Fluid and Macronutrients Aim Contents Fluids and fluid







- Slides: 69
Fluid and Macronutrients
Aim
Contents • Fluids and fluid balance • Carbohydrates • Fats • Proteins
Fluid balance is essential to life Fluid: • Acts as a solvent for ions and molecules • Acts as a transport medium • Acts a a lubricant • Regulates body temperature
Body water 1. Intracellular 2. Extracellular • Interstitial fluid • Plasma volume Focus on extracellular when providing clinical care
Regulation of fluid balance • Under very tight homeostatic control • Total volume fluctuates by less than 1%/day • Changes of 1 -2% can lead to illness and death
What affects fluid movement? • Variety of sensitive and highly complex mechanisms • Osmosis and hydrostatic pressure gradients • Sodium and Potassium • Normally – osmolality of plasma and interstitial fluids are equal
Plasma osmolality • Key factor in determining fluid movements • Slight changes in osmolality corrected by moving fluid between interstitial compartment and plasma • If osmolality increases- hypothalamus stimulated by thirst and increased ADH released • See reabsobtion of water from distal renal tubules and correction of osmolality • Decreased plasma volume also leads to rise in osmolality- Aldosterone is released resulting in increased Sodium and water retention
Important Clinical points • Renal function is key factor in regulation of fluid balance – impairment characterised by oedema • Thirst and age • Severely disturbed osmolality or volume depletion lead to the movement of fluid between intracellular and extracellular components – has fatal consequences if not treated promptly
Factors affecting fluid balance Fluid and Food intake – Healthy adult body requires approx: 3 L / day – 1. 5 L from fluid – 1 L from food – 300 ml metabolic processes
Fluid output Controlled by kidneys – plus “insensible” losses from skin, lungs and Gastrointestinal tract (GI) • Lungs – 400 ml lost / day in normal respiration (consider patients with hyperventilation) • Skin – lose 500 -750 ml / day normally ( increases when BMR increases In pyrexia – for every 1 degree rise in body temp need additional 500 ml / day • GI – loses high in diarrhoea and vomiting (short bowel syndrome)
Fluid requirements • Minimum intake – to replace all losses and provide adequate dilution for excretion of solutes via kidneys • Maximum intake from oral liquids – that which kidneys can excrete
Monitoring Fluid Balance • Important consideration in assessment of all patients • Fluid status of some patients will need very close monitoring (input and output charts and evaluation of blood – particularly Sodium and osmolality)
People at Risk of negative fluid balance (dehydration) • Critically ill • Patients given inappropriate nutritional or hydration support • Acute dehydration –in high fluid losses (life threatening in young children and frail elderly) • Chronic dehydration – results in constipation, headaches, lethargy, mental confusion and Urinary tract infections
Chronic dehydration
Fluid overload • Impaired cardiac , hepatic or renal function • Fluid restriction integral part of treatment
Fluids – the acute medical perspective • Renal function • Constipation • Urinary tract infections • Glycaemia
Fluids in hospital • 6 cups of tea / coffee (180 ml each) • Water jug
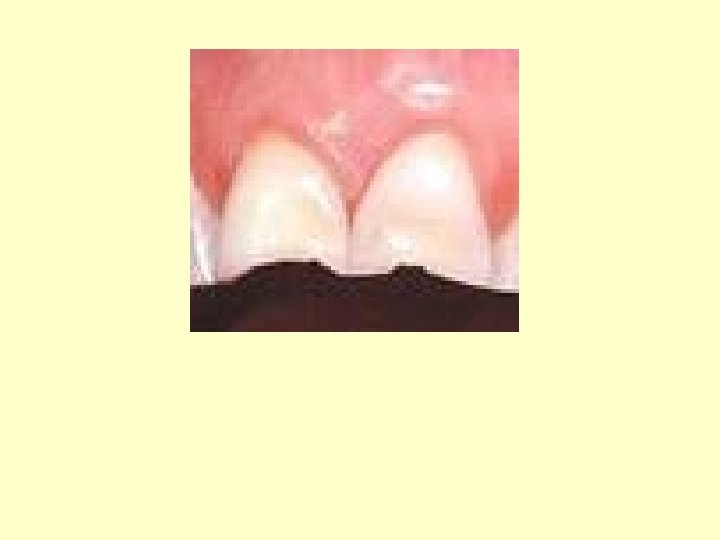
Fluids – the public health medicine perspective • Obesity • Dental health • Cancer • Osteoporosis

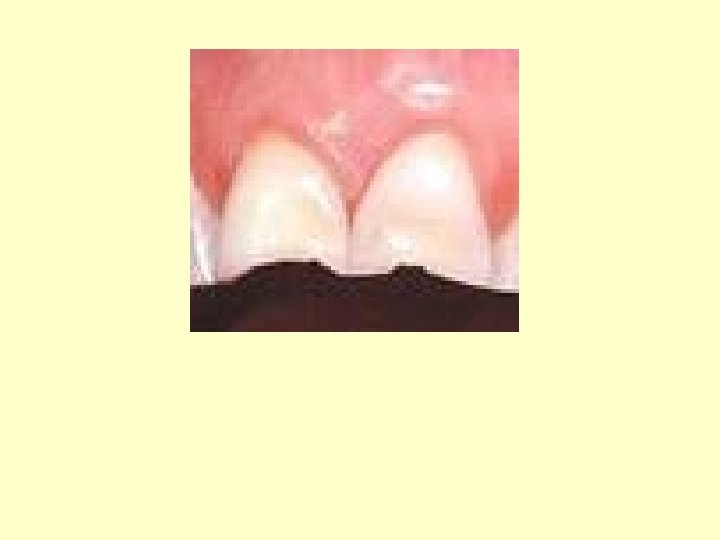
Fluids – some specifics • Water (flat and plain) and milk • Fruit juice based • Carbonated drinks • Milk shakes • Tea and coffee

Personal clinical favourites
A quick recap….
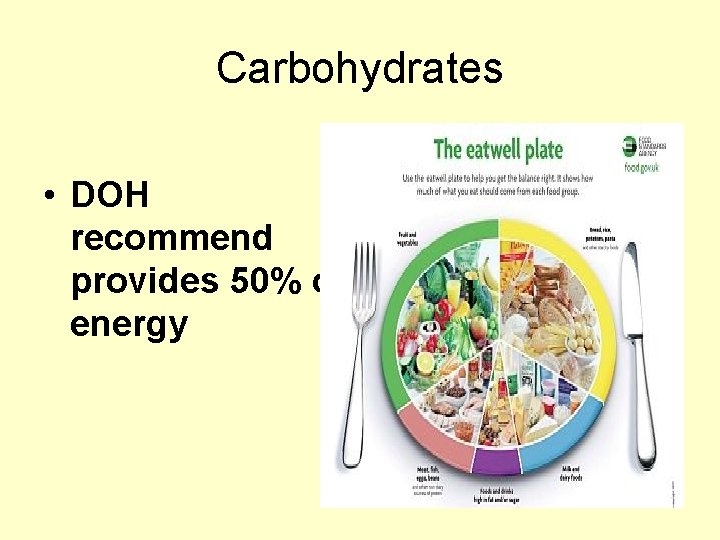
Carbohydrates • DOH recommend provides 50% of energy
Function of Carbohydrates • Energy – all carbs converted into glucose • Glucose vital fuel substrate for all body tissues (especially brain) • Blood glucose levels tightly maintained to meet fuel demands
After eating carbohydrate… • Blood glucose levels rise • Increased production of insulin • Increased cellular uptake of glucose • In body cells glucose oxidised as source of energy • Surplus glucose stored as glycogen – in liver and skeletal muscle • When glycogen stores saturated – glucose converted to fat and stored in adipose tissue
Dietary carbohydrates • Produced by plant synthesis of carbon dioxide and water (glucose) • Glucose converted into other sugars and starches (provide energy) • Glucose converted into cellulose and other non-starch polysaccharides (structure)
Available dietary carbohydrate 1. Sugars -Monosaccharide's (glucose, fructose and galactose) - Disaccharides (sucrose, lactose and maltose) 2. Starches (polysacharides)

Non-starch Polysacharides • Viscous polysaccharides blunt post prandial blood glucose responses • Viscous polysaccharides reduce total cholesterol (reduce LDL component) • Reduce gut transit time and increase stool weight
Foods high in NSP • Peas, beans, lentils • Sprouts, parsnips, spring greens • Granary, wholemeal bread and rye bread • Wholemeal pasta • Muesli and bran based breakfast cereals

Health implications of Carbohydrates • “Natural” sugars (fruit, veg and milk ) Contain vitamin C, beta-carotene, calcium and soluble fibre) • Starches – B vitamins, minerals, protein and fibre • “unnatural” sugars – fat and calories!
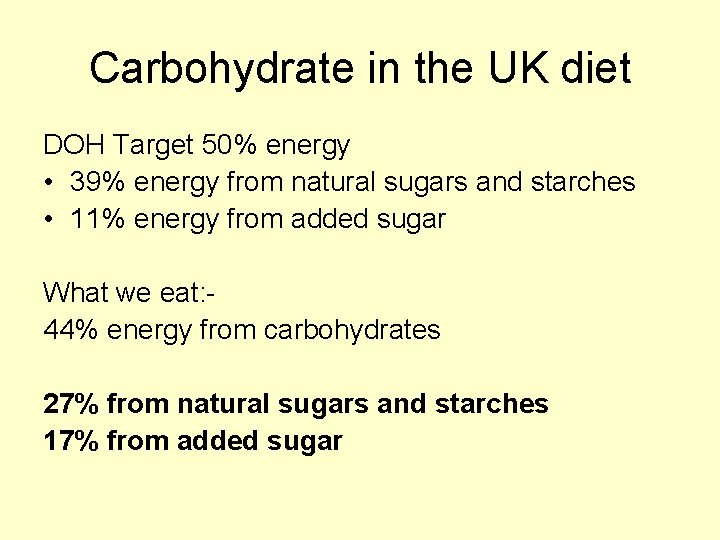
Carbohydrate in the UK diet DOH Target 50% energy • 39% energy from natural sugars and starches • 11% energy from added sugar What we eat: 44% energy from carbohydrates 27% from natural sugars and starches 17% from added sugar
Carbohydrates the acute medical perspective • Diabetes mellitus – dose of hypoglycaemic agents is tailored to intake of starches and natural sugars • Constipation • Carbohydrate intolerances – lactose intolerance, sucrose intolerance, starch intolerance, monosaccharide intolerances
Carbohydrates the acute medical perspective • Easily absorbed and palatable calories • Number of “supplements” available • Oral hygiene is important
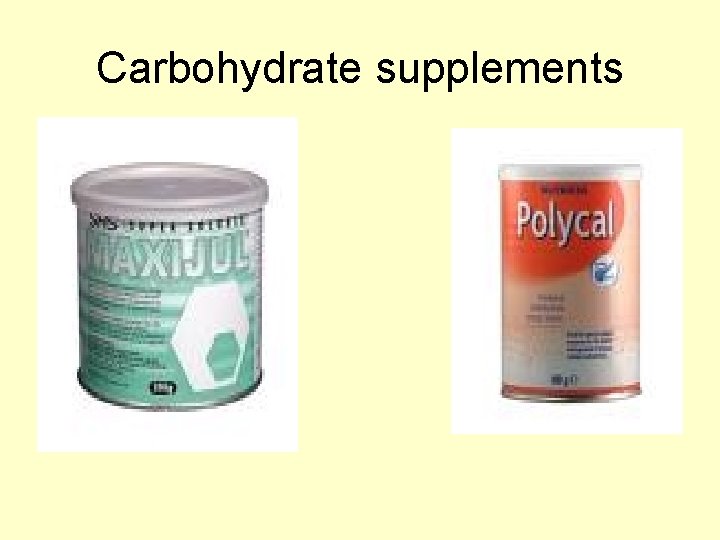
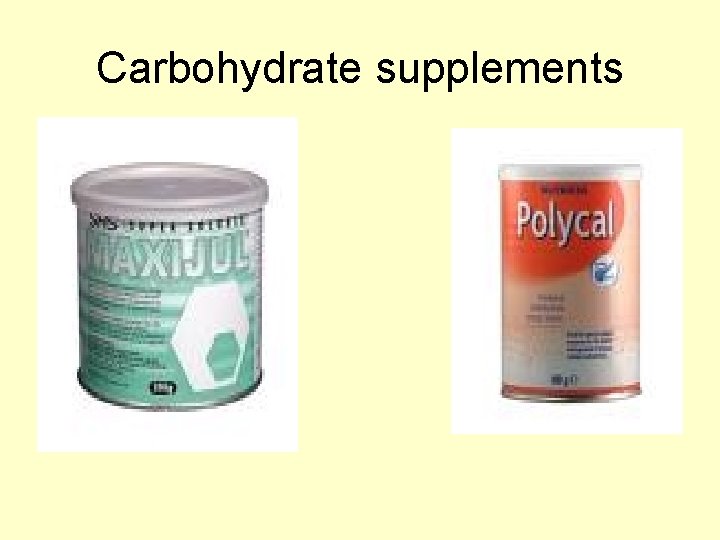
Carbohydrate supplements
Carbohydrates the public health medicine perspective • Obesity • Cancer • Constipation (fluid) • Oral health
A quick recap
Dietary Fats • DOH recommend 35% daily kcal's from fat 13% from monounsaturated fat 6% from polyunsaturated 11%from saturated fat We eat 40% daily calories from fat 12% from monounsaturated fat 6% from polyunsaturated 17%from saturated fat

Function of fats • Fuel for cells • Providing essential fatty acids • As a carrier for fat soluble vitamins • Insulation against heat loss • Providing a protective layer around essential organs • A structural component of brain tissue and myelin sheaths • Forming phospholipids • Substrate for hormone and prostaglandin synthesis • Body store of energy (adipose tissue)
Dietary fat • Saturated fats Storage fats of animals Meat fat Lard Butter Cheese cream
Polyunsaturated fats • Linoleic acid (omega 6) Sunflower, safflower, corn, palm, soya • Alpha-linolenic acid (omega 3) (EPA) Fish oils (DHA) Fish oils

Monounsaturated fats • Olive oil and rapeseed oil • Nuts and seeds • Present in lean meat e. g. 100 g beef - 1. 4 g saturated fat - 2. 3 g monounsaturated fat
Fat in the UK diet Very high fat foods (above 20 g / portion) Pizza Pilau rice Fried rice Chips Cauliflower cheese Cheese omelettes Fatty meat Poultry with skin Meat curries sausages Pies, puddings, pasties, sausage rolls, quiche Fried food Pastry / tarts 200 kcals from fat
Fat in the UK diet High fat foods 10 -20 g/portion Bread with thick spread Fruit pies and flans Double / whipping cream Full fat cheeses Poultry breast meat Red meat with marbling Beef burgers Luncheon meat Omelettes, fried eggs Scampi Peanuts Mayonnaise Chocolate Sponge puddings, trifles, cakes
How will we achieve Govt. guidelines on fat? • Cook from scratch • Eat at home more • Eat less fat rich foods (pies, cakes, chocolates) • Avoid obvious sources of fat • Use minimal fat in cooking and on/in food • Use lower fat dairy products
Fat – the acute medical perspective • Surgical outcomes poorer in obese • Infertility / poor pregnancy outcomes • Fat low satiety, taste enhancing – useful in treating energy malnutrition (underweight, renal patients, cancer patients)

Clinical fat supplements
Fat – the public health perspective • Obesity • Cardiovascular disease • Cancers
A quick recap….
Proteins • Vital for structure and metabolic operation of body • Major component of body tissues – essential for growth and maintenance of body structures • Production of enzymes • Transporters • Hormones • Immune function • Buffering function • Energy source when energy insufficiency
Structure of proteins • Made of chains of amino acids • Dipeptides, tripeptides, oligopeptides, Polypeptides • Dietary proteins are broken down by digestive enzymes • Some enter the body amino acid pool • Others transaminated into other amino acids • Surplus are deaminated – the amino acids converted to urea – excreted via the kidneys
Amino acids • Some essential • Some semi-essential • Some conditionally essential in critically ill
Essential amino acids • Some amino acids can’t be synthesized by the body – called essential amino acids • - 9 essential in adults and 10 in children Isoleucine Leucine Valine Lysine Methionine Phenylalanine Threonine Tryptophan Histidine (arginine)
Semi-essential amino acids • Can be readily synthesized from other amino acids provided that precursors amino acids are present in diet in large enough amounts • Cysteine • Tyrosine
Conditionally essential • Glutamine and Arginine are thought to be conditionally essential in critically ill people
Protein requirements • Continuous requirement for new sources of protein • In childhood and pregnancy higher requirements • Body designed to conserve proteins • Synthesis of protein takes place in all cells and tissues
Protein requirements • 200 -300 g protein turned over daily • Body's requirement is 3 -4 g / kg body weight • Requirements higher in children and lower in elderly • In trauma and starvation see negative protein balance
Protein in the UK diet (g per day) • 24 g from meat and meat products • 17 g from cereals • 14 g from milk and milk products • 7 g from vegetables • 4 g from fish • 2 g from eggs • 1 g from fruit
Protein – the acute medical perspective • Protein deficiency due to inadequate energy intake • Catabolic response to trauma • Failure to absorb or utelize protein (GI disorders, liver disease) • Excessive protein loss – renal disease, haemorrhage, exudative loses Poorer clinical outcomes
Protein - the acute medical perspective • Muscle wasting – heart • Increased susceptibility to infection • Poor wound healing • Oedema • Anaemia • Fatty infiltration of the liver
Protein supplements
Protein – the public health perspective Obesity Cardiovascular disease Cancer Renal function Demineralisation of bones
What we have talked about…. • Fluids and fluid balance • Carbohydrates • Fats • Proteins
A final thought from the BMJ Poor lifestyle choices – overweight, inactive and smoking reduce life expectancy by a minimum of 15 years