DRAFT MID CHESHIRE HOSPITALS NHS FT Review of

- Slides: 55
DRAFT MID CHESHIRE HOSPITALS NHS FT Review of the Trust’s clinical IT strategy and roadmap February 2016 CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 1
DRAFT Executive summary 1/3 The Trust’s 2012 -2017 IM&T strategy has been partially delivered, but there remains a significant amount to be done with respect to clinical IT in a context in which the strategic drivers have changed A review of MCHFT clinical IT conducted in late 2015 has identified that the Trust’s IM&T delivery had not been able to deliver the ambition set out in the 2012 – 2017 IM&T Strategy. Progress has been made in a number of areas. For example, there is good capability around day to day service delivery and infrastructure, and there are encouraging signs of clinical engagement. Moreover there has been good progress made in delivering the infrastructure components of the 2012 strategy. However, progress on new clinical applications, and in particular on the development of an electronic patient record (EPR) has stalled due to a combination of: limited capacity and capability to manage transformational clinical IT change; a demanding work programme focused on existing major in-hospital clinical applications, and; funding constraints. The priorities for the Trust’s clinical IT are clear, but there are significant practical constraints on making progress MCHFT IT sits in an environment that features a number of drivers, and constraints, but also some opportunities that will shape the strategy. Not least, the Trust has a clear business direction that places an emphasis on IT. There also a number of implications of the health economies in which the Trust sits that are factors in deciding the clinical IT strategy from 2016 onwards. Quality and safety of care, fit with the Trust’s strategic direction, and collaboration across the health economies to which MCHFT sits are the top priorities which clinical IT needs to support. At the same time, available funding, clinical and non-clinical capacity, moving the culture from one based on paper to one that is digital, and getting the supply chain to perform in line with this strategy are the major challenges. Priority clinical requirements are largely based around a single view of the patient, not just within the Trust but also across primary care, and other secondary care providers such as UHNM. There also some significant requirements for information that enables the Trust to demonstrate and improve performance both in terms of the quality of care it provides, and in financial terms. Any technology solutions also need to align with a set of clear design principles with the Trust looking for solutions that are proven and product based rather than developed locally and hard to maintain, and a focus on clinical IT that maximises the effectiveness and efficiency of the Trust. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 2
DRAFT Executive summary 2/3 This strategy recommends that the Trust focuses its efforts on three major technologies that are built progressively consistent with funding and capacity constraints Building on the progress the Trust has made on core infrastructure, clinical IT solutions that meet the priorities and requirements of the senior team can be constructed from a set of major building blocks which are: Ø Foundation technologies such as networks, servers and other communications technologies that provide the means of getting information from a to b. Ø Enabling technologies that manage the data associated with core hospital assets (staff, beds, theatres etc. ). Ø Exploiting technologies – the main focus for this strategy, namely: o An Electronic Document Management System (or Service) (EDMS) to digitise paper records. o A Clinical Portal to meet the majority of the immediate requirements for access to patient information both inside and outside the Trust. o A core integrated Electronic Patient Record System with integrated PAS and management functionality plus modules for Orders and results, A&E and progressively other modules including Electronic Prescribing and Medicines Administration functionality. In addition the Trust should consider lower cost standalone technologies for a number of specific needs that fit into the overall architecture framework that can add benefit with respect to the Trust's declared priorities without compromising the longer term direction of travel. The approach suggested builds digital functionality progressively in time (and in terms of cost and value), and recognises the Trust’s position today in terms of priorities, funding and capacity, and wider regional context. The roadmap for clinical IT at MCHFT is constructed to enable the strategy to be delivered over a 3 year timeframe with the aim of reaping significant benefits for patients and efficiencies in operations from modernised platforms by 2017/18. It recognises the Trust’s starting position and balances that with the risks of further delay to the Trust’s strategy, dependence on an ageing PAS, and the lead times. A benefits led approach that balances these factors is recommended and would require an injection of revenue funding in 2016/17. It is constructed to enable the strategy to be delivered over a 3 year timeframe with benefits accruing form year 1. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 3
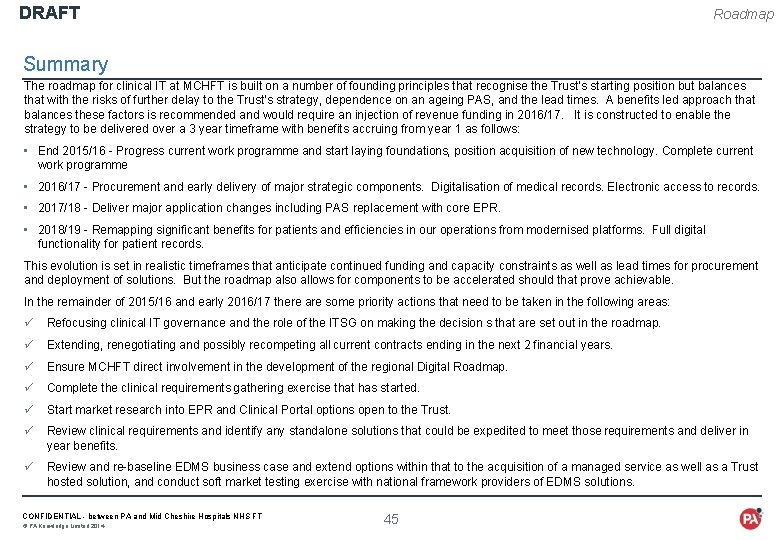
DRAFT Executive summary 3/3 In the remainder of 2015/16 and early 2016/17 there are some priority actions that need to be taken in the following areas: ü Refocusing clinical IT governance and the role of the ITSG on making the decisions that are set out in the roadmap. ü Extending, renegotiating and possibly recompeting all current contracts ending in the next 2 financial years. ü Ensure MCHFT direct involvement in the development of the regional Digital Roadmap. ü Complete the clinical requirements gathering exercise for Clinical IT that has started. ü Start market research into EPR and Clinical Portal options open to the Trust. ü Review clinical requirements and identify any standalone solutions that could be expedited to meet those requirements and deliver in year benefits. ü Review and re-baseline EDMS business case and extend options within that to the acquisition of a managed service as well as a Trust hosted solution, and conduct soft market testing exercise with national framework providers of EDMS solutions. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 4
DRAFT Contents Background - Where is the Trust on its clinical IT journey? • Progress made against the 2012 – 2017 IM&T Strategy • Core strengths of the Trust’s approach to clinical IT and delivery to date • Constraints that limit the clinical IT ambition • Wider health economy implications Requirements - What does the Trust need clinical IT to do for it looking forward? • Strategic priorities, drivers and constraints when making decisions on clinical IT • Requirements gathered for clinical IT • Implications of the Trust’s strategic objectives and national and regional pressures • Key design principles to enable the right clinical IT to be selected Strategy - What are the major IT platforms that could support the Trust’s strategic direction? • Typical “building blocks” for clinical IT in a Foundation Trust • The building blocks that are already in place at MCHFT • Options for the new clinical IT building blocks that need to be put in place • Recommended approach for clinical IT Roadmap - How could those clinical IT platforms be delivered over the next 3 years? • Principles underlying the recommended Roadmap • 3 year Roadmap for delivering the strategy • 12 month action plan including changes to existing projects • 3 month view of next steps CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 5
DRAFT BACKGROUND WHERE IS THE TRUST ON ITS IT JOURNEY? • Progress made against the 2012 – 2017 IM&T Strategy • Core strengths of the Trust’s approach to clinical IT and delivery to date • Constraints that limit the clinical IT ambition • Wider health economy implications CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 6
DRAFT Background Summary PA’s review of MCHFT clinical IT conducted in late 2015 concluded that the Trust’s IM&T delivery had not been able to deliver the ambition set out in the 2012 – 2017 IM&T Strategy. Progress has been made in a number of areas. For example, there is good capability around day to day service delivery and infrastructure, and there are encouraging signs of clinical engagement. Moreover, there has been good progress made in delivering the infrastructure components of the 2012 strategy. However, progress on new clinical applications, and in particular on the development of an electronic patient record (EPR) has stalled. There a number of reasons for this: • MCHFT IM&T has the core capabilities to manage the day to day, but limited capacity and capability to manage transformational clinical IT change; • the current change work programme is also demanding given the available capacity, and is focused on existing major in-hospital clinical applications, and; • funding available for transformation of clinical IT at MCHFT is limited. Looking forwards, MCHFT IT sits in an environment that features a number of drivers, and constraints, but also some opportunities that will shape the strategy. Not least, the Trust has a clear business direction that places an emphasis on IT. There also a number of implications of the health economies in which the Trust sits that are factors in deciding the clinical IT strategy from 2016 onwards. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 7
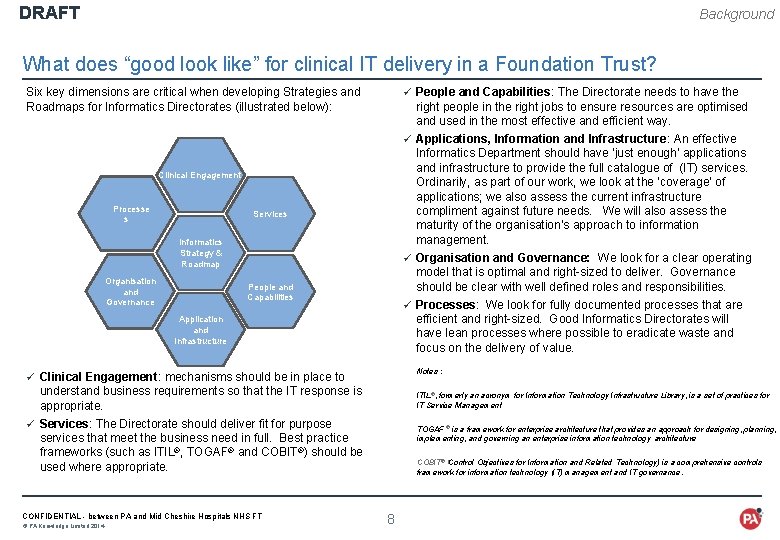
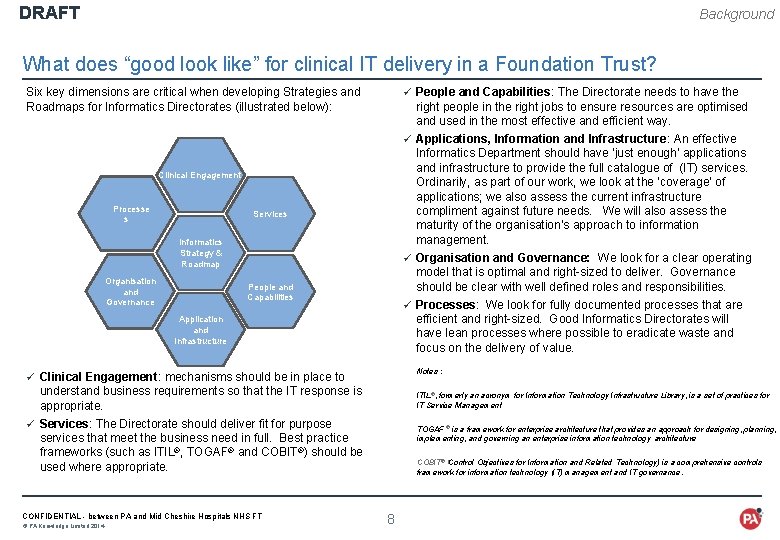
DRAFT Background What does “good look like” for clinical IT delivery in a Foundation Trust? ü People and Capabilities: The Directorate needs to have the Six key dimensions are critical when developing Strategies and Roadmaps for Informatics Directorates (illustrated below): right people in the right jobs to ensure resources are optimised and used in the most effective and efficient way. ü Applications, Information and Infrastructure: An effective Informatics Department should have ‘just enough’ applications and infrastructure to provide the full catalogue of (IT) services. Ordinarily, as part of our work, we look at the ‘coverage’ of applications; we also assess the current infrastructure compliment against future needs. We will also assess the maturity of the organisation’s approach to information management. Clinical Engagement Processe s Services Informatics Strategy & Roadmap Organisation and Governance ü Organisation and Governance: We look for a clear operating model that is optimal and right-sized to deliver. Governance should be clear with well defined roles and responsibilities. People and Capabilities ü Processes: We look for fully documented processes that are efficient and right-sized. Good Informatics Directorates will have lean processes where possible to eradicate waste and focus on the delivery of value. Application and Infrastructure Notes : ü Clinical Engagement: mechanisms should be in place to understand business requirements so that the IT response is appropriate. ü Services: The Directorate should deliver fit for purpose services that meet the business need in full. Best practice frameworks (such as ITIL®, TOGAF® and COBIT®) should be used where appropriate. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 ITIL®, formerly an acronym for Information Technology Infrastructure Library, is a set of practices for IT Service Management TOGAF ® is a framework for enterprise architecture that provides an approach for designing, planning, implementing, and governing an enterprise information technology architecture COBIT® (Control Objectives for Information and Related Technology) is a comprehensive controls framework for information technology (IT) management and IT governance. 8
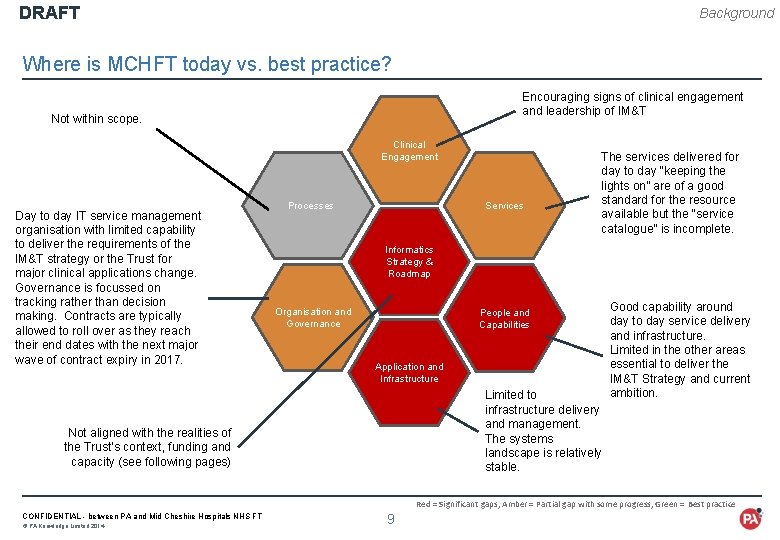
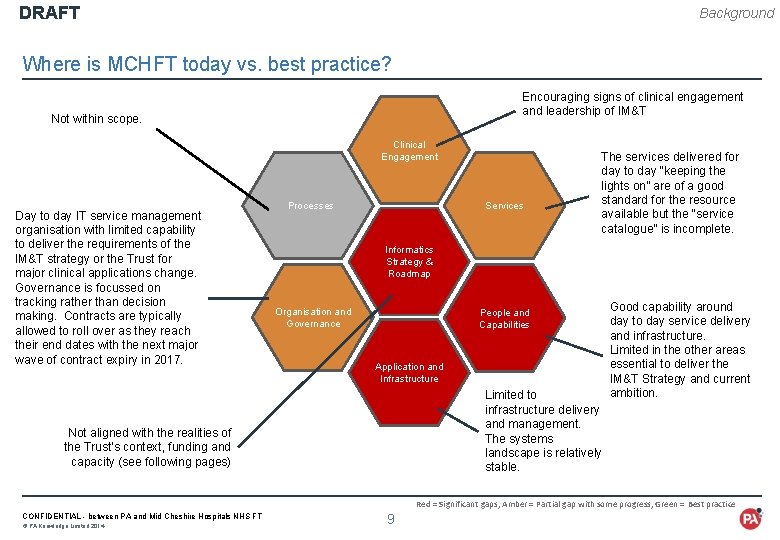
DRAFT Background Where is MCHFT today vs. best practice? Encouraging signs of clinical engagement and leadership of IM&T Not within scope. Clinical Engagement Day to day IT service management organisation with limited capability to deliver the requirements of the IM&T strategy or the Trust for major clinical applications change. Governance is focussed on tracking rather than decision making. Contracts are typically allowed to roll over as they reach their end dates with the next major wave of contract expiry in 2017. Services Processes The services delivered for day to day “keeping the lights on” are of a good standard for the resource available but the “service catalogue” is incomplete. Informatics Strategy & Roadmap Organisation and Governance People and Capabilities Application and Infrastructure Limited to infrastructure delivery and management. The systems landscape is relatively stable. Not aligned with the realities of the Trust’s context, funding and capacity (see following pages) Good capability around day to day service delivery and infrastructure. Limited in the other areas essential to deliver the IM&T Strategy and current ambition. Red = Significant gaps, Amber = Partial gap with some progress, Green = Best practice CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 9
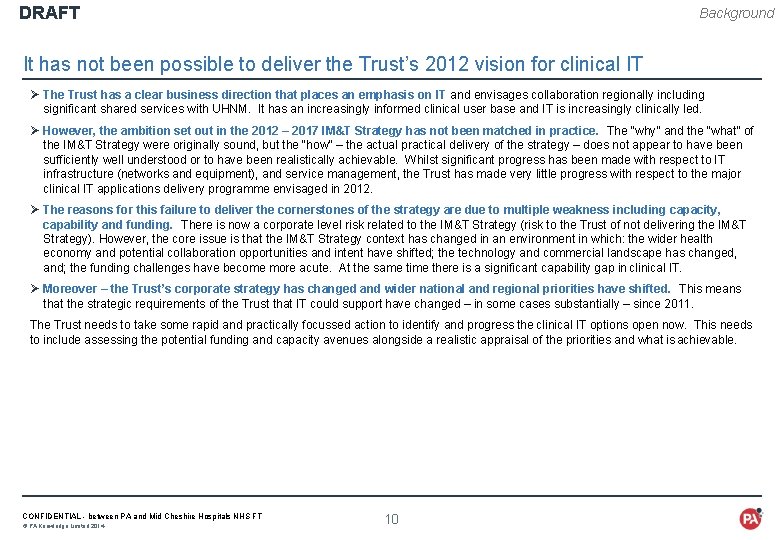
DRAFT Background It has not been possible to deliver the Trust’s 2012 vision for clinical IT Ø The Trust has a clear business direction that places an emphasis on IT and envisages collaboration regionally including significant shared services with UHNM. It has an increasingly informed clinical user base and IT is increasingly clinically led. Ø However, the ambition set out in the 2012 – 2017 IM&T Strategy has not been matched in practice. The “why” and the “what” of the IM&T Strategy were originally sound, but the “how” – the actual practical delivery of the strategy – does not appear to have been sufficiently well understood or to have been realistically achievable. Whilst significant progress has been made with respect to IT infrastructure (networks and equipment), and service management, the Trust has made very little progress with respect to the major clinical IT applications delivery programme envisaged in 2012. Ø The reasons for this failure to deliver the cornerstones of the strategy are due to multiple weakness including capacity, capability and funding. There is now a corporate level risk related to the IM&T Strategy (risk to the Trust of not delivering the IM&T Strategy). However, the core issue is that the IM&T Strategy context has changed in an environment in which: the wider health economy and potential collaboration opportunities and intent have shifted; the technology and commercial landscape has changed, and; the funding challenges have become more acute. At the same time there is a significant capability gap in clinical IT. Ø Moreover – the Trust’s corporate strategy has changed and wider national and regional priorities have shifted. This means that the strategic requirements of the Trust that IT could support have changed – in some cases substantially – since 2011. The Trust needs to take some rapid and practically focussed action to identify and progress the clinical IT options open now. This needs to include assessing the potential funding and capacity avenues alongside a realistic appraisal of the priorities and what is achievable. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 10
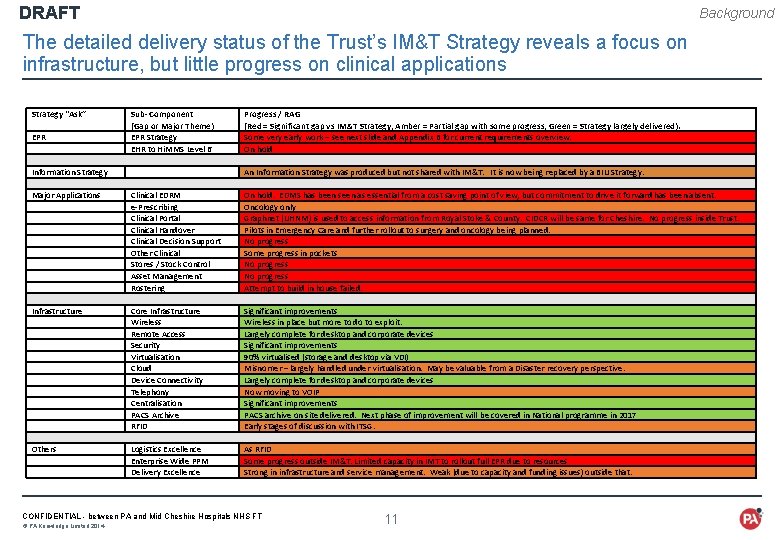
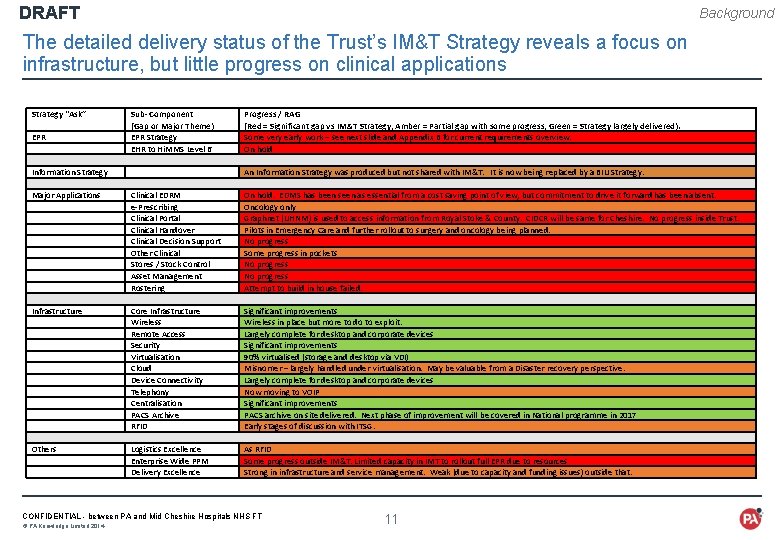
DRAFT Background The detailed delivery status of the Trust’s IM&T Strategy reveals a focus on infrastructure, but little progress on clinical applications Strategy “Ask” EPR Information Strategy Major Applications Infrastructure Others Sub- Component (Gap or Major Theme) EPR Strategy EHR to Hi. MMS Level 6 Progress / RAG (Red = Significant gap vs IM&T Strategy, Amber = Partial gap with some progress, Green = Strategy largely delivered). Some very early work – see next slide and Appendix B for current requirements overview. On hold An Information Strategy was produced but not shared with IM&T. It is now being replaced by a BIU Strategy. Clinical EDRM e-Prescribing Clinical Portal Clinical Handover Clinical Decision Support Other Clinical Stores / Stock Control Asset Management Rostering On hold. EDMS has been seen as essential from a cost saving point of view, but commitment to drive it forward has been absent. Oncology only Graphnet (UHNM) is used to access information from Royal Stoke & County. CIDCR will be same for Cheshire. No progress inside Trust. Pilots in Emergency Care and further rollout to surgery and oncology being planned. No progress Some progress in pockets No progress Attempt to build in house failed. Core Infrastructure Wireless Remote Access Security Virtualisation Cloud Device Connectivity Telephony Centralisation PACS Archive RFID Significant improvements Wireless in place but more to do to exploit. Largely complete for desktop and corporate devices Significant improvements 90% virtualised (storage and desktop via VDI) Misnomer – largely handled under virtualisation. May be valuable from a Disaster recovery perspective. Largely complete for desktop and corporate devices Now moving to VOIP Significant improvements PACS archive on site delivered. Next phase of improvement will be covered in National programme in 2017 Early stages of discussion with ITSG. Logistics Excellence Enterprise Wide PPM Delivery Excellence As RFID Some progress outside IM&T. Limited capacity in IMT to rollout full EPR due to resources Strong in infrastructure and service management. Weak (due to capacity and funding issues) outside that. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 11

DRAFT Background To effectively deliver a clinical IT strategy, an informatics function needs to have a number of core capabilities Strategy & Planning · Gathering requirements · Identifying potential solutions · Assessing ability to deliver Strategy & Planning Solutions Delivery · Technical delivery services · Non-technical delivery services Delivery Support · Customer Services and Solutions · Communications & Telephony · Maintenance Support CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 12 IM&T Support Services Solutions · Assessment against architectural principles · New innovations · R&D and Collaborations
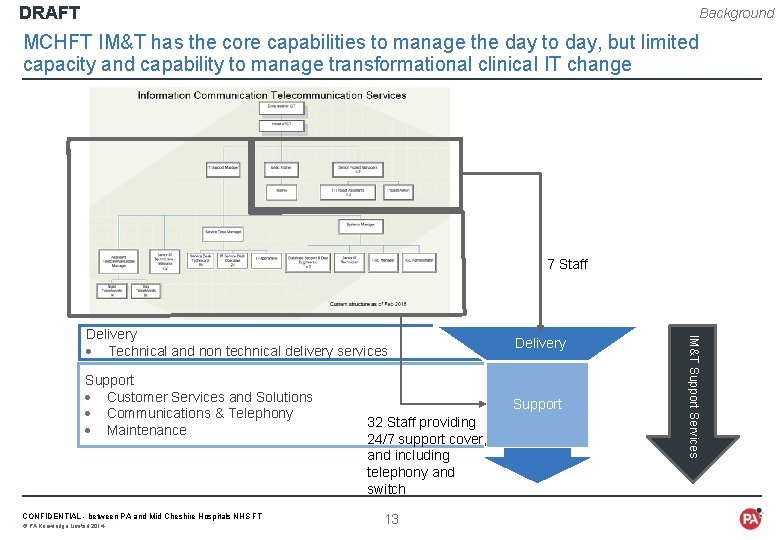
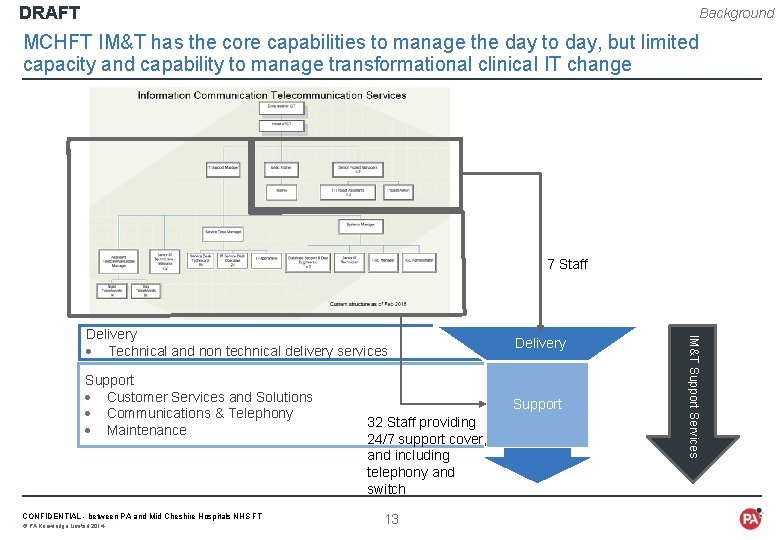
DRAFT Background MCHFT IM&T has the core capabilities to manage the day to day, but limited capacity and capability to manage transformational clinical IT change Strategy & Planning Solutions 7 Staff Delivery Support · Customer Services and Solutions · Communications & Telephony · Maintenance Support CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 32 Staff providing 24/7 support cover, and including telephony and switch 13 IM&T Support Services Delivery · Technical and non technical delivery services
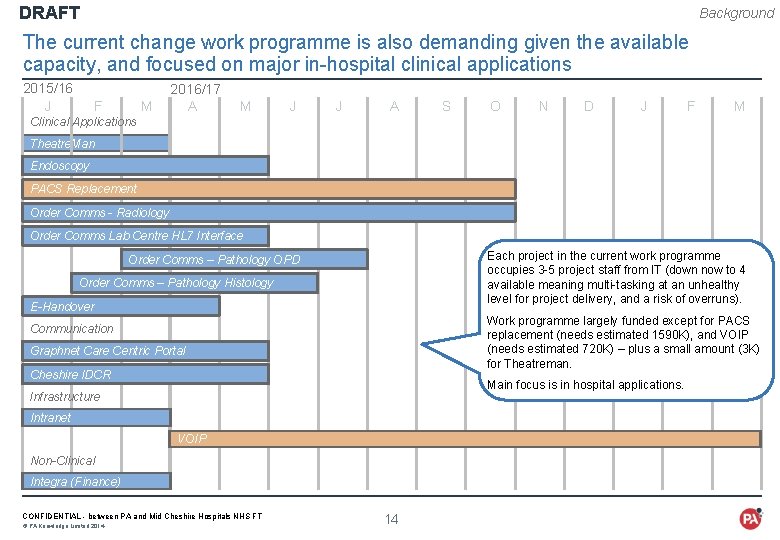
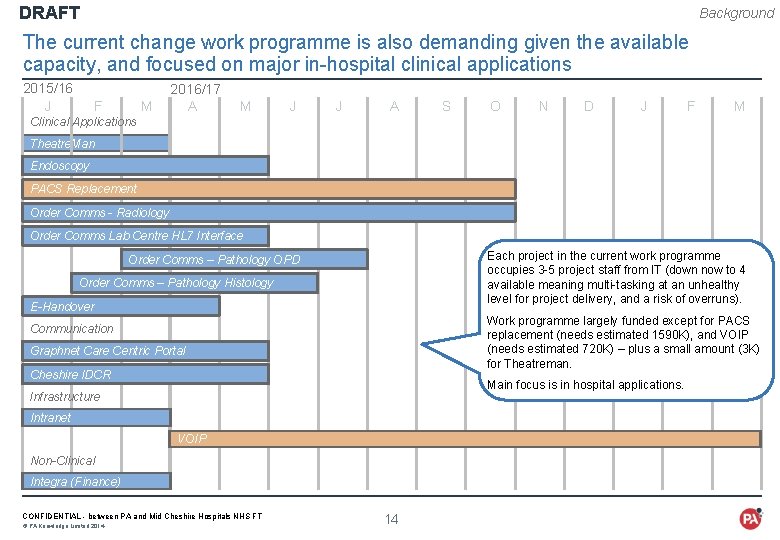
DRAFT Background The current change work programme is also demanding given the available capacity, and focused on major in-hospital clinical applications 2015/16 J 2016/17 F M A M J A S O N D J F M Clinical Applications Theatre. Man Endoscopy PACS Replacement Order Comms - Radiology Order Comms Lab Centre HL 7 Interface Each project in the current work programme occupies 3 -5 project staff from IT (down now to 4 available meaning multi-tasking at an unhealthy level for project delivery, and a risk of overruns). Order Comms – Pathology OPD Order Comms – Pathology Histology E-Handover Work programme largely funded except for PACS replacement (needs estimated 1590 K), and VOIP (needs estimated 720 K) – plus a small amount (3 K) for Theatreman. Communication Graphnet Care Centric Portal Cheshire IDCR Main focus is in hospital applications. Infrastructure Intranet VOIP Non-Clinical Integra (Finance) CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 14
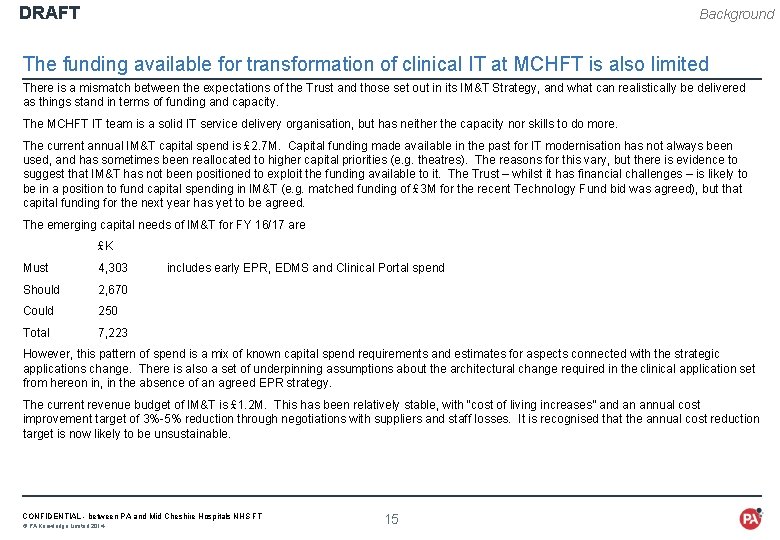
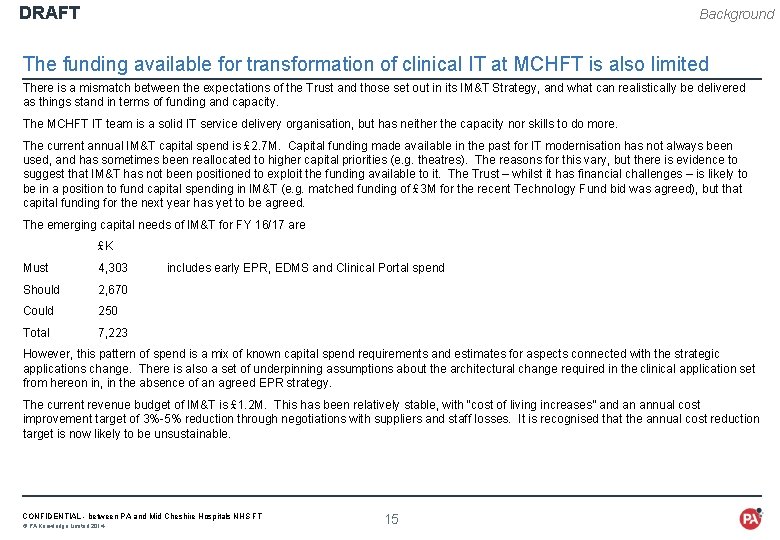
DRAFT Background The funding available for transformation of clinical IT at MCHFT is also limited There is a mismatch between the expectations of the Trust and those set out in its IM&T Strategy, and what can realistically be delivered as things stand in terms of funding and capacity. The MCHFT IT team is a solid IT service delivery organisation, but has neither the capacity nor skills to do more. The current annual IM&T capital spend is £ 2. 7 M. Capital funding made available in the past for IT modernisation has not always been used, and has sometimes been reallocated to higher capital priorities (e. g. theatres). The reasons for this vary, but there is evidence to suggest that IM&T has not been positioned to exploit the funding available to it. The Trust – whilst it has financial challenges – is likely to be in a position to fund capital spending in IM&T (e. g. matched funding of £ 3 M for the recent Technology Fund bid was agreed), but that capital funding for the next year has yet to be agreed. The emerging capital needs of IM&T for FY 16/17 are £K Must 4, 303 Should 2, 670 Could 250 Total 7, 223 includes early EPR, EDMS and Clinical Portal spend However, this pattern of spend is a mix of known capital spend requirements and estimates for aspects connected with the strategic applications change. There is also a set of underpinning assumptions about the architectural change required in the clinical application set from hereon in, in the absence of an agreed EPR strategy. The current revenue budget of IM&T is £ 1. 2 M. This has been relatively stable, with “cost of living increases” and an annual cost improvement target of 3%-5% reduction through negotiations with suppliers and staff losses. It is recognised that the annual cost reduction target is now likely to be unsustainable. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 15
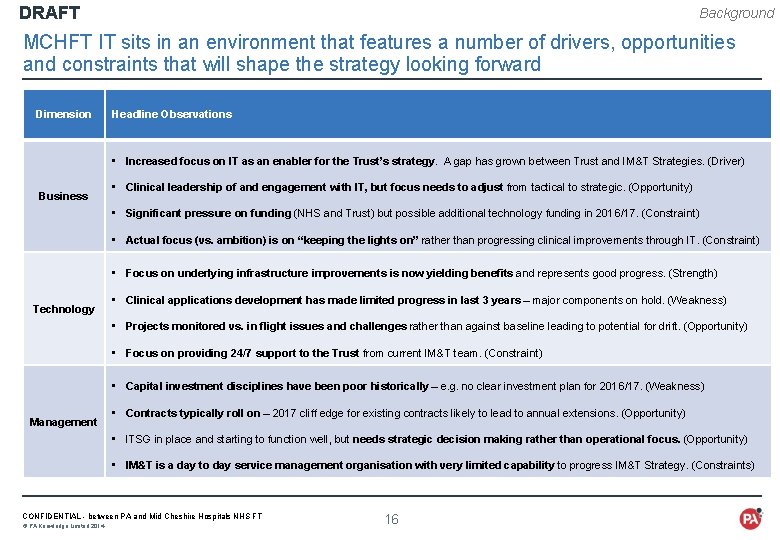
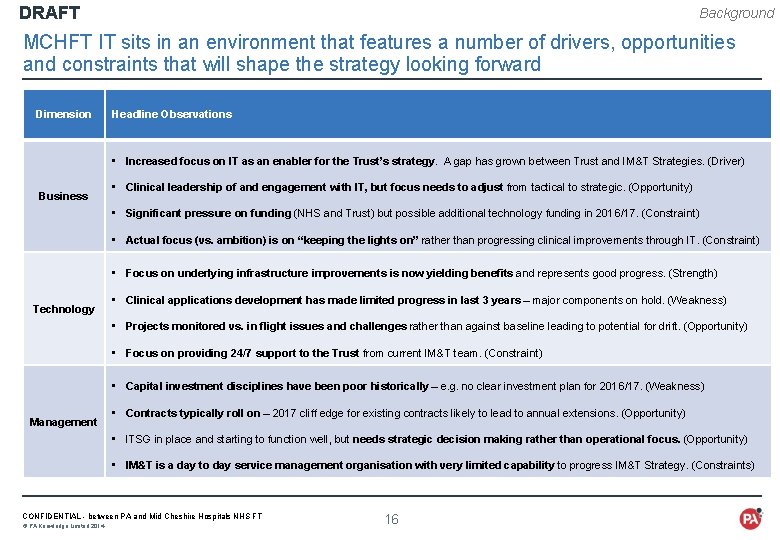
DRAFT Background MCHFT IT sits in an environment that features a number of drivers, opportunities and constraints that will shape the strategy looking forward Dimension Headline Observations • Increased focus on IT as an enabler for the Trust’s strategy. A gap has grown between Trust and IM&T Strategies. (Driver) Business • Clinical leadership of and engagement with IT, but focus needs to adjust from tactical to strategic. (Opportunity) • Significant pressure on funding (NHS and Trust) but possible additional technology funding in 2016/17. (Constraint) • Actual focus (vs. ambition) is on “keeping the lights on” rather than progressing clinical improvements through IT. (Constraint) • Focus on underlying infrastructure improvements is now yielding benefits and represents good progress. (Strength) Technology • Clinical applications development has made limited progress in last 3 years – major components on hold. (Weakness) • Projects monitored vs. in flight issues and challenges rather than against baseline leading to potential for drift. (Opportunity) • Focus on providing 24/7 support to the Trust from current IM&T team. (Constraint) • Capital investment disciplines have been poor historically – e. g. no clear investment plan for 2016/17. (Weakness) Management • Contracts typically roll on – 2017 cliff edge for existing contracts likely to lead to annual extensions. (Opportunity) • ITSG in place and starting to function well, but needs strategic decision making rather than operational focus. (Opportunity) • IM&T is a day to day service management organisation with very limited capability to progress IM&T Strategy. (Constraints) CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 16
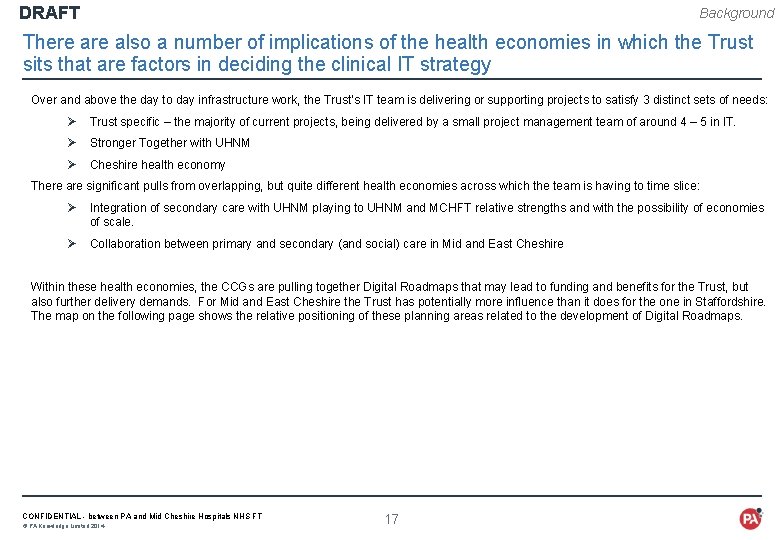
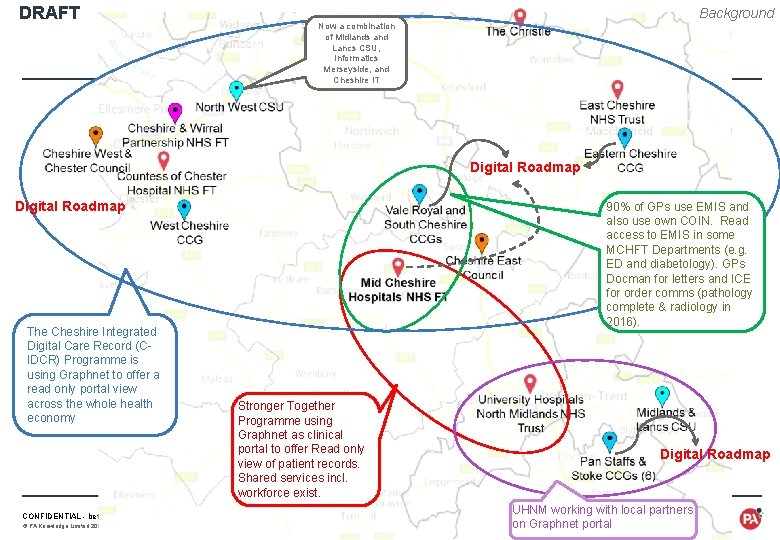
DRAFT Background There also a number of implications of the health economies in which the Trust sits that are factors in deciding the clinical IT strategy Over and above the day to day infrastructure work, the Trust’s IT team is delivering or supporting projects to satisfy 3 distinct sets of needs: Ø Trust specific – the majority of current projects, being delivered by a small project management team of around 4 – 5 in IT. Ø Stronger Together with UHNM Ø Cheshire health economy There are significant pulls from overlapping, but quite different health economies across which the team is having to time slice: Ø Integration of secondary care with UHNM playing to UHNM and MCHFT relative strengths and with the possibility of economies of scale. Ø Collaboration between primary and secondary (and social) care in Mid and East Cheshire Within these health economies, the CCGs are pulling together Digital Roadmaps that may lead to funding and benefits for the Trust, but also further delivery demands. For Mid and East Cheshire the Trust has potentially more influence than it does for the one in Staffordshire. The map on the following page shows the relative positioning of these planning areas related to the development of Digital Roadmaps. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 17
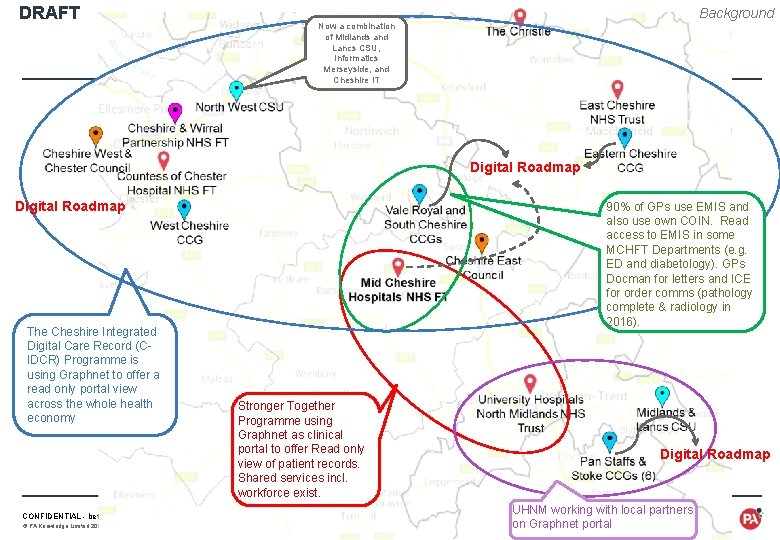
DRAFT Background Now a combination of Midlands and Lancs CSU, Informatics Merseyside, and Cheshire IT Digital Roadmap The Cheshire Integrated Digital Care Record (CIDCR) Programme is using Graphnet to offer a read only portal view across the whole health economy 90% of GPs use EMIS and also use own COIN. Read access to EMIS in some MCHFT Departments (e. g. ED and diabetology). GPs Docman for letters and ICE for order comms (pathology complete & radiology in 2016). Stronger Together Programme using Graphnet as clinical portal to offer Read only view of patient records. Shared services incl. workforce exist. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 Digital Roadmap 18 UHNM working with local partners on Graphnet portal
DRAFT REQUIREMENTS WHAT DOES THE TRUST NEED INFORMATION TECHNOLOGY TO DO FOR IT LOOKING FORWARD? CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 · Strategic priorities, drivers and constraints when making decisions on clinical IT · Requirements gathered for clinical IT · Implications of the Trust’s strategic objectives and national and regional pressures · Key design principles to enable the right clinical IT to be selected 19
DRAFT Requirements Summary The priorities for the Trust’s clinical IT are clear, but there are significant practical constraints on making progress. Quality and safety of care, fit with the Trust’s strategic direction, and collaboration across the health economies to which MCHFT sits are the top priorities which clinical IT needs to support. At the same time, available funding, clinical and non-clinical capacity, moving the culture from one based on paper to one that is digital, and getting the supply chain to perform in line with this strategy are the major challenges. Priority clinical requirements are largely based around a single view of the patient, not just within the Trust but also across primary care, and other secondary care providers such as UHNM. There also some significant requirements for information that enables the Trust to demonstrate and improve performance both in terms of the quality of care it provides, and in financial terms. Any technology solutions also need to align with a set of clear design principles with the Trust looking for solutions that are proven and product based rather than developed locally and hard to maintain, and a focus on clinical IT that maximises the effectiveness and efficiency of the Trust. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 20
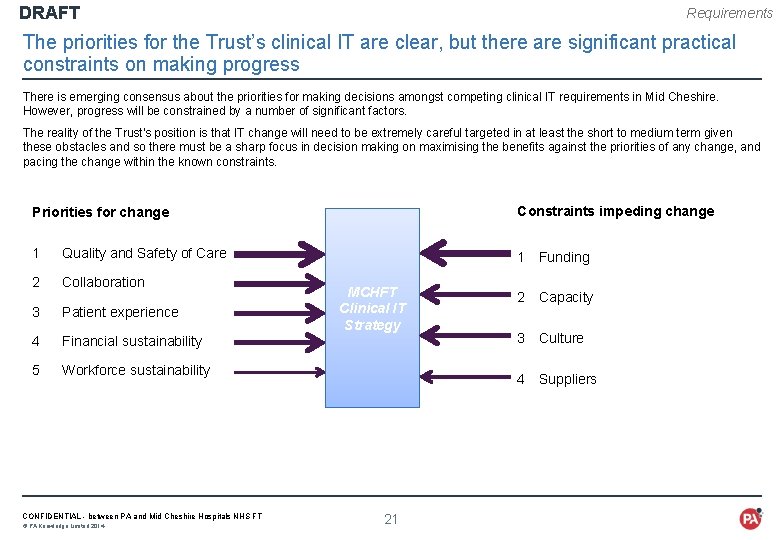
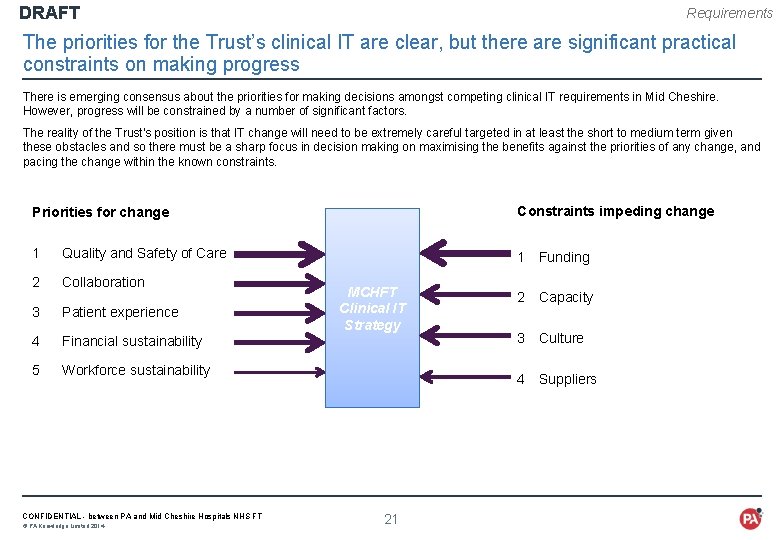
DRAFT Requirements The priorities for the Trust’s clinical IT are clear, but there are significant practical constraints on making progress There is emerging consensus about the priorities for making decisions amongst competing clinical IT requirements in Mid Cheshire. However, progress will be constrained by a number of significant factors. The reality of the Trust's position is that IT change will need to be extremely careful targeted in at least the short to medium term given these obstacles and so there must be a sharp focus in decision making on maximising the benefits against the priorities of any change, and pacing the change within the known constraints. Priorities for change Constraints impeding change 1 Quality and Safety of Care 1 Funding 2 Collaboration 3 Patient experience 4 Financial sustainability 5 Workforce sustainability CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 MCHFT Clinical IT Strategy 2 Capacity 3 Culture 4 Suppliers 21
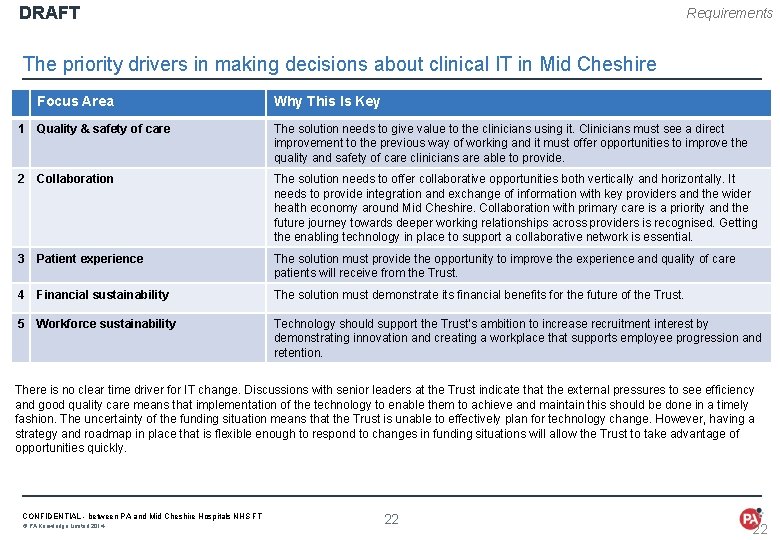
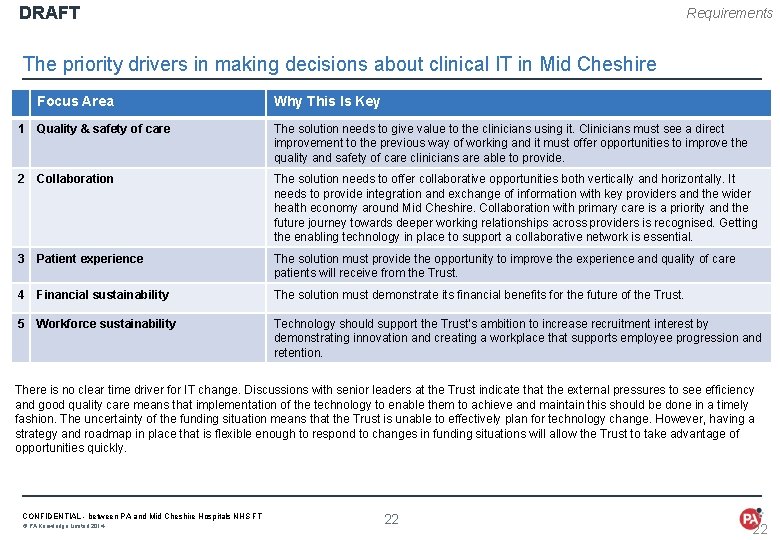
DRAFT Requirements The priority drivers in making decisions about clinical IT in Mid Cheshire Focus Area Why This Is Key 1 Quality & safety of care The solution needs to give value to the clinicians using it. Clinicians must see a direct improvement to the previous way of working and it must offer opportunities to improve the quality and safety of care clinicians are able to provide. 2 Collaboration The solution needs to offer collaborative opportunities both vertically and horizontally. It needs to provide integration and exchange of information with key providers and the wider health economy around Mid Cheshire. Collaboration with primary care is a priority and the future journey towards deeper working relationships across providers is recognised. Getting the enabling technology in place to support a collaborative network is essential. 3 Patient experience The solution must provide the opportunity to improve the experience and quality of care patients will receive from the Trust. 4 Financial sustainability The solution must demonstrate its financial benefits for the future of the Trust. 5 Workforce sustainability Technology should support the Trust’s ambition to increase recruitment interest by demonstrating innovation and creating a workplace that supports employee progression and retention. There is no clear time driver for IT change. Discussions with senior leaders at the Trust indicate that the external pressures to see efficiency and good quality care means that implementation of the technology to enable them to achieve and maintain this should be done in a timely fashion. The uncertainty of the funding situation means that the Trust is unable to effectively plan for technology change. However, having a strategy and roadmap in place that is flexible enough to respond to changes in funding situations will allow the Trust to take advantage of opportunities quickly. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 22 22
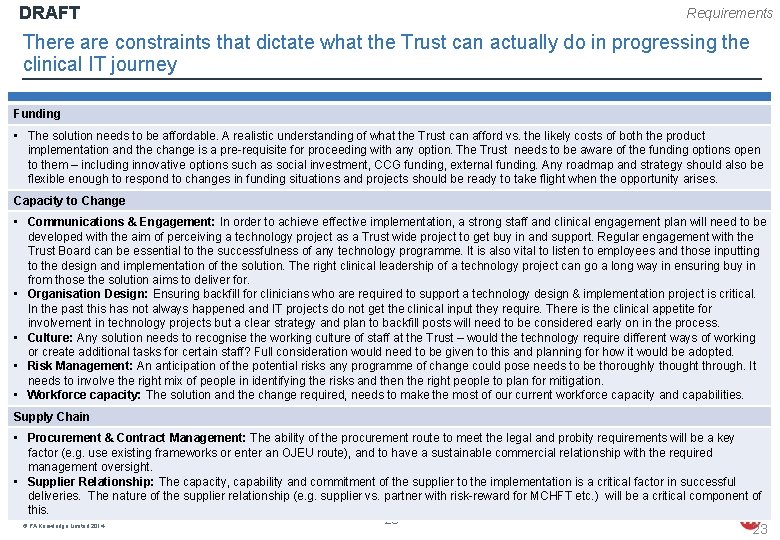
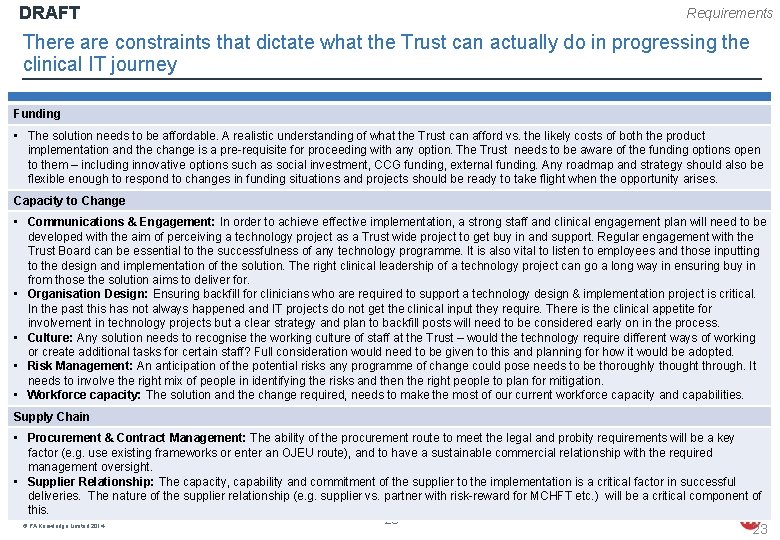
DRAFT Requirements There are constraints that dictate what the Trust can actually do in progressing the clinical IT journey Funding • The solution needs to be affordable. A realistic understanding of what the Trust can afford vs. the likely costs of both the product implementation and the change is a pre-requisite for proceeding with any option. The Trust needs to be aware of the funding options open to them – including innovative options such as social investment, CCG funding, external funding. Any roadmap and strategy should also be flexible enough to respond to changes in funding situations and projects should be ready to take flight when the opportunity arises. Capacity to Change • Communications & Engagement: In order to achieve effective implementation, a strong staff and clinical engagement plan will need to be developed with the aim of perceiving a technology project as a Trust wide project to get buy in and support. Regular engagement with the Trust Board can be essential to the successfulness of any technology programme. It is also vital to listen to employees and those inputting to the design and implementation of the solution. The right clinical leadership of a technology project can go a long way in ensuring buy in from those the solution aims to deliver for. • Organisation Design: Ensuring backfill for clinicians who are required to support a technology design & implementation project is critical. In the past this has not always happened and IT projects do not get the clinical input they require. There is the clinical appetite for involvement in technology projects but a clear strategy and plan to backfill posts will need to be considered early on in the process. • Culture: Any solution needs to recognise the working culture of staff at the Trust – would the technology require different ways of working or create additional tasks for certain staff? Full consideration would need to be given to this and planning for how it would be adopted. • Risk Management: An anticipation of the potential risks any programme of change could pose needs to be thoroughly thought through. It needs to involve the right mix of people in identifying the risks and then the right people to plan for mitigation. • Workforce capacity: The solution and the change required, needs to make the most of our current workforce capacity and capabilities. Supply Chain • Procurement & Contract Management: The ability of the procurement route to meet the legal and probity requirements will be a key factor (e. g. use existing frameworks or enter an OJEU route), and to have a sustainable commercial relationship with the required management oversight. • Supplier Relationship: The capacity, capability and commitment of the supplier to the implementation is a critical factor in successful deliveries. The nature of the supplier relationship (e. g. supplier vs. partner with risk-reward for MCHFT etc. ) will be a critical component of this. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 23 23
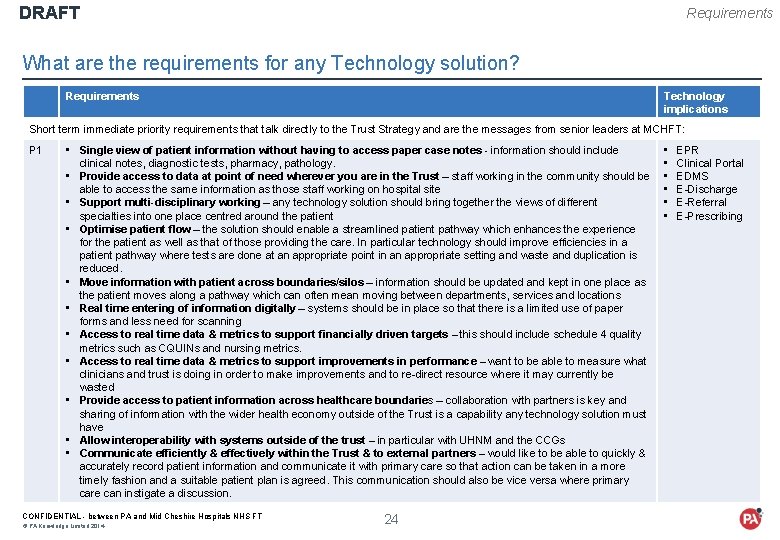
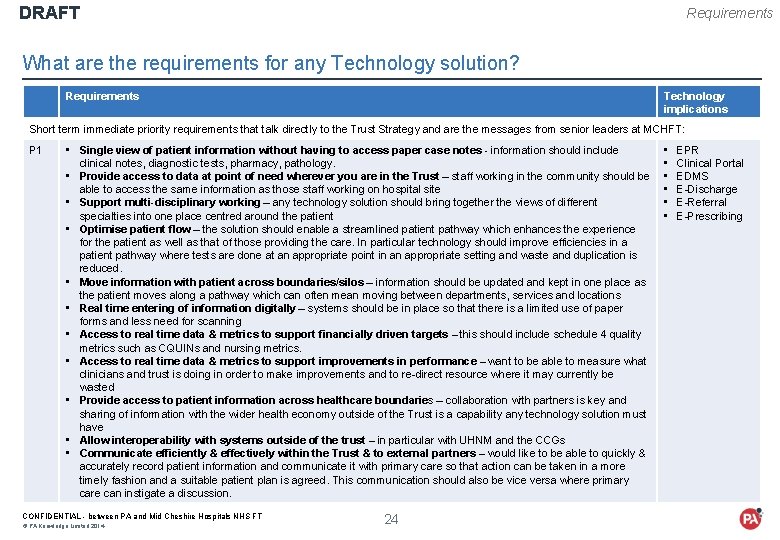
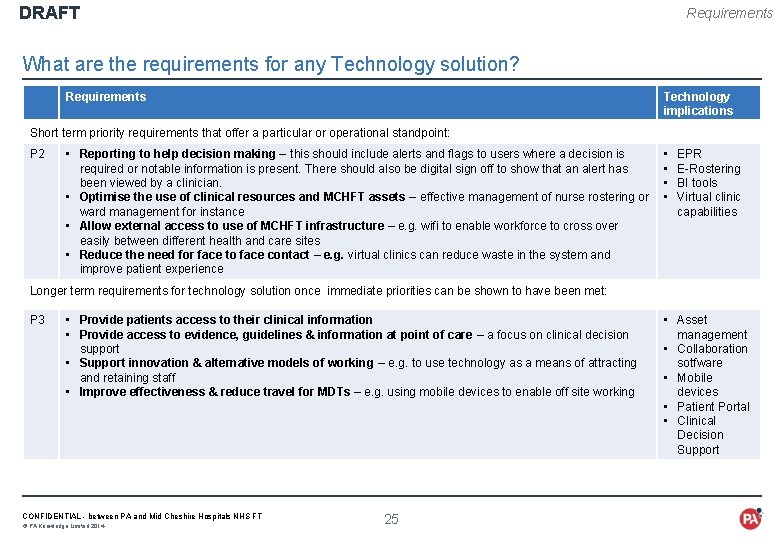
DRAFT Requirements What are the requirements for any Technology solution? Requirements Technology implications Short term immediate priority requirements that talk directly to the Trust Strategy and are the messages from senior leaders at MCHFT: P 1 • Single view of patient information without having to access paper case notes - information should include clinical notes, diagnostic tests, pharmacy, pathology. • Provide access to data at point of need wherever you are in the Trust – staff working in the community should be able to access the same information as those staff working on hospital site • Support multi-disciplinary working – any technology solution should bring together the views of different specialties into one place centred around the patient • Optimise patient flow – the solution should enable a streamlined patient pathway which enhances the experience for the patient as well as that of those providing the care. In particular technology should improve efficiencies in a patient pathway where tests are done at an appropriate point in an appropriate setting and waste and duplication is reduced. • Move information with patient across boundaries/silos – information should be updated and kept in one place as the patient moves along a pathway which can often mean moving between departments, services and locations • Real time entering of information digitally – systems should be in place so that there is a limited use of paper forms and less need for scanning • Access to real time data & metrics to support financially driven targets – this should include schedule 4 quality metrics such as CQUINs and nursing metrics. • Access to real time data & metrics to support improvements in performance – want to be able to measure what clinicians and trust is doing in order to make improvements and to re-direct resource where it may currently be wasted • Provide access to patient information across healthcare boundaries – collaboration with partners is key and sharing of information with the wider health economy outside of the Trust is a capability any technology solution must have • Allow interoperability with systems outside of the trust – in particular with UHNM and the CCGs • Communicate efficiently & effectively within the Trust & to external partners – would like to be able to quickly & accurately record patient information and communicate it with primary care so that action can be taken in a more timely fashion and a suitable patient plan is agreed. This communication should also be vice versa where primary care can instigate a discussion. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 24 • • • EPR Clinical Portal EDMS E-Discharge E-Referral E-Prescribing
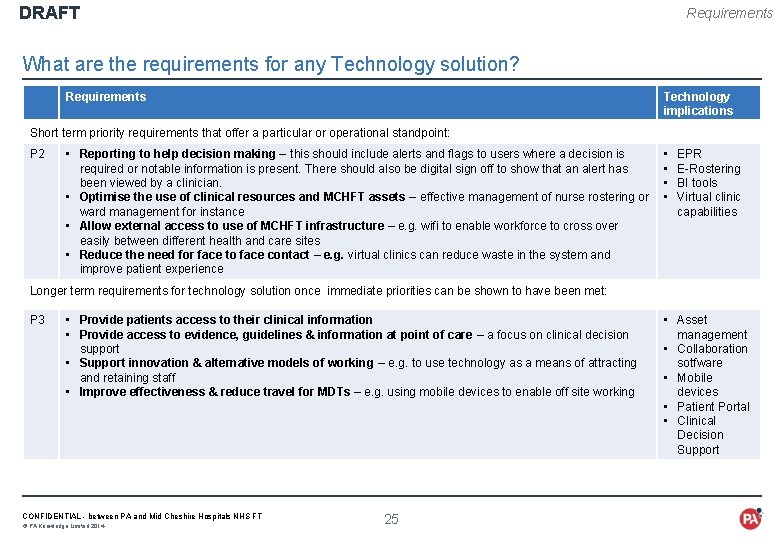
DRAFT Requirements What are the requirements for any Technology solution? Requirements Technology implications Short term priority requirements that offer a particular or operational standpoint: P 2 • Reporting to help decision making – this should include alerts and flags to users where a decision is required or notable information is present. There should also be digital sign off to show that an alert has been viewed by a clinician. • Optimise the use of clinical resources and MCHFT assets – effective management of nurse rostering or ward management for instance • Allow external access to use of MCHFT infrastructure – e. g. wifi to enable workforce to cross over easily between different health and care sites • Reduce the need for face to face contact – e. g. virtual clinics can reduce waste in the system and improve patient experience • • EPR E-Rostering BI tools Virtual clinic capabilities Longer term requirements for technology solution once immediate priorities can be shown to have been met: P 3 • Provide patients access to their clinical information • Provide access to evidence, guidelines & information at point of care – a focus on clinical decision support • Support innovation & alternative models of working – e. g. to use technology as a means of attracting and retaining staff • Improve effectiveness & reduce travel for MDTs – e. g. using mobile devices to enable off site working CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 25 • Asset management • Collaboration sotfware • Mobile devices • Patient Portal • Clinical Decision Support
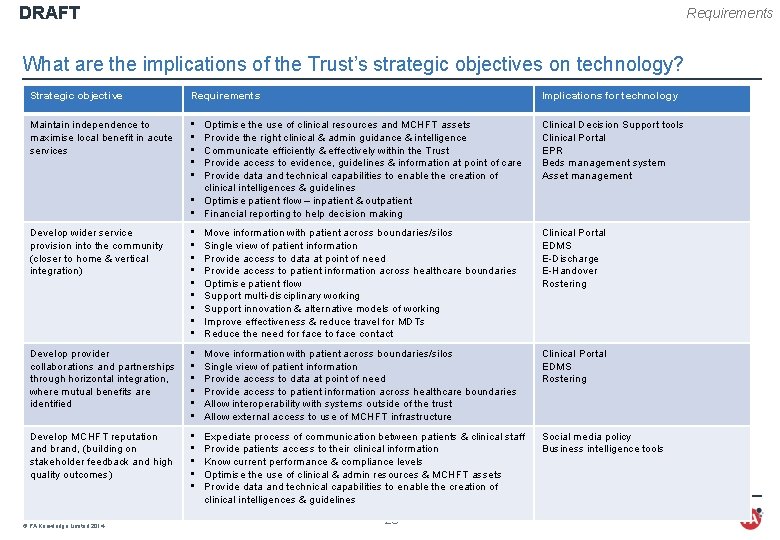
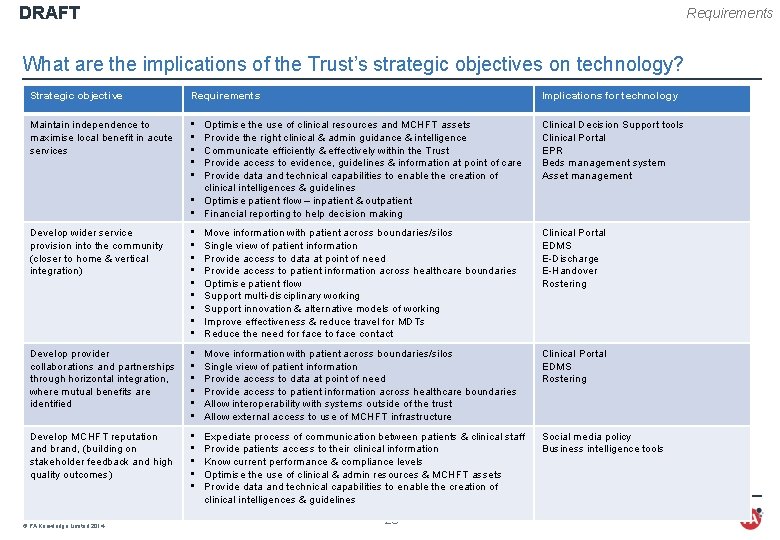
DRAFT Requirements What are the implications of the Trust’s strategic objectives on technology? Strategic objective Requirements Implications for technology Maintain independence to maximise local benefit in acute services • • • Optimise the use of clinical resources and MCHFT assets Provide the right clinical & admin guidance & intelligence Communicate efficiently & effectively within the Trust Provide access to evidence, guidelines & information at point of care Provide data and technical capabilities to enable the creation of clinical intelligences & guidelines • Optimise patient flow – inpatient & outpatient • Financial reporting to help decision making Clinical Decision Support tools Clinical Portal EPR Beds management system Asset management Develop wider service provision into the community (closer to home & vertical integration) • • • Move information with patient across boundaries/silos Single view of patient information Provide access to data at point of need Provide access to patient information across healthcare boundaries Optimise patient flow Support multi-disciplinary working Support innovation & alternative models of working Improve effectiveness & reduce travel for MDTs Reduce the need for face to face contact Clinical Portal EDMS E-Discharge E-Handover Rostering Develop provider collaborations and partnerships through horizontal integration, where mutual benefits are identified • • • Move information with patient across boundaries/silos Single view of patient information Provide access to data at point of need Provide access to patient information across healthcare boundaries Allow interoperability with systems outside of the trust Allow external access to use of MCHFT infrastructure Clinical Portal EDMS Rostering Develop MCHFT reputation and brand, (building on stakeholder feedback and high quality outcomes) • • • Expediate process of communication between patients & clinical staff Provide patients access to their clinical information Know current performance & compliance levels Optimise the use of clinical & admin resources & MCHFT assets Provide data and technical capabilities to enable the creation of clinical intelligences & guidelines Social media policy Business intelligence tools CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 26
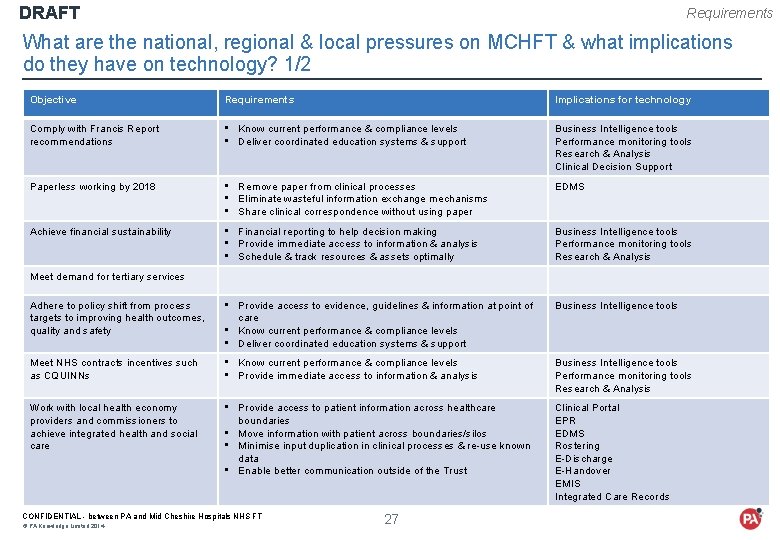
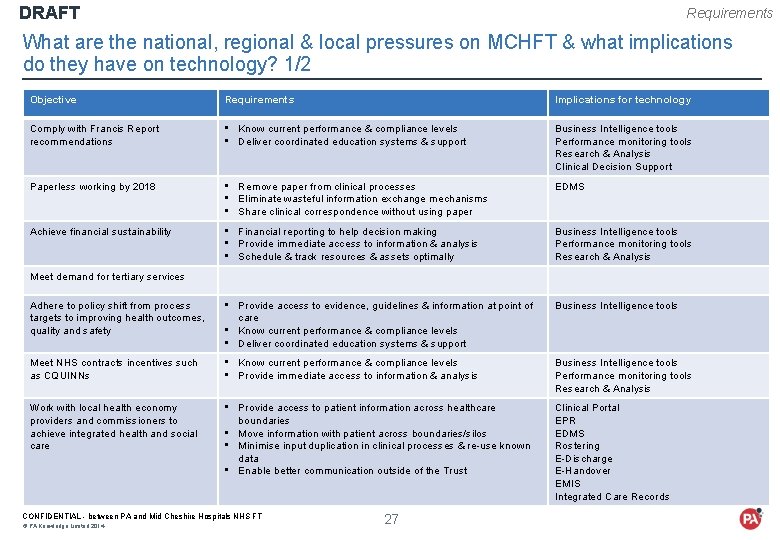
DRAFT Requirements What are the national, regional & local pressures on MCHFT & what implications do they have on technology? 1/2 Objective Requirements Implications for technology Comply with Francis Report recommendations • Know current performance & compliance levels • Deliver coordinated education systems & support Business Intelligence tools Performance monitoring tools Research & Analysis Clinical Decision Support Paperless working by 2018 • Remove paper from clinical processes • Eliminate wasteful information exchange mechanisms • Share clinical correspondence without using paper EDMS Achieve financial sustainability • Financial reporting to help decision making • Provide immediate access to information & analysis • Schedule & track resources & assets optimally Business Intelligence tools Performance monitoring tools Research & Analysis Adhere to policy shift from process targets to improving health outcomes, quality and safety • Provide access to evidence, guidelines & information at point of care • Know current performance & compliance levels • Deliver coordinated education systems & support Business Intelligence tools Meet NHS contracts incentives such as CQUINNs • Know current performance & compliance levels • Provide immediate access to information & analysis Business Intelligence tools Performance monitoring tools Research & Analysis Work with local health economy providers and commissioners to achieve integrated health and social care • Provide access to patient information across healthcare boundaries • Move information with patient across boundaries/silos • Minimise input duplication in clinical processes & re-use known data • Enable better communication outside of the Trust Clinical Portal EPR EDMS Rostering E-Discharge E-Handover EMIS Integrated Care Records Meet demand for tertiary services CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 27
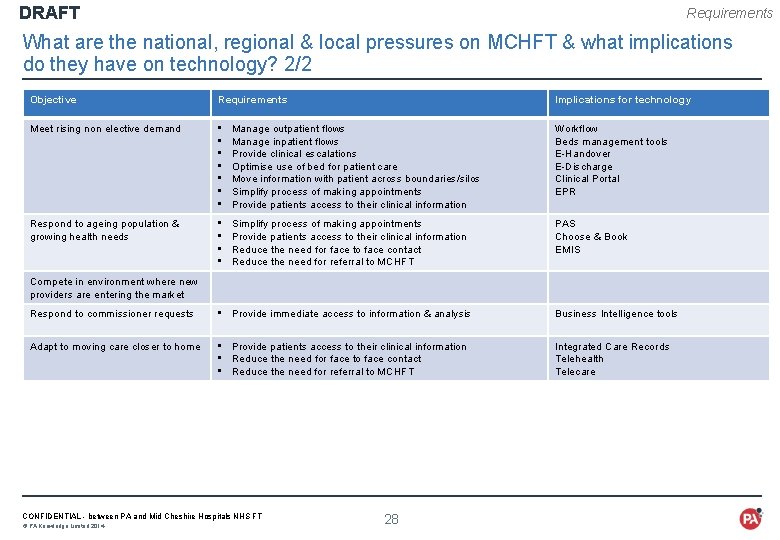
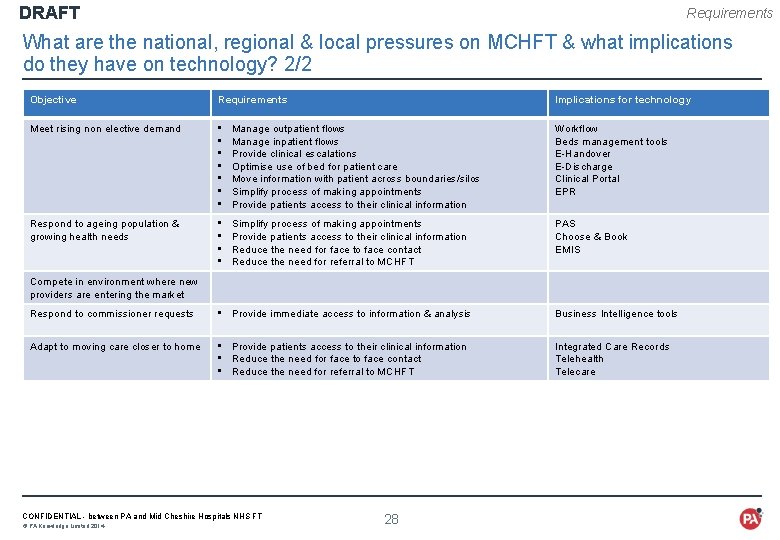
DRAFT Requirements What are the national, regional & local pressures on MCHFT & what implications do they have on technology? 2/2 Objective Requirements Implications for technology Meet rising non elective demand • • Manage outpatient flows Manage inpatient flows Provide clinical escalations Optimise use of bed for patient care Move information with patient across boundaries/silos Simplify process of making appointments Provide patients access to their clinical information Workflow Beds management tools E-Handover E-Discharge Clinical Portal EPR Respond to ageing population & growing health needs • • Simplify process of making appointments Provide patients access to their clinical information Reduce the need for face to face contact Reduce the need for referral to MCHFT PAS Choose & Book EMIS Compete in environment where new providers are entering the market Respond to commissioner requests • Provide immediate access to information & analysis Business Intelligence tools Adapt to moving care closer to home • Provide patients access to their clinical information • Reduce the need for face to face contact • Reduce the need for referral to MCHFT Integrated Care Records Telehealth Telecare CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 28
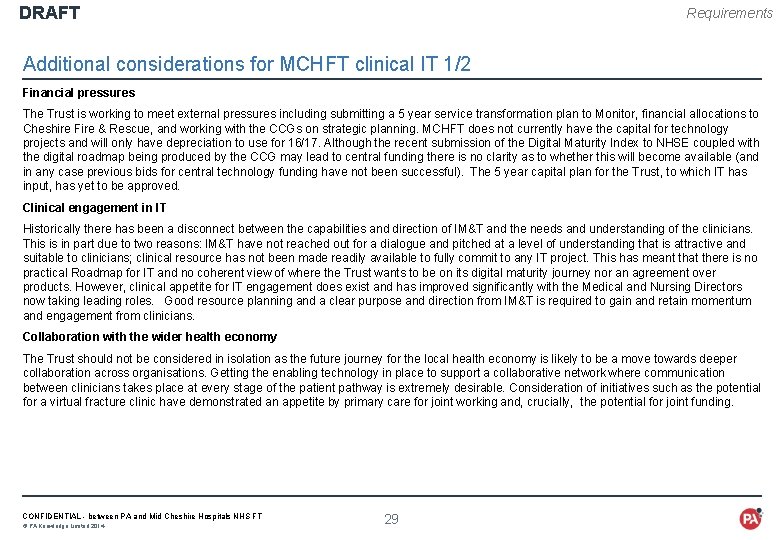
DRAFT Requirements Additional considerations for MCHFT clinical IT 1/2 Financial pressures The Trust is working to meet external pressures including submitting a 5 year service transformation plan to Monitor, financial allocations to Cheshire Fire & Rescue, and working with the CCGs on strategic planning. MCHFT does not currently have the capital for technology projects and will only have depreciation to use for 16/17. Although the recent submission of the Digital Maturity Index to NHSE coupled with the digital roadmap being produced by the CCG may lead to central funding there is no clarity as to whether this will become available (and in any case previous bids for central technology funding have not been successful). The 5 year capital plan for the Trust, to which IT has input, has yet to be approved. Clinical engagement in IT Historically there has been a disconnect between the capabilities and direction of IM&T and the needs and understanding of the clinicians. This is in part due to two reasons: IM&T have not reached out for a dialogue and pitched at a level of understanding that is attractive and suitable to clinicians; clinical resource has not been made readily available to fully commit to any IT project. This has meant that there is no practical Roadmap for IT and no coherent view of where the Trust wants to be on its digital maturity journey nor an agreement over products. However, clinical appetite for IT engagement does exist and has improved significantly with the Medical and Nursing Directors now taking leading roles. Good resource planning and a clear purpose and direction from IM&T is required to gain and retain momentum and engagement from clinicians. Collaboration with the wider health economy The Trust should not be considered in isolation as the future journey for the local health economy is likely to be a move towards deeper collaboration across organisations. Getting the enabling technology in place to support a collaborative network where communication between clinicians takes place at every stage of the patient pathway is extremely desirable. Consideration of initiatives such as the potential for a virtual fracture clinic have demonstrated an appetite by primary care for joint working and, crucially, the potential for joint funding. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 29
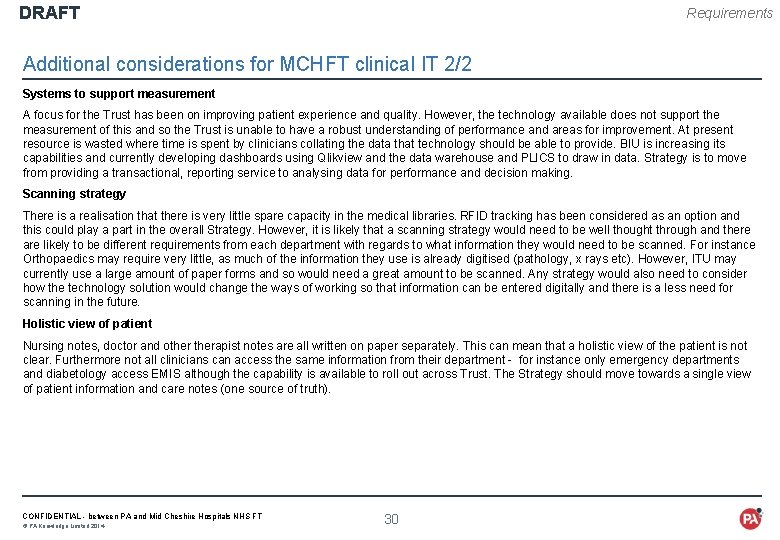
DRAFT Requirements Additional considerations for MCHFT clinical IT 2/2 Systems to support measurement A focus for the Trust has been on improving patient experience and quality. However, the technology available does not support the measurement of this and so the Trust is unable to have a robust understanding of performance and areas for improvement. At present resource is wasted where time is spent by clinicians collating the data that technology should be able to provide. BIU is increasing its capabilities and currently developing dashboards using Qlikview and the data warehouse and PLICS to draw in data. Strategy is to move from providing a transactional, reporting service to analysing data for performance and decision making. Scanning strategy There is a realisation that there is very little spare capacity in the medical libraries. RFID tracking has been considered as an option and this could play a part in the overall Strategy. However, it is likely that a scanning strategy would need to be well thought through and there are likely to be different requirements from each department with regards to what information they would need to be scanned. For instance Orthopaedics may require very little, as much of the information they use is already digitised (pathology, x rays etc). However, ITU may currently use a large amount of paper forms and so would need a great amount to be scanned. Any strategy would also need to consider how the technology solution would change the ways of working so that information can be entered digitally and there is a less need for scanning in the future. Holistic view of patient Nursing notes, doctor and otherapist notes are all written on paper separately. This can mean that a holistic view of the patient is not clear. Furthermore not all clinicians can access the same information from their department - for instance only emergency departments and diabetology access EMIS although the capability is available to roll out across Trust. The Strategy should move towards a single view of patient information and care notes (one source of truth). CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 30
DRAFT Requirements What are the design principles for a Technology solution? 1/2 The design principles set the ground rules for the technology solution. Agreeing the design principles early on in the process will mean that the supplier can provide a solution that meets your expectations. It will also help to guide the testing phase of any technology implementation as there will be a set of rules that the solution will need to meet. The following core design principles have emerged across MCHFT 1. Solution fit • A solution that has been proven elsewhere in the NHS • The solution minimises the need for bespoke or in-house development • Solution must not limit the upgrade path • The solution does not replace ‘like for like’ (the technology changes ways of working) • No big bang approach to implementation 2. Supports efficiency & effectiveness • Accurate and agreed upfront coding • Solution reduces waste in the system e. g. technology should replace unneccesary human work in auditing • Any mobile devices must comply with infection control principles • Does not create the opportunity to take processes off the system • Limits need for scanning and viewing scanned documents • The solution facilitates real time entering of information digitally • Reduces need for printing CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 31
DRAFT Requirements What are the design principles for a Technology solution? 2/2 3. Integration • The solution is interoperable with systems outside of the Trust • Integration with existing systems is possible 4. Access • Ability to be accessed from multiple locations • Ability to be viewed from mobile devices 5. Usability • No more than 1 click to access core patient information • Highest value information set available to all users • User interface is easy and simple • Single sign on CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 32
DRAFT STRATEGY - WHAT ARE THE MAJOR IT PLATFORMS THAT COULD SUPPORT THE TRUST’S STRATEGIC DIRECTION? CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 33 • Typical “building blocks” for clinical IT in a Foundation Trust • The building blocks that are already in place at MCHFT • Options for the new clinical IT building blocks that need to be put in place • Recommended approach for clinical IT
DRAFT Strategy Summary Building on the progress the Trust has made on core infrastructure, clinical IT solutions that meet the priorities and requirements of the senior team can be constructed from a set of major building blocks which are: • Foundation technologies such as networks, servers and other communications technologies that provide the means of getting information from a to b. These have been the focus for IM&T to a large extent over the past five years. • Enabling technologies that manage the data associated with core hospital assets (staff, beds, theatres etc. ). These needs can often be met by standalone solutions. • Exploiting technologies – the main focus for this strategy - including: • Technologies that allow clinical and intelligence information to be shared across and outside the hospital, and enable relevant clinical information from outside to be accessed within the hospital (e. g. clinical portals) • Technologies that deliver direct clinical benefit by managing patient and clinical workflow information at the front line (e. g. EPR). • Technologies that derive additional clinical, operational and management intelligence from other system and present them in ways that facilitate decision making. This strategy recommends that the Trust focuses its efforts on three major technologies that are built progressively consistent with funding and capacity constraints, namely: • An Electronic Document Management System (or Service) (EDMS) to digitise paper records. • A Clinical Portal to meet the majority of the immediate requirements for access to patient information both inside and outside the Trust. • A core integrated Electronic Patient Record System with integrated PAS and management functionality plus modules for Orders and results, A&E and progressively other modules including Electronic Prescribing and Medicines Administration functionality. In addition, the Trust should consider lower cost standalone technologies for a number of specific needs that fit into the overall architecture framework that can add benefit with respect to the Trust's declared priorities without compromising the longer term direction of travel. The approach suggested builds digital functionality progressively in time (and in terms of cost and value), and reognises the Trust’s position today in terms of priorities, funding and capacity, and wider regional context. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 34
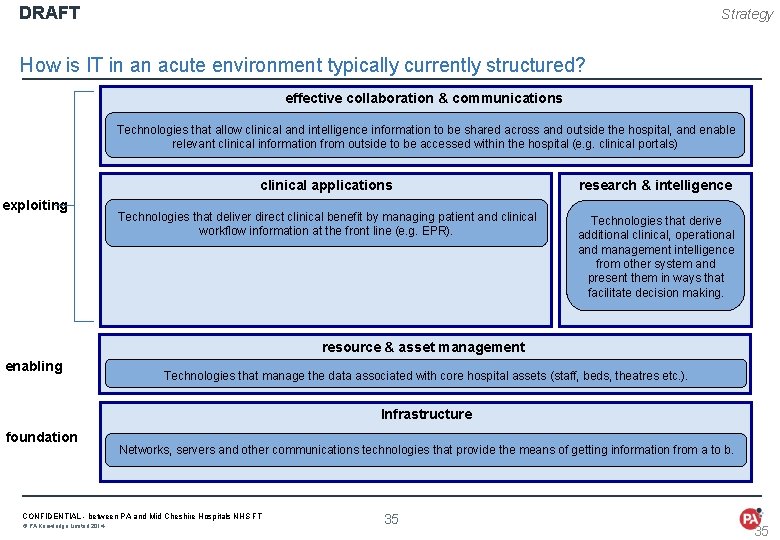
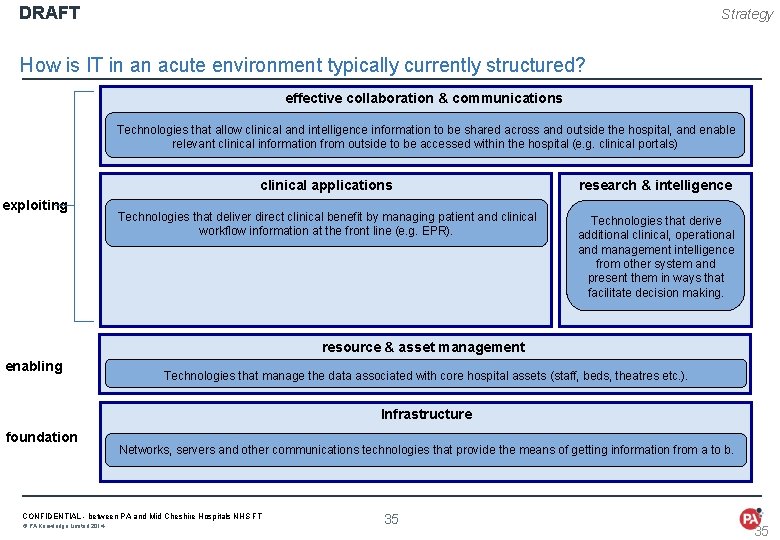
DRAFT Strategy How is IT in an acute environment typically currently structured? effective collaboration & communications Technologies that allow clinical and intelligence information to be shared across and outside the hospital, and enable relevant clinical information from outside to be accessed within the hospital (e. g. clinical portals) exploiting clinical applications research & intelligence Technologies that deliver direct clinical benefit by managing patient and clinical workflow information at the front line (e. g. EPR). Technologies that derive additional clinical, operational and management intelligence from other system and present them in ways that facilitate decision making. resource & asset management enabling Technologies that manage the data associated with core hospital assets (staff, beds, theatres etc. ). Infrastructure foundation Networks, servers and other communications technologies that provide the means of getting information from a to b. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 35 35
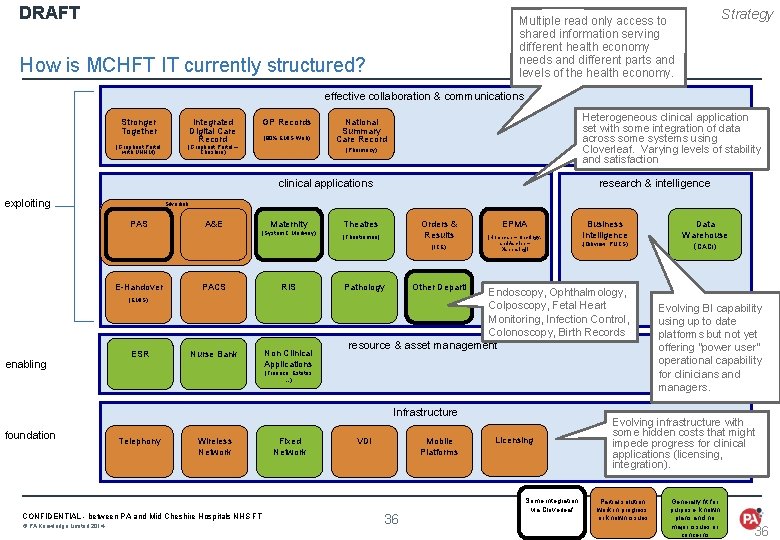
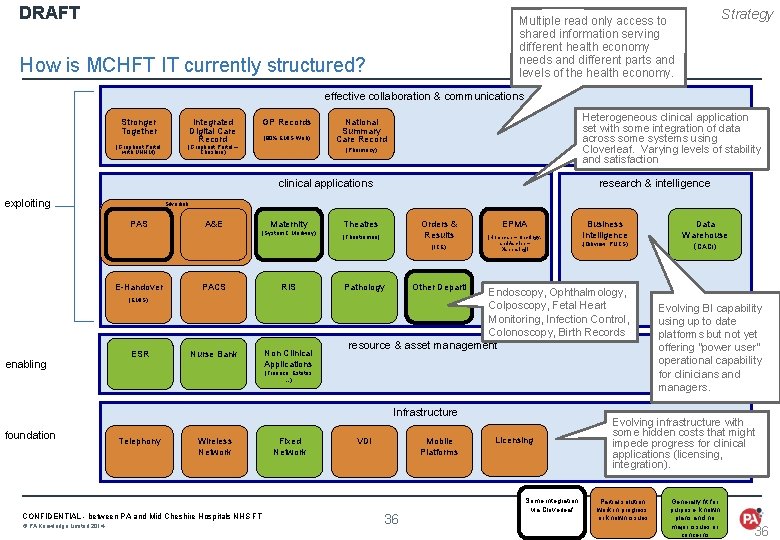
DRAFT Strategy Multiple read only access to shared information serving different health economy needs and different parts and levels of the health economy. How is MCHFT IT currently structured? effective collaboration & communications Stronger Together (Graphnet Portal with UHNM) Integrated Digital Care Record GP Records (90% EMIS Web) (Graphnet Portal – Cheshire) Heterogeneous clinical application set with some integration of data across some systems using Cloverleaf. Varying levels of stability and satisfaction National Summary Care Record (Pharmacy) clinical applications exploiting Silverlink PAS A&E Maternity (System C Medway) E-Handover PACS RIS (EMIS) enabling research & intelligence ESR Nurse Bank Non Clinical Applications Theatres (Theatreman) Orders & Results (Homecare – Oncology, EPMA (ICE) and Ascribe – Dispensing)i (Qikview, PLICS) Endoscopy, Ophthalmology, Colposcopy, Fetal Heart Monitoring, Infection Control, Colonoscopy, Birth Records resource & asset management (Finance, Estates …) Telephony Wireless Network CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 ( Fixed Network Data Warehouse (CACI) Other Departl Pathology Infrastructure foundation Business Intelligence VDI Mobile Platforms 36 Licensing Some integration via Cloverleaf Evolving BI capability using up to date platforms but not yet offering “power user” operational capability for clinicians and managers. Evolving infrastructure with some hidden costs that might impede progress for clinical applications (licensing, integration). Partial solution, work in progress, or known issues Generally fit for purpose, known plans and no major issues or concerns 36
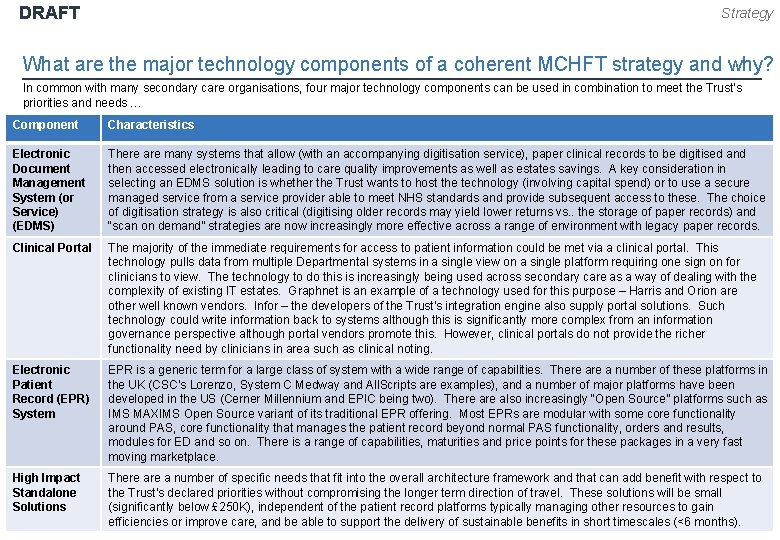
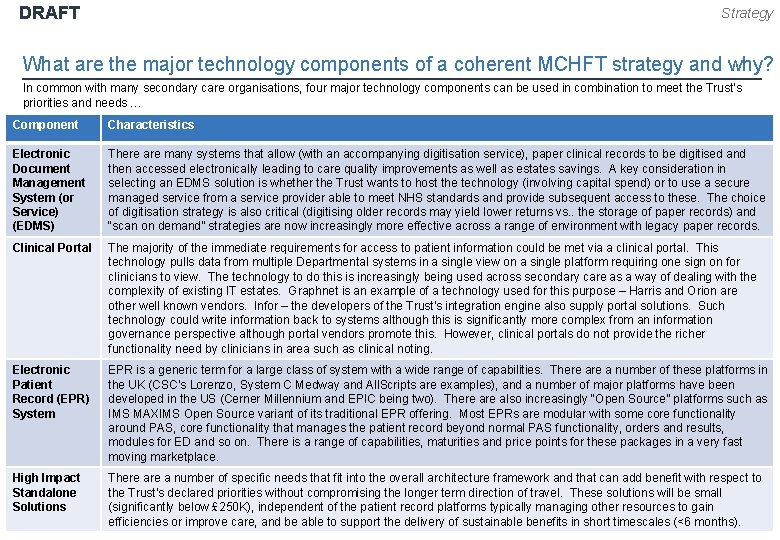
DRAFT Strategy What are the major technology components of a coherent MCHFT strategy and why? In common with many secondary care organisations, four major technology components can be used in combination to meet the Trust’s priorities and needs … Component Characteristics Electronic Document Management System (or Service) (EDMS) There are many systems that allow (with an accompanying digitisation service), paper clinical records to be digitised and then accessed electronically leading to care quality improvements as well as estates savings. A key consideration in selecting an EDMS solution is whether the Trust wants to host the technology (involving capital spend) or to use a secure managed service from a service provider able to meet NHS standards and provide subsequent access to these. The choice of digitisation strategy is also critical (digitising older records may yield lower returns vs. . the storage of paper records) and “scan on demand” strategies are now increasingly more effective across a range of environment with legacy paper records. Clinical Portal The majority of the immediate requirements for access to patient information could be met via a clinical portal. This technology pulls data from multiple Departmental systems in a single view on a single platform requiring one sign on for clinicians to view. The technology to do this is increasingly being used across secondary care as a way of dealing with the complexity of existing IT estates. Graphnet is an example of a technology used for this purpose – Harris and Orion are other well known vendors. Infor – the developers of the Trust's integration engine also supply portal solutions. Such technology could write information back to systems although this is significantly more complex from an information governance perspective although portal vendors promote this. However, clinical portals do not provide the richer functionality need by clinicians in area such as clinical noting. Electronic Patient Record (EPR) System EPR is a generic term for a large class of system with a wide range of capabilities. There a number of these platforms in the UK (CSC’s Lorenzo, System C Medway and All. Scripts are examples), and a number of major platforms have been developed in the US (Cerner Millennium and EPIC being two). There also increasingly “Open Source” platforms such as IMS MAXIMS Open Source variant of its traditional EPR offering. Most EPRs are modular with some core functionality around PAS, core functionality that manages the patient record beyond normal PAS functionality, orders and results, modules for ED and so on. There is a range of capabilities, maturities and price points for these packages in a very fast moving marketplace. High Impact Standalone Solutions There a number of specific needs that fit into the overall architecture framework and that can add benefit with respect to the Trust's declared priorities without compromising the longer term direction of travel. These solutions will be small (significantly below £ 250 K), independent of the patient record platforms typically managing other resources to gain CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT 37 © PA Knowledge Limited 2014 efficiencies or improve care, and be able to support the delivery of sustainable benefits in short timescales (<6 months).
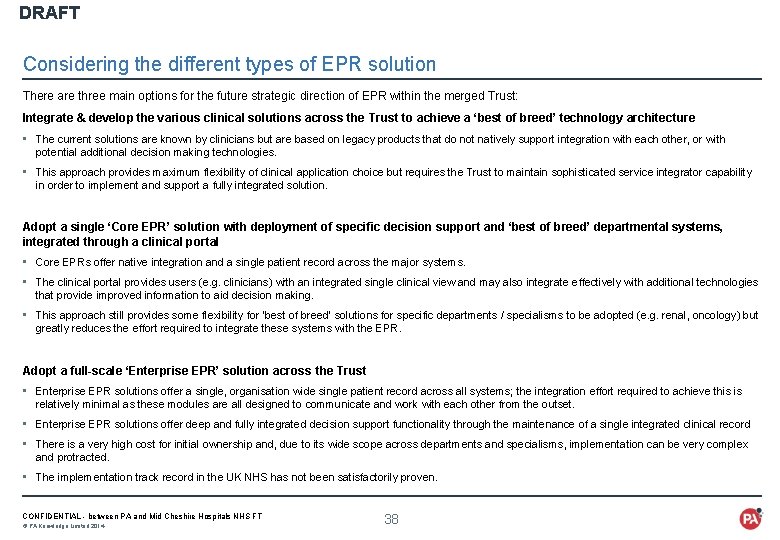
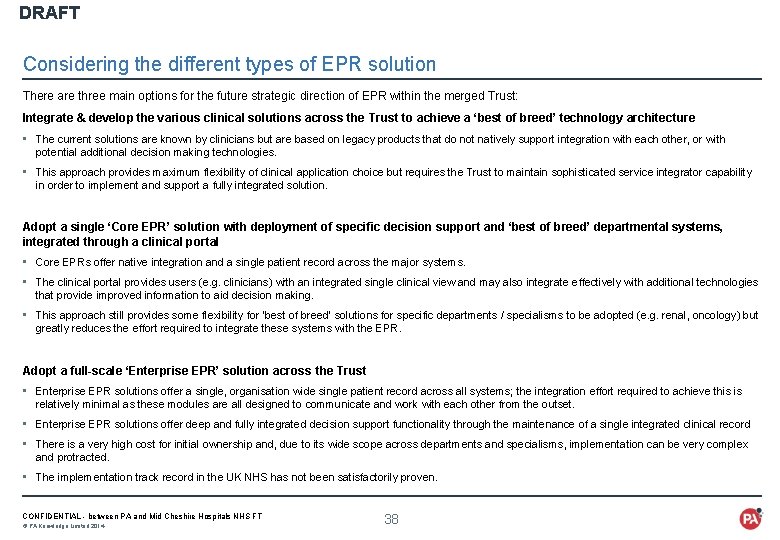
DRAFT Considering the different types of EPR solution There are three main options for the future strategic direction of EPR within the merged Trust: Integrate & develop the various clinical solutions across the Trust to achieve a ‘best of breed’ technology architecture • The current solutions are known by clinicians but are based on legacy products that do not natively support integration with each other, or with potential additional decision making technologies. • This approach provides maximum flexibility of clinical application choice but requires the Trust to maintain sophisticated service integrator capability in order to implement and support a fully integrated solution. Adopt a single ‘Core EPR’ solution with deployment of specific decision support and ‘best of breed’ departmental systems, integrated through a clinical portal • Core EPRs offer native integration and a single patient record across the major systems. • The clinical portal provides users (e. g. clinicians) with an integrated single clinical view and may also integrate effectively with additional technologies that provide improved information to aid decision making. • This approach still provides some flexibility for ‘best of breed’ solutions for specific departments / specialisms to be adopted (e. g. renal, oncology) but greatly reduces the effort required to integrate these systems with the EPR. Adopt a full-scale ‘Enterprise EPR’ solution across the Trust • Enterprise EPR solutions offer a single, organisation wide single patient record across all systems; the integration effort required to achieve this is relatively minimal as these modules are all designed to communicate and work with each other from the outset. • Enterprise EPR solutions offer deep and fully integrated decision support functionality through the maintenance of a single integrated clinical record • There is a very high cost for initial ownership and, due to its wide scope across departments and specialisms, implementation can be very complex and protracted. • The implementation track record in the UK NHS has not been satisfactorily proven. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 38
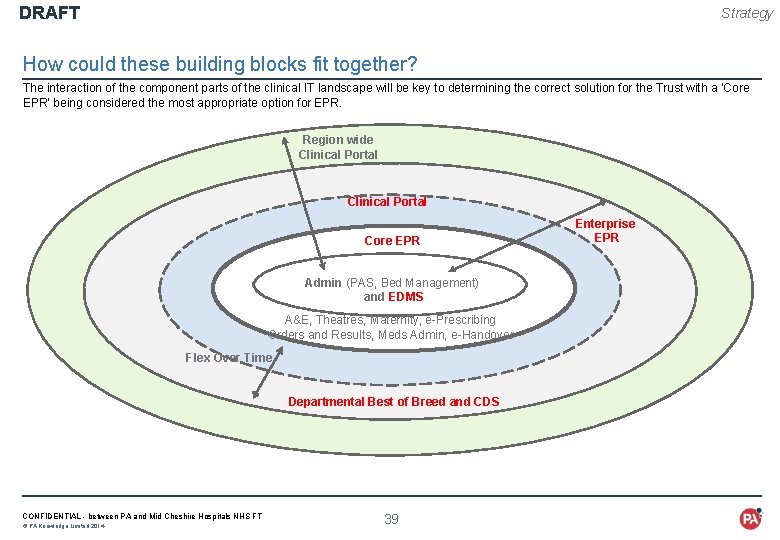
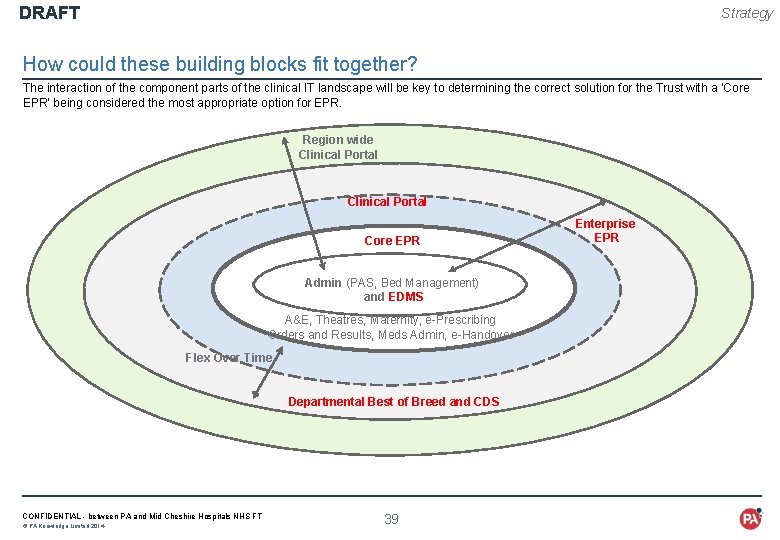
DRAFT Strategy How could these building blocks fit together? The interaction of the component parts of the clinical IT landscape will be key to determining the correct solution for the Trust with a ‘Core EPR’ being considered the most appropriate option for EPR. Region wide Clinical Portal Core EPR Admin (PAS, Bed Management) and EDMS A&E, Theatres, Maternity, e-Prescribing Orders and Results, Meds Admin, e-Handover Flex Over Time Departmental Best of Breed and CDS CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 39 Enterprise EPR
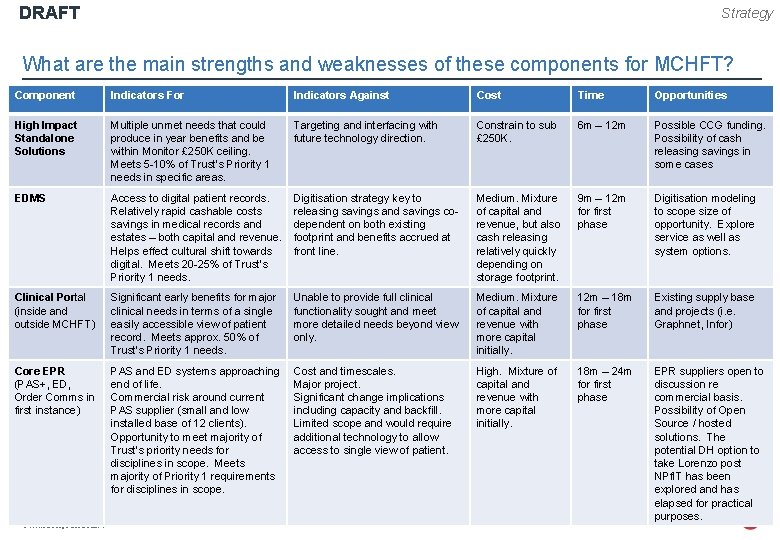
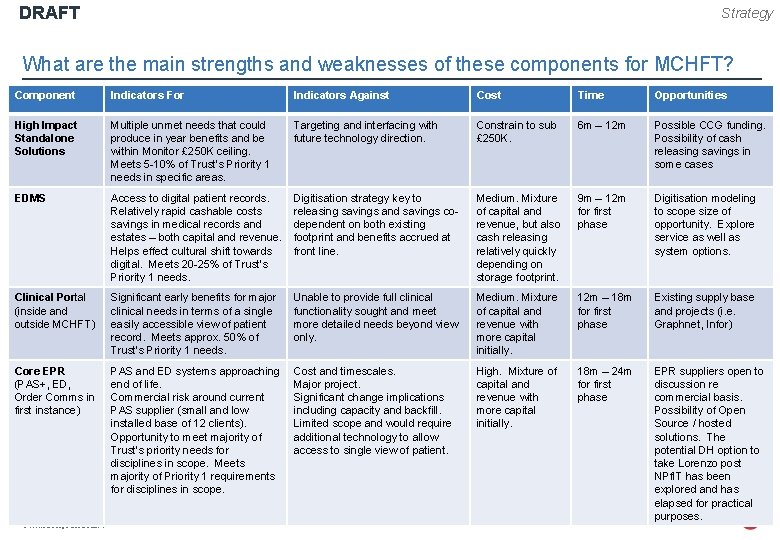
DRAFT Strategy What are the main strengths and weaknesses of these components for MCHFT? Component Indicators For Indicators Against Cost Time Opportunities High Impact Standalone Solutions Multiple unmet needs that could produce in year benefits and be within Monitor £ 250 K ceiling. Meets 5 -10% of Trust’s Priority 1 needs in specific areas. Targeting and interfacing with future technology direction. Constrain to sub £ 250 K. 6 m – 12 m Possible CCG funding. Possibility of cash releasing savings in some cases EDMS Access to digital patient records. Relatively rapid cashable costs savings in medical records and estates – both capital and revenue. Helps effect cultural shift towards digital. Meets 20 -25% of Trust’s Priority 1 needs. Digitisation strategy key to releasing savings and savings codependent on both existing footprint and benefits accrued at front line. Medium. Mixture of capital and revenue, but also cash releasing relatively quickly depending on storage footprint. 9 m – 12 m for first phase Digitisation modeling to scope size of opportunity. Explore service as well as system options. Clinical Portal (inside and outside MCHFT) Significant early benefits for major clinical needs in terms of a single easily accessible view of patient record. Meets approx. 50% of Trust’s Priority 1 needs. Unable to provide full clinical functionality sought and meet more detailed needs beyond view only. Medium. Mixture of capital and revenue with more capital initially. 12 m – 18 m for first phase Existing supply base and projects (i. e. Graphnet, Infor) Core EPR (PAS+, ED, Order Comms in first instance) PAS and ED systems approaching end of life. Commercial risk around current PAS supplier (small and low installed base of 12 clients). Opportunity to meet majority of Trust’s priority needs for disciplines in scope. Meets majority of Priority 1 requirements for disciplines in scope. Cost and timescales. Major project. Significant change implications including capacity and backfill. Limited scope and would require additional technology to allow access to single view of patient. High. Mixture of capital and revenue with more capital initially. 18 m – 24 m for first phase EPR suppliers open to discussion re commercial basis. Possibility of Open Source / hosted solutions. The potential DH option to take Lorenzo post NPf. IT has been explored and has elapsed for practical purposes. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 40
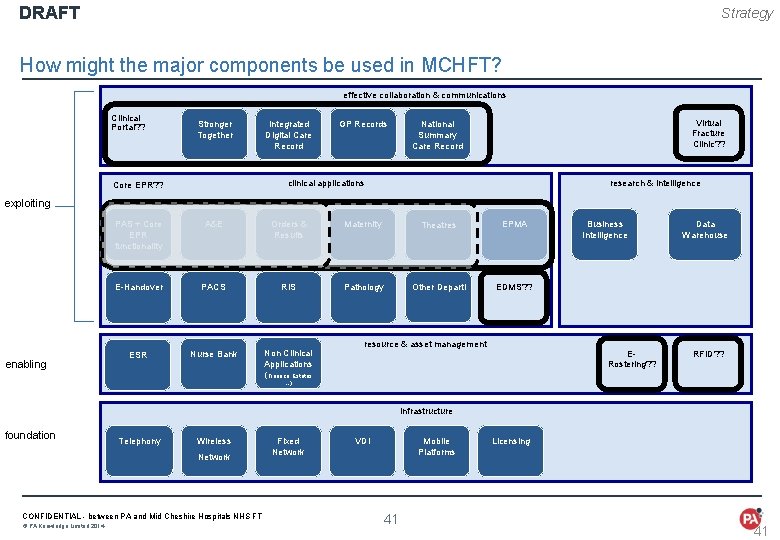
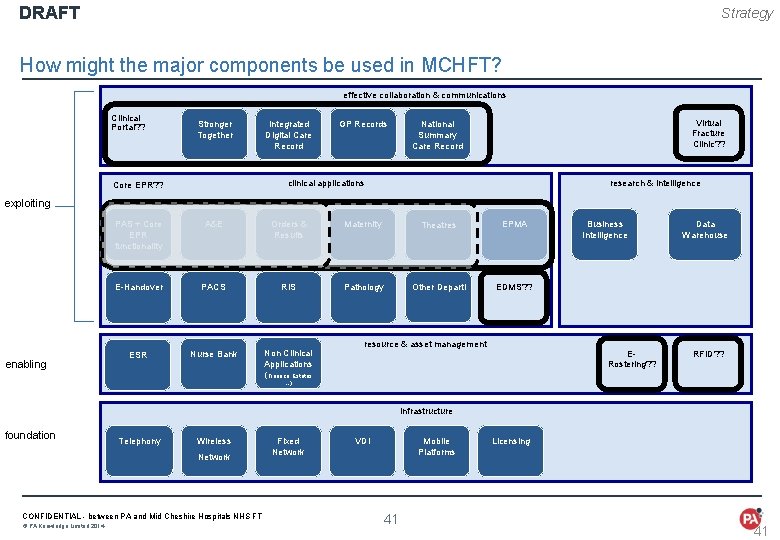
DRAFT Strategy How might the major components be used in MCHFT? effective collaboration & communications Clinical Portal? ? Stronger Together Integrated Digital Care Record GP Records Virtual Fracture Clinic? ? National Summary Care Record clinical applications Core EPR? ? research & intelligence exploiting enabling PAS + Core EPR functionality A&E Orders & Results Maternity Theatres EPMA E-Handover PACS RIS Pathology Other Departl EDMS? ? ESR Nurse Bank Non Clinical Applications (Finance, Estates resource & asset management Business Intelligence ERostering? ? Data Warehouse RFID? ? …) Infrastructure foundation Telephony Wireless Network CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 Fixed Network VDI Mobile Platforms 41 Licensing 41
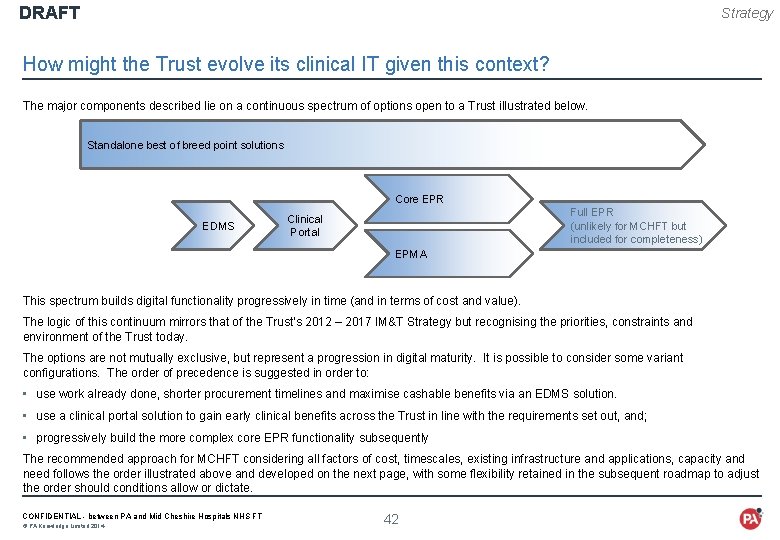
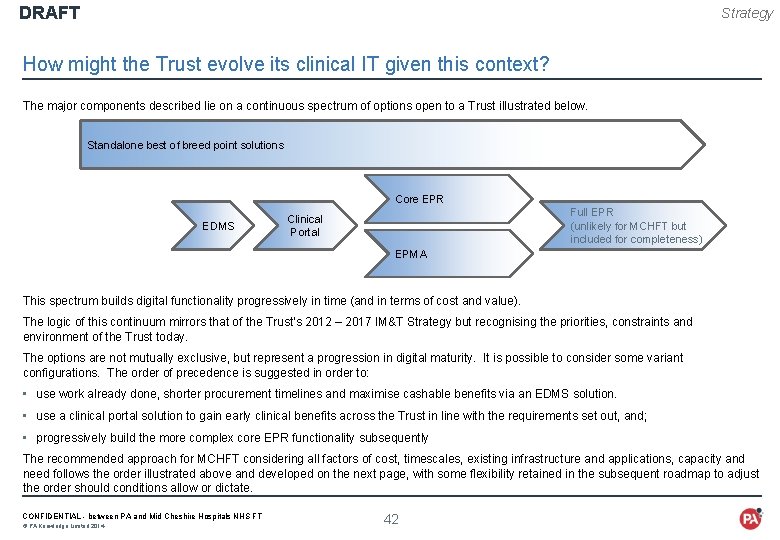
DRAFT Strategy How might the Trust evolve its clinical IT given this context? The major components described lie on a continuous spectrum of options open to a Trust illustrated below. Standalone best of breed point solutions Core EPR EDMS Full EPR (unlikely for MCHFT but included for completeness) Clinical Portal EPMA This spectrum builds digital functionality progressively in time (and in terms of cost and value). The logic of this continuum mirrors that of the Trust’s 2012 – 2017 IM&T Strategy but recognising the priorities, constraints and environment of the Trust today. The options are not mutually exclusive, but represent a progression in digital maturity. It is possible to consider some variant configurations. The order of precedence is suggested in order to: • use work already done, shorter procurement timelines and maximise cashable benefits via an EDMS solution. • use a clinical portal solution to gain early clinical benefits across the Trust in line with the requirements set out, and; • progressively build the more complex core EPR functionality subsequently The recommended approach for MCHFT considering all factors of cost, timescales, existing infrastructure and applications, capacity and need follows the order illustrated above and developed on the next page, with some flexibility retained in the subsequent roadmap to adjust the order should conditions allow or dictate. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 42
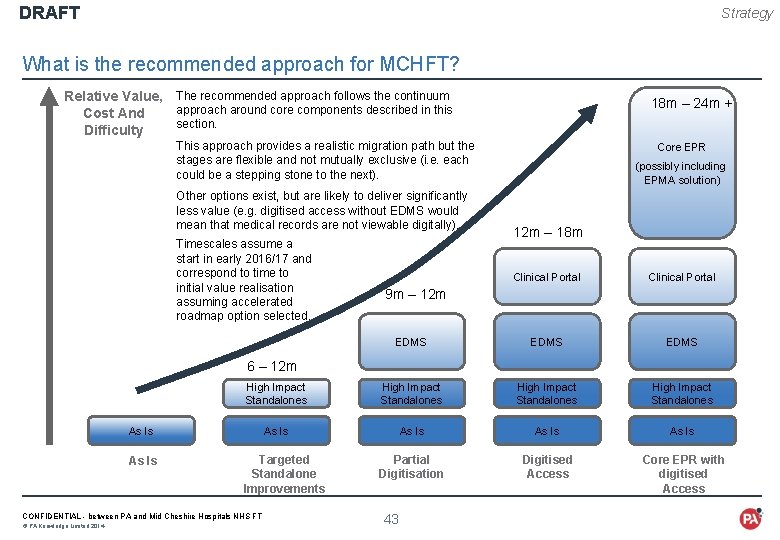
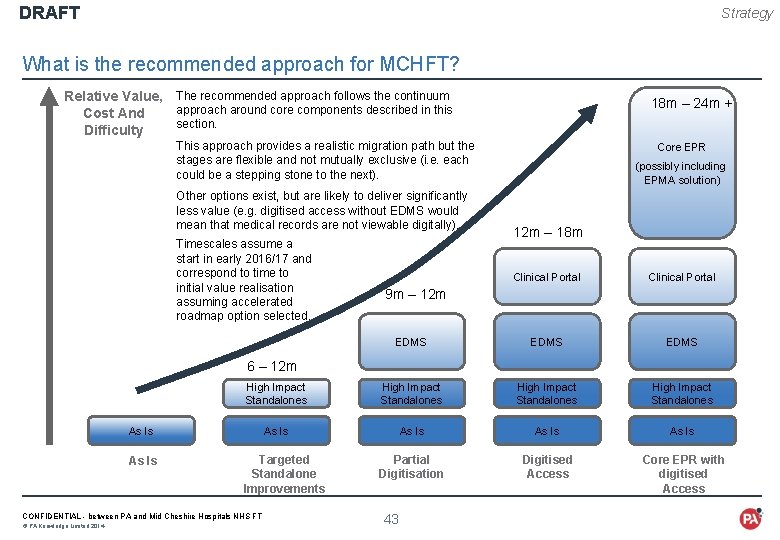
DRAFT Strategy What is the recommended approach for MCHFT? Relative Value, The recommended approach follows the continuum approach around core components described in this Cost And section. Difficulty 18 m – 24 m + This approach provides a realistic migration path but the stages are flexible and not mutually exclusive (i. e. each could be a stepping stone to the next). Other options exist, but are likely to deliver significantly less value (e. g. digitised access without EDMS would mean that medical records are not viewable digitally). Timescales assume a start in early 2016/17 and correspond to time to initial value realisation assuming accelerated roadmap option selected. Core EPR (possibly including EPMA solution) 12 m – 18 m Clinical Portal EDMS High Impact Standalones As Is Partial Digitisation Digitised Access Core EPR with digitised Access 9 m – 12 m 6 – 12 m As Is Targeted Standalone Improvements CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 43
DRAFT ROADMAP - HOW COULD THE IT COMPONENTS BE DELIVERED OVER THE NEXT 3 YEARS? CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 · Principles underlying the recommended Roadmap · 3 year Roadmap for delivering the strategy · 12 month action plan including changes to existing projects · 3 month view of next steps 44
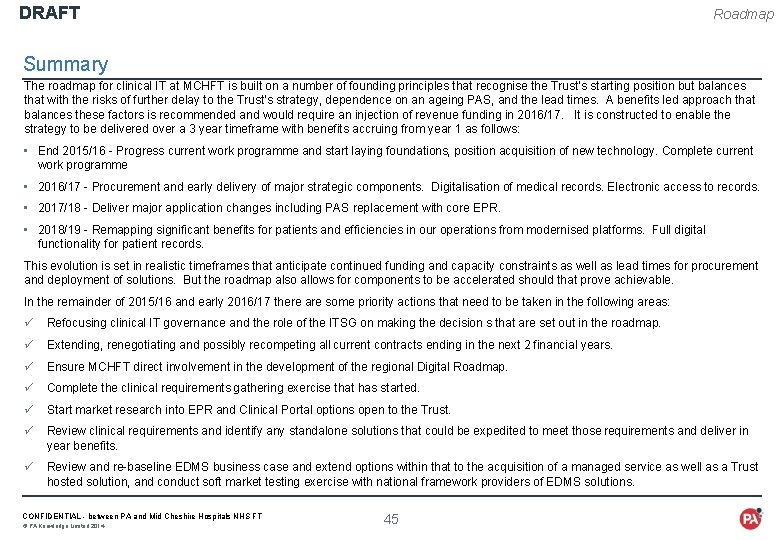
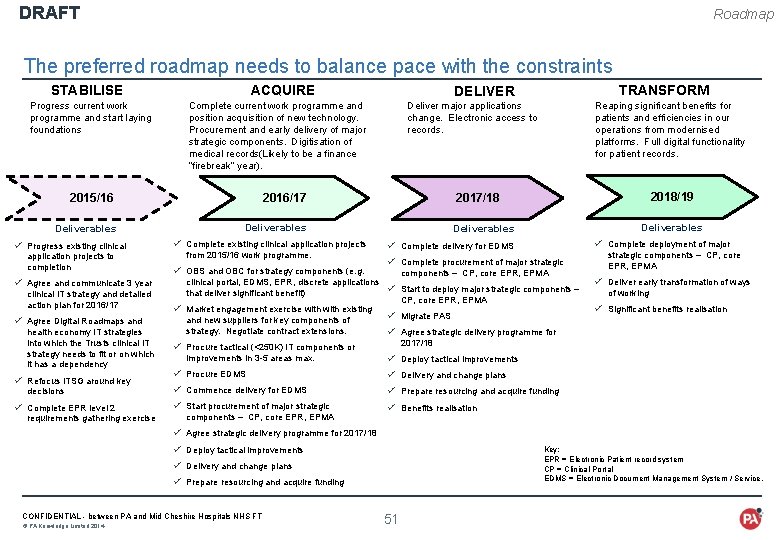
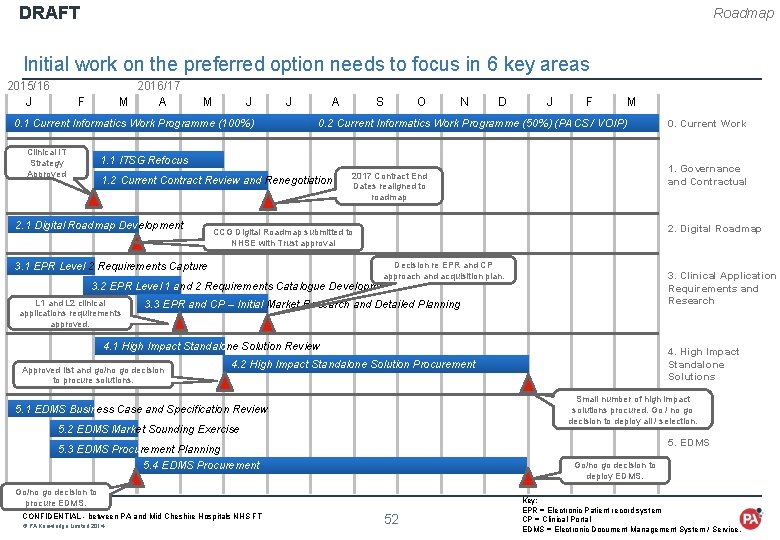
DRAFT Roadmap Summary The roadmap for clinical IT at MCHFT is built on a number of founding principles that recognise the Trust’s starting position but balances that with the risks of further delay to the Trust’s strategy, dependence on an ageing PAS, and the lead times. A benefits led approach that balances these factors is recommended and would require an injection of revenue funding in 2016/17. It is constructed to enable the strategy to be delivered over a 3 year timeframe with benefits accruing from year 1 as follows: • End 2015/16 - Progress current work programme and start laying foundations, position acquisition of new technology. Complete current work programme • 2016/17 - Procurement and early delivery of major strategic components. Digitalisation of medical records. Electronic access to records. • 2017/18 - Deliver major application changes including PAS replacement with core EPR. • 2018/19 - Remapping significant benefits for patients and efficiencies in our operations from modernised platforms. Full digital functionality for patient records. This evolution is set in realistic timeframes that anticipate continued funding and capacity constraints as well as lead times for procurement and deployment of solutions. But the roadmap also allows for components to be accelerated should that prove achievable. In the remainder of 2015/16 and early 2016/17 there are some priority actions that need to be taken in the following areas: ü Refocusing clinical IT governance and the role of the ITSG on making the decision s that are set out in the roadmap. ü Extending, renegotiating and possibly recompeting all current contracts ending in the next 2 financial years. ü Ensure MCHFT direct involvement in the development of the regional Digital Roadmap. ü Complete the clinical requirements gathering exercise that has started. ü Start market research into EPR and Clinical Portal options open to the Trust. ü Review clinical requirements and identify any standalone solutions that could be expedited to meet those requirements and deliver in year benefits. ü Review and re-baseline EDMS business case and extend options within that to the acquisition of a managed service as well as a Trust hosted solution, and conduct soft market testing exercise with national framework providers of EDMS solutions. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 45
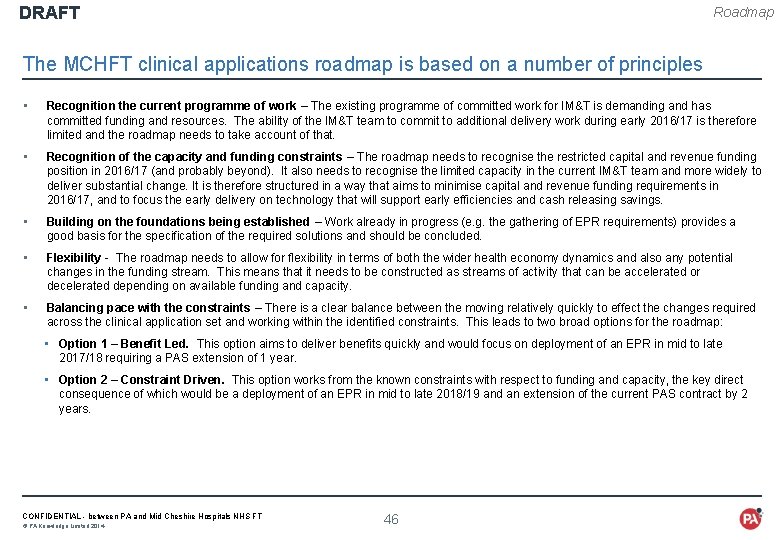
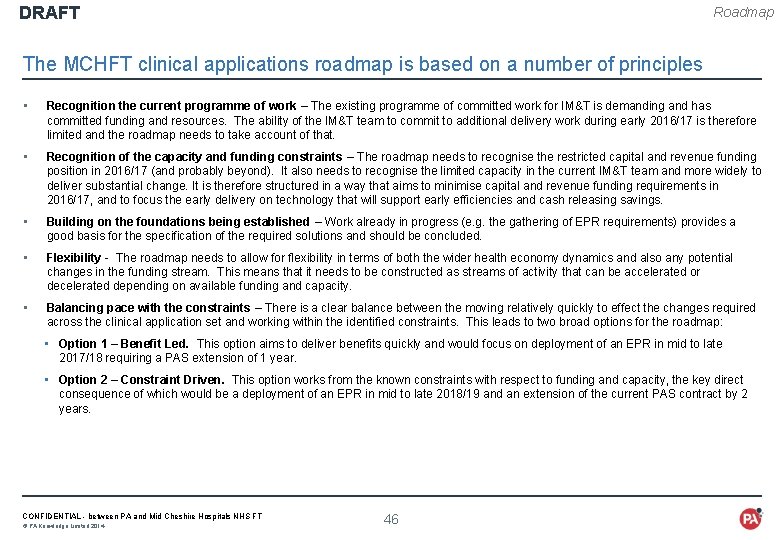
DRAFT Roadmap The MCHFT clinical applications roadmap is based on a number of principles • Recognition the current programme of work – The existing programme of committed work for IM&T is demanding and has committed funding and resources. The ability of the IM&T team to commit to additional delivery work during early 2016/17 is therefore limited and the roadmap needs to take account of that. • Recognition of the capacity and funding constraints – The roadmap needs to recognise the restricted capital and revenue funding position in 2016/17 (and probably beyond). It also needs to recognise the limited capacity in the current IM&T team and more widely to deliver substantial change. It is therefore structured in a way that aims to minimise capital and revenue funding requirements in 2016/17, and to focus the early delivery on technology that will support early efficiencies and cash releasing savings. • Building on the foundations being established – Work already in progress (e. g. the gathering of EPR requirements) provides a good basis for the specification of the required solutions and should be concluded. • Flexibility - The roadmap needs to allow for flexibility in terms of both the wider health economy dynamics and also any potential changes in the funding stream. This means that it needs to be constructed as streams of activity that can be accelerated or decelerated depending on available funding and capacity. • Balancing pace with the constraints – There is a clear balance between the moving relatively quickly to effect the changes required across the clinical application set and working within the identified constraints. This leads to two broad options for the roadmap: • Option 1 – Benefit Led. This option aims to deliver benefits quickly and would focus on deployment of an EPR in mid to late 2017/18 requiring a PAS extension of 1 year. • Option 2 – Constraint Driven. This option works from the known constraints with respect to funding and capacity, the key direct consequence of which would be a deployment of an EPR in mid to late 2018/19 and an extension of the current PAS contract by 2 years. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 46
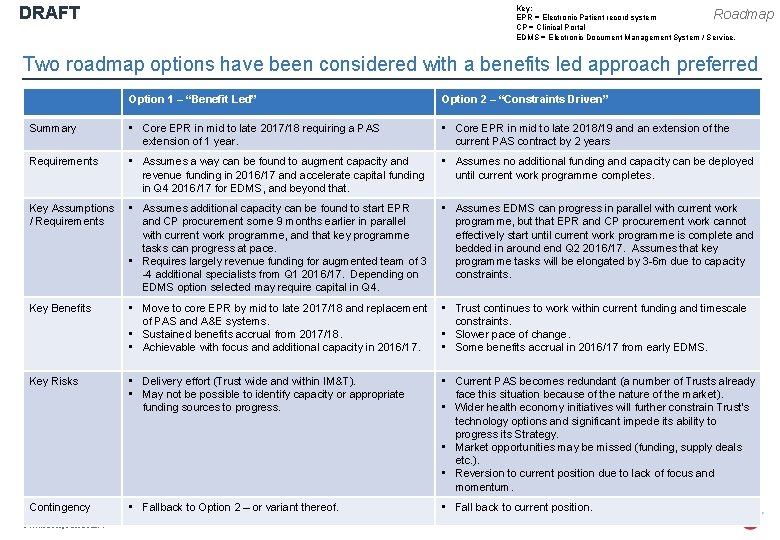
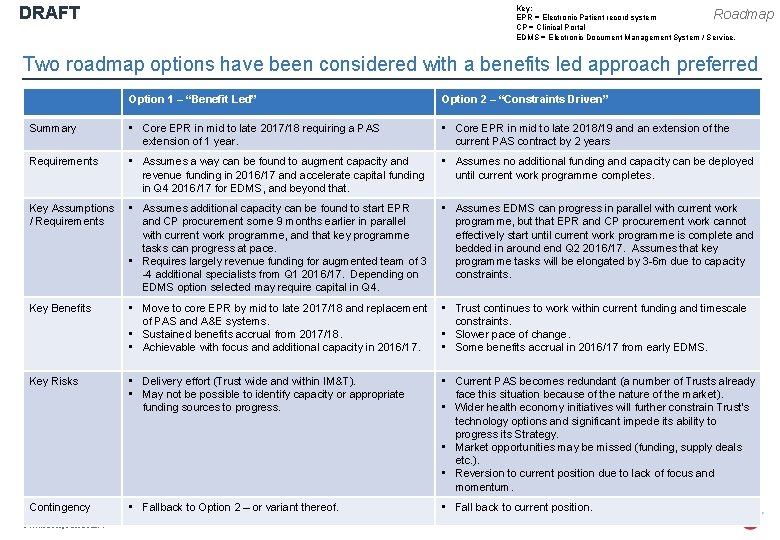
DRAFT Key: EPR = Electronic Patient record system CP = Clinical Portal EDMS = Electronic Document Management System / Service. Roadmap Two roadmap options have been considered with a benefits led approach preferred Option 1 – “Benefit Led” Option 2 – “Constraints Driven” Summary • Core EPR in mid to late 2017/18 requiring a PAS extension of 1 year. • Core EPR in mid to late 2018/19 and an extension of the current PAS contract by 2 years Requirements • Assumes a way can be found to augment capacity and revenue funding in 2016/17 and accelerate capital funding in Q 4 2016/17 for EDMS, and beyond that. • Assumes no additional funding and capacity can be deployed until current work programme completes. Key Assumptions / Requirements • Assumes additional capacity can be found to start EPR and CP procurement some 9 months earlier in parallel with current work programme, and that key programme tasks can progress at pace. • Requires largely revenue funding for augmented team of 3 -4 additional specialists from Q 1 2016/17. Depending on EDMS option selected may require capital in Q 4. • Assumes EDMS can progress in parallel with current work programme, but that EPR and CP procurement work cannot effectively start until current work programme is complete and bedded in around end Q 2 2016/17. Assumes that key programme tasks will be elongated by 3 -6 m due to capacity constraints. Key Benefits • Move to core EPR by mid to late 2017/18 and replacement • Trust continues to work within current funding and timescale of PAS and A&E systems. constraints. • Sustained benefits accrual from 2017/18. • Slower pace of change. • Achievable with focus and additional capacity in 2016/17. • Some benefits accrual in 2016/17 from early EDMS. Key Risks • Delivery effort (Trust wide and within IM&T). • May not be possible to identify capacity or appropriate funding sources to progress. • Current PAS becomes redundant (a number of Trusts already face this situation because of the nature of the market). • Wider health economy initiatives will further constrain Trust’s technology options and significant impede its ability to progress its Strategy. • Market opportunities may be missed (funding, supply deals etc. ). • Reversion to current position due to lack of focus and momentum. Contingency • Fallback to Option 2 – or variant thereof. • Fall back to current position. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 47
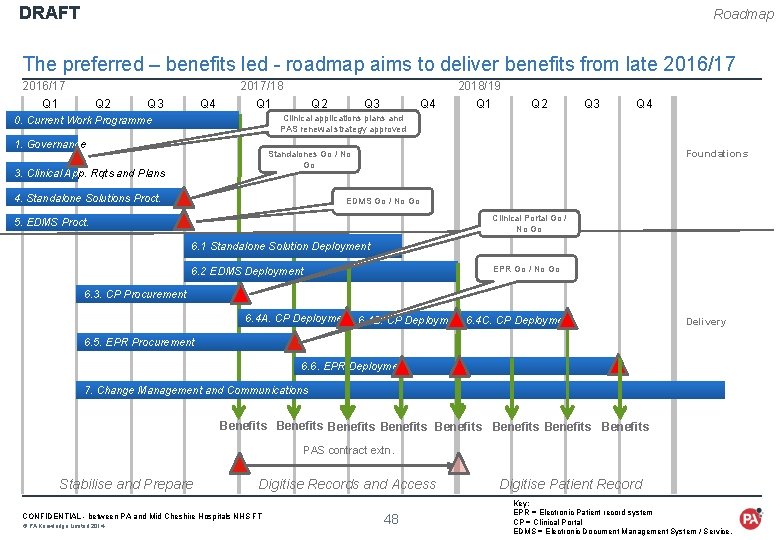
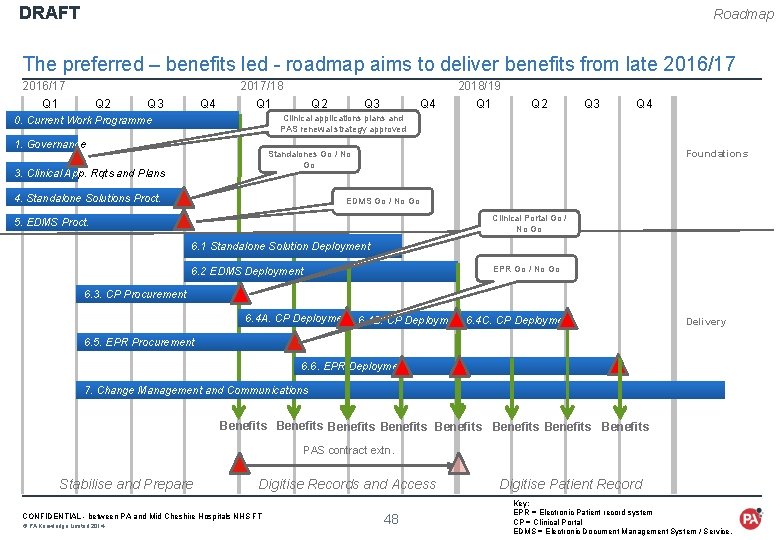
DRAFT Roadmap The preferred – benefits led - roadmap aims to deliver benefits from late 2016/17 2017/18 2018/19 Q 1 Q 2 Q 3 Q 4 Clinical applications plans and PAS renewal strategy approved 0. Current Work Programme 1. Governance Foundations Standalones Go / No Go 3. Clinical App. Rqts and Plans 4. Standalone Solutions Proct. EDMS Go / No Go Clinical Portal Go / No Go 5. EDMS Proct. 6. 1 Standalone Solution Deployment EPR Go / No Go 6. 2 EDMS Deployment 6. 3. CP Procurement 6. 4 A. CP Deployment 6. 4 B. CP Deployment 6. 4 C. CP Deployment Delivery 6. 5. EPR Procurement 6. 6. EPR Deployment 7. Change Management and Communications Benefits Benefits PAS contract extn. Stabilise and Prepare Digitise Records and Access CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 48 Digitise Patient Record Key: EPR = Electronic Patient record system CP = Clinical Portal EDMS = Electronic Document Management System / Service.
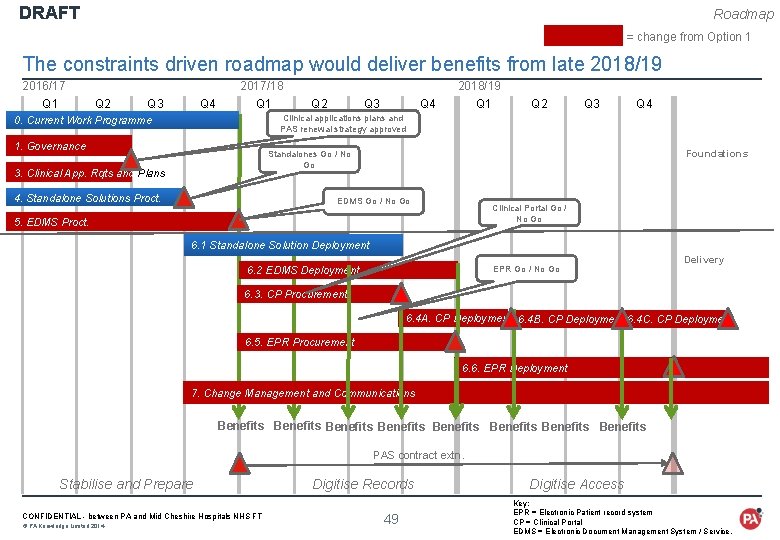
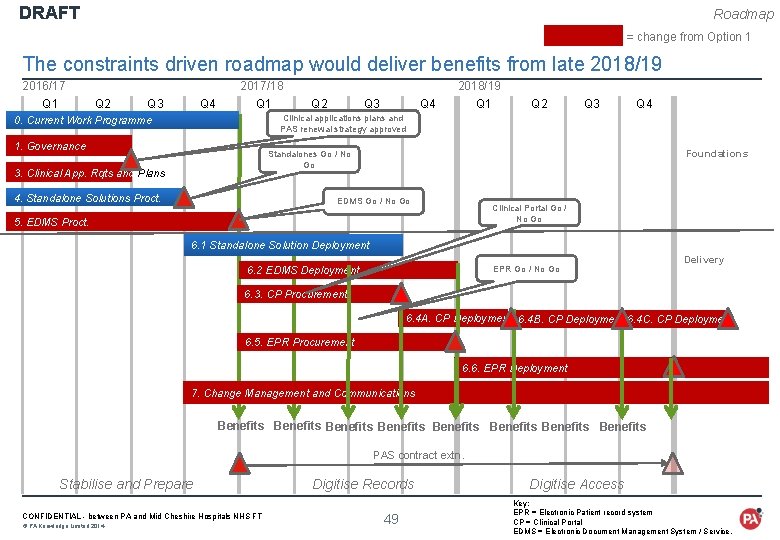
DRAFT Roadmap = change from Option 1 The constraints driven roadmap would deliver benefits from late 2018/19 2016/17 2017/18 2018/19 Q 1 Q 2 Q 3 Q 4 Clinical applications plans and PAS renewal strategy approved 0. Current Work Programme 1. Governance Foundations Standalones Go / No Go 3. Clinical App. Rqts and Plans 4. Standalone Solutions Proct. EDMS Go / No Go Clinical Portal Go / No Go 5. EDMS Proct. 6. 1 Standalone Solution Deployment EPR Go / No Go 6. 2 EDMS Deployment Delivery 6. 3. CP Procurement 6. 4 A. CP Deployment 6. 4 B. CP Deployment 6. 4 C. CP Deployment 6. 5. EPR Procurement 6. 6. EPR Deployment 7. Change Management and Communications Benefits Benefits PAS contract extn. Stabilise and Prepare CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 Digitise Records 49 Digitise Access Key: EPR = Electronic Patient record system CP = Clinical Portal EDMS = Electronic Document Management System / Service.
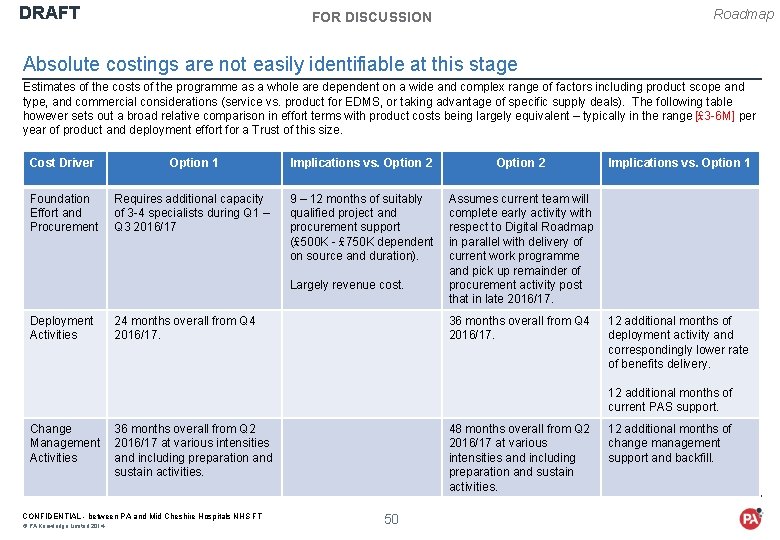
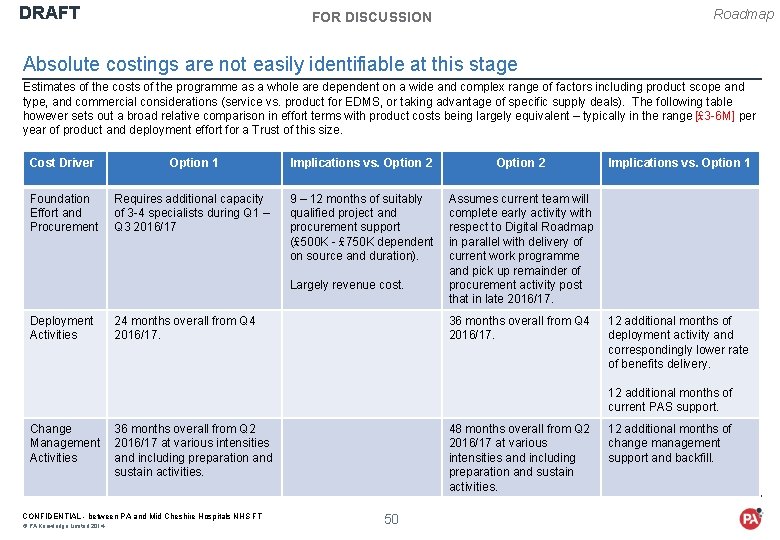
DRAFT Roadmap FOR DISCUSSION Absolute costings are not easily identifiable at this stage Estimates of the costs of the programme as a whole are dependent on a wide and complex range of factors including product scope and type, and commercial considerations (service vs. product for EDMS, or taking advantage of specific supply deals). The following table however sets out a broad relative comparison in effort terms with product costs being largely equivalent – typically in the range [£ 3 -6 M] per year of product and deployment effort for a Trust of this size. Cost Driver Option 1 Implications vs. Option 2 Foundation Effort and Procurement Requires additional capacity of 3 -4 specialists during Q 1 – Q 3 2016/17 9 – 12 months of suitably qualified project and procurement support (£ 500 K - £ 750 K dependent on source and duration). Assumes current team will complete early activity with respect to Digital Roadmap in parallel with delivery of current work programme and pick up remainder of procurement activity post that in late 2016/17. Largely revenue cost. Deployment Activities 24 months overall from Q 4 2016/17. 36 months overall from Q 4 2016/17. Implications vs. Option 1 12 additional months of deployment activity and correspondingly lower rate of benefits delivery. 12 additional months of current PAS support. Change 36 months overall from Q 2 Management 2016/17 at various intensities Activities and including preparation and sustain activities. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 48 months overall from Q 2 2016/17 at various intensities and including preparation and sustain activities. 50 12 additional months of change management support and backfill.
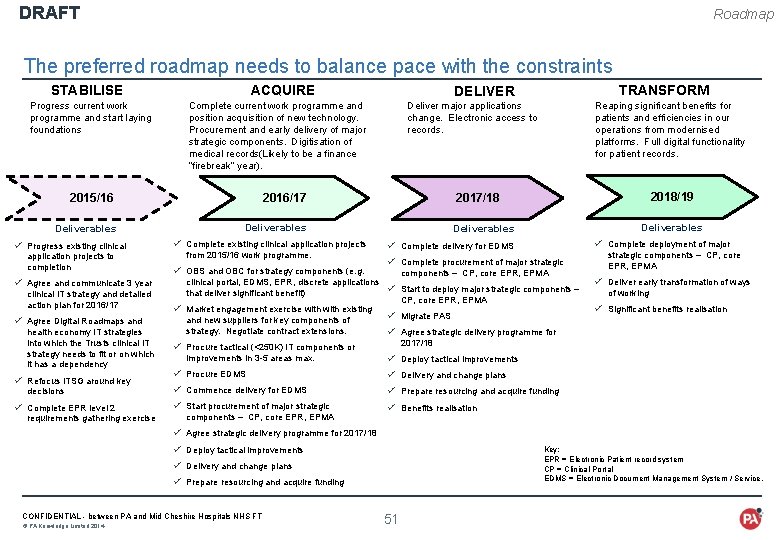
DRAFT Roadmap The preferred roadmap needs to balance pace with the constraints STABILISE Progress current work programme and start laying foundations ACQUIRE Complete current work programme and . position acquisition of new technology. Procurement and early delivery of major strategic components. Digitisation of medical records(Likely to be a finance “firebreak” year). 2015/16 Deliverables ü Progress existing clinical application projects to completion ü Agree and communicate 3 year clinical IT strategy and detailed action plan for 2016/17 ü Agree Digital Roadmaps and health economy IT strategies into which the Trusts clinical IT strategy needs to fit or on which it has a dependency ü Refocus ITSG around key decisions ü Complete EPR level 2 requirements gathering exercise Deliver major applications change. Electronic access to records. 2016/17 from 2015/16 work programme. ü OBS and OBC for strategy components (e. g. Reaping significant benefits for patients and efficiencies in our operations from modernised platforms. Full digital functionality for patient records. 2018/19 2017/18 Deliverables ü Complete existing clinical application projects TRANSFORM DELIVER Deliverables ü Complete deployment of major ü Complete delivery for EDMS ü Complete procurement of major strategic components – CP, core EPR, EPMA clinical portal, EDMS, EPR, discrete applications ü Start to deploy major strategic components – that deliver significant benefit) CP, core EPR, EPMA ü Market engagement exercise with existing ü Migrate PAS and new suppliers for key components of strategy. Negotiate contract extensions. ü Agree strategic delivery programme for 2017/18 ü Procure tactical (<250 K) IT components or improvements in 3 -5 areas max. ü Deliver early transformation of ways of working ü Significant benefits realisation ü Deploy tactical improvements ü Procure EDMS ü Delivery and change plans ü Commence delivery for EDMS ü Prepare resourcing and acquire funding ü Start procurement of major strategic ü Benefits realisation components – CP, core EPR, EPMA strategic components – CP, core EPR, EPMA ü Agree strategic delivery programme for 2017/18 ü Deploy tactical improvements Key: EPR = Electronic Patient record system CP = Clinical Portal EDMS = Electronic Document Management System / Service. ü Delivery and change plans ü Prepare resourcing and acquire funding CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 51
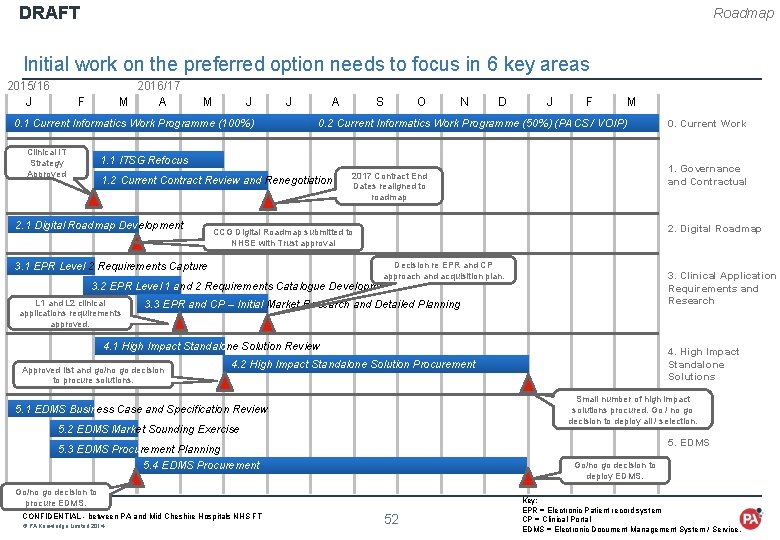
DRAFT Roadmap Initial work on the preferred option needs to focus in 6 key areas 2015/16 J 2016/17 F M A M J A S O N D J F M 0. 1 Current Informatics Work Programme (100%) Clinical IT Strategy Approved 0. 2 Current Informatics Work Programme (50%) (PACS / VOIP) 1. 1 ITSG Refocus 1. 2 Current Contract Review and Renegotiation 2. 1 Digital Roadmap Development 1. Governance and Contractual 2017 Contract End Dates realigned to roadmap 2. Digital Roadmap CCG Digital Roadmap submitted to NHSE with Trust approval Decision re EPR and CP approach and acquisition plan. 3. 1 EPR Level 2 Requirements Capture 3. Clinical Application Requirements and Research 3. 2 EPR Level 1 and 2 Requirements Catalogue Development L 1 and L 2 clinical applications requirements approved. 3. 3 EPR and CP – Initial Market Research and Detailed Planning 4. 1 High Impact Standalone Solution Review Approved list and go/no go decision to procure solutions. Small number of high impact solutions procured. Go / no go decision to deploy all / selection. 5. 1 EDMS Business Case and Specification Review 5. 2 EDMS Market Sounding Exercise 5. EDMS 5. 3 EDMS Procurement Planning 5. 4 EDMS Procurement Go/no go decision to deploy EDMS. Go/no go decision to procure EDMS. © PA Knowledge Limited 2014 4. High Impact Standalone Solutions 4. 2 High Impact Standalone Solution Procurement CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT 0. Current Work 52 Key: EPR = Electronic Patient record system CP = Clinical Portal EDMS = Electronic Document Management System / Service.
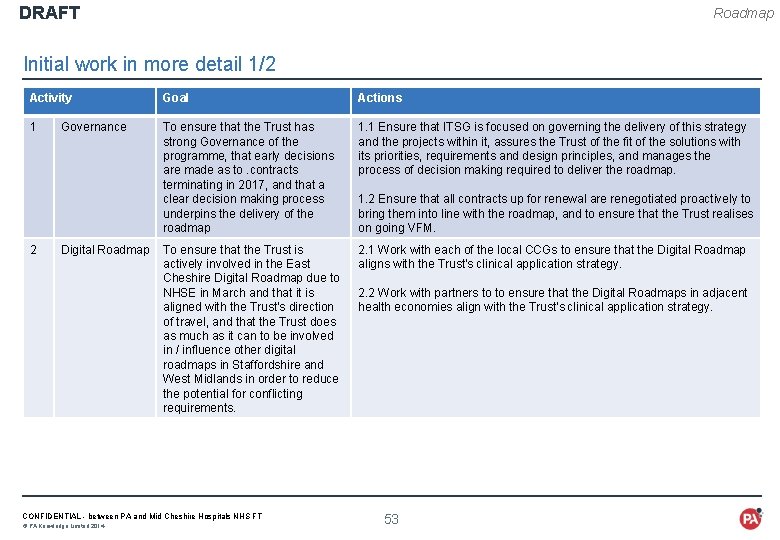
DRAFT Roadmap Initial work in more detail 1/2 Activity Goal Actions 1 To ensure that the Trust has strong Governance of the programme, that early decisions are made as to. contracts terminating in 2017, and that a clear decision making process underpins the delivery of the roadmap 1. 1 Ensure that ITSG is focused on governing the delivery of this strategy and the projects within it, assures the Trust of the fit of the solutions with its priorities, requirements and design principles, and manages the process of decision making required to deliver the roadmap. To ensure that the Trust is actively involved in the East Cheshire Digital Roadmap due to NHSE in March and that it is aligned with the Trust's direction of travel, and that the Trust does as much as it can to be involved in / influence other digital roadmaps in Staffordshire and West Midlands in order to reduce the potential for conflicting requirements. 2. 1 Work with each of the local CCGs to ensure that the Digital Roadmap aligns with the Trust's clinical application strategy. 2 Governance Digital Roadmap CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 1. 2 Ensure that all contracts up for renewal are renegotiated proactively to bring them into line with the roadmap, and to ensure that the Trust realises on going VFM. 2. 2 Work with partners to to ensure that the Digital Roadmaps in adjacent health economies align with the Trust's clinical application strategy. 53
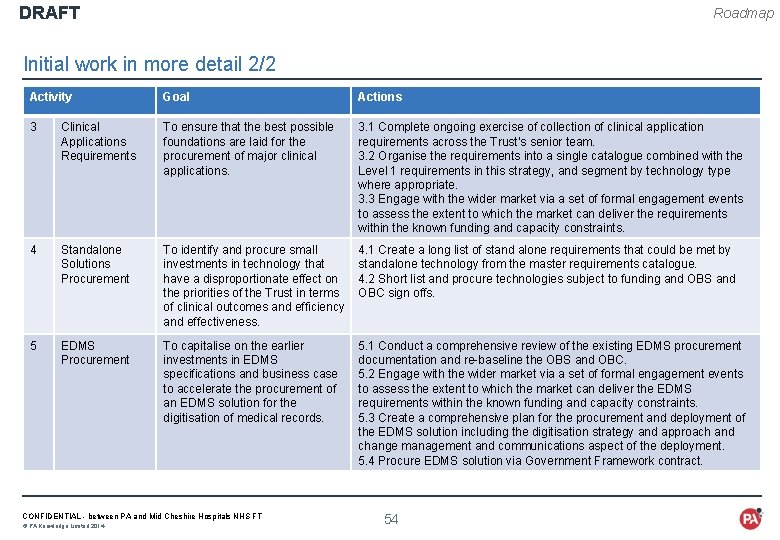
DRAFT Roadmap Initial work in more detail 2/2 Activity Goal Actions 3 Clinical Applications Requirements To ensure that the best possible foundations are laid for the procurement of major clinical applications. 3. 1 Complete ongoing exercise of collection of clinical application requirements across the Trust’s senior team. 3. 2 Organise the requirements into a single catalogue combined with the Level 1 requirements in this strategy, and segment by technology type where appropriate. 3. 3 Engage with the wider market via a set of formal engagement events to assess the extent to which the market can deliver the requirements within the known funding and capacity constraints. 4 Standalone Solutions Procurement To identify and procure small investments in technology that have a disproportionate effect on the priorities of the Trust in terms of clinical outcomes and efficiency and effectiveness. 4. 1 Create a long list of stand alone requirements that could be met by standalone technology from the master requirements catalogue. 4. 2 Short list and procure technologies subject to funding and OBS and OBC sign offs. 5 EDMS Procurement To capitalise on the earlier investments in EDMS specifications and business case to accelerate the procurement of an EDMS solution for the digitisation of medical records. 5. 1 Conduct a comprehensive review of the existing EDMS procurement documentation and re-baseline the OBS and OBC. 5. 2 Engage with the wider market via a set of formal engagement events to assess the extent to which the market can deliver the EDMS requirements within the known funding and capacity constraints. 5. 3 Create a comprehensive plan for the procurement and deployment of the EDMS solution including the digitisation strategy and approach and change management and communications aspect of the deployment. 5. 4 Procure EDMS solution via Government Framework contract. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 54
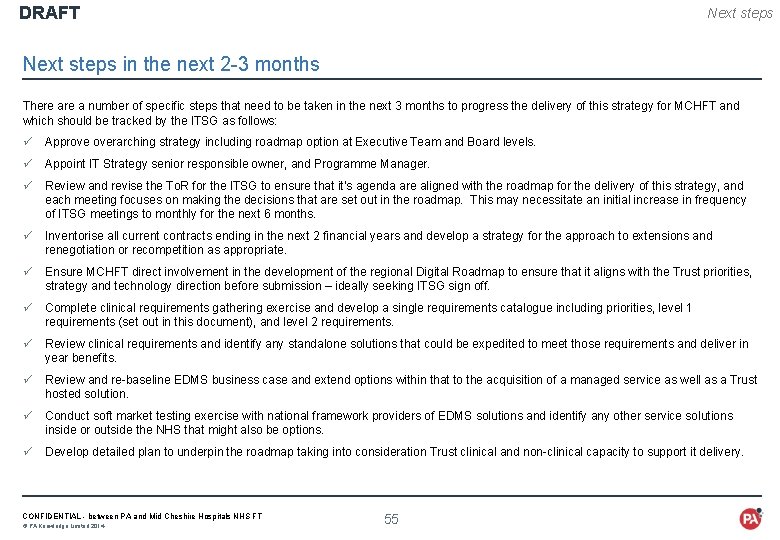
DRAFT Next steps in the next 2 -3 months There a number of specific steps that need to be taken in the next 3 months to progress the delivery of this strategy for MCHFT and which should be tracked by the ITSG as follows: ü Approve overarching strategy including roadmap option at Executive Team and Board levels. ü Appoint IT Strategy senior responsible owner, and Programme Manager. ü Review and revise the To. R for the ITSG to ensure that it’s agenda are aligned with the roadmap for the delivery of this strategy, and each meeting focuses on making the decisions that are set out in the roadmap. This may necessitate an initial increase in frequency of ITSG meetings to monthly for the next 6 months. ü Inventorise all current contracts ending in the next 2 financial years and develop a strategy for the approach to extensions and renegotiation or recompetition as appropriate. ü Ensure MCHFT direct involvement in the development of the regional Digital Roadmap to ensure that it aligns with the Trust priorities, strategy and technology direction before submission – ideally seeking ITSG sign off. ü Complete clinical requirements gathering exercise and develop a single requirements catalogue including priorities, level 1 requirements (set out in this document), and level 2 requirements. ü Review clinical requirements and identify any standalone solutions that could be expedited to meet those requirements and deliver in year benefits. ü Review and re-baseline EDMS business case and extend options within that to the acquisition of a managed service as well as a Trust hosted solution. ü Conduct soft market testing exercise with national framework providers of EDMS solutions and identify any other service solutions inside or outside the NHS that might also be options. ü Develop detailed plan to underpin the roadmap taking into consideration Trust clinical and non-clinical capacity to support it delivery. CONFIDENTIAL - between PA and Mid Cheshire Hospitals NHS FT © PA Knowledge Limited 2014 55
 Uhl management structure
Uhl management structure Portsmouth hospitals nhs trust jobs
Portsmouth hospitals nhs trust jobs Portsmouth hospital trust values
Portsmouth hospital trust values Western sussex hospitals nhs foundation trust board
Western sussex hospitals nhs foundation trust board Uhcw library
Uhcw library Objective of draw frame
Objective of draw frame Cheshire constabulary
Cheshire constabulary Cheshire cat allusion in fahrenheit 451
Cheshire cat allusion in fahrenheit 451 Cheshire golf union
Cheshire golf union Cheshire and merseyside training hub
Cheshire and merseyside training hub Cheshire ireland pay scale
Cheshire ireland pay scale St claret school barrackpore
St claret school barrackpore David cheshire aecom
David cheshire aecom Trickster archtype
Trickster archtype Fahrenheit 451 hook
Fahrenheit 451 hook Cheshire and merseyside stp
Cheshire and merseyside stp Midterm for one for short
Midterm for one for short Mid year budget review
Mid year budget review Mid year budget review
Mid year budget review University hospitals
University hospitals Application of computer in hospital
Application of computer in hospital Lokmanya hospitals private limited
Lokmanya hospitals private limited Fhpl jaipur
Fhpl jaipur Weaknesses examples
Weaknesses examples Louisiana department of health health standards section
Louisiana department of health health standards section Bed management in hospitals
Bed management in hospitals Dnv vs jcaho
Dnv vs jcaho 2 bin inventory hospitals
2 bin inventory hospitals Erp for hospitals
Erp for hospitals Lean hospitals
Lean hospitals Ipsg
Ipsg Mghs wheelers
Mghs wheelers Bcp for hospitals
Bcp for hospitals Mandatory standards
Mandatory standards Medisep hospitals in kerala
Medisep hospitals in kerala Echs visakhapatnam
Echs visakhapatnam National accreditation board for hospitals
National accreditation board for hospitals Lean hospitals mark graban
Lean hospitals mark graban Va hospitals in alaska
Va hospitals in alaska University of iowa hospitals and clinics
University of iowa hospitals and clinics Writ of certiorari ap gov example
Writ of certiorari ap gov example Narrative review vs systematic review
Narrative review vs systematic review What is inclusion and exclusion
What is inclusion and exclusion Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Narrative review vs systematic review
Narrative review vs systematic review Small gas engines chapter 8 answers
Small gas engines chapter 8 answers Draft outline pelatihan
Draft outline pelatihan Down draft
Down draft Network slicing draft
Network slicing draft Mla format rough draft
Mla format rough draft Cohen v california
Cohen v california First draft of a report on the edvac
First draft of a report on the edvac Draft for discussion
Draft for discussion Thesis draft
Thesis draft Drafts in portfolio
Drafts in portfolio Draft
Draft