Eugene Yevstratov MD Institute of Cardiology and Cardiovascular



- Slides: 27
Eugene Yevstratov, MD Institute of Cardiology and Cardiovascular Surgery, Favaloro Foundation Buenos Aires, Argentina October/2002
Goals of Myocardial protection 1. Protect against ischemic injury 2. Provide a motionless, bloodless field 3. Allow effective post-ischemic myocardial resuscitation
Spectrum of myocardial ischemic injury Acute ischemic disfunction Preconditioning Stunning Hibernation Necrosis vs. Apoptosis
Acute ischemic disfunction Reversible contractile failure Perfusion pressure O 2 supply Inmediate recovery

Preconditioning Reversible Slowed energy utilization Reduction in myocardial necrosis Increase protective abilities of myocardium Presented as a normal proper protective reaction of the ischemic myocardium Recovery Hs, Ds
Stunning Parcialy Reversible May be accompained by endothelial disfunction (NO) causing reduced coronary blood flow Result of ischemia-reperfusion insult Mediated by increased intracellular Ca accumulation Recovery in Hs, Wks
Hibernation Parcialy Reversible Related to poor myocardial blood flow Chronic Recovery Wks, Mo
Necrosis Irreversible Hyper contracture - “contracture band necrosis”, “stone heart” Osmotic/ionic dysregulation, membrane injury Cell swelling&disruption Lysis
Apoptosis Irreversible Death signal Cell shrinkage Cytoplasmic and nuclear condensation Phagocytosis
Systems involved into membrane injury MAC( membrane attack complex) Adenosine dependent receptors K+ATP dependent chanels NHE(sodium hydrogen exchanger)
Cellular effects of ischemia Altered membrane potential Altered ion distribution(increase intracellular. Ca++/Na++) Cellular swelling Cytoskeletal Disorganisation Increased hypoxantine Decreased ATP Decreased phosphocreatine Decreased Glutatione Cellular Acidosis
Straqtegies for Heart protection Increase the O 2 offer Decreae oxygen demand Methabolical intervention Prevention of demand increased Substrate disponsability
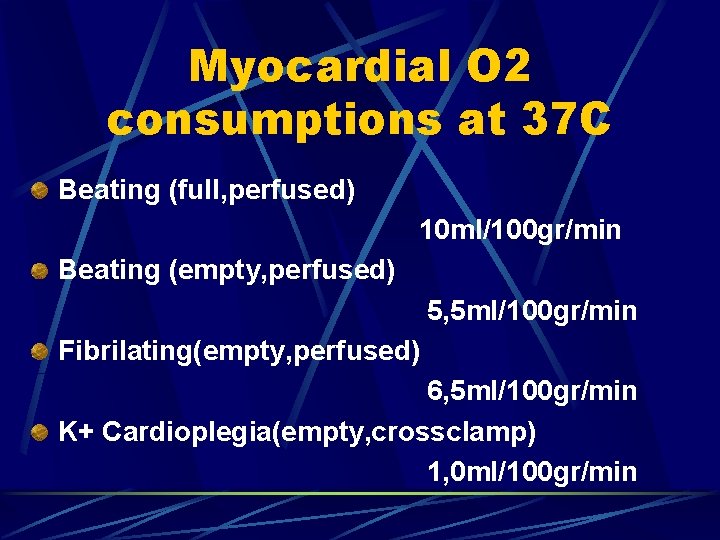
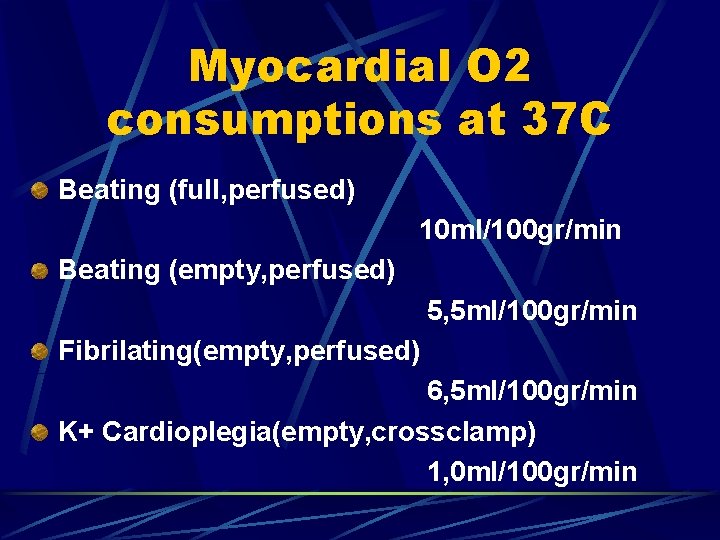
Myocardial O 2 consumptions at 37 C Beating (full, perfused) 10 ml/100 gr/min Beating (empty, perfused) 5, 5 ml/100 gr/min Fibrilating(empty, perfused) 6, 5 ml/100 gr/min K+ Cardioplegia(empty, crossclamp) 1, 0 ml/100 gr/min
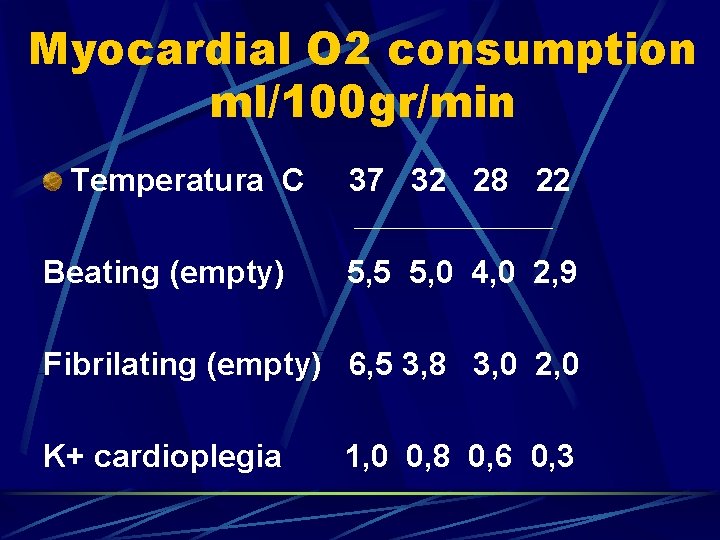
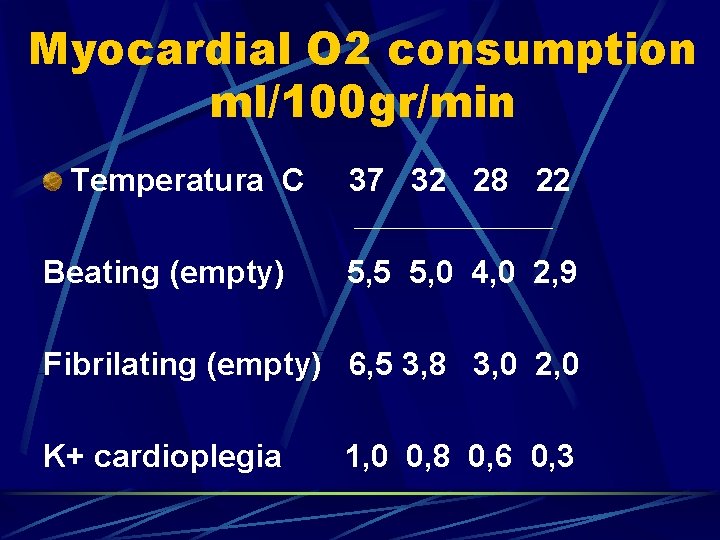
Myocardial O 2 consumption ml/100 gr/min Temperatura C Beating (empty) 37 32 28 22 5, 5 5, 0 4, 0 2, 9 Fibrilating (empty) 6, 5 3, 8 3, 0 2, 0 K+ cardioplegia 1, 0 0, 8 0, 6 0, 3
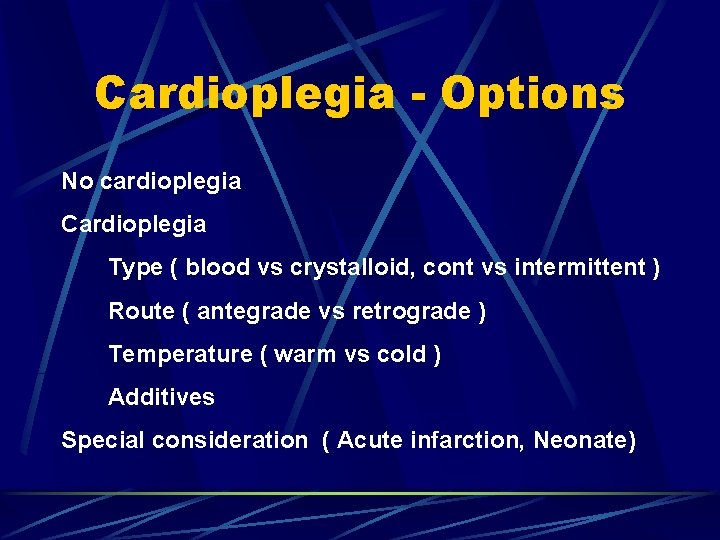
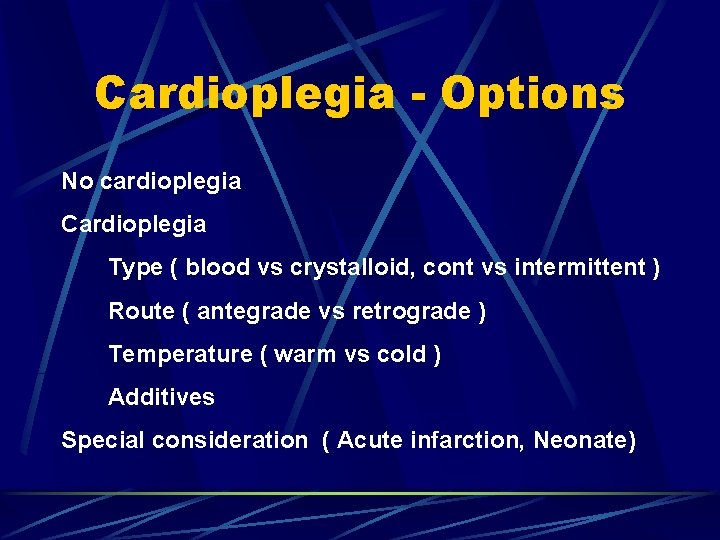
Cardioplegia - Options No cardioplegia Cardioplegia Type ( blood vs crystalloid, cont vs intermittent ) Route ( antegrade vs retrograde ) Temperature ( warm vs cold ) Additives Special consideration ( Acute infarction, Neonate)

Rivero Cardioplegia solutions 1 2
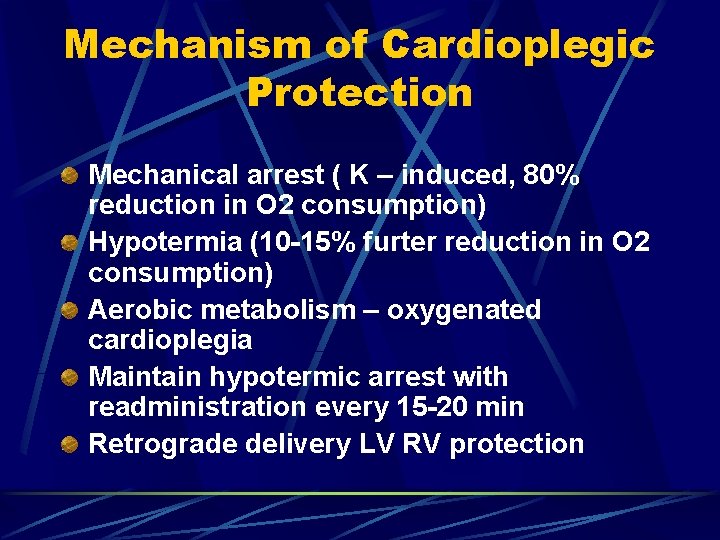
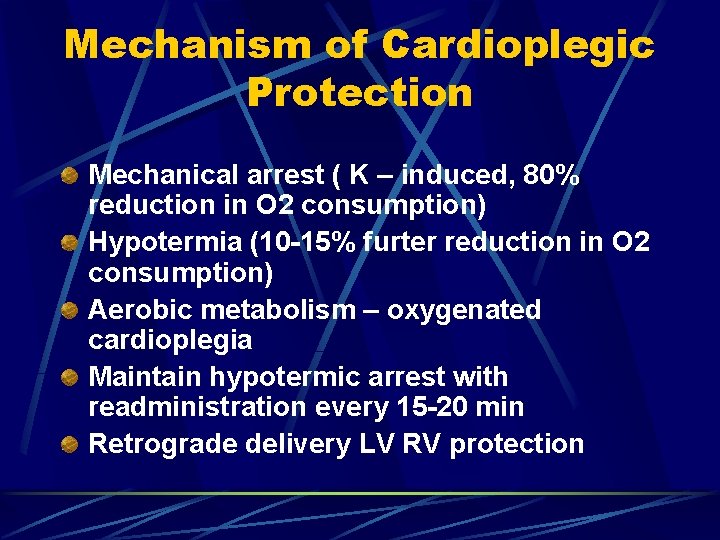
Mechanism of Cardioplegic Protection Mechanical arrest ( K – induced, 80% reduction in O 2 consumption) Hypotermia (10 -15% furter reduction in O 2 consumption) Aerobic metabolism – oxygenated cardioplegia Maintain hypotermic arrest with readministration every 15 -20 min Retrograde delivery LV RV protection
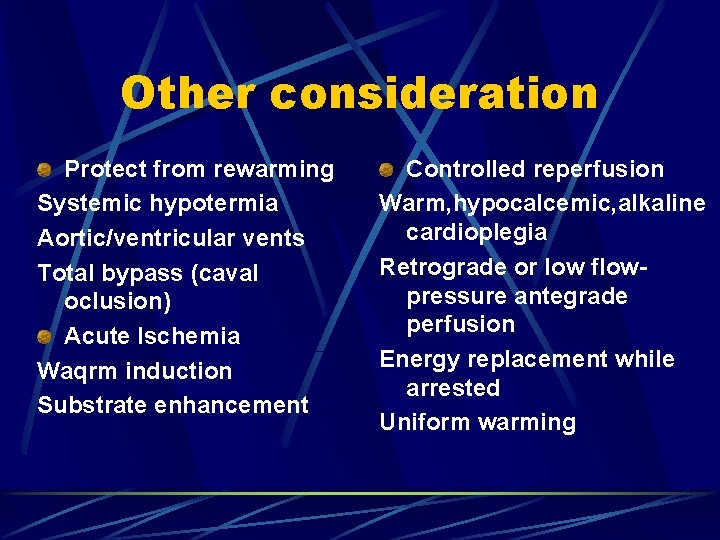
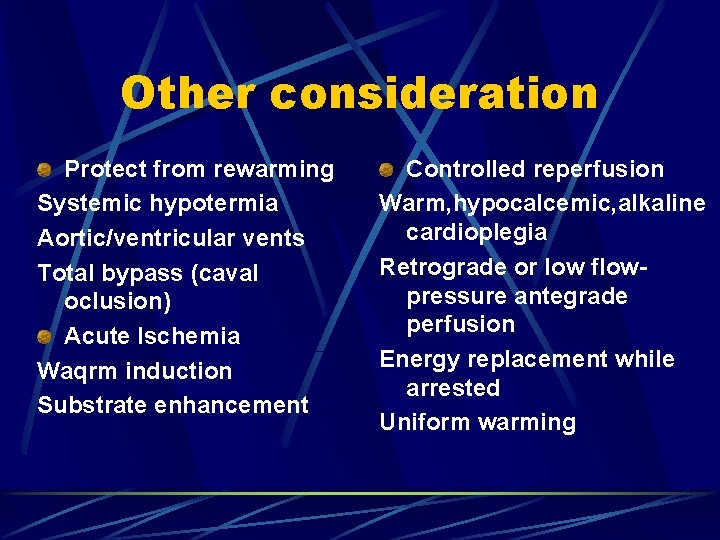
Other consideration Protect from rewarming Systemic hypotermia Aortic/ventricular vents Total bypass (caval oclusion) Acute Ischemia Waqrm induction Substrate enhancement Controlled reperfusion Warm, hypocalcemic, alkaline cardioplegia Retrograde or low flowpressure antegrade perfusion Energy replacement while arrested Uniform warming
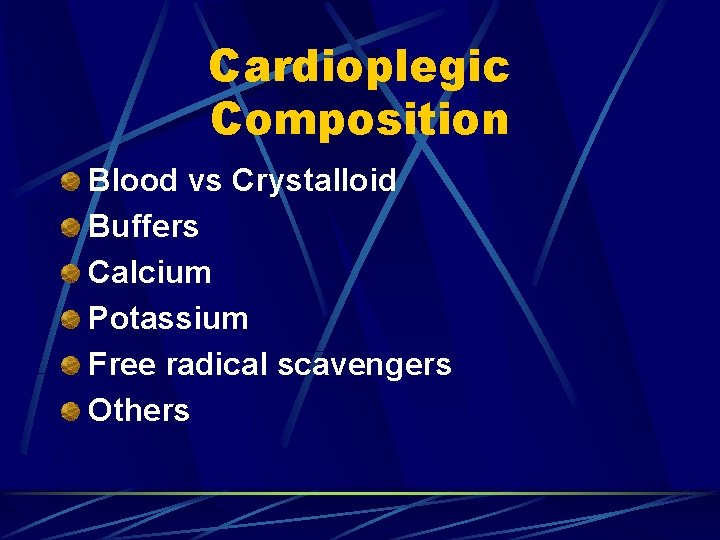
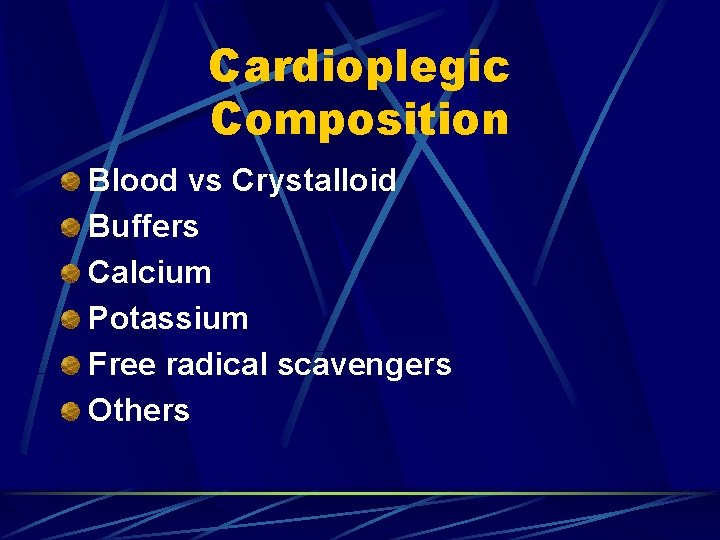
Cardioplegic Composition Blood vs Crystalloid Buffers Calcium Potassium Free radical scavengers Others
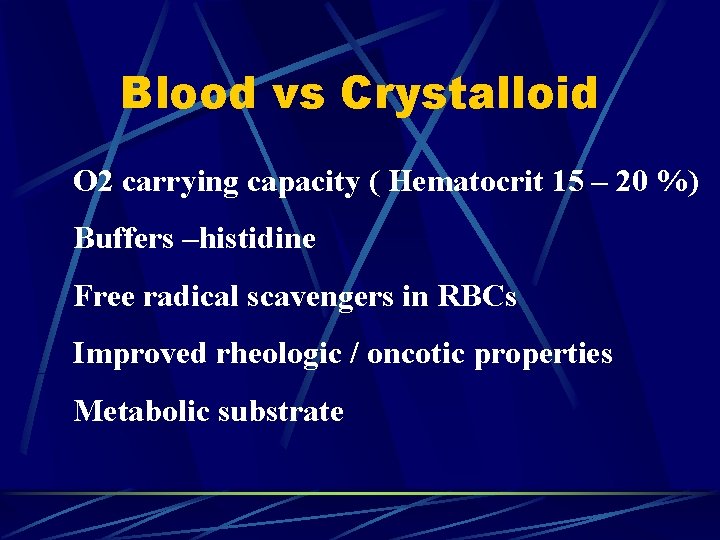
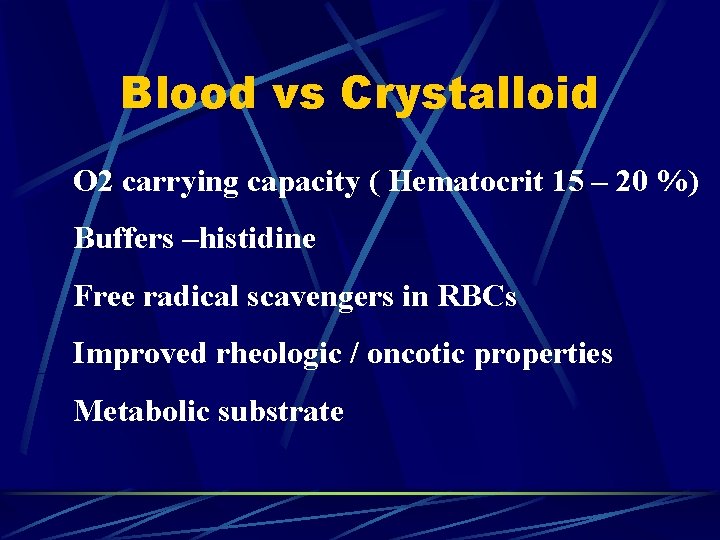
Blood vs Crystalloid O 2 carrying capacity ( Hematocrit 15 – 20 %) Buffers –histidine Free radical scavengers in RBCs Improved rheologic / oncotic properties Metabolic substrate
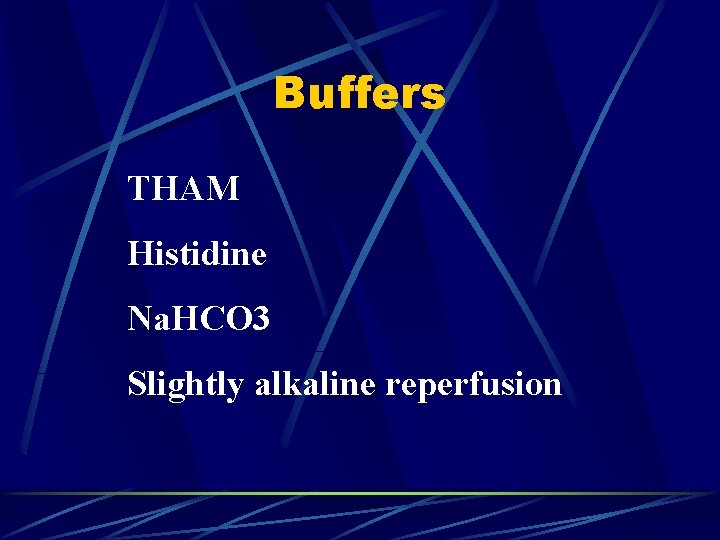
Buffers THAM Histidine Na. HCO 3 Slightly alkaline reperfusion
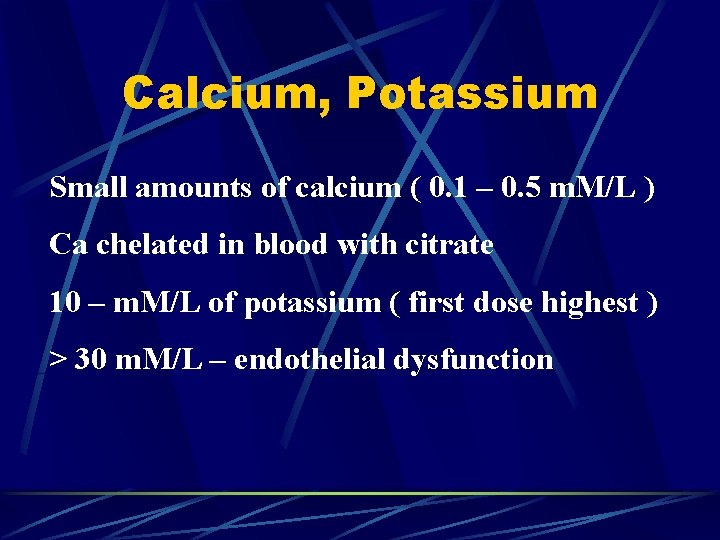
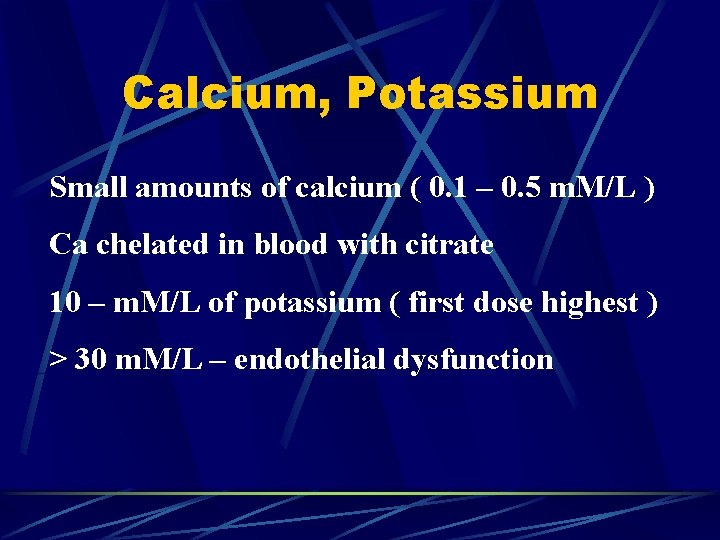
Calcium, Potassium Small amounts of calcium ( 0. 1 – 0. 5 m. M/L ) Ca chelated in blood with citrate 10 – m. M/L of potassium ( first dose highest ) > 30 m. M/L – endothelial dysfunction
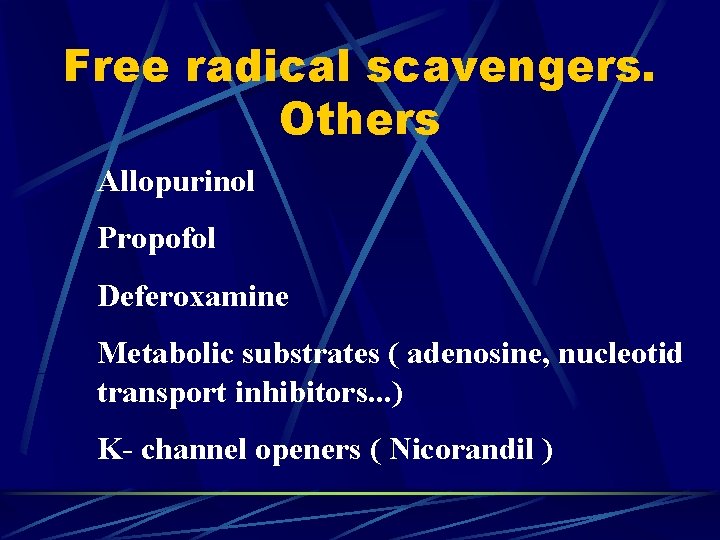
Free radical scavengers. Others Allopurinol Propofol Deferoxamine Metabolic substrates ( adenosine, nucleotid transport inhibitors. . . ) K- channel openers ( Nicorandil )
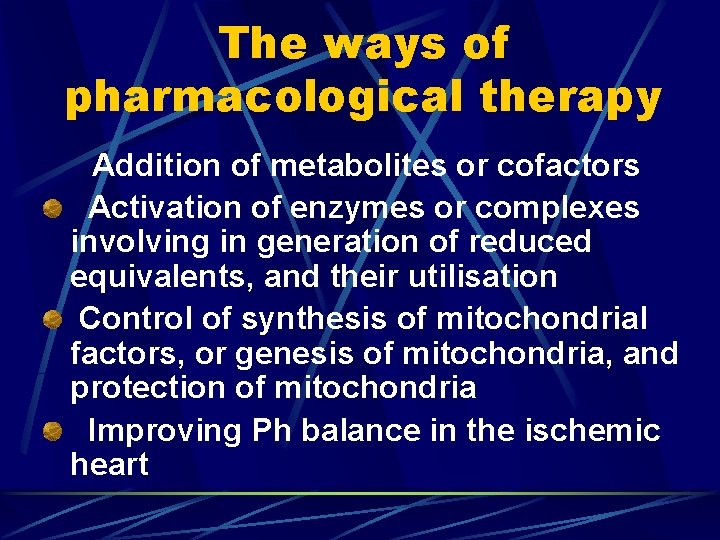
The ways of pharmacological therapy Addition of metabolites or cofactors Activation of enzymes or complexes involving in generation of reduced equivalents, and their utilisation Control of synthesis of mitochondrial factors, or genesis of mitochondria, and protection of mitochondria Improving Ph balance in the ischemic heart

Institute of Cardiology and Cardiovascular Surgery, Favaloro Foundation Buenos Aires, Argentina The End Eugene Yevstratov E-mail Fax 001775 679 2870
 Cardiovascular research institute basel
Cardiovascular research institute basel Westcliffe medical centre shipley
Westcliffe medical centre shipley Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Cardiology procedures chapter 47
Cardiology procedures chapter 47 Accp cardiology prn
Accp cardiology prn Acc sports cardiology
Acc sports cardiology Service line management
Service line management Gpwsi cardiology
Gpwsi cardiology Muse cardiology
Muse cardiology Elias hanna cardiology
Elias hanna cardiology Craig ainsworth cardiology
Craig ainsworth cardiology Hall-garcia cardiology associates
Hall-garcia cardiology associates Enloe cardiology
Enloe cardiology Justin davies cardiology
Justin davies cardiology Cardiology structured reporting
Cardiology structured reporting Accp cardiology prn journal club
Accp cardiology prn journal club Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Formal equivalence and dynamic equivalence examples
Formal equivalence and dynamic equivalence examples Chapter 19 the cardiovascular system blood vessels
Chapter 19 the cardiovascular system blood vessels Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Maniobra de azoulay
Maniobra de azoulay What makes up the circulatory system
What makes up the circulatory system Rias cardiovascular
Rias cardiovascular Rat cardiovascular system simulation
Rat cardiovascular system simulation Fresenius ncp
Fresenius ncp Cardiovascular/lymphatic system it's totally tubular
Cardiovascular/lymphatic system it's totally tubular When does stroke volume increase
When does stroke volume increase