https www yenepoya edu in 11242020 3 55

- Slides: 47

https: //www. yenepoya. edu. in 11/24/2020 3: 55 PM Yenepoya Nursing College (NAME) 1
Unit VI Chronic Renal Failure PRESENTED BY: Ms. Pavithra K Lecturer, MSN dept REVIEWED BY: Mr. Gireesh G R Asso. Professor, MSN dept
LEARNING OBJECTIVES At the end of the class students will be able to • define Chronic renal failure • enlist the causes of Chronic renal failure • Explain the patho- physiology of Chronic renal failure • Enlist the clinical features of Chronic renal failure • enumerate the management of Chronic renal failure
DEFINITION: Chronic renal failure is an irreversible and progressive reduction of functioning renal tissue that is when kidneys are no longer capable of maintaining an internal environment that is consistent with life
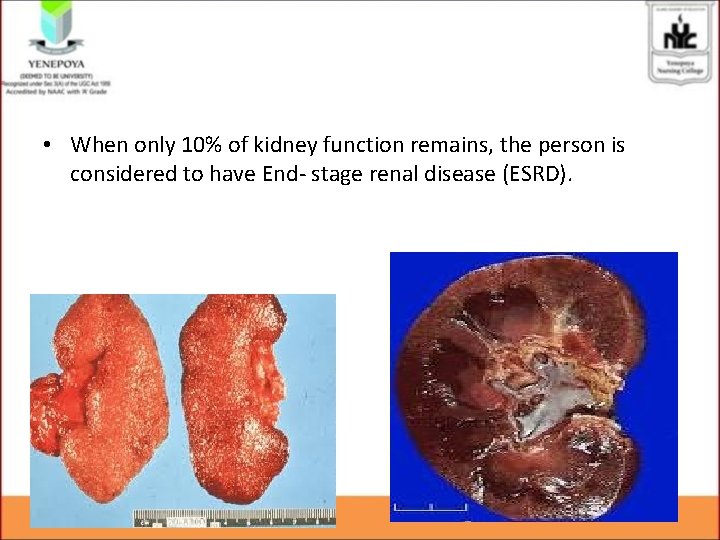
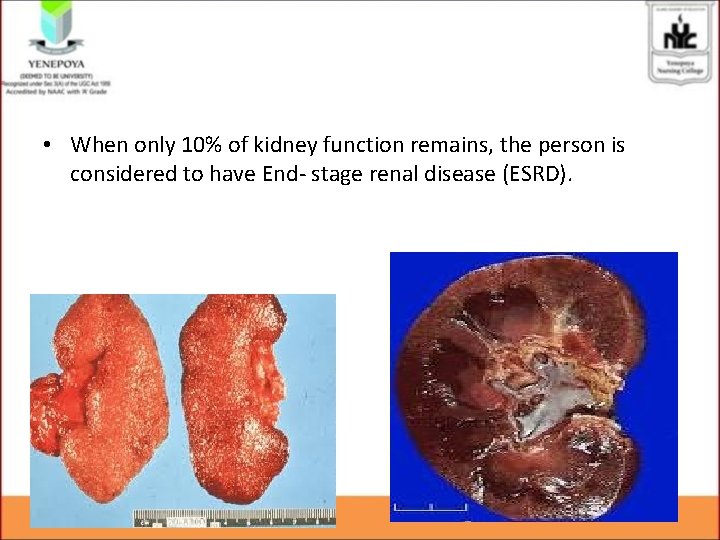
• When only 10% of kidney function remains, the person is considered to have End- stage renal disease (ESRD).
Etiology • Pre-renal cause • Intra renal cause • Post renal cause
Other ETIOLOGY • • AKI Chronic Glomeruloneohritis Polycystic kidney disease Repeated pyelonephritis DM HTN SLE
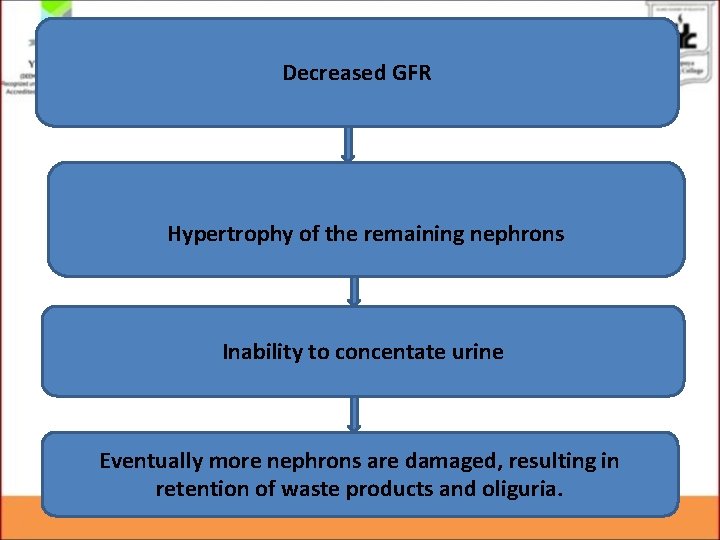
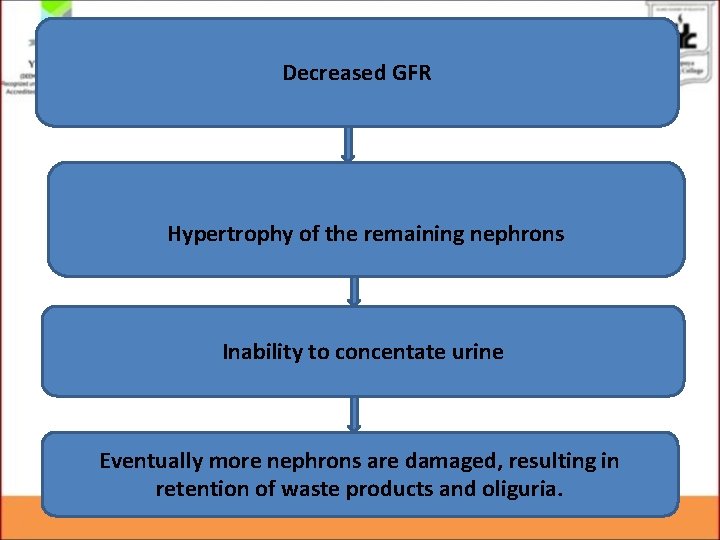
Decreased GFR Hypertrophy of the remaining nephrons Inability to concentate urine Eventually more nephrons are damaged, resulting in retention of waste products and oliguria.
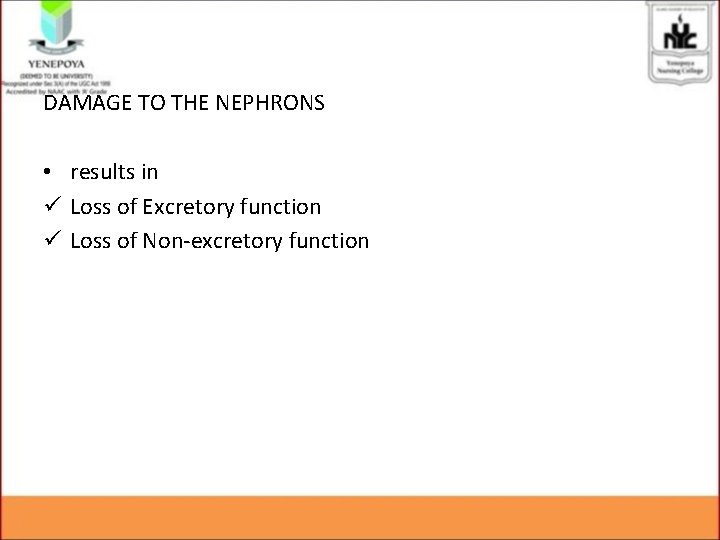
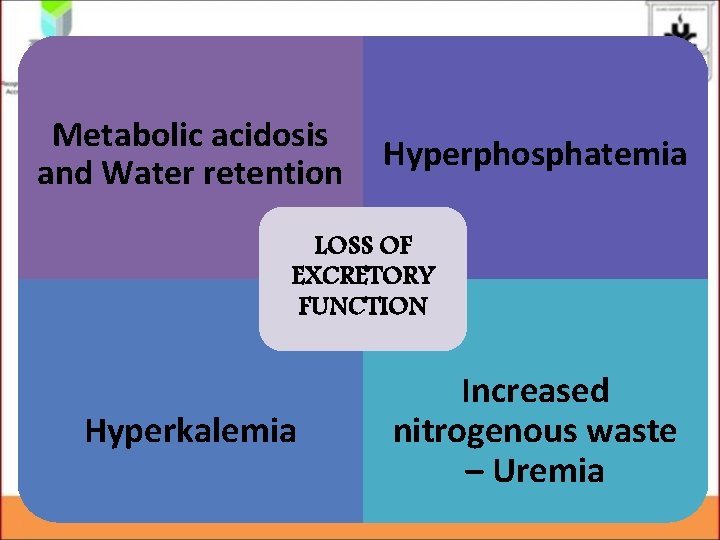
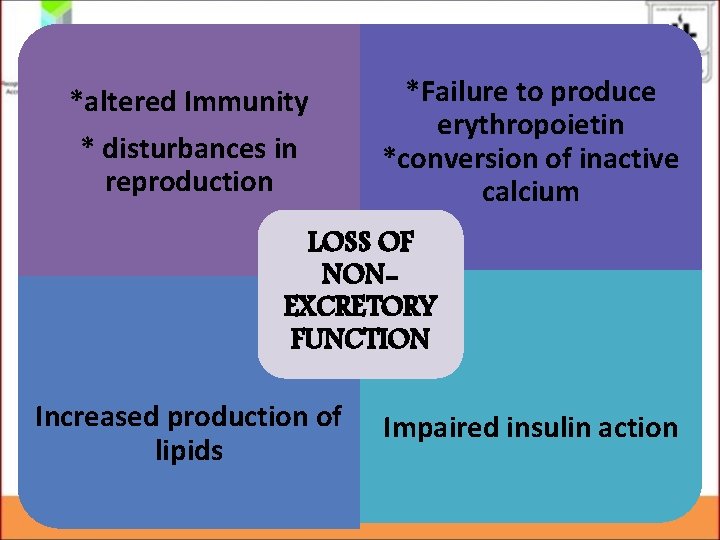
DAMAGE TO THE NEPHRONS • results in ü Loss of Excretory function ü Loss of Non-excretory function
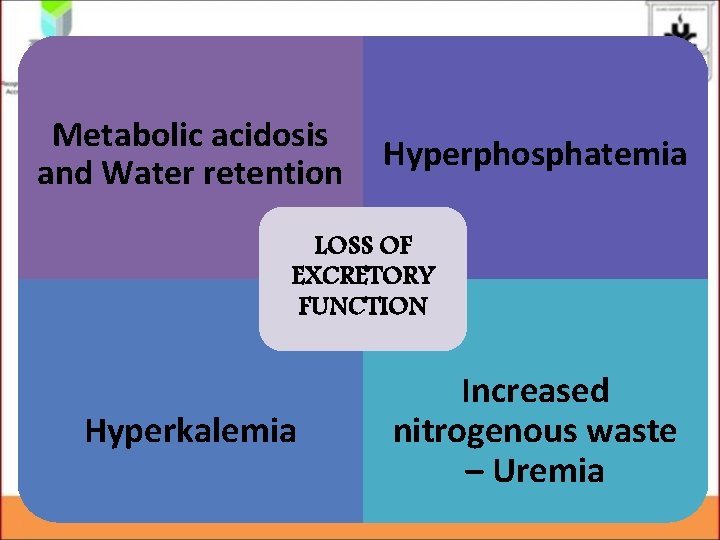
Metabolic acidosis and Water retention Hyperphosphatemia LOSS OF EXCRETORY FUNCTION Hyperkalemia Increased nitrogenous waste – Uremia
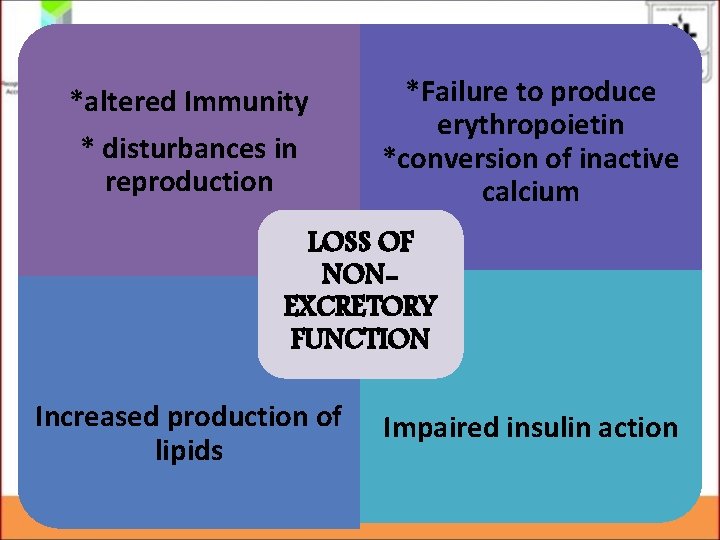
*altered Immunity * disturbances in reproduction *Failure to produce erythropoietin *conversion of inactive calcium LOSS OF NONEXCRETORY FUNCTION Increased production of lipids Impaired insulin action
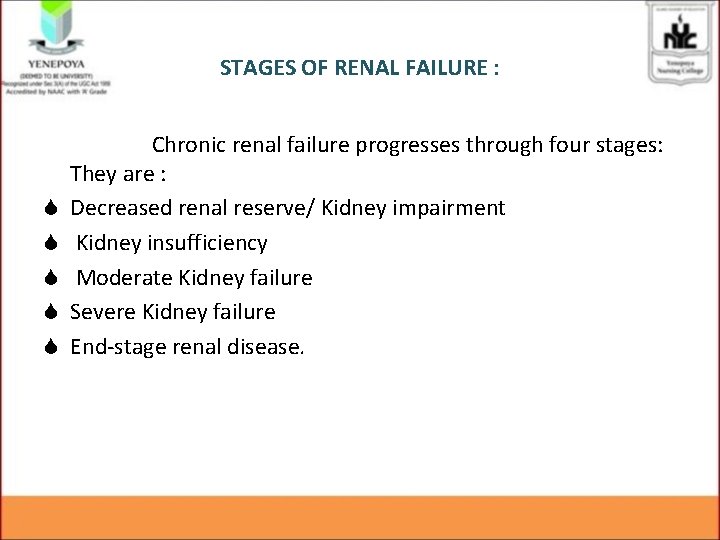
STAGES OF RENAL FAILURE : S S S Chronic renal failure progresses through four stages: They are : Decreased renal reserve/ Kidney impairment Kidney insufficiency Moderate Kidney failure Severe Kidney failure End-stage renal disease.
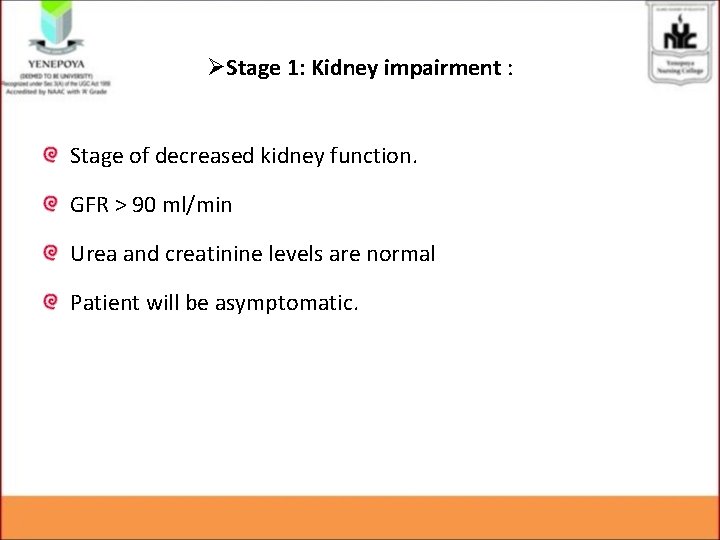
ØStage 1: Kidney impairment : Stage of decreased kidney function. GFR > 90 ml/min Urea and creatinine levels are normal Patient will be asymptomatic.
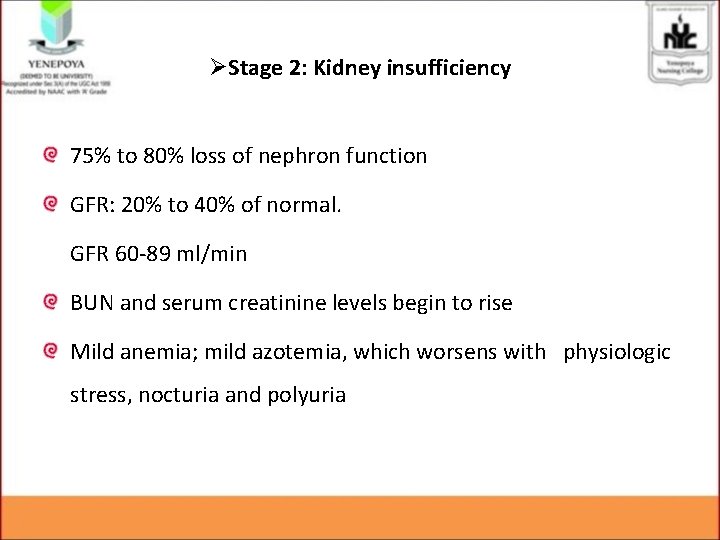
ØStage 2: Kidney insufficiency 75% to 80% loss of nephron function GFR: 20% to 40% of normal. GFR 60 -89 ml/min BUN and serum creatinine levels begin to rise Mild anemia; mild azotemia, which worsens with physiologic stress, nocturia and polyuria
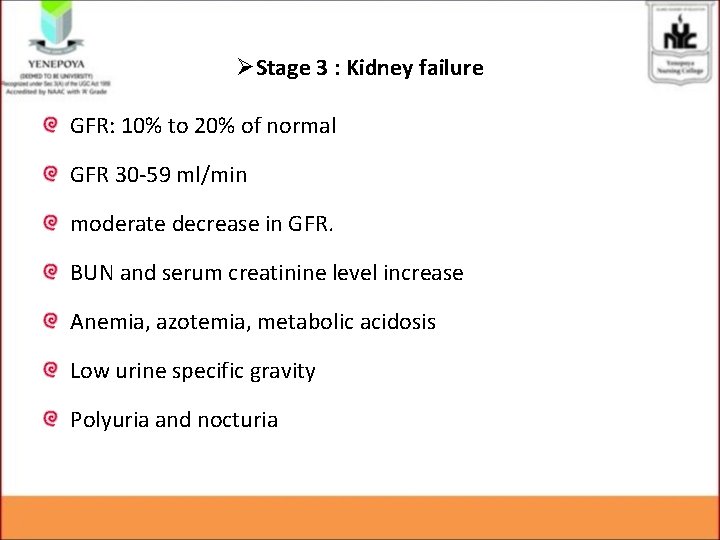
ØStage 3 : Kidney failure GFR: 10% to 20% of normal GFR 30 -59 ml/min moderate decrease in GFR. BUN and serum creatinine level increase Anemia, azotemia, metabolic acidosis Low urine specific gravity Polyuria and nocturia
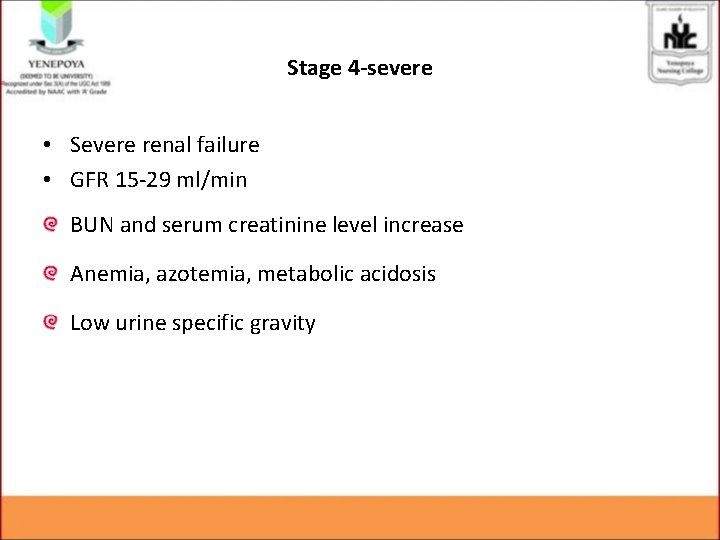
Stage 4 -severe • Severe renal failure • GFR 15 -29 ml/min BUN and serum creatinine level increase Anemia, azotemia, metabolic acidosis Low urine specific gravity
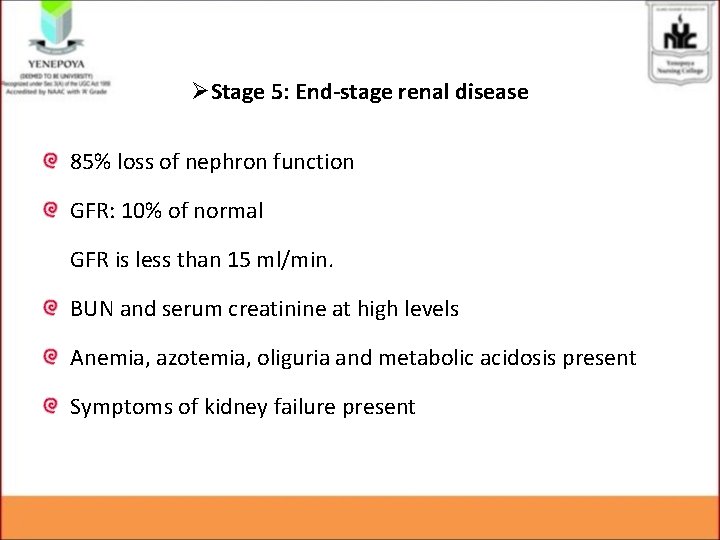
ØStage 5: End-stage renal disease 85% loss of nephron function GFR: 10% of normal GFR is less than 15 ml/min. BUN and serum creatinine at high levels Anemia, azotemia, oliguria and metabolic acidosis present Symptoms of kidney failure present
CLINICAL MANIFESTATIONS Ø As nephron destruction progresses to ESRD, the manifestations are described as Uremic syndrome.
1. URINARY SYSTEM • polyuria results from the inability of the kidneys to concentrate urine • Nocturia • The specific gravity of urine gradually becomes low • As CKD worsens, oliguria develops and eventually anuria (urine output<40 ml per 24 hours) develops
2. METABOLIC DISTURBANCES : Ø Waste product accumulation Ø Elevated triglycerides
3. ELECTROLYTE AND ACID BASE IMBALANCES : Ø Ø Ø Potassium -high Sodium -hypo Calcium-hypo phosphate-hyper Metabolic acidosis
4. HEMATOLOGIC SYSTEM : Ø Anemia Ø Infection
5. CARDIOVASCULAR SYSTEM : Ø Ø hypertension, left ventricular hypertrophy congestive heart failure. Cardiac arrhythmias
6. RESPIRATORY SYSTEM : Ø Ø kussumaul respiration Dypnoea pulmonary edema pneumonitis.
7. GASTROINTESTINAL SYSTEM : Ø Mucosal Ø Stomatitis Ø malnutrition.
9. MUSCULOSKELETAL SYSTEM : • kidney fails to activate vitamin D, calcium absorption is impaired and serum calcium decreases. • Renal osteodystrophy is a bone disease that occurs when kidneys fails to maintain proper levels of calcium and phosphorus in the blood • it includes Osteomalacia and Osteitis fibrosa.
8. NEUROLOGIC SYSTEM : Ø This occur as a result of increased nitrogenous waste products, electrolyte imbalances, metabolic acidosis Ø Seizures and coma Ø Peripheral neuropathy Ø Muscular weakness
10. INTEGUMENTARY SYSTEM : Ø yellow-gray discoloration of the skin. This change is a result of the absorption and retention of urinary pigments. Ø The skin appears pale and is dry and scaly
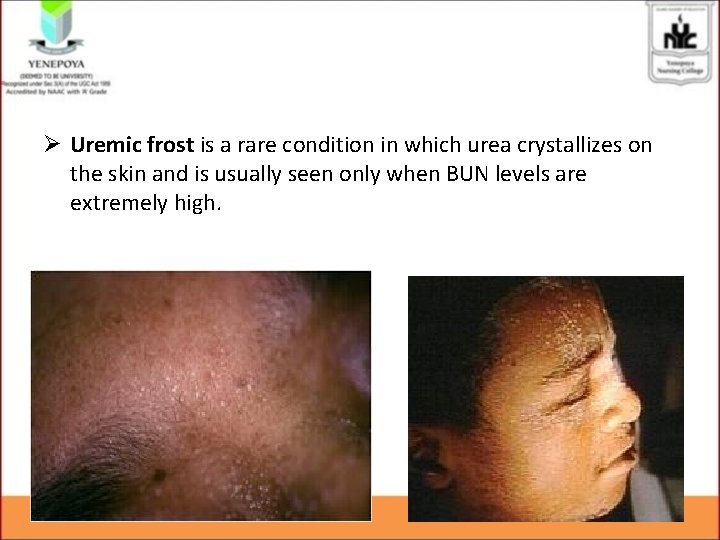
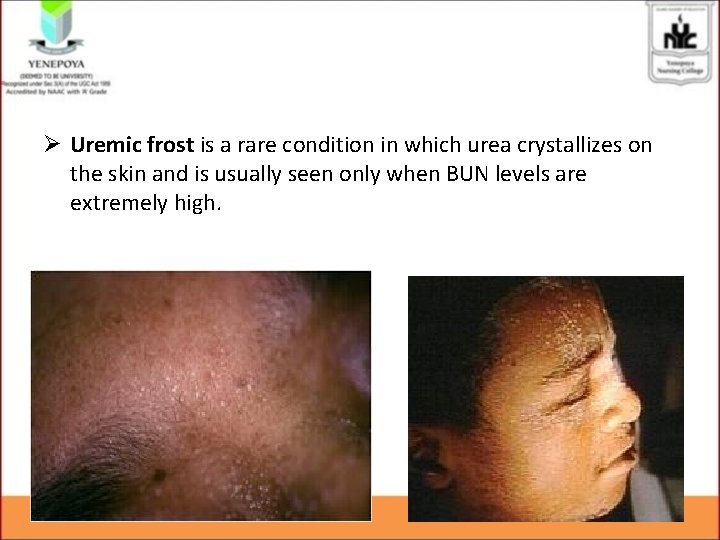
Ø Uremic frost is a rare condition in which urea crystallizes on the skin and is usually seen only when BUN levels are extremely high.
12. ENDOCRINE SYSTEM : Ø hypothyroidism. 13. PSYCHOLOGICAL CHANGES : Ø behavioural changes, Ø withdrawal Ø depression
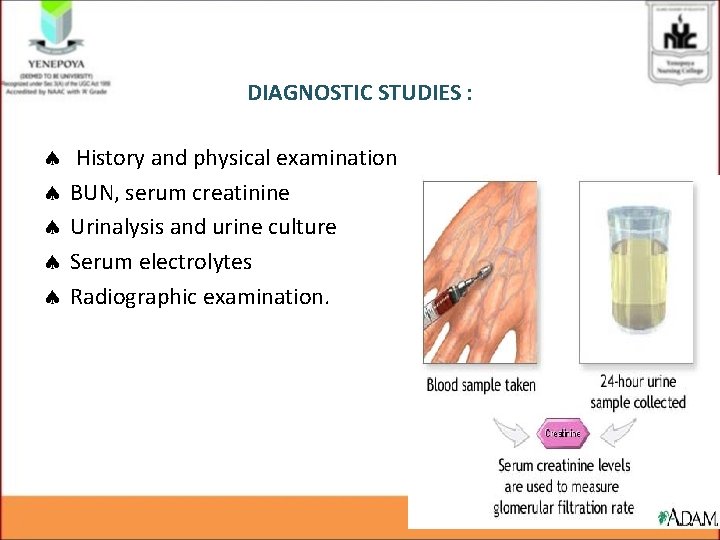
DIAGNOSTIC STUDIES : History and physical examination BUN, serum creatinine Urinalysis and urine culture Serum electrolytes Radiographic examination.
MANAGEMENT : The main goals • To preserve renal function • To delay the need for dialysis or transplantation as long as feasible. • To alleviate extra-renal manifestations as much as possible. • To improve blood chemistry values. • To provide an optimal quality of life
• Medical management : It can be accomplished by controlling the disease process by • Controlling the blood pressure • Reducing the dietary protein intake
1. • • Hypertension : sodium and fluid restriction Fluid intake restriction, - urine output + 500 ml. Administration of antihypertensive drugs- Multiple drugs The antihypertensive drugs most commonly used are – diuretics (e. g. furosemide), – ß- adrenergic blockers (e. g. metaprolol), – calcium channel blockers(e. g. nifedipine) – ACE inhibitors(e. g. captopril)
2. Protein restriction • the daily intake of Protein diet 0. 5 -0. 6 gm/kg body weight without dialysis. • Once the patient starts with dialysis, 1. 2 to 1. 3 g/kg per day. • carbohydrate -50 Kcal/Kg/day.
• Anemia : • The recombinant form of human erythropoietin, helps in regulating the erythropoietic factor. • It is administered SC or IV , 3 times in a week, in a calculated dose of 50 unit/kg body weight.
• • • Parenteral iron (Venofer) Supplemental folic acid (1 mg daily) is usually given Renal osteodystrophy : calcium carbonate and calcium acetate Oral preparation such as calcitriol Sevelamer (Renagel) is a new phosphate binder.
• Gastrointestinal disturbances : • The smell and taste of ammonia resulting from urea breakdown • Vinegar mouthwashes • antacids every 2 to 4 hours to decrease GI irritation. • Phosphate restriction : • Phosphate should be limited to approximately 1000 mg a day. • Foods that are high in phosphate include dairy products like milk, ice cream, cheese should be limited.
: • Hyperkalemia : • Decrease the dietary intake of potassium rich foods. • Exchange resins such as sodium polystyrene sulphonate can be given as oral or as retention enema. • In severe situation, hemodialysis is indicated
Metabolic acidosis : Sodium bicarbonate Sodium restriction : Sodium restricted diets vary between 2 to 4 g depending on the degree of edema and hypertension. • Avoiding high sodium foods such as Processed meats, pickled foods, salads etc. • Fluid • •
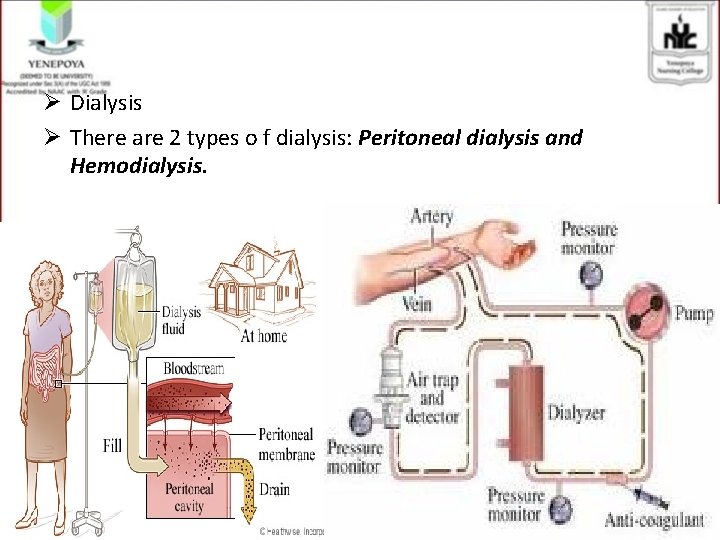
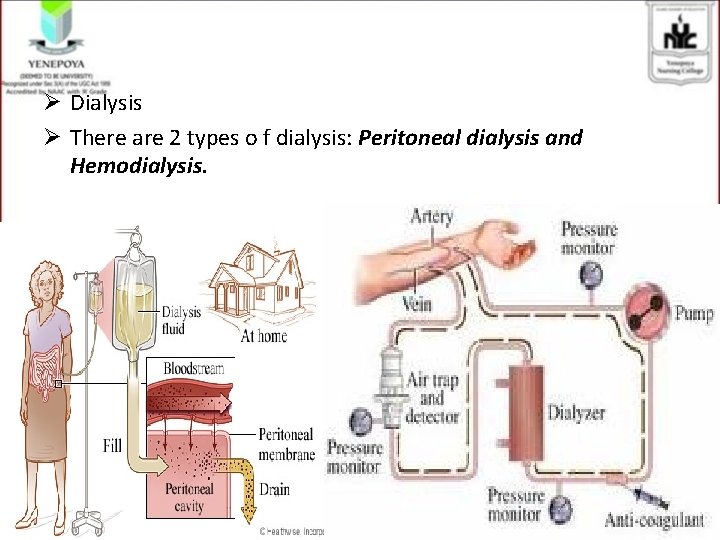
Ø Dialysis Ø There are 2 types o f dialysis: Peritoneal dialysis and Hemodialysis.
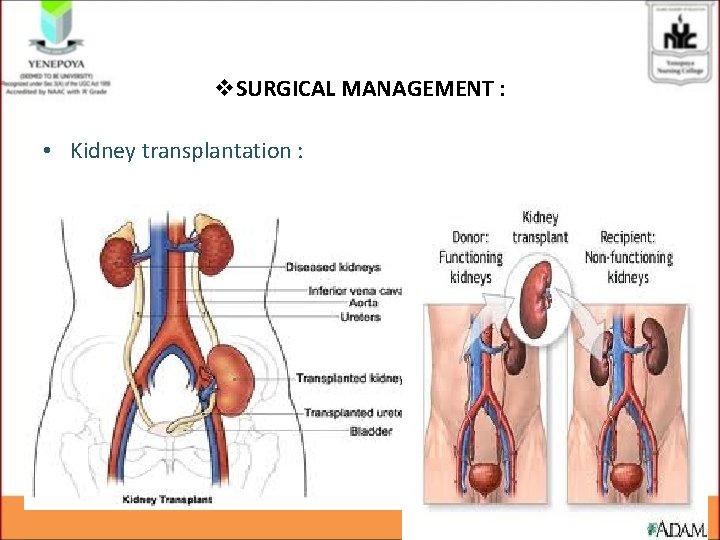
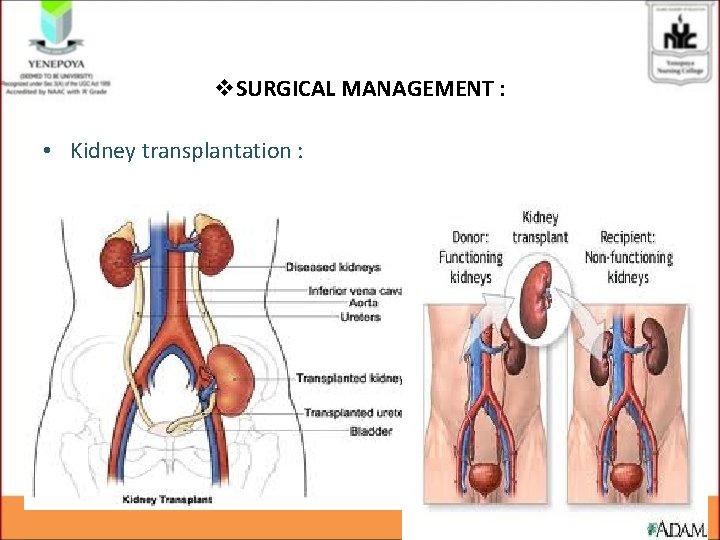
v. SURGICAL MANAGEMENT : • Kidney transplantation :
ü It is the surgical implantation of human kidney from a compatible donor. ü It eliminates the dependence on dialysis ü need for dietary restrictions ü provides the opportunity to return to normal life activities
Nursing assessment: • Assess for the risk factors and etiological factors • Assess for the urine out • Assess for the Kidney function test • Assess for the fluid status • Assess for the electrolyte imbalance
NURSING DIAGNOSIS • Excess fluid volume related to compromised regulatory mechanisms secondary to acute renal failure as evidenced by peripheral edema and weight gain. • Risk for decreased Cardiac Output related to inadequate blood pumped by the heart to meet metabolic demands of the body. (diuretic phase)
Other Nursing Diagnosis. • Risk for arrythmia r/t hyperkalemia as evidenced by reduced renal excretion • Electrolyte imbalance r/t fluid retension as evidenced by edema • Altered nutritional status r/t dietary restriction • Risk for infection r/t compromised immune function
• • • Activity intolerance r/t fatigue and restriction of activities Risk for GI bleeding r/t gastric irritation Risk for altered thought process r/t uraemic syndrome Sleep pattern disturbance r/t anxiety Ineffective individual coping r/t long term , irreversible disease.