Control 2561 Title A Practical Approach for the

- Slides: 24
Control #: 2561 Title: A Practical Approach for the Differential Diagnosis in Trigeminal Nerve Involvement e. Ed. E#: e. Ed. E-46
A Practical Approach for The Differential Diagnosis in The Trigeminal Nerve Involvement Diego Cardoso Fragoso Thiago Luiz P. D. Scoppetta Felipe Torres Pacheco Renato Hoffmann Nunes Antônio Carlos Martins Maia Junior Antônio José da Rocha Irmandade da Santa Casa de Misericórdia de São Paulo Serviço de Diagnóstico por Imagem
There is no conflict of interest in this presentation
BACKGROUND Click to display Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References • Trigeminal nerve and spinal trigeminal nucleus involvement can occur in a wide range of diseases. Trigeminal neuropathy may be the only or one of several clinical signs of an underlying disease. • Based on clinical examination alone, it is not always possible to precisely locate a lesion along the course of the trigeminal nerve. Therefore, trigeminal nerve dysfunction has become a common indication for imaging. • Our purpose is to review the trigeminal nerve intracranial anatomy and discuss the spectrum of pathologic conditions that affect the brainstem and cisternal segments of the trigeminal nerve, with special emphasis on their peculiarities in order to narrow the differential diagnosis.
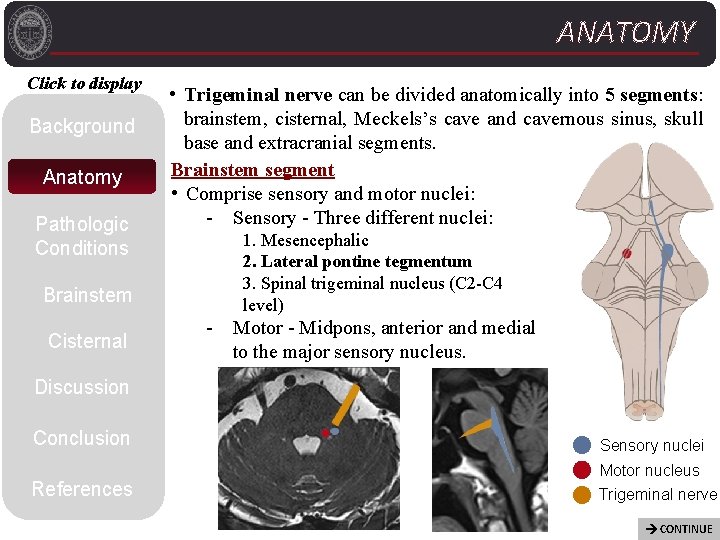
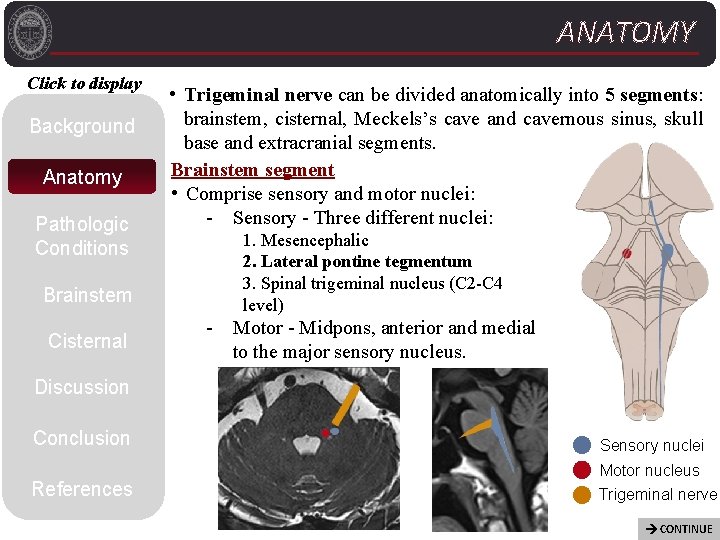
ANATOMY Click to display Background Anatomy Pathologic Conditions Brainstem Cisternal • Trigeminal nerve can be divided anatomically into 5 segments: brainstem, cisternal, Meckels’s cave and cavernous sinus, skull base and extracranial segments. Brainstem segment • Comprise sensory and motor nuclei: - Sensory - Three different nuclei: 1. Mesencephalic 2. Lateral pontine tegmentum 3. Spinal trigeminal nucleus (C 2 -C 4 level) - Motor - Midpons, anterior and medial to the major sensory nucleus. Discussion Conclusion Sensory nuclei References Motor nucleus Trigeminal nerve CONTINUE
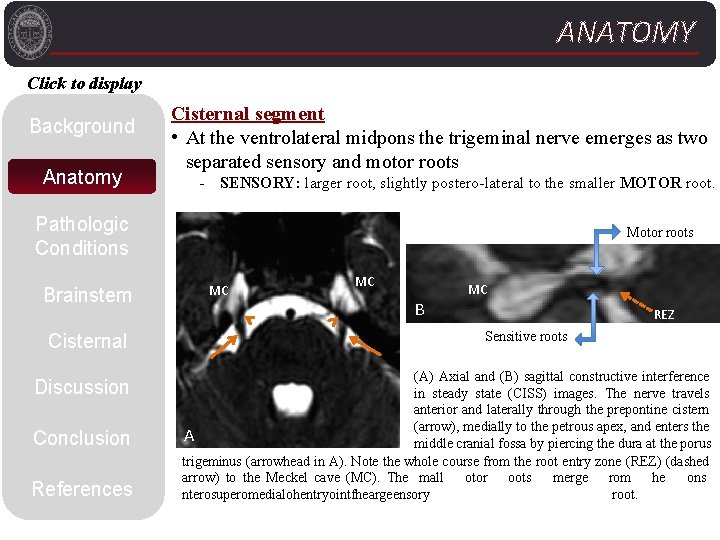
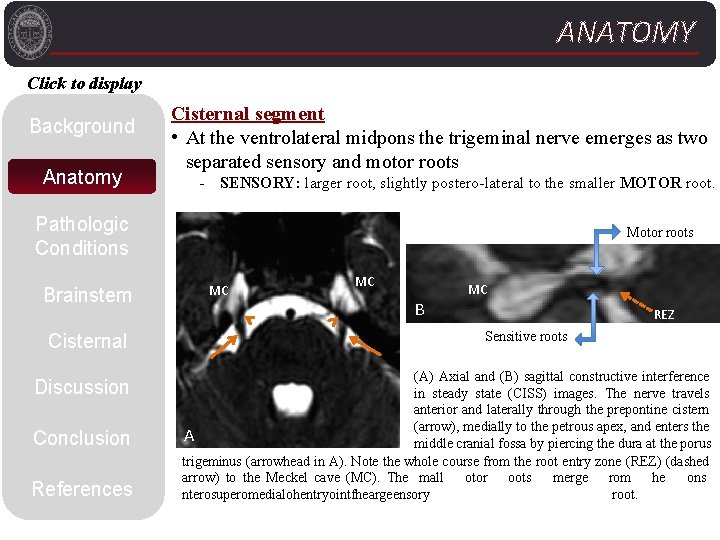
ANATOMY Click to display Background Anatomy Cisternal segment • At the ventrolateral midpons the trigeminal nerve emerges as two separated sensory and motor roots - SENSORY: larger root, slightly postero-lateral to the smaller MOTOR root. Pathologic Conditions Brainstem Cisternal Discussion Conclusion References Motor roots MC MC B MC REZ Sensitive roots (A) Axial and (B) sagittal constructive interference in steady state (CISS) images. The nerve travels anterior and laterally through the prepontine cistern (arrow), medially to the petrous apex, and enters the A middle cranial fossa by piercing the dura at the porus trigeminus (arrowhead in A). Note the whole course from the root entry zone (REZ) (dashed arrow) to the Meckel cave (MC). The mall otor oots merge rom he ons nterosuperomedialohentryointfheargeensory root.
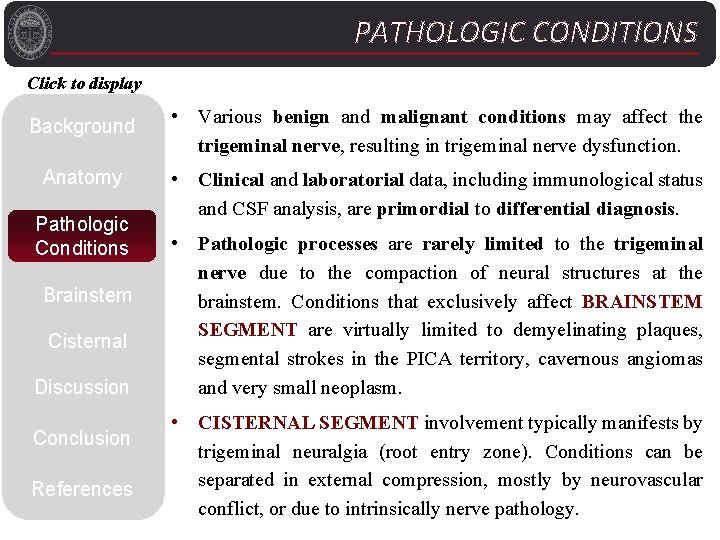
PATHOLOGIC CONDITIONS Click to display Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References • Various benign and malignant conditions may affect the trigeminal nerve, resulting in trigeminal nerve dysfunction. • Clinical and laboratorial data, including immunological status and CSF analysis, are primordial to differential diagnosis. • Pathologic processes are rarely limited to the trigeminal nerve due to the compaction of neural structures at the brainstem. Conditions that exclusively affect BRAINSTEM SEGMENT are virtually limited to demyelinating plaques, segmental strokes in the PICA territory, cavernous angiomas and very small neoplasm. • CISTERNAL SEGMENT involvement typically manifests by trigeminal neuralgia (root entry zone). Conditions can be separated in external compression, mostly by neurovascular conflict, or due to intrinsically nerve pathology.
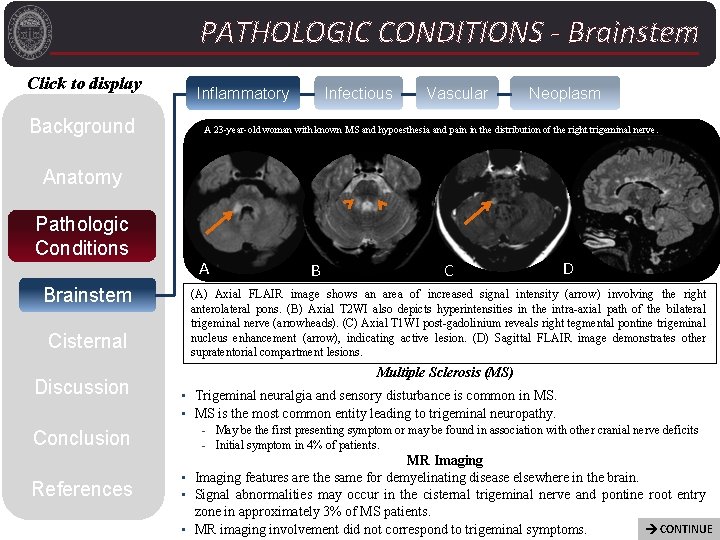
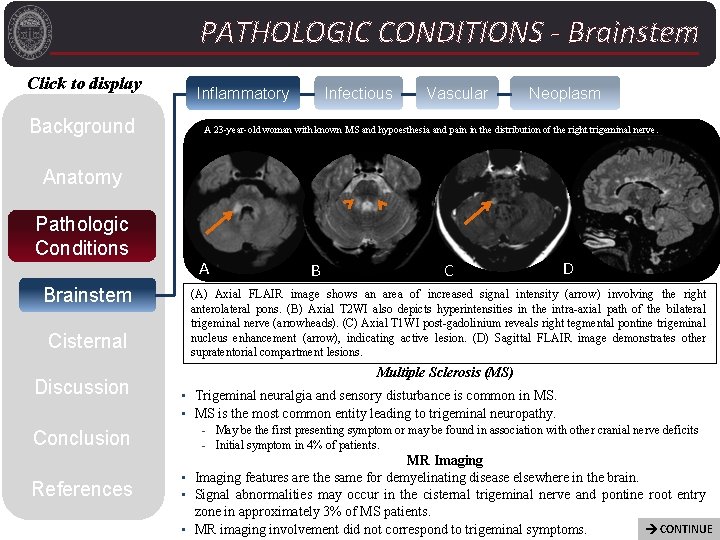
PATHOLOGIC CONDITIONS - Brainstem Click to display Background Inflammatory Infectious Vascular Neoplasm A 23 -year-old woman with known MS and hypoesthesia and pain in the distribution of the right trigeminal nerve. Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References A B C D (A) Axial FLAIR image shows an area of increased signal intensity (arrow) involving the right anterolateral pons. (B) Axial T 2 WI also depicts hyperintensities in the intra-axial path of the bilateral trigeminal nerve (arrowheads). (C) Axial T 1 WI post-gadolinium reveals right tegmental pontine trigeminal nucleus enhancement (arrow), indicating active lesion. (D) Sagittal FLAIR image demonstrates other supratentorial compartment lesions. Multiple Sclerosis (MS) • Trigeminal neuralgia and sensory disturbance is common in MS. • MS is the most common entity leading to trigeminal neuropathy. - May be the first presenting symptom or may be found in association with other cranial nerve deficits - Initial symptom in 4% of patients. MR Imaging • Imaging features are the same for demyelinating disease elsewhere in the brain. • Signal abnormalities may occur in the cisternal trigeminal nerve and pontine root entry zone in approximately 3% of MS patients. CONTINUE • MR imaging involvement did not correspond to trigeminal symptoms.
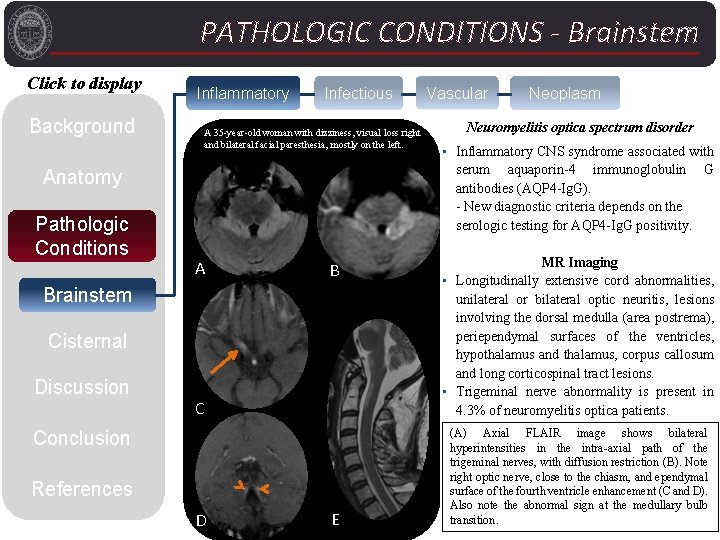
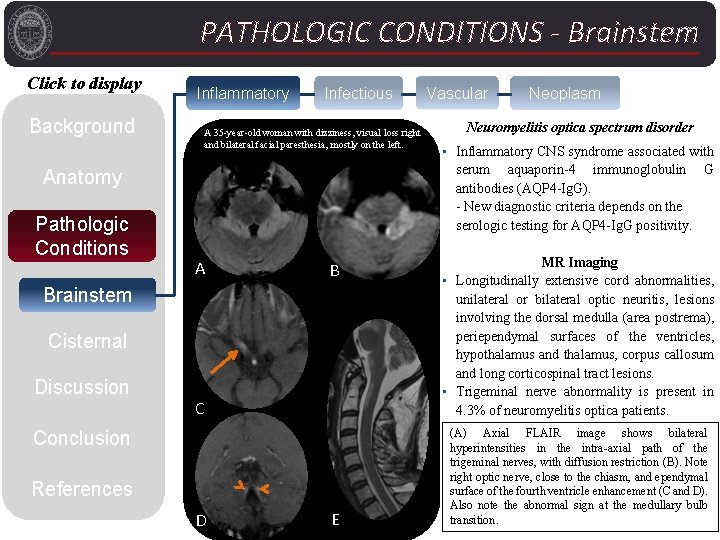
PATHOLOGIC CONDITIONS - Brainstem Click to display Background Inflammatory Infectious A 35 -year-old woman with dizziness, visual loss right and bilateral facial paresthesia, mostly on the left. Anatomy Pathologic Conditions Neoplasm Neuromyelitis optica spectrum disorder • Inflammatory CNS syndrome associated with serum aquaporin-4 immunoglobulin G antibodies (AQP 4 -Ig. G). - New diagnostic criteria depends on the serologic testing for AQP 4 -Ig. G positivity. C MR Imaging • Longitudinally extensive cord abnormalities, unilateral or bilateral optic neuritis, lesions involving the dorsal medulla (area postrema), periependymal surfaces of the ventricles, hypothalamus and thalamus, corpus callosum and long corticospinal tract lesions. • Trigeminal nerve abnormality is present in 4. 3% of neuromyelitis optica patients. D (A) Axial FLAIR image shows bilateral hyperintensities in the intra-axial path of the trigeminal nerves, with diffusion restriction (B). Note right optic nerve, close to the chiasm, and ependymal surface of the fourth ventricle enhancement (C and D). Also note the abnormal sign at the medullary bulb transition. A B Brainstem Cisternal Discussion Vascular Conclusion References E
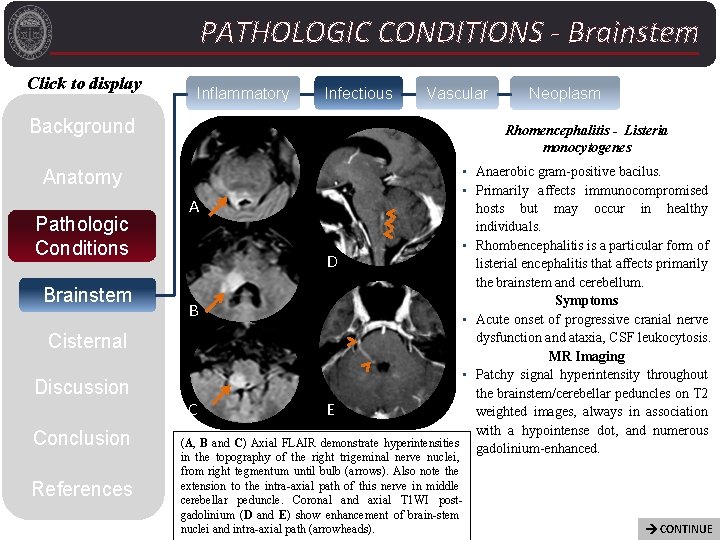
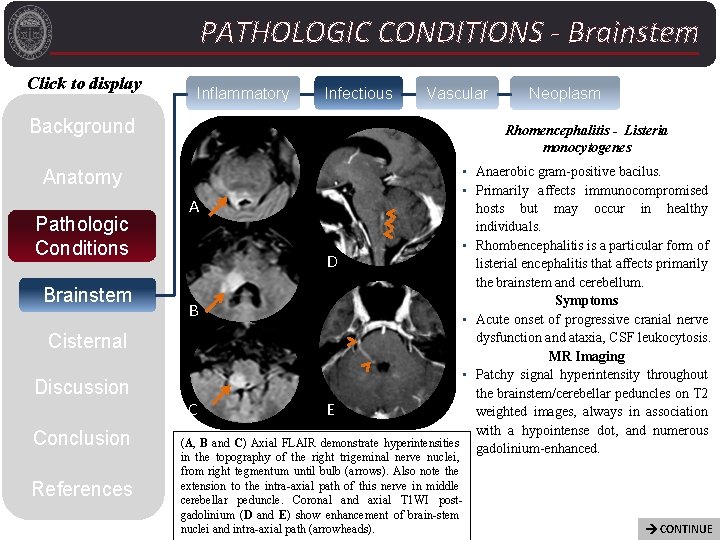
PATHOLOGIC CONDITIONS - Brainstem Click to display Inflammatory Infectious Vascular Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References Neoplasm Rhomencephalitis - Listeria monocytogenes • Anaerobic gram-positive bacilus. • Primarily affects immunocompromised A hosts but may occur in healthy individuals. • Rhombencephalitis is a particular form of D listerial encephalitis that affects primarily the brainstem and cerebellum. Symptoms B • Acute onset of progressive cranial nerve dysfunction and ataxia, CSF leukocytosis. MR Imaging • Patchy signal hyperintensity throughout the brainstem/cerebellar peduncles on T 2 C E weighted images, always in association with a hypointense dot, and numerous (A, B and C) Axial FLAIR demonstrate hyperintensities gadolinium-enhanced. in the topography of the right trigeminal nerve nuclei, from right tegmentum until bulb (arrows). Also note the extension to the intra-axial path of this nerve in middle cerebellar peduncle. Coronal and axial T 1 WI postgadolinium (D and E) show enhancement of brain-stem nuclei and intra-axial path (arrowheads). CONTINUE
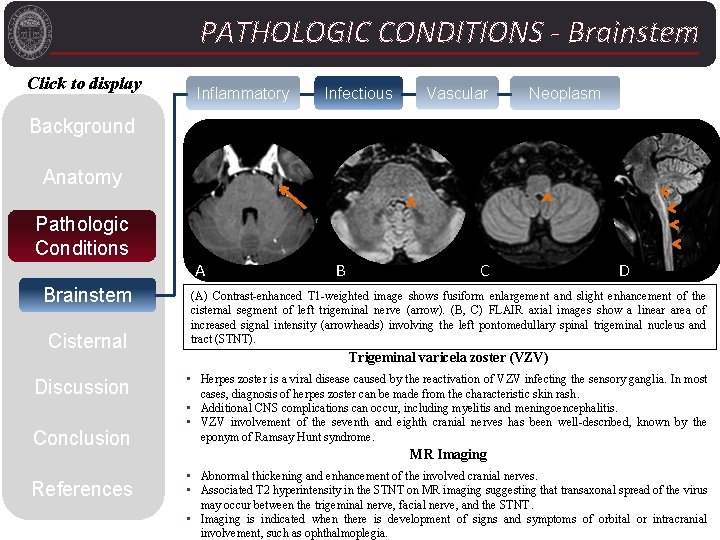
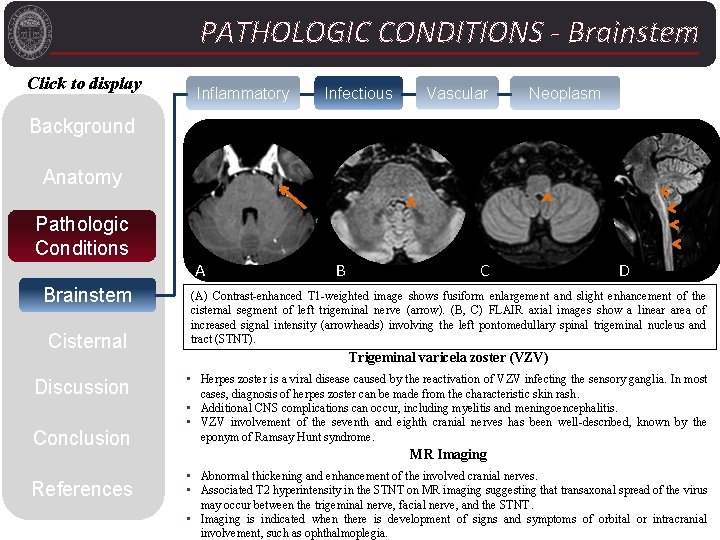
PATHOLOGIC CONDITIONS - Brainstem Click to display Inflammatory Infectious Vascular Neoplasm Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References A B C D (A) Contrast-enhanced T 1 -weighted image shows fusiform enlargement and slight enhancement of the cisternal segment of left trigeminal nerve (arrow). (B, C) FLAIR axial images show a linear area of increased signal intensity (arrowheads) involving the left pontomedullary spinal trigeminal nucleus and tract (STNT). Trigeminal varicela zoster (VZV) • Herpes zoster is a viral disease caused by the reactivation of VZV infecting the sensory ganglia. In most cases, diagnosis of herpes zoster can be made from the characteristic skin rash. • Additional CNS complications can occur, including myelitis and meningoencephalitis. • VZV involvement of the seventh and eighth cranial nerves has been well-described, known by the eponym of Ramsay Hunt syndrome. MR Imaging • Abnormal thickening and enhancement of the involved cranial nerves. • Associated T 2 hyperintensity in the STNT on MR imaging suggesting that transaxonal spread of the virus may occur between the trigeminal nerve, facial nerve, and the STNT. • Imaging is indicated when there is development of signs and symptoms of orbital or intracranial involvement, such as ophthalmoplegia.
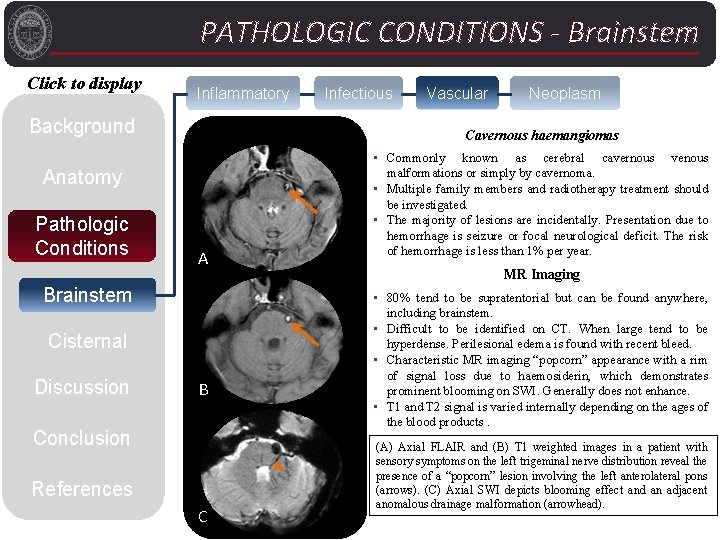
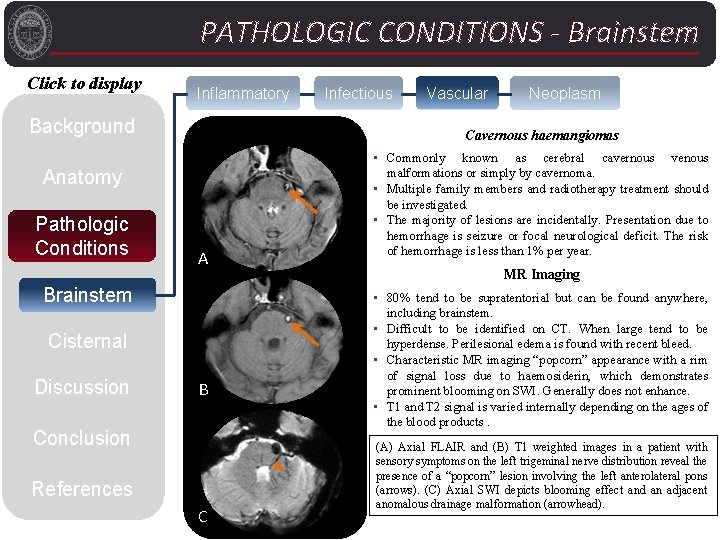
PATHOLOGIC CONDITIONS - Brainstem Click to display Inflammatory Background A Brainstem Cisternal Discussion Vascular Neoplasm Cavernous haemangiomas Anatomy Pathologic Conditions Infectious B Conclusion References C • Commonly known as cerebral cavernous venous malformations or simply by cavernoma. • Multiple family members and radiotherapy treatment should be investigated. • The majority of lesions are incidentally. Presentation due to hemorrhage is seizure or focal neurological deficit. The risk of hemorrhage is less than 1% per year. MR Imaging • 80% tend to be supratentorial but can be found anywhere, including brainstem. • Difficult to be identified on CT. When large tend to be hyperdense. Perilesional edema is found with recent bleed. • Characteristic MR imaging “popcorn” appearance with a rim of signal loss due to haemosiderin, which demonstrates prominent blooming on SWI. Generally does not enhance. • T 1 and T 2 signal is varied internally depending on the ages of the blood products. (A) Axial FLAIR and (B) T 1 weighted images in a patient with sensory symptoms on the left trigeminal nerve distribution reveal the presence of a “popcorn” lesion involving the left anterolateral pons (arrows). (C) Axial SWI depicts blooming effect and an adjacent anomalous drainage malformation (arrowhead).
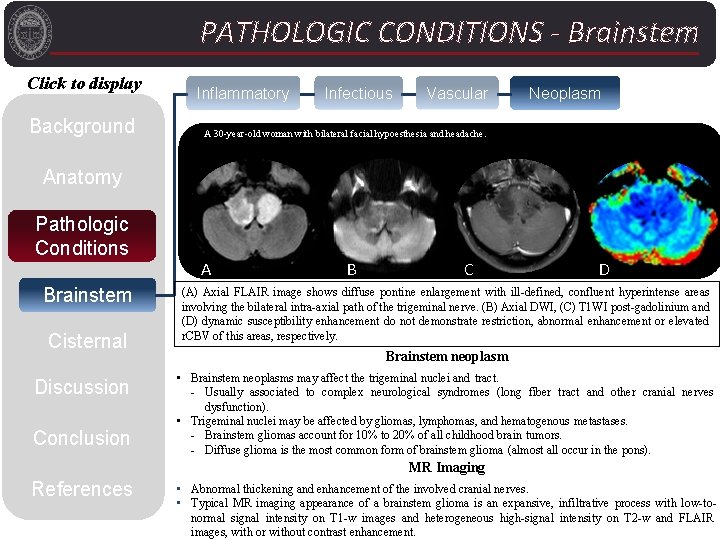
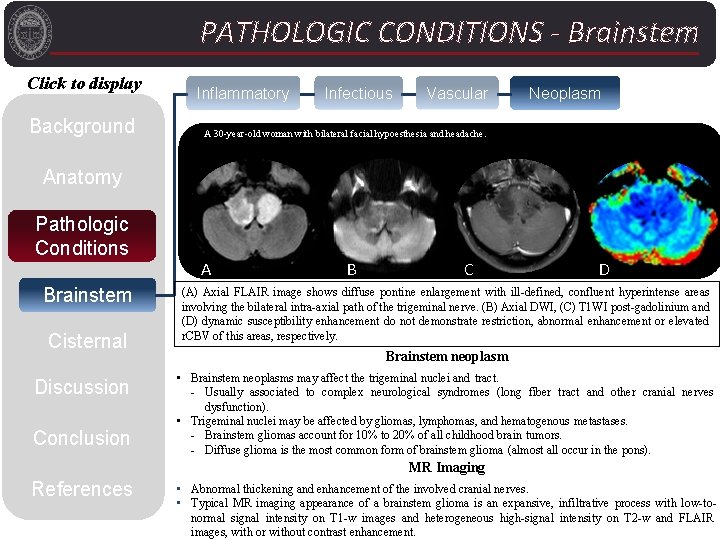
PATHOLOGIC CONDITIONS - Brainstem Click to display Background Inflammatory Infectious Vascular Neoplasm A 30 -year-old woman with bilateral facial hypoesthesia and headache. Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion A B C D (A) Axial FLAIR image shows diffuse pontine enlargement with ill-defined, confluent hyperintense areas involving the bilateral intra-axial path of the trigeminal nerve. (B) Axial DWI, (C) T 1 WI post-gadolinium and (D) dynamic susceptibility enhancement do not demonstrate restriction, abnormal enhancement or elevated r. CBV of this areas, respectively. Brainstem neoplasm • Brainstem neoplasms may affect the trigeminal nuclei and tract. - Usually associated to complex neurological syndromes (long fiber tract and other cranial nerves dysfunction). • Trigeminal nuclei may be affected by gliomas, lymphomas, and hematogenous metastases. - Brainstem gliomas account for 10% to 20% of all childhood brain tumors. - Diffuse glioma is the most common form of brainstem glioma (almost all occur in the pons). MR Imaging References • Abnormal thickening and enhancement of the involved cranial nerves. • Typical MR imaging appearance of a brainstem glioma is an expansive, infiltrative process with low-tonormal signal intensity on T 1 -w images and heterogeneous high-signal intensity on T 2 -w and FLAIR images, with or without contrast enhancement.
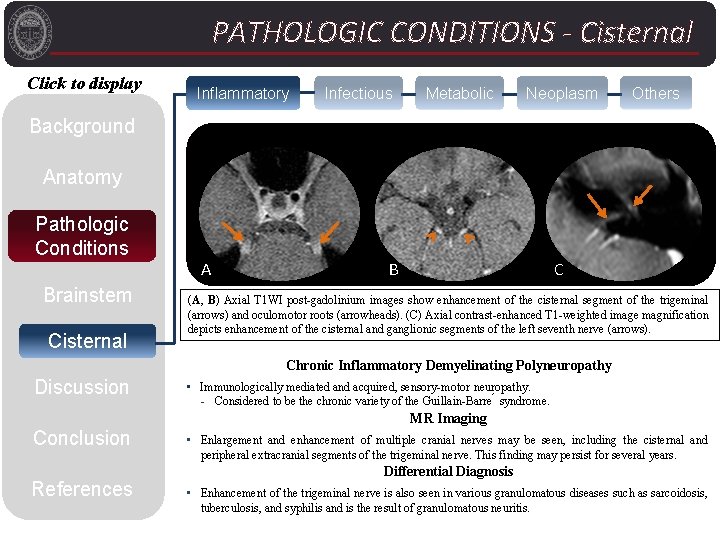
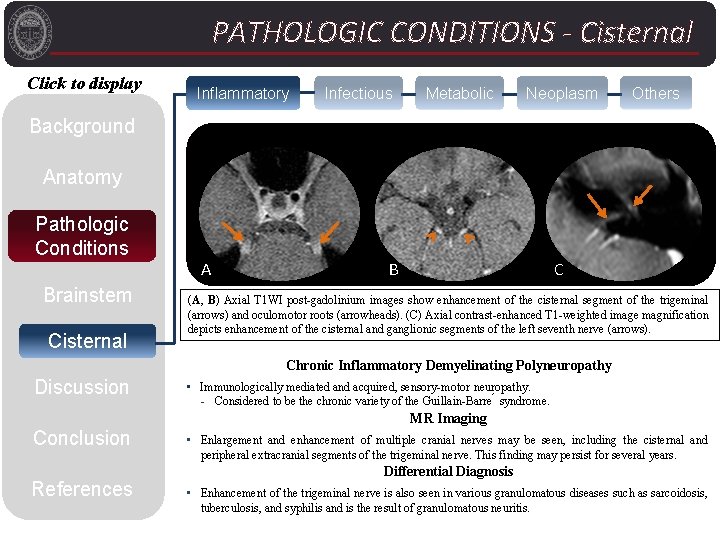
PATHOLOGIC CONDITIONS - Cisternal Click to display Inflammatory Infectious Metabolic Neoplasm Others Background Anatomy Pathologic Conditions Brainstem Cisternal A B C (A, B) Axial T 1 WI post-gadolinium images show enhancement of the cisternal segment of the trigeminal (arrows) and oculomotor roots (arrowheads). (C) Axial contrast-enhanced T 1 -weighted image magnification depicts enhancement of the cisternal and ganglionic segments of the left seventh nerve (arrows). Chronic Inflammatory Demyelinating Polyneuropathy Discussion • Immunologically mediated and acquired, sensory-motor neuropathy. - Considered to be the chronic variety of the Guillain-Barre syndrome. MR Imaging Conclusion References • Enlargement and enhancement of multiple cranial nerves may be seen, including the cisternal and peripheral extracranial segments of the trigeminal nerve. This finding may persist for several years. Differential Diagnosis • Enhancement of the trigeminal nerve is also seen in various granulomatous diseases such as sarcoidosis, tuberculosis, and syphilis and is the result of granulomatous neuritis.
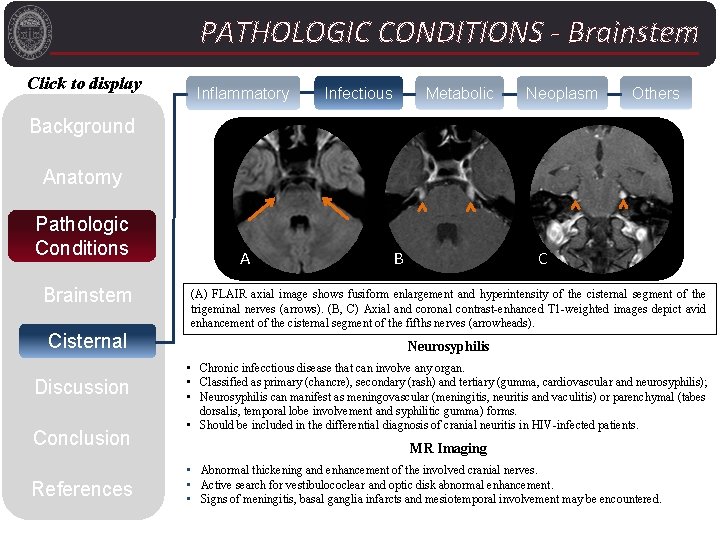
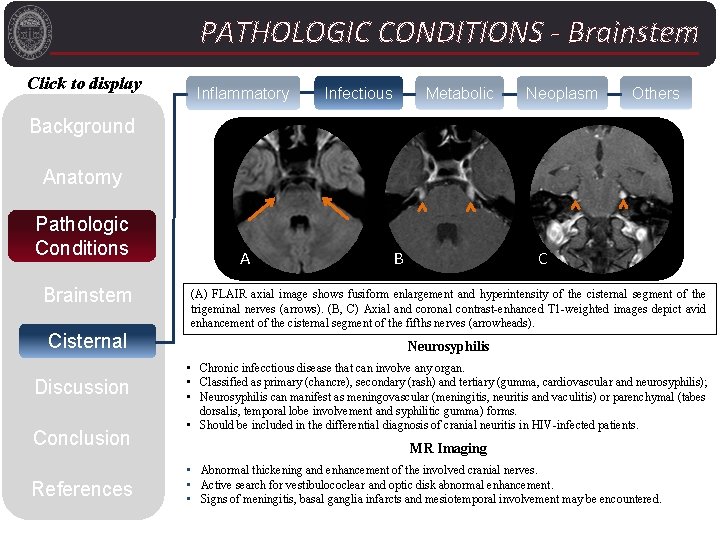
PATHOLOGIC CONDITIONS - Brainstem Click to display Inflammatory Infectious Metabolic Neoplasm Others Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References A B C (A) FLAIR axial image shows fusiform enlargement and hyperintensity of the cisternal segment of the trigeminal nerves (arrows). (B, C) Axial and coronal contrast-enhanced T 1 -weighted images depict avid enhancement of the cisternal segment of the fifths nerves (arrowheads). Neurosyphilis • Chronic infecctious disease that can involve any organ. • Classified as primary (chancre), secondary (rash) and tertiary (gumma, cardiovascular and neurosyphilis); • Neurosyphilis can manifest as meningovascular (meningitis, neuritis and vaculitis) or parenchymal (tabes dorsalis, temporal lobe involvement and syphilitic gumma) forms. • Should be included in the differential diagnosis of cranial neuritis in HIV-infected patients. MR Imaging • Abnormal thickening and enhancement of the involved cranial nerves. • Active search for vestibulococlear and optic disk abnormal enhancement. • Signs of meningitis, basal ganglia infarcts and mesiotemporal involvement may be encountered.
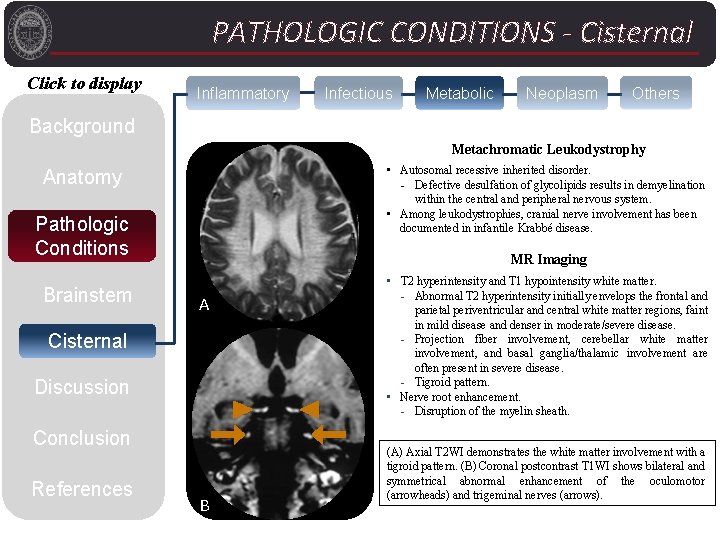
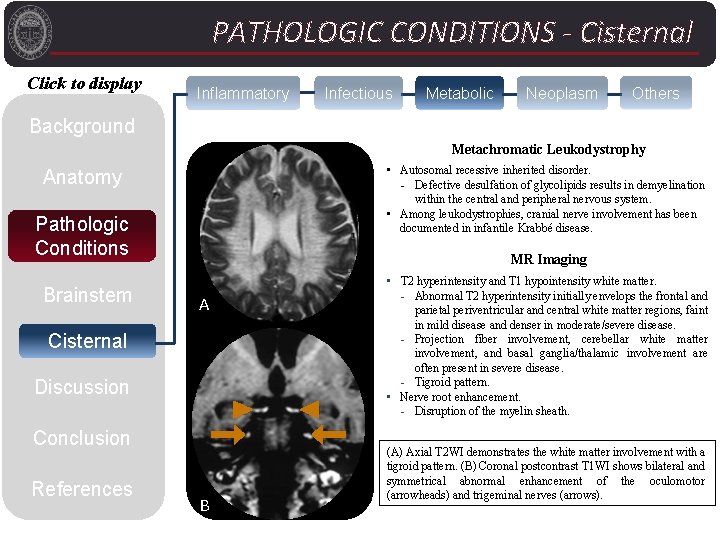
PATHOLOGIC CONDITIONS - Cisternal Click to display Inflammatory Infectious Metabolic Neoplasm Others Background Metachromatic Leukodystrophy • Autosomal recessive inherited disorder. - Defective desulfation of glycolipids results in demyelination within the central and peripheral nervous system. • Among leukodystrophies, cranial nerve involvement has been documented in infantile Krabbé disease. Anatomy Pathologic Conditions Brainstem MR Imaging A Cisternal Discussion Conclusion References B • T 2 hyperintensity and T 1 hypointensity white matter. - Abnormal T 2 hyperintensity initially envelops the frontal and parietal periventricular and central white matter regions, faint in mild disease and denser in moderate/severe disease. - Projection fiber involvement, cerebellar white matter involvement, and basal ganglia/thalamic involvement are often present in severe disease. - Tigroid pattern. • Nerve root enhancement. - Disruption of the myelin sheath. (A) Axial T 2 WI demonstrates the white matter involvement with a tigroid pattern. (B) Coronal postcontrast T 1 WI shows bilateral and symmetrical abnormal enhancement of the oculomotor (arrowheads) and trigeminal nerves (arrows).
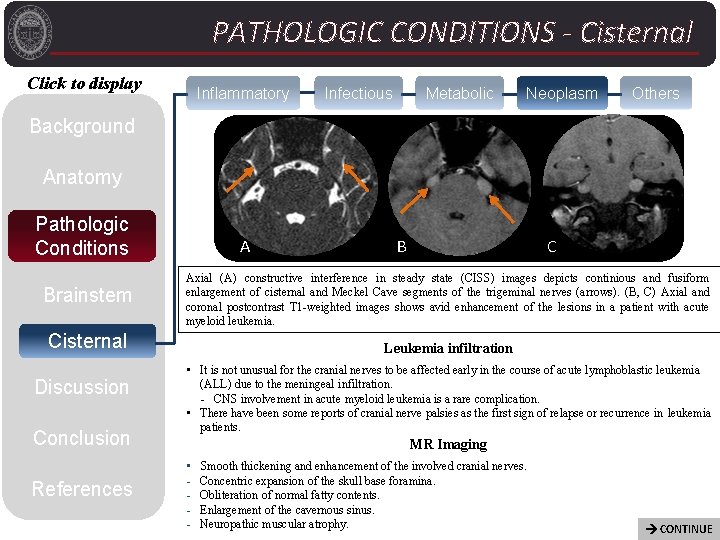
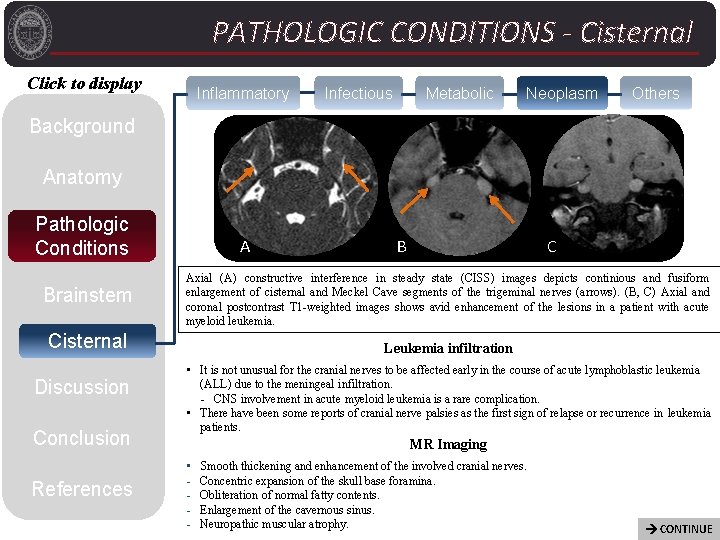
PATHOLOGIC CONDITIONS - Cisternal Click to display Inflammatory Infectious Metabolic Neoplasm Others Background Anatomy Pathologic Conditions Brainstem A Conclusion References C Axial (A) constructive interference in steady state (CISS) images depicts continious and fusiform enlargement of cisternal and Meckel Cave segments of the trigeminal nerves (arrows). (B, C) Axial and coronal postcontrast T 1 -weighted images shows avid enhancement of the lesions in a patient with acute myeloid leukemia. Cisternal Discussion B Leukemia infiltration • It is not unusual for the cranial nerves to be affected early in the course of acute lymphoblastic leukemia (ALL) due to the meningeal infiltration. - CNS involvement in acute myeloid leukemia is a rare complication. • There have been some reports of cranial nerve palsies as the first sign of relapse or recurrence in leukemia patients. MR Imaging • - Smooth thickening and enhancement of the involved cranial nerves. Concentric expansion of the skull base foramina. Obliteration of normal fatty contents. Enlargement of the cavernous sinus. Neuropathic muscular atrophy. CONTINUE
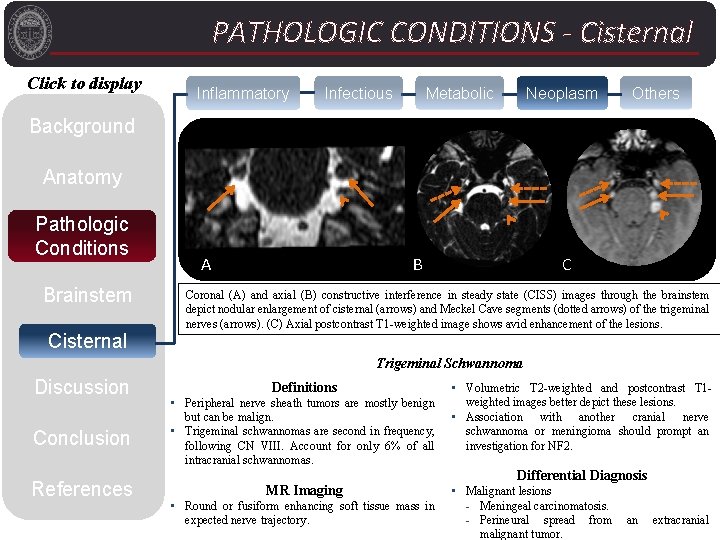
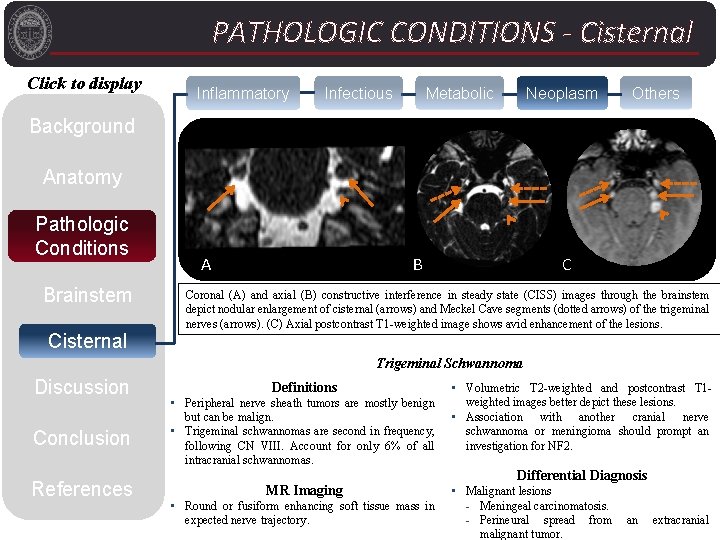
PATHOLOGIC CONDITIONS - Cisternal Click to display Inflammatory Infectious Metabolic Neoplasm Others Background C Anatomy Pathologic Conditions Brainstem A B C Coronal (A) and axial (B) constructive interference in steady state (CISS) images through the brainstem depict nodular enlargement of cisternal (arrows) and Meckel Cave segments (dotted arrows) of the trigeminal nerves (arrows). (C) Axial postcontrast T 1 -weighted image shows avid enhancement of the lesions. Cisternal Trigeminal Schwannoma Discussion Conclusion References Definitions • Peripheral nerve sheath tumors are mostly benign but can be malign. • Trigeminal schwannomas are second in frequency, following CN VIII. Account for only 6% of all intracranial schwannomas. MR Imaging • Round or fusiform enhancing soft tissue mass in expected nerve trajectory. • Volumetric T 2 -weighted and postcontrast T 1 weighted images better depict these lesions. • Association with another cranial nerve schwannoma or meningioma should prompt an investigation for NF 2. Differential Diagnosis • Malignant lesions - Meningeal carcinomatosis. - Perineural spread from an extracranial malignant tumor.
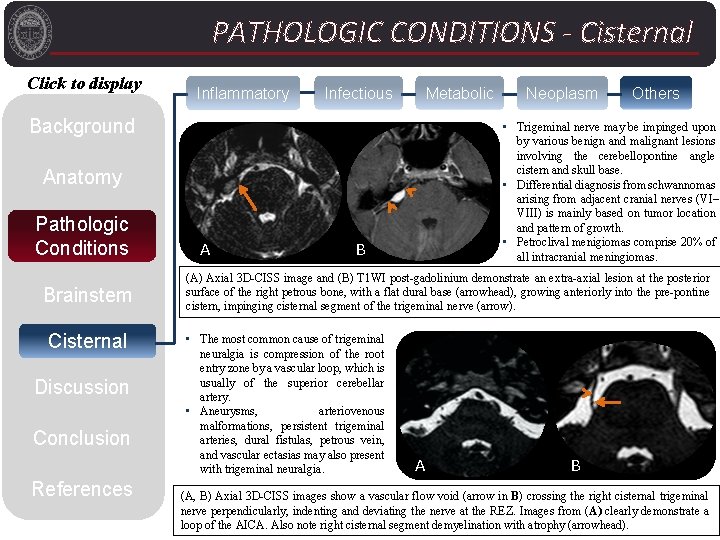
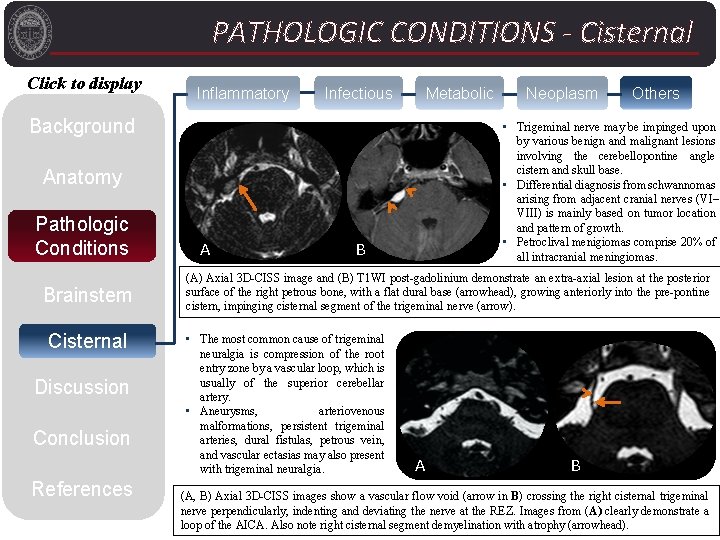
PATHOLOGIC CONDITIONS - Cisternal Click to display Inflammatory Infectious Metabolic Background Brainstem Cisternal Discussion Conclusion References A Others • Trigeminal nerve may be impinged upon by various benign and malignant lesions involving the cerebellopontine angle cistern and skull base. • Differential diagnosis from schwannomas arising from adjacent cranial nerves (VI– VIII) is mainly based on tumor location and pattern of growth. • Petroclival menigiomas comprise 20% of all intracranial meningiomas. Anatomy Pathologic Conditions Neoplasm B (A) Axial 3 D-CISS image and (B) T 1 WI post-gadolinium demonstrate an extra-axial lesion at the posterior surface of the right petrous bone, with a flat dural base (arrowhead), growing anteriorly into the pre-pontine cistern, impinging cisternal segment of the trigeminal nerve (arrow). • The most common cause of trigeminal neuralgia is compression of the root entry zone by a vascular loop, which is usually of the superior cerebellar artery. • Aneurysms, arteriovenous malformations, persistent trigeminal arteries, dural fistulas, petrous vein, and vascular ectasias may also present with trigeminal neuralgia. A B (A, B) Axial 3 D-CISS images show a vascular flow void (arrow in B) crossing the right cisternal trigeminal nerve perpendicularly, indenting and deviating the nerve at the REZ. Images from (A) clearly demonstrate a loop of the AICA. Also note right cisternal segment demyelination with atrophy (arrowhead).
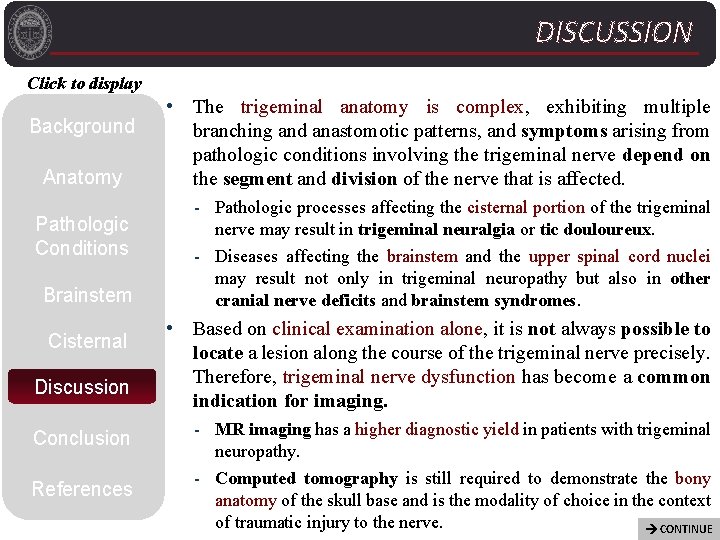
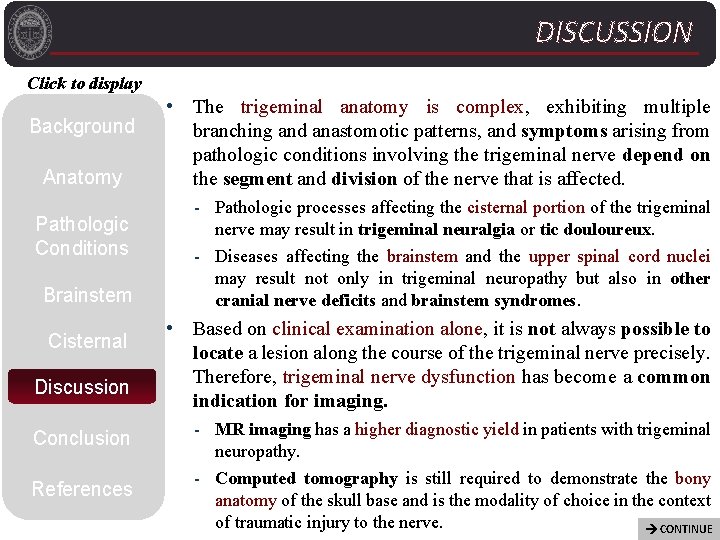
DISCUSSION Click to display Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References • The trigeminal anatomy is complex, exhibiting multiple branching and anastomotic patterns, and symptoms arising from pathologic conditions involving the trigeminal nerve depend on the segment and division of the nerve that is affected. - Pathologic processes affecting the cisternal portion of the trigeminal nerve may result in trigeminal neuralgia or tic douloureux. - Diseases affecting the brainstem and the upper spinal cord nuclei may result not only in trigeminal neuropathy but also in other cranial nerve deficits and brainstem syndromes. • Based on clinical examination alone, it is not always possible to locate a lesion along the course of the trigeminal nerve precisely. Therefore, trigeminal nerve dysfunction has become a common indication for imaging. - MR imaging has a higher diagnostic yield in patients with trigeminal neuropathy. - Computed tomography is still required to demonstrate the bony anatomy of the skull base and is the modality of choice in the context of traumatic injury to the nerve. CONTINUE
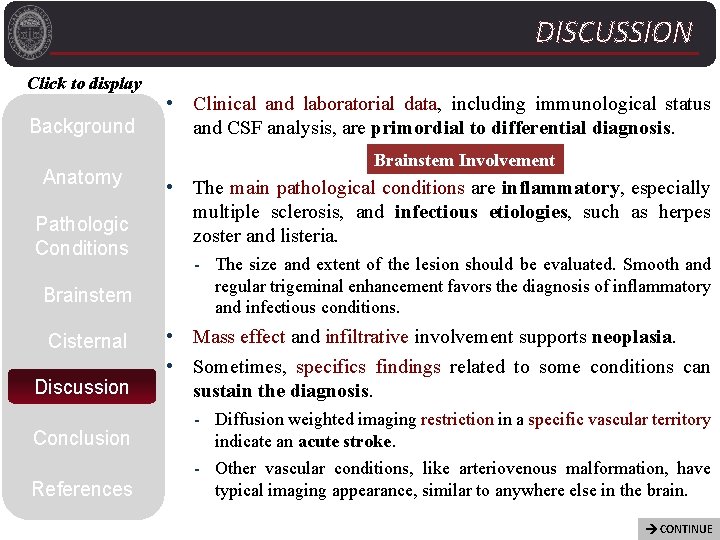
DISCUSSION Click to display Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References • Clinical and laboratorial data, including immunological status and CSF analysis, are primordial to differential diagnosis. Brainstem Involvement • The main pathological conditions are inflammatory, especially multiple sclerosis, and infectious etiologies, such as herpes zoster and listeria. - The size and extent of the lesion should be evaluated. Smooth and regular trigeminal enhancement favors the diagnosis of inflammatory and infectious conditions. • Mass effect and infiltrative involvement supports neoplasia. • Sometimes, specifics findings related to some conditions can sustain the diagnosis. - Diffusion weighted imaging restriction in a specific vascular territory indicate an acute stroke. - Other vascular conditions, like arteriovenous malformation, have typical imaging appearance, similar to anywhere else in the brain. CONTINUE
DISCUSSION Click to display Background Anatomy Cisternal Involvement • Enhancement of the trigeminal nerve is seen in various inflammatory and infectious diseases. - Clinical and laboratory evaluation, including analysis of cerebrospinal fluid, will narrow the differential diagnosis. Pathologic Conditions • Both benign and malignant tumors results in gadolinium enhancement of the preganglionic segment: Brainstem - Usually enlarged, with irregular or smooth margins (the correct diagnosis can only be suggested if the clinical background is known). Cisternal Discussion Conclusion References • Metabolic conditions, although rare, should be included in the differential diagnosis, such as metachromatic leukodystrophy and Krabbé disease. - Delayed neurodevelopment and peripheral neuropathy, mostly in children. • Trigeminal neuralgia due compression of the root entry zone is mainly caused by aberrant loops of arteries or veins. - MR imaging with tailored protocol confidently demonstrate the neurovascular conflict.
CONCLUSION Click to display Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References • Imaging of patients with trigeminal neuropathy requires thorough understanding of the anatomy and physiology of this cranial nerve. • A clinically oriented segmental approach to trigeminal nerve pathology is important to guide high-resolution imaging studies to achieve the maximum imaging capability in the evaluation of patients with trigeminal dysfunction. • There a wide variety of disorders that affect the trigeminal pathway. Knowledge of the imaging features of usual and even unusual pathologic conditions can prevent their misinterpretation and facilitate the correct diagnosis.

REFERENCES Click to display Background Anatomy Pathologic Conditions Brainstem Cisternal Discussion Conclusion References 1. Kamel HA, Toland J. Trigeminal nerve anatomy: illustrated using examples of abnormalities. American Journal of Roentgenology. 2001 Jan; 176(1): 247– 51. 2. Saremi F, Helmy M, Farzin S, Zee CS, Go JL. MRI of Cranial Nerve Enhancement. American Journal of Roentgenology. 2005 Dec; 185(6): 1487– 97. 3. Mills RJ, Young CA, Smith ET. Central trigeminal involvement in multiple sclerosis using high-resolution MRI at 3 T. The British Journal of Radiology. 2010 Jun; 83(990): 493– 8. 4. Fritz J, Vogel W, Bares R, Horger M. Radiologic Spectrum of Extramedullary Relapse of Myelogenous Leukemia in Adults. American Journal of Roentgenology. 2007 Jul; 189(1): 209– 18. 5. Gonella M, Fischbein N, So Y. Disorders of the Trigeminal System. Semin Neurol. © Thieme Medical Publishers; 2009 Feb 12; 29(01): 036– 44. 6. Becker M, Kohler R, Vargas MI, Viallon M, Delavelle J. Pathology of the Trigeminal Nerve. Neuroimaging Clinics of North America. 2008 May; 18(2): 283– 307. 7. Borges A, Casselman J. European Journal of Radiology. Elsevier Ireland Ltd; 2010 May 1; 74(2): 323– 40. 8. Bathla G, Hegde AN. The trigeminal nerve: An illustrated review of its imaging anatomy and pathology. Clinical Radiology. The Royal College of Radiologists; 2013; 68(2): 203– 13. 9. Maia ACM, da Rocha AJ, da Silva CJ, Rosemberg S. Multiple Cranial Nerve Enhancement: A New MR Imaging Finding in Metachromatic Leukodystrophy. American Journal of Neuroradiology. 2007 Jun 1; 28(6): 999– 9. 10. Seidel E, Hansen C, Urban PP, et al. Idiopathic trigeminal sensory neuropathy with gadolinium enhancement in the cisternal segment. Neurology 2000; 54: 1191– 2. 11. Guedes BF, Cury RG. Trigeminal nerve thickening in chronic inflammatory demyelinating polyneuropathy. Arq Neuro. Psiquiatr. 2015 Jul 1; 73(7): 634– 5. 12. Wingerchuk DM, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology; 2015 Jul 14; 85: 177– 89. 13. Tamojit Chaudhuri DM, Kamlesh Y. Symptomatic trigeminal neuralgia as the first presentation of acute lymphoblastic leukemia. Ann Indian Acad Neurol. 2013 Jul-Sep; 16(3): 463– 464. 14. Vasilatou D, Papageorgiou S, Bazani E, Prasouli A, Economopoulou C, Roumpakis C, et al. Case Report CNS Involvement in AML Patient Treated with 5 -Azacytidine. Case Reports in Hematology. Hindawi Publishing Corporation; 2014 Aug 14; : 1– 4. 15. Mills RJ, Young CA, Smith ET. Central trigeminal involvement in multiple sclerosis using high-resolution MRI at 3 T. The British Journal of Radiology. 2010 Jun; 83(990): 493– 8. 16. Atsuhiko S, Masahiro M, Hiroki M, Tomohiko U, et al. Trigeminal root entry zone involvement in neuromyelitis optica and multiple sclerosis. Journal of the Neurological Neurosciences. 2015 August; 355: 147– 149. 17. Fischbein NJ, Prados MD, Wara W, et al. Radiologic evaluation of brain stem tumors. Correlation of MRI appearance with clinical outcome. Pediatr Neuro- surg 1996; 24: 9– 23. 18. Brisman R, Kandji AG, Mooji RB. Trigeminal nerve-blood vessel relationship as revealed by high resolution magnetic resonance imaging and its effect on pain relief after gamma knife radiosurgery for trigeminal neuralgia. Neurosurgery 2002; 50: 1261– 6. 19. Tancioni F, Gaetani P, Villani L, et al. Neurinoma of the trigeminal root and atypical trigeminal neuralgia. Surg Neurol 1995; 44: 36– 42.