Evaluating Running Injuries in Clinic Jim Chesnutt M







- Slides: 52
Evaluating Running Injuries in Clinic Jim Chesnutt, M. D. OHSU Sports Medicine Program OHSU Orthopaedics and Rehabilitation and Family Medicine
Common Running Injuries • Look at biomechanics of running • Consider factors leading to overuse injury • Identify common running injuries • Learn treatment and prevention strategies
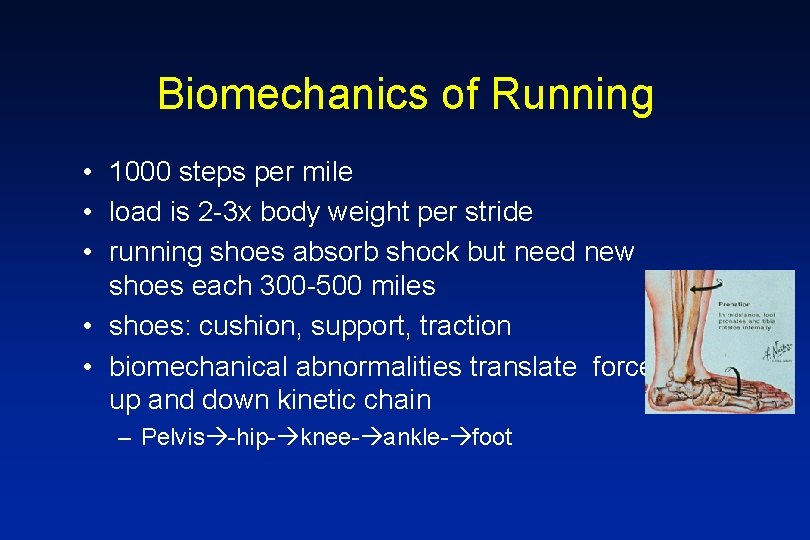
Biomechanics of Running • 1000 steps per mile • load is 2 -3 x body weight per stride • running shoes absorb shock but need new shoes each 300 -500 miles • shoes: cushion, support, traction • biomechanical abnormalities translate forces up and down kinetic chain – Pelvis -hip- knee- ankle- foot
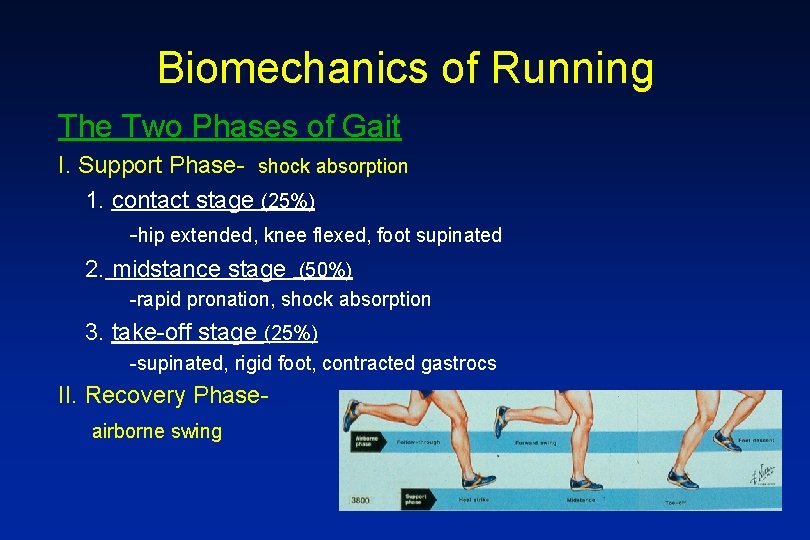
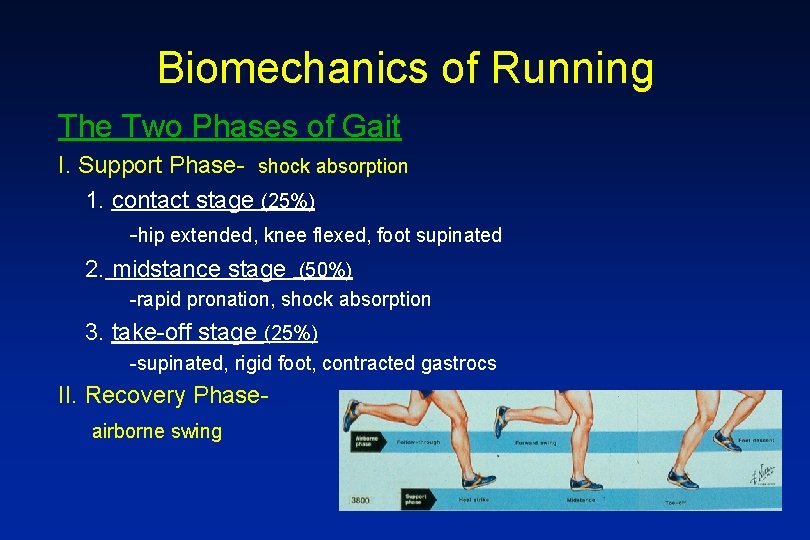
Biomechanics of Running The Two Phases of Gait I. Support Phase- shock absorption 1. contact stage (25%) -hip extended, knee flexed, foot supinated 2. midstance stage (50%) -rapid pronation, shock absorption 3. take-off stage (25%) -supinated, rigid foot, contracted gastrocs II. Recovery Phaseairborne swing
Common Overuse Syndromes Mechanisms of Injury 1. repetitive motion/ stress 2. microtrauma 3. stress or trauma >> adaptation or repair 4. chronic or progressive pain and dysfxn or mechanical failure (macrotrauma) 5. phases of healing : I. inflammatory( 1 -5 days) II. regeneration( 3 - 42 days) III. remodeling( 14+ days)
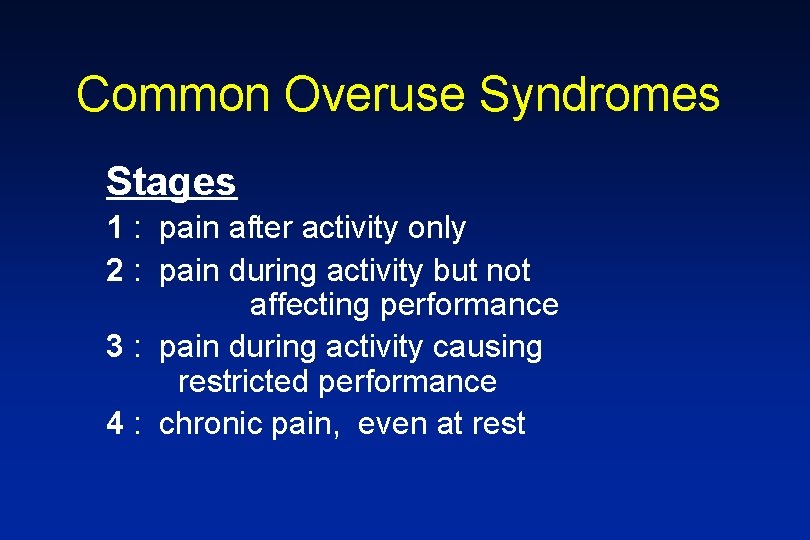
Common Overuse Syndromes Stages 1 : pain after activity only 2 : pain during activity but not affecting performance 3 : pain during activity causing restricted performance 4 : chronic pain, even at rest
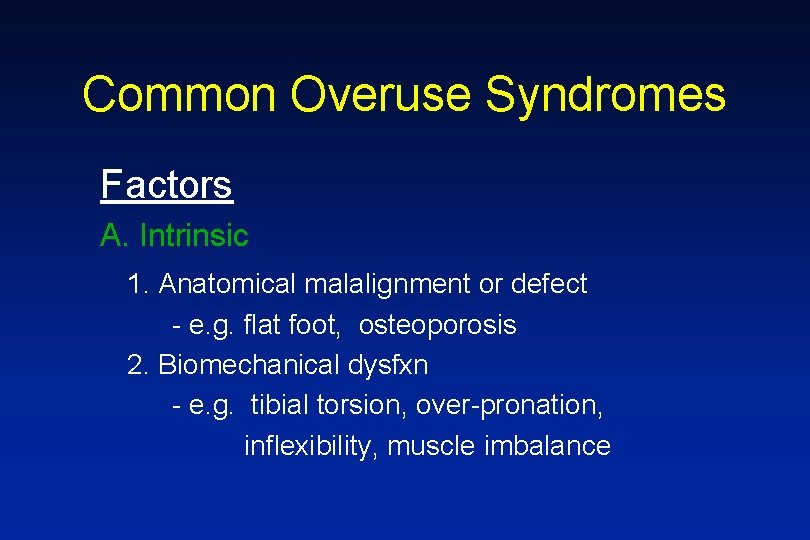
Common Overuse Syndromes Factors A. Intrinsic 1. Anatomical malalignment or defect - e. g. flat foot, osteoporosis 2. Biomechanical dysfxn - e. g. tibial torsion, over-pronation, inflexibility, muscle imbalance
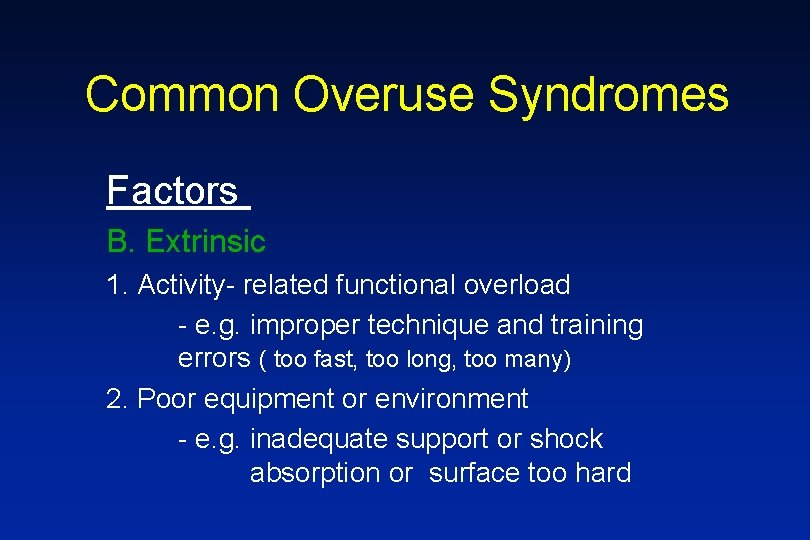
Common Overuse Syndromes Factors B. Extrinsic 1. Activity- related functional overload - e. g. improper technique and training errors ( too fast, too long, too many) 2. Poor equipment or environment - e. g. inadequate support or shock absorption or surface too hard
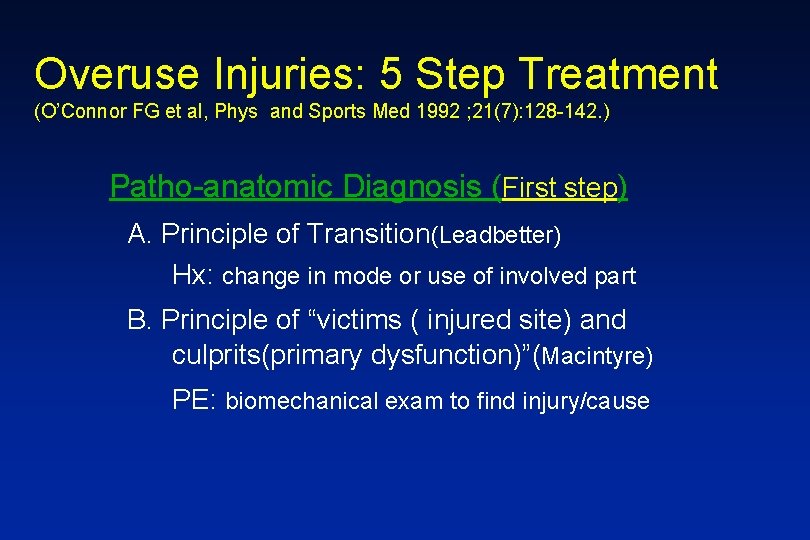
Overuse Injuries: 5 Step Treatment (O’Connor FG et al, Phys and Sports Med 1992 ; 21(7): 128 -142. ) Patho-anatomic Diagnosis (First step) A. Principle of Transition(Leadbetter) Hx: change in mode or use of involved part B. Principle of “victims ( injured site) and culprits(primary dysfunction)”(Macintyre) PE: biomechanical exam to find injury/cause
Running Injuries Risks: 1) >40 miles/ wk 2) previous injury 3) >10% increase mileage per wk 4) foot, knee, and hip malalignment (hyper-pronation, weak hip flexor)
Common Running Injuries Most common: 1) Patellofemoral Pain Syndrome 2) Medial Tibial Stress Syndrome (“shin splints”) 3) Iliotibial Band Friction Syndrome 4) Plantar Fasciitis 5) Achilles’ Tendinitis
Common Running Injuries 6. Stress Fracture of Tibia 7. Stress Fracture of Femur 8. Exertional Compartment Syndrome 9. Female Athlete Triad 10. Iron Deficiency

Patellofemoral Pain Syndrome • Combination of various syndromes including patellar subluxation, pain and “chondromalacia” • More common in females • Classical anterior knee pain, crepitance, and occ. swelling as well as “positive theater sign”
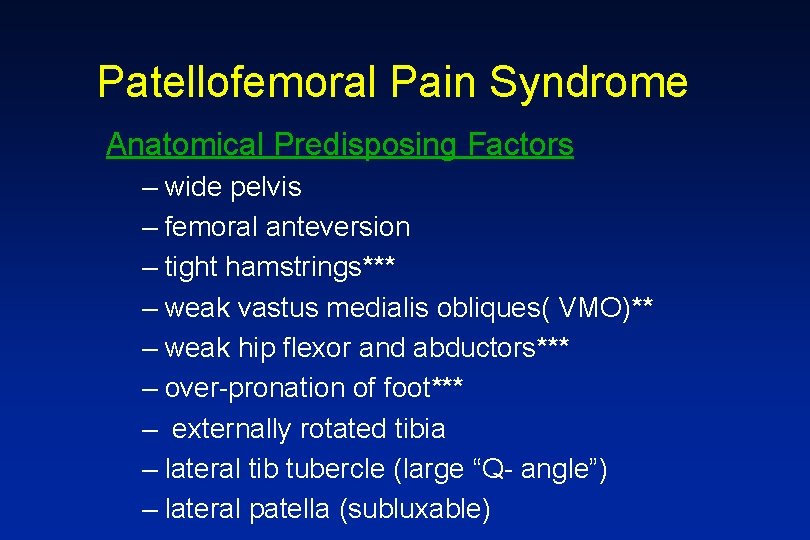
Patellofemoral Pain Syndrome Anatomical Predisposing Factors – wide pelvis – femoral anteversion – tight hamstrings*** – weak vastus medialis obliques( VMO)** – weak hip flexor and abductors*** – over-pronation of foot*** – externally rotated tibia – lateral tib tubercle (large “Q- angle”) – lateral patella (subluxable)
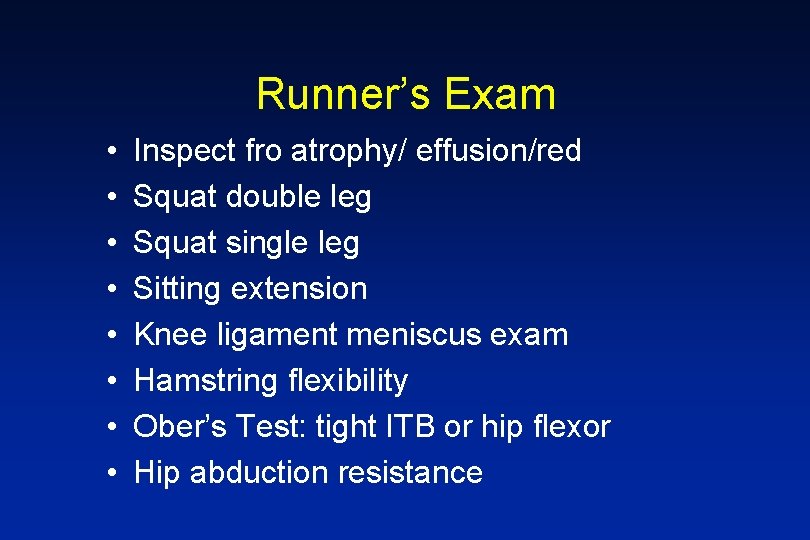
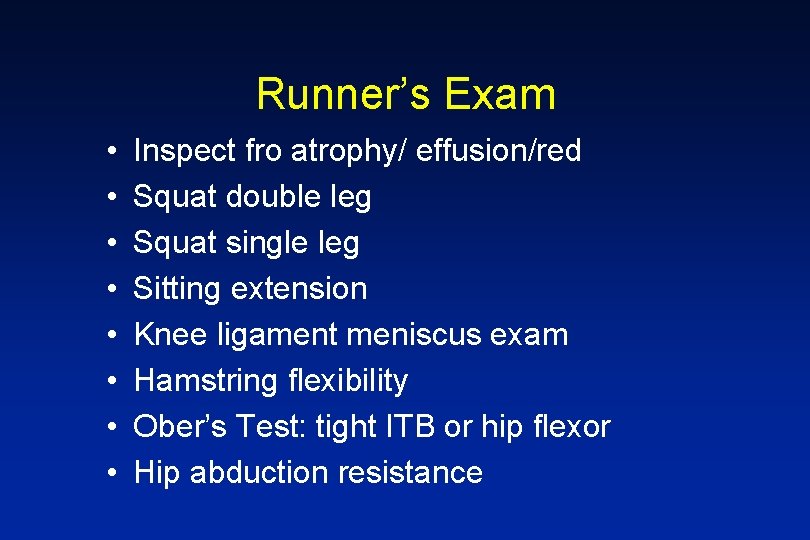
Runner’s Exam • • Inspect fro atrophy/ effusion/red Squat double leg Squat single leg Sitting extension Knee ligament meniscus exam Hamstring flexibility Ober’s Test: tight ITB or hip flexor Hip abduction resistance





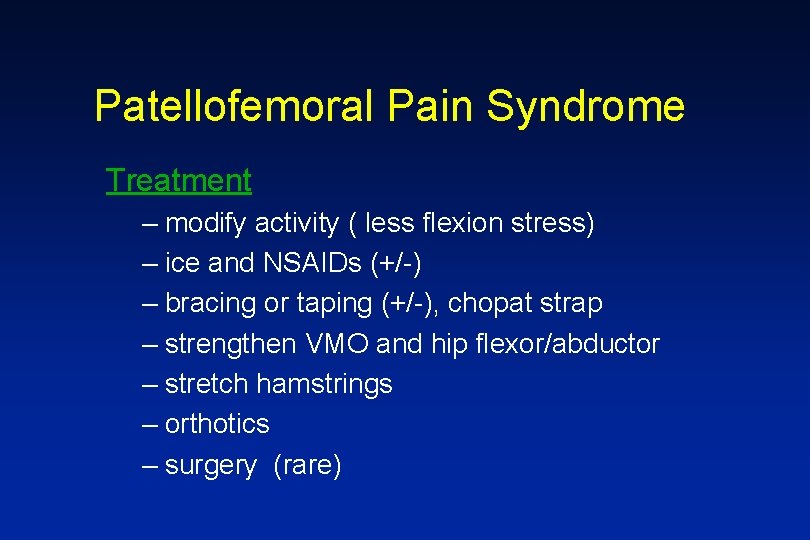
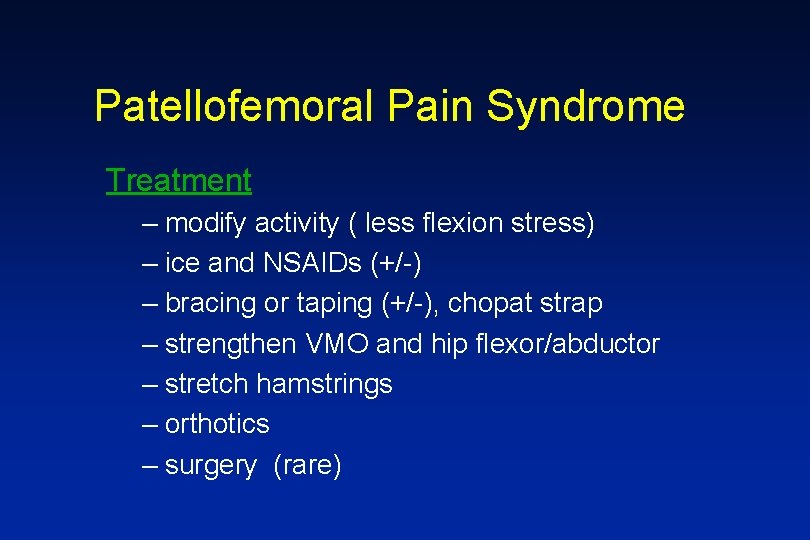
Patellofemoral Pain Syndrome Treatment – modify activity ( less flexion stress) – ice and NSAIDs (+/-) – bracing or taping (+/-), chopat strap – strengthen VMO and hip flexor/abductor – stretch hamstrings – orthotics – surgery (rare)
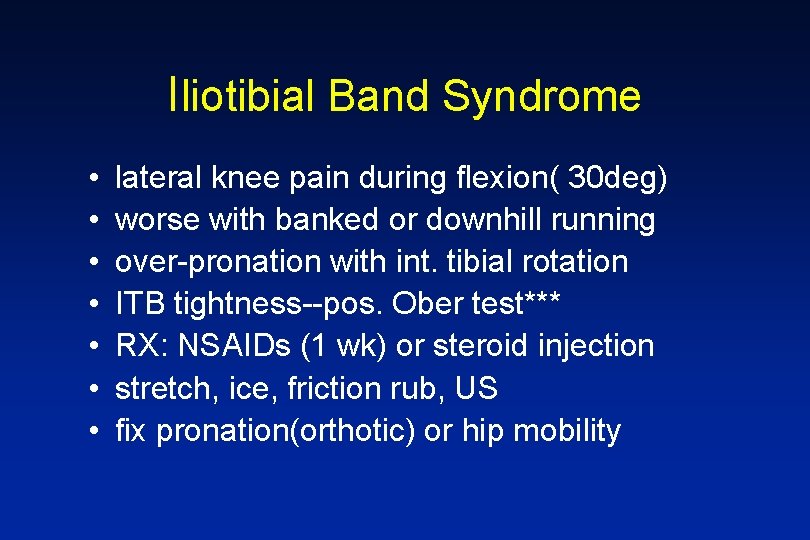
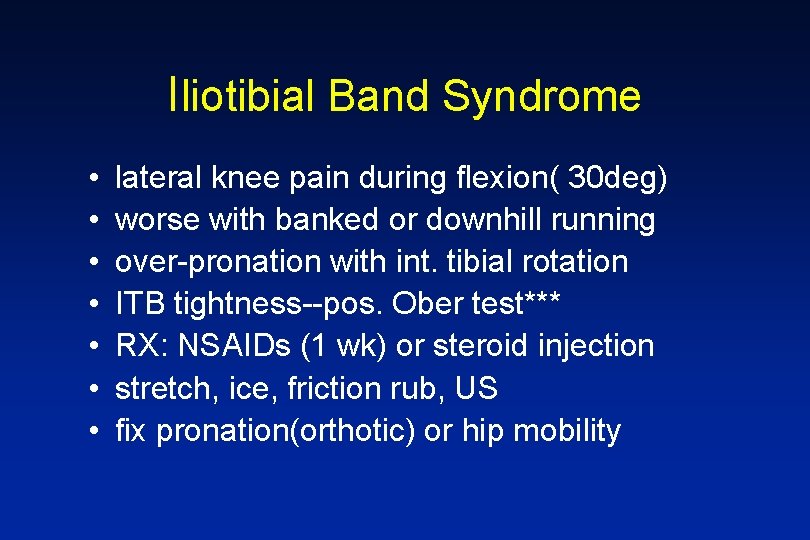
Iliotibial Band Syndrome • • lateral knee pain during flexion( 30 deg) worse with banked or downhill running over-pronation with int. tibial rotation ITB tightness--pos. Ober test*** RX: NSAIDs (1 wk) or steroid injection stretch, ice, friction rub, US fix pronation(orthotic) or hip mobility
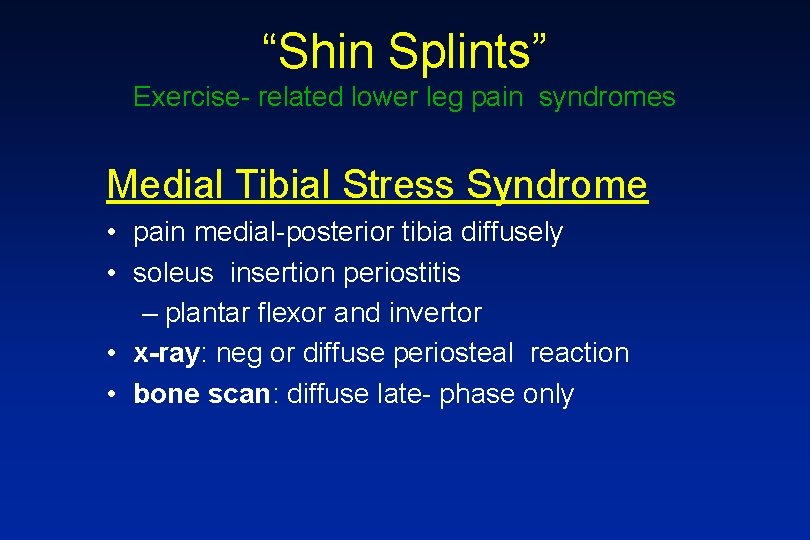
“Shin Splints” Exercise- related lower leg pain syndromes Medial Tibial Stress Syndrome • pain medial-posterior tibia diffusely • soleus insertion periostitis – plantar flexor and invertor • x-ray: neg or diffuse periosteal reaction • bone scan: diffuse late- phase only
Medial Tibial Stress Syndrome Factors • runner, hard surface, poor cushion • poor conditioning, sudden increased intensity and duration ( > 10% per week) • excessive and rapid pronation, tight Achilles
Medial Tibial Stress Syndrome Treatment • relative rest (5 -7 d) • ice massage • NSAIDs • Achilles stretch • better shoes – medial stabilizer – cushioning • not surgery
Lateral Tibial Periostitis • pain lat-ant tibia diffusely • tibialis anterior insertion – dorsiflexor, evertor • x-ray/ bone scan : same • factors: – tight Achilles*** – increased hills/dorsiflexion • Rx: same
Exertional Compartment Syndrome • • • pain increases with activity resolves after rest, not immediate no bone pain muscle herniation is diagnostic elevated compartment pressure(>30 mm hg) – anterior 50 -60% – deep posterior 20 -30% – all others 20% • factors: non-traumatic, unknown • Rx: fasciotomy or limit activity
Nerve and Vascular Entrapment • Peroneal Nerve – Lateral post knee pain – Lateral calf / foot pain and numbness – Peroneal weakness and foot drop • Posterior Tibial Artery – Compressed in the popliteal region – May be positional – May cause pain and numbness
Tibial Stress Fracture • focal tibial pain (esp with 3 pt bending) • medial or lateral (different types) • bending force from muscle tension – tension: ant-lat, mid – compression: post-med, distal/ prox • pain despite rest/ treatment for 2 wks
Tibial Stress Fracture • xray: – medial: focal periosteal thickening (post-med) – lateral: “dreaded black line” fracture (ant-lat) • bone scan: focal uptake( all phases) – positive 3 -5 d post pain increase – key study to diagnose
Imaging in Stress Fracture • bone scan: ( $500) • focal uptake( all phases) – positive 3 -5 d post pain increase – key study to diagnose – Sensitive but not specific • MRI: ( $1500+) – Early-( 1 -3 days) focal T 2 increase signal in area of edema in marrow and bone – Later- low T 1 signal indicates feacture line – Sensitive and specific and anatomic detail
Tibial Stress Fracture Factors • hard surface, poor shoes • anatomical malalignment – foot pronation – leg length, rotation, or hip problem • abrupt training increase • osteoporosis • jumping sports (esp ant-lat tibia fx )
Tibial Stress Fracture • Ant-lateral: caution!! – – higher rate nonunion 20% to full fx average 1 yr off sport consider bone stimulator, IM rod • Medial: – more common – heals with 4 -6 wks rest, slow progress **Often bilateral and recurrent**
Tibial Stress Fracture Treatment • improve shock absorbing or reduce stress - shoes , surface, rest, modified activity • long air casts • orthotic • augment bone healing – No NSAIDs – calcium 1200 mg/day – estrogen status/eating disorder/ osteoporosis

Orthotics • Have been shown to treat 75% of injured runners successfully • Mechanism: limitation of abnormal pronation and subtalar motion • Off -the -shelf models can be as effective, less costly as custom
Stress Fractures • Incidence: track( 13 -52%)- tibia, navic ballet( 22 -45%)- MT, fibula • Most common sites: tibia( 30 -50%), fibula, metatarsal, femur, tarsal (navicular). • Female > male by 3 -10 x • High risk in amenorrhea, high mileage – 37% of college women, 50% amenorrheic - Female Athlete Triad -anorexia, amenorrhea, osteoporosis
Female Athlete Triad • Low energy balance/ Eating disorder – Overtraining – Undereating of calories • Amenorhea – Fewer that 4 menstrual periods/ yr • Osteoporosis
Low Iron: Runners Anemia • Runners consume more iron that general public • Low iron effects performance • Screen females/? men with ferritin – Level above 30 -60 is probably best Iron is best taken as food items: meats, fish, legumes, greens, tofu, eggs , nuts, dried fruits Supplement if low: caution for overload
High Risk Stress Fractures • • Femoral neck Anterior cortex tibia Tarsal navicular Base of 5 th metatarsal -Often delay in diagnosis -Poor outcomes if not treated with proper immolization and non-wt bearing
Femoral Neck Stress Fractures • • • Vague anterior thigh or groin pain Pain with extreme IR/ER or hopping on leg Average 3 month delay in diagnosis, AVN risk Lateral -superior, tension side -- serious Medial, compression---less serious MRI superior to bone scan – 1: edema only – 2: fracture line less than 50% – 3: fracture line > 50%
Femoral Neck Stress Fractures • Non-wt bearing until asymptomatic – Usually 4 -8 weeks initially • Progressive functional rehabilitation • Re image if not progressing as expected • Refer to orthopaedic surgeon if fracture line is >50% to consider immediate pinning
Stress Fractures • Healing- average 3 -6 weeks 2 wks: metatarsal and fibula 6 -8 wks: most other bones 4+ months: anterior tibia, navicular, Jones fx • Localized SF heals 2 x rate of complete SF • Recurrence: 50% overall (13% at 1 yr)
Plantar Fasciitis • most common cause of heal pain • medial calcaneal tubercle, origin of central band of plantar fascia • painful first step of the morning • relieved with exercise, pain resting • no pain with lateral compression • xray rarely useful, spur irrelevant
Plantar Fasciitis Factors • • • excess pronation or high, rigid arch women > men overweight and/or overtraining poor arch support or cushion tight heel cords
Plantar Fasciitis Treatment • • • modify activity and weight orthotics, arch support, or heel cups ice and NSAIDs stretch Achilles and calves cortisone shot (caution fat pad atrophy) nite splints (83% effective if used right)
Achilles Tendinitis • 15% of all running injuries • mostly males • Achilles takes highest force in the body- up to 8 x body wt , running • combined gastrocs and soleus • occurs 2 -6 cm above calcaneus at site of low blood flow • usually tendinosis when chronic
Achilles Tendinitis Factors 1. poor body mechanics - poor flexibility or alignment 2. training errors 3. environmental factors 4. athletic shoes
Achilles Tendinitis Treatment • Physical therapy – specialized stretch program – ice and/or ultrasound • NSAIDs but no cortisone injections • Orthotics and initial heel lift • Surgery- 90% to full activity and 75% to high level
Running Shoe Prescription • Evaluate shoe wear pattern and foot type – Rigid foot – Normal foot – Floppy Foot • Shoe type
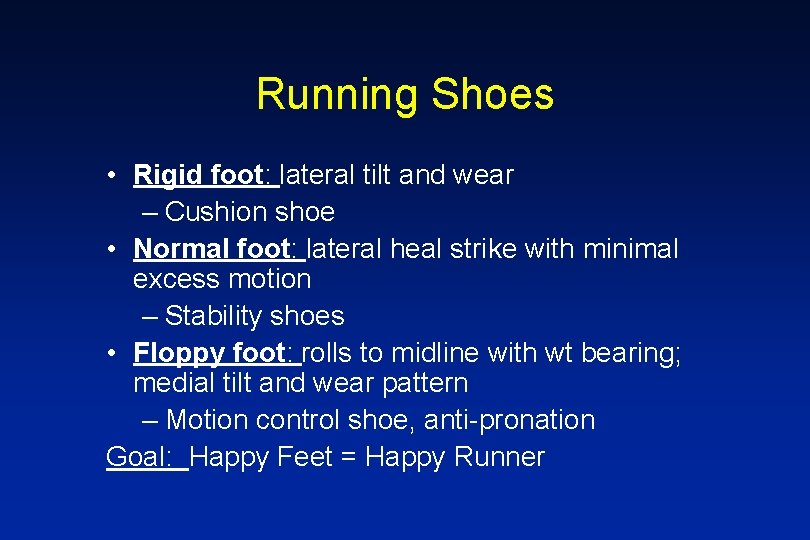
Running Shoes • Rigid foot: lateral tilt and wear – Cushion shoe • Normal foot: lateral heal strike with minimal excess motion – Stability shoes • Floppy foot: rolls to midline with wt bearing; medial tilt and wear pattern – Motion control shoe, anti-pronation Goal: Happy Feet = Happy Runner
References • Asplund C, Brown D. The Running Shoe Presciption. The Phys and Sportsmed. Vol. 33 (1), Jan 2005. • Cole C, Seto C, Gazewood J. Plantar Fasciitis: Evidenced-Based Review of Diagnosis and Therapy. Am Fam Phys. , Vol 72 ( 11), Dec 2005. • Hreljac A. Impact and Overuse Injuries in Runners. Med Sc in Sports & Exercise. Vol 36 (5), 2004. • Hurwitz S. Athletic Foot and Ankle Injuries. Clinics in Sports Medicine. Vol 23 (1), Jan 2004.
References • Kennedy J, et al. Foot and ankle injuries in the adolescent runner. Current Opinion in Pediatrics. Vol 17, 2005. • Lun V, Meeuwisse WH, et al. Relation between running injury and static lower limb alignment in recreational runners. Br. J. Sports Med. Vol 38, 2004. • Mellion M, et al. The Team Physician’s Handbook, 2 nd ed. Hanley and Belfus. 1997. • Niemuth P et al. Hip Muscle Weakness and Overuse Injuries in Recreational Runners. Clin J Sports Med. Vol 15 (1), Jan 2005.
 Jim chesnutt
Jim chesnutt Once upon a time there lived a little girl name
Once upon a time there lived a little girl name Running running running
Running running running The wife of his youth
The wife of his youth Uc davis web scheduler
Uc davis web scheduler Injuries to muscles and bones chapter 15
Injuries to muscles and bones chapter 15 Sentinel injuries in infants are
Sentinel injuries in infants are How are sports injuries classified and managed
How are sports injuries classified and managed Who do dill and scout meet outside?
Who do dill and scout meet outside? Injury prevention, safety and first aid
Injury prevention, safety and first aid Chapter 12 lesson 2 improving your fitness
Chapter 12 lesson 2 improving your fitness Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Neil beidleman
Neil beidleman Which osha document summarizes occupational injuries
Which osha document summarizes occupational injuries Examples of intentional injury
Examples of intentional injury Bo taoshi injuries
Bo taoshi injuries An epidemiologic survey of roller skating injuries
An epidemiologic survey of roller skating injuries Westfield sports injuries
Westfield sports injuries Chapter 14:2 preventing accidents and injuries
Chapter 14:2 preventing accidents and injuries Chop saw injuries
Chop saw injuries Common track and field injuries
Common track and field injuries Emergency care and first aid ppt
Emergency care and first aid ppt Chapter 4 preventing injuries through fitness
Chapter 4 preventing injuries through fitness Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Unit 15:7 providing first aid for heat exposure
Unit 15:7 providing first aid for heat exposure Sports injuries angus, on
Sports injuries angus, on Glycerin and gelatin fake skin
Glycerin and gelatin fake skin Climatic injury
Climatic injury Chapter 14 bleeding shock and soft tissue injuries
Chapter 14 bleeding shock and soft tissue injuries Glasgow minor injuries
Glasgow minor injuries Deadly dozen itls
Deadly dozen itls The hunger games chapter 18 questions and answers
The hunger games chapter 18 questions and answers Injuries first aid
Injuries first aid Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Miniscus replacement
Miniscus replacement Kristen wilson injuries
Kristen wilson injuries Chapter 17 providing first aid
Chapter 17 providing first aid What is katniss’ prediction as she readies herself?
What is katniss’ prediction as she readies herself? Fundamentals of throwing a football
Fundamentals of throwing a football Poem about intentional injuries
Poem about intentional injuries Jsp 539
Jsp 539 Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries This technique requires two sturdy poles and a blanket
This technique requires two sturdy poles and a blanket Carl clinton construction
Carl clinton construction Characters of firearm injuries
Characters of firearm injuries Preventing hand injuries
Preventing hand injuries Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Evaluating sales force performance
Evaluating sales force performance In identifying company resources with competitive value
In identifying company resources with competitive value Order of operations and evaluating expressions
Order of operations and evaluating expressions Interior backgrounds
Interior backgrounds