Slide 1 Intravenous Fluids in Children NPSA Guidelines


- Slides: 27
Slide 1 Intravenous Fluids in Children NPSA Guidelines Dr Pam Cupples SPAN Meeting Friday the 20 th of April 2007 Dunkeld
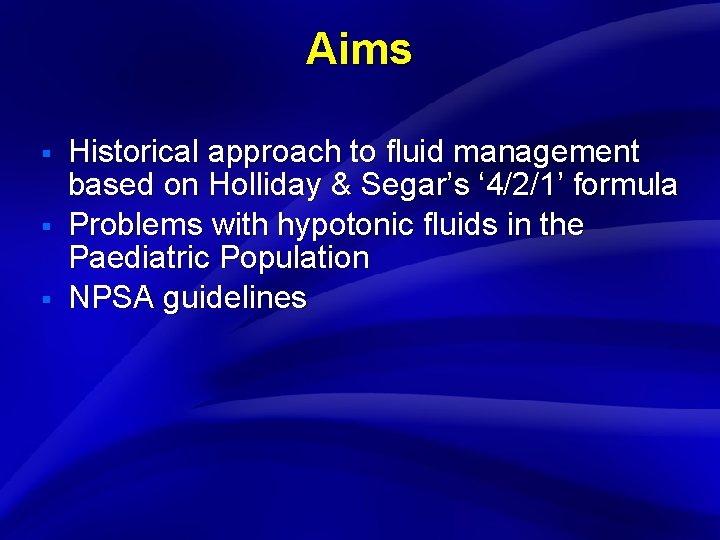
Slide 2 Aims § § § Historical approach to fluid management based on Holliday & Segar’s ‘ 4/2/1’ formula Problems with hypotonic fluids in the Paediatric Population NPSA guidelines
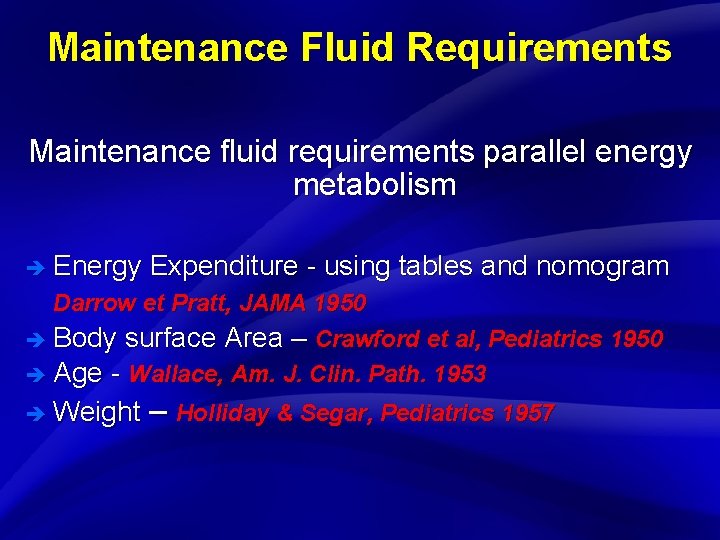
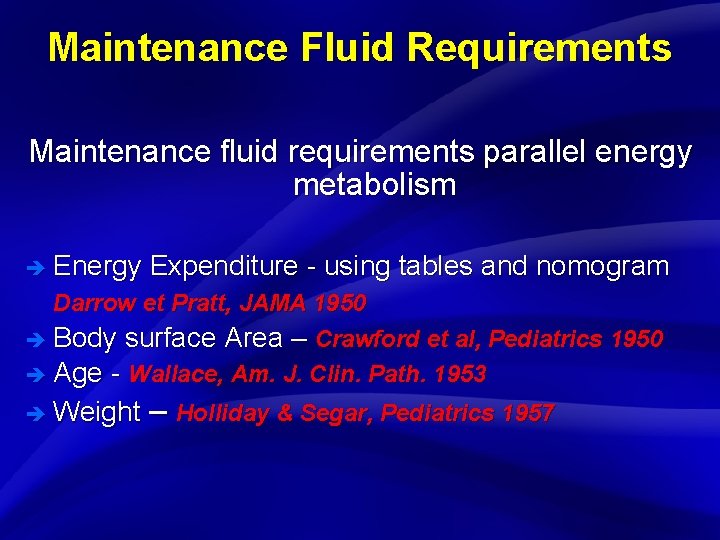
Slide 3 Maintenance Fluid Requirements Maintenance fluid requirements parallel energy metabolism è Energy Expenditure - using tables and nomogram Darrow et Pratt, JAMA 1950 è Body surface Area – Crawford et al, Pediatrics 1950 è Age - Wallace, Am. J. Clin. Path. 1953 è Weight – Holliday & Segar, Pediatrics 1957
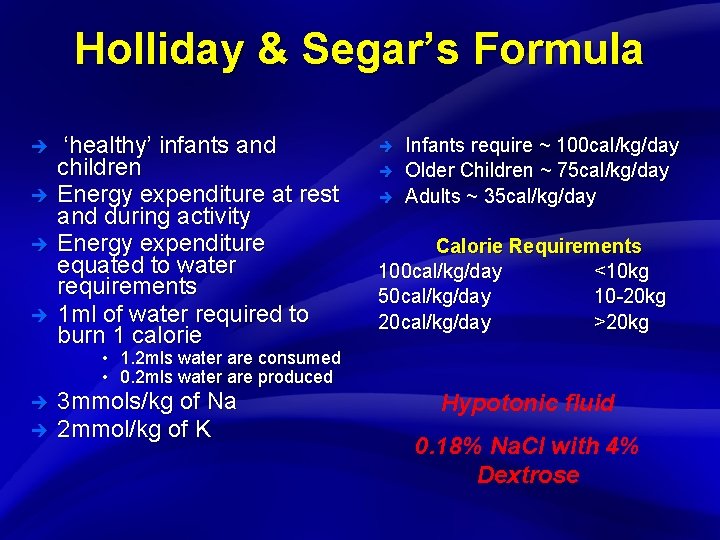
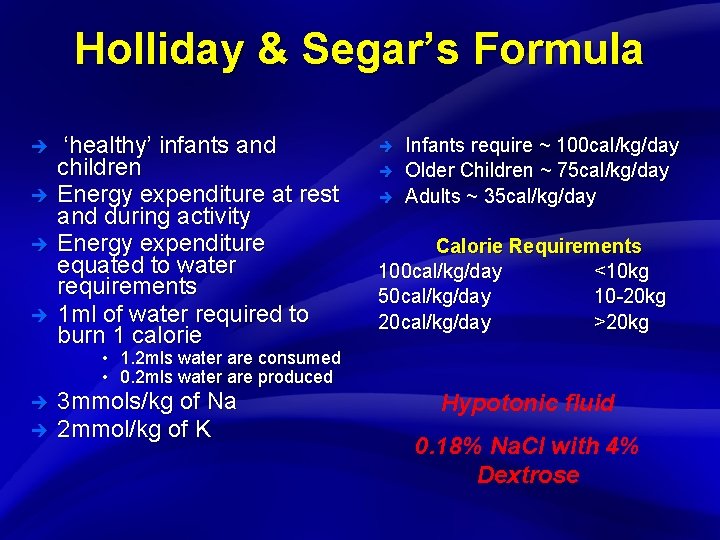
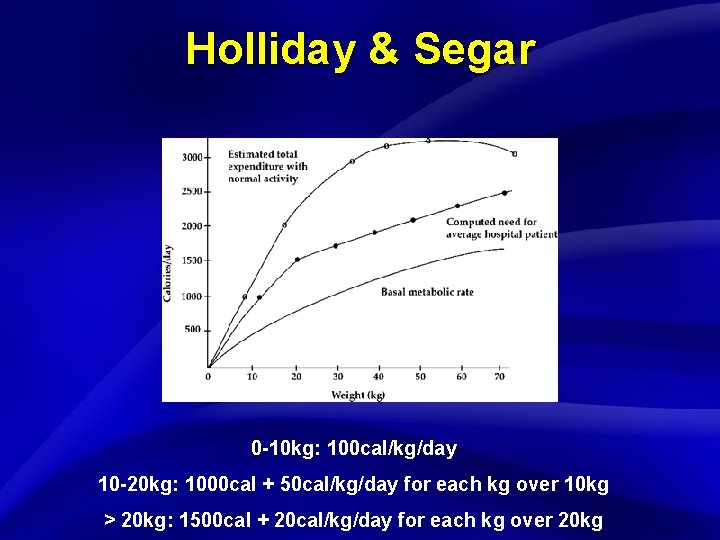
Slide 4 Holliday & Segar’s Formula è è ‘healthy’ infants and children Energy expenditure at rest and during activity Energy expenditure equated to water requirements 1 ml of water required to burn 1 calorie è è è Infants require ~ 100 cal/kg/day Older Children ~ 75 cal/kg/day Adults ~ 35 cal/kg/day Calorie Requirements 100 cal/kg/day <10 kg 50 cal/kg/day 10 -20 kg 20 cal/kg/day >20 kg • 1. 2 mls water are consumed • 0. 2 mls water are produced è è 3 mmols/kg of Na 2 mmol/kg of K Hypotonic fluid 0. 18% Na. Cl with 4% Dextrose
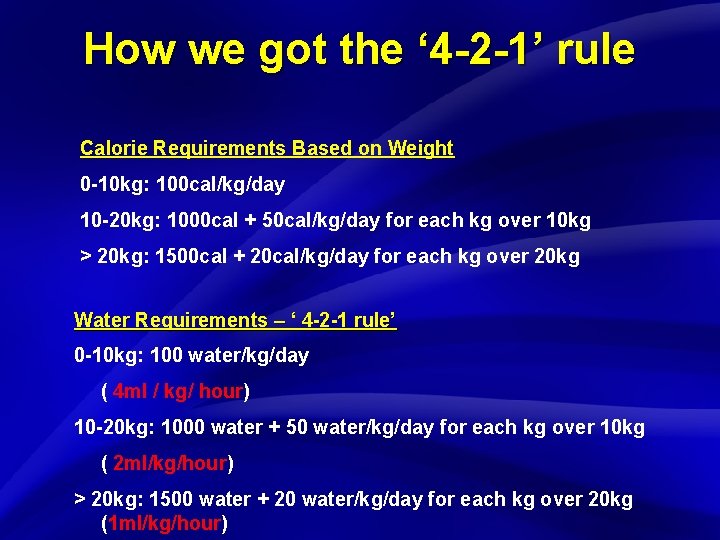
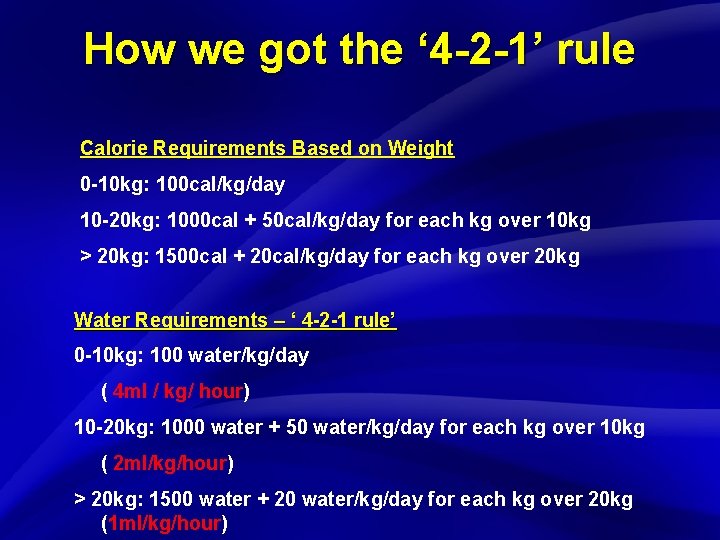
Slide 5 How we got the ‘ 4 -2 -1’ rule Calorie Requirements Based on Weight 0 -10 kg: 100 cal/kg/day 10 -20 kg: 1000 cal + 50 cal/kg/day for each kg over 10 kg > 20 kg: 1500 cal + 20 cal/kg/day for each kg over 20 kg Water Requirements – ‘ 4 -2 -1 rule’ 0 -10 kg: 100 water/kg/day ( 4 ml / kg/ hour) 10 -20 kg: 1000 water + 50 water/kg/day for each kg over 10 kg ( 2 ml/kg/hour) > 20 kg: 1500 water + 20 water/kg/day for each kg over 20 kg (1 ml/kg/hour)
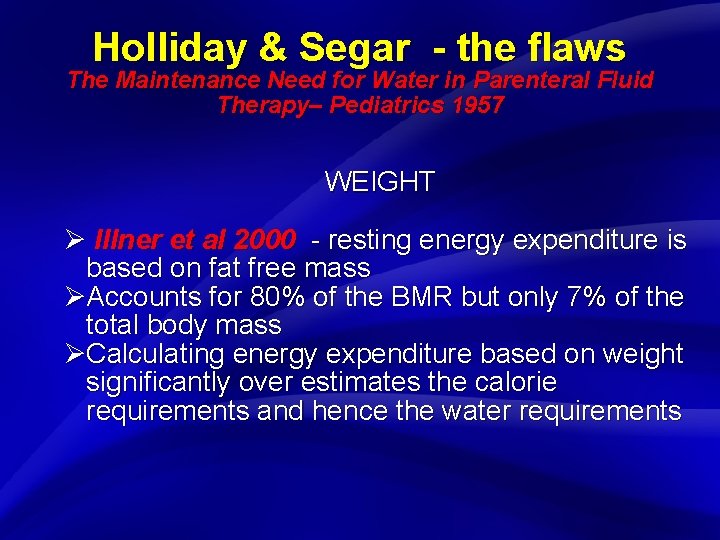
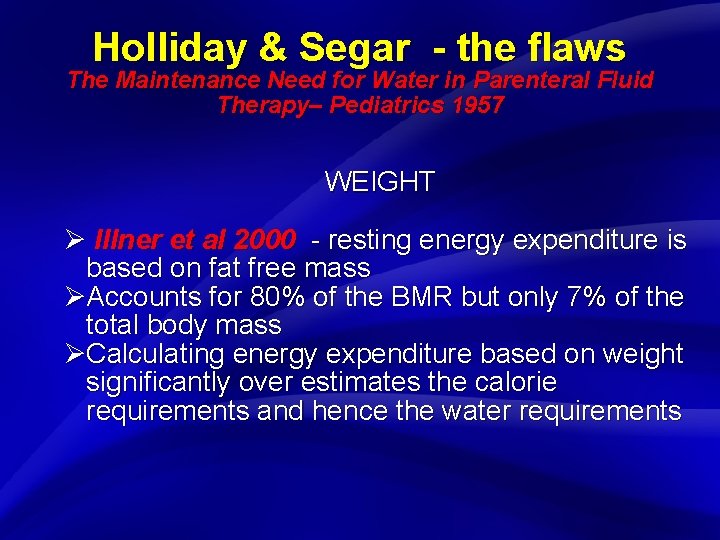
Slide 6 Holliday & Segar - the flaws The Maintenance Need for Water in Parenteral Fluid Therapy– Pediatrics 1957 WEIGHT Ø Illner et al 2000 - resting energy expenditure is based on fat free mass ØAccounts for 80% of the BMR but only 7% of the total body mass ØCalculating energy expenditure based on weight significantly over estimates the calorie requirements and hence the water requirements
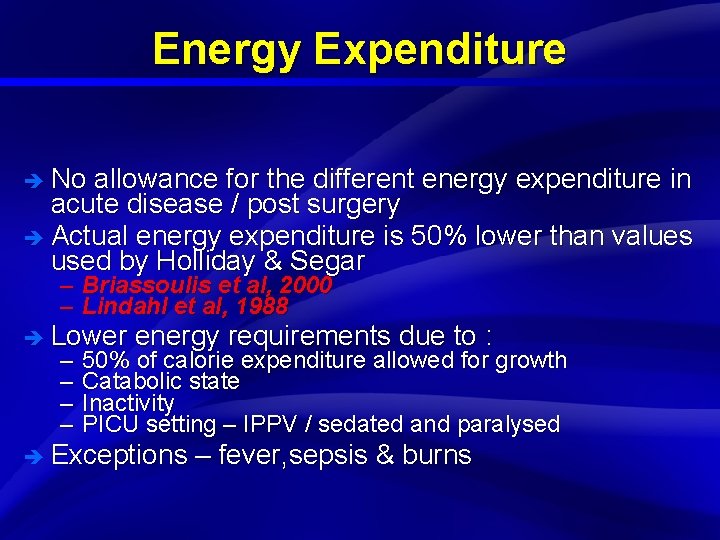
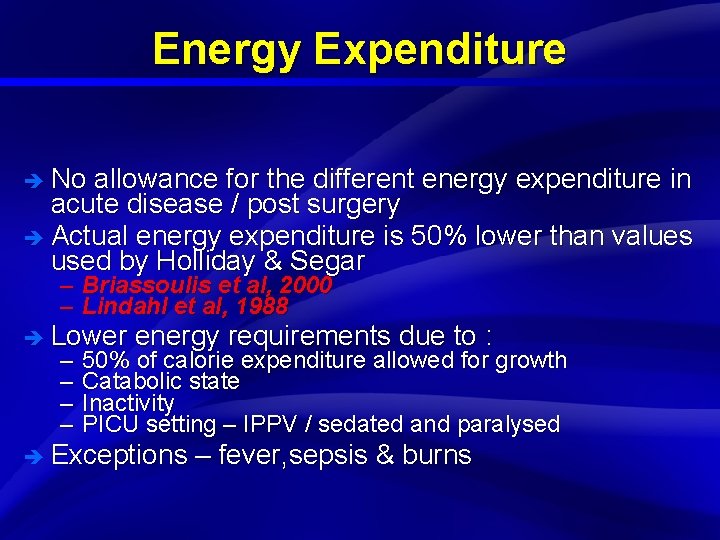
Slide 7 Energy Expenditure è No allowance for the different energy expenditure in acute disease / post surgery è Actual energy expenditure is 50% lower than values used by Holliday & Segar – Briassoulis et al, 2000 – Lindahl et al, 1988 è Lower – – energy requirements due to : 50% of calorie expenditure allowed for growth Catabolic state Inactivity PICU setting – IPPV / sedated and paralysed è Exceptions – fever, sepsis & burns
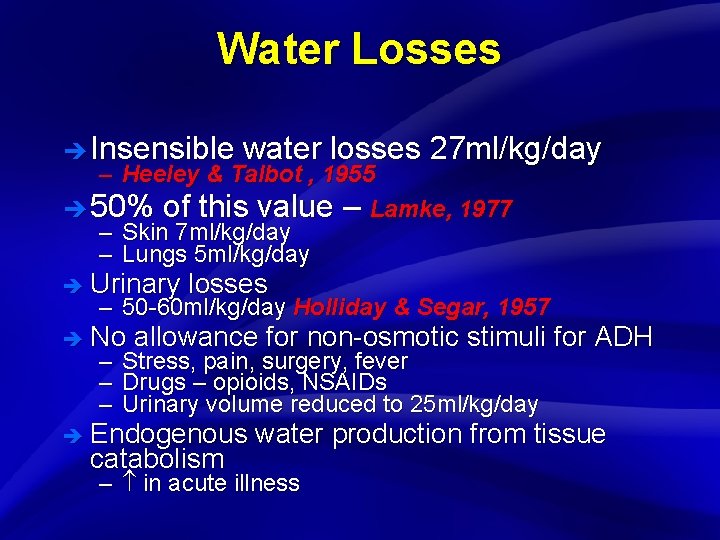
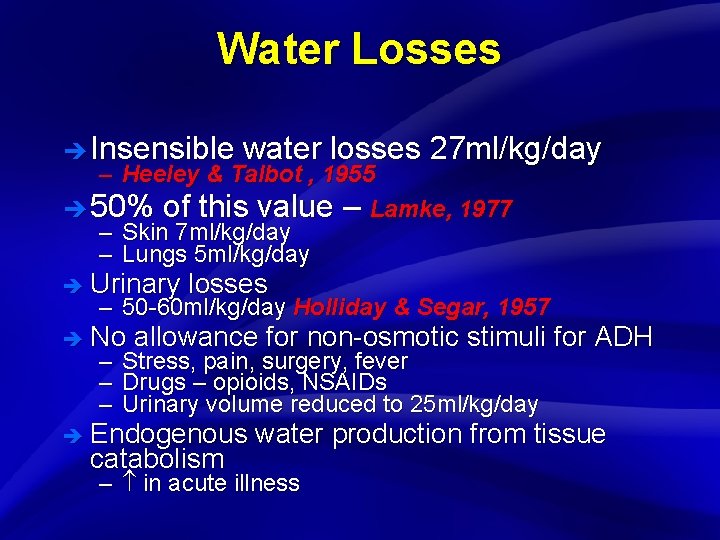
Slide 8 Water Losses è Insensible water losses 27 ml/kg/day – Heeley & Talbot , 1955 è 50% of this value – Lamke, 1977 – Skin 7 ml/kg/day – Lungs 5 ml/kg/day è Urinary losses – 50 -60 ml/kg/day Holliday & Segar, 1957 è No – – – allowance for non-osmotic stimuli for ADH Stress, pain, surgery, fever Drugs – opioids, NSAIDs Urinary volume reduced to 25 ml/kg/day è Endogenous catabolism water production from tissue – in acute illness

Slide 9
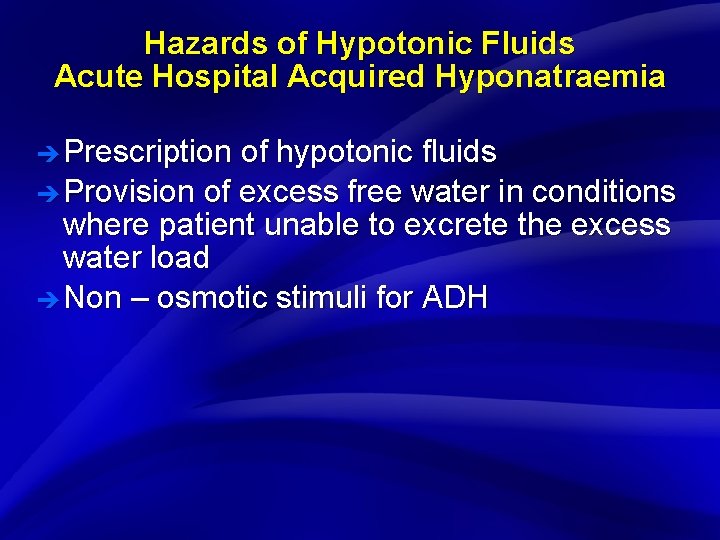
Slide 10 Hazards of Hypotonic Fluids Acute Hospital Acquired Hyponatraemia è Prescription of hypotonic fluids è Provision of excess free water in conditions where patient unable to excrete the excess water load è Non – osmotic stimuli for ADH
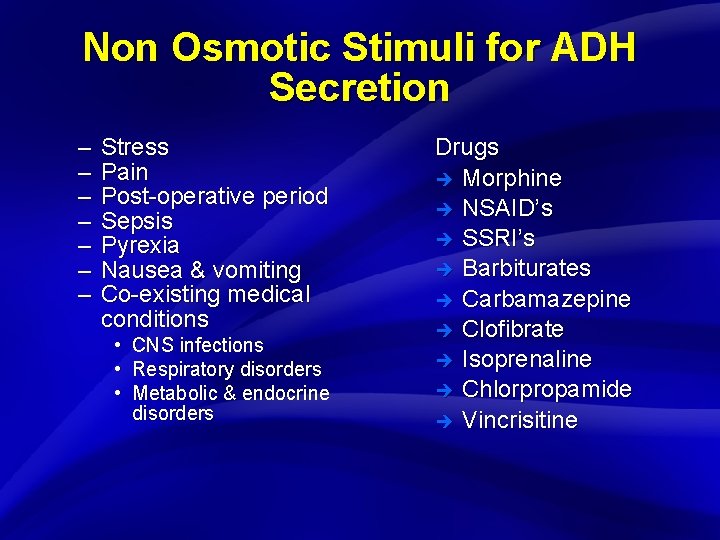
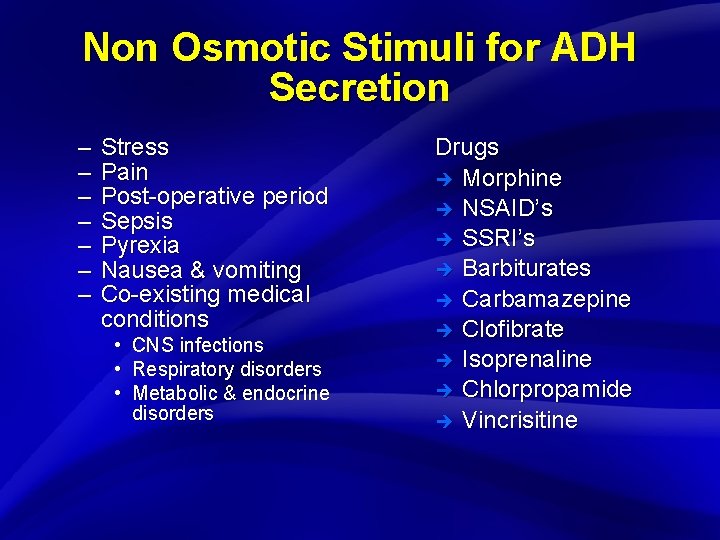
Slide 11 Non Osmotic Stimuli for ADH Secretion – – – – Stress Pain Post-operative period Sepsis Pyrexia Nausea & vomiting Co-existing medical conditions • • • CNS infections Respiratory disorders Metabolic & endocrine disorders Drugs è Morphine è NSAID’s è SSRI’s è Barbiturates è Carbamazepine è Clofibrate è Isoprenaline è Chlorpropamide è Vincrisitine
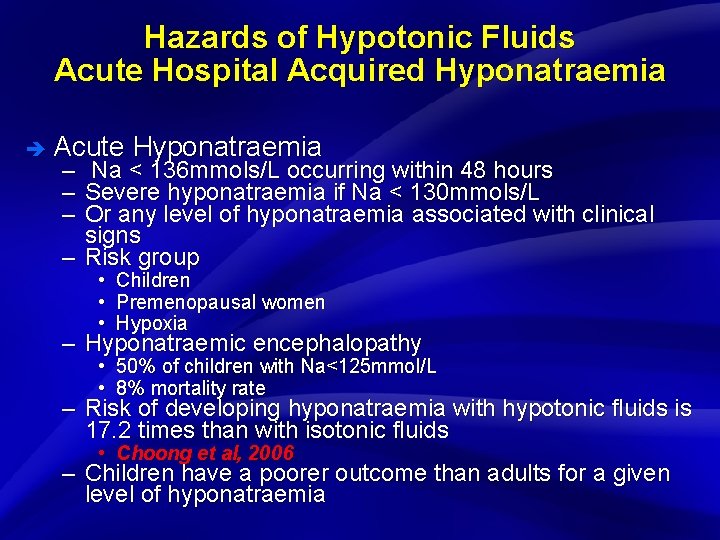
Slide 12 Hazards of Hypotonic Fluids Acute Hospital Acquired Hyponatraemia è Acute – – – Hyponatraemia Na < 136 mmols/L occurring within 48 hours Severe hyponatraemia if Na < 130 mmols/L Or any level of hyponatraemia associated with clinical signs – Risk group • Children • Premenopausal women • Hypoxia – Hyponatraemic encephalopathy • 50% of children with Na<125 mmol/L • 8% mortality rate – Risk of developing hyponatraemia with hypotonic fluids is 17. 2 times than with isotonic fluids • Choong et al, 2006 – Children have a poorer outcome than adults for a given level of hyponatraemia
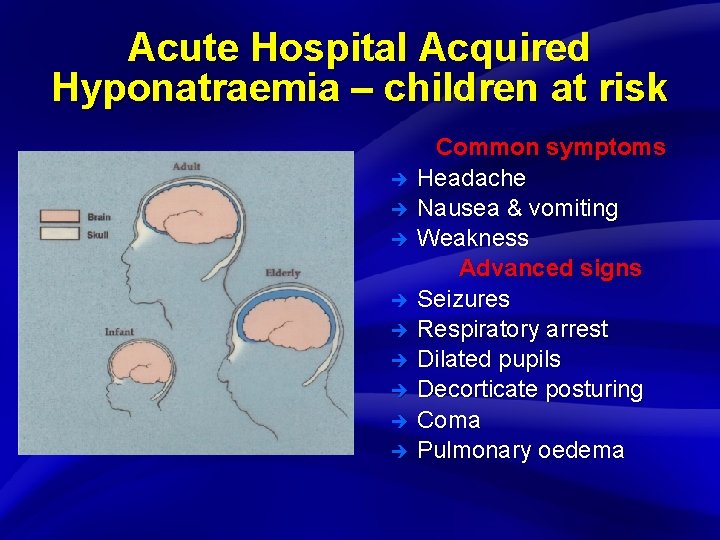
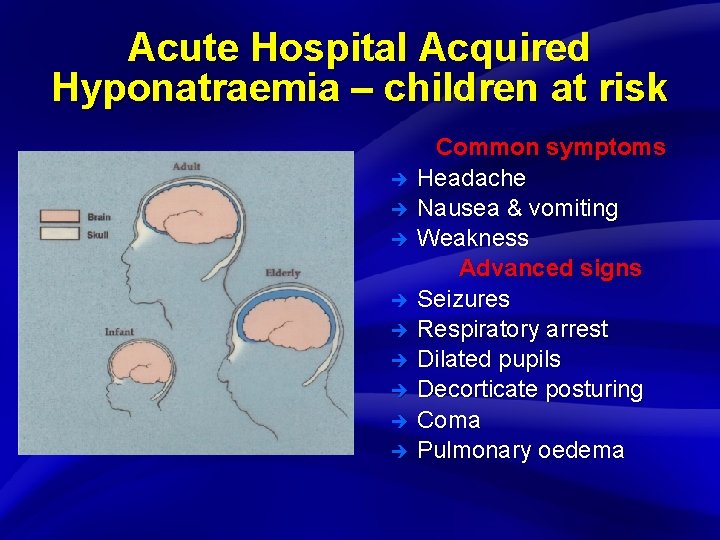
Slide 13 Acute Hospital Acquired Hyponatraemia – children at risk è è è è è Common symptoms Headache Nausea & vomiting Weakness Advanced signs Seizures Respiratory arrest Dilated pupils Decorticate posturing Coma Pulmonary oedema
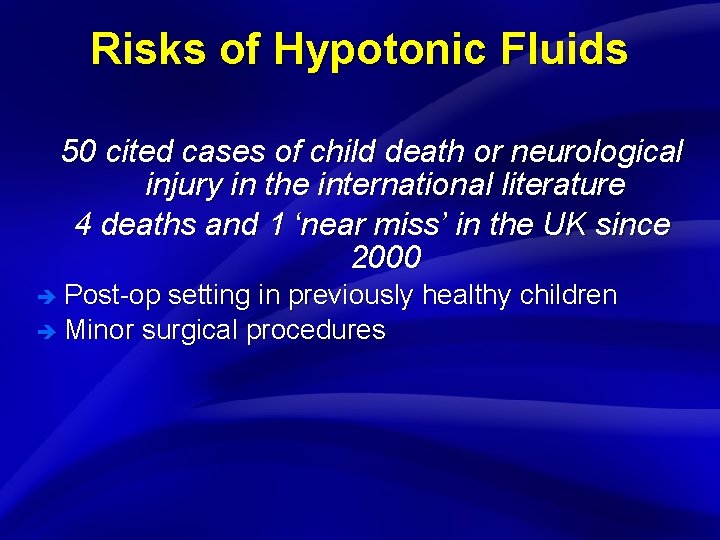
Slide 14 Risks of Hypotonic Fluids 50 cited cases of child death or neurological injury in the international literature 4 deaths and 1 ‘near miss’ in the UK since 2000 è Post-op setting in previously healthy children è Minor surgical procedures
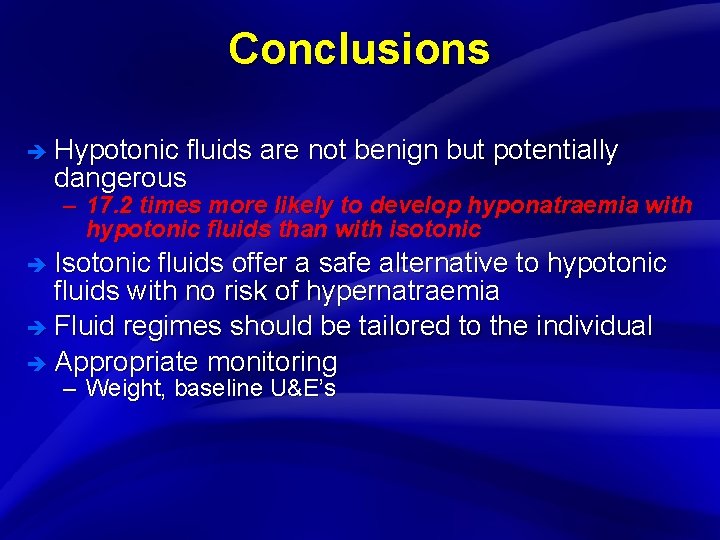
Slide 15 Conclusions è Hypotonic fluids are not benign but potentially dangerous – 17. 2 times more likely to develop hyponatraemia with hypotonic fluids than with isotonic è Isotonic fluids offer a safe alternative to hypotonic fluids with no risk of hypernatraemia è Fluid regimes should be tailored to the individual è Appropriate monitoring – Weight, baseline U&E’s
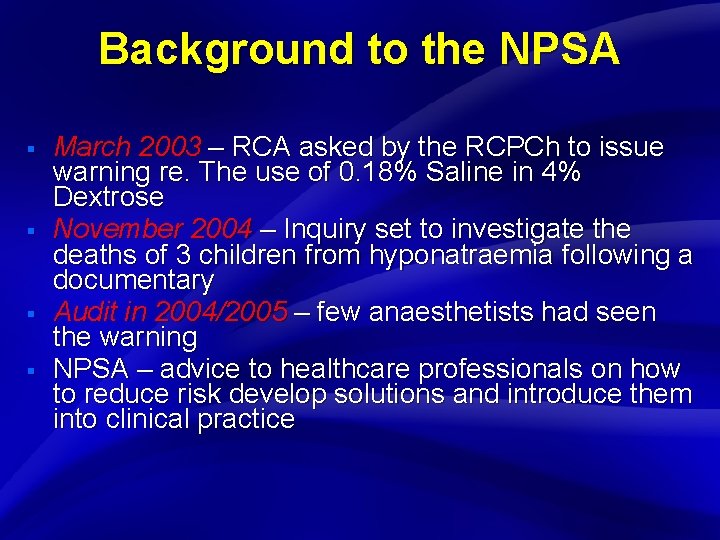
Slide 16 Background to the NPSA § § March 2003 – RCA asked by the RCPCh to issue warning re. The use of 0. 18% Saline in 4% Dextrose November 2004 – Inquiry set to investigate the deaths of 3 children from hyponatraemia following a documentary Audit in 2004/2005 – few anaesthetists had seen the warning NPSA – advice to healthcare professionals on how to reduce risk develop solutions and introduce them into clinical practice
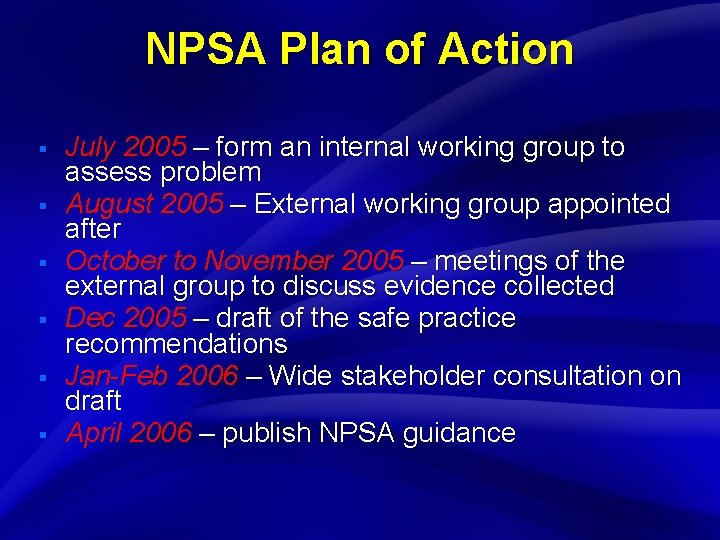
Slide 17 NPSA Plan of Action § § § July 2005 – form an internal working group to assess problem August 2005 – External working group appointed after October to November 2005 – meetings of the external group to discuss evidence collected Dec 2005 – draft of the safe practice recommendations Jan-Feb 2006 – Wide stakeholder consultation on draft April 2006 – publish NPSA guidance
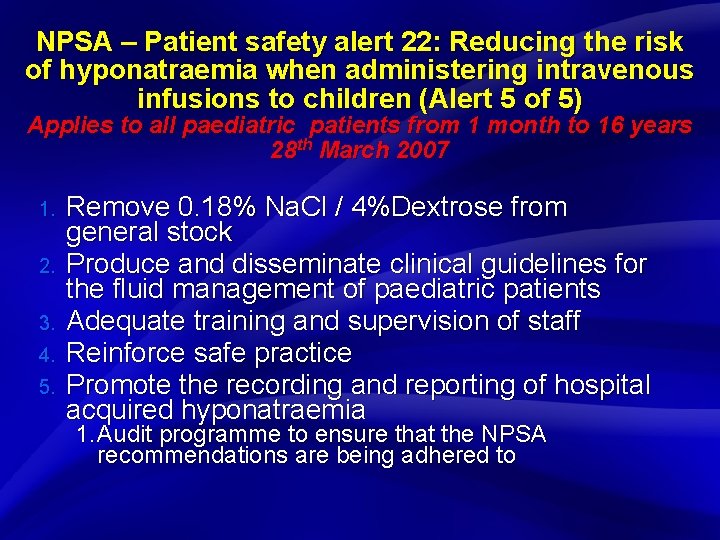
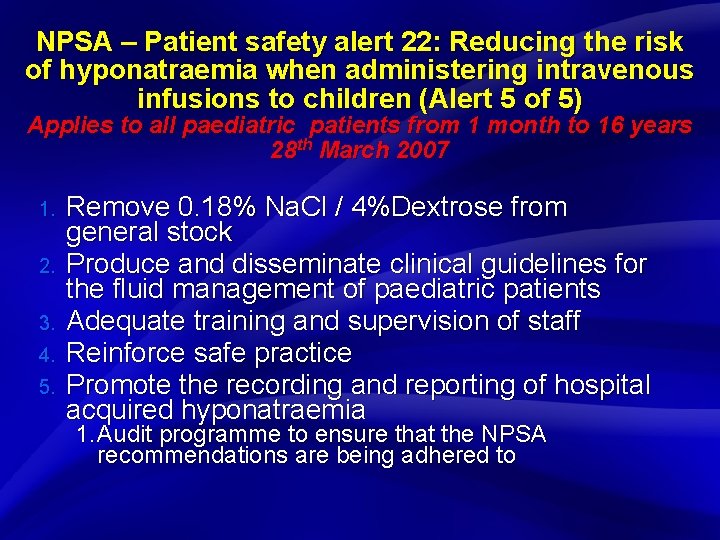
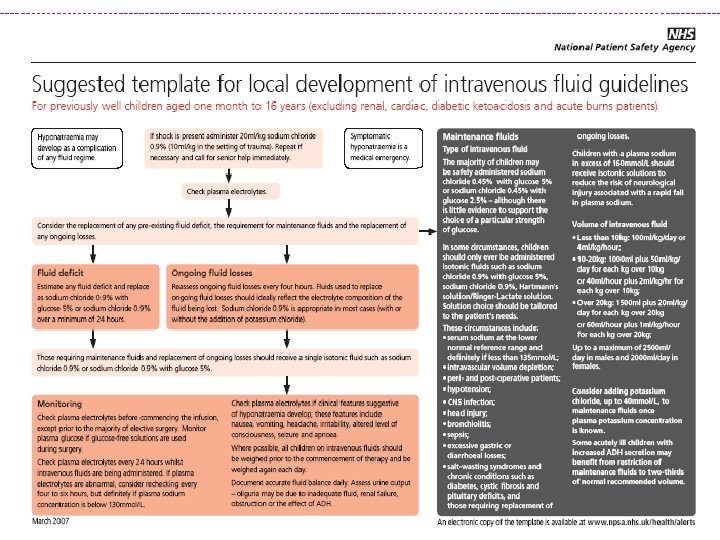
Slide 18 NPSA – Patient safety alert 22: Reducing the risk of hyponatraemia when administering intravenous infusions to children (Alert 5 of 5) Applies to all paediatric patients from 1 month to 16 years 28 th March 2007 1. 2. 3. 4. 5. Remove 0. 18% Na. Cl / 4%Dextrose from general stock Produce and disseminate clinical guidelines for the fluid management of paediatric patients Adequate training and supervision of staff Reinforce safe practice Promote the recording and reporting of hospital acquired hyponatraemia 1. Audit programme to ensure that the NPSA recommendations are being adhered to
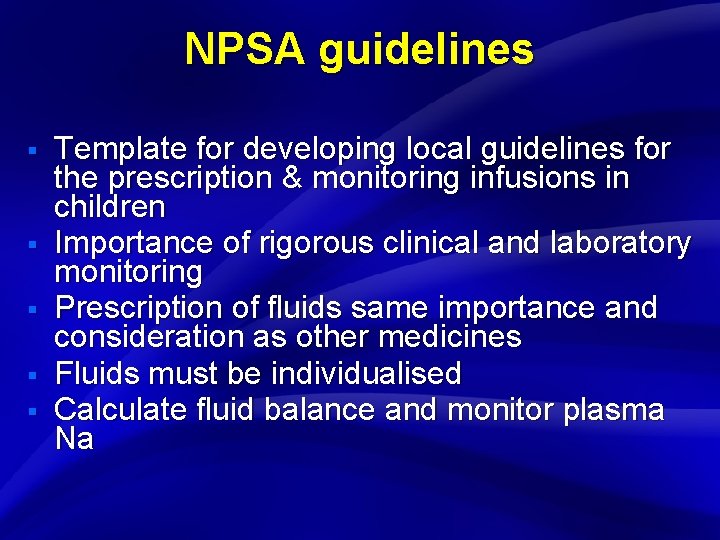
Slide 19 NPSA guidelines § § § Template for developing local guidelines for the prescription & monitoring infusions in children Importance of rigorous clinical and laboratory monitoring Prescription of fluids same importance and consideration as other medicines Fluids must be individualised Calculate fluid balance and monitor plasma Na
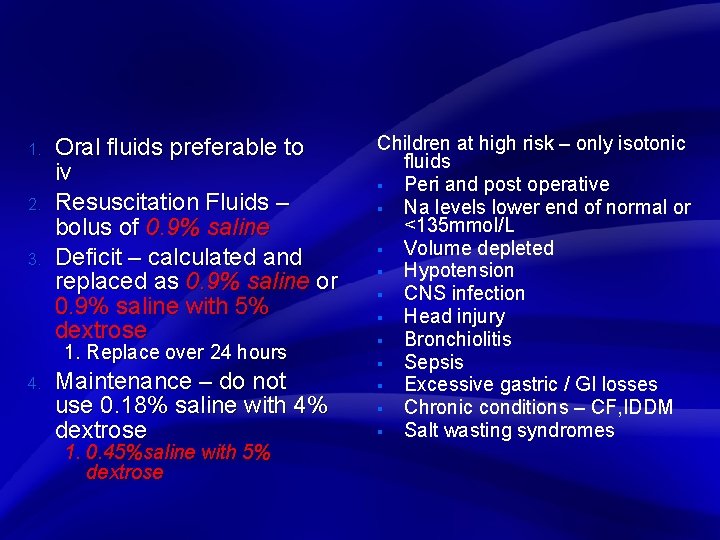
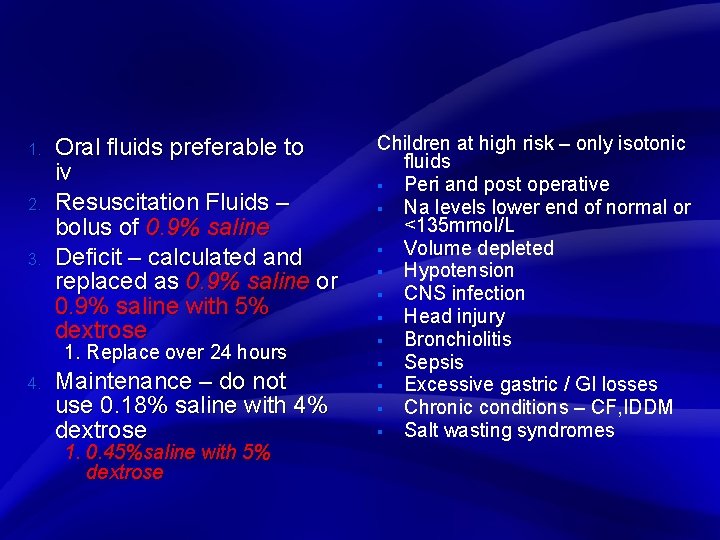
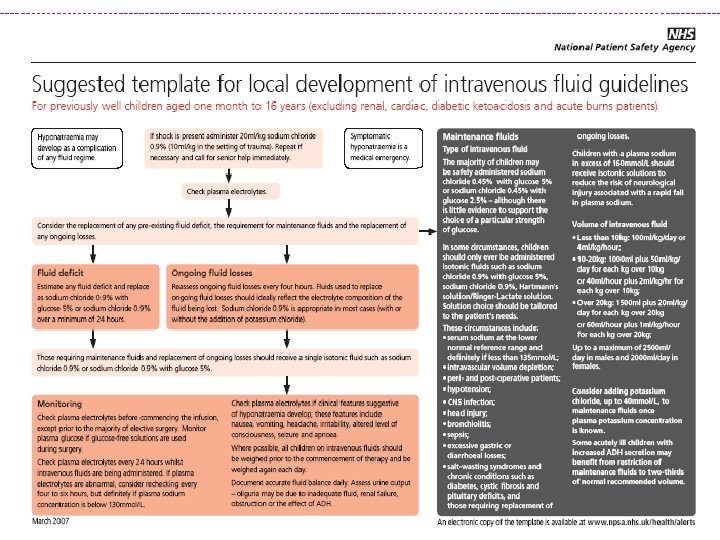
Slide 20 1. 2. 3. Oral fluids preferable to iv Resuscitation Fluids – bolus of 0. 9% saline Deficit – calculated and replaced as 0. 9% saline or 0. 9% saline with 5% dextrose 1. Replace over 24 hours 4. Maintenance – do not use 0. 18% saline with 4% dextrose 1. 0. 45%saline with 5% dextrose Children at high risk – only isotonic fluids § Peri and post operative § Na levels lower end of normal or <135 mmol/L § Volume depleted § Hypotension § CNS infection § Head injury § Bronchiolitis § Sepsis § Excessive gastric / GI losses § Chronic conditions – CF, IDDM § Salt wasting syndromes
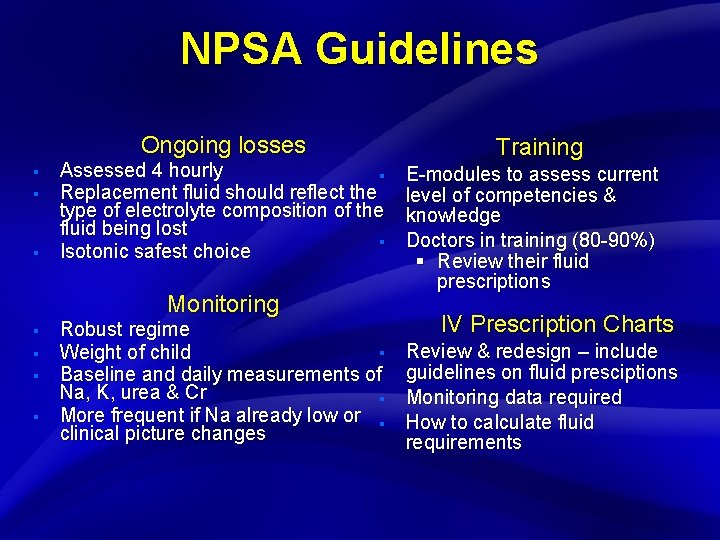
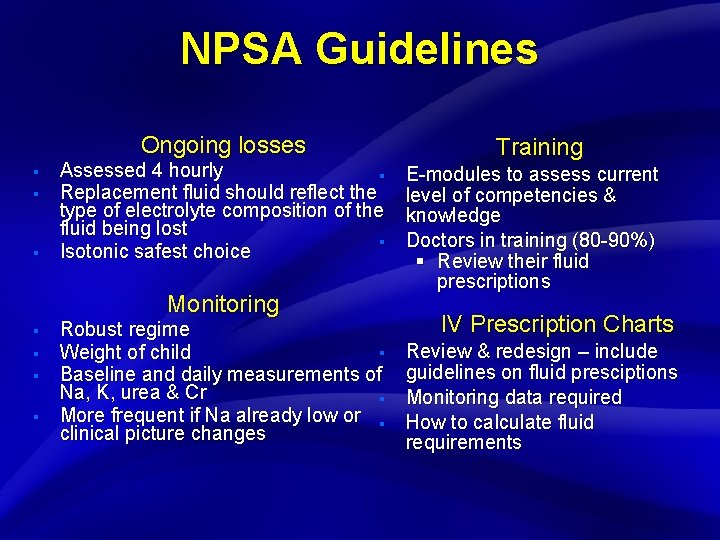
Slide 21 NPSA Guidelines Ongoing losses § § § Assessed 4 hourly § Replacement fluid should reflect the type of electrolyte composition of the fluid being lost § Isotonic safest choice Monitoring § § Robust regime § Weight of child Baseline and daily measurements of Na, K, urea & Cr § More frequent if Na already low or § clinical picture changes Training E-modules to assess current level of competencies & knowledge Doctors in training (80 -90%) § Review their fluid prescriptions IV Prescription Charts Review & redesign – include guidelines on fluid presciptions Monitoring data required How to calculate fluid requirements
Slide 22

Slide 23 www. npsa. nhs. uk/health/alerts
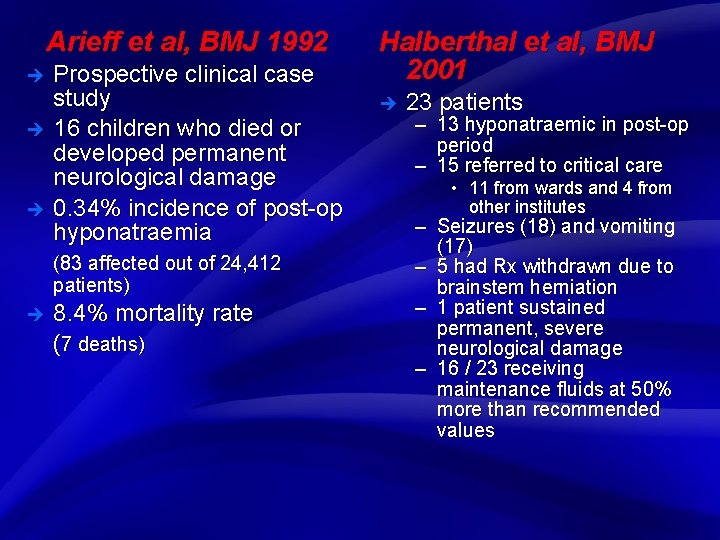
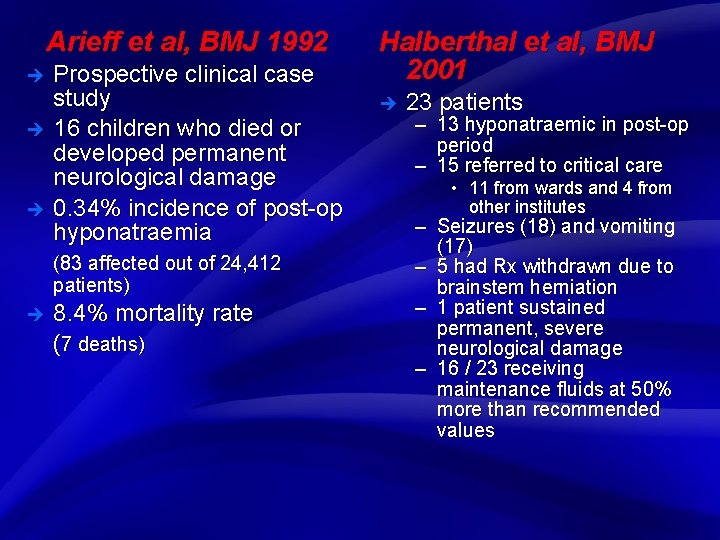
Slide 24 Arieff et al, BMJ 1992 è è è Prospective clinical case study 16 children who died or developed permanent neurological damage 0. 34% incidence of post-op hyponatraemia (83 affected out of 24, 412 patients) è 8. 4% mortality rate (7 deaths) Halberthal et al, BMJ 2001 è 23 patients – 13 hyponatraemic in post-op period – 15 referred to critical care • 11 from wards and 4 from other institutes – Seizures (18) and vomiting (17) – 5 had Rx withdrawn due to brainstem herniation – 1 patient sustained permanent, severe neurological damage – 16 / 23 receiving maintenance fluids at 50% more than recommended values
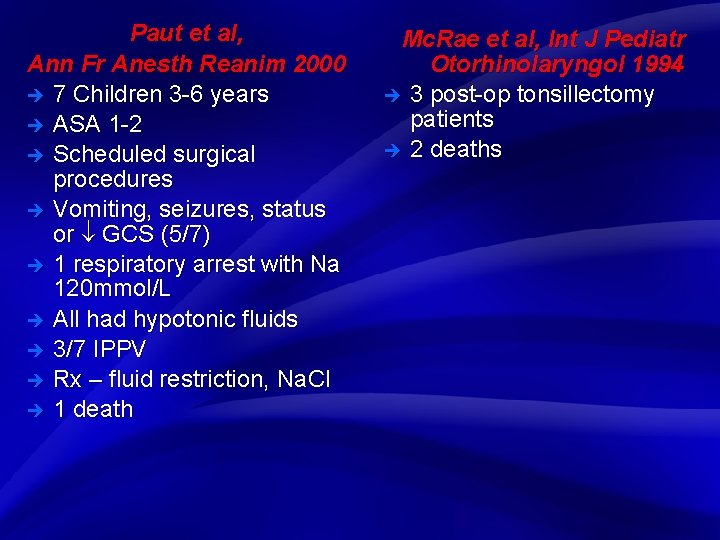
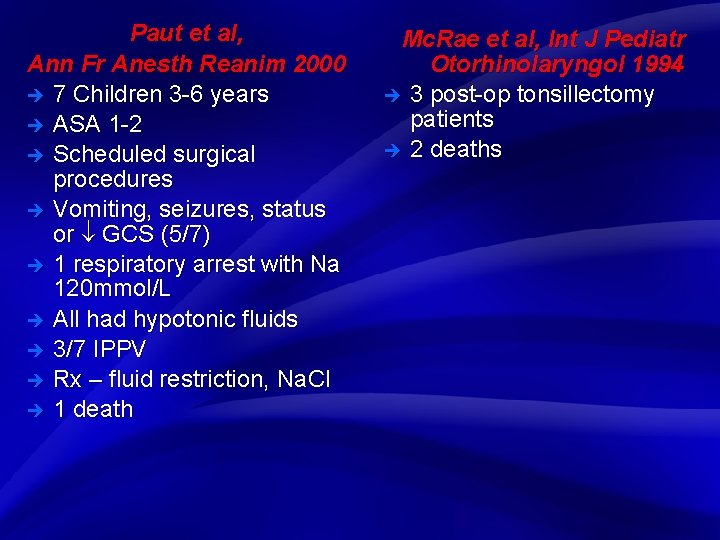
Slide 25 Paut et al, Ann Fr Anesth Reanim 2000 è 7 Children 3 -6 years è ASA 1 -2 è Scheduled surgical procedures è Vomiting, seizures, status or GCS (5/7) è 1 respiratory arrest with Na 120 mmol/L è All had hypotonic fluids è 3/7 IPPV è Rx – fluid restriction, Na. Cl è 1 death Mc. Rae et al, Int J Pediatr Otorhinolaryngol 1994 è 3 post-op tonsillectomy patients è 2 deaths
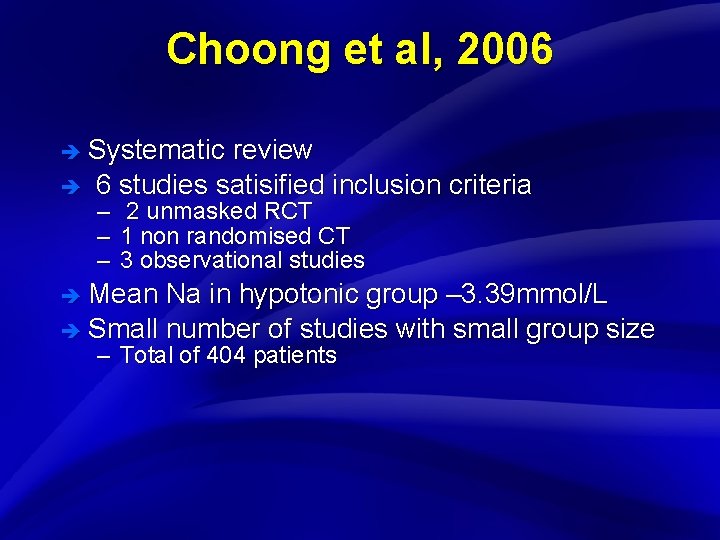
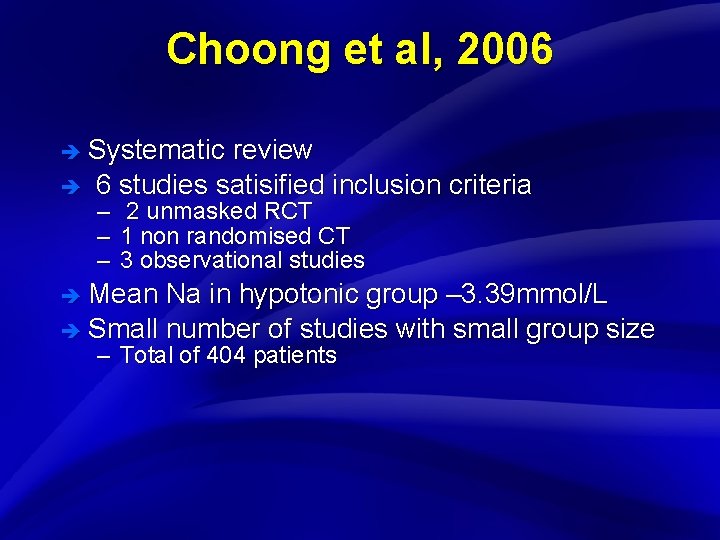
Slide 26 Choong et al, 2006 è Systematic è review 6 studies satisified inclusion criteria – – – 2 unmasked RCT 1 non randomised CT 3 observational studies è Mean Na in hypotonic group – 3. 39 mmol/L è Small number of studies with small group size – Total of 404 patients
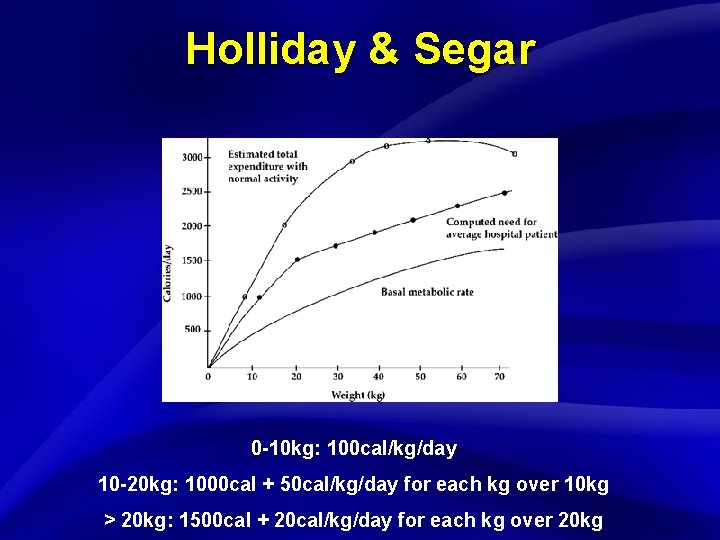
Slide 27 Holliday & Segar 0 -10 kg: 100 cal/kg/day 10 -20 kg: 1000 cal + 50 cal/kg/day for each kg over 10 kg > 20 kg: 1500 cal + 20 cal/kg/day for each kg over 20 kg
 Toe and heel dance
Toe and heel dance National standard for user applied labelling
National standard for user applied labelling Injectable medication administration pretest
Injectable medication administration pretest Cannula colour coding
Cannula colour coding What is my three word location
What is my three word location Iv cannulation ppt
Iv cannulation ppt Line & catheter label - intravenous burette
Line & catheter label - intravenous burette Infiltration extravasation phlebitis
Infiltration extravasation phlebitis Iv cannula labelling
Iv cannula labelling Medication administration 3 pretest
Medication administration 3 pretest Factoring problems
Factoring problems Static fluids
Static fluids Volumetric properties of pure fluids
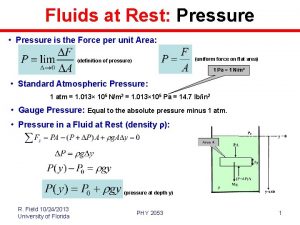
Volumetric properties of pure fluids Fluids at rest
Fluids at rest Compressible and incompressible fluids
Compressible and incompressible fluids Movement of body fluids
Movement of body fluids Chapter 18 fluids and electrolytes
Chapter 18 fluids and electrolytes Fluids at rest
Fluids at rest Evaluation test for suppositories
Evaluation test for suppositories Compressible and incompressible fluids
Compressible and incompressible fluids Fluids at rest
Fluids at rest Fluids mechanics
Fluids mechanics Viscosity unit
Viscosity unit Fluids at rest
Fluids at rest Crystalloids and colloids examples
Crystalloids and colloids examples Parental fluid
Parental fluid 4/2/1 rule
4/2/1 rule Fluids
Fluids