History and Fundamentals of Oocyte Maturation in Vitro




- Slides: 22
History and Fundamentals of Oocyte Maturation in Vitro H. I. Nielsen Libya 日本国 H. 2007 I. Nielsen 2007
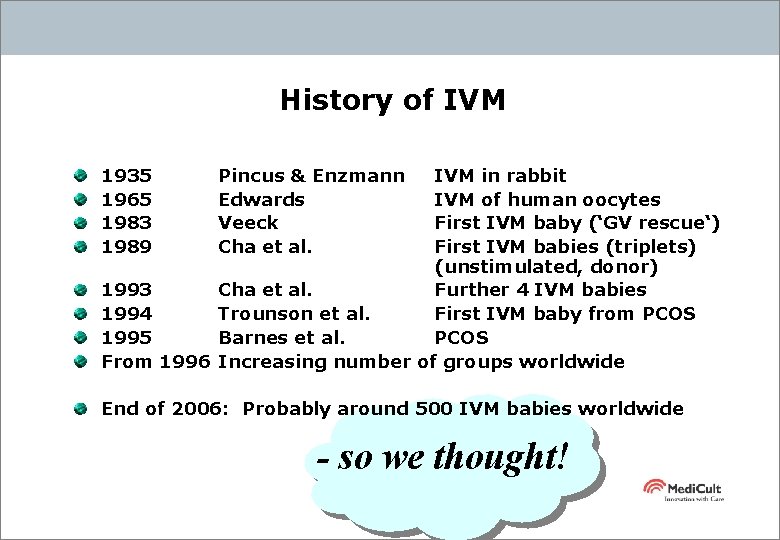
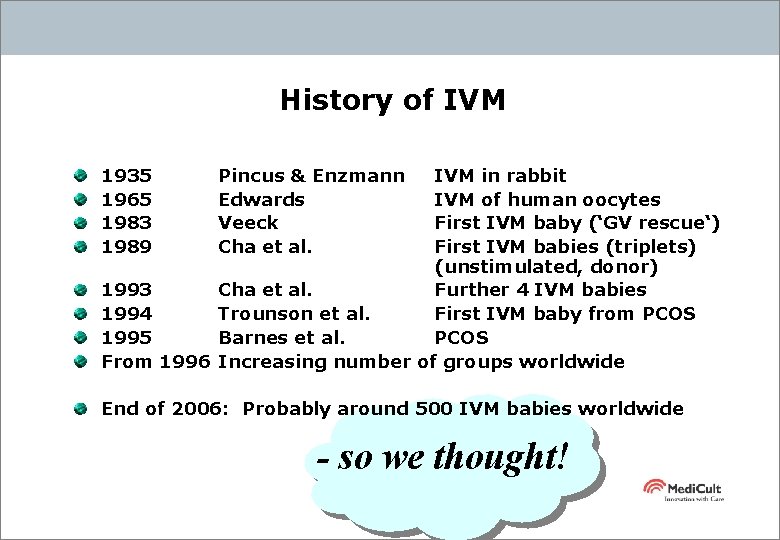
History of IVM 1935 1965 1983 1989 1993 1994 1995 From Pincus & Enzmann Edwards Veeck Cha et al. IVM in rabbit IVM of human oocytes First IVM baby (‘GV rescue‘) First IVM babies (triplets) (unstimulated, donor) Cha et al. Further 4 IVM babies Trounson et al. First IVM baby from PCOS Barnes et al. PCOS 1996 Increasing number of groups worldwide End of 2006: Probably around 500 IVM babies worldwide - so we thought!
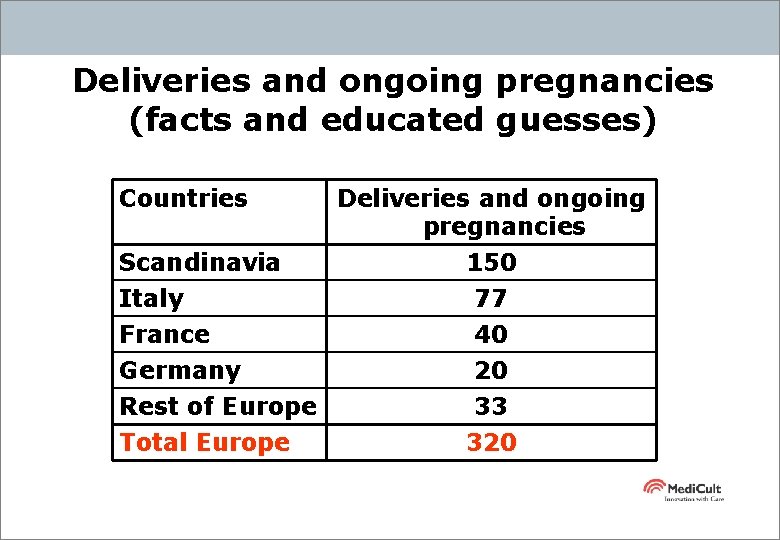
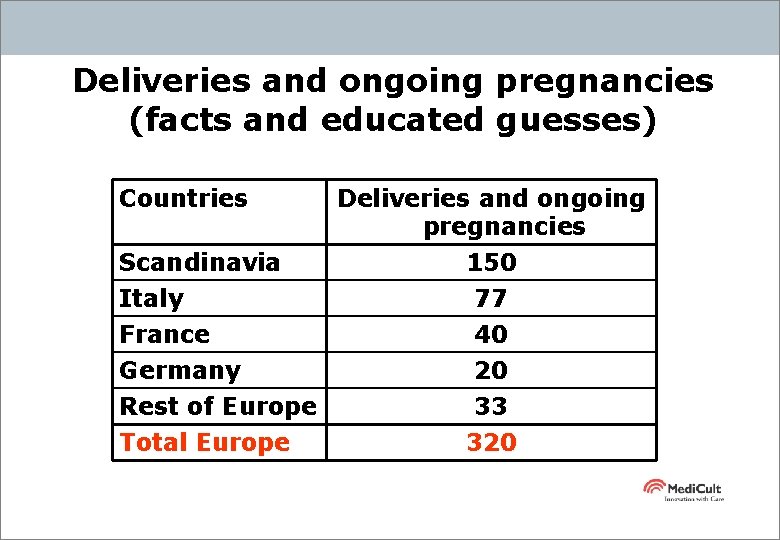
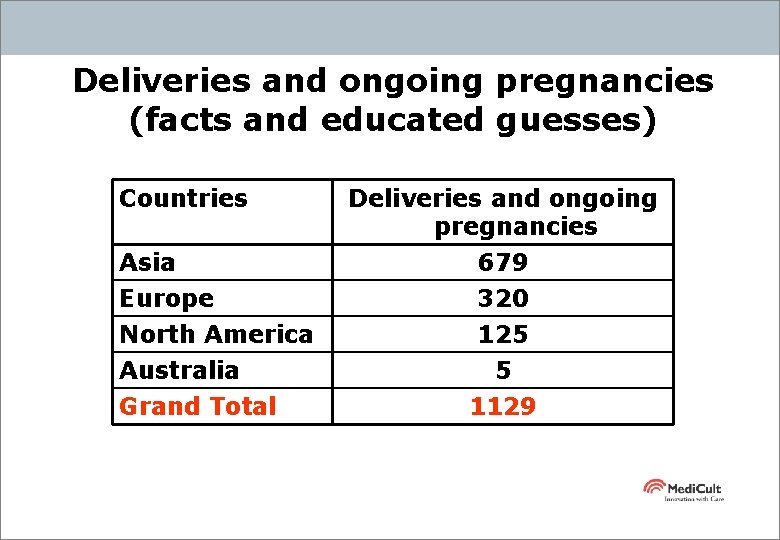
Deliveries and ongoing pregnancies (facts and educated guesses) Countries Deliveries and ongoing pregnancies Scandinavia 150 Italy France Germany Rest of Europe Total Europe 77 40 20 33 320
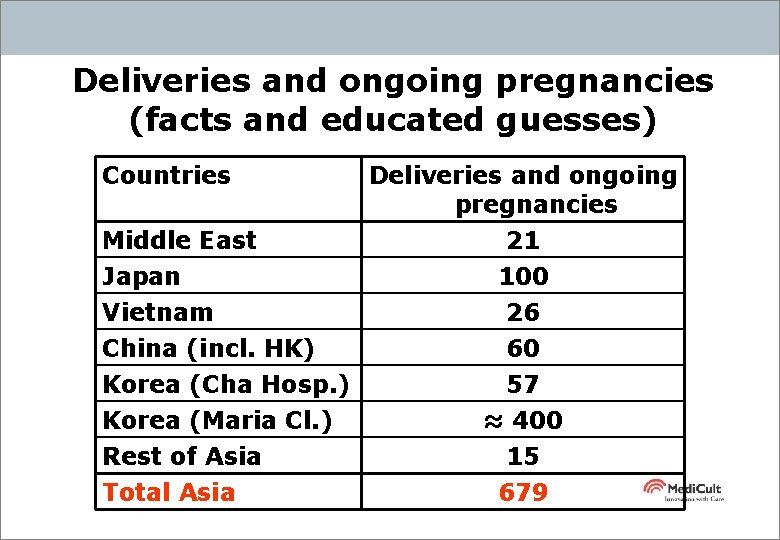
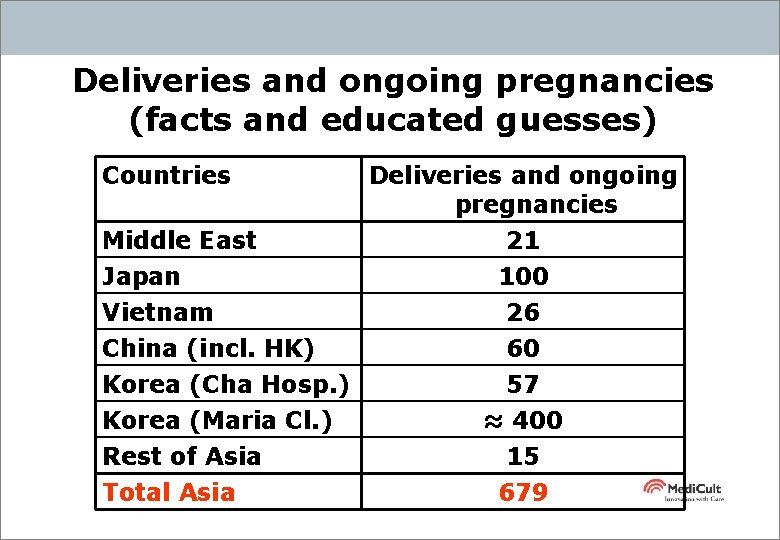
Deliveries and ongoing pregnancies (facts and educated guesses) Countries Middle East Japan Vietnam China (incl. HK) Korea (Cha Hosp. ) Korea (Maria Cl. ) Rest of Asia Total Asia Deliveries and ongoing pregnancies 21 100 26 60 57 ≈ 400 15 679
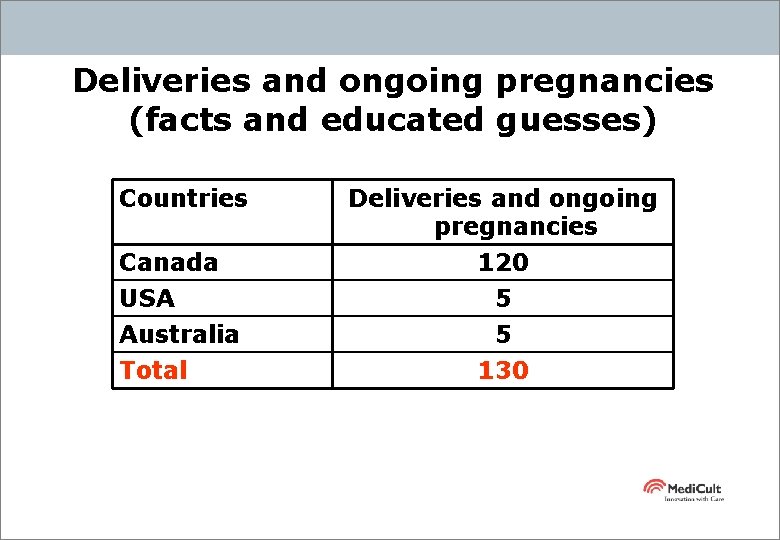
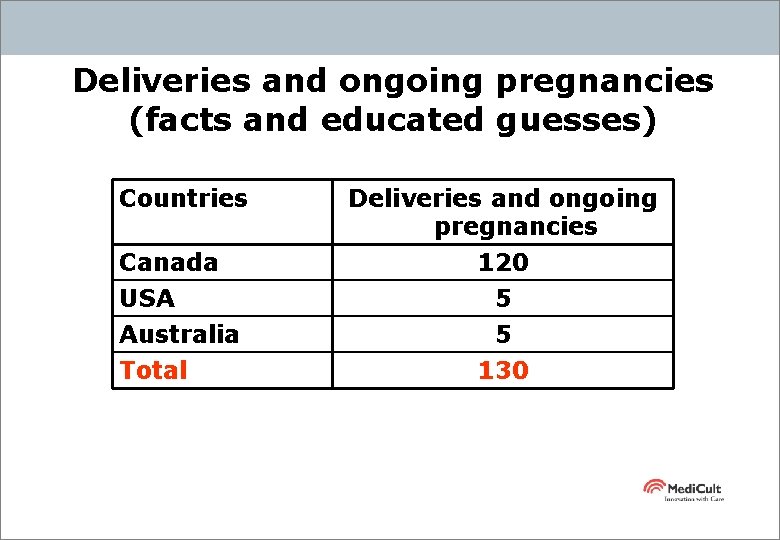
Deliveries and ongoing pregnancies (facts and educated guesses) Countries Deliveries and ongoing pregnancies Canada 120 USA Australia Total 5 5 130
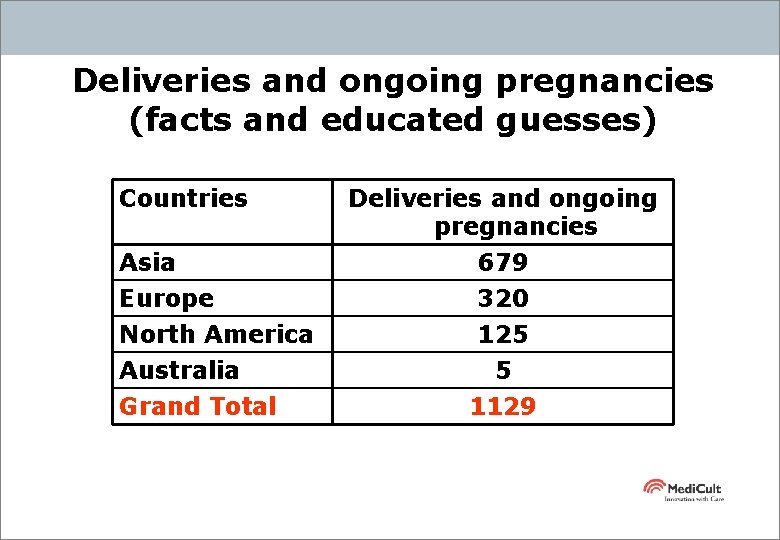
Deliveries and ongoing pregnancies (facts and educated guesses) Countries Asia Europe North America Australia Grand Total Deliveries and ongoing pregnancies 679 320 125 5 1129
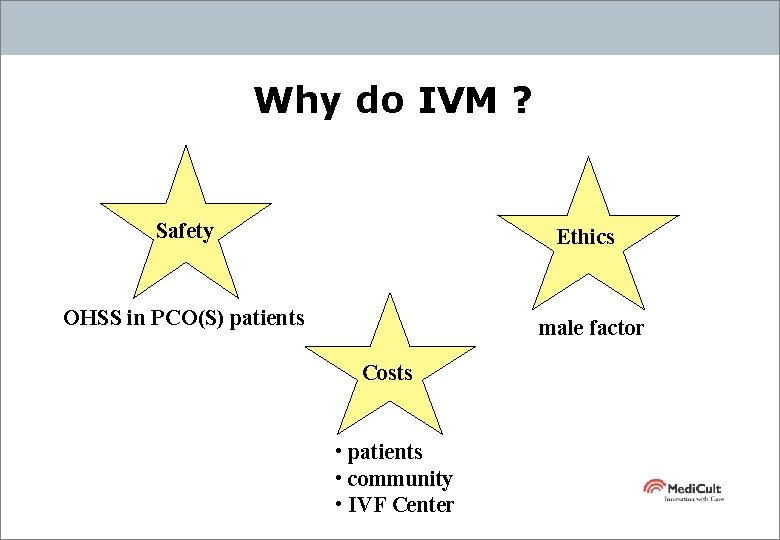
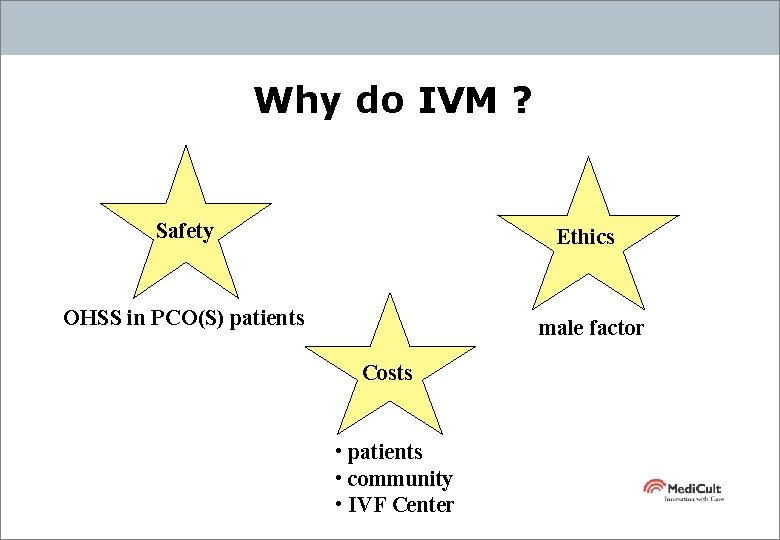
Why do IVM ? Safety Ethics OHSS in PCO(S) patients male factor Costs • patients • community • IVF Center
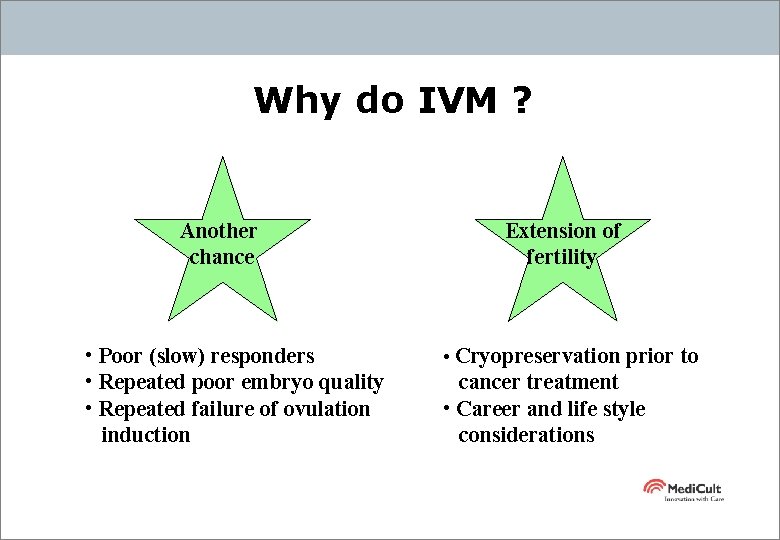
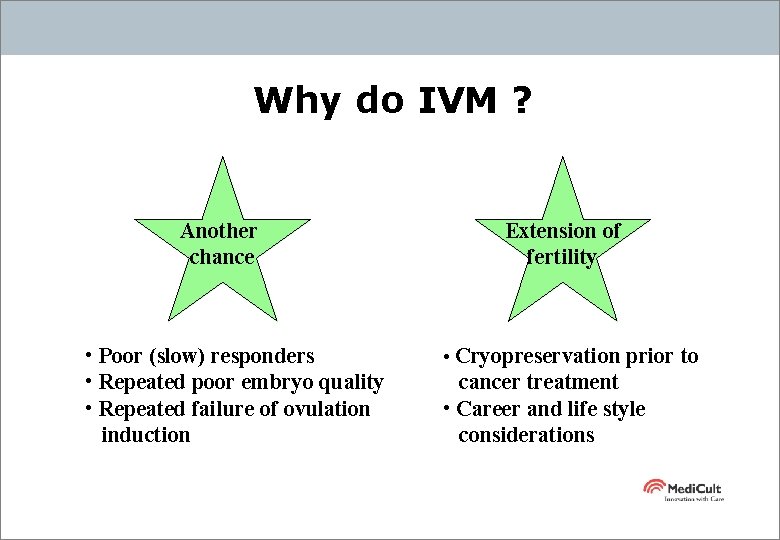
Why do IVM ? Another chance • Poor (slow) responders • Repeated poor embryo quality • Repeated failure of ovulation induction Extension of fertility • Cryopreservation prior to cancer treatment • Career and life style considerations
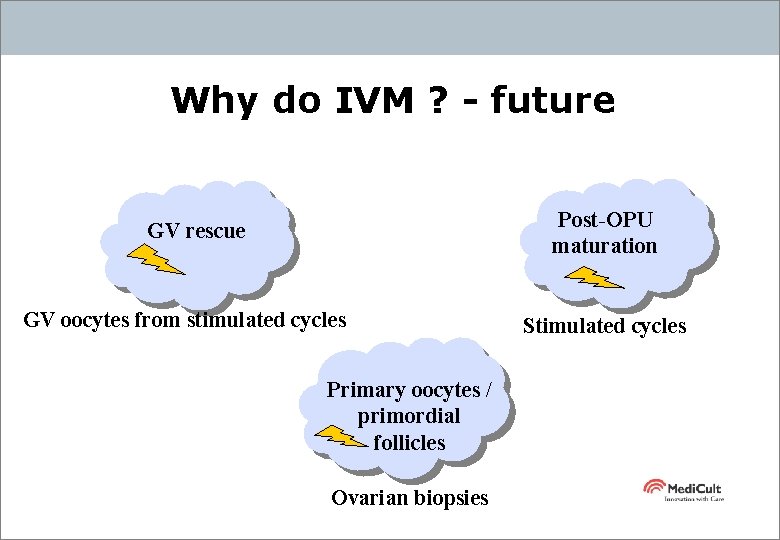
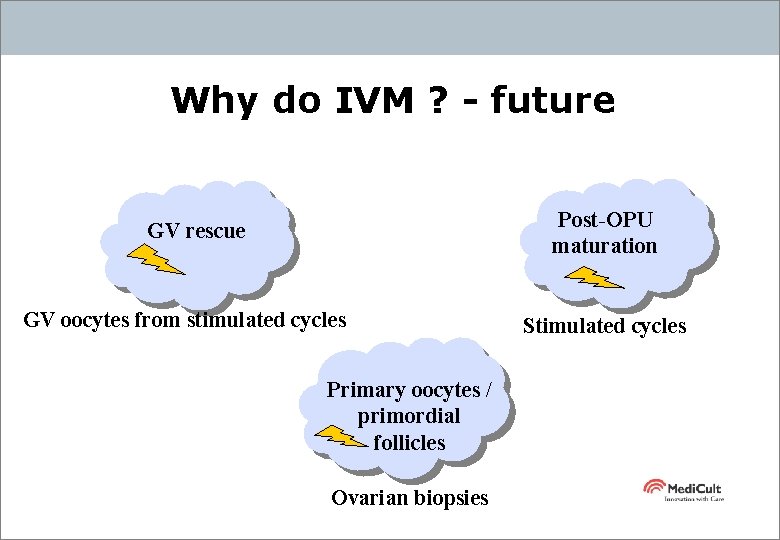
Why do IVM ? - future Post-OPU maturation GV rescue GV oocytes from stimulated cycles Primary oocytes / primordial follicles Ovarian biopsies Stimulated cycles

Scientific background for IVM Oogenesis Follicular development Follicular selection Follicular atresia
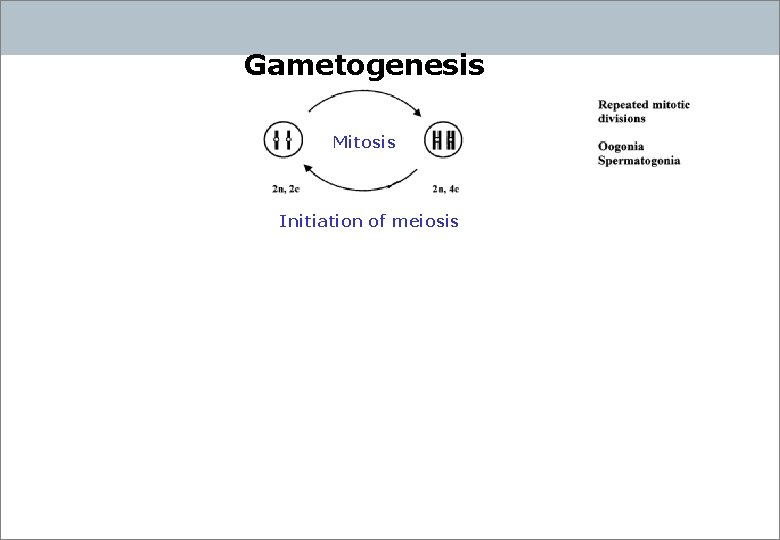
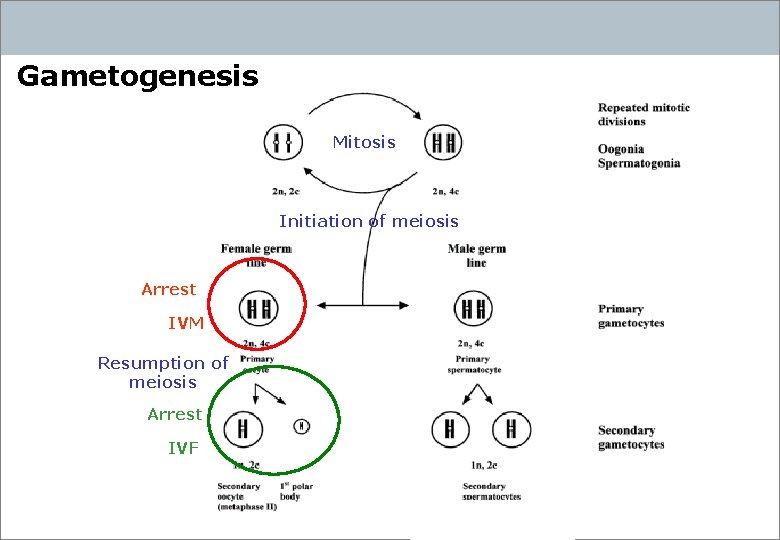
Gametogenesis Mitosis Initiation of meiosis
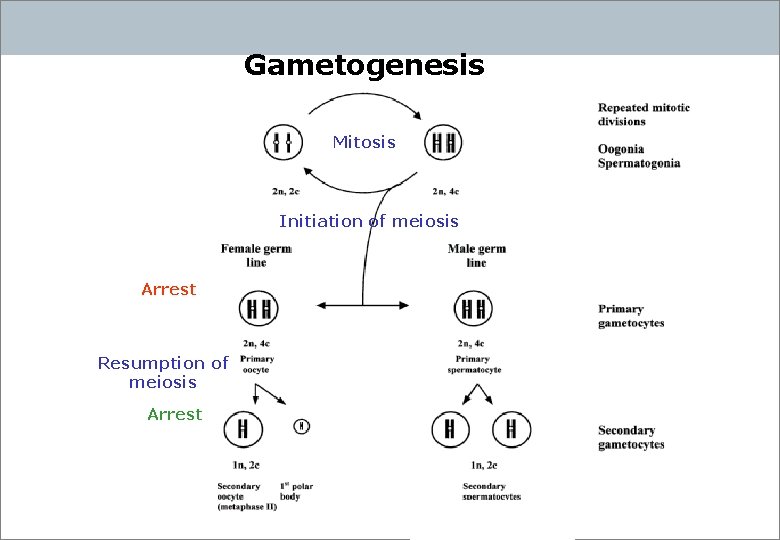
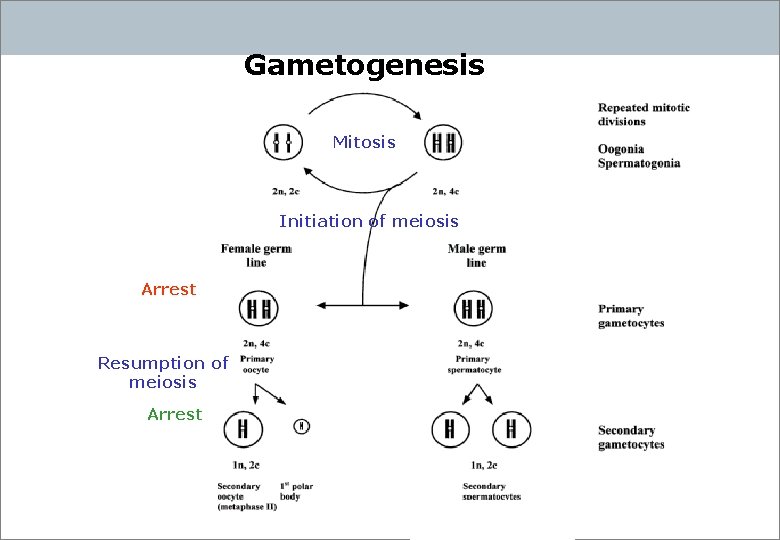
Gametogenesis Mitosis Initiation of meiosis Arrest Resumption of meiosis Arrest
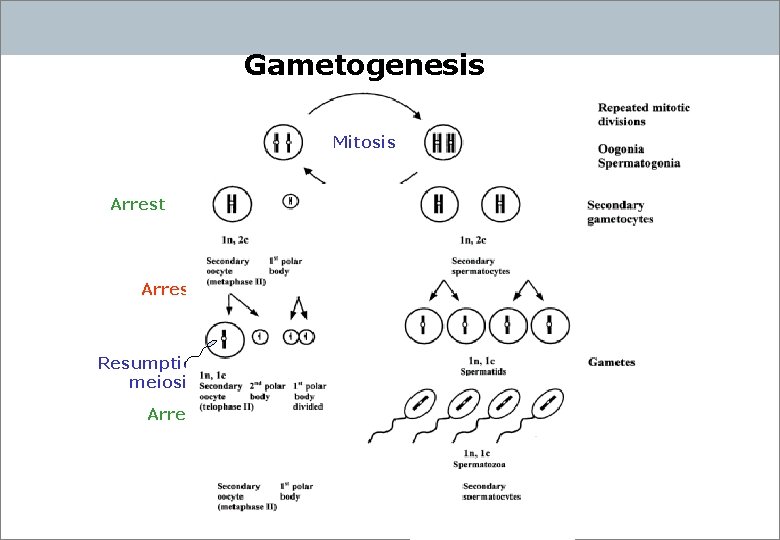
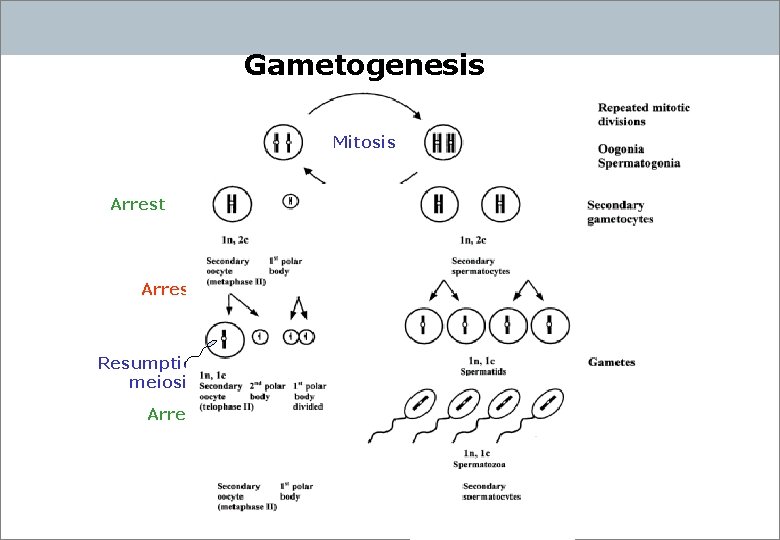
Gametogenesis Mitosis Arrest Resumption of meiosis Arrest Initiation of meiosis
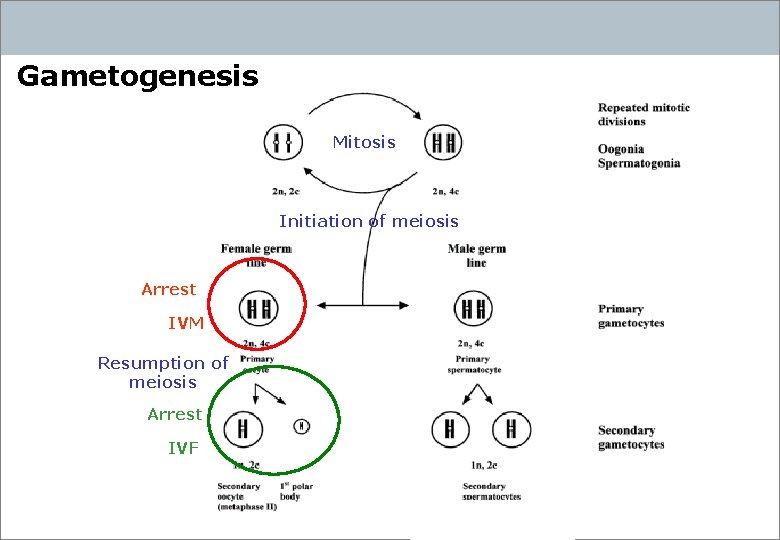
Gametogenesis Mitosis Initiation of meiosis Arrest IVM Resumption of meiosis Arrest IVF
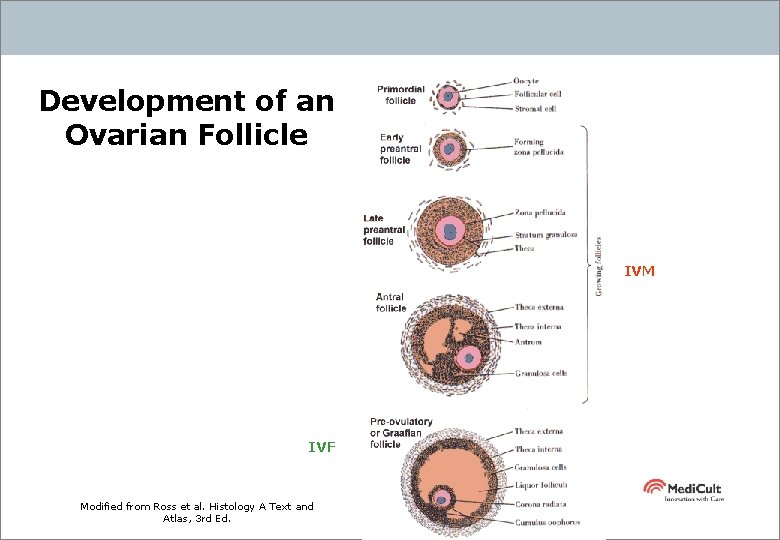
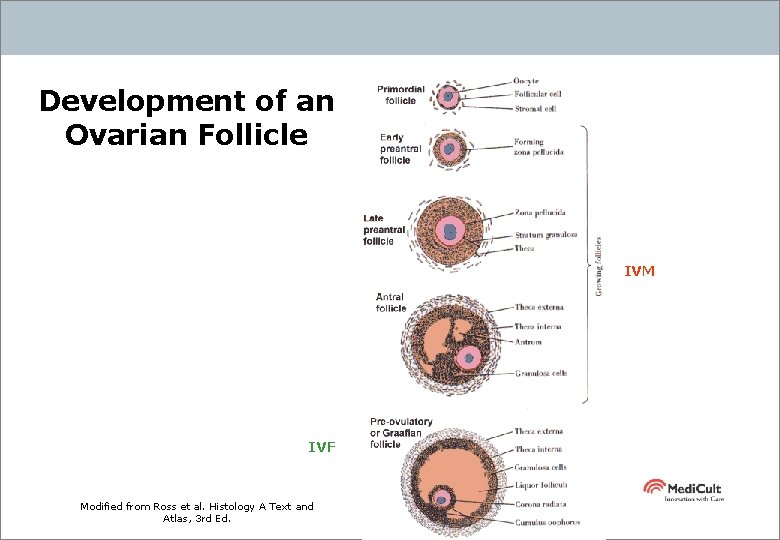
Development of an Ovarian Follicle IVM IVF Modified from Ross et al. Histology A Text and Atlas, 3 rd Ed.
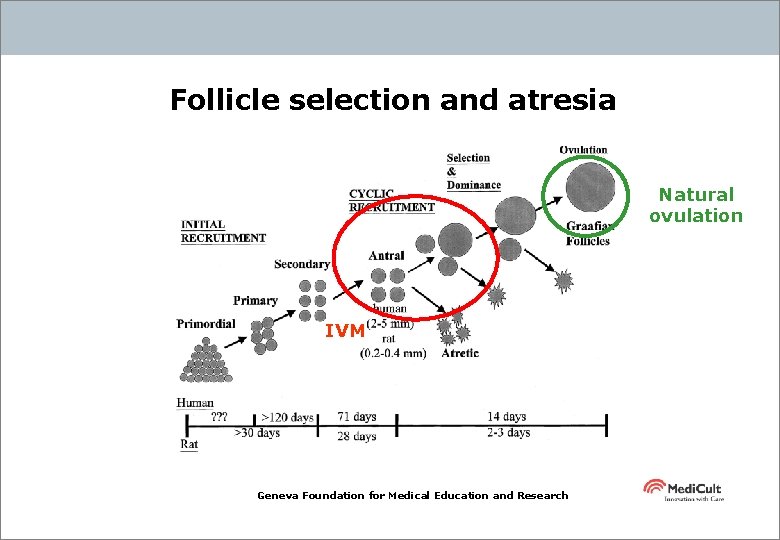
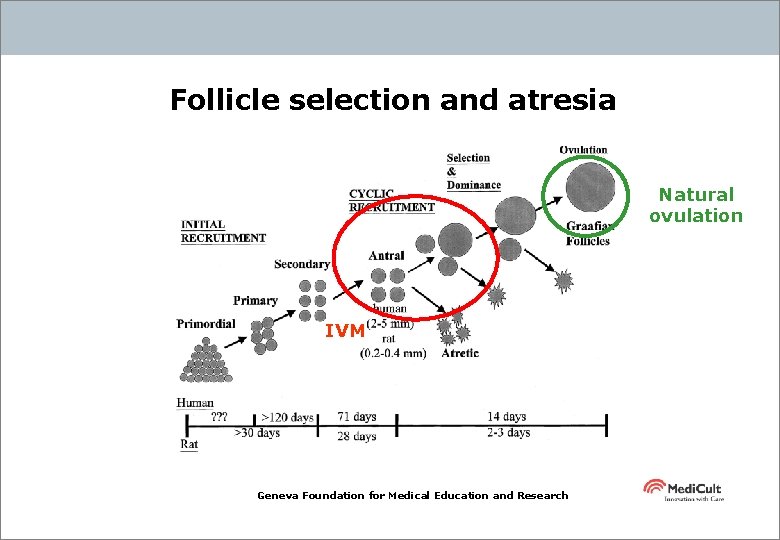
Follicle selection and atresia Natural ovulation IVM Geneva Foundation for Medical Education and Research
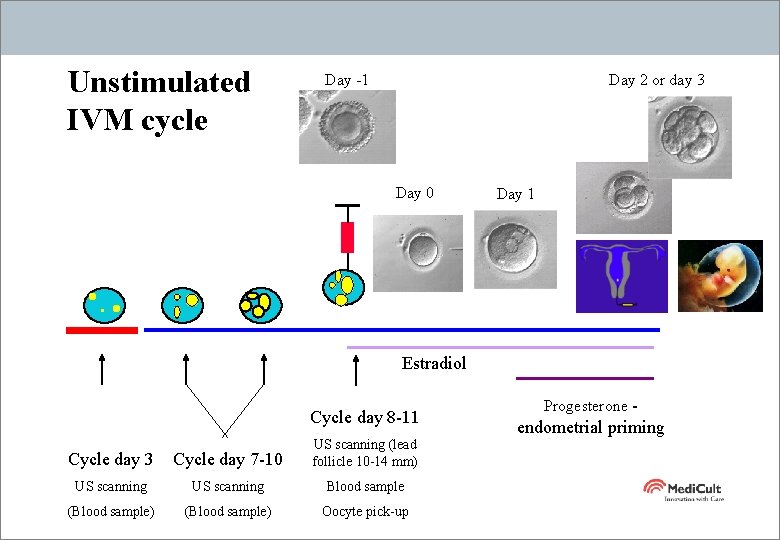
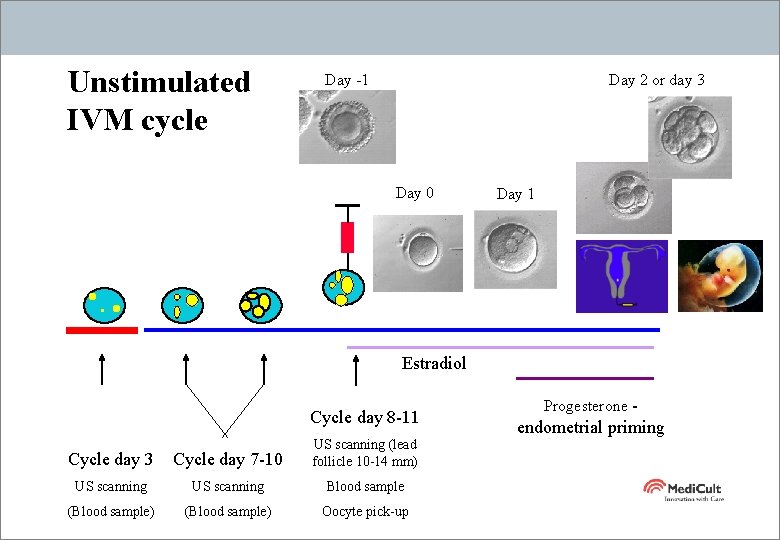
Unstimulated IVM cycle Day -1 Day 2 or day 3 Day 0 Day 1 Estradiol Cycle day 8 -11 Cycle day 3 Cycle day 7 -10 US scanning (lead follicle 10 -14 mm) US scanning Blood sample (Blood sample) Oocyte pick-up Progesterone - endometrial priming

Traditional IVF versus IVM Traditional IVF IVM® • • • Relatively many oocytes/embryos ’High’ pregnancy rate / OPU Down regulation • • Daily hormone injections • • • h. CG injection Emotional stress Long treatment time - 4 -6 weeks • • Potential side effects (e. g. OHSS) Fewer oocytes and embryos Lower pregnancy rate / OPU - BUT No down regulation, no manipulation of hormone balance No hormone injections – or Minimal hormone injections (PCOS) (No h. CG injection) Reduced psychological impact Reduced treatment time – 2 weeks Reduced interference with daily life No known side effects (e. g. OHSS)

Average 3. 0 29
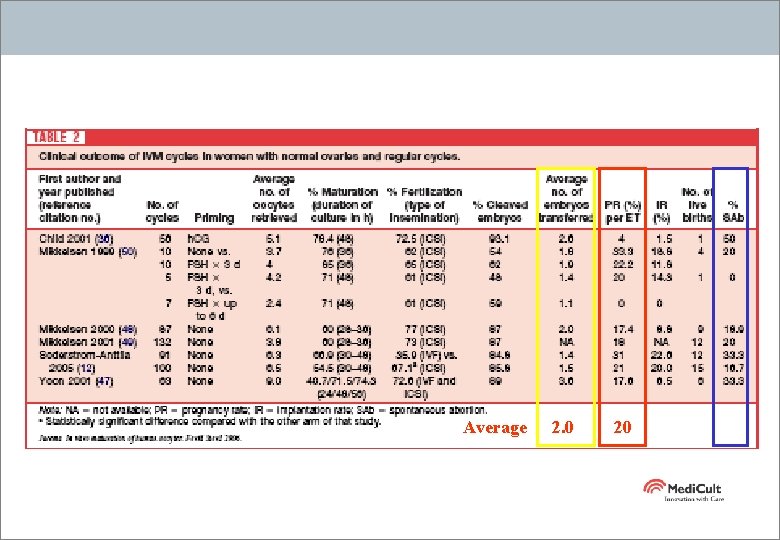
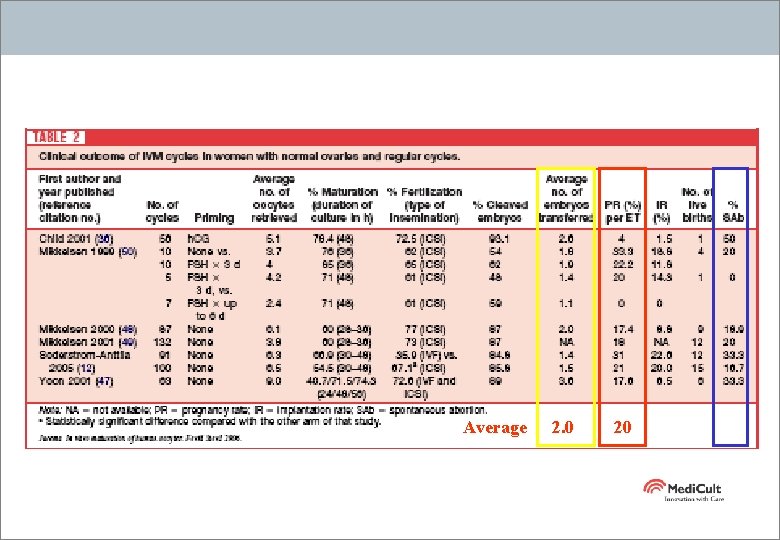
Average 2. 0 20
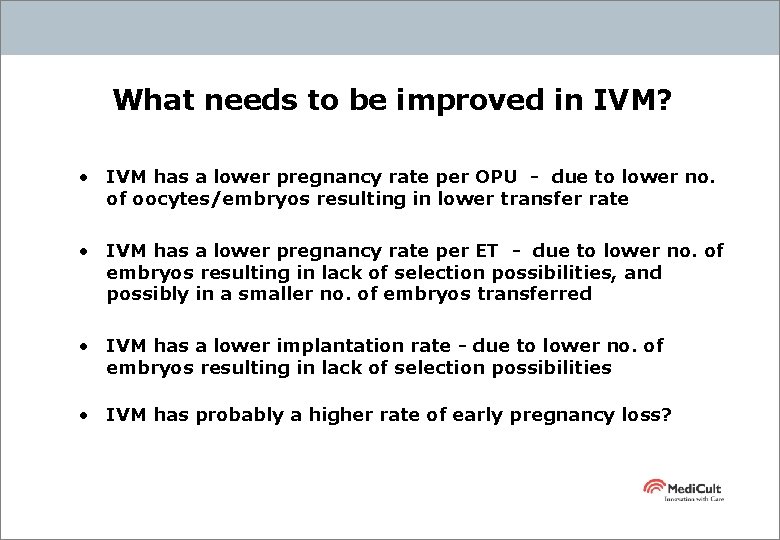
What needs to be improved in IVM? • IVM has a lower pregnancy rate per OPU - due to lower no. of oocytes/embryos resulting in lower transfer rate • IVM has a lower pregnancy rate per ET - due to lower no. of embryos resulting in lack of selection possibilities, and possibly in a smaller no. of embryos transferred • IVM has a lower implantation rate - due to lower no. of embryos resulting in lack of selection possibilities • IVM has probably a higher rate of early pregnancy loss?

Shukran
 Digestion chimique
Digestion chimique Procedure for isolation of cells for in vitro culture
Procedure for isolation of cells for in vitro culture Vitro data center
Vitro data center Wetboek familierecht
Wetboek familierecht Tumacenje ige
Tumacenje ige Sap netweaver portal vitro
Sap netweaver portal vitro Felice shieh
Felice shieh Secondary oocyte and ovum
Secondary oocyte and ovum Primary oocyte haploid or diploid
Primary oocyte haploid or diploid Is mitosis asexual
Is mitosis asexual Metaphase mitosis
Metaphase mitosis Primary oocyte haploid or diploid
Primary oocyte haploid or diploid Meiosis ii stages
Meiosis ii stages Primary oocyte haploid or diploid
Primary oocyte haploid or diploid Secondary follicles
Secondary follicles Primary oocyte
Primary oocyte An oocyte is
An oocyte is Tunica vaginalis
Tunica vaginalis Masoderm
Masoderm Extraembryonic membranes in human embryo
Extraembryonic membranes in human embryo D
D Oogenesis animation
Oogenesis animation Oogenesis
Oogenesis