Drug Induced Renal Diseases Dr Marriam Zaka Lecturer

- Slides: 30
Drug Induced Renal Diseases Dr. Marriam Zaka Lecturer Institute of Pharmacy, Faculty of Pharmaceutical and Allied Health Sciences LCWU, Lahore.
Kidney Function Along with the liver, the kidneys are another part of the waste processing system of the body -- thus urine goes from the kidneys into the bladder. The kidneys also help regulate blood pressure and the production of red blood cells.
What tests are run to assess kidney function? we cannot live without adequately functioning kidneys. Therefore, it may be necessary with certain drugs to run some of the following tests periodically to determine whether those drugs are harming this vital organs. The following tests are often given monthly as part of the complete metabolic panel with blood drawn before or during regular monitoring of diseases.
BUN (Blood Urea Nitrogen or Urea Nitrogen). This is the concentration of nitrogen(within urea) in the serum(but not in red blood cells). A waste product, derived from protein breakdown, produced in the liver and excreted by way of the kidneys. High values may mean that the kidneys are not working as well as they should. BUN is also elevated by blood loss, dehydration, high protein diets and/or strenuous exercise which may temporarily and artificially raise levels. A low BUN level may be the result of liver disease, a low protein diet, pregnancy, or drinking an extreme amount of water.
Creatinine. A waste product largely from muscle metabolism (breakdown). Concentration of creatinine in the blood depends upon the amount of muscle that you have and the ability of your kidneys to excrete creatinine. High values, especially with high BUN levels, may indicate problems with the kidneys. Low values are generally not considered significant.
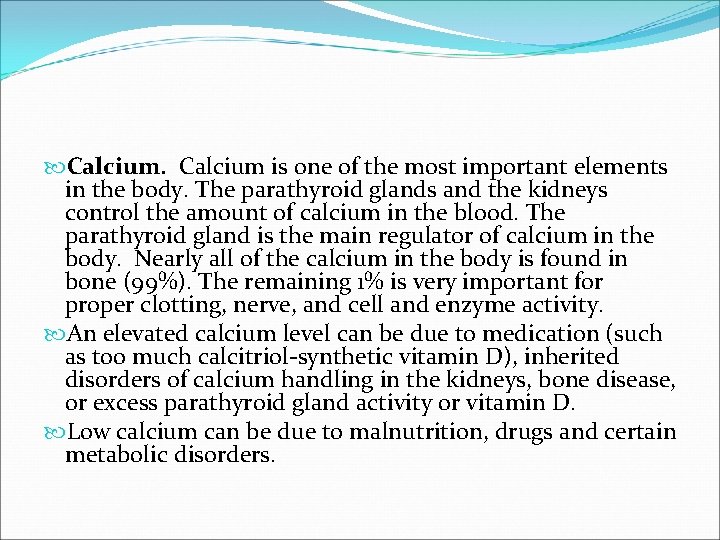
Calcium is one of the most important elements in the body. The parathyroid glands and the kidneys control the amount of calcium in the blood. The parathyroid gland is the main regulator of calcium in the body. Nearly all of the calcium in the body is found in bone (99%). The remaining 1% is very important for proper clotting, nerve, and cell and enzyme activity. An elevated calcium level can be due to medication (such as too much calcitriol-synthetic vitamin D), inherited disorders of calcium handling in the kidneys, bone disease, or excess parathyroid gland activity or vitamin D. Low calcium can be due to malnutrition, drugs and certain metabolic disorders.
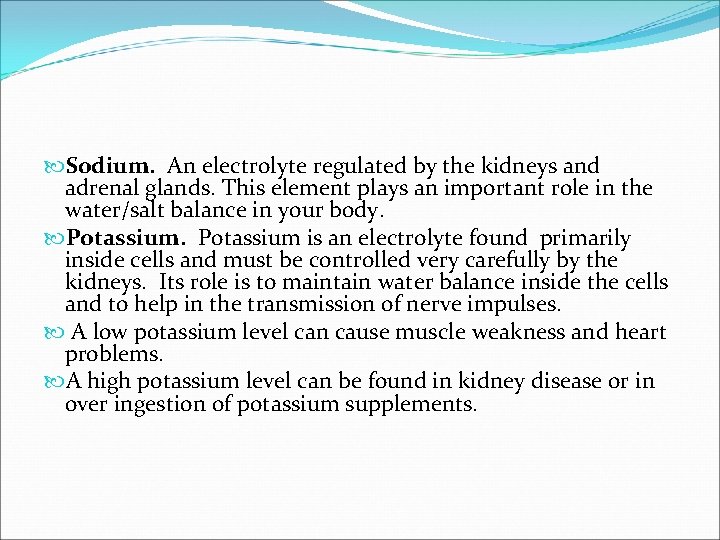
Sodium. An electrolyte regulated by the kidneys and adrenal glands. This element plays an important role in the water/salt balance in your body. Potassium is an electrolyte found primarily inside cells and must be controlled very carefully by the kidneys. Its role is to maintain water balance inside the cells and to help in the transmission of nerve impulses. A low potassium level can cause muscle weakness and heart problems. A high potassium level can be found in kidney disease or in over ingestion of potassium supplements.
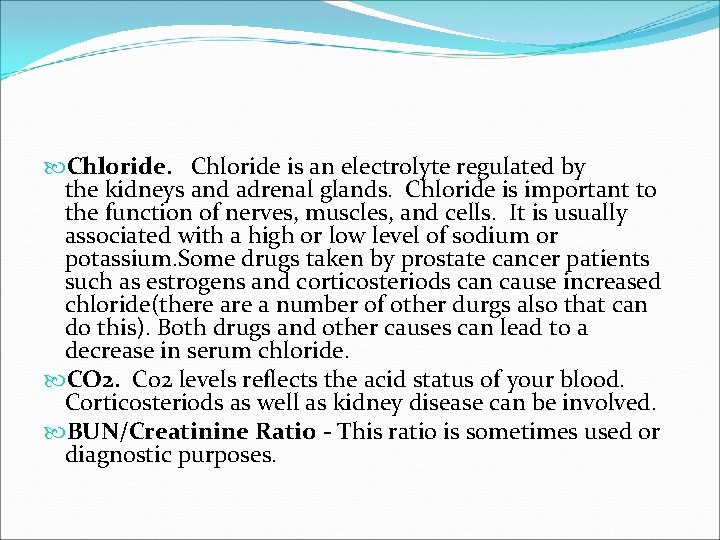
Chloride is an electrolyte regulated by the kidneys and adrenal glands. Chloride is important to the function of nerves, muscles, and cells. It is usually associated with a high or low level of sodium or potassium. Some drugs taken by prostate cancer patients such as estrogens and corticosteriods can cause increased chloride(there a number of other durgs also that can do this). Both drugs and other causes can lead to a decrease in serum chloride. CO 2. Co 2 levels reflects the acid status of your blood. Corticosteriods as well as kidney disease can be involved. BUN/Creatinine Ratio - This ratio is sometimes used or diagnostic purposes.
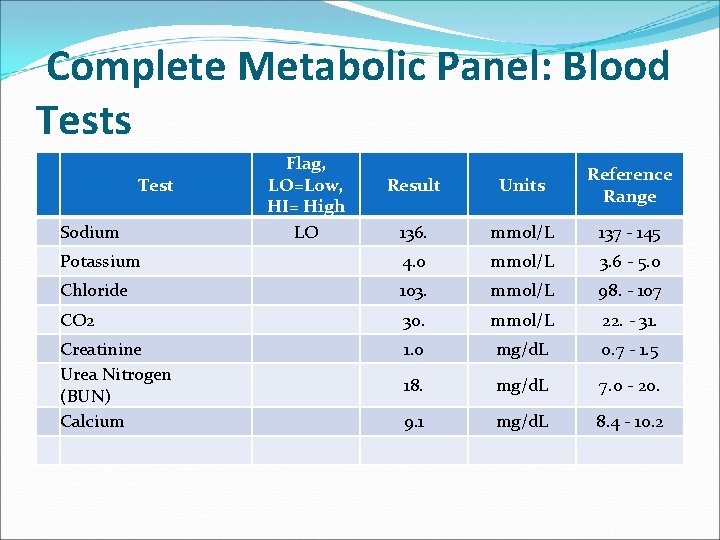
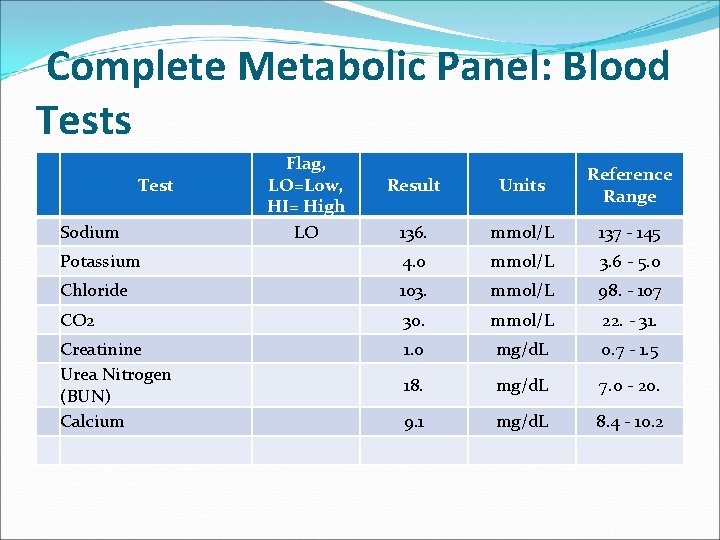
Complete Metabolic Panel: Blood Tests Test Sodium Flag, LO=Low, HI= High LO Result Units Reference Range 136. mmol/L 137 - 145 Potassium 4. 0 mmol/L 3. 6 - 5. 0 Chloride 103. mmol/L 98. - 107 CO 2 30. mmol/L 22. - 31. Creatinine Urea Nitrogen (BUN) Calcium 1. 0 mg/d. L 0. 7 - 1. 5 18. mg/d. L 7. 0 - 20. 9. 1 mg/d. L 8. 4 - 10. 2
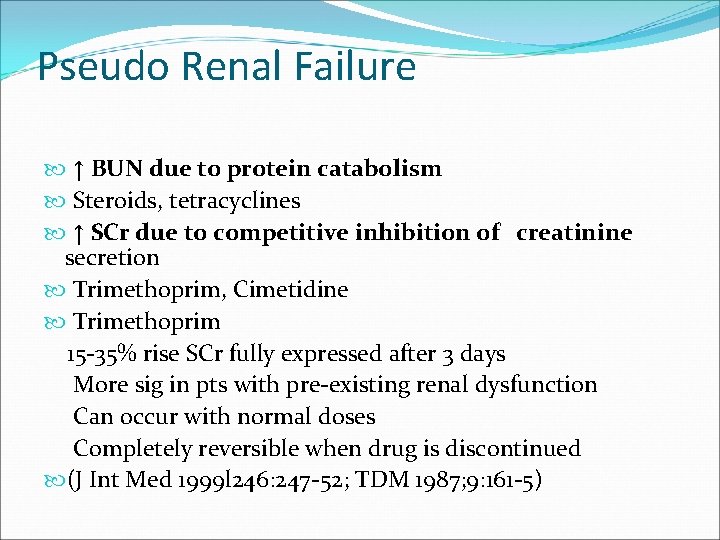
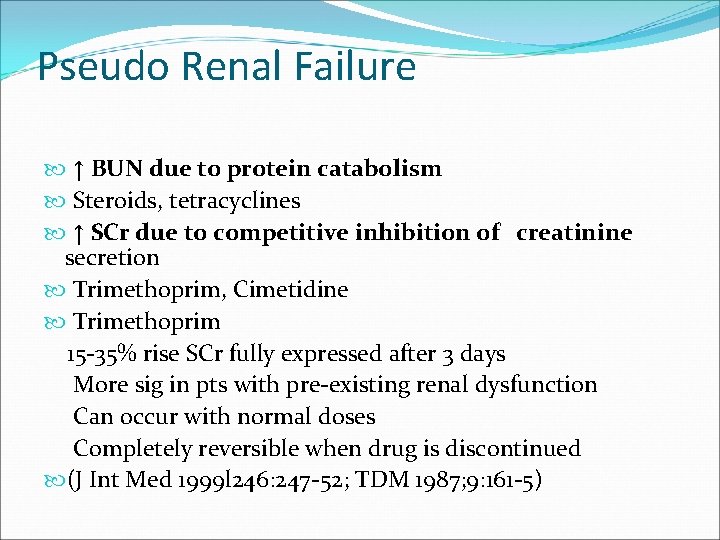
Pseudo Renal Failure ↑ BUN due to protein catabolism Steroids, tetracyclines ↑ SCr due to competitive inhibition of creatinine secretion Trimethoprim, Cimetidine Trimethoprim 15 -35% rise SCr fully expressed after 3 days More sig in pts with pre-existing renal dysfunction Can occur with normal doses Completely reversible when drug is discontinued (J Int Med 1999 l 246: 247 -52; TDM 1987; 9: 161 -5)
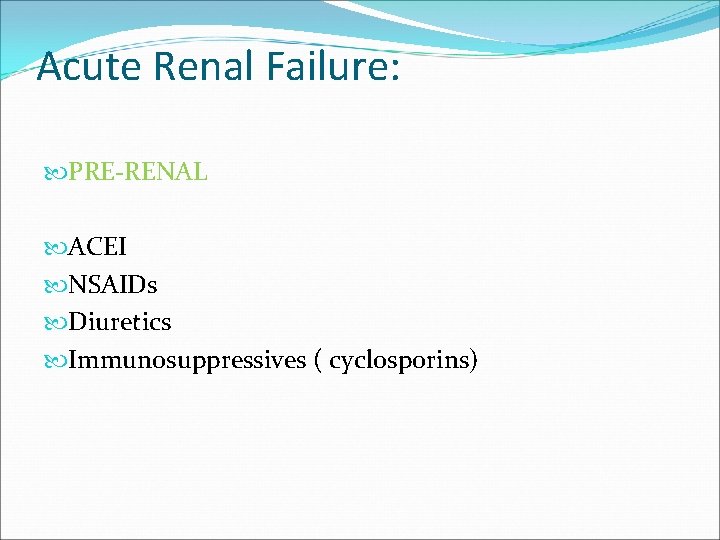
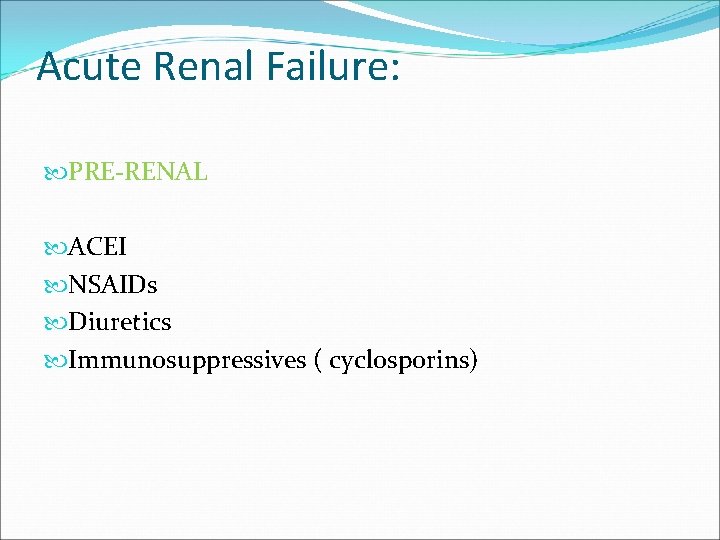
Acute Renal Failure: PRE-RENAL ACEI NSAIDs Diuretics Immunosuppressives ( cyclosporins)
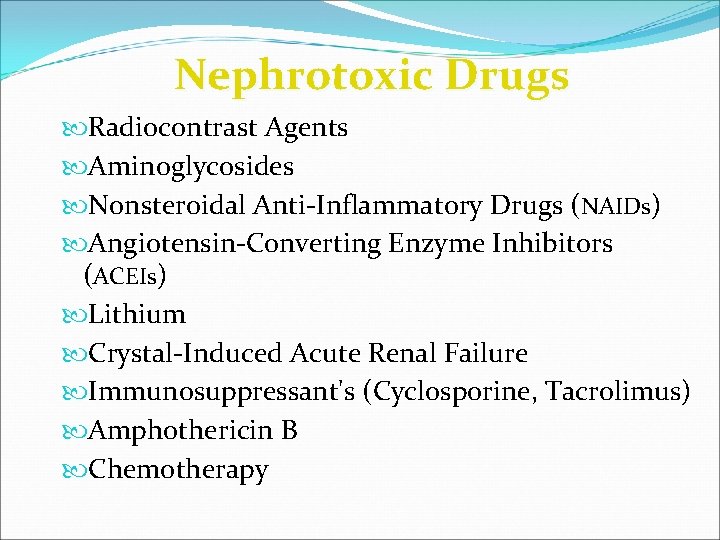
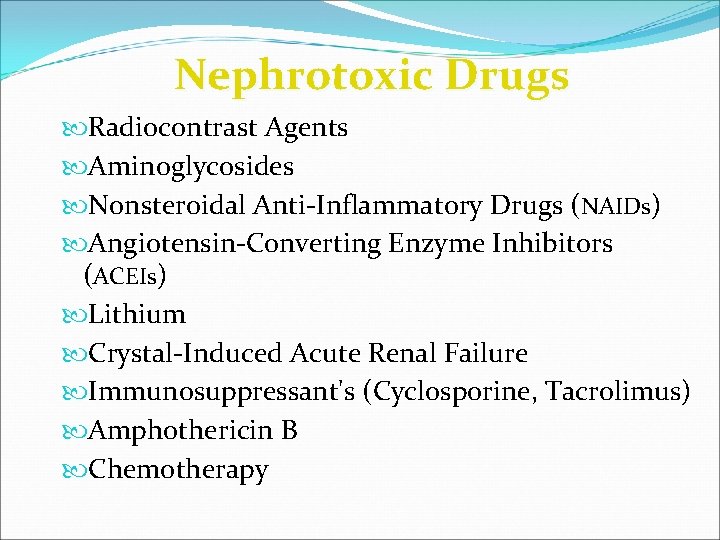
Nephrotoxic Drugs Radiocontrast Agents Aminoglycosides Nonsteroidal Anti-Inflammatory Drugs (NAIDs) Angiotensin-Converting Enzyme Inhibitors (ACEIs) Lithium Crystal-Induced Acute Renal Failure Immunosuppressant's (Cyclosporine, Tacrolimus) Amphothericin B Chemotherapy
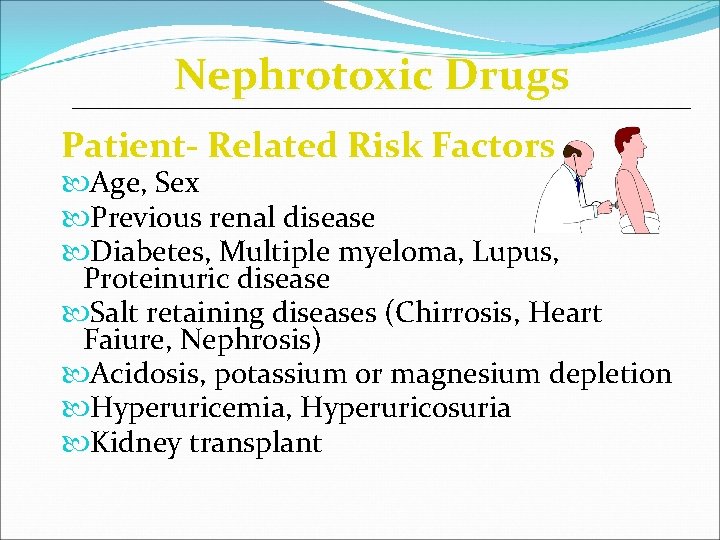
Nephrotoxic Drugs Patient- Related Risk Factors Age, Sex Previous renal disease Diabetes, Multiple myeloma, Lupus, Proteinuric disease Salt retaining diseases (Chirrosis, Heart Faiure, Nephrosis) Acidosis, potassium or magnesium depletion Hyperuricemia, Hyperuricosuria Kidney transplant

Nephrotoxic Drugs Drug - Related Risk Factors Inherent nephrotoxic effects Dose Duration, frequency and form of administration Repeated exposure Drug interaction (synergistic toxic effects)
Radiocontrast Agents First generation - Ionic monomers, hyperosmolal; Diatrizoate, Iothalamate Second generation: Nonionic monomers, lower osmolality Iopamidol, Iohexol, Iopromide, Ioversol Newest agents: Nonionic dimers, iso-osmolal Iodixanol
Radiocontrast Agents Risk Factors: Underlying renal disease (Cr >1. 5 mg/d. L) Diabetic nephropathy, Heart Failure, i. e. Hypovolemia Multiple Myeloma Dose (lower doses safer but not necessarily safe)
Radiocontrast Agents Incidence Negligible when renal function is normal (even if diabetic) 4 -11% in patients with Cr 1. 5 – 4. 0 mg/d. L 50% if Cr > 4. 0 mg/d. L and in diabetic nephropathy Diagnosis Characteristic rise in plasma Cr following administration of the agent
Radiocontrast Agents Therapy: Hydratation √ ; Mannitol ? Diuretics ? Acetylcystein, theophyllin, calcium channel blockers Prevention: Use of alternative diagnostic procedures in high risk patients Avoidance of volume deletion or other nephrotoxins Low-doses of low- or iso-somolar agent IV saline or acetylcysteine
Aminoglycosides Amikacin Gentamicin Neomicin Kanamicin Streptomycin Tobramycin
Aminoglycosides Patient- Related Risk Factors n Age n Previous renal disease n Dehydratation, Volume depletion n Potassium or magnesium depletion n Liver Disease (renal hypoperfusion) n Sepsis ( endotixuns, volume depletion, renal hypo perfusion)
Aminoglycosides Drug - Related Risk Factors n Inherent nephrotoxic effects Gentamicin > Amikicin & Tombamycin n Prolonged high trough levels (> 2. 0 ng/ml) n Dose; Duration; Frequency Single daily dose; “Post-antibiotic” effect n Drug interaction: Cephalothin Cyclosporin A; Cisplatin, Cephalosporins, NSAIDs, ACEIs, Diuretics
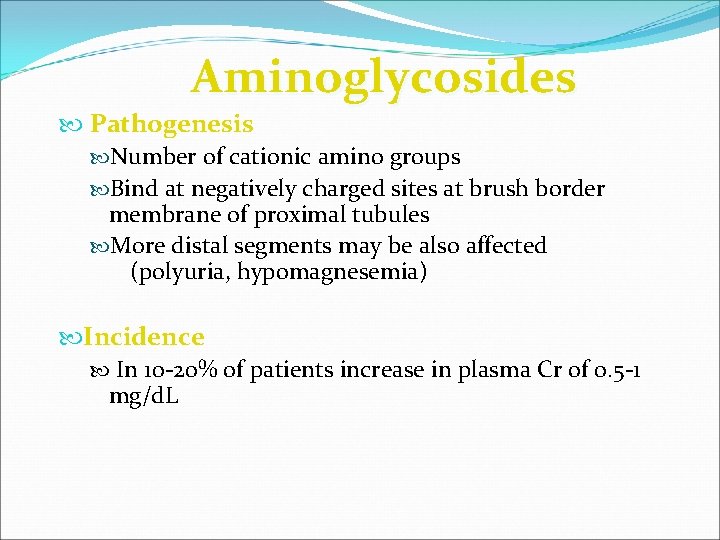
Aminoglycosides Pathogenesis Number of cationic amino groups Bind at negatively charged sites at brush border membrane of proximal tubules More distal segments may be also affected (polyuria, hypomagnesemia) Incidence In 10 -20% of patients increase in plasma Cr of 0. 5 -1 mg/d. L
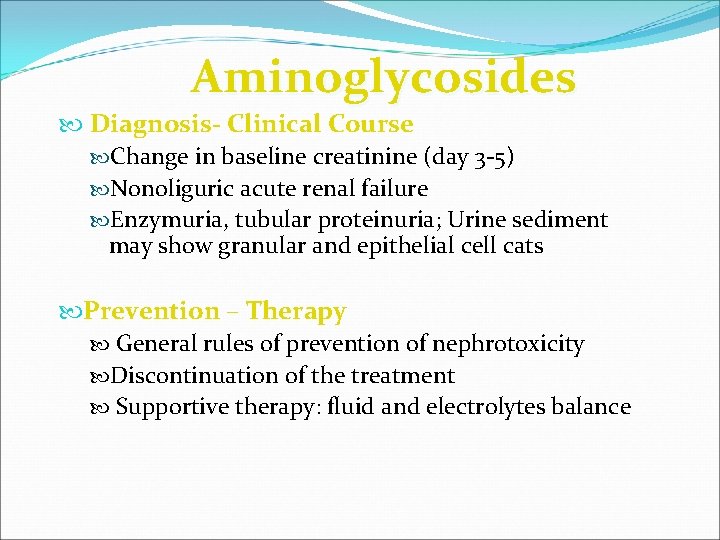
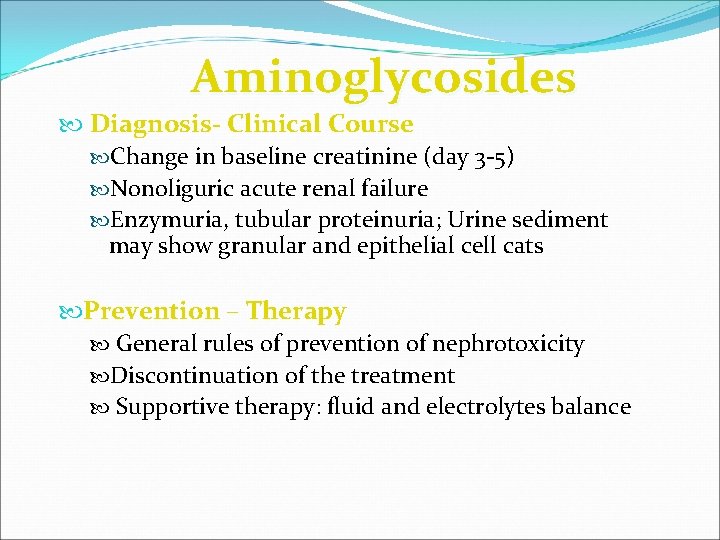
Aminoglycosides Diagnosis- Clinical Course Change in baseline creatinine (day 3 -5) Nonoliguric acute renal failure Enzymuria, tubular proteinuria; Urine sediment may show granular and epithelial cell cats Prevention – Therapy General rules of prevention of nephrotoxicity Discontinuation of the treatment Supportive therapy: fluid and electrolytes balance
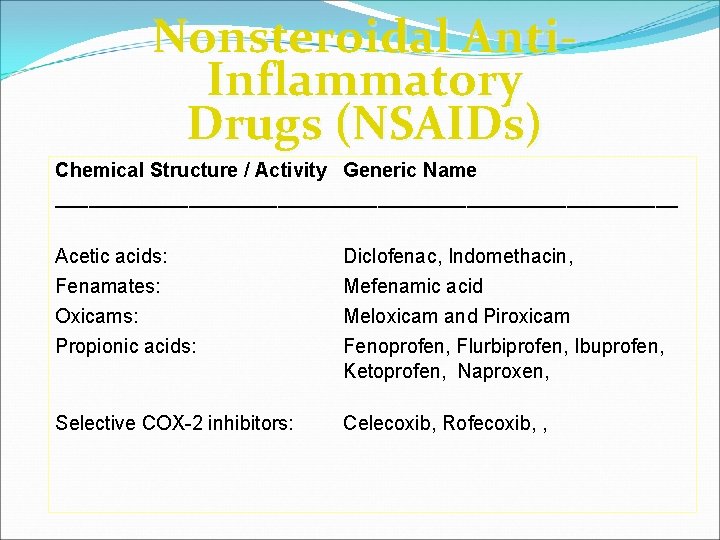
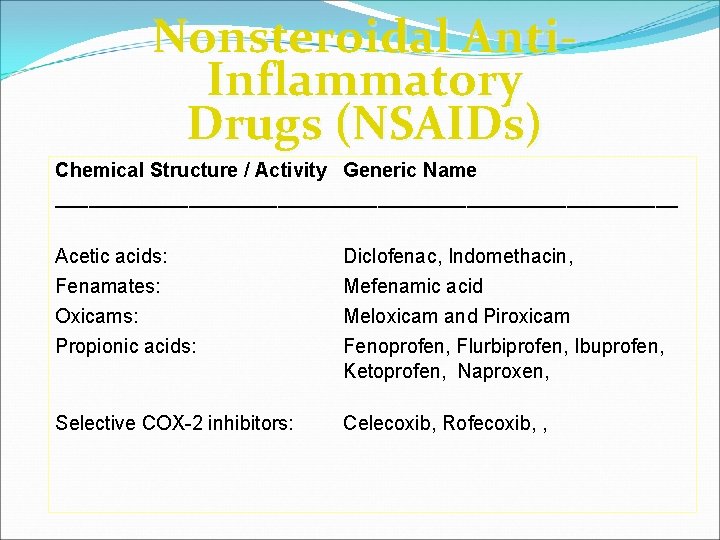
Nonsteroidal Anti. Inflammatory Drugs (NSAIDs) Chemical Structure / Activity Generic Name ____________________________ Acetic acids: Fenamates: Oxicams: Propionic acids: Diclofenac, Indomethacin, Mefenamic acid Meloxicam and Piroxicam Fenoprofen, Flurbiprofen, Ibuprofen, Ketoprofen, Naproxen, Selective COX-2 inhibitors: Celecoxib, Rofecoxib, ,
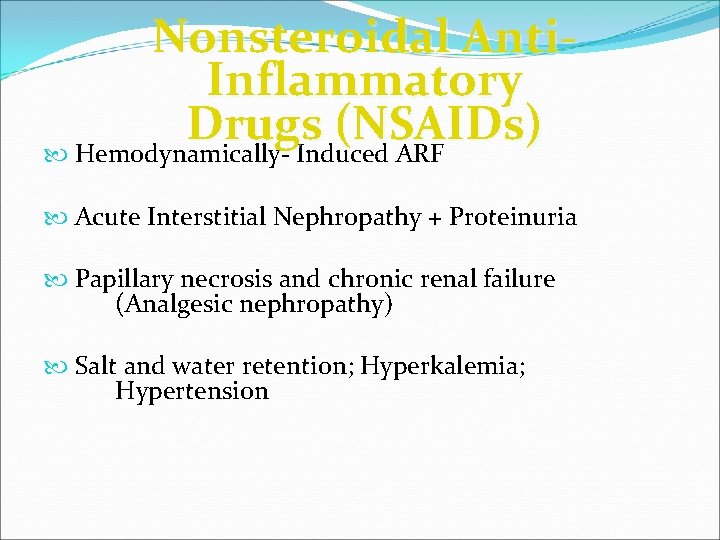
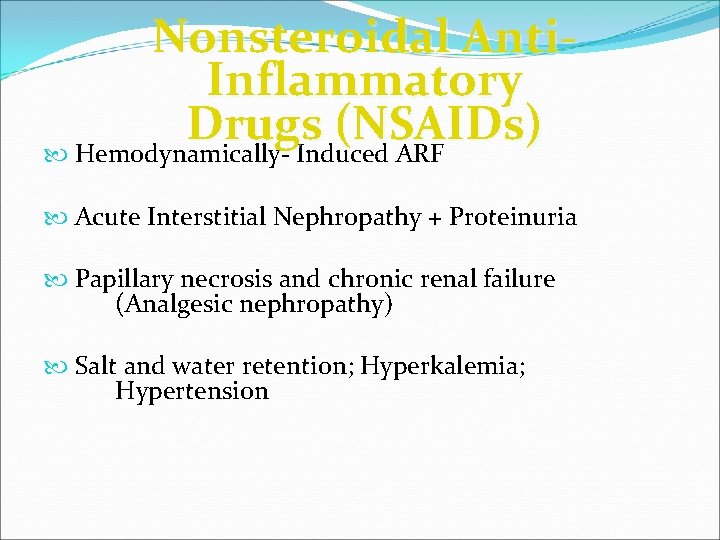
Nonsteroidal Anti. Inflammatory Drugs (NSAIDs) Hemodynamically- Induced ARF Acute Interstitial Nephropathy + Proteinuria Papillary necrosis and chronic renal failure (Analgesic nephropathy) Salt and water retention; Hyperkalemia; Hypertension
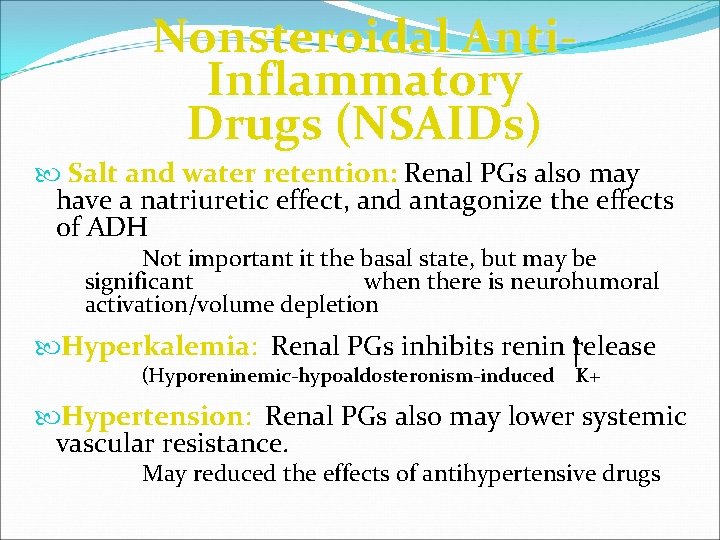
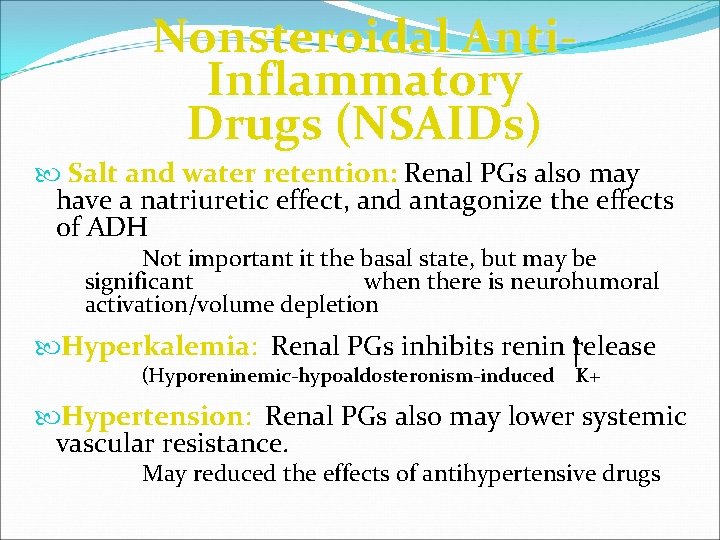
Nonsteroidal Anti. Inflammatory Drugs (NSAIDs) Salt and water retention: Renal PGs also may have a natriuretic effect, and antagonize the effects of ADH Not important it the basal state, but may be significant when there is neurohumoral activation/volume depletion Hyperkalemia: Renal PGs inhibits renin release (Hyporeninemic-hypoaldosteronism-induced K+ Hypertension: Renal PGs also may lower systemic vascular resistance. May reduced the effects of antihypertensive drugs
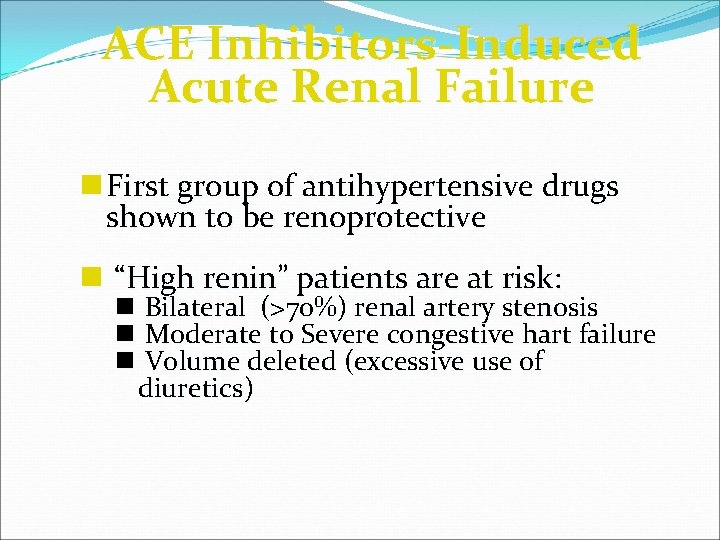
ACE Inhibitors-Induced Acute Renal Failure n First group of antihypertensive drugs shown to be renoprotective n “High renin” patients are at risk: n Bilateral (>70%) renal artery stenosis n Moderate to Severe congestive hart failure n Volume deleted (excessive use of diuretics)
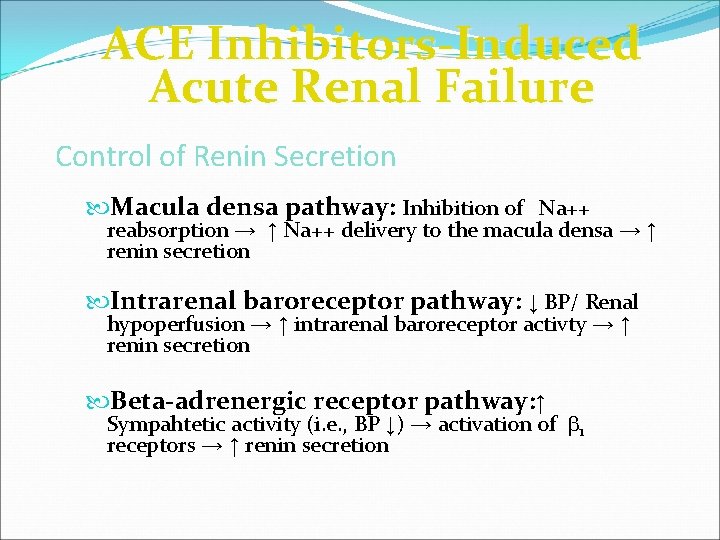
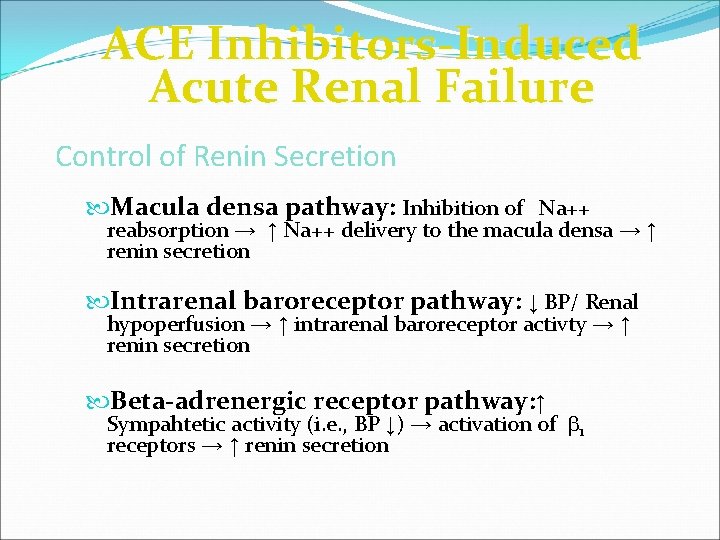
ACE Inhibitors-Induced Acute Renal Failure Control of Renin Secretion Macula densa pathway: Inhibition of Na++ reabsorption → ↑ Na++ delivery to the macula densa → ↑ renin secretion Intrarenal baroreceptor pathway: ↓ BP/ Renal hypoperfusion → ↑ intrarenal baroreceptor activty → ↑ renin secretion Beta-adrenergic receptor pathway: ↑ Sympahtetic activity (i. e. , BP ↓) → activation of b 1 receptors → ↑ renin secretion
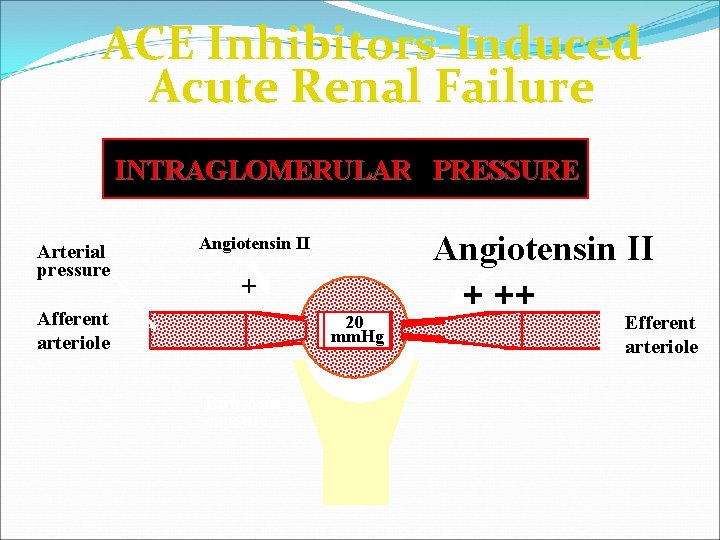
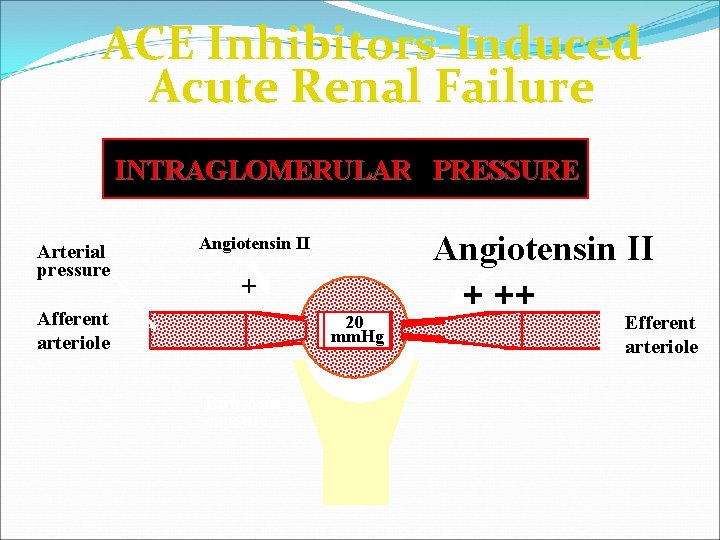
ACE Inhibitors-Induced Acute Renal Failure INTRAGLOMERULAR PRESSURE Arterial pressure Angiotensin II + + Afferent arteriole 20 mm. Hg Bowman’s capsule Angiotensin II + ++ Efferent arteriole
Amphothericin B n Used for the treatment of often life-threatening fungal infections. n Tubular injury and renal vasoconstriction proposed to have an important role in pathogenesis n Drop in GFR mediated at least in part via TGF mechanisms n Volume expansion (salt loading) may reduces drop in GFR but not tubular toxicity n Usually reversible with discontinuation of therapy n The new liposomal (phospholipid vesicles) preparations seem to be less toxic
 Lecturer's name
Lecturer's name Res extra commercium
Res extra commercium Diagnostico etiologico
Diagnostico etiologico Example of ion dipole
Example of ion dipole Pozorovací arch žáka
Pozorovací arch žáka Distinguish between renal corpuscle and renal tubule
Distinguish between renal corpuscle and renal tubule Drug induced thrombocytopenia
Drug induced thrombocytopenia Drug induced parkinson
Drug induced parkinson Drug induced sle
Drug induced sle Methods of adulteration of crude drugs
Methods of adulteration of crude drugs Jeannie watkins
Jeannie watkins Lecturer in charge
Lecturer in charge Designation lecturer
Designation lecturer Lecturer in charge
Lecturer in charge Pearson lecturer resources
Pearson lecturer resources Spe distinguished lecturer
Spe distinguished lecturer Cfa lecturer handbook
Cfa lecturer handbook Designation of lecturer
Designation of lecturer 140000/120
140000/120 Afternoon teacher
Afternoon teacher Lecturer asad ali
Lecturer asad ali Guest lecturer in geography
Guest lecturer in geography Lector vs lecturer
Lector vs lecturer Photography lecturer
Photography lecturer Lecturer name
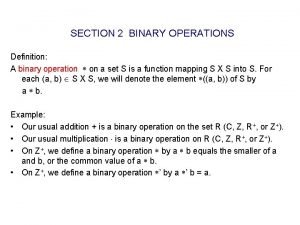
Lecturer name Example of binary operation
Example of binary operation Self siphonage
Self siphonage Vertical
Vertical Hyperlink-induced topic search
Hyperlink-induced topic search Induced strategic behavior
Induced strategic behavior Lymphoma alcohol
Lymphoma alcohol