Disorders of Lid Dr Ajai Agrawal Additional Professor












- Slides: 56
Disorders of Lid Dr Ajai Agrawal Additional Professor Department of Ophthalmology AIIMS, Rishikesh 1
Acknowledgement • Photographs and figures in this presentation are courtesy of • Dr. Brad Bowling (Kanski’s Clinical Ophthalmology) • Dr. J. R. O. Collin (A Manual of Systematic Eyelid Surgery) 2
Learning Objectives • At the end of this class the students shall be able to : • Understand the structure and function of the eyelids • Recognize common diseases of the eyelids • Comprehend the principles of managing eyelid diseases 3
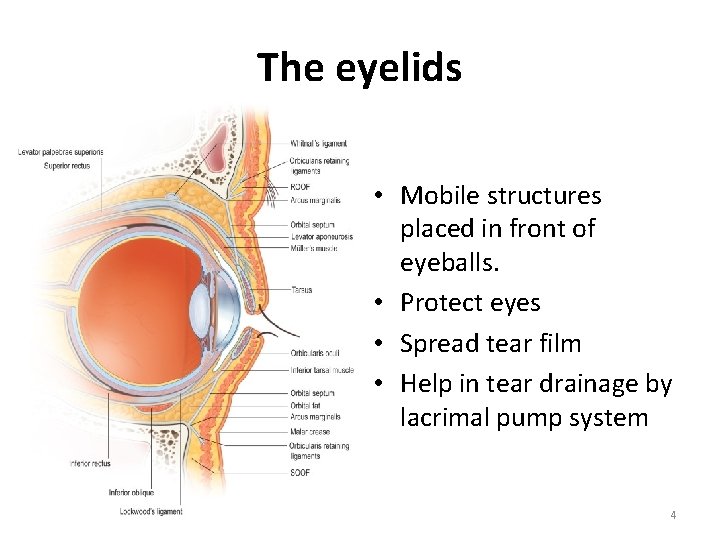
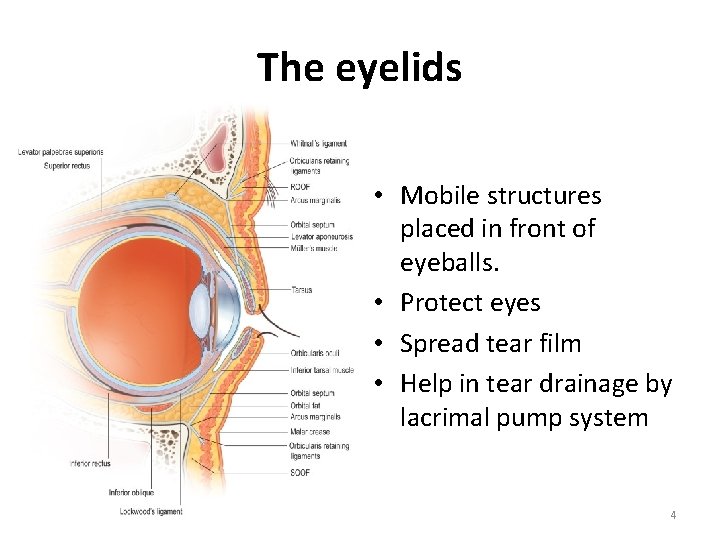
The eyelids • Mobile structures placed in front of eyeballs. • Protect eyes • Spread tear film • Help in tear drainage by lacrimal pump system 4
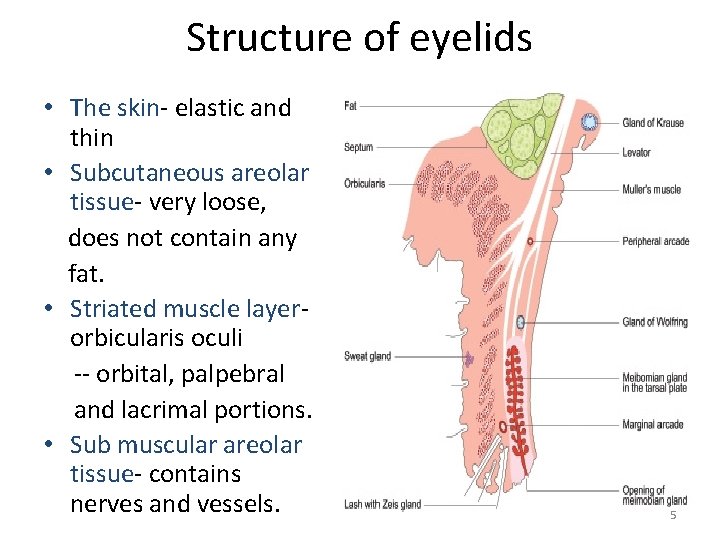
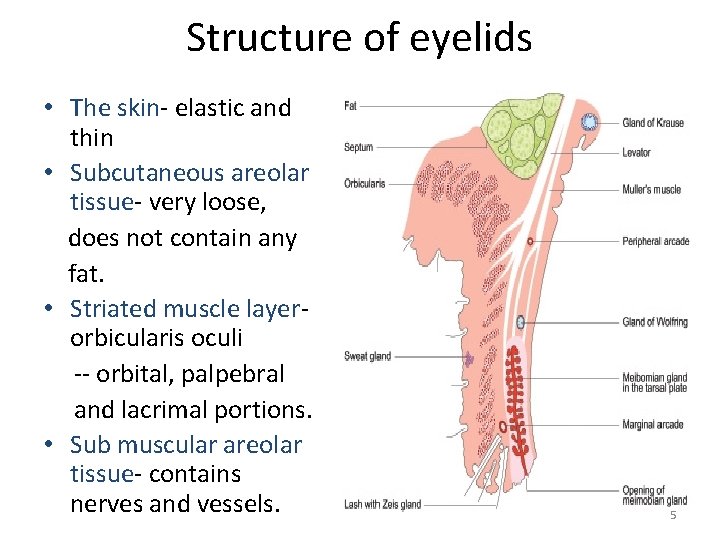
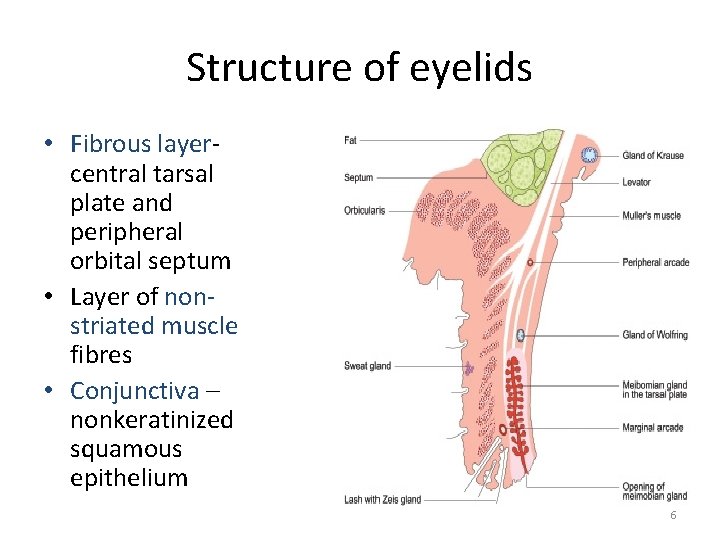
Structure of eyelids • The skin- elastic and thin • Subcutaneous areolar tissue- very loose, does not contain any fat. • Striated muscle layerorbicularis oculi -- orbital, palpebral and lacrimal portions. • Sub muscular areolar tissue- contains nerves and vessels. 5
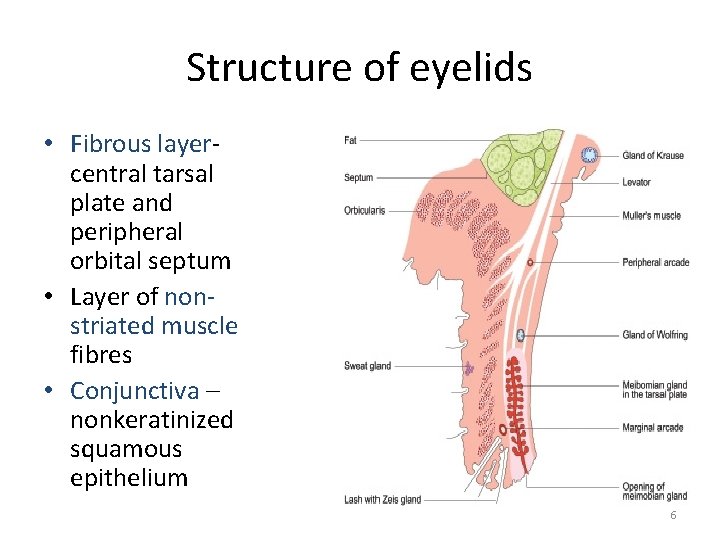
Structure of eyelids • Fibrous layercentral tarsal plate and peripheral orbital septum • Layer of nonstriated muscle fibres • Conjunctiva – nonkeratinized squamous epithelium 6
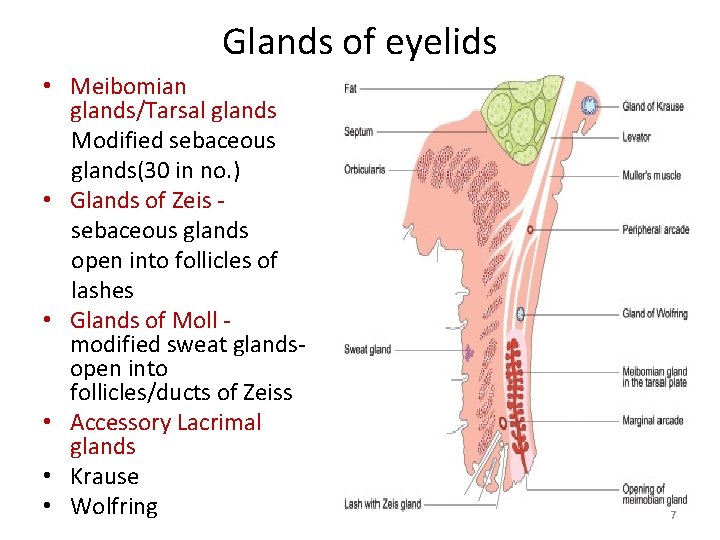
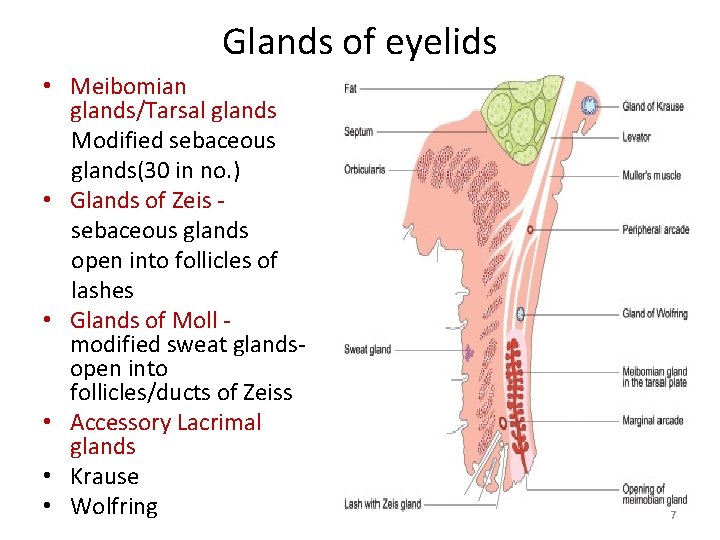
Glands of eyelids • Meibomian glands/Tarsal glands Modified sebaceous glands(30 in no. ) • Glands of Zeis sebaceous glands open into follicles of lashes • Glands of Moll modified sweat glandsopen into follicles/ducts of Zeiss • Accessory Lacrimal glands • Krause • Wolfring 7
Edema of lids • Inflammatory edema Dermatitis, stye, insect bite • Passive edema Renal disease, Cardiac failure, Cavernous sinus thrombosis 8

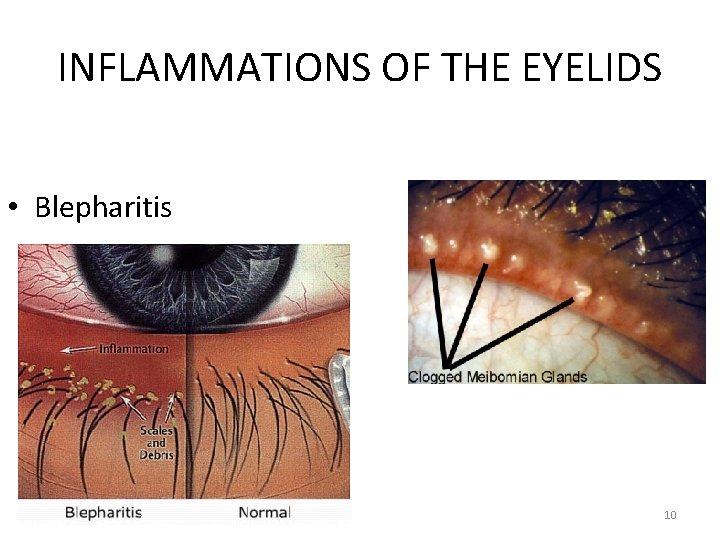
INFLAMMATIONS OF THE EYELIDS • Blepharitis Subacute or chronic lid margin inflammation 1. Anterior blepharitis. 2. Posterior blepharitis. 9
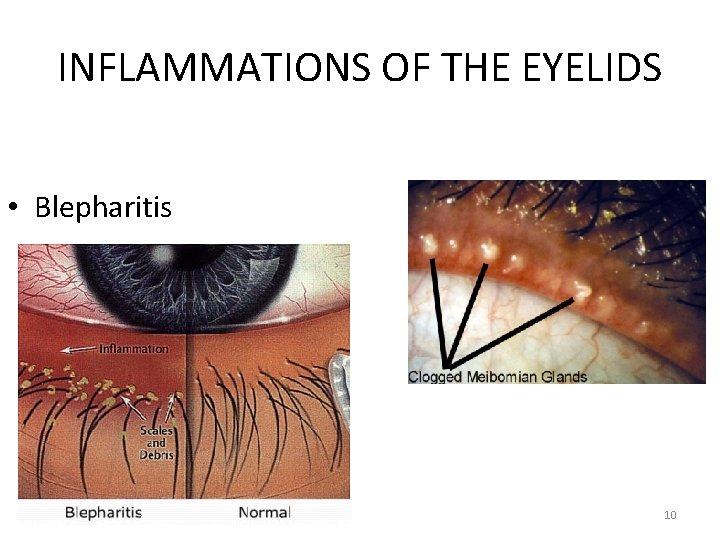
INFLAMMATIONS OF THE EYELIDS • Blepharitis 10
INFLAMMATIONS OF THE EYELIDS 1. Anterior blepharitis Squamous/Seborrhoeic White dandruff like scales on the lid margin among eyelashes • Ulcerative Chronic staphylococcal infection- hard crusts and ulcers Treatment Warm compresses Lid hygiene, cleaning with diluted baby shampoo Topical : antibiotic, steroids, tear substitutes Oral : Azithromycin 500 mg OD for 3 days. • 11
INFLAMMATIONS OF THE EYELIDS • Posterior blepharitis Meibomian seborrhoea Meibomianitis Treatment: Warm compress, lid hygiene & massage. Oral doxycycline/erythromycin for 6 wks. 12
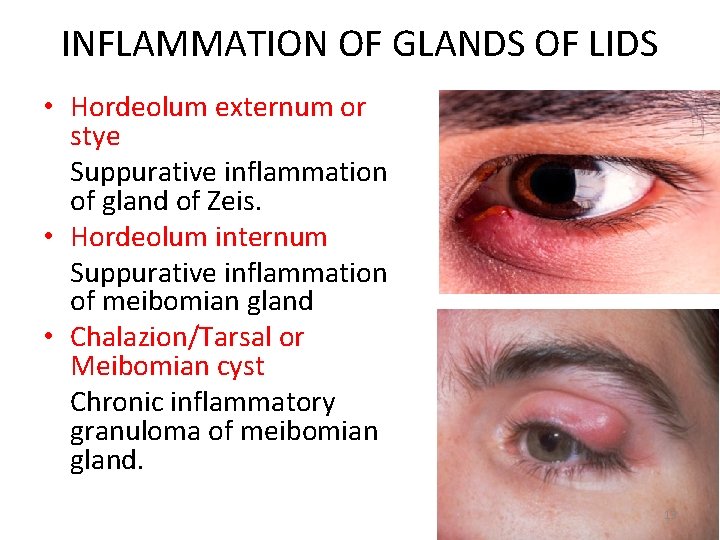
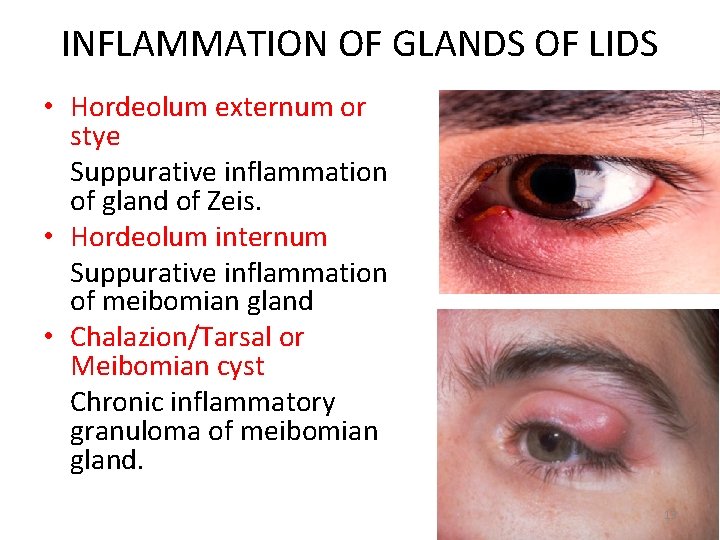
INFLAMMATION OF GLANDS OF LIDS • Hordeolum externum or stye Suppurative inflammation of gland of Zeis. • Hordeolum internum Suppurative inflammation of meibomian gland • Chalazion/Tarsal or Meibomian cyst Chronic inflammatory granuloma of meibomian gland. 13
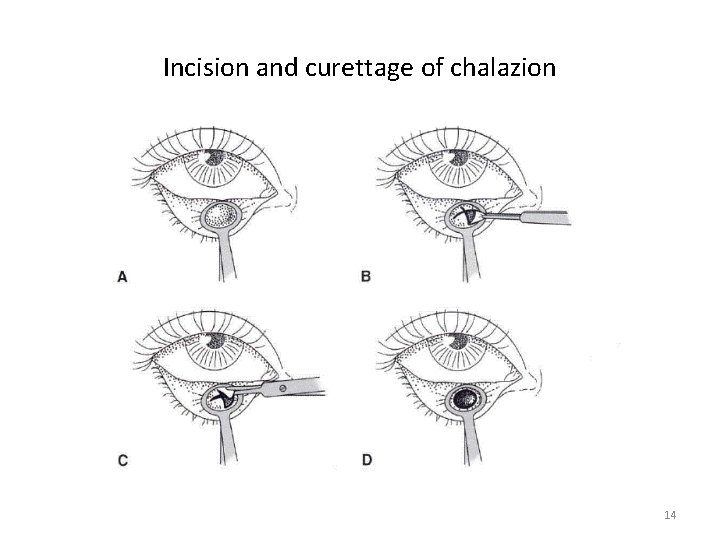
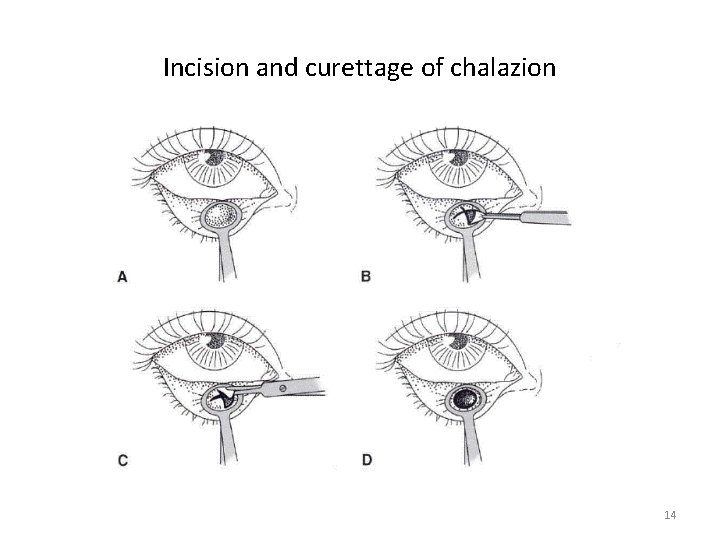
Incision and curettage of chalazion 14
ANOMALIES IN POSITION OF LASHES AND LIDS • • • Blepharospasm Trichiasis Entropion Ectropion Symblepharon Ankyloblepharon Blepharophimosis Lagophthalmos Blepharoptosis 15

• Blepharospasm Involuntary, sustained and forcible closure of lids. Essential blepharospasm-Rare, idiopathic. Treatment: Botulinum toxin Facial denervation Reflex blepharospasm- Vth nerve reflex Sensory stimulation Treatment: of causative disease(Eg. corneal ulcer) 16
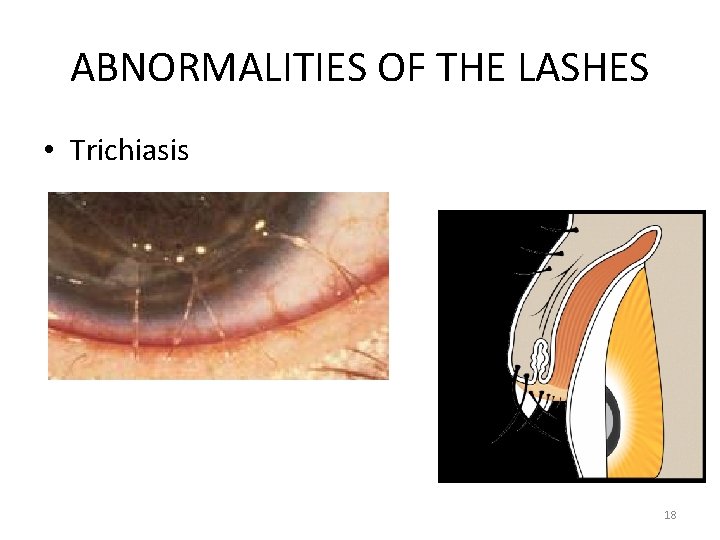
• Trichiasis Misdirection of cilia, directed backwards to rub cornea. Causes: Trachoma, blepharitis, scars, chemical burns, Steven-Johnson syndrome. Treatment: Epilation Electrolysis Cryosurgery Argon laser application 17
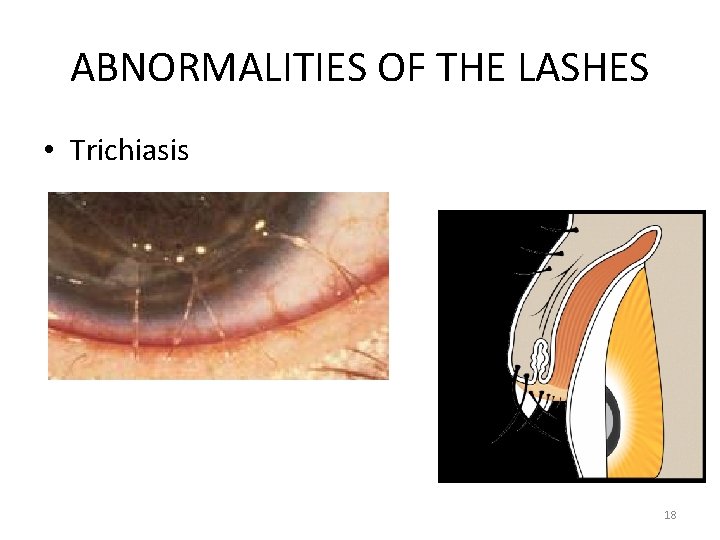
ABNORMALITIES OF THE LASHES • Trichiasis 18
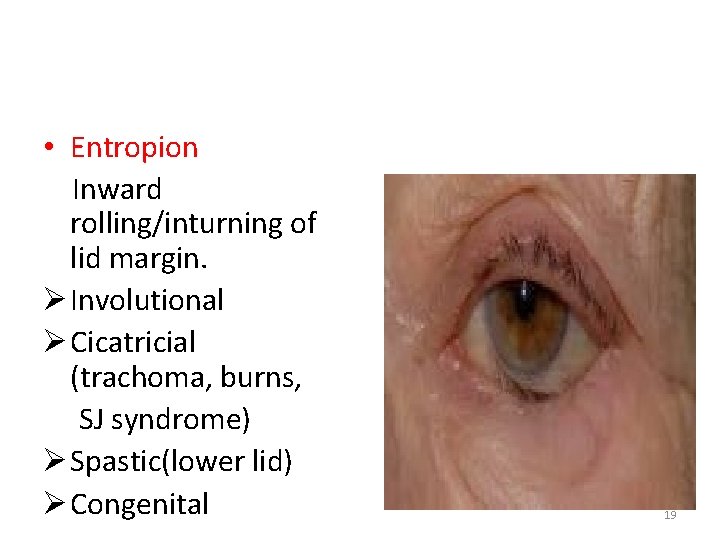
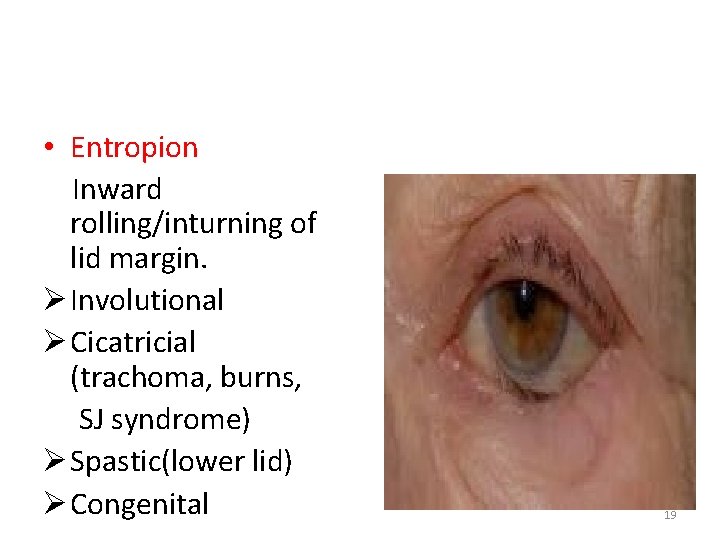
• Entropion Inward rolling/inturning of lid margin. Ø Involutional Ø Cicatricial (trachoma, burns, SJ syndrome) Ø Spastic(lower lid) Ø Congenital 19
• Involutional Entropion (age related) v Horizontal lid laxity v Vertical lid instability v Over-riding of pretarsal plate v Orbital septum laxity 20

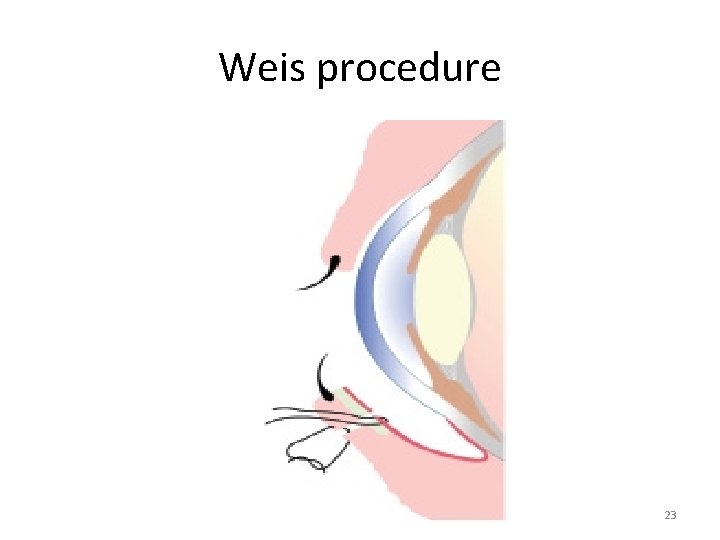
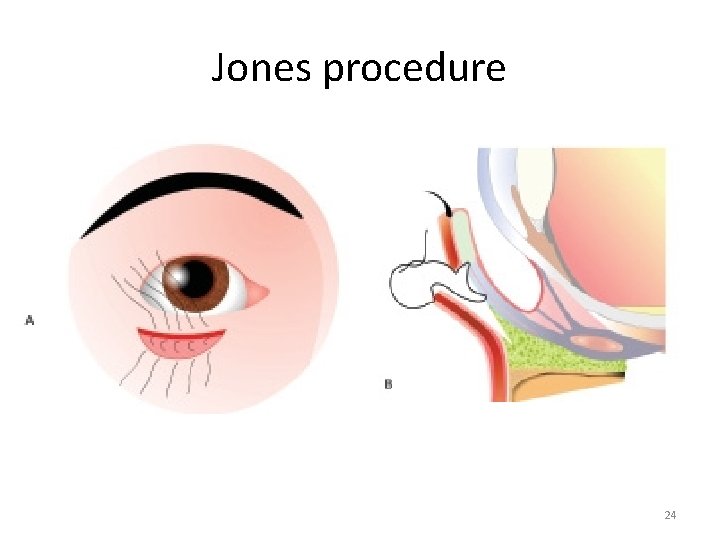
Surgical procedures for entropion • Transverse everting sutures (Quickert) • Transverse blepharotomy with everting sutures- Weis procedure • Jones procedure- tucking of inferior lid retractors (recurrences) 21

Transverse everting sutures 22
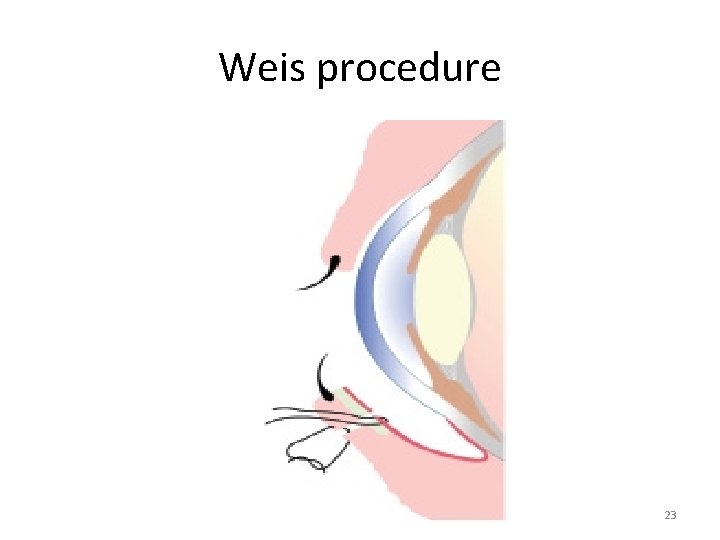
Weis procedure 23
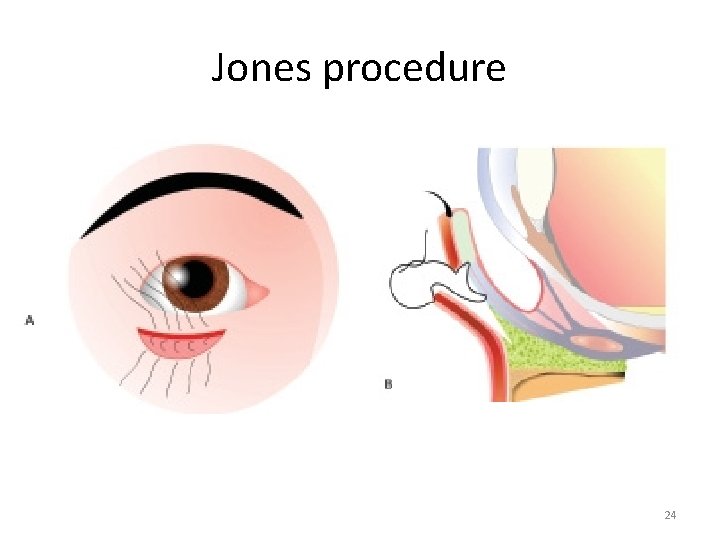
Jones procedure 24
• Cicatricial entropion Due to conjunctival scarring Causes: Trachoma, chemical burns Treatment : Tarsal fracture/ wedge resection 25

Tarsal Fracture 26
ECTROPION • Eversion of lid margins and lashes away from the globe. Ø Acquired – Involutional/senile-lower lid Cicatricial- burns and injuries Paralytic- 7 th nerve paralysis Mechanical-tumors/proptosis Ø Congenital 27

ECTROPION 28
• Involutional Ectropion (Age Related) Ø Horizontal lid laxity Ø Medial canthal tendon laxity Ø Lateral canthal tendon laxity Ø Disinsertion of lower lid retractors 29
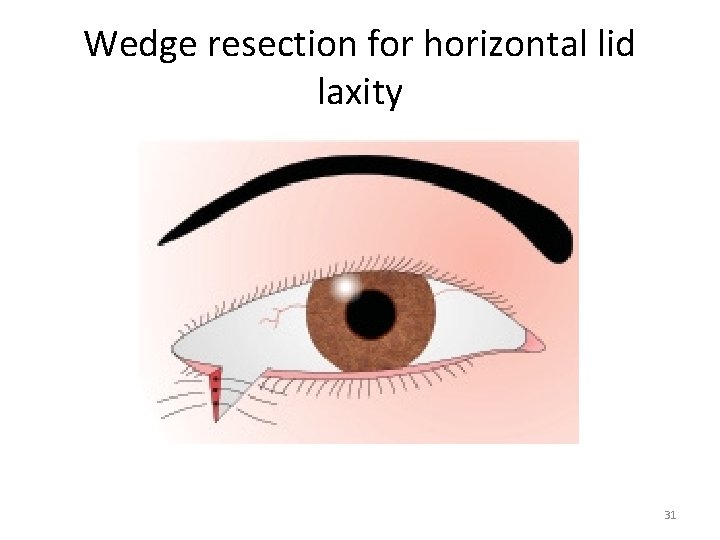
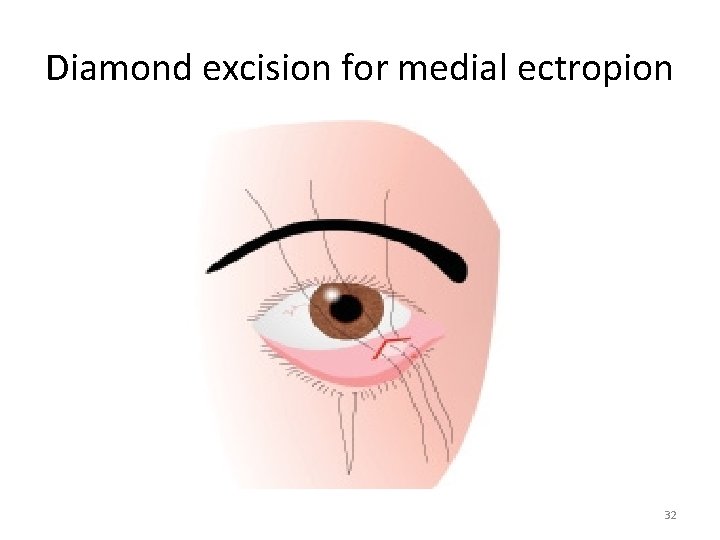
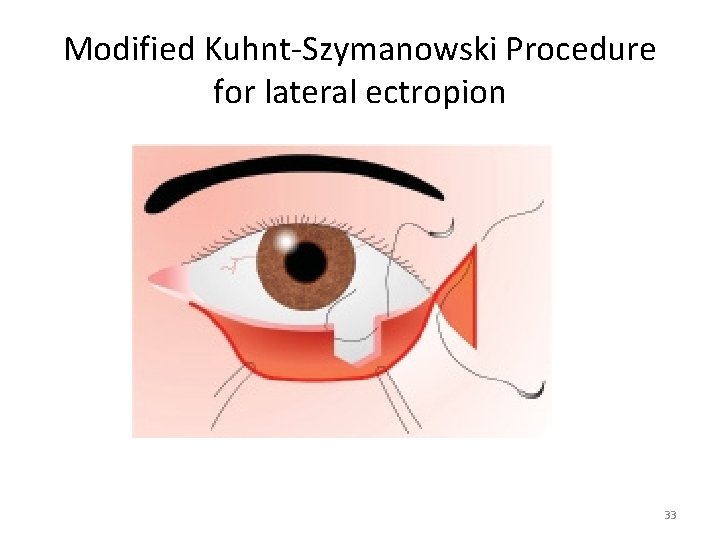
• Treatment Ø Wedge resection for horizontal lid laxity Ø Diamond excision for medial ectropion Ø Kuhnt-Szymanowski Procedure modified by Byron Smith for lateral ectropion 30
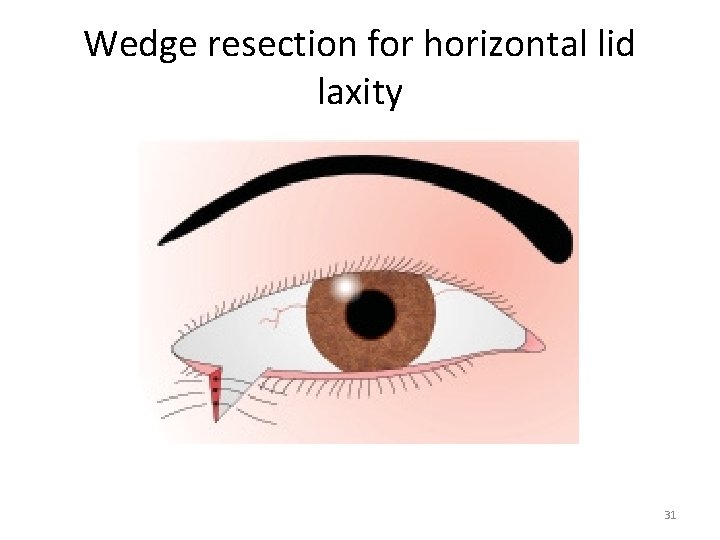
Wedge resection for horizontal lid laxity 31
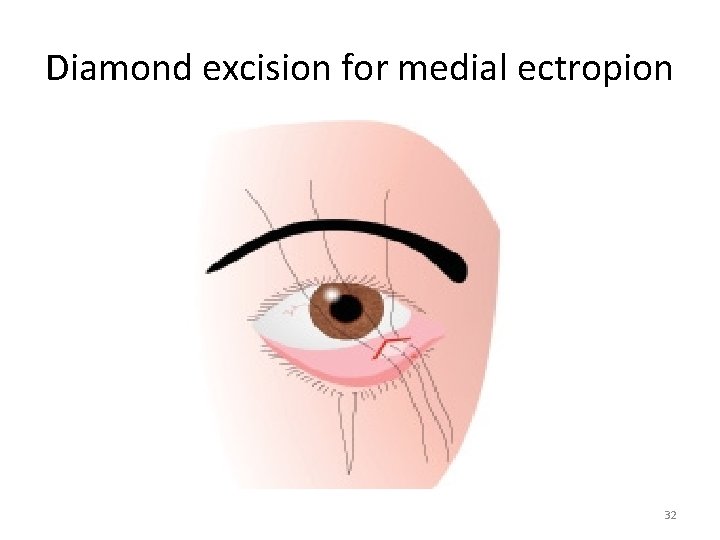
Diamond excision for medial ectropion 32
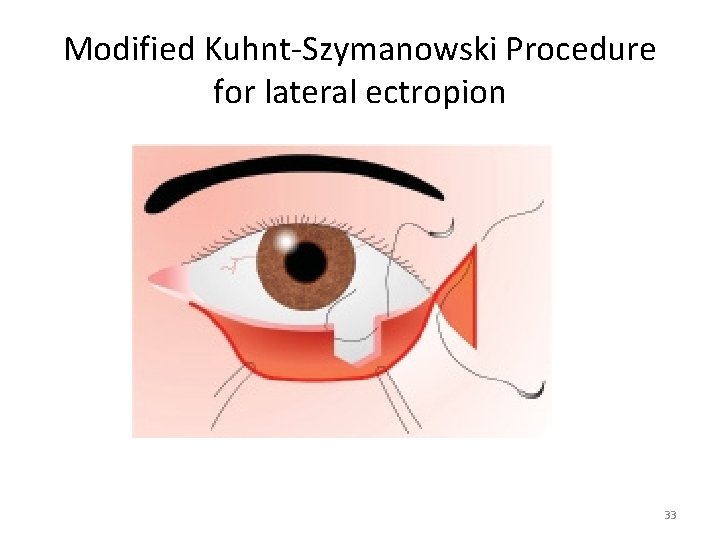
Modified Kuhnt-Szymanowski Procedure for lateral ectropion 33

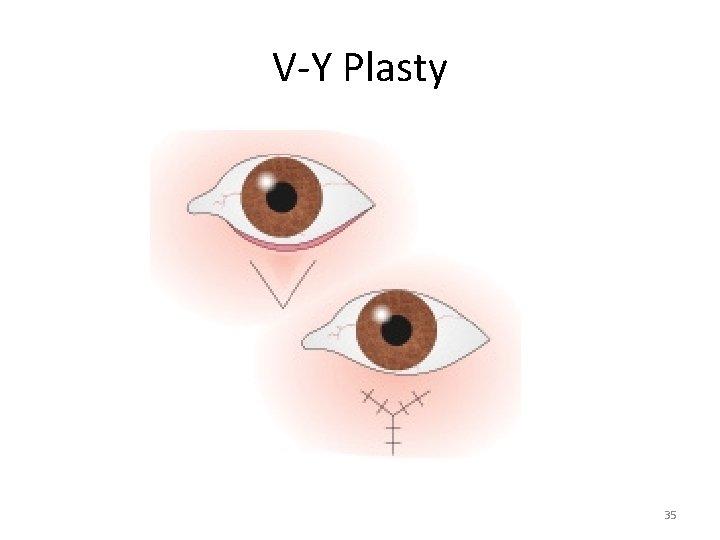
• Cicatricial Ectropion Due to burn, trauma, chronic inflammation of skin or surgical scarring. Treated with Z/ V-Y Plasty or skin grafts. 34
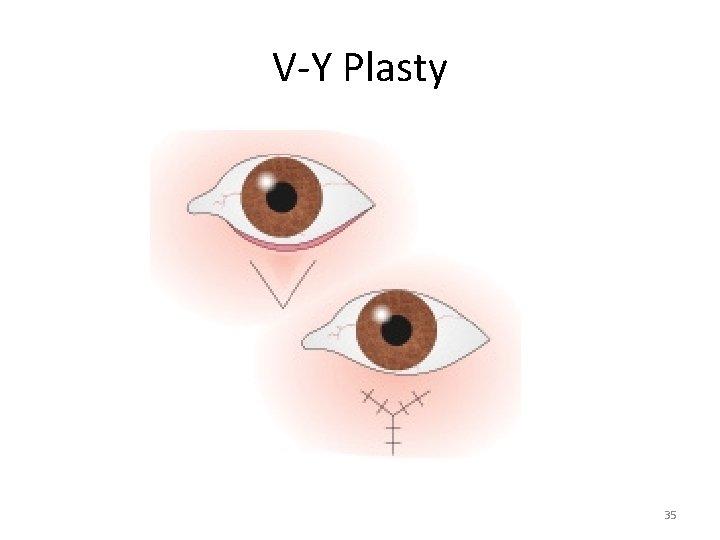
V-Y Plasty 35
• Paralytic Ectropion Due to Facial nerve palsy Treated by: Tarsorrhaphy Medial canthoplasty Lateral canthal sling Upper lid lowering • Mechanical ectropion (tumours)- corrected by treating the underlying cause. 36
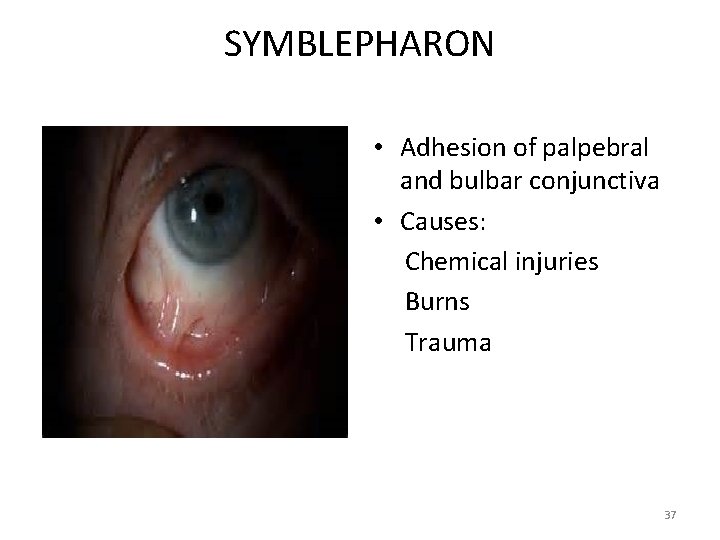
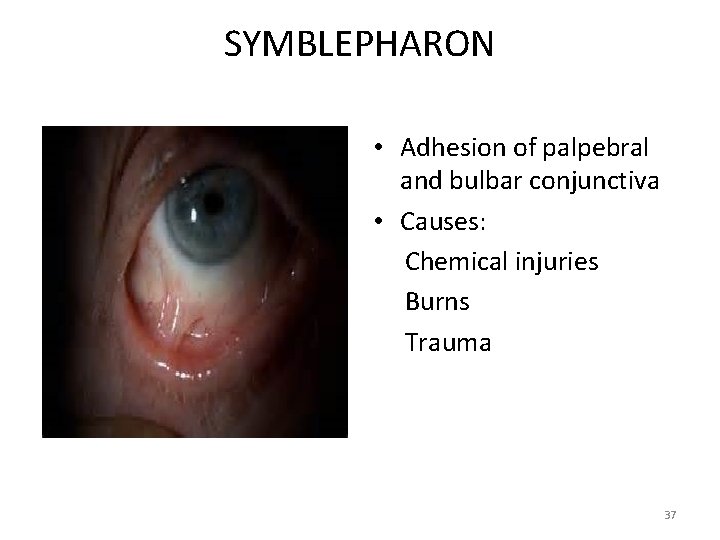
SYMBLEPHARON • Adhesion of palpebral and bulbar conjunctiva • Causes: Chemical injuries Burns Trauma 37
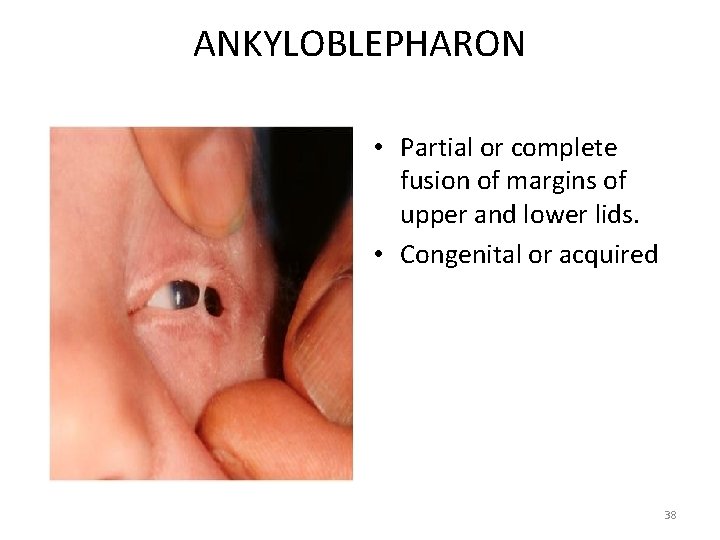
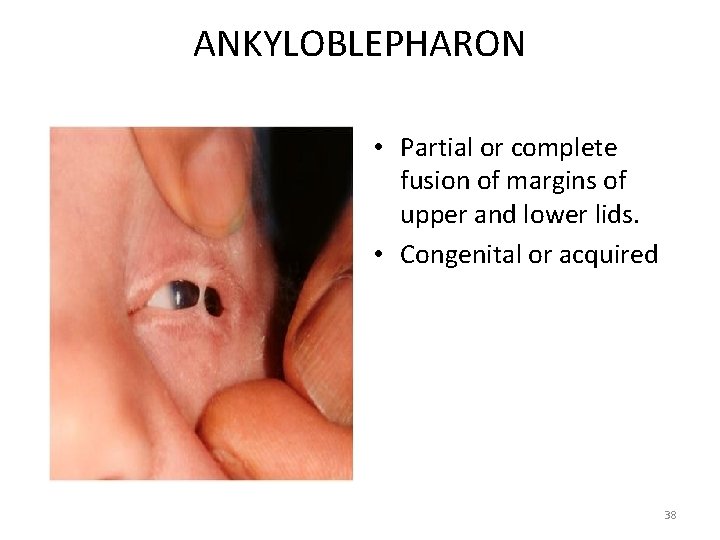
ANKYLOBLEPHARON • Partial or complete fusion of margins of upper and lower lids. • Congenital or acquired 38
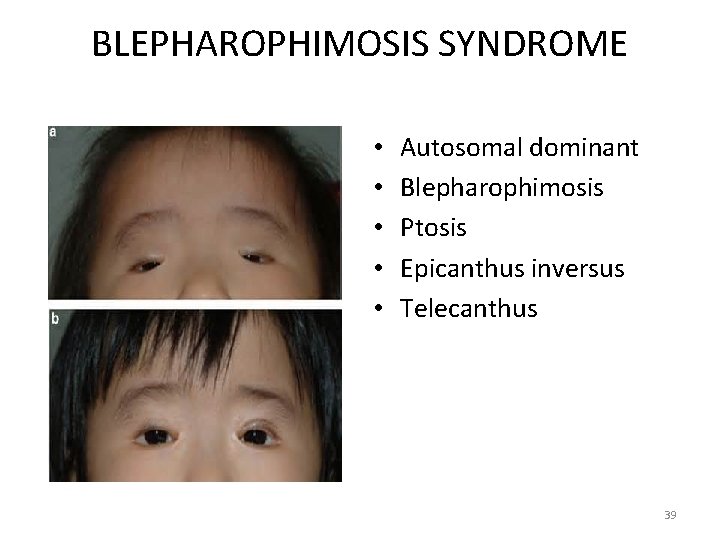
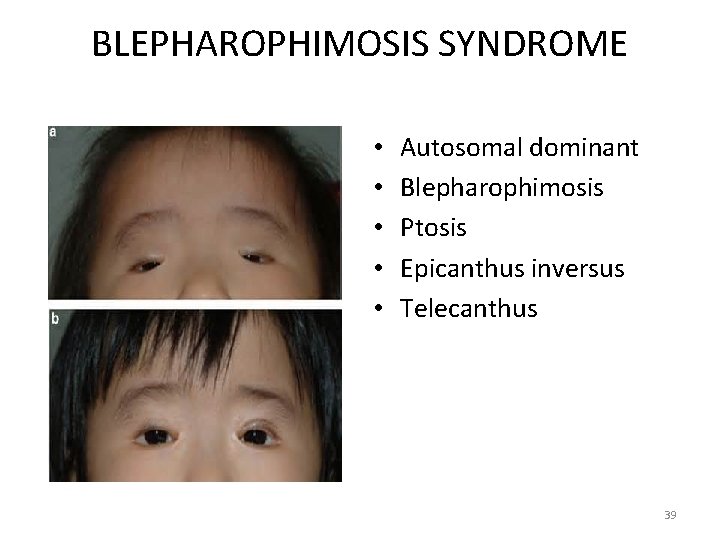
BLEPHAROPHIMOSIS SYNDROME • • • Autosomal dominant Blepharophimosis Ptosis Epicanthus inversus Telecanthus 39

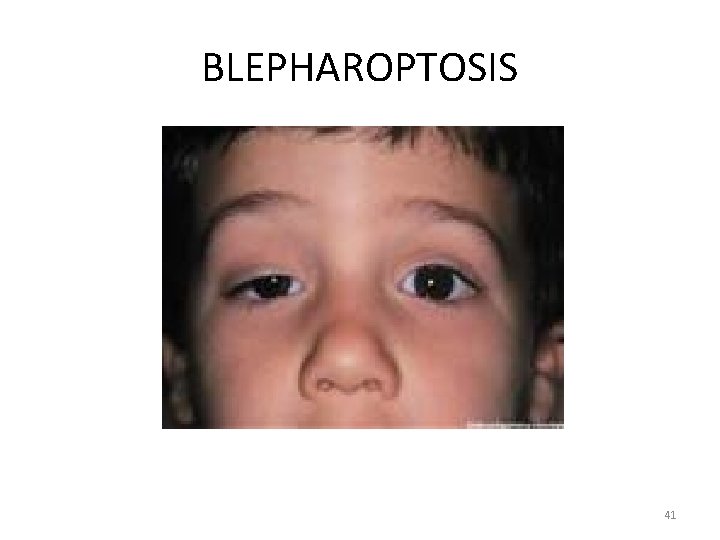
BLEPHAROPTOSIS • Abnormal drooping of the upper lid to a level that covers more than 2 mm of the superior cornea. 1. Congenital Simple Complicated 2. Acquired Neurogenic- 3 rd Nerve palsy, Horner’s syndrome Myogenic – Myasthenia , Myotonic dystrophy Aponeurotic- Involutional, postoperative Mechanical- lid tumors 40
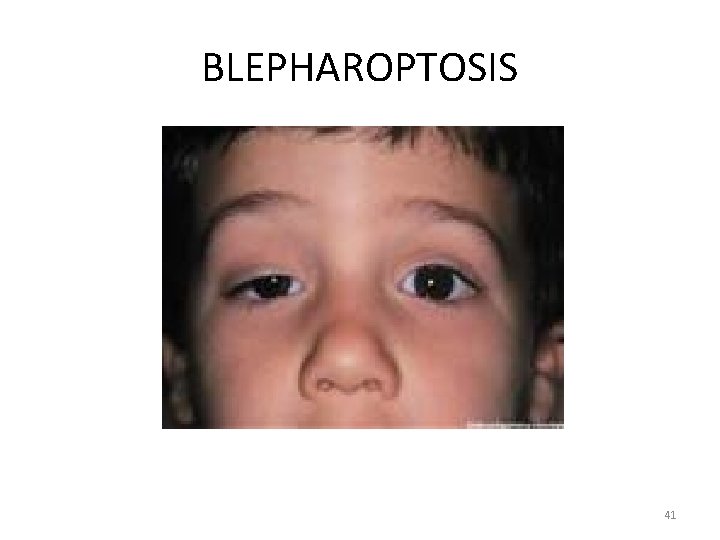
BLEPHAROPTOSIS 41
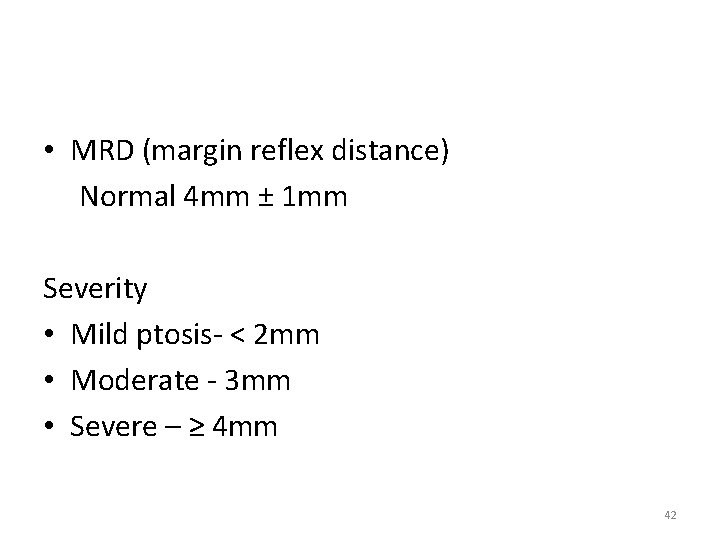
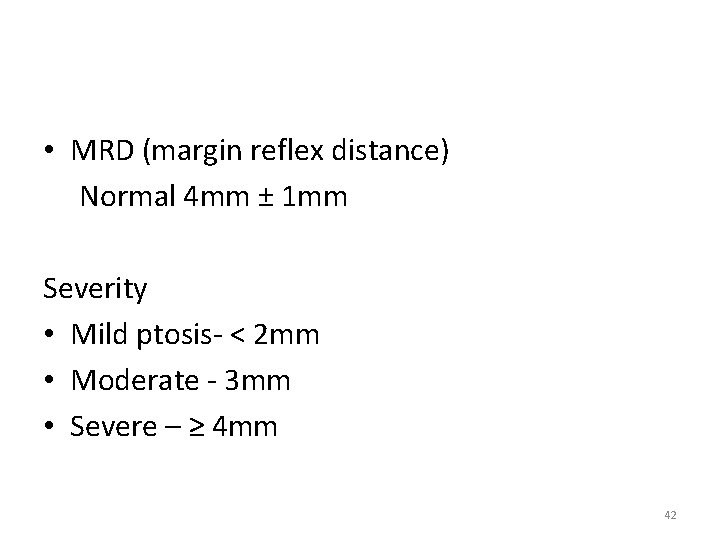
• MRD (margin reflex distance) Normal 4 mm ± 1 mm Severity • Mild ptosis- < 2 mm • Moderate - 3 mm • Severe – ≥ 4 mm 42

• Levator Palpebrae Superioris (LPS) Action Good > 8 mm Fair 5 -7 Poor ≤ 4 mm 43

SURGICAL TREATMENT • Fasanella-Servat operation LPS action good Mild ptosis < 2 mm Horner’s syndrome 44
SURGICAL TREATMENT • LPS Resection (Conjunctival approach) LPS action fair Any type of ptosis Moderate congenital or acquired ptosis 45

SURGICAL TREATMENT • LPS Resection (Skin approach) • Most preferred surgery for ptosis correction LPS action fair Any type of ptosis For larger resection in congenital or acquired ptosis. 46
SURGICAL TREATMENT • LPS Resection with aponeurotic reinsertion LPS action fair Any type of ptosis Acquired ptosis. 47

SURGICAL TREATMENT • Frontalis Sling surgery (Brow suspension) LPS action poor Ptosis >2 mm Congenital ptosis 48
NEOPLASMS OF LIDS • Benign lesions Ø Xanthelasma Ø Naevus or mole Ø Haemangioma Ø Neurofibromatosis 49
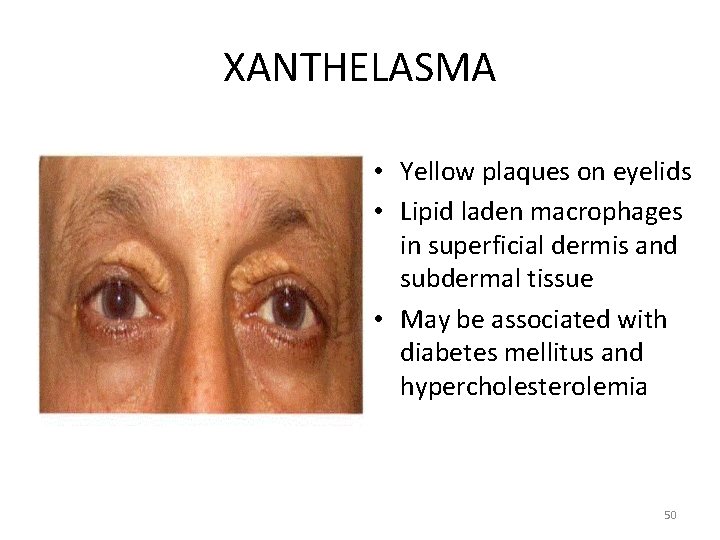
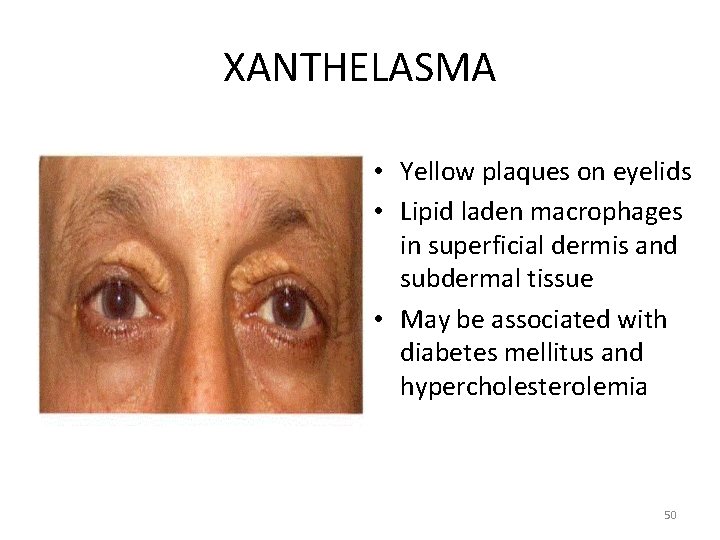
XANTHELASMA • Yellow plaques on eyelids • Lipid laden macrophages in superficial dermis and subdermal tissue • May be associated with diabetes mellitus and hypercholesterolemia 50
• Malignant tumours Ø Basal cell carcinoma Ø Squamous cell carcinoma Ø Sebaceous gland carcinoma Ø Malignant melanoma 51
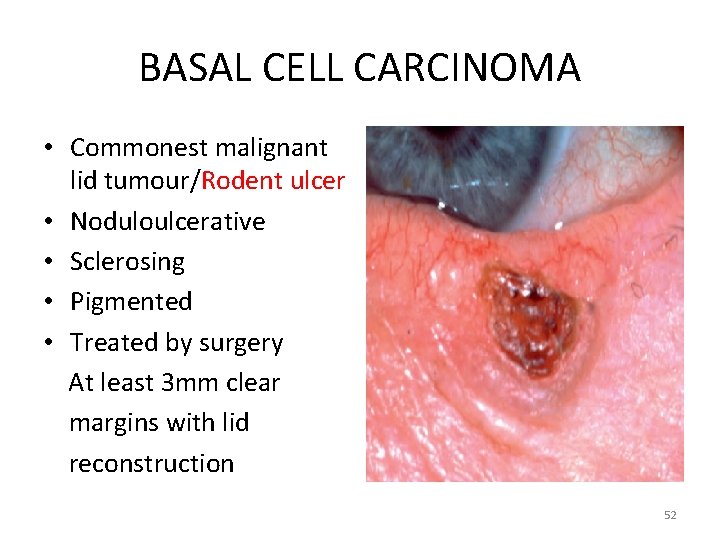
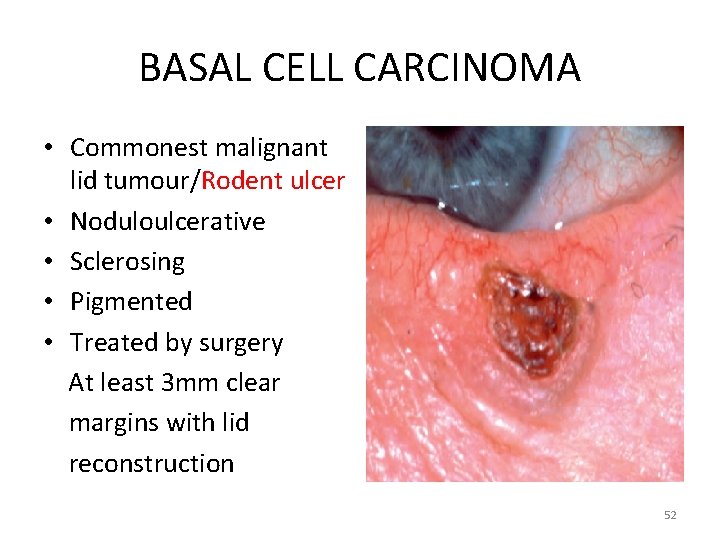
BASAL CELL CARCINOMA • Commonest malignant lid tumour/Rodent ulcer • Noduloulcerative • Sclerosing • Pigmented • Treated by surgery At least 3 mm clear margins with lid reconstruction 52
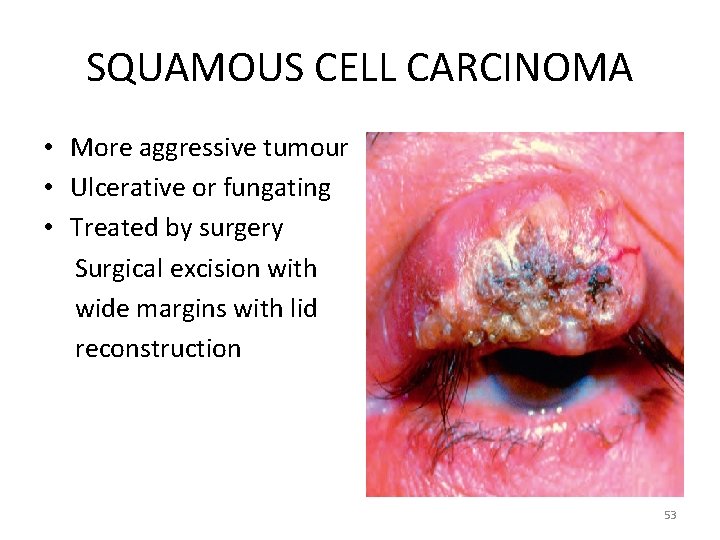
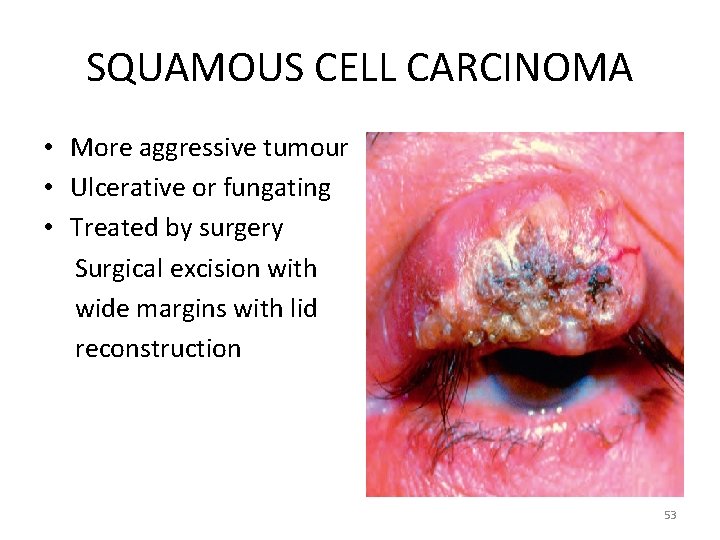
SQUAMOUS CELL CARCINOMA • More aggressive tumour • Ulcerative or fungating • Treated by surgery Surgical excision with wide margins with lid reconstruction 53
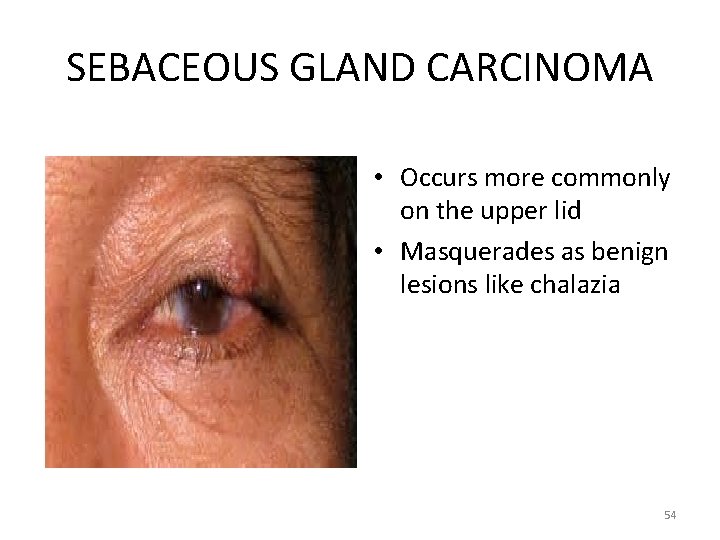
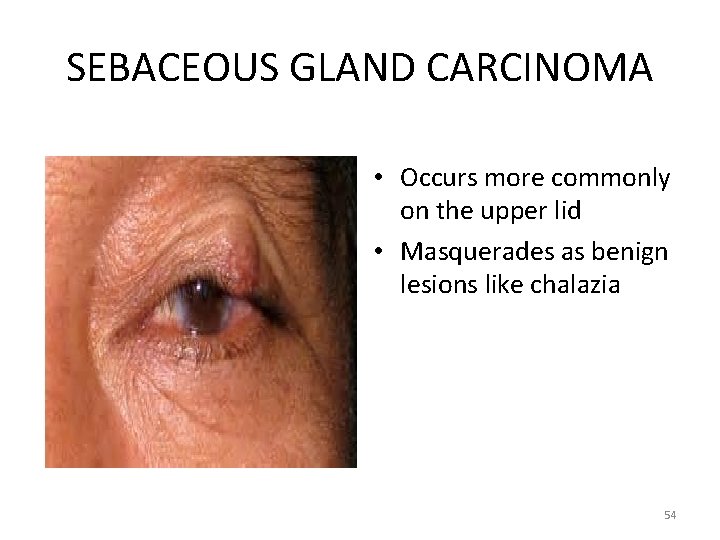
SEBACEOUS GLAND CARCINOMA • Occurs more commonly on the upper lid • Masquerades as benign lesions like chalazia 54
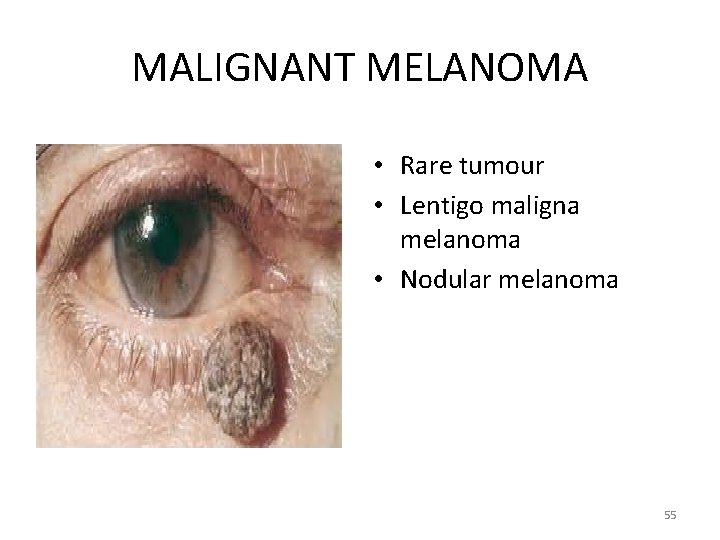
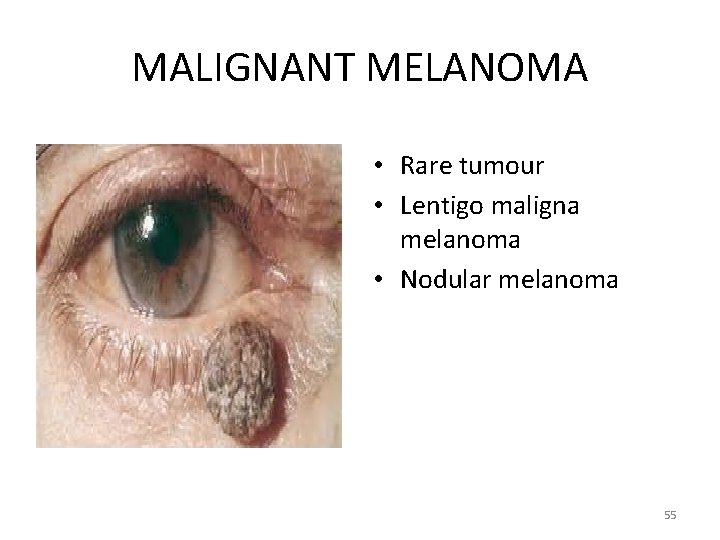
MALIGNANT MELANOMA • Rare tumour • Lentigo maligna melanoma • Nodular melanoma 55
Thank You 56
 Ajai nair
Ajai nair Promotion from assistant to associate professor
Promotion from assistant to associate professor Crown root ratio
Crown root ratio Shankarlal agrawal science college salekasa
Shankarlal agrawal science college salekasa Bio medical waste management introduction
Bio medical waste management introduction Divyakant agrawal
Divyakant agrawal Subodh agrawal
Subodh agrawal Ca rakesh agrawal
Ca rakesh agrawal Anoop agrawal
Anoop agrawal Shweta agarwal iit madras
Shweta agarwal iit madras Vishwani agrawal
Vishwani agrawal Asptro
Asptro Dr deepak agrawal
Dr deepak agrawal Dr raj agrawal
Dr raj agrawal Nikolay yakovets
Nikolay yakovets Agrawal-kayal-saxena
Agrawal-kayal-saxena Krati agrawal
Krati agrawal Lig lag
Lig lag U lid
U lid Large rectangular pan, often with a lid and a meat rack.
Large rectangular pan, often with a lid and a meat rack. Hashitoxicosis
Hashitoxicosis Trojí lid
Trojí lid Conjunctival injection
Conjunctival injection Dry eye symptoms
Dry eye symptoms Lid lag
Lid lag Ad lid
Ad lid Fuso horario linha internacional de data
Fuso horario linha internacional de data What is lever
What is lever Sql lid
Sql lid Feyza pelin haksever
Feyza pelin haksever Inclined plane wrapped around a pole
Inclined plane wrapped around a pole Standard data quality dimensions kpmg
Standard data quality dimensions kpmg Classification of simple machine
Classification of simple machine Hexaflexercise
Hexaflexercise Lid driven cavity
Lid driven cavity Screw examples
Screw examples Universal conditional statement examples
Universal conditional statement examples Existential universal statements examples
Existential universal statements examples Lid lag
Lid lag Lid care solüsyon
Lid care solüsyon Structuralism
Structuralism Flip your lid
Flip your lid What is some slang words
What is some slang words Additional aspects of aqueous equilibria
Additional aspects of aqueous equilibria Chapter 9 inventories additional valuation issues
Chapter 9 inventories additional valuation issues Additional features of er model ppt
Additional features of er model ppt Additional process
Additional process Additional topics in trigonometry
Additional topics in trigonometry Formula for surface area of pyramids
Formula for surface area of pyramids Volume of prism and cylinders worksheet
Volume of prism and cylinders worksheet Fire watchers are additional personnel
Fire watchers are additional personnel Askov in public health dentistry
Askov in public health dentistry 6-1 additional practice the polygon angle-sum theorems
6-1 additional practice the polygon angle-sum theorems 10-5 secant lines and segments
10-5 secant lines and segments Additional member system scotland
Additional member system scotland 5-3 additional vocabulary support bisectors in triangles
5-3 additional vocabulary support bisectors in triangles Pros of fptp
Pros of fptp