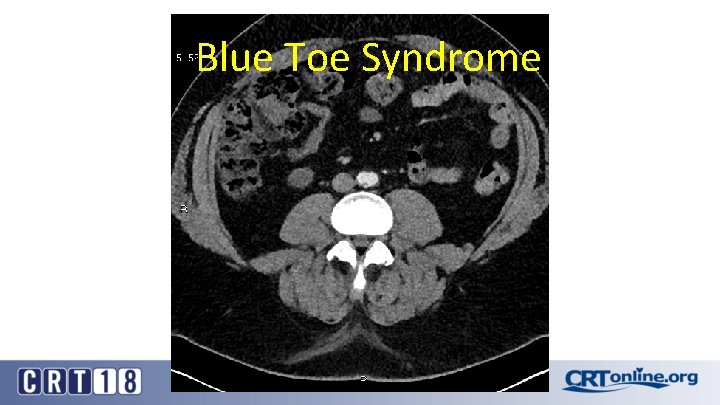
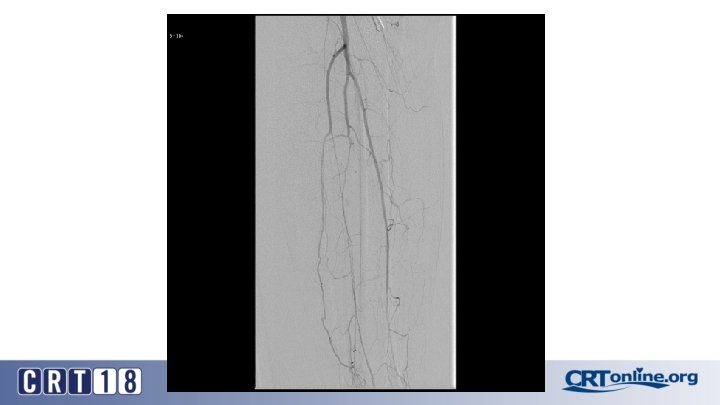
Blue Toe Syndrome























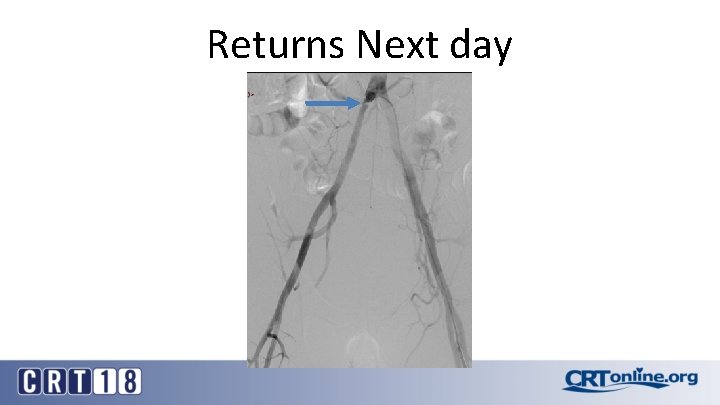
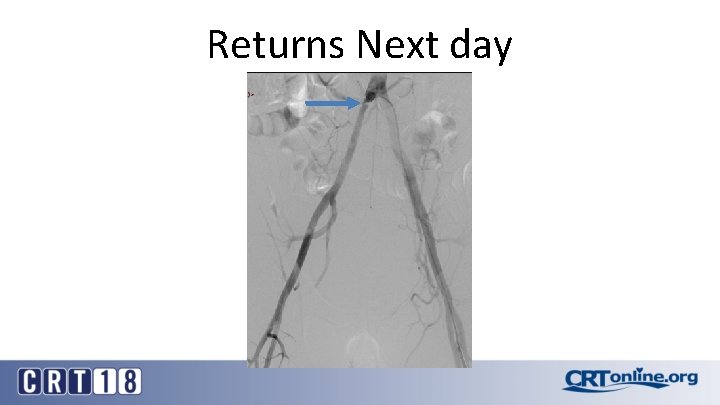
Returns Next day






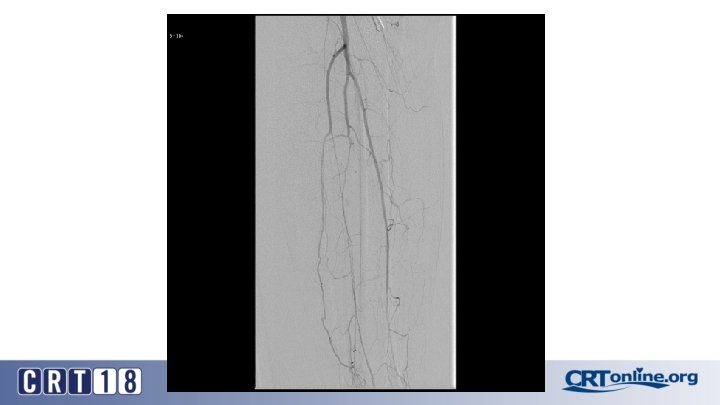
Failed recanalization: BKA
Case selection bias leads to wide ranging conclusions • Only one RCT of CS versus BMS (Mwipatayi, 2011): CS ultrasound based restenosis and TLR superior to BMS) • One large recent case series (Revuelta, 2014): BMS patency at 30 months markedly superior to CS for TASC C/D • Unlikely to see additional RCT given low failure rate of all iliac stents • All these studies have case selection bias • We need a way to dive into the sub-groups that preoccupy our thinking about stent selection without a prospective blinded trial Revuelta S, et al. Endovascular treatment of external iliac artery occlusive disease: midterm results. J Endovasc Ther. 2014; 21(2): 223 -9.
Propensity score analysis • • • Propensity score matching (PSM) is a statistical technique that attempts to better estimate the effect of a intervention by accounting for the covariates that predict who will get a particular treatment PSM attempts to reduce the bias due to confounding variables that could be hidden or ignored when simply comparing treatment outcomes It is a linear combination of known covariates into a single score It balances treatment and control groups on a number of covariates without losing a large number of observations. (i. e. if the treatment and control groups were balanced on a number of covariates one at a time, large numbers of observations would be needed) Caveat: it can only balance out measurable co-variables and cannot balance hidden factors in device selection Vikatmaa P. Commentary on "Outcomes of Self Expanding Polytetrafluoroethylene Covered Stent versus Bare Metal Stent for Chronic Iliac Artery Occlusion in Matched Cohorts Using Propensity Score Modeling". Eur J Vasc Endovasc Surg. 2017; 54: 186.
CS Compared to BMS in iliac occlusion • 2009 and December 2015, 128 iliac artery occlusions were stented • A CS was implanted in 78 iliac arteries (61%) and a BMS in 50 (49%) • After propensity score matching (lesion site and length separated and associated femoropopliteal disease included) (47 for each group). • Technical success was 98% • Complication rates same: 12% vs. 12%, p = 1. 0 • 30 day mortality rates same: 2% vs. 2%, p = 1. 0 Piazza M, et al. Outcomes of polytetrafluoroethylene-covered stent versus bare-metal stent in the primary treatment of severe iliac artery obstructive lesions. J Vasc Surg. 2015; 62(5): 1210 -8.

CS superior to BMS, in the right setting • At 36 months (average 23 ± 17) overall primary patency only approached significance: 87% vs. 66%, p =. 06 • For TASC D, CS: 88% vs. BMS: 54% (p =. 03) • Patency was in favor of CSs for occlusions > 3. 5 cm in length (p =. 04), total lesion length > 6 cm (p =. 04), and occlusion with calcification > 75% of the arterial wall circumference (p =. 01) • Kissing stent patency also superior with CS
 Left internal iliac artery
Left internal iliac artery Branches off aortic arch
Branches off aortic arch Posterior abdominal wall
Posterior abdominal wall Pelvic arteries
Pelvic arteries Sma origin
Sma origin Uncovered interest rate parity formula
Uncovered interest rate parity formula To cut food into small uneven pieces
To cut food into small uneven pieces Rate parity rule
Rate parity rule Cooking food uncovered without added liquid or fat
Cooking food uncovered without added liquid or fat Rabies vaccine dose schedule
Rabies vaccine dose schedule Basic cooking methods
Basic cooking methods To inform the readers/listeners about a newsworthy event.
To inform the readers/listeners about a newsworthy event. Pelvic girdle muscles and ligaments
Pelvic girdle muscles and ligaments Appendiculolith
Appendiculolith Shifting dullness
Shifting dullness Iliofemoral ligament
Iliofemoral ligament Left lymphatic duct
Left lymphatic duct Foot arteries
Foot arteries Iliac tubercle
Iliac tubercle Iliac stent complications
Iliac stent complications Falciform margin
Falciform margin 坐骨神經是由下列何神經叢所發出
坐骨神經是由下列何神經叢所發出 Anastemosis
Anastemosis Anterior superior iliac spine
Anterior superior iliac spine Difference between anatomy and physiology
Difference between anatomy and physiology Rubinova vaza
Rubinova vaza Art-labeling activity: figure 7.30a
Art-labeling activity: figure 7.30a Soleal line tibia
Soleal line tibia Dr. fritz sennheiser
Dr. fritz sennheiser Teori atribusi fritz heider
Teori atribusi fritz heider Fritz perls biography
Fritz perls biography Lars fritz
Lars fritz Timeline of the microscope
Timeline of the microscope Müllersche mimikry beispiel
Müllersche mimikry beispiel Angst vor selbstwerdung
Angst vor selbstwerdung Ernst deger
Ernst deger Fritz caspers
Fritz caspers Fritz öhman
Fritz öhman Daniel ansorge
Daniel ansorge Fredrick niland
Fredrick niland Experimento de fritz went
Experimento de fritz went