UNIT 6 REPRODUCTION AND DEVELOPMENT PART 1 THE













- Slides: 67
UNIT 6 REPRODUCTION AND DEVELOPMENT PART 1 THE REPRODUCTIVE SYSTEMS ZOOL-1072 Human Anatomy and Physiology
FEMALE REPRODUCTIVE SYSTEM

Introduction Purpose of sexual reproduction Fertilization Gynecology �Diagnosis and treatment of female reproductive diseases Urology �Urinary system and issues with male reproductive system Andrology �Male reproductive disorders
Female reproductive system Gonads – ovaries Uterine (fallopian) tubes or oviducts Uterus Vagina External organs – vulva or pudendum Mammary glands
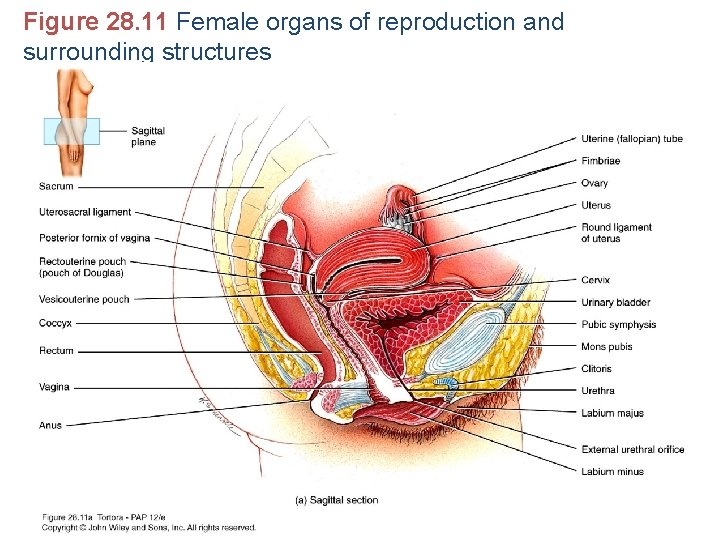
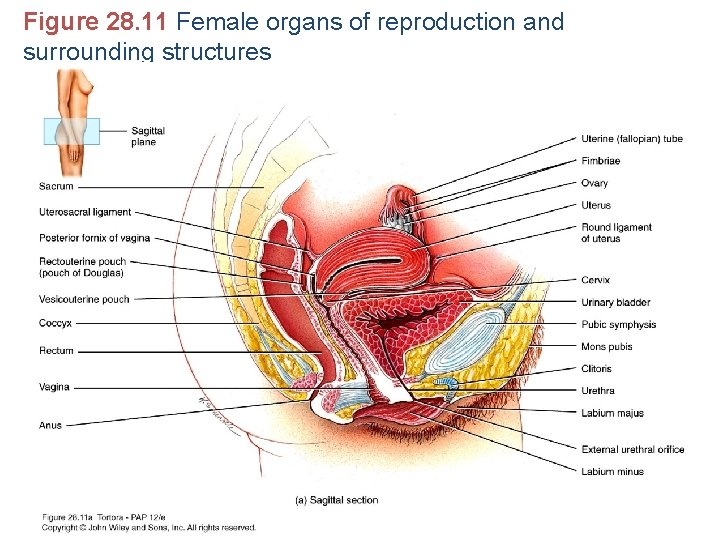
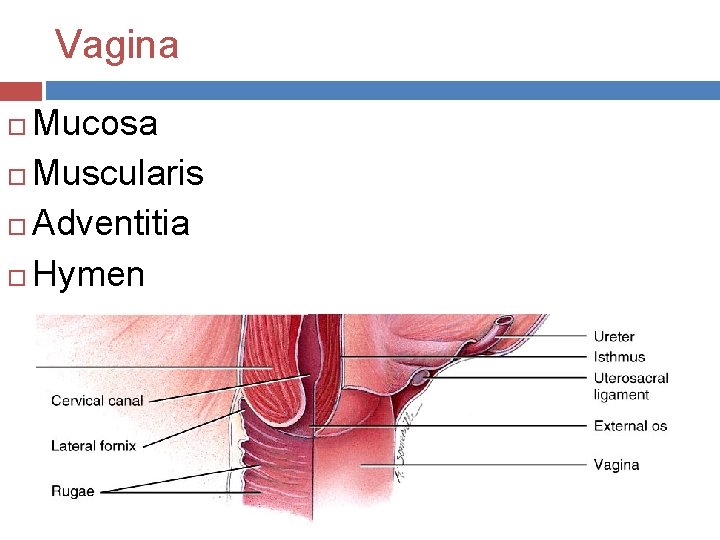
Figure 28. 11 Female organs of reproduction and surrounding structures

Figure 28. 11 Female organs of reproduction and surrounding structures
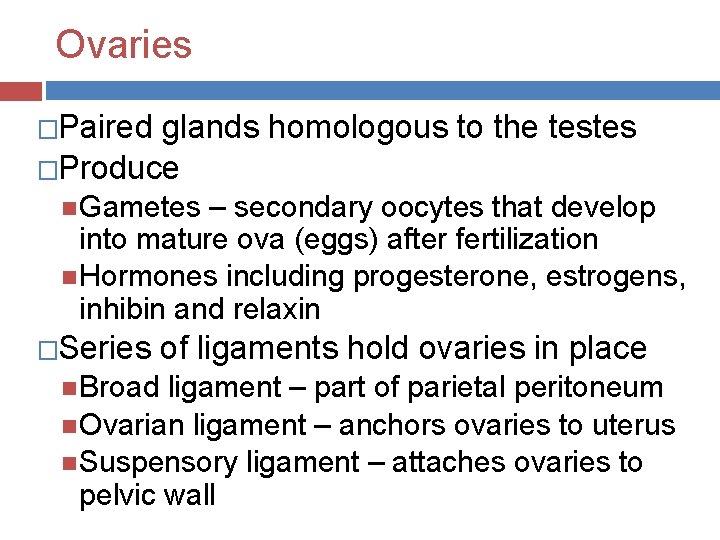
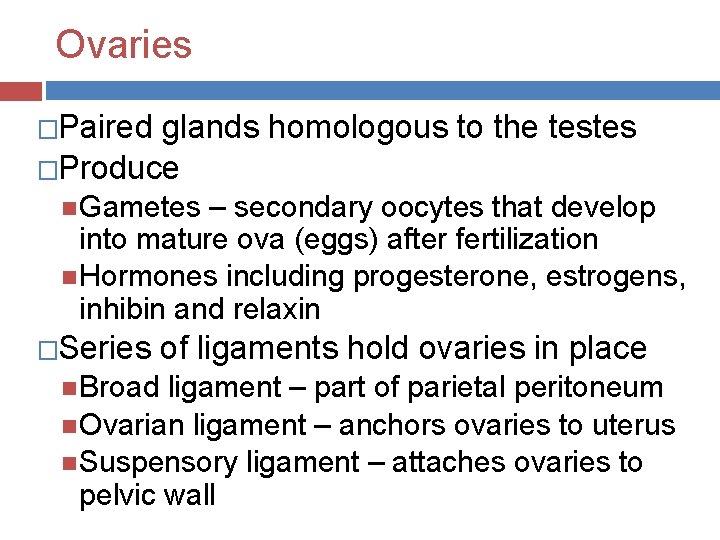
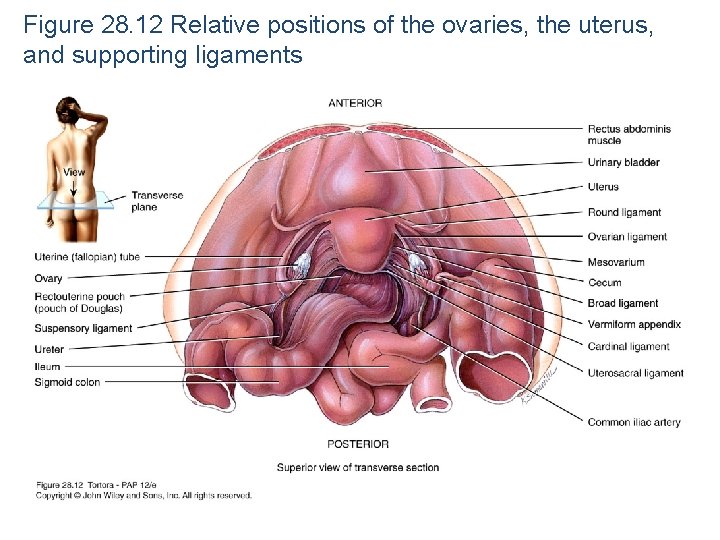
Ovaries �Paired glands homologous to the testes �Produce Gametes – secondary oocytes that develop into mature ova (eggs) after fertilization Hormones including progesterone, estrogens, inhibin and relaxin �Series of ligaments hold ovaries in place Broad ligament – part of parietal peritoneum Ovarian ligament – anchors ovaries to uterus Suspensory ligament – attaches ovaries to pelvic wall
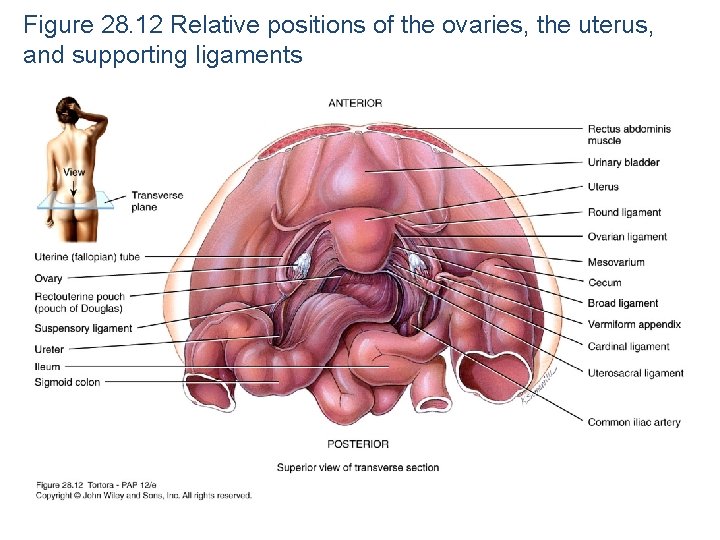
Figure 28. 12 Relative positions of the ovaries, the uterus, and supporting ligaments
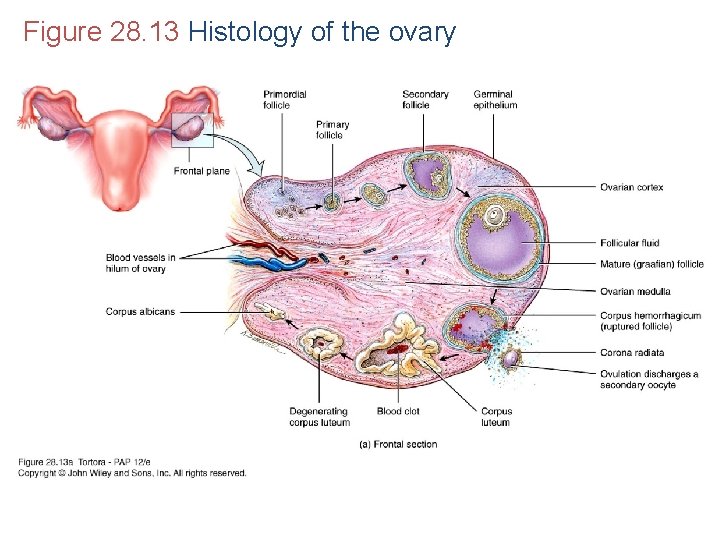
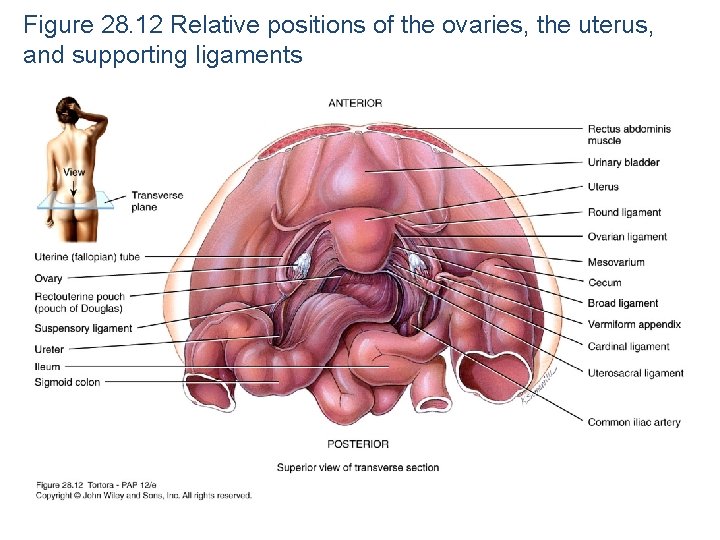
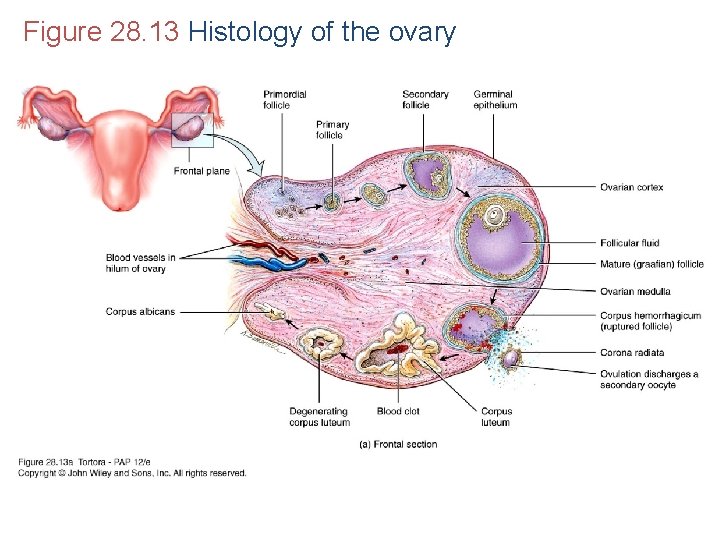
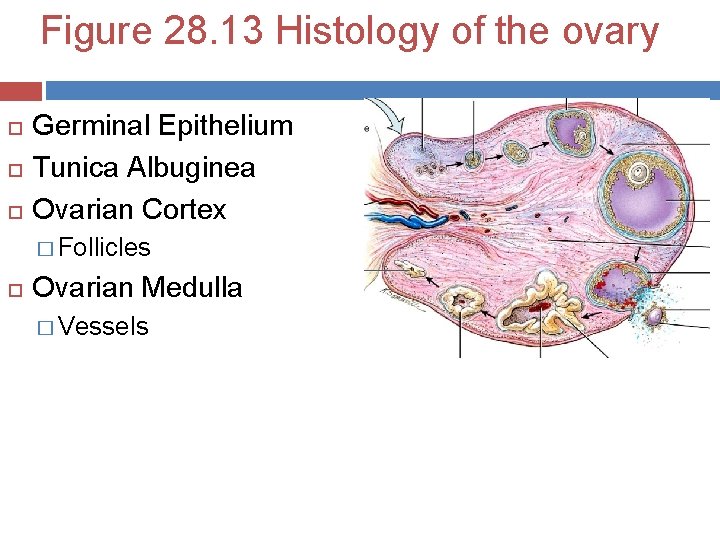
Figure 28. 13 Histology of the ovary
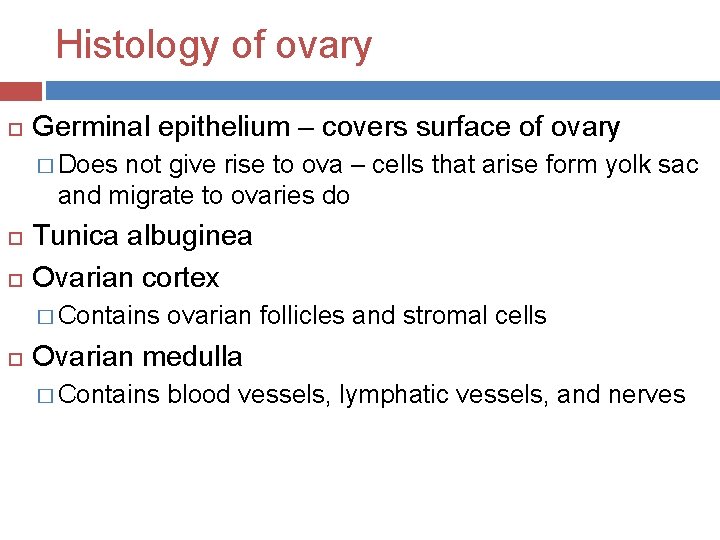
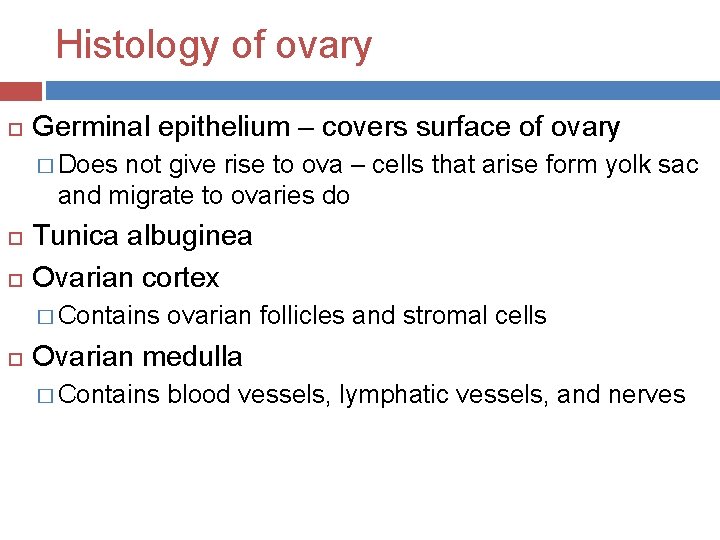
Histology of ovary Germinal epithelium – covers surface of ovary � Does not give rise to ova – cells that arise form yolk sac and migrate to ovaries do Tunica albuginea Ovarian cortex � Contains ovarian follicles and stromal cells Ovarian medulla � Contains blood vessels, lymphatic vessels, and nerves

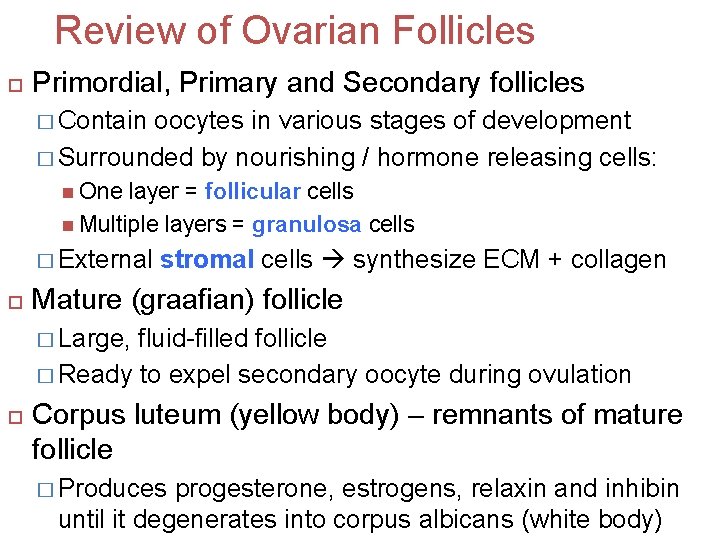
Ovarian Follicles Ovarian follicles – in cortex; consist of oocytes in various stages of development � Surrounding cells nourish developing oocyte and secrete estrogens as follicle grows Mature (graafian) follicle – large, fluid-filled follicle ready to expel secondary oocyte during ovulation Corpus luteum – remnants of mature follicle after ovulation � Produces progesterone, estrogens, relaxin and inhibin until it degenerates into corpus albicans

Figure 28. 13 Histology of the ovary

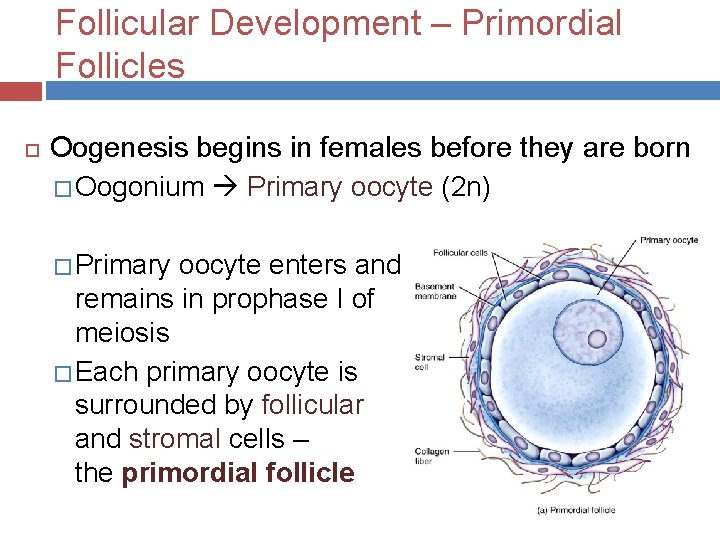
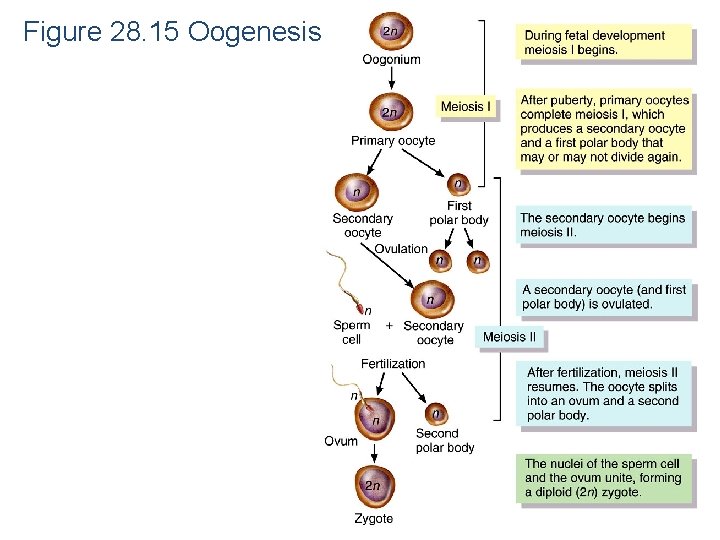
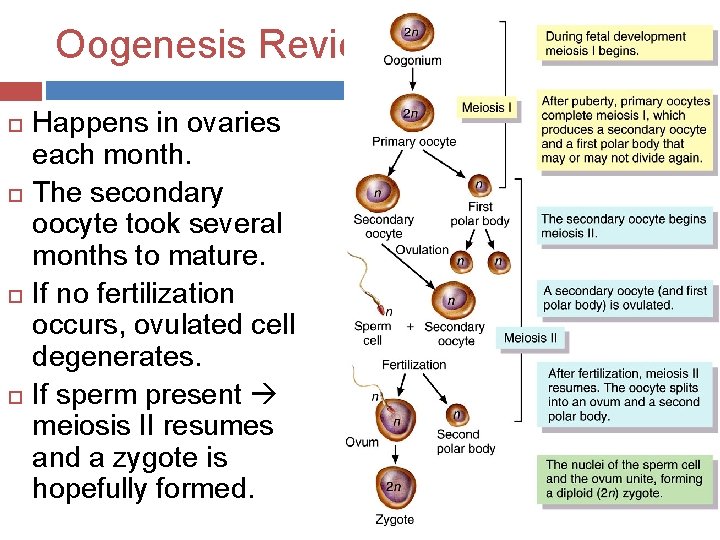
Oogenesis and follicular development Oogenesis begins before females are born Essentially same steps of meiosis as spermatogenesis During early fetal development, primordial (primitive) germ cells migrate to ovaries Germ cells then differentiate into oogonia – diploid (2 n) stem cells Before birth, most germ cells degenerate – atresia A “few” develop into primary oocytes that enter meiosis I during fetal development � Each covered by single layer of flat follicular cells – primordial follicle � About 200, 000 to 2, 000 at birth, 40, 000 remain at puberty, and around 400 will mature during a lifetime
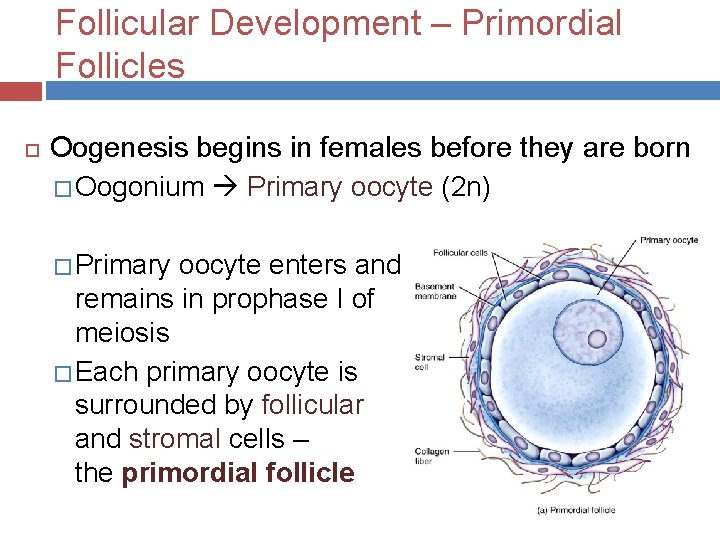
Follicular Development – Primordial Follicles Oogenesis begins in females before they are born � Oogonium Primary oocyte (2 n) � Primary oocyte enters and remains in prophase I of meiosis � Each primary oocyte is surrounded by follicular and stromal cells – the primordial follicle
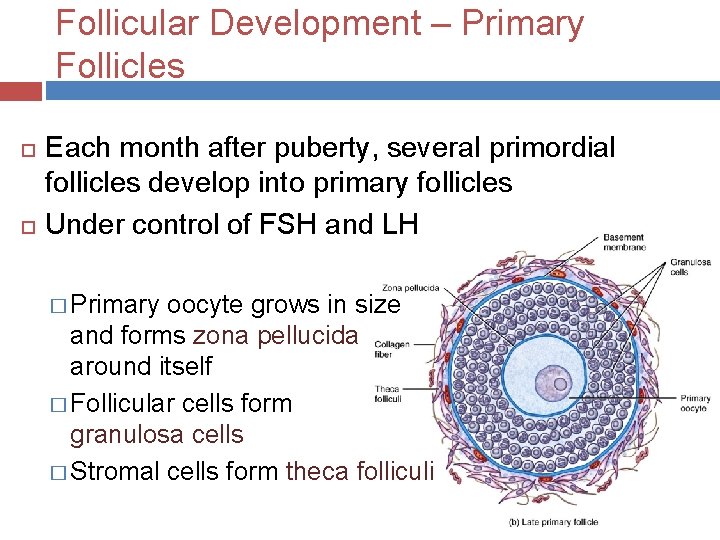
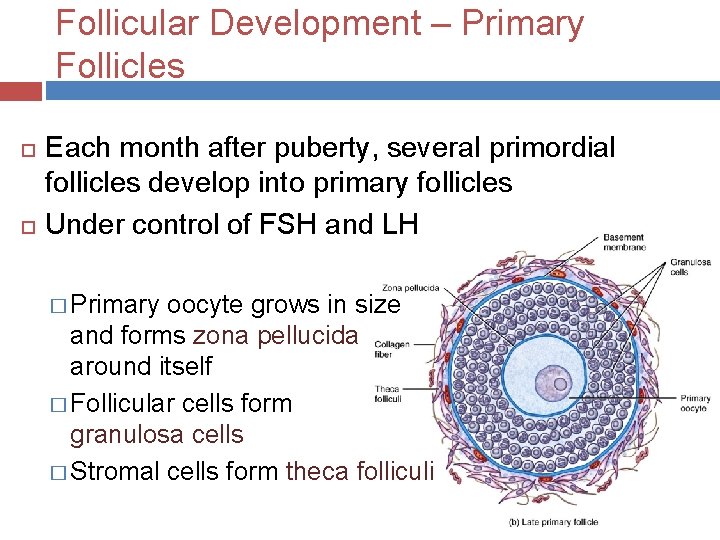
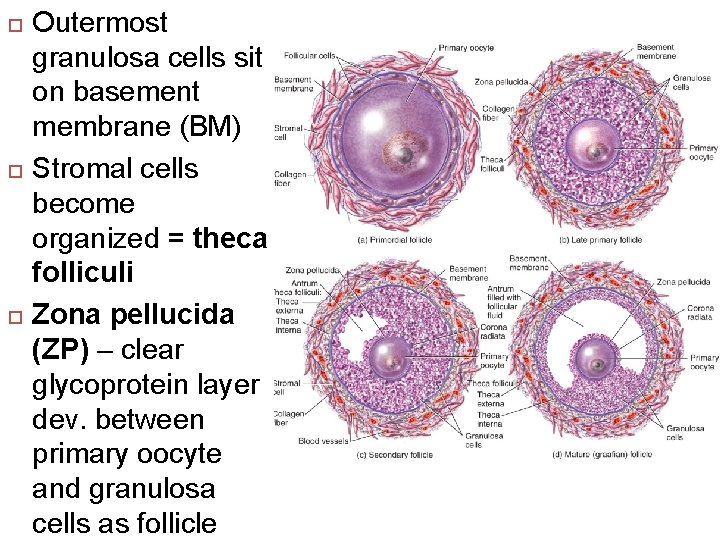
Follicular Development – Primary Follicles Each month after puberty, several primordial follicles develop into primary follicles Under control of FSH and LH � Primary oocyte grows in size and forms zona pellucida around itself � Follicular cells form granulosa cells � Stromal cells form theca folliculi
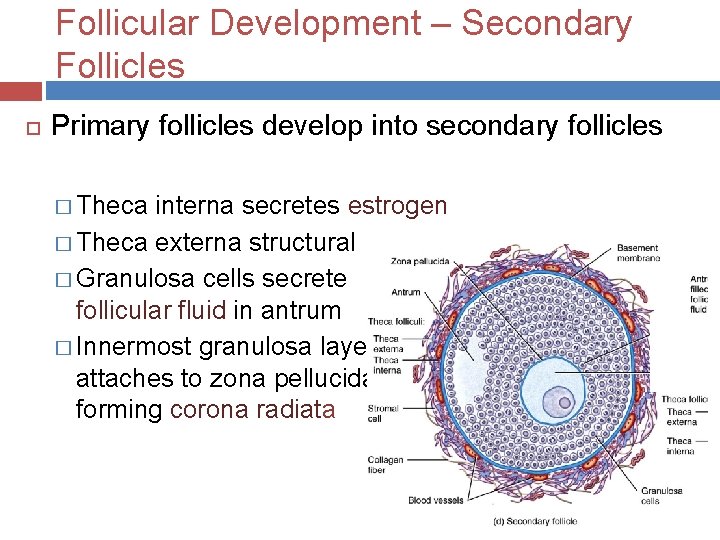
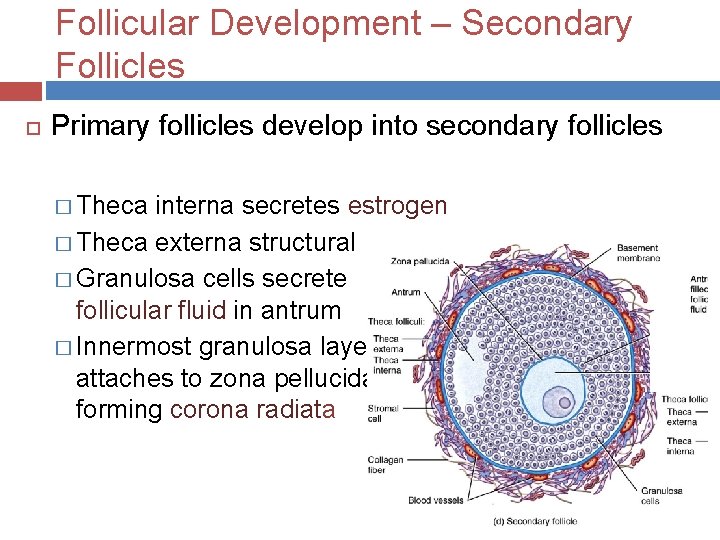
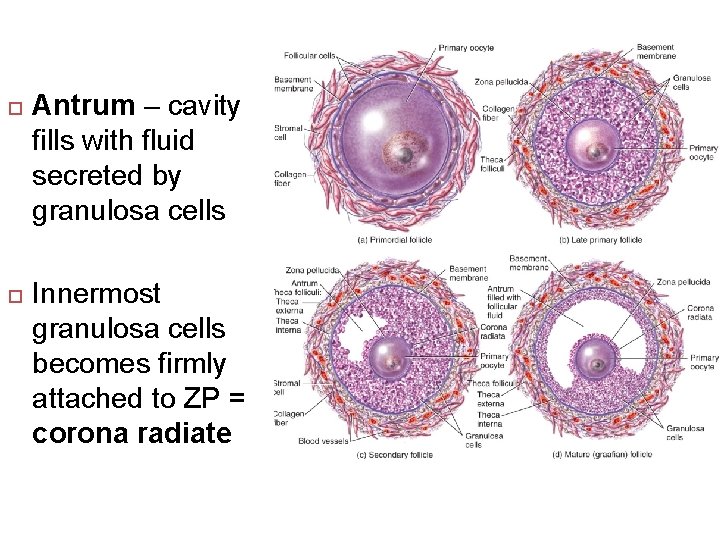
Follicular Development – Secondary Follicles Primary follicles develop into secondary follicles � Theca interna secretes estrogen � Theca externa structural � Granulosa cells secrete follicular fluid in antrum � Innermost granulosa layer attaches to zona pellucida forming corona radiata
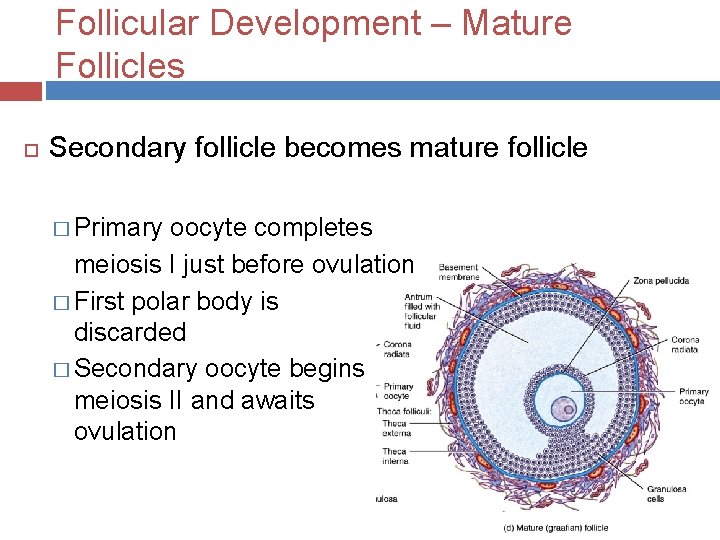
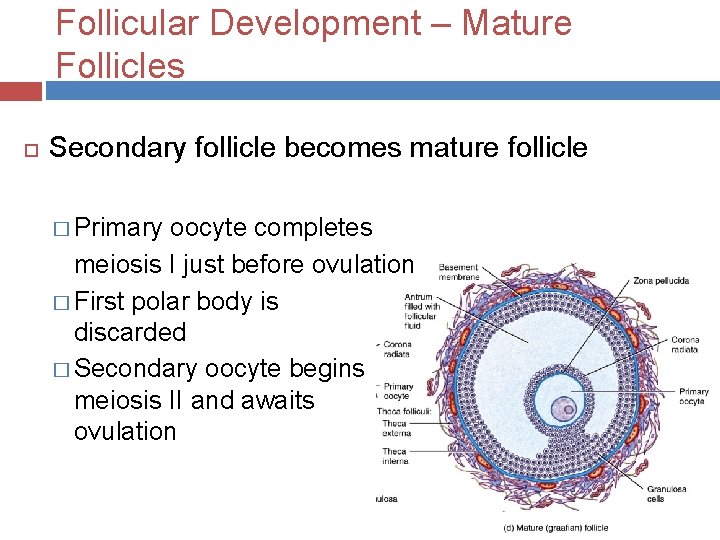
Follicular Development – Mature Follicles Secondary follicle becomes mature follicle � Primary oocyte completes meiosis I just before ovulation � First polar body is discarded � Secondary oocyte begins meiosis II and awaits ovulation
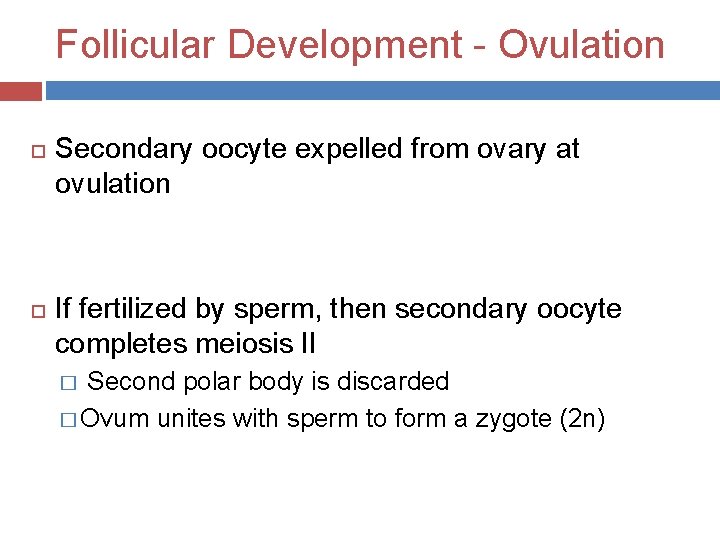
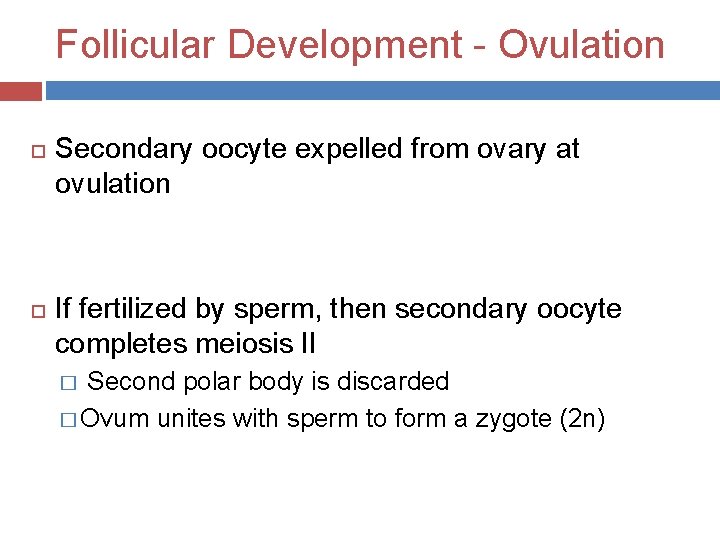
Follicular Development - Ovulation Secondary oocyte expelled from ovary at ovulation If fertilized by sperm, then secondary oocyte completes meiosis II � Second polar body is discarded � Ovum unites with sperm to form a zygote (2 n)
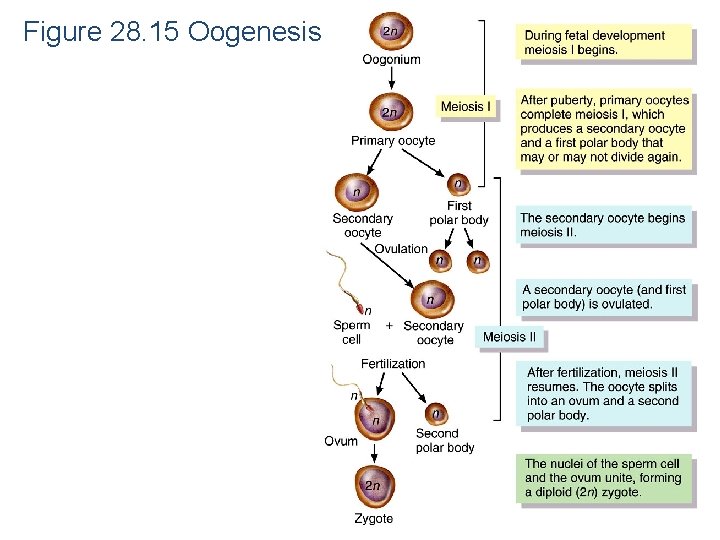
Figure 28. 15 Oogenesis

Tuesday Quickly review follicular development and clarify a few terms from yesterday. Continue with uterine tube, uterus, mucus, vagina, vulva, perineum, mammary glands Tomorrow – start the female reproductive cycle
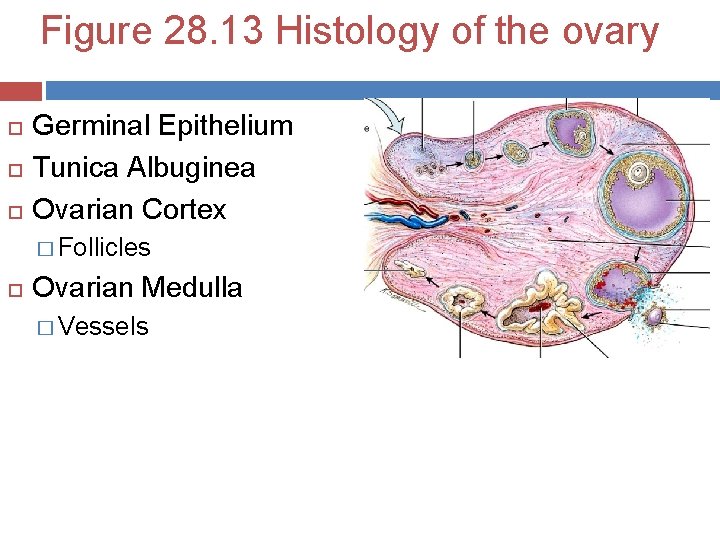
Figure 28. 13 Histology of the ovary Germinal Epithelium Tunica Albuginea Ovarian Cortex � Follicles Ovarian Medulla � Vessels
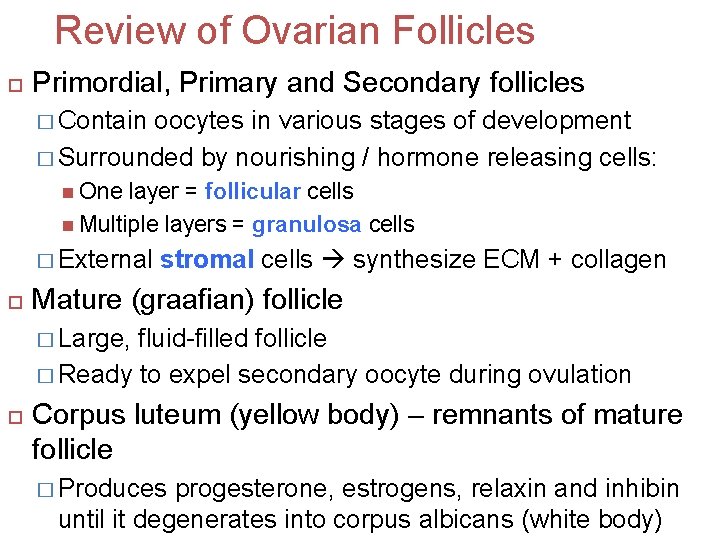
Review of Ovarian Follicles Primordial, Primary and Secondary follicles � Contain oocytes in various stages of development � Surrounded by nourishing / hormone releasing cells: One layer = follicular cells Multiple layers = granulosa cells � External stromal cells synthesize ECM + collagen Mature (graafian) follicle � Large, fluid-filled follicle � Ready to expel secondary oocyte during ovulation Corpus luteum (yellow body) – remnants of mature follicle � Produces progesterone, estrogens, relaxin and inhibin until it degenerates into corpus albicans (white body)
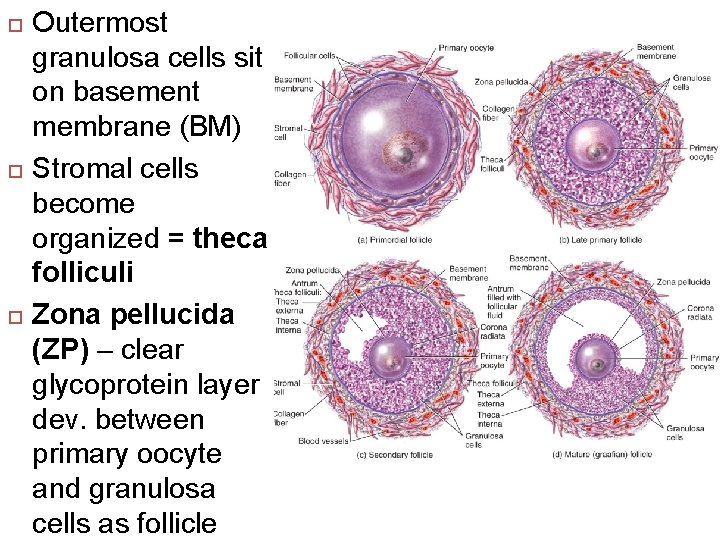
Outermost granulosa cells sit on basement membrane (BM) Stromal cells become organized = theca folliculi Zona pellucida (ZP) – clear glycoprotein layer dev. between primary oocyte and granulosa cells as follicle
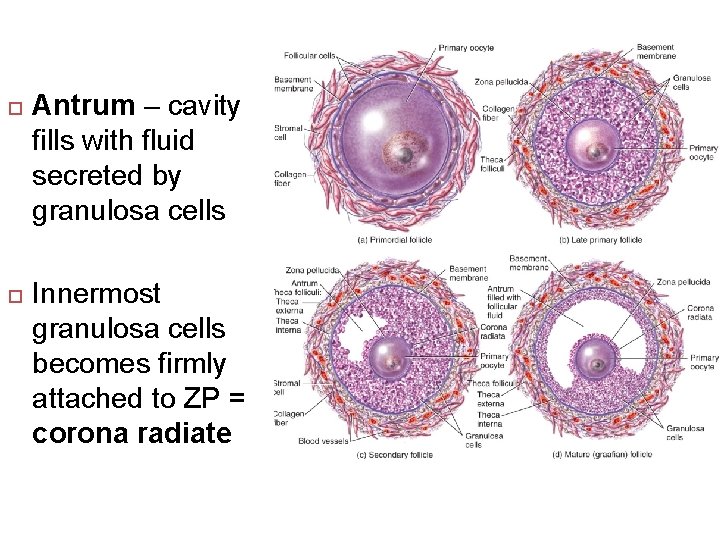
Antrum – cavity fills with fluid secreted by granulosa cells Innermost granulosa cells becomes firmly attached to ZP = corona radiate
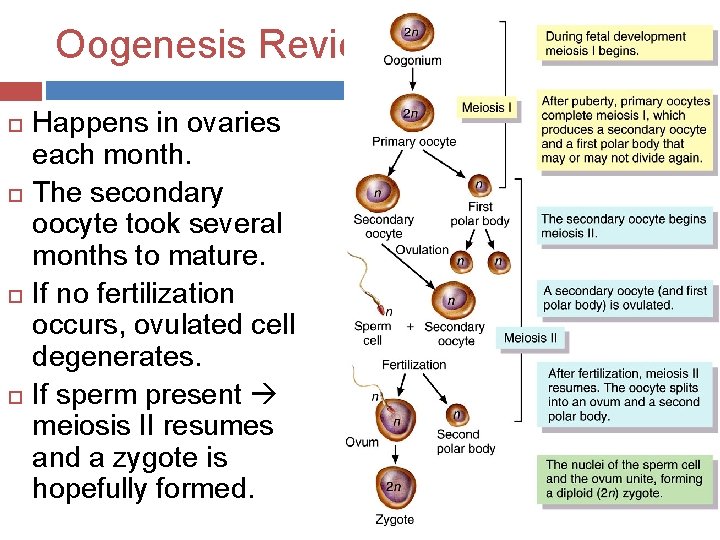
Oogenesis Review Happens in ovaries each month. The secondary oocyte took several months to mature. If no fertilization occurs, ovulated cell degenerates. If sperm present meiosis II resumes and a zygote is hopefully formed.
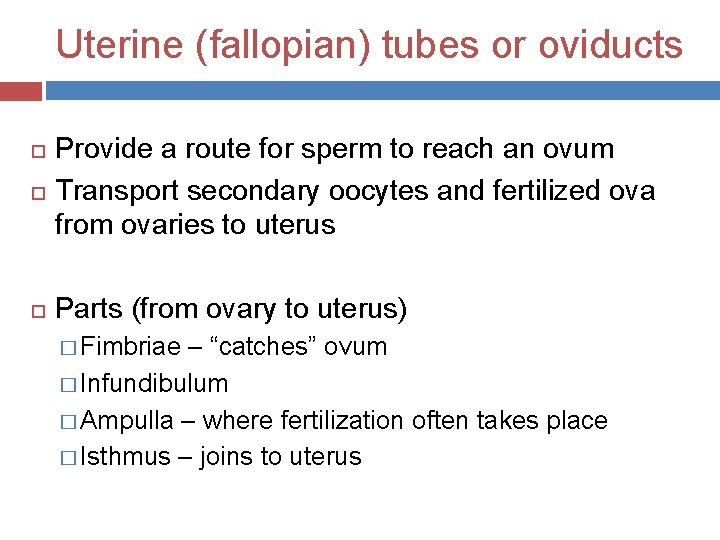
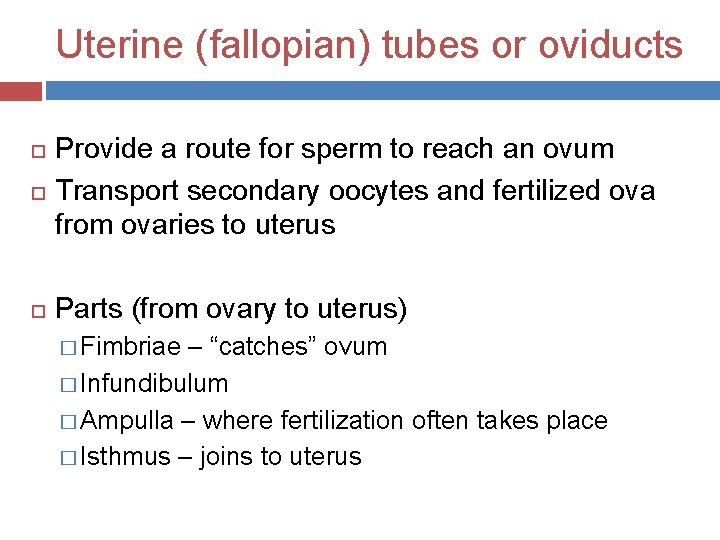
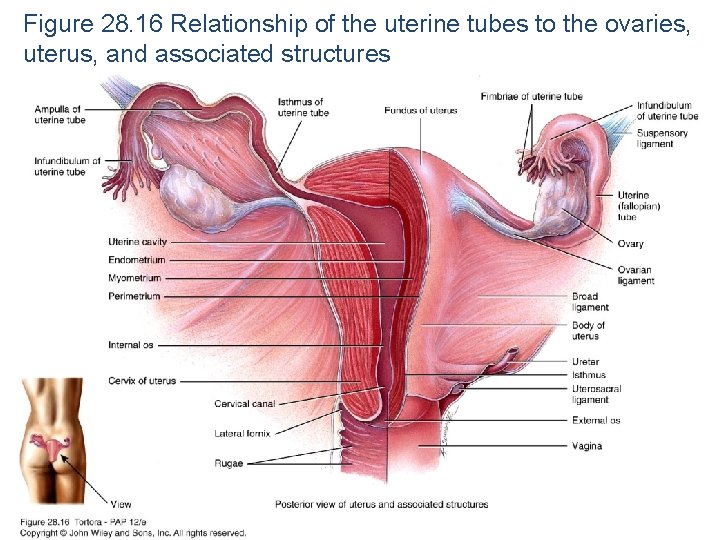
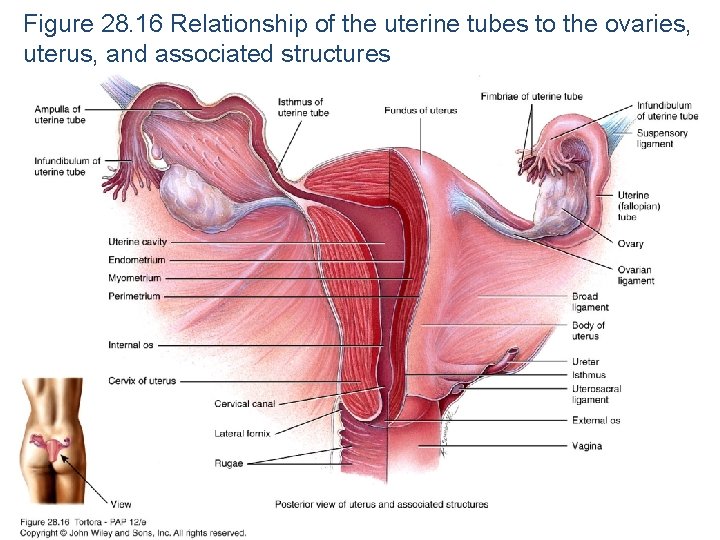
Uterine (fallopian) tubes or oviducts Provide a route for sperm to reach an ovum Transport secondary oocytes and fertilized ova from ovaries to uterus Parts (from ovary to uterus) � Fimbriae – “catches” ovum � Infundibulum � Ampulla – where fertilization often takes place � Isthmus – joins to uterus
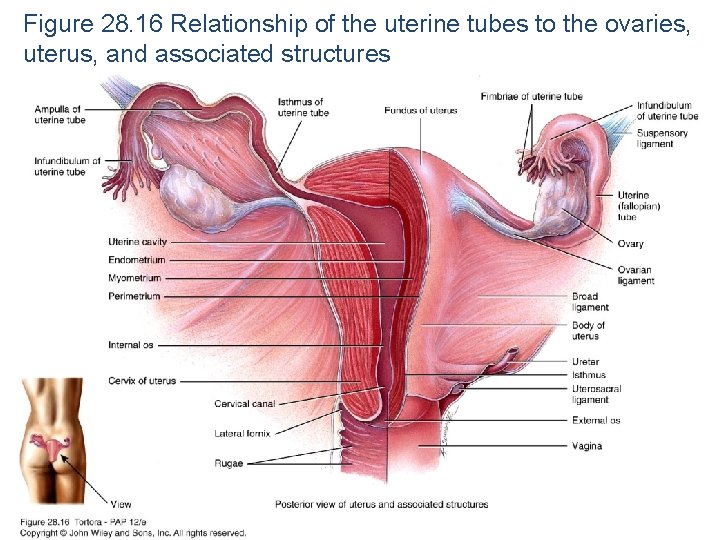
Figure 28. 16 Relationship of the uterine tubes to the ovaries, uterus, and associated structures
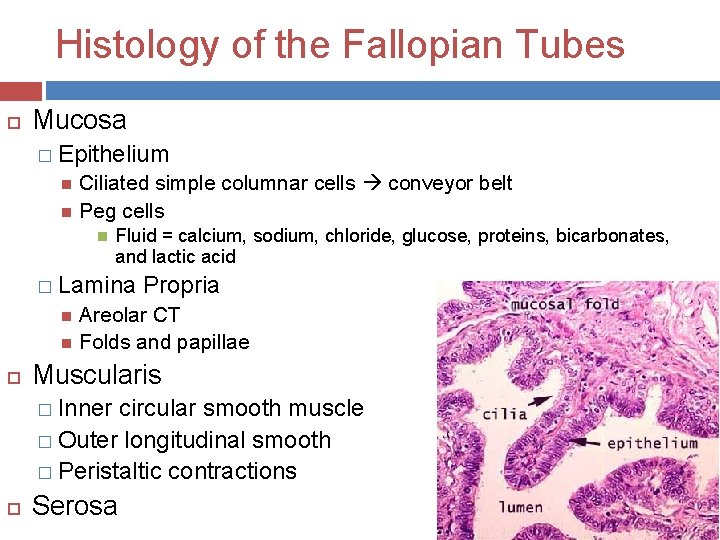
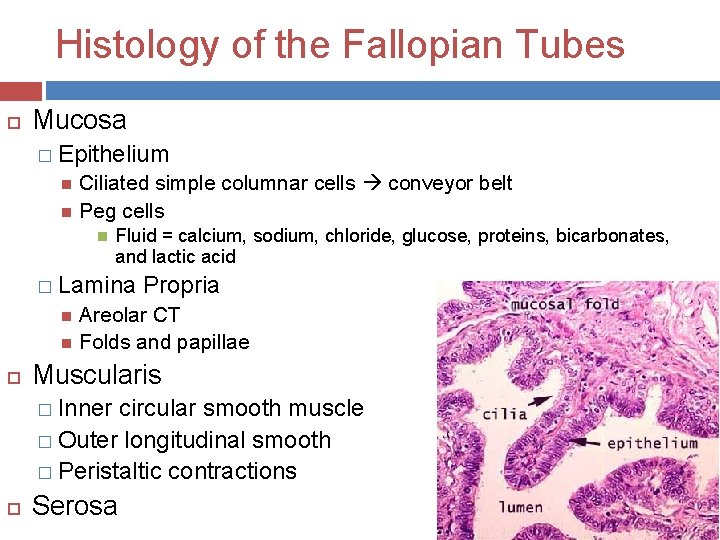
Histology of the Fallopian Tubes Mucosa � Epithelium Ciliated simple columnar cells conveyor belt Peg cells Fluid = calcium, sodium, chloride, glucose, proteins, bicarbonates, and lactic acid � Lamina Propria Areolar CT Folds and papillae Muscularis � Inner circular smooth muscle � Outer longitudinal smooth � Peristaltic contractions Serosa
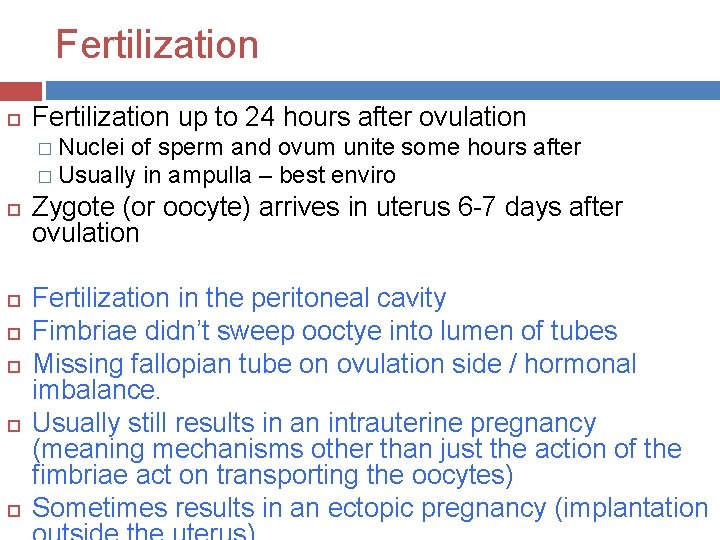
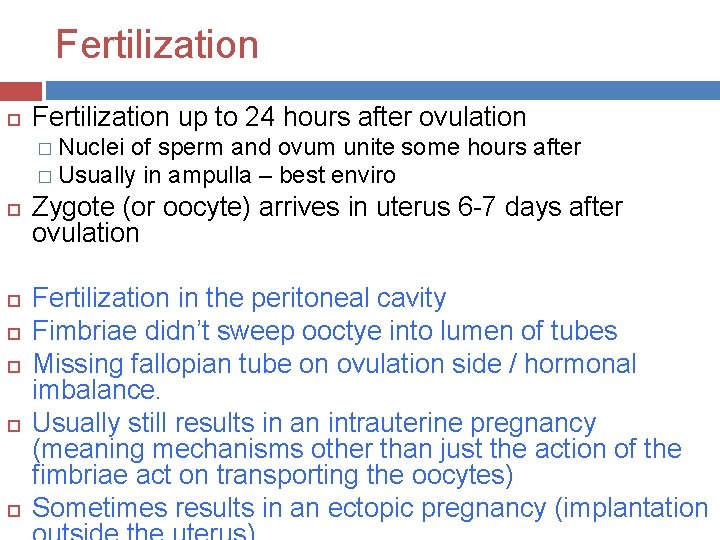
Fertilization up to 24 hours after ovulation � Nuclei of sperm and ovum unite some hours after � Usually in ampulla – best enviro Zygote (or oocyte) arrives in uterus 6 -7 days after ovulation Fertilization in the peritoneal cavity Fimbriae didn’t sweep ooctye into lumen of tubes Missing fallopian tube on ovulation side / hormonal imbalance. Usually still results in an intrauterine pregnancy (meaning mechanisms other than just the action of the fimbriae act on transporting the oocytes) Sometimes results in an ectopic pregnancy (implantation
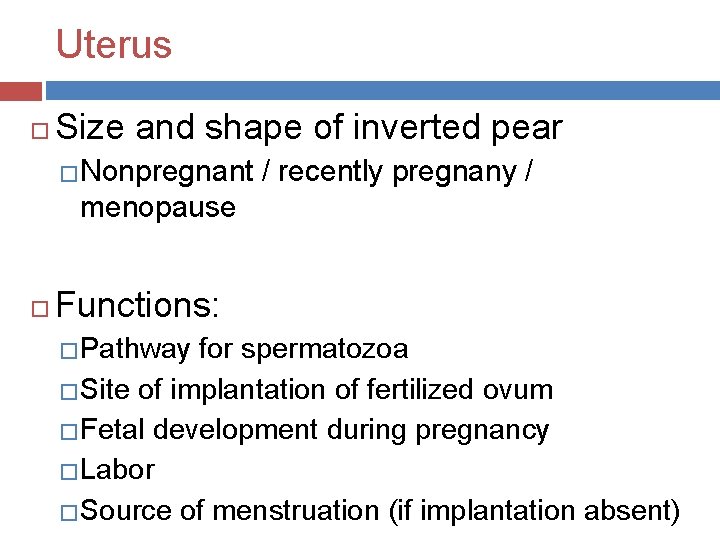
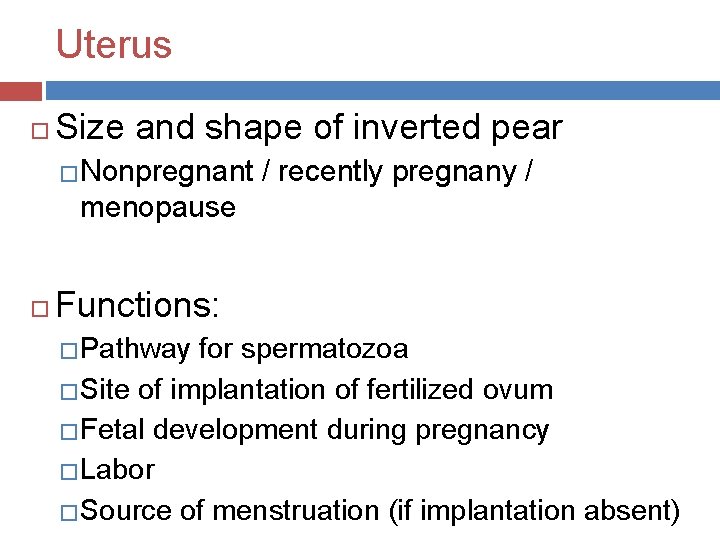
Uterus Size and shape of inverted pear �Nonpregnant / recently pregnany / menopause Functions: � Pathway for spermatozoa � Site of implantation of fertilized ovum � Fetal development during pregnancy � Labor � Source of menstruation (if implantation absent)

Uterus Anatomy �Fundus �Body Uterine cavity �Isthmus �Cervix (opens into vagina) Cervical canal �Normally anteflexed – anterior & superior over bladder �Ligaments maintain position – broad and
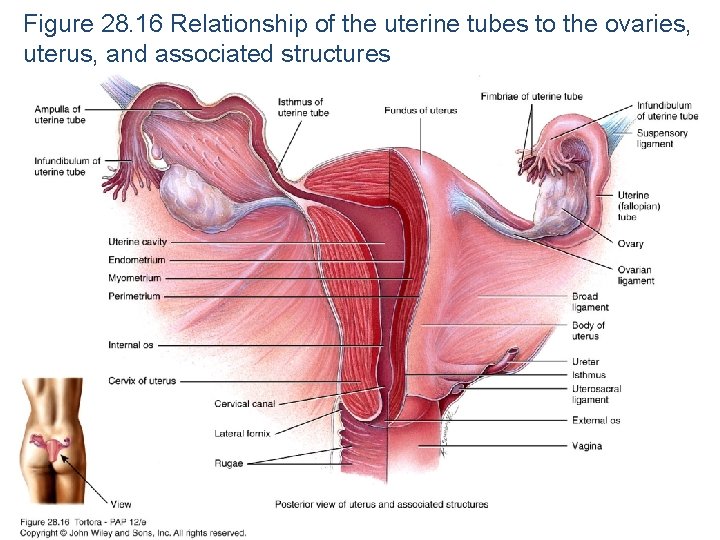
Figure 28. 16 Relationship of the uterine tubes to the ovaries, uterus, and associated structures
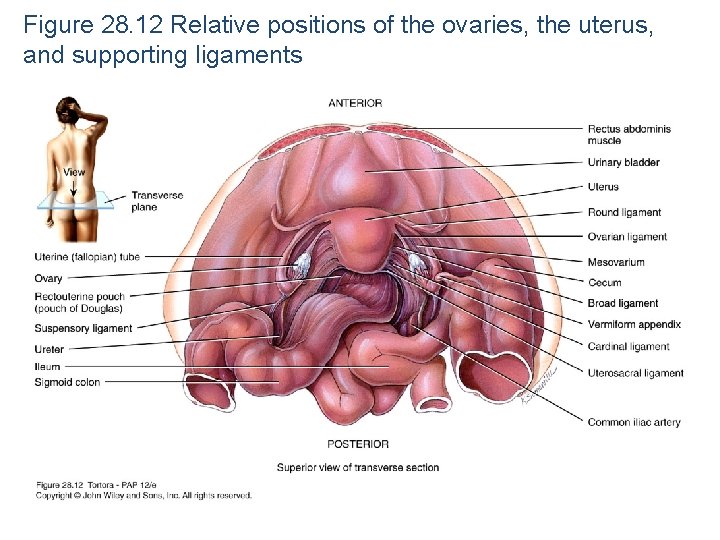
Figure 28. 12 Relative positions of the ovaries, the uterus, and supporting ligaments
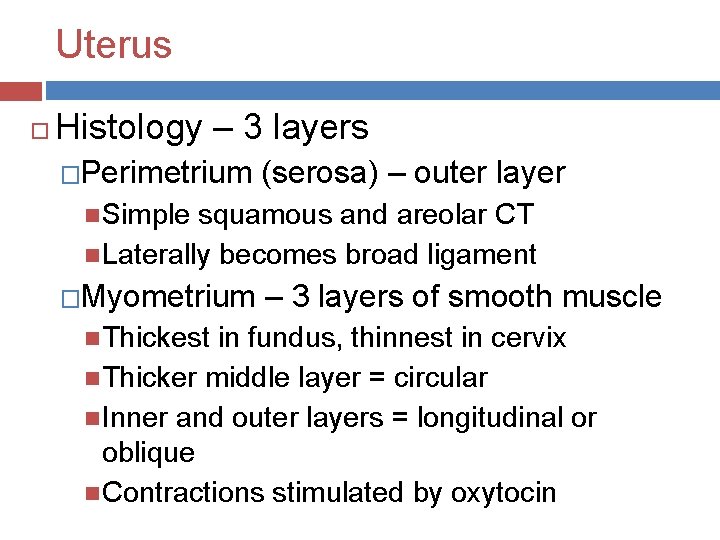
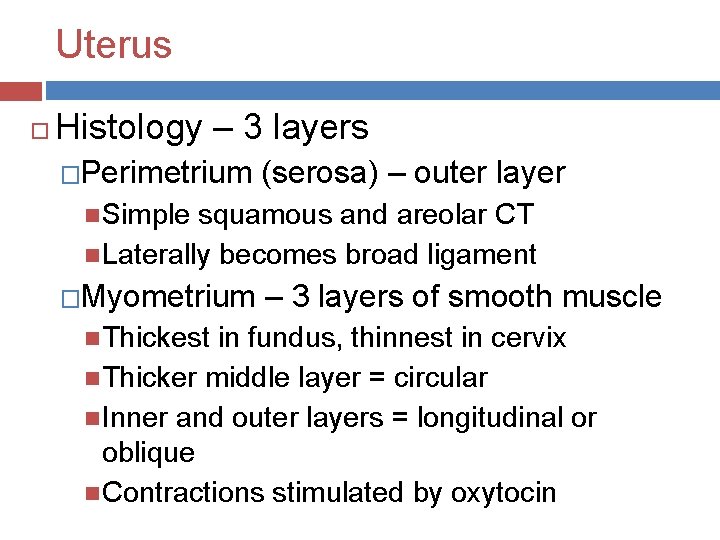
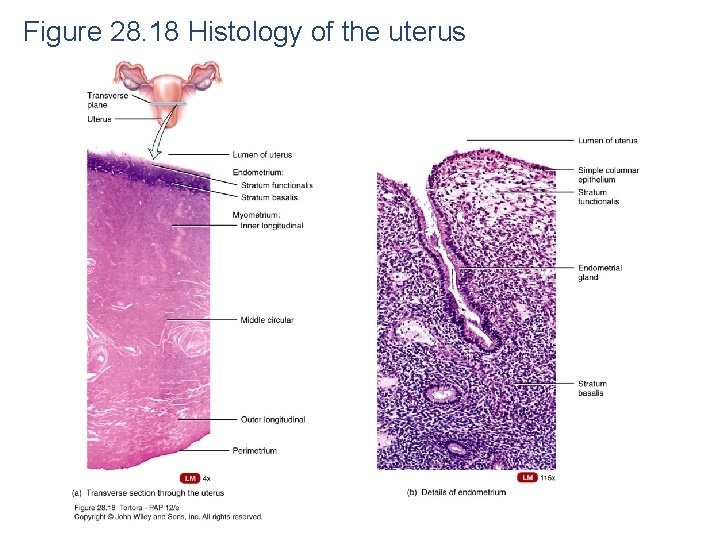
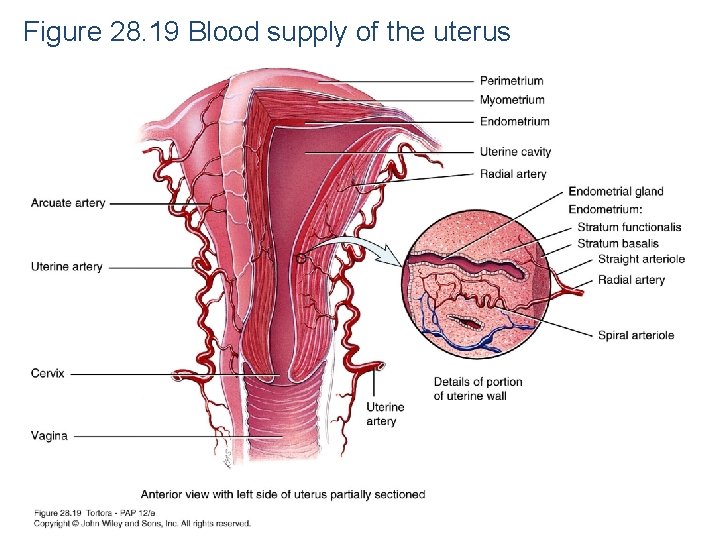
Uterus Histology – 3 layers �Perimetrium (serosa) – outer layer Simple squamous and areolar CT Laterally becomes broad ligament �Myometrium – 3 layers of smooth muscle Thickest in fundus, thinnest in cervix Thicker middle layer = circular Inner and outer layers = longitudinal or oblique Contractions stimulated by oxytocin
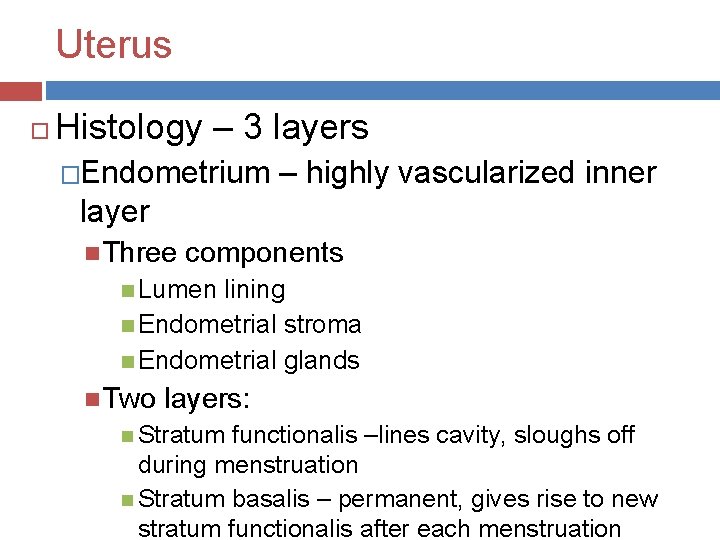
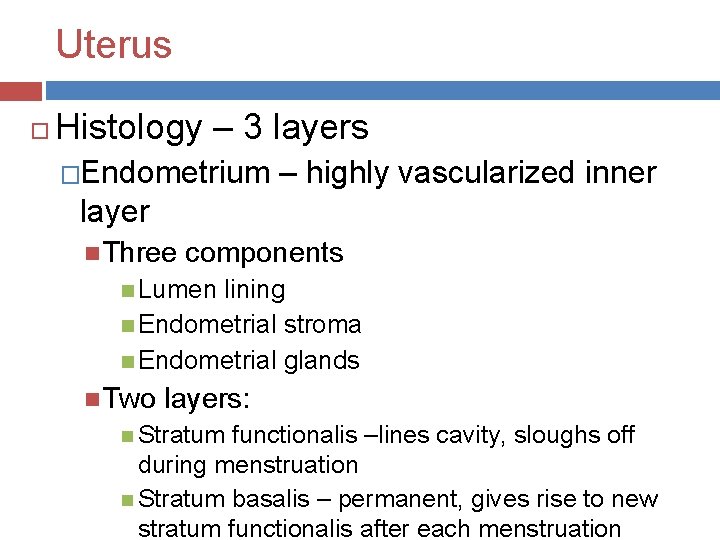
Uterus Histology – 3 layers �Endometrium – highly vascularized inner layer Three components Lumen lining Endometrial stroma Endometrial glands Two layers: Stratum functionalis –lines cavity, sloughs off during menstruation Stratum basalis – permanent, gives rise to new stratum functionalis after each menstruation
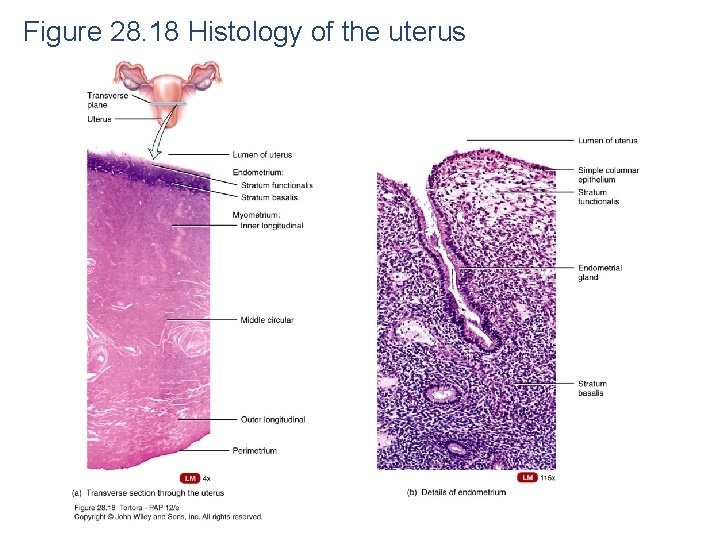
Figure 28. 18 Histology of the uterus
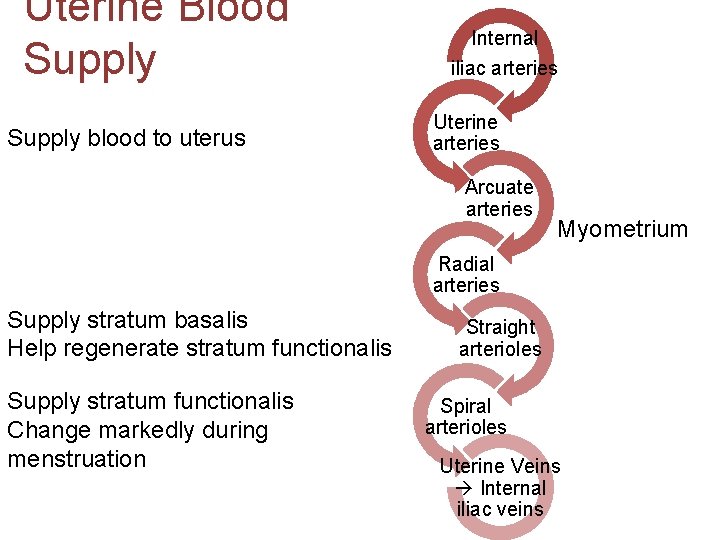
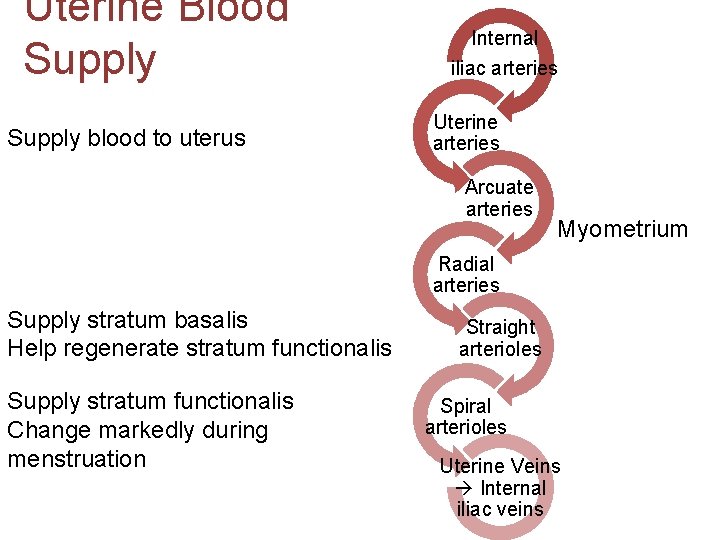
Uterine Blood Supply blood to uterus Internal iliac arteries Uterine arteries Arcuate arteries Myometrium Radial arteries Supply stratum basalis Help regenerate stratum functionalis Supply stratum functionalis Change markedly during menstruation Straight arterioles Spiral arterioles Uterine Veins Internal iliac veins
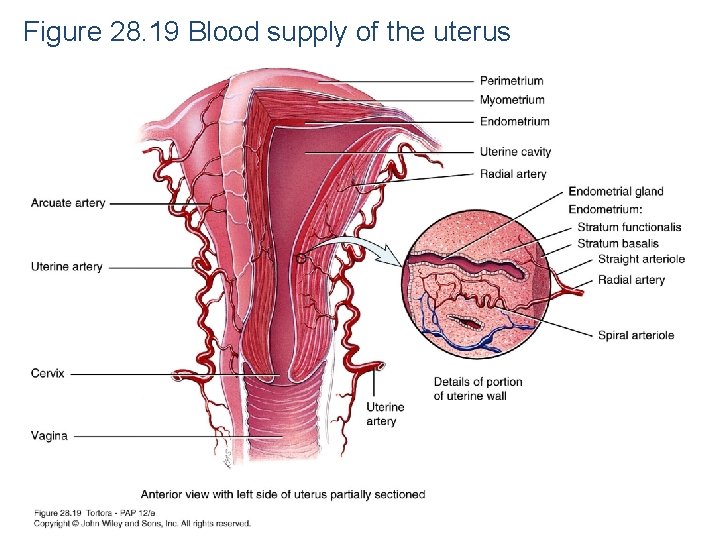
Figure 28. 19 Blood supply of the uterus
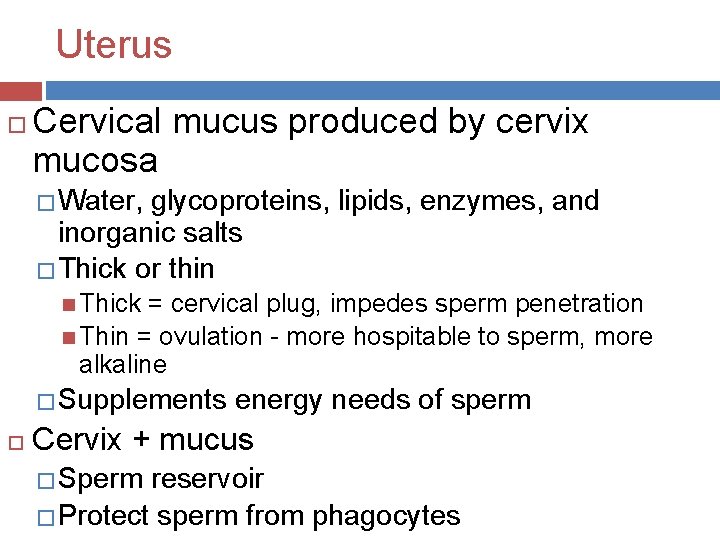
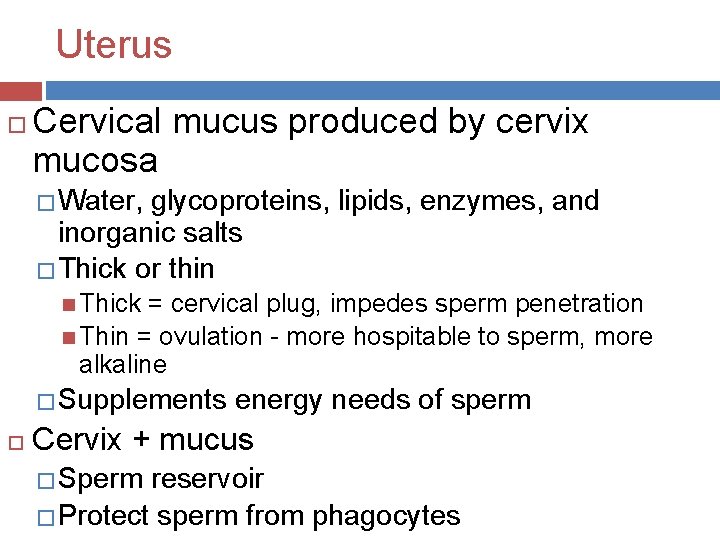
Uterus Cervical mucus produced by cervix mucosa � Water, glycoproteins, lipids, enzymes, and inorganic salts � Thick or thin Thick = cervical plug, impedes sperm penetration Thin = ovulation - more hospitable to sperm, more alkaline � Supplements energy needs of sperm Cervix + mucus � Sperm reservoir � Protect sperm from phagocytes
Wednesday Notes on the vagina, vulva, perineum, mammary glands. Begin the female reproductive cycle. Clarification from Jason on follicular anatomy: theca follicula (theca interna / externa) zona pellucida stromal cells corona radiata basement membrane antrum follicular cells to granulosa cells Friday – lab period (maybe start lecture………. ) � Reminder female and male repro labs + RYK are due at the end of class Friday Monday – start our last topic
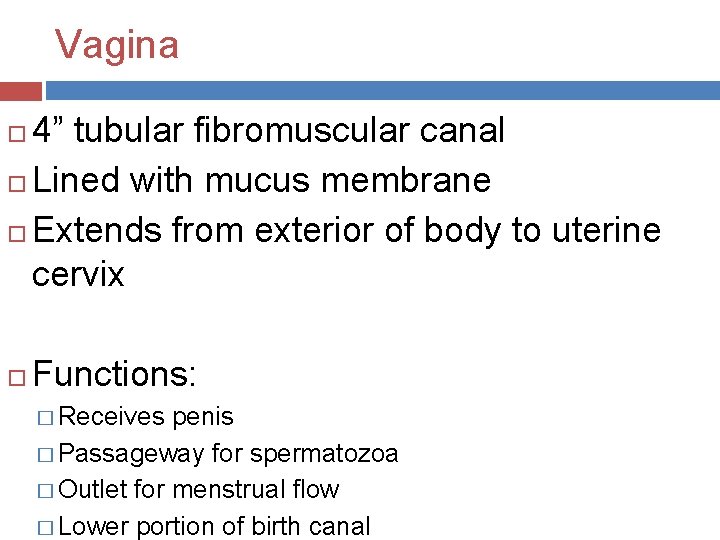
Vagina 4” tubular fibromuscular canal Lined with mucus membrane Extends from exterior of body to uterine cervix Functions: � Receives penis � Passageway for spermatozoa � Outlet for menstrual flow � Lower portion of birth canal
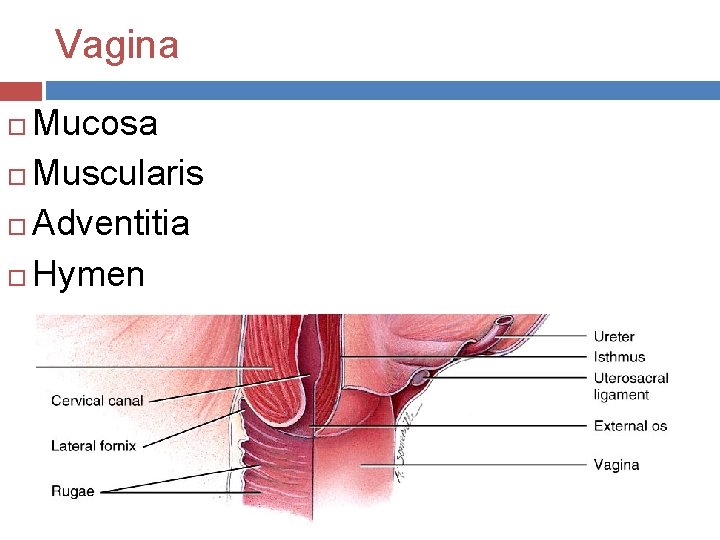
Vagina Mucosa Muscularis Adventitia Hymen
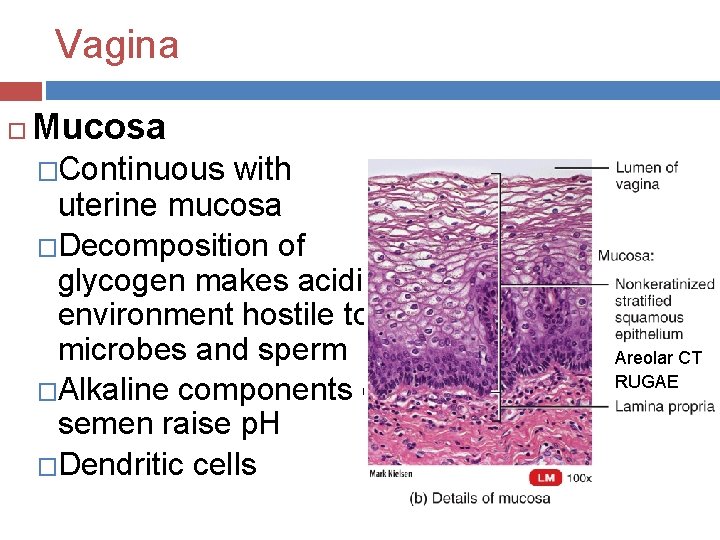
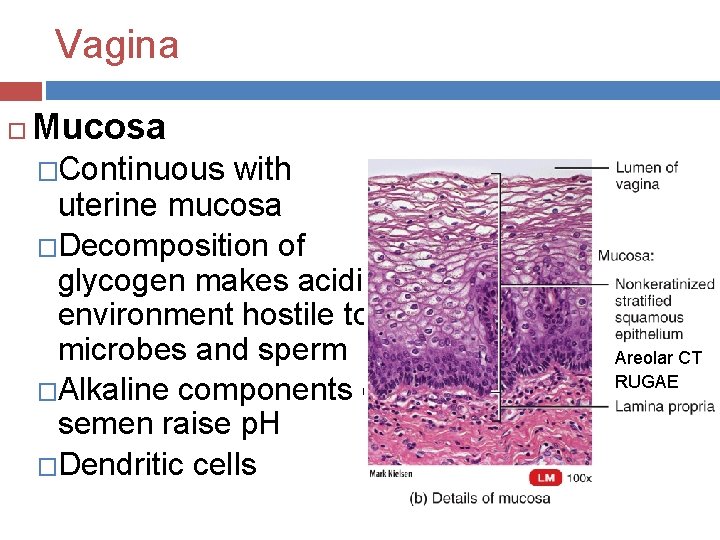
Vagina Mucosa �Continuous with uterine mucosa �Decomposition of glycogen makes acidic environment hostile to microbes and sperm �Alkaline components of semen raise p. H �Dendritic cells Areolar CT RUGAE
Vagina Muscularis � Smooth muscle � Outer circular layer & inner longitudinal layer � Stretchy Adventitia � Superficial layer – areolar CT � Anchors vagina to adjacent organs Hymen � Thin fold of vascularized mucous membrane
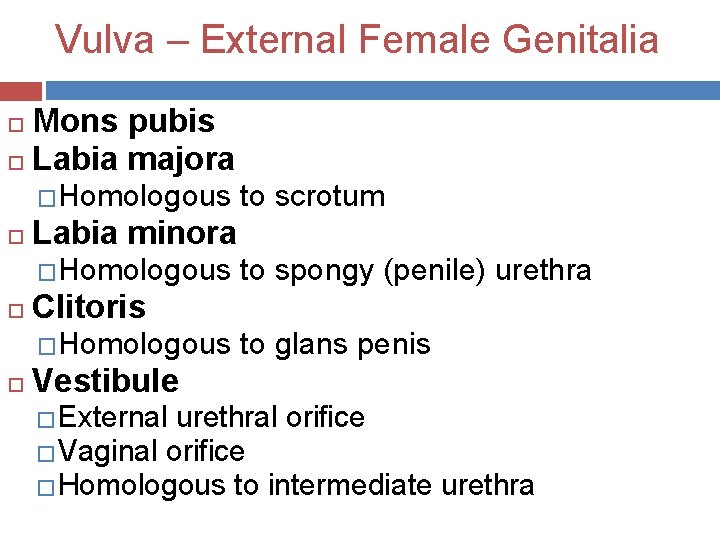
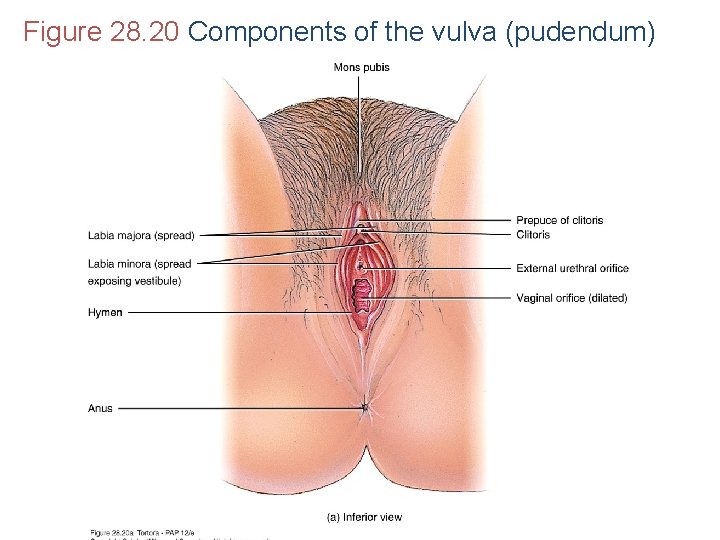
Vulva – External Female Genitalia Mons pubis Labia majora �Homologous to scrotum Labia minora �Homologous to spongy (penile) urethra Clitoris �Homologous to glans penis Vestibule �External urethral orifice �Vaginal orifice �Homologous to intermediate urethra
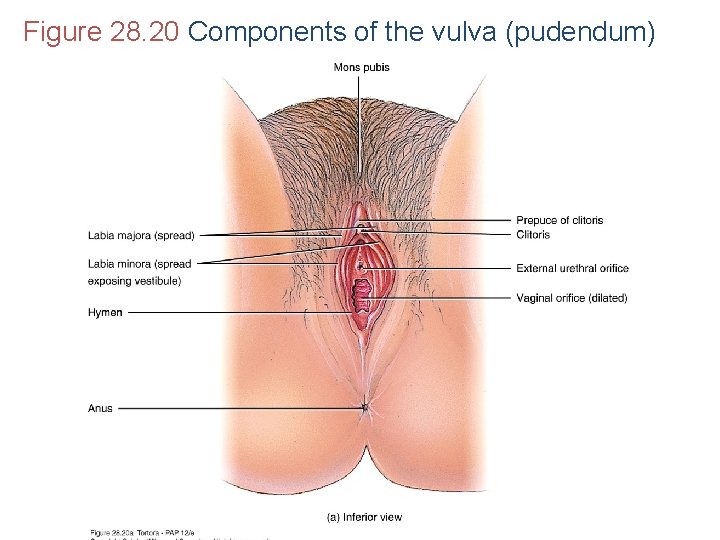
Figure 28. 20 Components of the vulva (pudendum)

Vulva – External Female Genitalia Hymen Paraurethral (Skene’s) gland �Homologous to prostate Greater vestibular (Bartholin’s) gland �Homologous to bulbourethral glands Lesser vestibular gland Bulb of the vestibule �Homologous to corpus spongiosum and bulb of penis
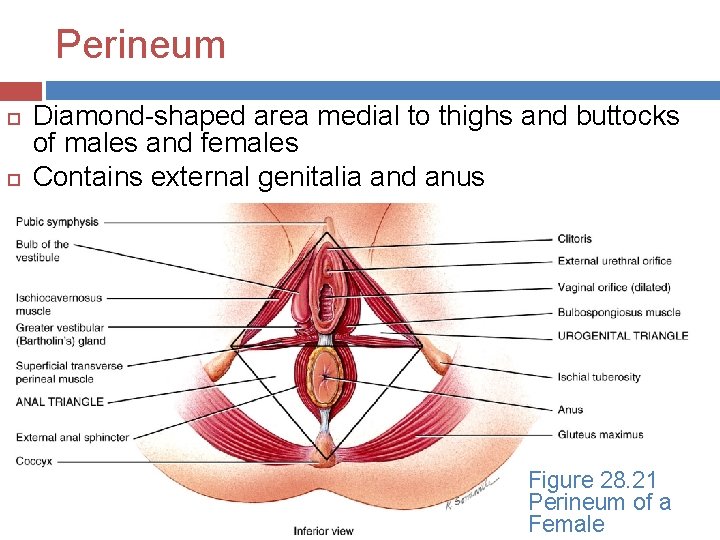
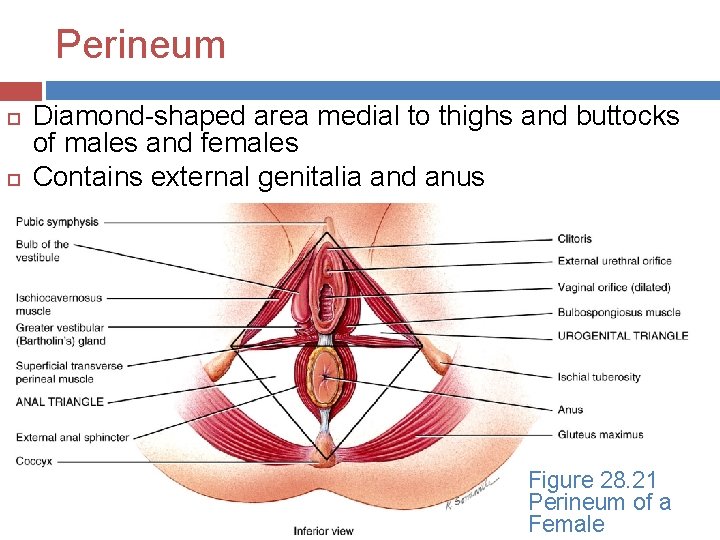
Perineum Diamond-shaped area medial to thighs and buttocks of males and females Contains external genitalia and anus Figure 28. 21 Perineum of a Female
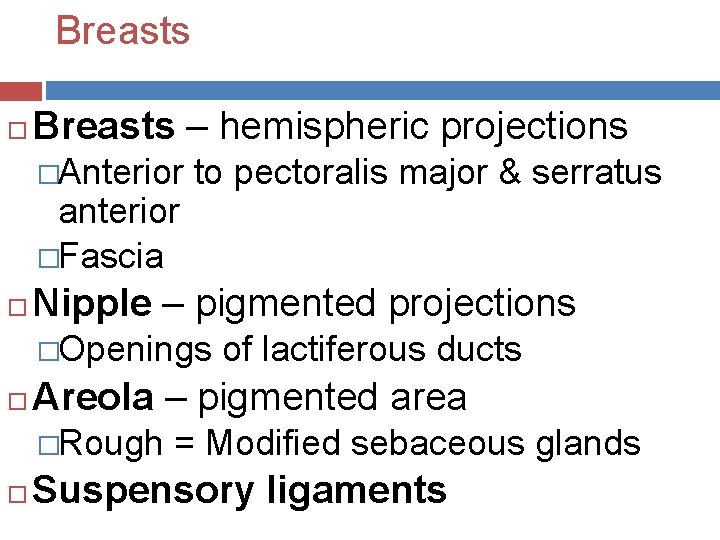
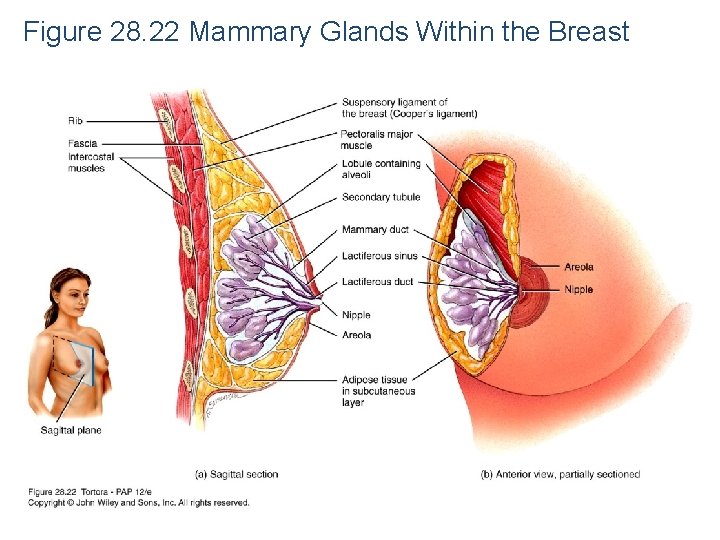
Breasts – hemispheric projections �Anterior to pectoralis major & serratus anterior �Fascia Nipple – pigmented projections �Openings of lactiferous ducts Areola – pigmented area �Rough = Modified sebaceous glands Suspensory ligaments

Mammary glands Mammary gland – modified sudoriferous gland that produces milk � 15 -20 lobes separated by adipose tissue �Lobes divided into lobules �Lobules composed of alveoli (milk-secreting glands) �Myoepithelial cells Synthesis, secretion & ejection of milk = lactation �Prolactin (ant. pit. ) & oxytocin (post. pit. )
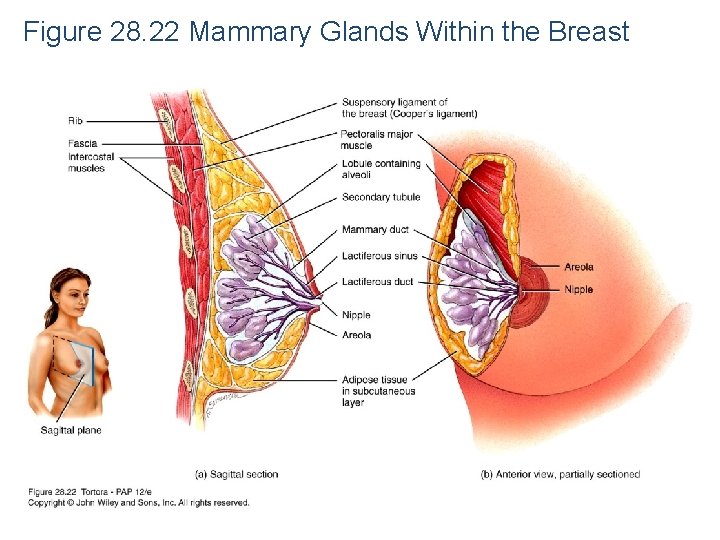
Figure 28. 22 Mammary Glands Within the Breast

FEMALE REPRODUCTIVE CYCLE
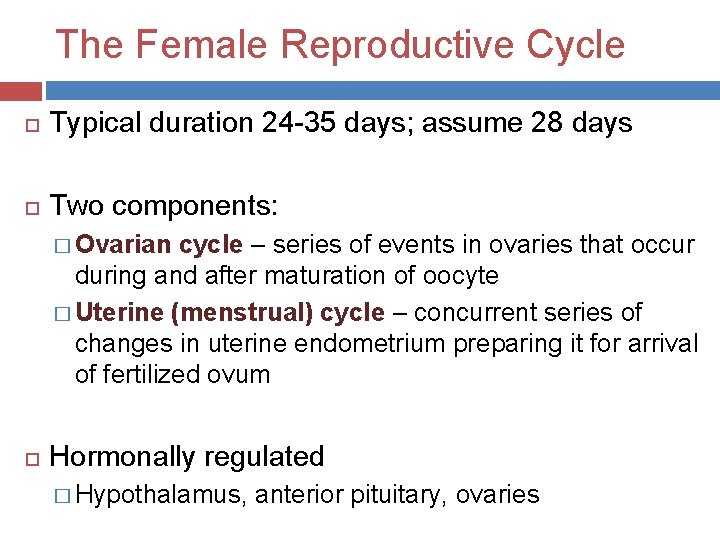
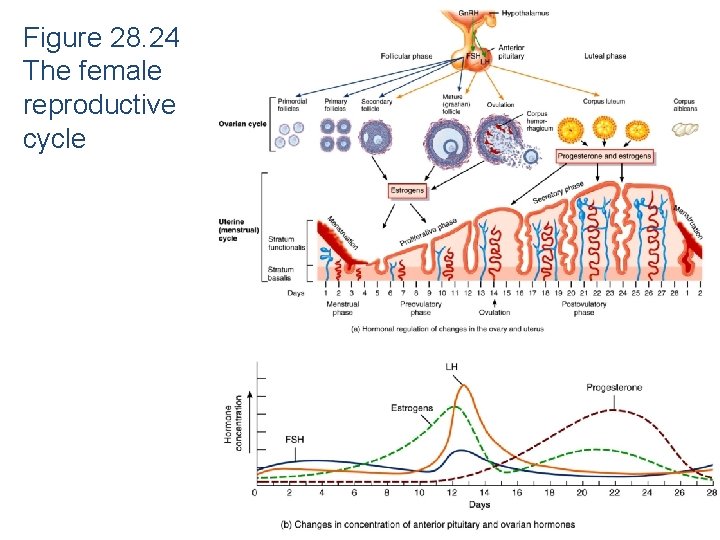
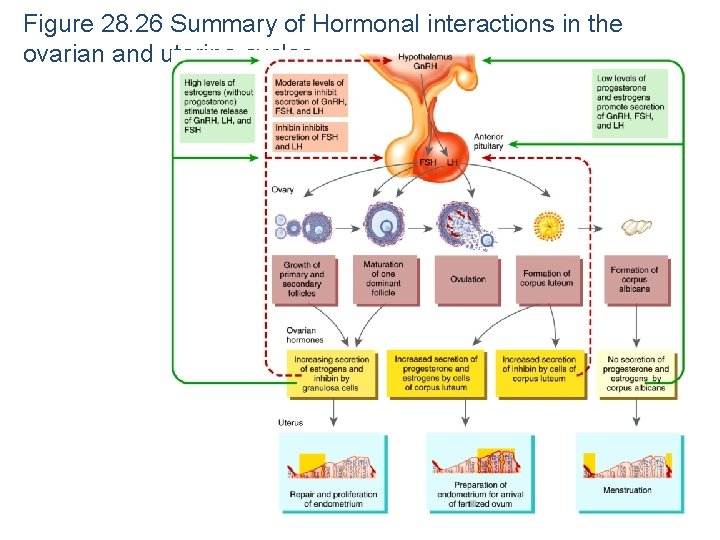
The Female Reproductive Cycle Typical duration 24 -35 days; assume 28 days Two components: � Ovarian cycle – series of events in ovaries that occur during and after maturation of oocyte � Uterine (menstrual) cycle – concurrent series of changes in uterine endometrium preparing it for arrival of fertilized ovum Hormonally regulated � Hypothalamus, anterior pituitary, ovaries
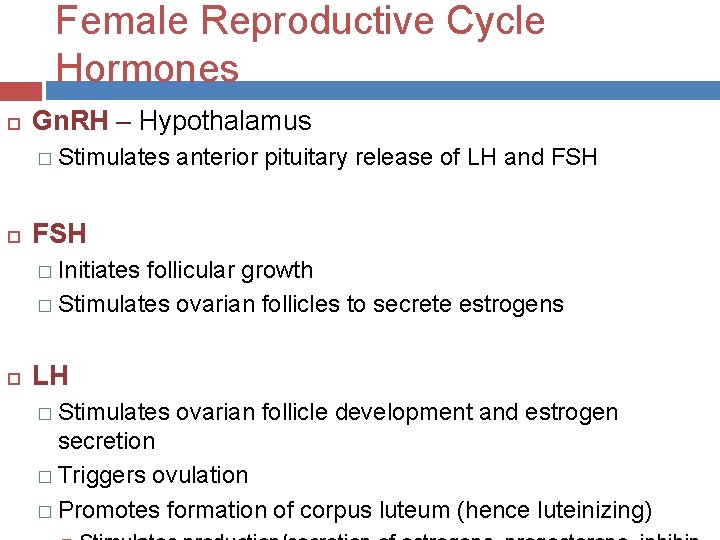
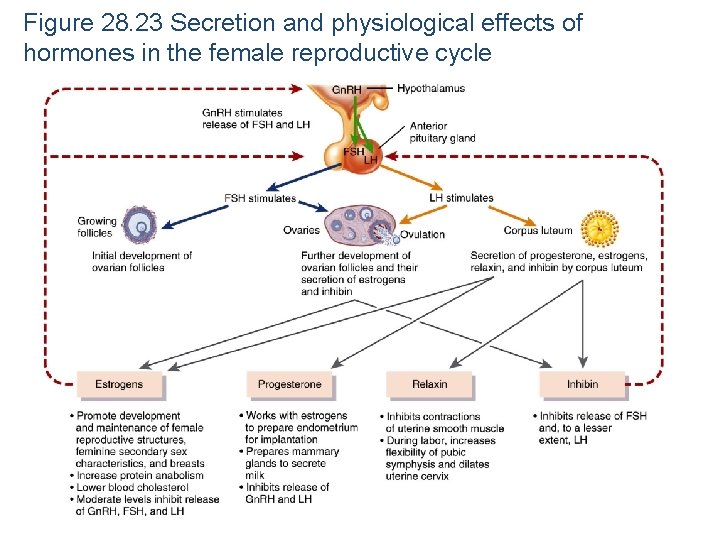
Female Reproductive Cycle Hormones Gn. RH – Hypothalamus � Stimulates anterior pituitary release of LH and FSH � Initiates follicular growth � Stimulates ovarian follicles to secrete estrogens LH � Stimulates ovarian follicle development and estrogen secretion � Triggers ovulation � Promotes formation of corpus luteum (hence luteinizing)
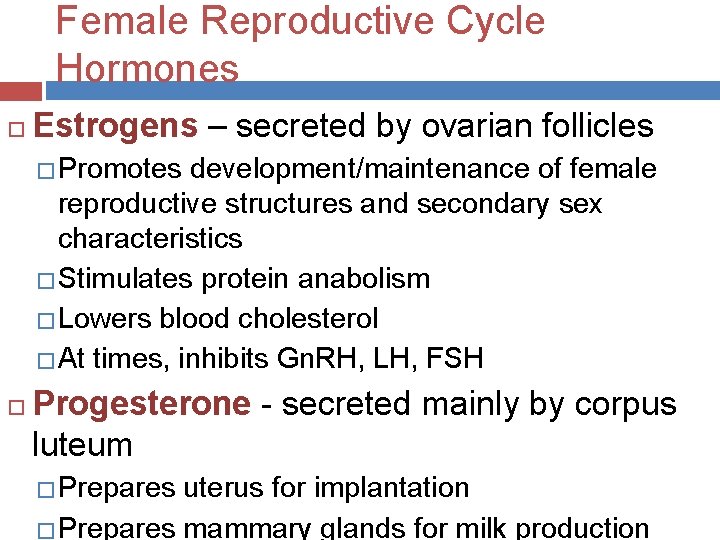
Female Reproductive Cycle Hormones Estrogens – secreted by ovarian follicles � Promotes development/maintenance of female reproductive structures and secondary sex characteristics � Stimulates protein anabolism � Lowers blood cholesterol � At times, inhibits Gn. RH, LH, FSH Progesterone - secreted mainly by corpus luteum � Prepares uterus for implantation � Prepares mammary glands for milk production
Female Reproductive Cycle Hormones Relaxin - produced by corpus luteum �Inhibits uterine contraction �Increases flexibility of pubic symphysis �Dilates uterine cervix Inhibin – produced by follicles and corpus luteum �Inhibits secretion of FSH and LH
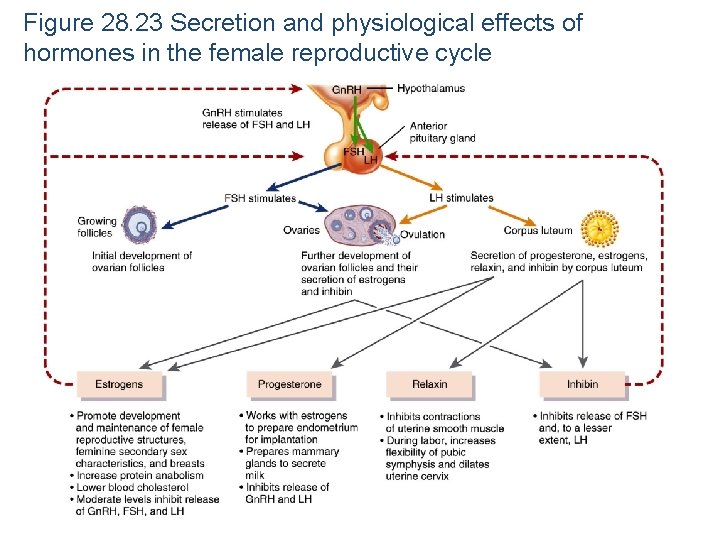
Figure 28. 23 Secretion and physiological effects of hormones in the female reproductive cycle

Female Reproductive Cycle Phases 1. Menstrual phase Day 1 -5 2. Preovulatory phase Day 6 -13 3. Ovulation Day 14 4. Postovulatory phase Day 15 -28
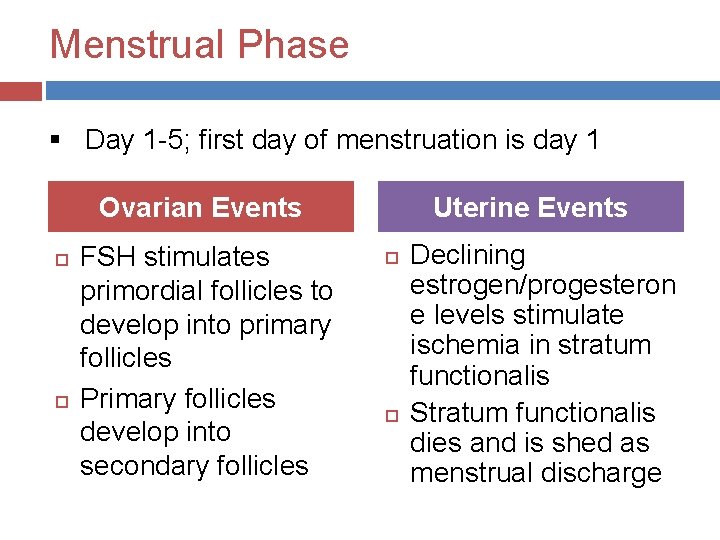
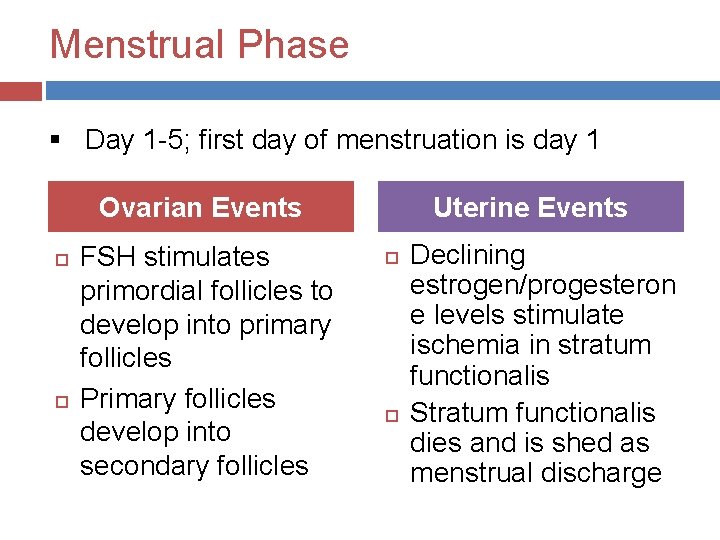
Menstrual Phase § Day 1 -5; first day of menstruation is day 1 Ovarian Events FSH stimulates primordial follicles to develop into primary follicles Primary follicles develop into secondary follicles Uterine Events Declining estrogen/progesteron e levels stimulate ischemia in stratum functionalis Stratum functionalis dies and is shed as menstrual discharge

Preovulatory Phase § Day 6 -13 Ovarian Events Secondary follicles secrete estrogen and inhibin One secondary follicle becomes dominant and develops into a mature follicle Uterine Events Rising estrogen levels stimulate growth of stratum functionalis Referred to as proliferative phase
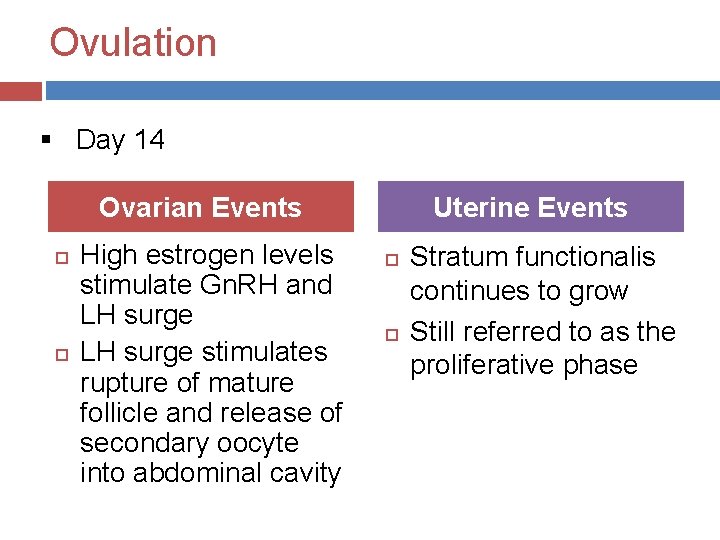
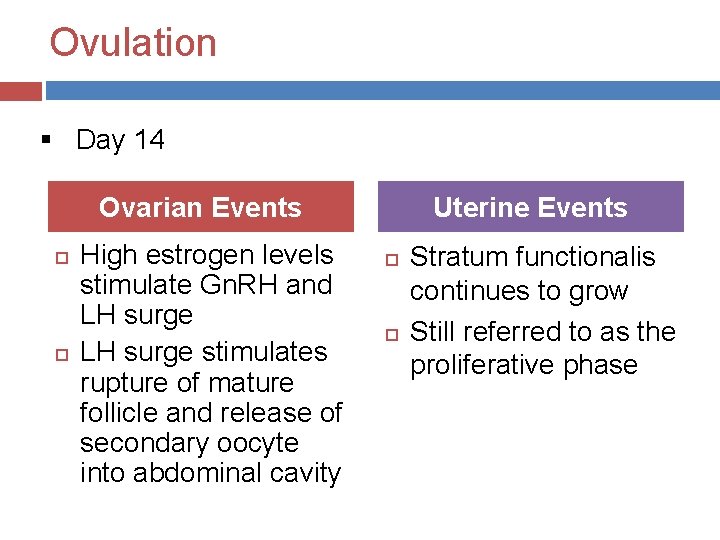
Ovulation § Day 14 Ovarian Events High estrogen levels stimulate Gn. RH and LH surge stimulates rupture of mature follicle and release of secondary oocyte into abdominal cavity Uterine Events Stratum functionalis continues to grow Still referred to as the proliferative phase
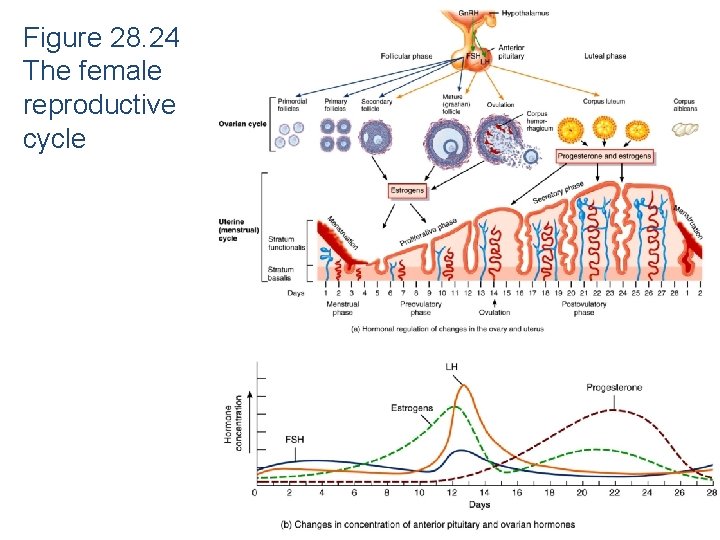
Figure 28. 24 The female reproductive cycle
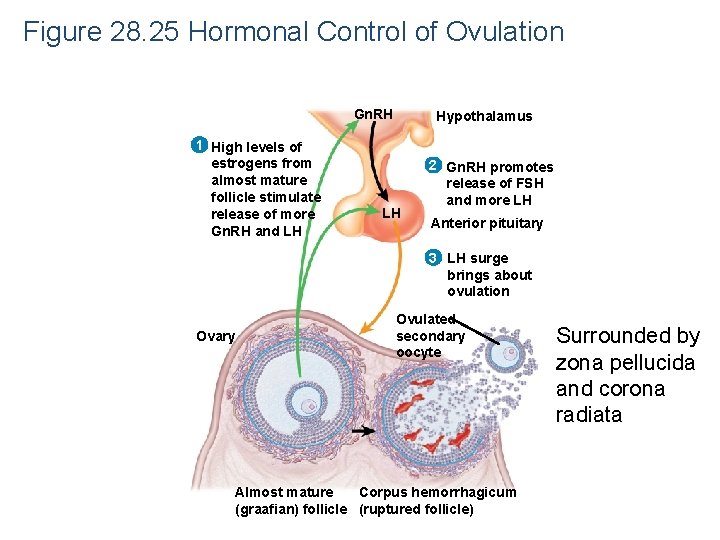
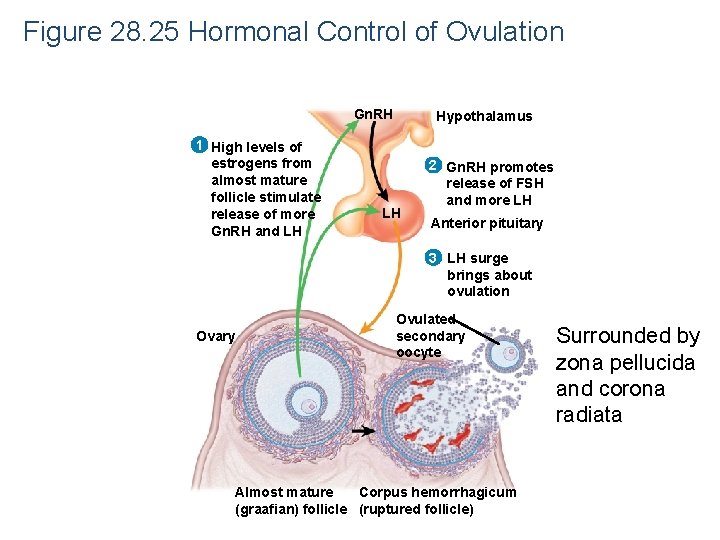
Figure 28. 25 Hormonal Control of Ovulation Gn. RH 1 High levels of estrogens from almost mature follicle stimulate release of more Gn. RH and LH Hypothalamus LH 2 Gn. RH promotes release of FSH and more LH Anterior pituitary 3 LH surge brings about ovulation Ovary Ovulated secondary oocyte Almost mature Corpus hemorrhagicum (graafian) follicle (ruptured follicle) Surrounded by zona pellucida and corona radiata
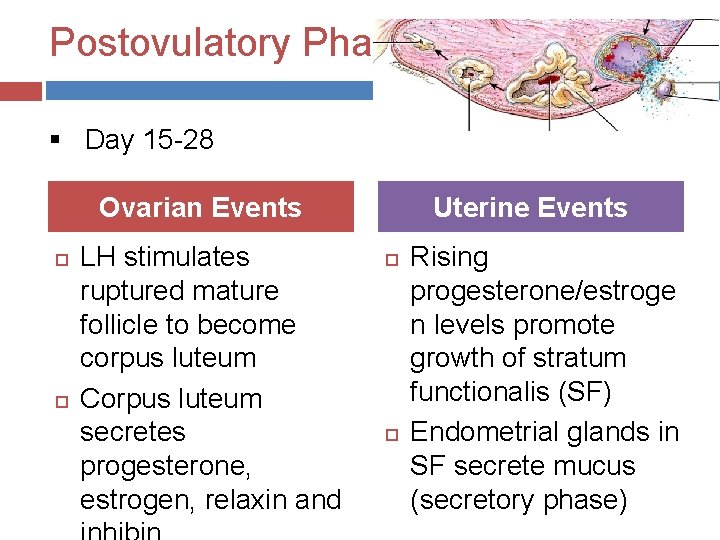
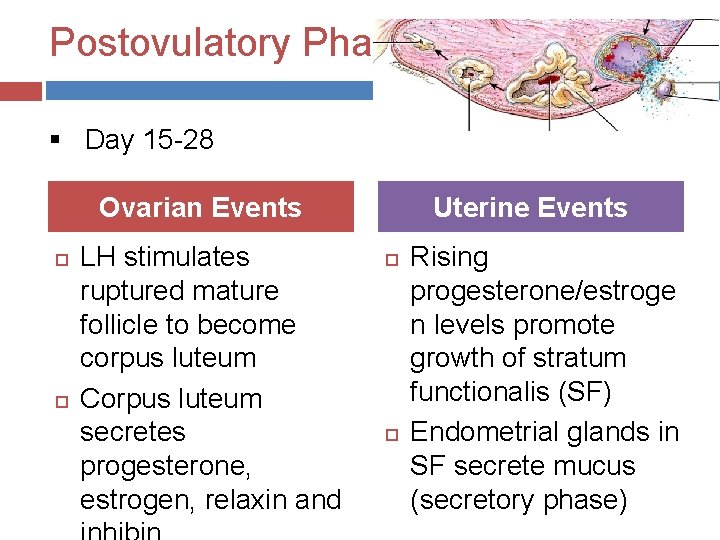
Postovulatory Phase § Day 15 -28 Ovarian Events LH stimulates ruptured mature follicle to become corpus luteum Corpus luteum secretes progesterone, estrogen, relaxin and Uterine Events Rising progesterone/estroge n levels promote growth of stratum functionalis (SF) Endometrial glands in SF secrete mucus (secretory phase)

What Happens if the Oocyte is NOT Fertilized? In ovary � Corpus luteum lifespan = 2 weeks � Corpus luteum degenerates into corpus albicans � Progesterone and estrogen levels drop � Gn. RH levels rise � Gn. RH stimulates FSH/LH release; follicular growth resumes � A new cycle begins In uterus � Decreased progesterone/estrogen levels stimulate
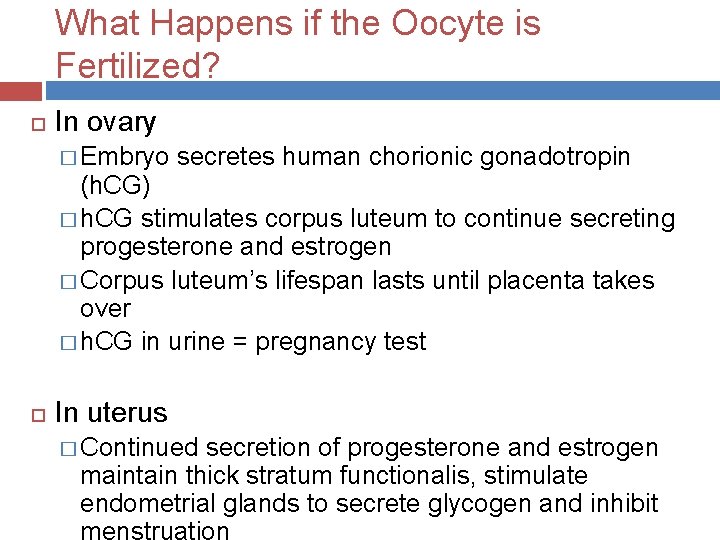
What Happens if the Oocyte is Fertilized? In ovary � Embryo secretes human chorionic gonadotropin (h. CG) � h. CG stimulates corpus luteum to continue secreting progesterone and estrogen � Corpus luteum’s lifespan lasts until placenta takes over � h. CG in urine = pregnancy test In uterus � Continued secretion of progesterone and estrogen maintain thick stratum functionalis, stimulate endometrial glands to secrete glycogen and inhibit
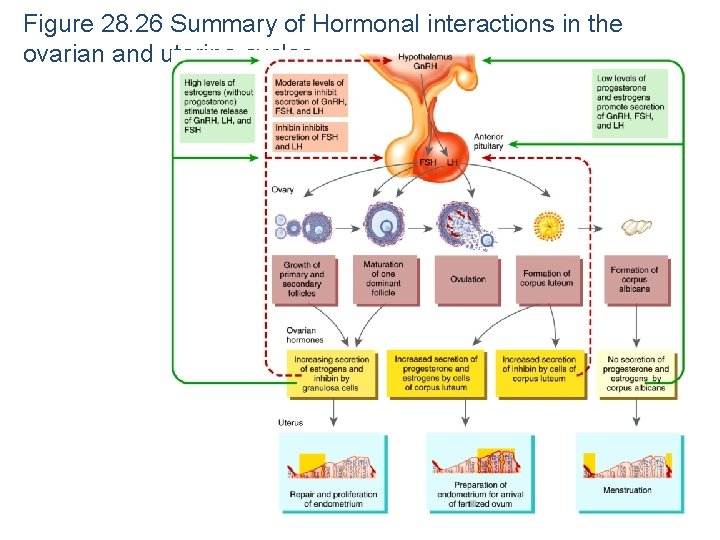
Figure 28. 26 Summary of Hormonal interactions in the ovarian and uterine cycles