Iliac Artery Aneurysms What and How to Treat
- Slides: 29
Iliac Artery Aneurysms: What and How to Treat Misaki Kiguchi, MD, MBA, MSc Med. Star Washington Hospital Med. Star Georgetown University Hospital Washington, DC
Misaki Kiguchi, MD, MBA, MSc I have no relevant financial relationships
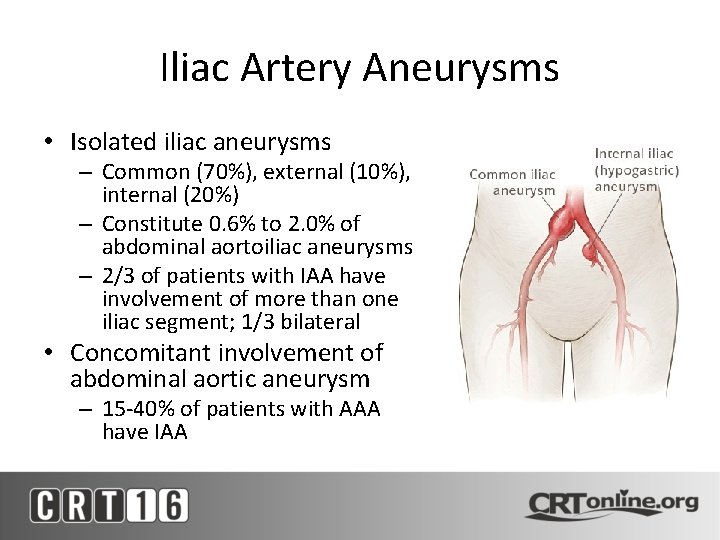
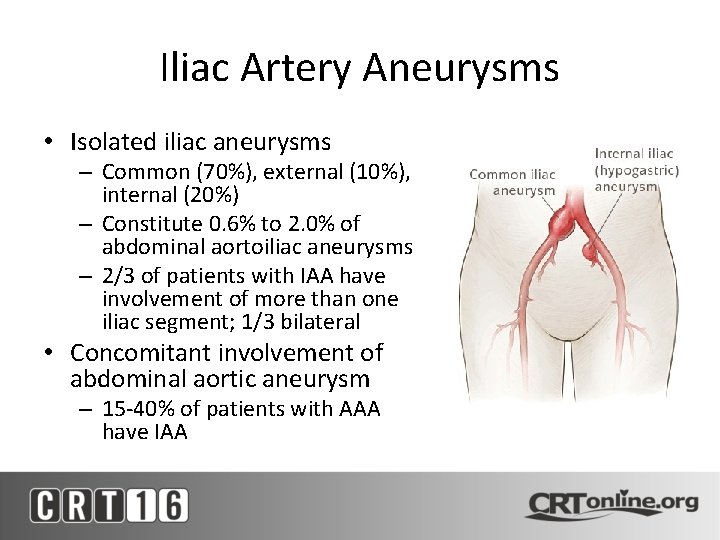
Iliac Artery Aneurysms • Isolated iliac aneurysms – Common (70%), external (10%), internal (20%) – Constitute 0. 6% to 2. 0% of abdominal aortoiliac aneurysms – 2/3 of patients with IAA have involvement of more than one iliac segment; 1/3 bilateral • Concomitant involvement of abdominal aortic aneurysm – 15 -40% of patients with AAA have IAA
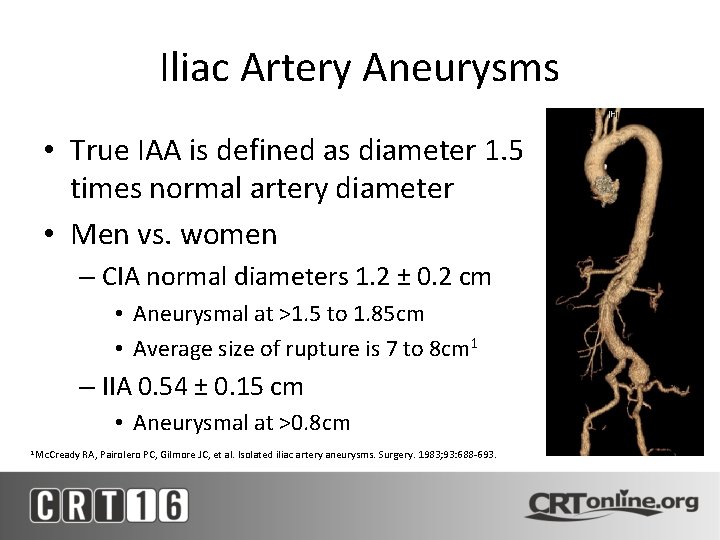
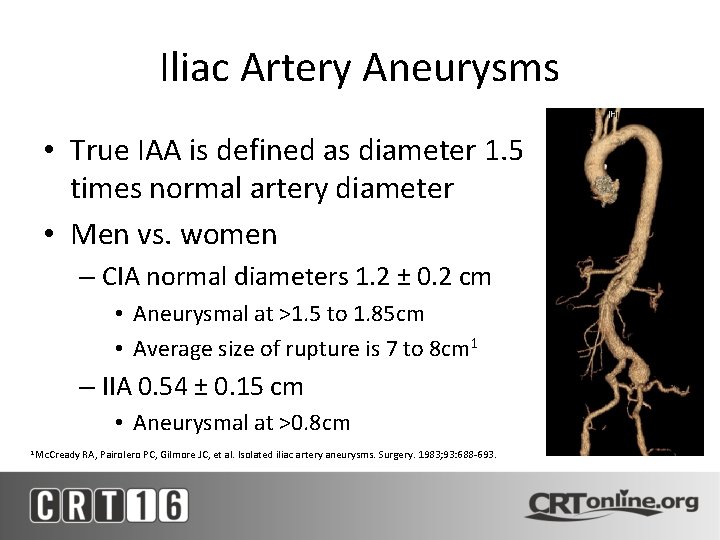
Iliac Artery Aneurysms • True IAA is defined as diameter 1. 5 times normal artery diameter • Men vs. women – CIA normal diameters 1. 2 ± 0. 2 cm • Aneurysmal at >1. 5 to 1. 85 cm • Average size of rupture is 7 to 8 cm 1 – IIA 0. 54 ± 0. 15 cm • Aneurysmal at >0. 8 cm 1 Mc. Cready RA, Pairolero PC, Gilmore JC, et al. Isolated iliac artery aneurysms. Surgery. 1983; 93: 688 -693.
Risk Factors • Similar risk factors to degenerative large vessel aneurysms – Male gender – White race – Advanced age – Smoking – Hypertension • Predicted faster iliac artery expansion compared to normotensive patients 1 `Huang Y, Gloviczki P, Duncan AA, et al. Common iliac artery aneurysm: expansion rate and results of open surgical and endovascular repair. J Vasc Surg 2008; 47: 1203
Rate of Expansion • Isolated IIA – isolated IAAs <3 cm in diameter expanded at an average rate of 1. 1 mm per year, whereas aneurysms >3 cm expanded by 2. 6 mm per year 1 • Concomitant with AAA – iliac artery expansion depended upon baseline iliac diameter 2 1 Santilli SM, Wernsing SE, Lee ES. Expansion rates and outcomes for iliac artery aneurysms. J Vasc Surg 2000; 31: 114. E, Da Giau G, Gruppo M, et al. Natural history of common iliac arteries after aorto-aortic graft insertion during elective open abdominal aortic aneurysm repair: a prospective study. Surgery 2008; 144: 822 2 Ballotta
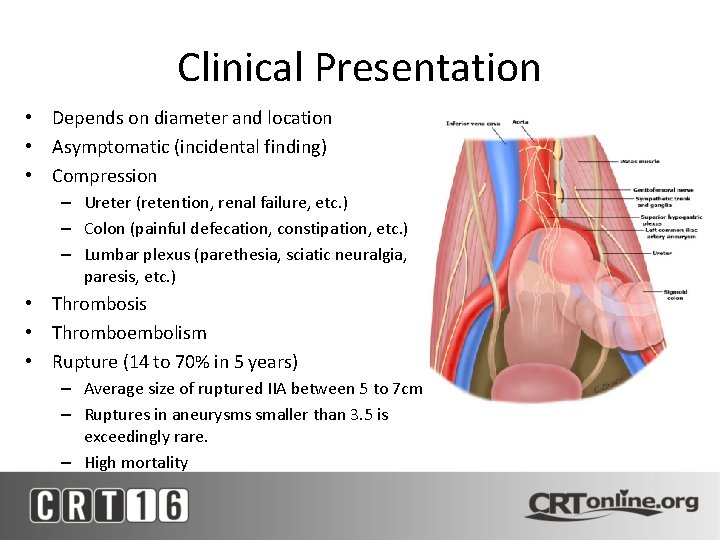
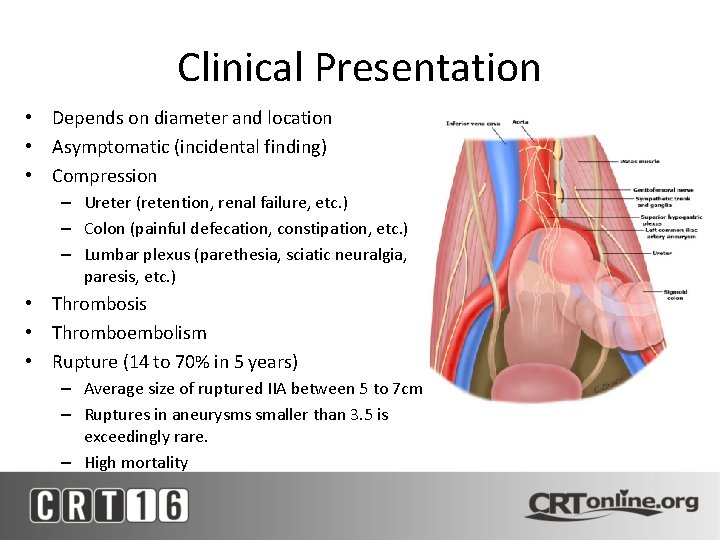
Clinical Presentation • Depends on diameter and location • Asymptomatic (incidental finding) • Compression – Ureter (retention, renal failure, etc. ) – Colon (painful defecation, constipation, etc. ) – Lumbar plexus (parethesia, sciatic neuralgia, paresis, etc. ) • Thrombosis • Thromboembolism • Rupture (14 to 70% in 5 years) – Average size of ruptured IIA between 5 to 7 cm – Ruptures in aneurysms smaller than 3. 5 is exceedingly rare. – High mortality
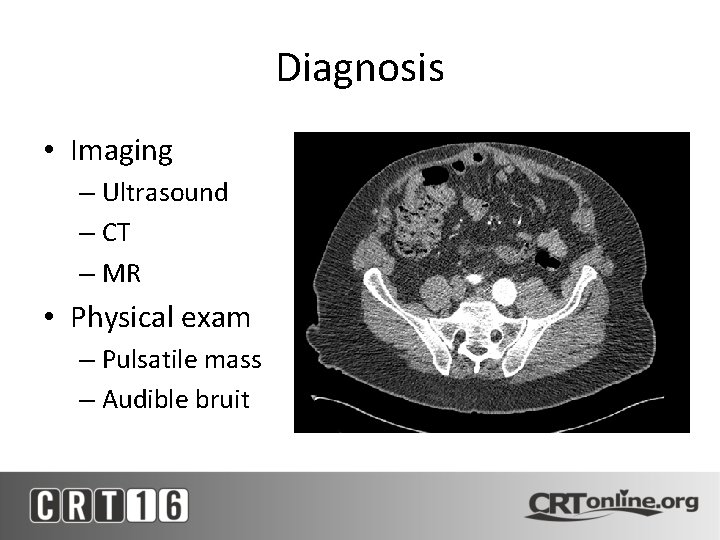
Diagnosis • Imaging – Ultrasound – CT – MR • Physical exam – Pulsatile mass – Audible bruit
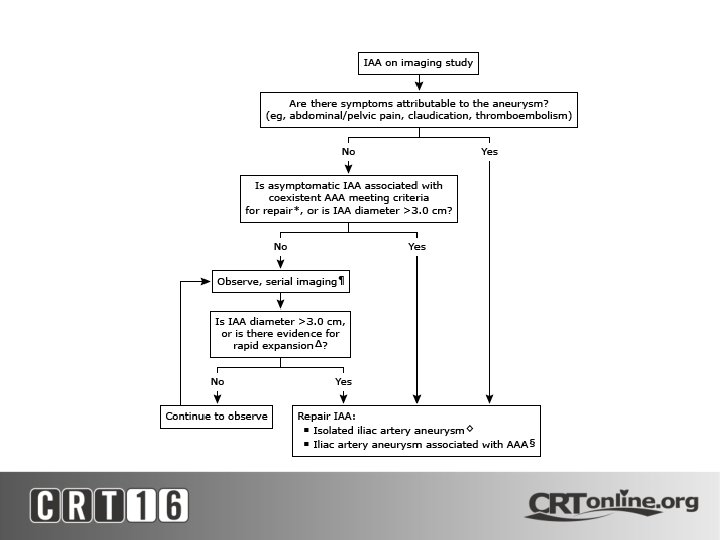
Management • Early diagnosis, careful surveillance of small iliac aneurysms and repair of symptomatic and larger iliac aneurysms reduces the morbidity and mortality associated with IAA. • Multiple studies have found that mortality ranges from 20 to 55 percent for emergent repair of IAA compared with about 1 percent for elective repair • Medical management of risk factor modification Desiron Q, Detry O, Sakalihasan N, et al. Isolated atherosclerotic aneurysms of the iliac arteries. Ann Vasc Surg 1995; 9 Suppl: S 62.
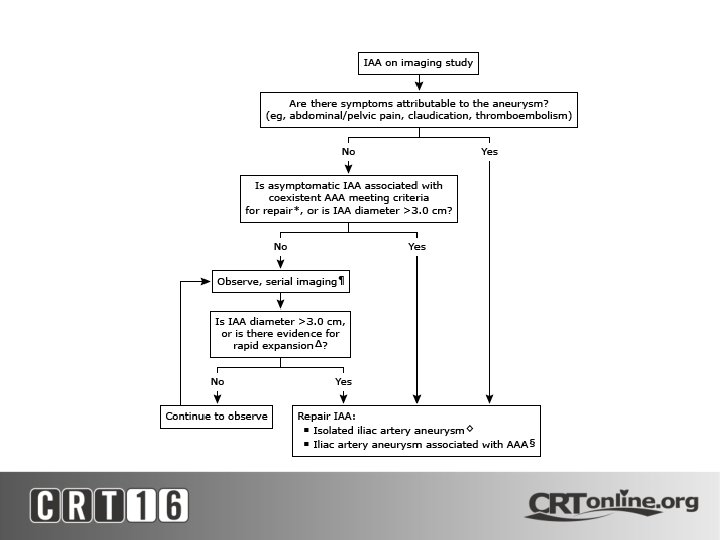
Indications for Repair • Ruptured IAA – Ruptured IAA is a surgical emergency and repair should be performed without delay. • Symptomatic IAA – Patients who present with symptoms generally have larger aneurysms that are at a high risk for rupture and IAA should be repaired urgently. • Rapidly expanding IAA – Rapidly expanding IAA (≥ 7 mm in six months or >1 cm in one year). • Asymptomatic IAA ≥ 3. 0 cm. • Coexistent AAA repair – Patients with AAA associated with common iliac arteries ≥ 2. 5 cm are treated by using a bifurcated graft rather than a tube graft. In association with endovascular aneurysm repair of AAA, common iliac aneurysms of any size are treated to obtain an adequate distal seal zone
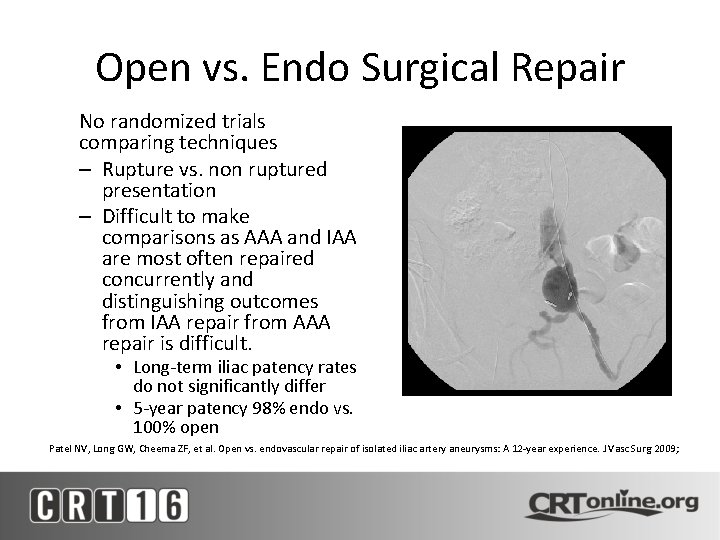
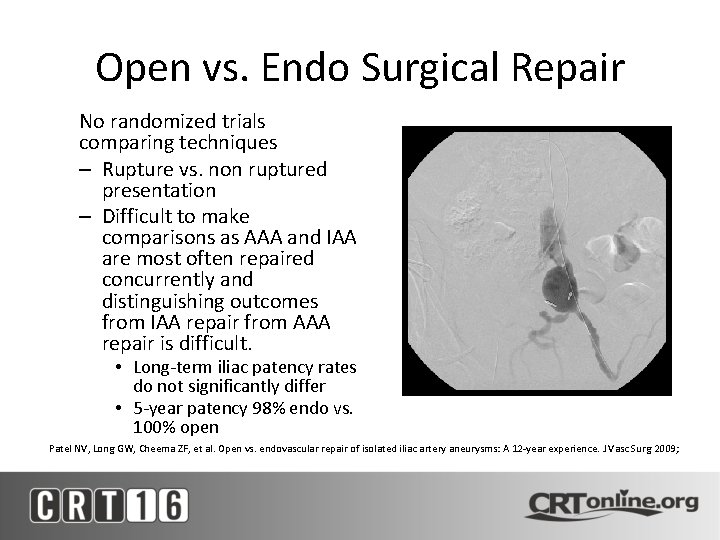
Open vs. Endo Surgical Repair No randomized trials comparing techniques – Rupture vs. non ruptured presentation – Difficult to make comparisons as AAA and IAA are most often repaired concurrently and distinguishing outcomes from IAA repair from AAA repair is difficult. • Long-term iliac patency rates do not significantly differ • 5 -year patency 98% endo vs. 100% open Patel NV, Long GW, Cheema ZF, et al. Open vs. endovascular repair of isolated iliac artery aneurysms: A 12 -year experience. J Vasc Surg 2009;
Open vs. Endo Surgical Repair • Endovascular repair is associated with significantly decreased morbidity • Advantages include: – Elimination of the complications associated with pelvic dissection such as: • Damage to sympathetic and parasympathetic nerves, resulting in erectile dysfunction or retrograde ejaculation • Disruption of lymphatic channels, resulting in lymphatic leak – Avoidance of open surgery in patients with prior abdominal or pelvic surgery – Reduction of perioperative morbidity, thus allowing the treatment of patients at high-risk for open surgery 1, 2 1 Huang Y, Gloviczki P, Duncan AA, et al. Common iliac artery aneurysm: expansion rate and results of open surgical and endovascular repair. J Vasc Surg. 2008; 47: 1203 -1211. GA, Nassef AH, Antoniou SA, et al. Endovascular treatment of isolated internal iliac artery aneurysms. Vascular. 2011; 19: 291 -300. 2 Antoniou
CIA Aneurysm Repair: Open • Bilateral CIA or with AAA managed with aortobiiliac or aorto-bifemoral bypass • Interposition grafting of the CIA – Maintains collateral flow to the pelvis and IMA • Large CIA associated with compressive symptoms should be opened and repaired directly
IIA Aneurysm Repair: Open • Interposition grafting of the IIA – Maintains antegrade flow to the pelvis – Ligation has advantage of limited pelvic dissection – However, sac may fail to decompress due to retrograde filling through collateral branches – Must individually ligate
Open vs. Endo Surgical Repair • Endovascular repair is indicated when anatomy is suitable and compressive symptoms are absent. – Endovascular repair will not lead to immediate decompression
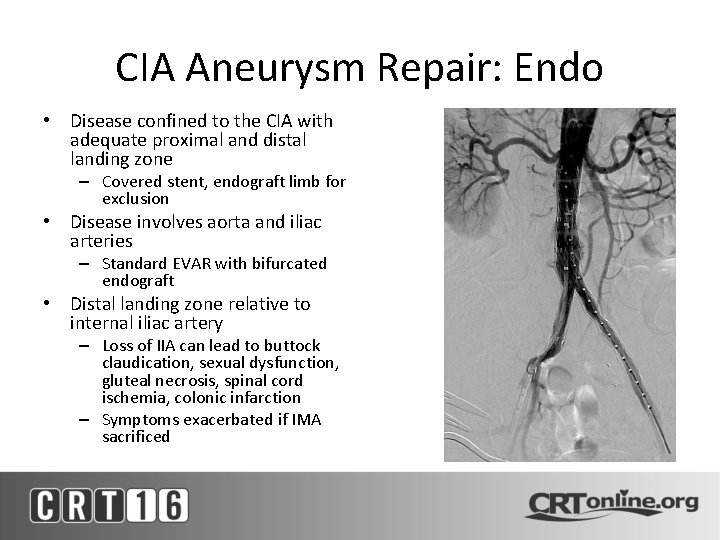
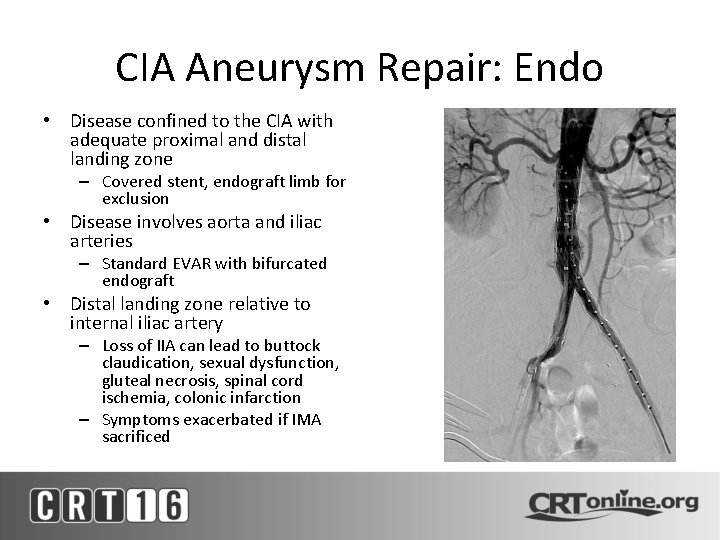
CIA Aneurysm Repair: Endo • Disease confined to the CIA with adequate proximal and distal landing zone – Covered stent, endograft limb for exclusion • Disease involves aorta and iliac arteries – Standard EVAR with bifurcated endograft • Distal landing zone relative to internal iliac artery – Loss of IIA can lead to buttock claudication, sexual dysfunction, gluteal necrosis, spinal cord ischemia, colonic infarction – Symptoms exacerbated if IMA sacrificed
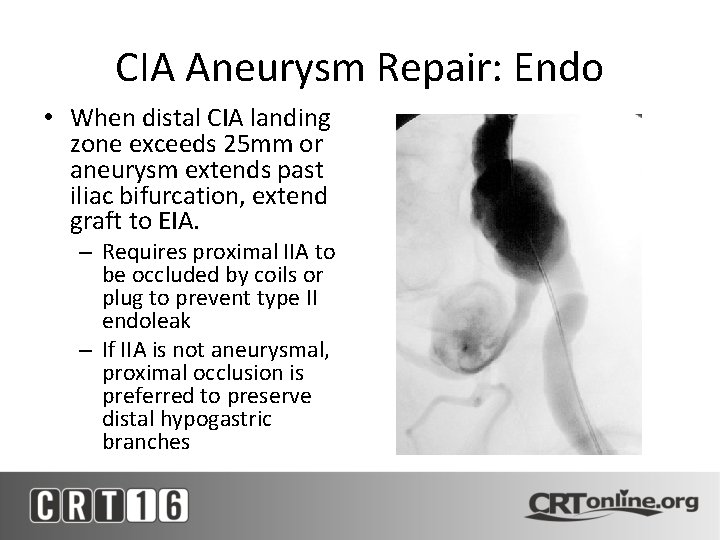
CIA Aneurysm Repair: Endo • When distal CIA landing zone exceeds 25 mm or aneurysm extends past iliac bifurcation, extend graft to EIA. – Requires proximal IIA to be occluded by coils or plug to prevent type II endoleak – If IIA is not aneurysmal, proximal occlusion is preferred to preserve distal hypogastric branches
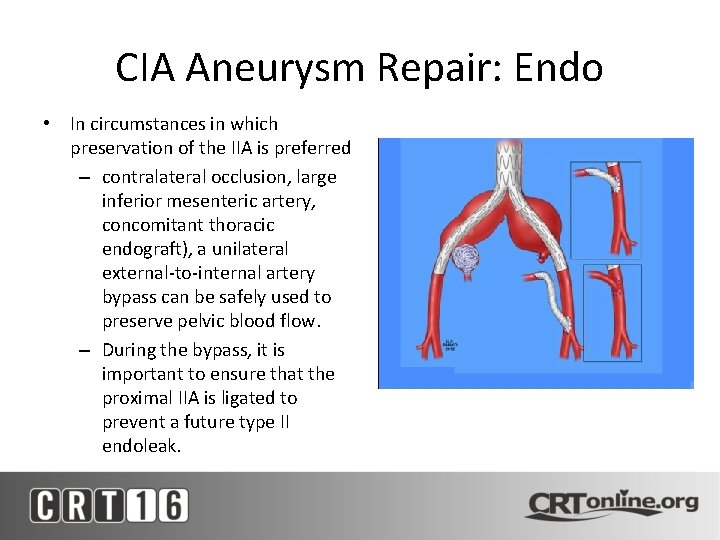
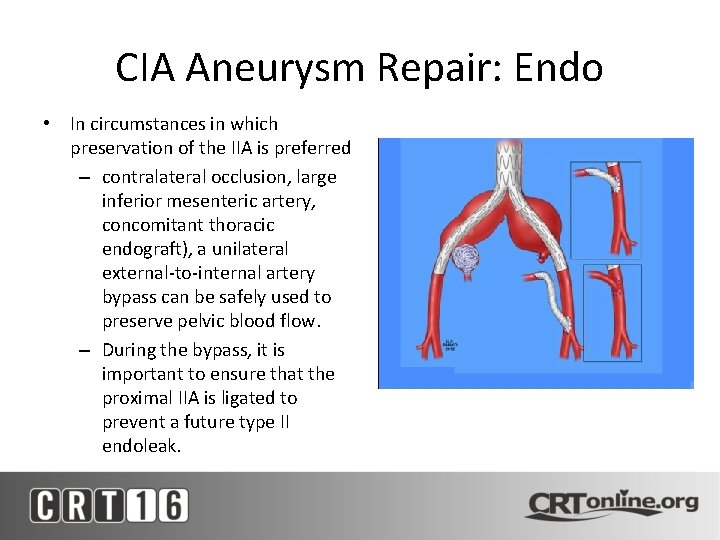
CIA Aneurysm Repair: Endo • In circumstances in which preservation of the IIA is preferred – contralateral occlusion, large inferior mesenteric artery, concomitant thoracic endograft), a unilateral external-to-internal artery bypass can be safely used to preserve pelvic blood flow. – During the bypass, it is important to ensure that the proximal IIA is ligated to prevent a future type II endoleak.
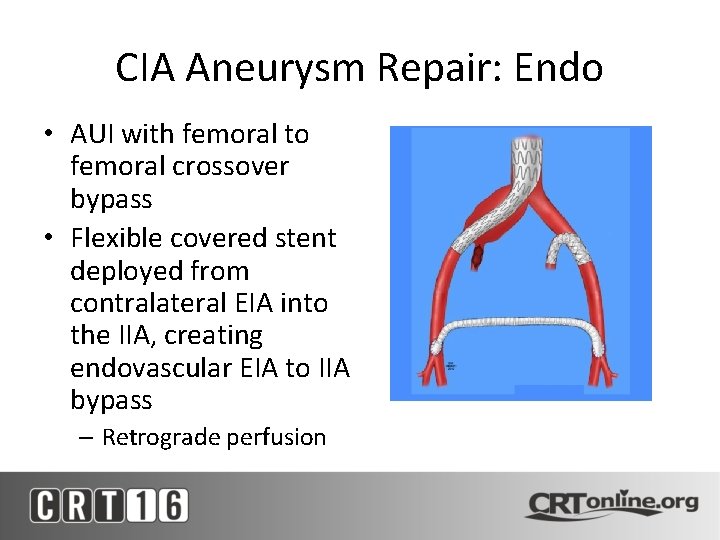
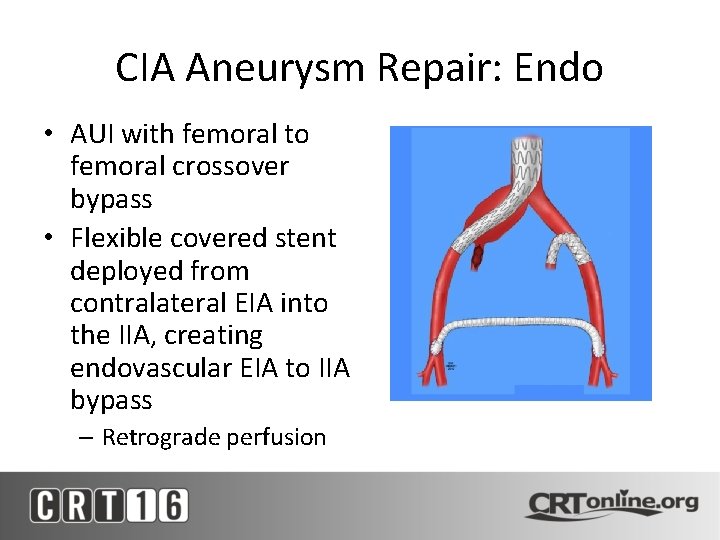
CIA Aneurysm Repair: Endo • AUI with femoral to femoral crossover bypass • Flexible covered stent deployed from contralateral EIA into the IIA, creating endovascular EIA to IIA bypass – Retrograde perfusion
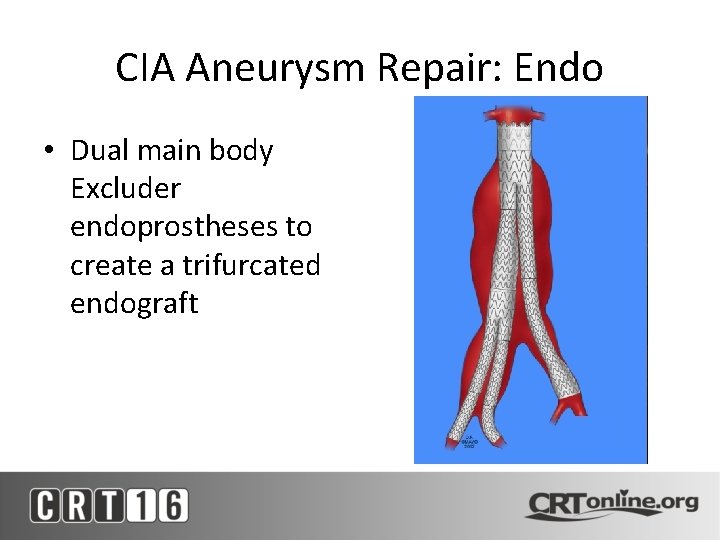
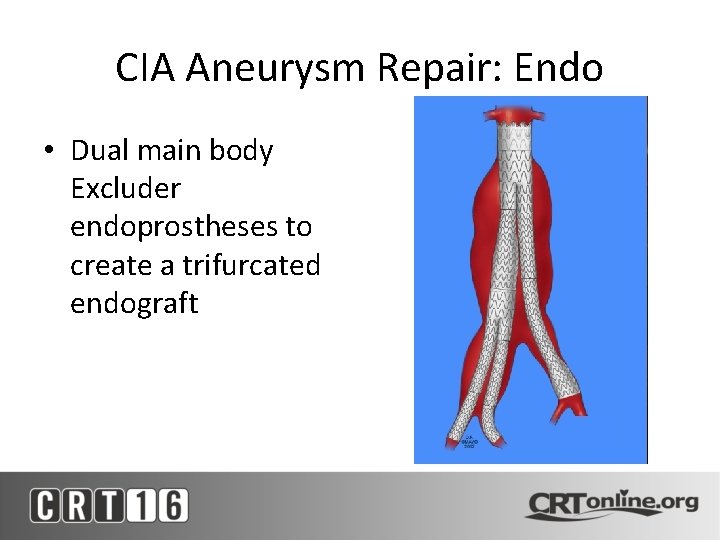
CIA Aneurysm Repair: Endo • Dual main body Excluder endoprostheses to create a trifurcated endograft
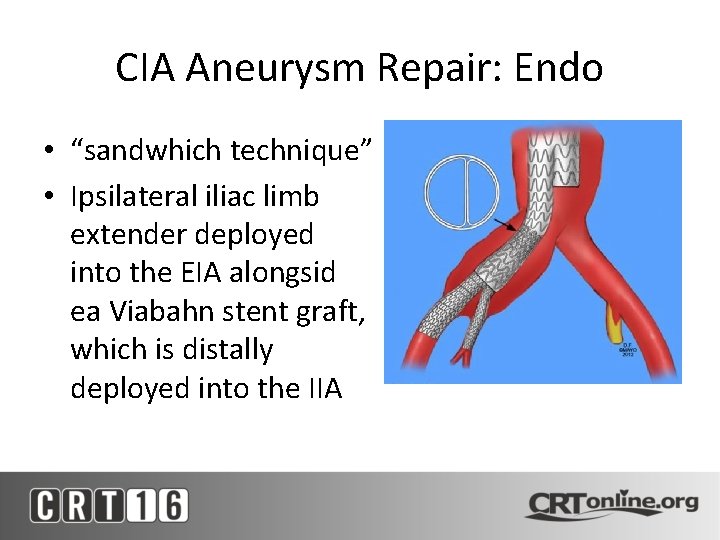
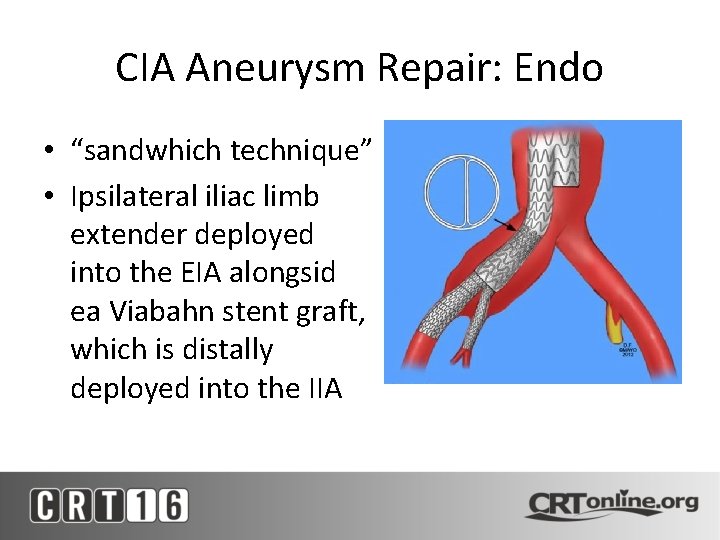
CIA Aneurysm Repair: Endo • “sandwhich technique” • Ipsilateral iliac limb extender deployed into the EIA alongsid ea Viabahn stent graft, which is distally deployed into the IIA
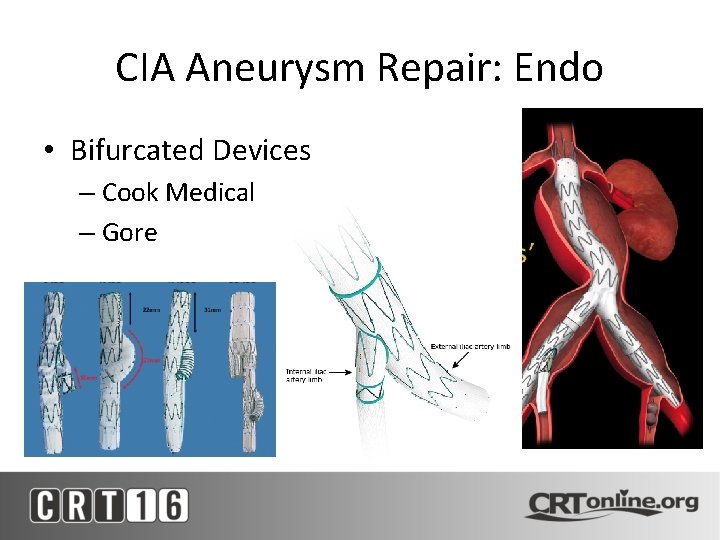
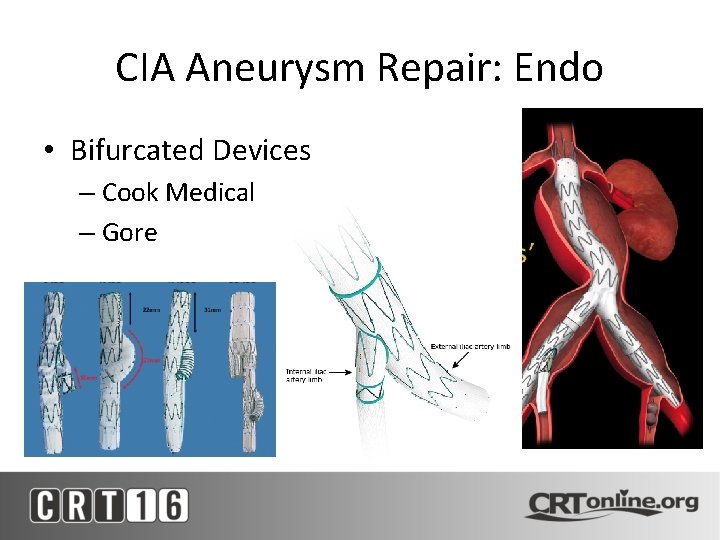
CIA Aneurysm Repair: Endo • Bifurcated Devices – Cook Medical – Gore
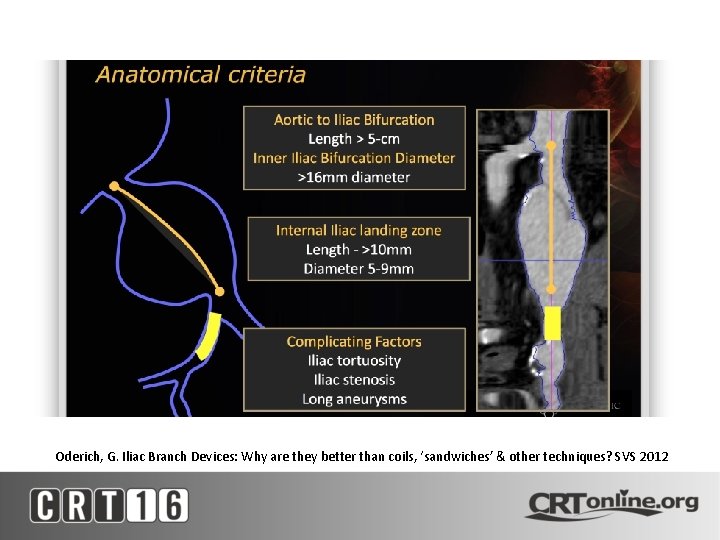
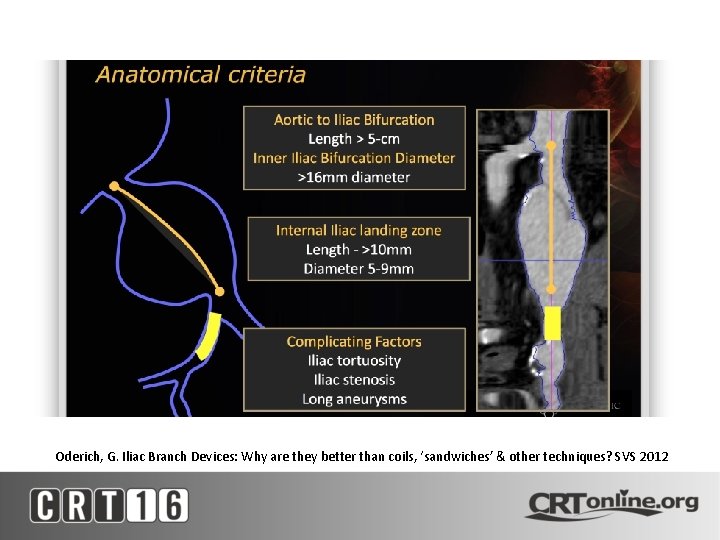
Oderich, G. Iliac Branch Devices: Why are they better than coils, ‘sandwiches’ & other techniques? SVS 2012
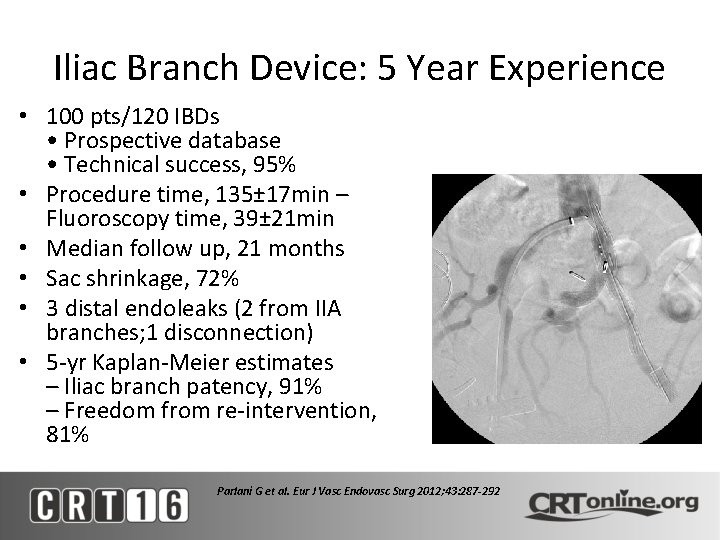
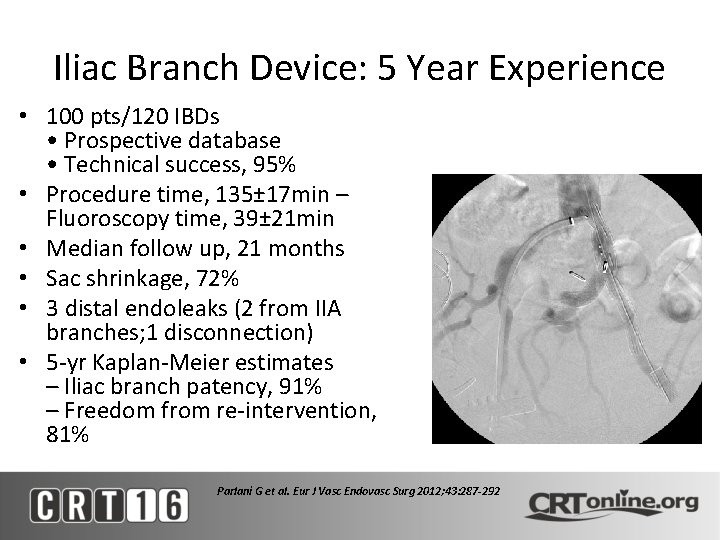
Iliac Branch Device: 5 Year Experience • 100 pts/120 IBDs • Prospective database • Technical success, 95% • Procedure time, 135± 17 min – Fluoroscopy time, 39± 21 min • Median follow up, 21 months • Sac shrinkage, 72% • 3 distal endoleaks (2 from IIA branches; 1 disconnection) • 5 -yr Kaplan-Meier estimates – Iliac branch patency, 91% – Freedom from re-intervention, 81% Parlani G et al. Eur J Vasc Endovasc Surg 2012; 43: 287 -292
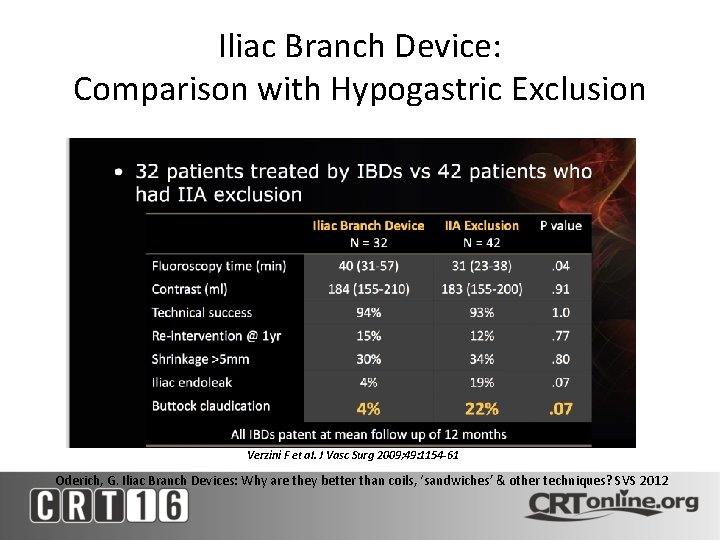
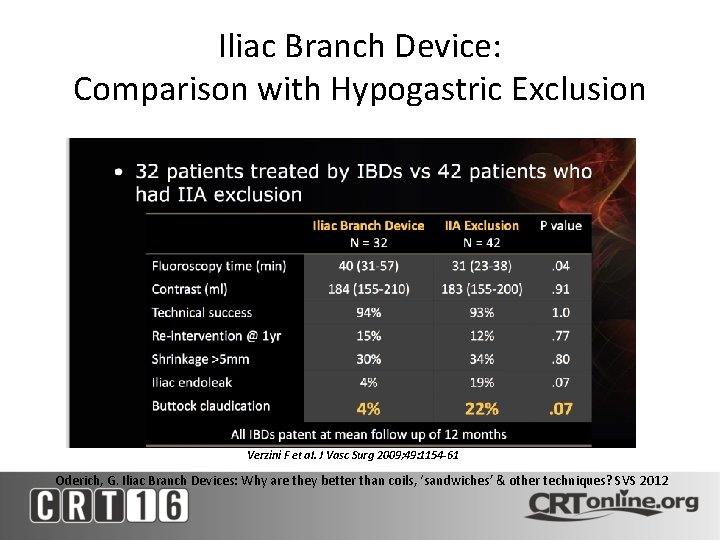
Iliac Branch Device: Comparison with Hypogastric Exclusion Verzini F et al. J Vasc Surg 2009; 49: 1154 -61 Oderich, G. Iliac Branch Devices: Why are they better than coils, ‘sandwiches’ & other techniques? SVS 2012
CIA Aneurysm Repair: Endo • IIA Aneurysms – Ability to preserve IIA flow is greatly reduced in the setting of IIA aneurysms – Challenging because of limited proximal and distal landing zones – Most often coil embolized or plugged
Complications • Open repair – Extremity ischemia – Distal embolization – Cardiac and pulmonary morbidity – Pelvic ischemia • Endo repair – Endoleak – Graft kinking – Pelvic ischemia
Conclusions • Majority of iliac aneurysms can be treated with endovascular techniques • Preservation of hypogastric arteries can be accomplished through various techniques
 Anterior epigastric artery
Anterior epigastric artery Internal iliac artery mnemonic
Internal iliac artery mnemonic Subscapular vein cat
Subscapular vein cat Branches off aortic arch
Branches off aortic arch How do we treat the life the life how we treat
How do we treat the life the life how we treat Mesenteric artery origin
Mesenteric artery origin Iliac region
Iliac region Iliac tubercle
Iliac tubercle Epigastric vs hypogastric
Epigastric vs hypogastric Shifting dullness
Shifting dullness Iliac stent complications
Iliac stent complications Iliac crest level
Iliac crest level Proximal tibia
Proximal tibia Interior trunk
Interior trunk Outcropping muscles
Outcropping muscles Sonja bone
Sonja bone Muscles of the pelvic girdle
Muscles of the pelvic girdle Posterior tibial artery
Posterior tibial artery Common iliac
Common iliac Superior ramus of the pubis
Superior ramus of the pubis Anterior inferior iliac spine
Anterior inferior iliac spine Falciform fascia
Falciform fascia Who is mr. kirwin and how does he treat victor?
Who is mr. kirwin and how does he treat victor? How did cyrus treat the people he conquered
How did cyrus treat the people he conquered Equation for number needed to treat
Equation for number needed to treat Invitation to treat
Invitation to treat How does juliet treat paris
How does juliet treat paris Which seedless plants have been used to treat bee stings
Which seedless plants have been used to treat bee stings Number needed to treat calculation
Number needed to treat calculation Offer
Offer