COVID 19 Interim Final Rule 4302020 Effective March




- Slides: 46
COVID 19 Interim Final Rule 4/30/2020 Effective March 1 st, 2020 Marion Salwin, CPC, COC, CRC, CPC I Director of Physician & Regulatory Compliance Amy Gendron, RHIT, CCS Director, Clinical and Regulatory Compliance Karen Miska, BS MT(ASCP) Revenue Excellence – Revenue Integrity Director
“We all have the capacity to be a superhero. In order to become one, you just have to find your unique power or ability and exploit it for the greater good. The cape and mask are optional accessories, but a kind heart is essential” Robert Clancy © 2019 Trinity Health 2
CMS Interim Final Rule CMS 5531, published 4/30/20 • The interim final rule can be viewed here: Medicare and Medicaid IFC: Additional Policy and Regulatory Revisions in Response to the COVID 19 Public Health Emergency (CMS 5531 IFC) (PDF) List of Hospital Outpatient Services and List of Partial Hospitalization Program Services Accompanying the 4/30/2020 IFC (ZIP) List of lab test codes for COVID 19, Influenza, RSV (PDF) • Information in the interim final rule and this summary are applicable for the duration of the PHE unless otherwise noted. • Information retroactive to March 1, 2020 unless otherwise noted © 2019 Trinity Health 3
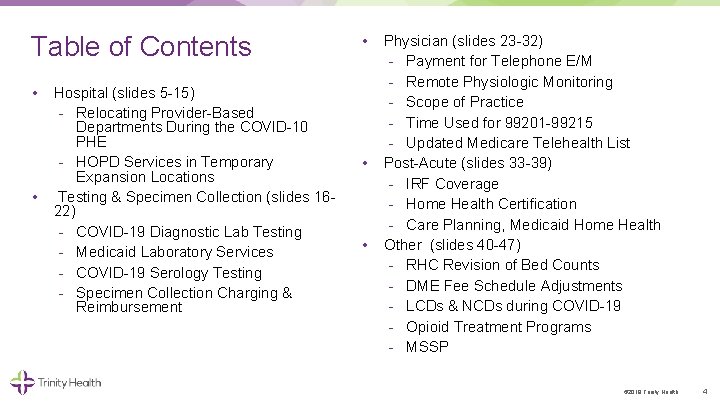
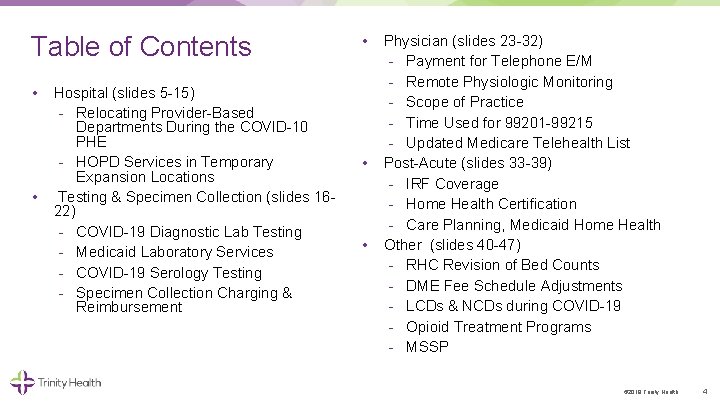
Table of Contents • • Hospital (slides 5 15) Relocating Provider Based Departments During the COVID 10 PHE HOPD Services in Temporary Expansion Locations Testing & Specimen Collection (slides 16 22) COVID 19 Diagnostic Lab Testing Medicaid Laboratory Services COVID 19 Serology Testing Specimen Collection Charging & Reimbursement • • • Physician (slides 23 32) Payment for Telephone E/M Remote Physiologic Monitoring Scope of Practice Time Used for 99201 99215 Updated Medicare Telehealth List Post Acute (slides 33 39) IRF Coverage Home Health Certification Care Planning, Medicaid Home Health Other (slides 40 47) RHC Revision of Bed Counts DME Fee Schedule Adjustments LCDs & NCDs during COVID 19 Opioid Treatment Programs MSSP © 2019 Trinity Health 4

Hospital © 2019 Trinity Health 5
E. Treatment of Certain Relocating PBDs Under the PHE (pages 33 43) • Applies to on campus or excepted off campus provider based departments that relocate due to the PHE. CMS expanded the extraordinary circumstances relocation policy so these locations can retain OPPS payment rates • Non excepted locations (using PN modifier) can relocate and they remain non excepted so do not need to request relocation approval from RO • Can relocate a PBD into multiple locations, or, only relocate a portion of a PBD • Hospitals without Walls initiative allows for patient’s home to be considered a PBD for hospital outpatients • If relocated PBDs will be billed as the main hospital, no provider enrollment actions required • Need to submit exception request to the CMS Regional Office (RO) for on campus and excepted off campus expanded to temporary locations Can begin providing services at the new temporary locations before submitting request © 2019 Trinity Health 6
E. Treatment of Certain Relocating PBDs Under the PHE (pages 33 43) • • On-campus or excepted off-campus provider-based departments that relocate due to the PHE must submit exception request to RO by e-mail with 120 days of starting services. Request must include: Hospital CCN Address of current PBD location Address(es) of relocated PBD(s) Date began providing services at relocated PBD Brief justification for relocation and its impact on hospital’s response to COVID 19 including why new location is appropriate for furnishing covered services Attestation that relocation is not inconsistent with States emergency preparedness or pandemic plan Patient’s home can be considered a relocated off campus PBD. Only need to submit one request, not one for each patient’s home Use PO modifier for the relocated PBD if the expanded exception request process is completed and approved If request is not submitted or is denied the visits need to be billing with modifier PN, any previously paid must be rebilled © 2019 Trinity Health 7
F. Furnishing OP Services in Temporary Expansion Locations of Hospital (pages 43 60) • Services can be provided in expanded locations including the patient’s home as long as conditions of participation (that have not been waived) are met • CMS has grouped into three categories: Hospital outpatient therapy, education and training services that do not need to be in person Hosp services associated with a professional telehealth service In person services provided by hospital clinical staff • Need to be registered as hospital outpatient • Medical record documentation is required for reason and necessity of the visit/service • Orders for services still required © 2019 Trinity Health 8
F. Furnishing OP Services in Temporary Expansion Locations of Hospital (pages 43 60) Hospital OP Therapy, Education and Training Services • Examples include therapy, DSMT, MNT, psychotherapy • Services can be furnished through telecommunication Both audio and visual recommended but can be audio only if patient does not have visual capability • CMS has provided a list of examples, not all inclusive • Bill as if furnished in the hospital using existing CDMs • If these services were normally provided on-campus, bill these remote services with PO modifier and include condition code DR • PHP is covered on pages 48 53 © 2019 Trinity Health 9
F. Furnishing OP Services in Temporary Expansion Locations of Hospital (pages 43 60) Hosp services associated with a professional telehealth service (telephone only service codes 99441 99443 are being add to telehealth list) • Hospital services cover administrative and clinical support, labor, equipment, overhead, etc • If professional that normally practices in a PBD furnishes telehealth to a patient at home or other remote site, the hospital can bill the telehealth originating site facility fee, HCPCS Q 3014, which has a national payment rate of $26. 65 Normal OPPS PBD technical payment would be $116 • Bill with modifier PO or PN as usual for that clinic • Use condition code DR • May need CS modifier if the provider “visit” resulted in an order for the COVID 19 test or collection of the specimen © 2019 Trinity Health 10
F. Furnishing OP Services in Temporary Expansion Locations of Hospital (pages 43 60) In person clinical staff services • Services cannot be provided through telecommunication, hospital staff need to treat the patient in person • Examples include wound care, chemotherapy and other drug administration • Need to be careful of overlapping with HHA services • If patient under a home health plan of care, the hospital should only provide services that cannot be furnished by the HHA • Bill as if furnished in the hospital using existing CDMs • Use modifiers PO and PN as applicable; include condition code DR © 2019 Trinity Health 11
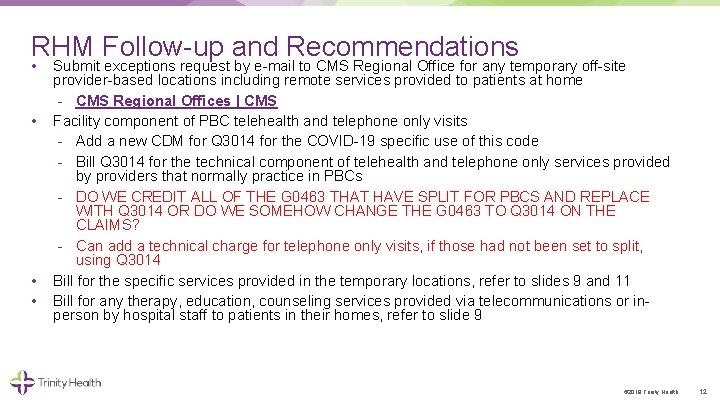
RHM Follow up and Recommendations • • Submit exceptions request by e mail to CMS Regional Office for any temporary off site provider based locations including remote services provided to patients at home CMS Regional Offices | CMS Facility component of PBC telehealth and telephone only visits Add a new CDM for Q 3014 for the COVID 19 specific use of this code Bill Q 3014 for the technical component of telehealth and telephone only services provided by providers that normally practice in PBCs DO WE CREDIT ALL OF THE G 0463 THAT HAVE SPLIT FOR PBCS AND REPLACE WITH Q 3014 OR DO WE SOMEHOW CHANGE THE G 0463 TO Q 3014 ON THE CLAIMS? Can add a technical charge for telephone only visits, if those had not been set to split, using Q 3014 Bill for the specific services provided in the temporary locations, refer to slides 9 and 11 Bill for any therapy, education, counseling services provided via telecommunications or in person by hospital staff to patients in their homes, refer to slide 9 © 2019 Trinity Health 12
Placeholder for RO request language © 2019 Trinity Health 13
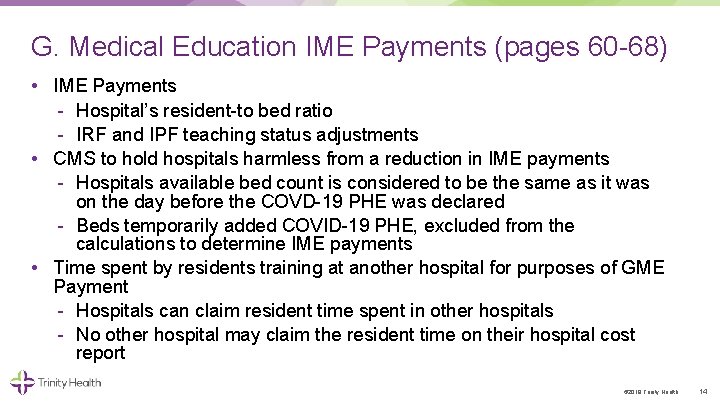
G. Medical Education IME Payments (pages 60 68) • IME Payments Hospital’s resident to bed ratio IRF and IPF teaching status adjustments • CMS to hold hospitals harmless from a reduction in IME payments Hospitals available bed count is considered to be the same as it was on the day before the COVD 19 PHE was declared Beds temporarily added COVID 19 PHE, excluded from the calculations to determine IME payments • Time spent by residents training at another hospital for purposes of GME Payment Hospitals can claim resident time spent in other hospitals No other hospital may claim the resident time on their hospital cost report © 2019 Trinity Health 14
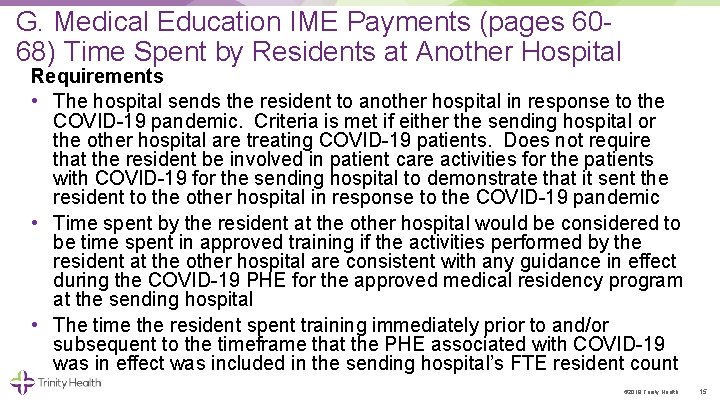
G. Medical Education IME Payments (pages 60 68) Time Spent by Residents at Another Hospital Requirements • The hospital sends the resident to another hospital in response to the COVID 19 pandemic. Criteria is met if either the sending hospital or the other hospital are treating COVID 19 patients. Does not require that the resident be involved in patient care activities for the patients with COVID 19 for the sending hospital to demonstrate that it sent the resident to the other hospital in response to the COVID 19 pandemic • Time spent by the resident at the other hospital would be considered to be time spent in approved training if the activities performed by the resident at the other hospital are consistent with any guidance in effect during the COVID 19 PHE for the approved medical residency program at the sending hospital • The time the resident spent training immediately prior to and/or subsequent to the timeframe that the PHE associated with COVID 19 was in effect was included in the sending hospital’s FTE resident count © 2019 Trinity Health 15
U. Hospital VBP Extraordinary Circumstance Exception Policy (pages 164 168) • CMS will be able to grant exceptions for impacted regions rather than each hospital submitting ECE request This aligns the VBP ECE with other quality reporting programs • Not required to report NHSN HAI measures and HCAHPS survey data for calendar quarters: Q 4 2019, Q 1 2020 and Q 2 2020. Have option to submit all or part of this data • Exclude qualifying claims data from mortality, complications and Medicare Spending per Beneficiary measures of calendar quarters: Q 1 2020 and Q 2 2020 © 2019 Trinity Health 16
COVID 19 Testing and Specimen Collection © 2019 Trinity Health 17
C. Modified Requirements for Ordering COVID 19 Tests (pages 27 31) • CMS wants to remove testing barrier of obtaining an order • COVID 19 testing can be ordered by any healthcare professional authorized under state law • COVID-19 testing can be performed without an order If no order, Lab/Hospital needs to notify patient of results • CMS did not provide any ICD 10 coding guidance for the tests performed without orders, Trinity Health’s guidance would be Z 11. 59 • If there is an order, physician’s NPI should be used for billing • If there is no provider order, the hospital’s NPI should be used for billing • Removing same requirement for Flu and RSV testing if they need to be ruled out • CMS provided a list of impacted codes that do not need an order © 2019 Trinity Health 18
V. COVID 19 Serology Testing (pages 168 170) • On an interim basis, CMS will cover COVID 19 serology testing performed through FDA authorized tests • Bill only once per sample, cannot bill additionally for confirmatory or repeat tests • CMS does not indicate any specific coding or payment amounts. • AMA has created two COVID 19 serology (antibody) testing codes: 86328 and 86769 © 2019 Trinity Health 19
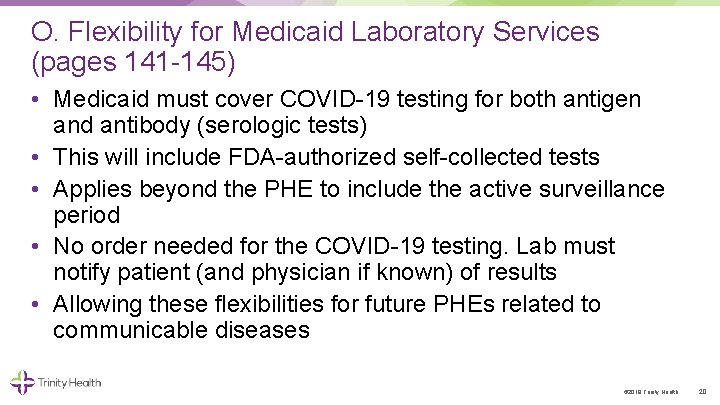
O. Flexibility for Medicaid Laboratory Services (pages 141 145) • Medicaid must cover COVID 19 testing for both antigen and antibody (serologic tests) • This will include FDA authorized self collected tests • Applies beyond the PHE to include the active surveillance period • No order needed for the COVID 19 testing. Lab must notify patient (and physician if known) of results • Allowing these flexibilities for future PHEs related to communicable diseases © 2019 Trinity Health 20
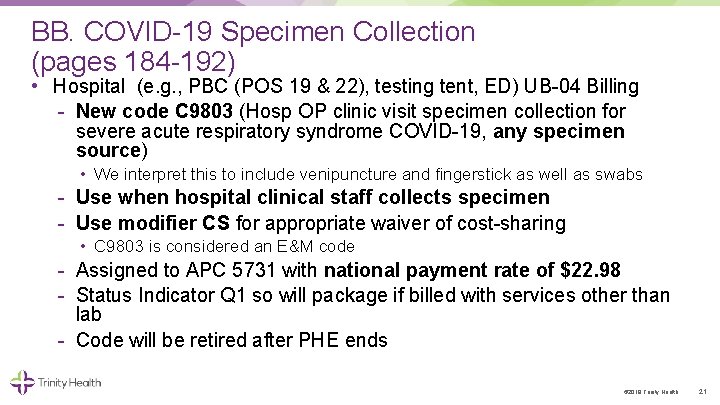
BB. COVID 19 Specimen Collection (pages 184 192) • Hospital (e. g. , PBC (POS 19 & 22), testing tent, ED) UB 04 Billing New code C 9803 (Hosp OP clinic visit specimen collection for severe acute respiratory syndrome COVID 19, any specimen source) • We interpret this to include venipuncture and fingerstick as well as swabs Use when hospital clinical staff collects specimen Use modifier CS for appropriate waiver of cost sharing • C 9803 is considered an E&M code Assigned to APC 5731 with national payment rate of $22. 98 Status Indicator Q 1 so will package if billed with services other than lab Code will be retired after PHE ends © 2019 Trinity Health 21
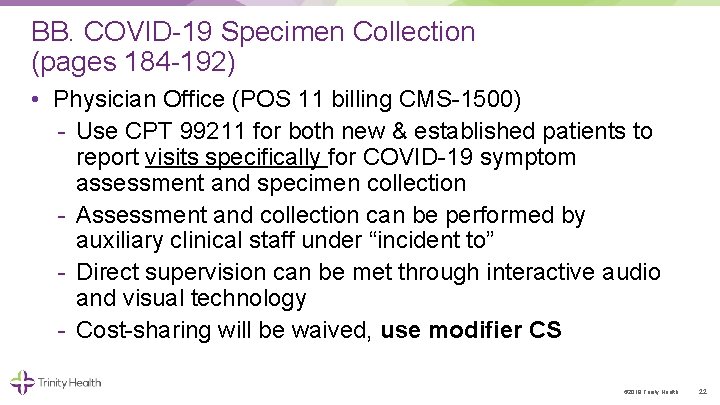
BB. COVID 19 Specimen Collection (pages 184 192) • Physician Office (POS 11 billing CMS 1500) Use CPT 99211 for both new & established patients to report visits specifically for COVID 19 symptom assessment and specimen collection Assessment and collection can be performed by auxiliary clinical staff under “incident to” Direct supervision can be met through interactive audio and visual technology Cost sharing will be waived, use modifier CS © 2019 Trinity Health 22
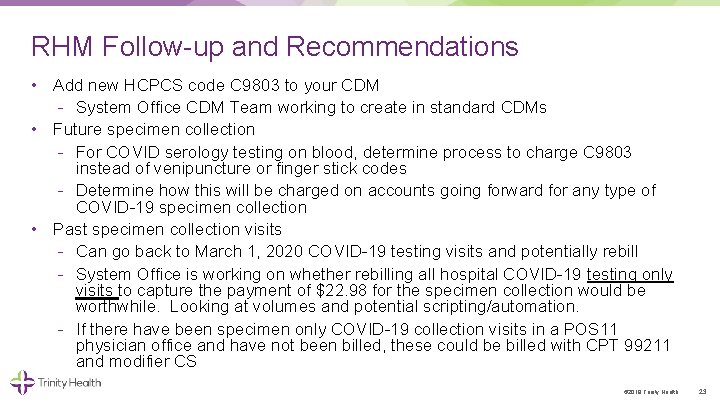
RHM Follow up and Recommendations • Add new HCPCS code C 9803 to your CDM System Office CDM Team working to create in standard CDMs • Future specimen collection For COVID serology testing on blood, determine process to charge C 9803 instead of venipuncture or finger stick codes Determine how this will be charged on accounts going forward for any type of COVID 19 specimen collection • Past specimen collection visits Can go back to March 1, 2020 COVID 19 testing visits and potentially rebill System Office is working on whether rebilling all hospital COVID 19 testing only visits to capture the payment of $22. 98 for the specimen collection would be worthwhile. Looking at volumes and potential scripting/automation. If there have been specimen only COVID 19 collection visits in a POS 11 physician office and have not been billed, these could be billed with CPT 99211 and modifier CS © 2019 Trinity Health 23

Physician © 2019 Trinity Health 24
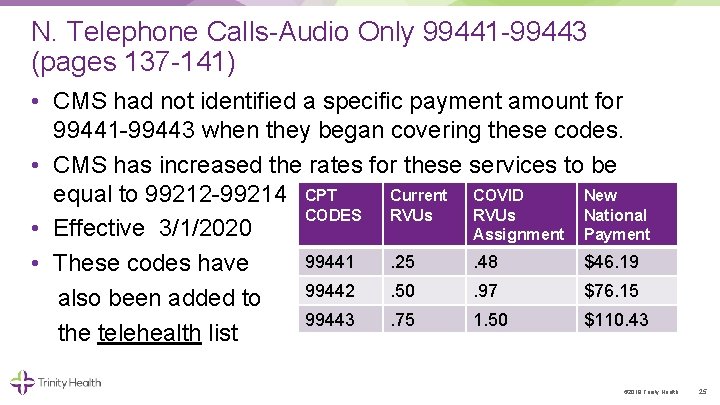
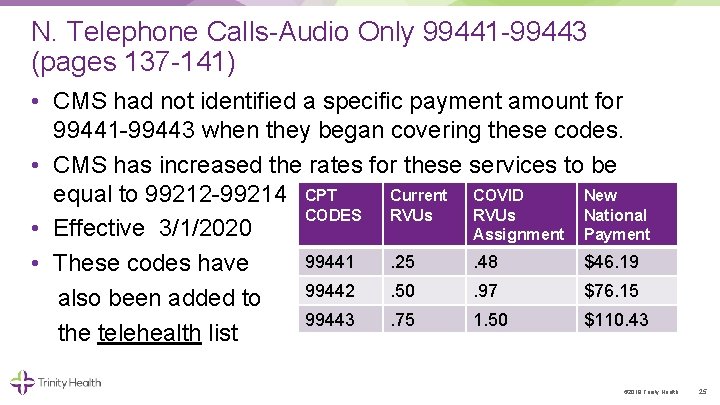
N. Telephone Calls Audio Only 99441 99443 (pages 137 141) • CMS had not identified a specific payment amount for 99441 99443 when they began covering these codes. • CMS has increased the rates for these services to be Current COVID New equal to 99212 99214 CPT CODES RVUs National • Effective 3/1/2020 Assignment Payment 99441. 25. 48 $46. 19 • These codes have 99442. 50. 97 $76. 15 also been added to 99443. 75 1. 50 $110. 43 the telehealth list © 2019 Trinity Health 25
CC. Remote Physiologic Monitoring (pages 192 194) • • RPM can be provided to new or established patients Codes: 99091, 99453, 99454, 99457, 99458, 99473, 99474 Consent can be obtained at the time of service This monitoring is helpful for COVID 19 related cases but may not be needed for the duration described by CPT codes • RPM has to be provided for at least 2 days but can be less than the 16 out of 30 days described in the CPT code All other code requirements must be met • Payment for this shorter monitoring period is restricted to patients with suspected or confirmed COVID-19 © 2019 Trinity Health 26
B. Scope of Practice (pages 19 27) Documentation • General Policy that allows for all members of the medical team to add documentation in the medical record Must be reviewed and verified (signed) by the appropriate clinician “Appropriate clinician” is defined as an individual who has the “delegated” benefit under Medicare law and is authorized to furnish and bill for professional services, regardless of acting in a teaching role, may review & verify (date and sign), rather than re document. © 2019 Trinity Health 27
Z. Medical Decision Making (MDM), Defined Time for E/M Services, 99201— 99215 (page 182) • In the March rule, CMS published different typical times for E/M services done via telehealth based on time • CMS now says that stakeholders told them that was too confusing • Use CPT times as defined in the CPT Manual 2020 © 2019 Trinity Health 28
AA. Updating the Telehealth List (pages 182 183) • CMS will continue to update the telehealth list through sub regulatory communication by posting updates at the following: https: //www. cms. gov/Medicare General Information/Telehealth Codes • The list was updated on April 30 th • The list includes expands the services that can be provided by audio only (if visual is not available) (identified in column D) © 2019 Trinity Health 29
B. Scope of Practice (pages 19 27) • Prior to the PHE, only physicians are permitted to supervise diagnostic tests • During the PHE, NPs, CNSs, PAs and CNMs may order, furnish directly and supervise the performance of diagnostic tests, as defined by state law • Allowing diagnostic tests to be performed by a PA without physician supervision, when authorized to perform the tests under state law © 2019 Trinity Health 30
B. Scope of Practice (pages 19 27) • Outpatient Physical Therapists & Occupational Therapists Applies only to those currently enrolled with Medicare and billing on a CMS 1500 claim form Allow PTs and OTs to delegate maintenance therapy services to PTAs and OTAs when they oversee the patients course of treatment, when clinically appropriate Utilize appropriate CO and CQ modifiers for therapy services provided by OTAs and PTAs © 2019 Trinity Health 31
B. Scope of Practice Pharmacists Providing Services Incident to a Physician’s Services (pages 19 27) • Clarification directed to pharmacist’s employed in a physician office and/or medical group. May provide services “incident to” to a physician, with appropriate level of supervision Services must not be paid under Medicare Part D benefit Within pharmacist’s state scope of practice and applicable state law © 2019 Trinity Health 32
B. Scope of Practice Pharmacists Providing Services Incident to a Physician’s Services (pages 19 27) • Pharmacists can work with a physician or other practitioner to provide assessment and specimen collection services, and the physician or other practitioner can bill Medicare for the services. • Applicable to non hospital retail pharmacies (e. g. , CVS, Walgreens) Pharmacists also can perform certain COVID 19 tests if they are enrolled in Medicare as a laboratory, in accordance with a pharmacist’s scope of practice and state law. With these changes, beneficiaries may be tested at “parking lot” test sites operated by pharmacies and other entities consistent with state requirements. © 2019 Trinity Health 33

Post Acute Care © 2019 Trinity Health 34
K. IRF Coverage and Classification Changes for Free standing IRFs (pages 79 83) • The CARES Act waives the three hour rule requirement during the COVID 19 PHE. Meaning the minimum requirements of 3 hours therapy per day or 15 hours per week does not have to be met, however attempted. • Medical records should be annotated to the effect that therapy was limited due to COVID 19. • Free standing IRFs can operate as surge locations to house acute care patients, refer to pages 79 83 35
A. HHA Value Based Purchasing Program Reporting (pages 15 19) • Aligning HHA VBP with HHA QRP during the PHE • HHA VBP Model states include: Iowa, Maryland, Florida and Massachusetts • HHA VBP data to be reported at same time/manner as HHA QRP data • Exceptions or extensions granted to HHA QRP will also apply to HHA VBP • HHA VBP calculated using OASIS are still required to be reported during the PHE but with additional time to report © 2019 Trinity Health 36
J. & P. Home Health Policy Updates (page 76 and 145) • Applicable for Medicare and Medicaid Order, certify, re certify, care plan development and oversight extended to other providers • CNMs, NPs, CNSs, or PAs • Must follow state regulations Revised definition of “homebound” status to include suspected COVID 19 or has a medically contraindicated condition placing patient at an increased risk of harm due to COVID 19 exposure, or increased risk of susceptibility. Amending the regulations at parts 409, 424, and 484 to define a NP, a CNS, and a PA, to perform these services permanently. • Applicable to Medicaid only Updates to DMEPOS services as well, notable difference from Medicare – mimics policy and eliminates differentiation 37
T. Delay in the Compliance Date of Certain Reporting Requirements Adopted for IRFs, LTCHs, HHAs and SNFs (page 159 164) • Delaying the compliance dates for the collection and reporting of TOH Information Measures and SPADEs • Current versions of IRF PAI, LTCH and Oasis will remain in effect until at least one full fiscal or calendar year end after the COVID 19 PHE ends • SNFs will not be required to begin reporting on the new MDS for TOH and SPADEs measures for at least two full fiscal years after the PHE end; although the newer MDS may be released sooner; CMS will work with stakeholders to determine an appropriate timeline for release at the conclusion of the PHE 38
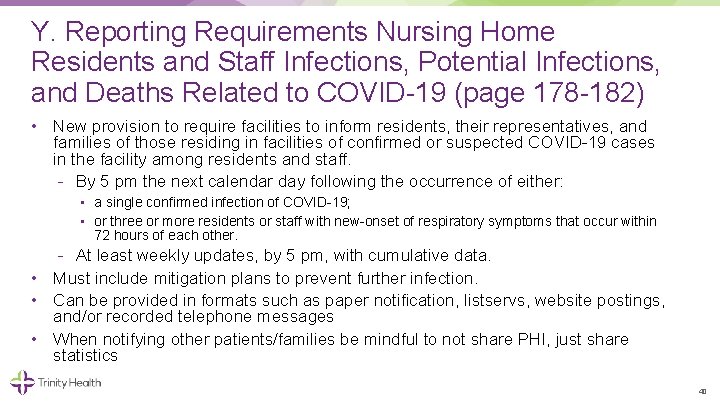
Y. Reporting Requirements Nursing Home Residents and Staff Infections, Potential Infections, and Deaths Related to COVID 19 (page 178 182) • Explicit at least weekly reporting requirements to the CDC/NHSN for confirmed or suspected cases suspected and confirmed COVID 19 infections among residents and staff, including residents previously treated for COVID 19; total deaths and COVID 19 deaths among residents and staff; personal protective equipment and hygiene supplies in the facility; ventilator capacity and supplies available in the facility; resident beds and census; access to COVID 19 testing while the resident is in the facility; staffing shortages; 39
Y. Reporting Requirements Nursing Home Residents and Staff Infections, Potential Infections, and Deaths Related to COVID 19 (page 178 182) • New provision to require facilities to inform residents, their representatives, and families of those residing in facilities of confirmed or suspected COVID 19 cases in the facility among residents and staff. By 5 pm the next calendar day following the occurrence of either: • a single confirmed infection of COVID 19; • or three or more residents or staff with new onset of respiratory symptoms that occur within 72 hours of each other. At least weekly updates, by 5 pm, with cumulative data. • Must include mitigation plans to prevent further infection. • Can be provided in formats such as paper notification, listservs, website postings, and/or recorded telephone messages • When notifying other patients/families be mindful to not share PHI, just share statistics 40

Other © 2019 Trinity Health 41
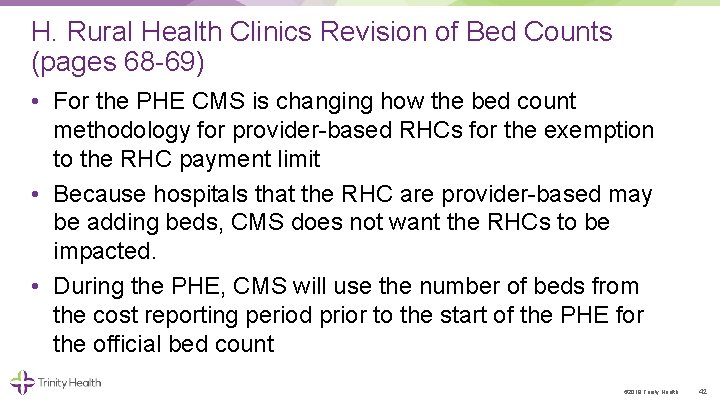
H. Rural Health Clinics Revision of Bed Counts (pages 68 69) • For the PHE CMS is changing how the bed count methodology for provider based RHCs for the exemption to the RHC payment limit • Because hospitals that the RHC are provider based may be adding beds, CMS does not want the RHCs to be impacted. • During the PHE, CMS will use the number of beds from the cost reporting period prior to the start of the PHE for the official bed count © 2019 Trinity Health 42
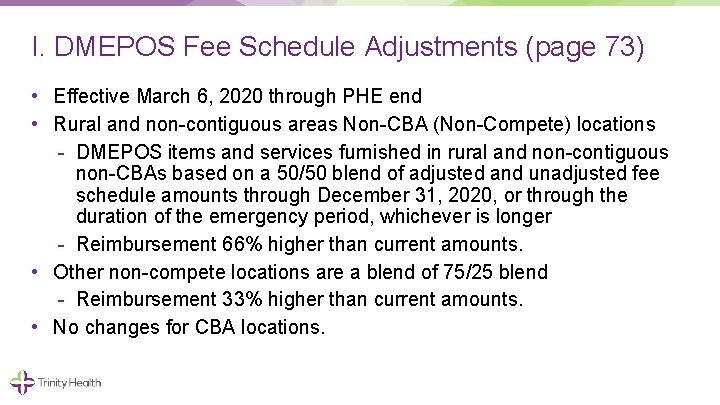
I. DMEPOS Fee Schedule Adjustments (page 73) • Effective March 6, 2020 through PHE end • Rural and non contiguous areas Non CBA (Non Compete) locations DMEPOS items and services furnished in rural and non contiguous non CBAs based on a 50/50 blend of adjusted and unadjusted fee schedule amounts through December 31, 2020, or through the duration of the emergency period, whichever is longer Reimbursement 66% higher than current amounts. • Other non compete locations are a blend of 75/25 blend Reimbursement 33% higher than current amounts. • No changes for CBA locations.
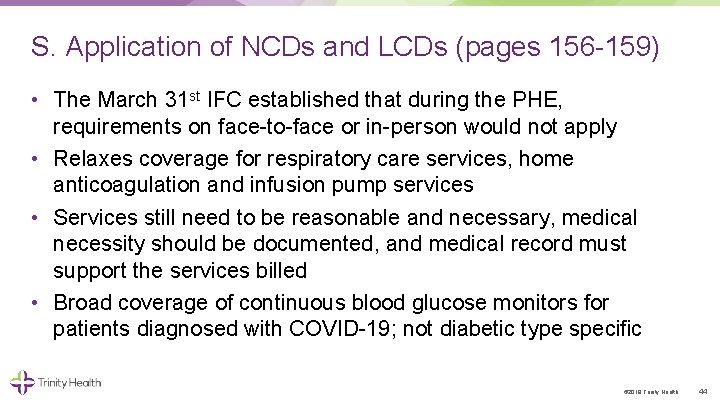
S. Application of NCDs and LCDs (pages 156 159) • The March 31 st IFC established that during the PHE, requirements on face to face or in person would not apply • Relaxes coverage for respiratory care services, home anticoagulation and infusion pump services • Services still need to be reasonable and necessary, medical necessity should be documented, and medical record must support the services billed • Broad coverage of continuous blood glucose monitors for patients diagnosed with COVID 19; not diabetic type specific © 2019 Trinity Health 44
M. Opioid Treatment Programs (pages 31 33) • Now allowed to be provided using audio only telephone calls (previously limited to two way interactive audio and video communication) Therapy Counseling Additional Counseling Periodic Assessments © 2019 Trinity Health 45
Resources • Interim Final Rule 4/30/2020 • American Medical Association, Current Procedural Terminology (CPT), 2020 © 2019 Trinity Health 46