Clinical Information F69 Adenocarcinoma ampulla of vater 5






- Slides: 22

Clinical Information F/69 Adenocarcinoma, ampulla of vater (5 years ago) CT : multiple intraabdominal lymph node enlargement PET CT: uterus body and cervix, FDG uptake Liquid-Based Preparation
1



13 8, 9
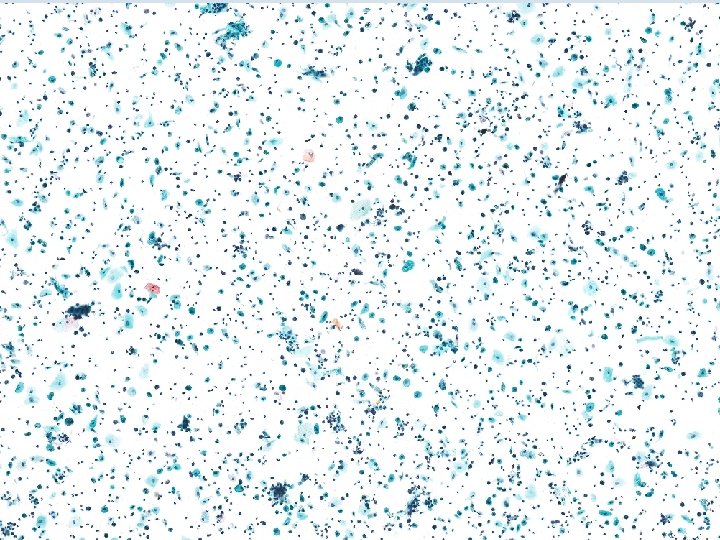
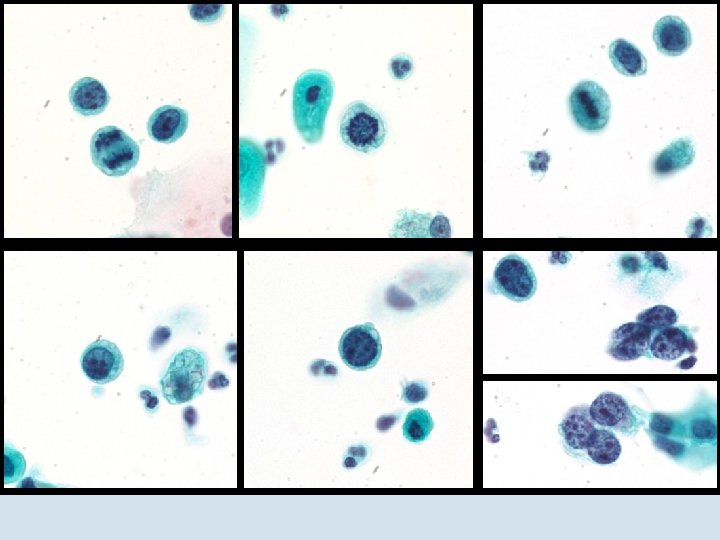
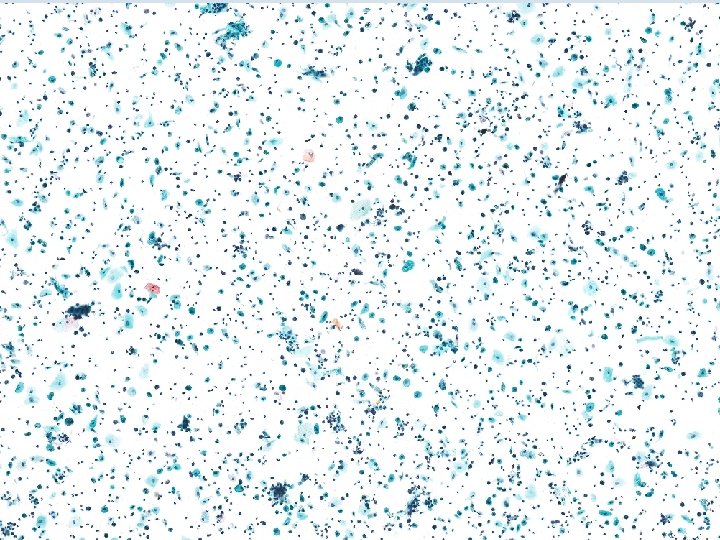
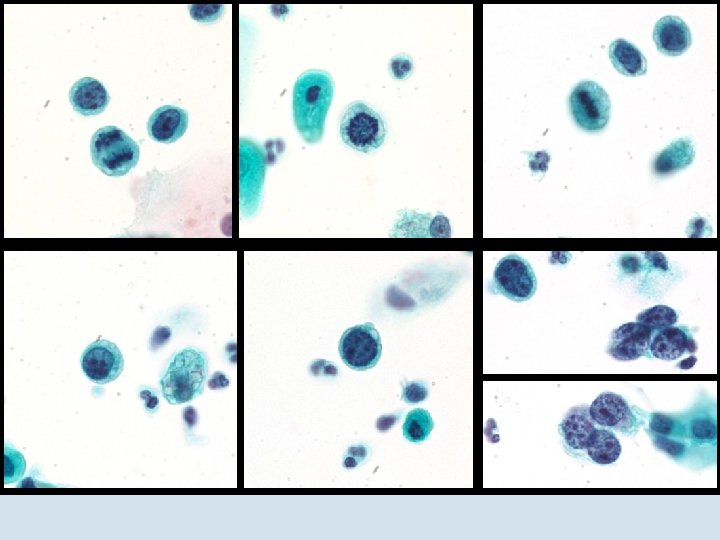
Cytologic Findings high cellularity specimen inflammatory background with normal atrophic squamous and glandular cells Many isolated atypical cells l Round to oval l Large pleomorphic nuclei l Coarse chromatin l Small nucleoli : more than 2 l Irregular nuclear membrane with lobulation l Mitotic activity : frequent ( 3/10 HPFs) l Scanty cytoplasm l Intracytoplasmic vacuole
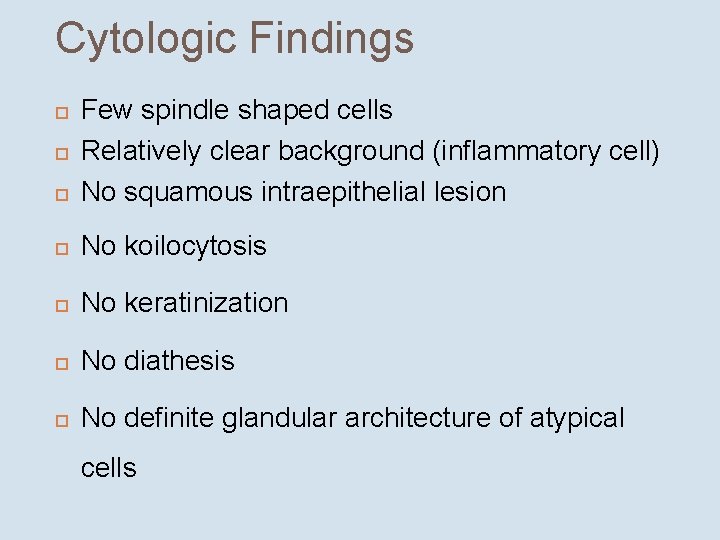
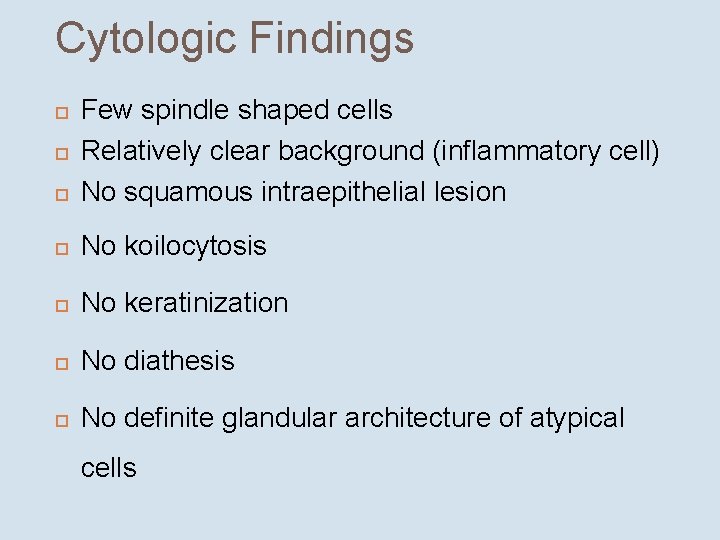
Cytologic Findings Few spindle shaped cells Relatively clear background (inflammatory cell) No squamous intraepithelial lesion No koilocytosis No keratinization No diathesis No definite glandular architecture of atypical cells

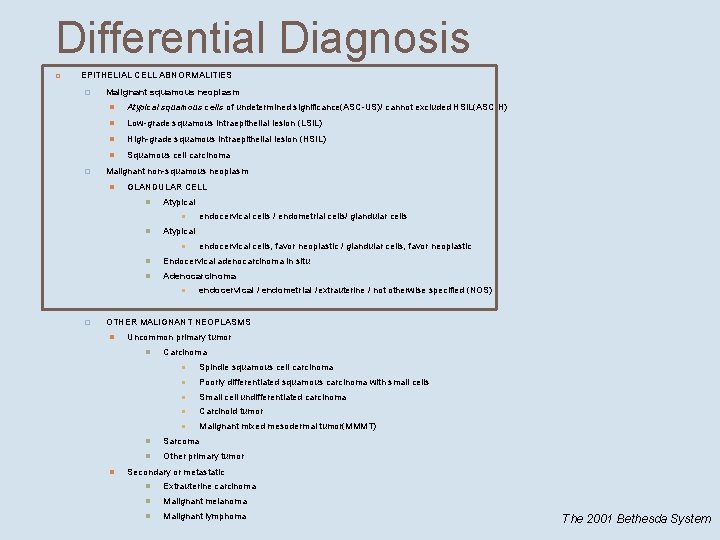
Differential Diagnosis EPITHELIAL CELL ABNORMALITIES � � Malignant squamous neoplasm Atypical squamous cells of undetermined significance(ASC-US)/ cannot excluded HSIL(ASC-H) Low-grade squamous intraepithelial lesion (LSIL) High-grade squamous intraepithelial lesion (HSIL) Squamous cell carcinoma Malignant non-squamous neoplasm GLANDULAR CELL Atypical Endocervical adenocarcinoma in situ Adenocarcinoma � endocervical cells / endometrial cells/ glandular cells endocervical cells, favor neoplastic / glandular cells, favor neoplastic endocervical / endometrial /extrauterine / not otherwise specified (NOS) OTHER MALIGNANT NEOPLASMS Uncommon primary tumor Carcinoma Spindle squamous cell carcinoma Poorly differentiated squamous carcinoma with small cells Small cell undifferentiated carcinoma Carcinoid tumor Malignant mixed mesodermal tumor(MMMT) Sarcoma Other primary tumor Secondary or metastatic Extrauterine carcinoma Malignant melanoma Malignant lymphoma The 2001 Bethesda System
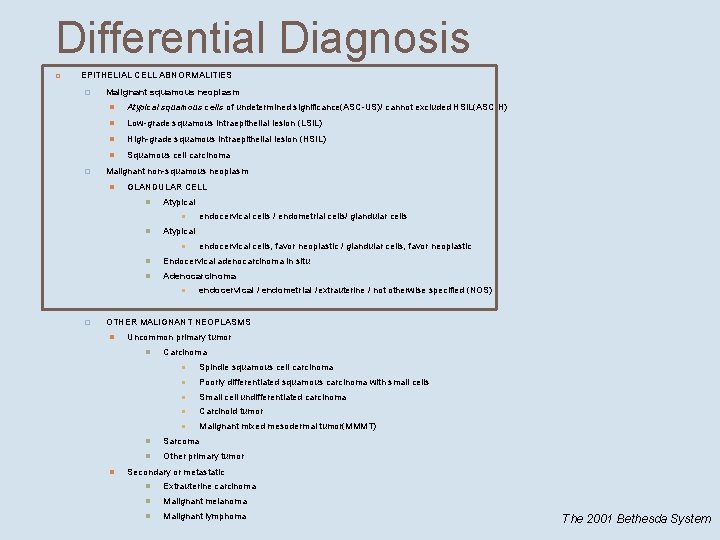
Differential Diagnosis EPITHELIAL CELL ABNORMALITIES � � Malignant squamous neoplasm Atypical squamous cells of undetermined significance(ASC-US)/ cannot excluded HSIL(ASC-H) Low-grade squamous intraepithelial lesion (LSIL) High-grade squamous intraepithelial lesion (HSIL) Squamous cell carcinoma Malignant non-squamous neoplasm GLANDULAR CELL Atypical Endocervical adenocarcinoma in situ Adenocarcinoma � endocervical cells / endometrial cells/ glandular cells endocervical cells, favor neoplastic / glandular cells, favor neoplastic endocervical / endometrial /extrauterine / not otherwise specified (NOS) OTHER MALIGNANT NEOPLASMS Uncommon primary tumor Carcinoma Spindle squamous cell carcinoma Poorly differentiated squamous carcinoma with small cells Small cell undifferentiated carcinoma Carcinoid tumor Malignant mixed mesodermal tumor(MMMT) Sarcoma Other primary tumor Secondary or metastatic Extrauterine carcinoma Malignant melanoma Malignant lymphoma The 2001 Bethesda System
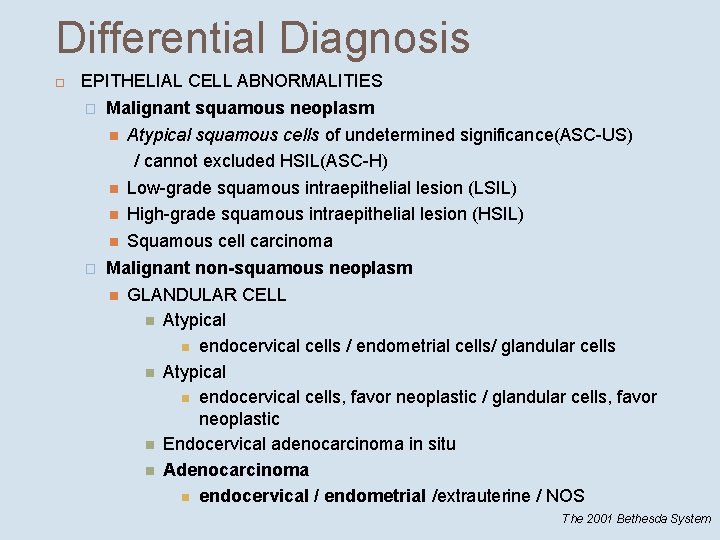
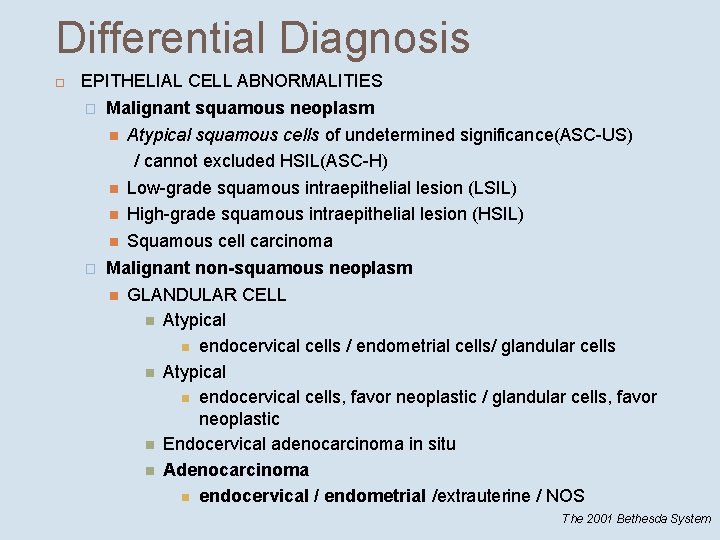
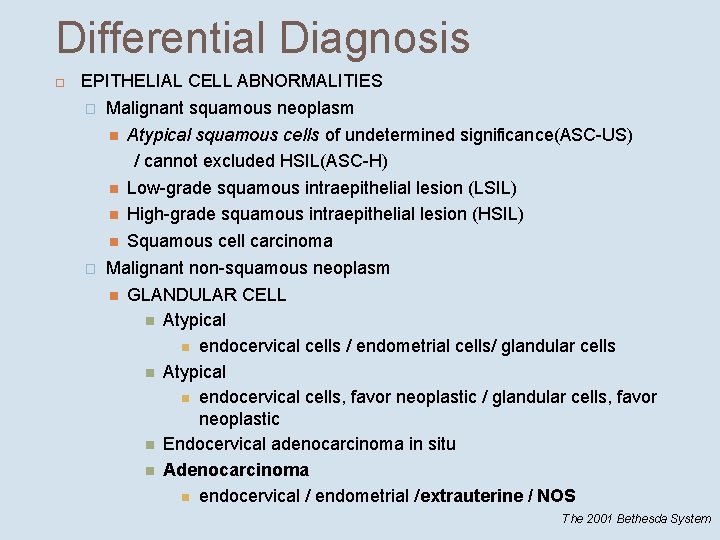
Differential Diagnosis EPITHELIAL CELL ABNORMALITIES � Malignant squamous neoplasm Atypical squamous cells of undetermined significance(ASC-US) / cannot excluded HSIL(ASC-H) Low-grade squamous intraepithelial lesion (LSIL) High-grade squamous intraepithelial lesion (HSIL) Squamous cell carcinoma � Malignant non-squamous neoplasm GLANDULAR CELL Atypical endocervical cells / endometrial cells/ glandular cells Atypical endocervical cells, favor neoplastic / glandular cells, favor neoplastic Endocervical adenocarcinoma in situ Adenocarcinoma endocervical / endometrial /extrauterine / NOS The 2001 Bethesda System
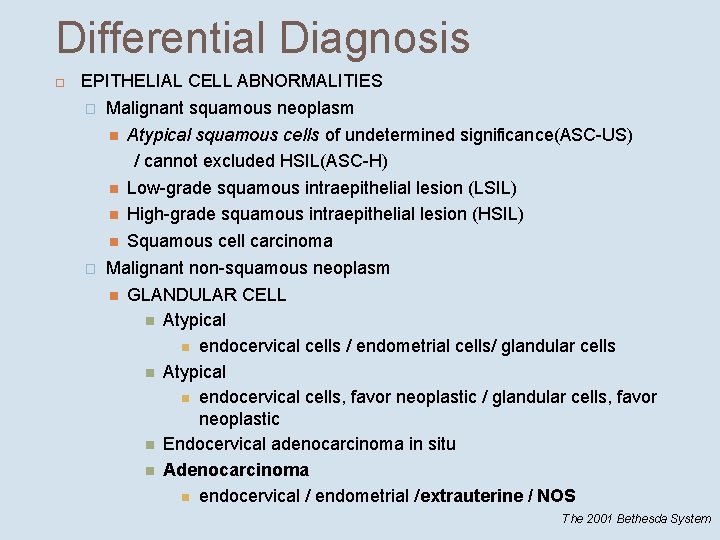
Differential Diagnosis EPITHELIAL CELL ABNORMALITIES � Malignant squamous neoplasm Atypical squamous cells of undetermined significance(ASC-US) / cannot excluded HSIL(ASC-H) Low-grade squamous intraepithelial lesion (LSIL) High-grade squamous intraepithelial lesion (HSIL) Squamous cell carcinoma � Malignant non-squamous neoplasm GLANDULAR CELL Atypical endocervical cells / endometrial cells/ glandular cells Atypical endocervical cells, favor neoplastic / glandular cells, favor neoplastic Endocervical adenocarcinoma in situ Adenocarcinoma endocervical / endometrial /extrauterine / NOS The 2001 Bethesda System
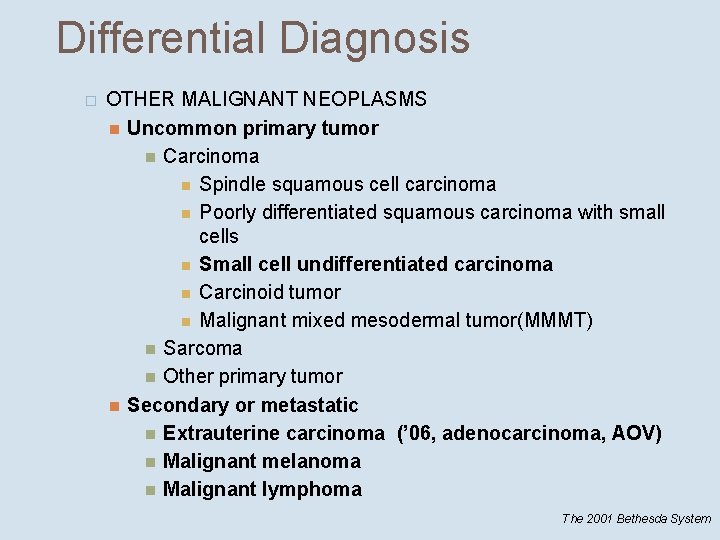
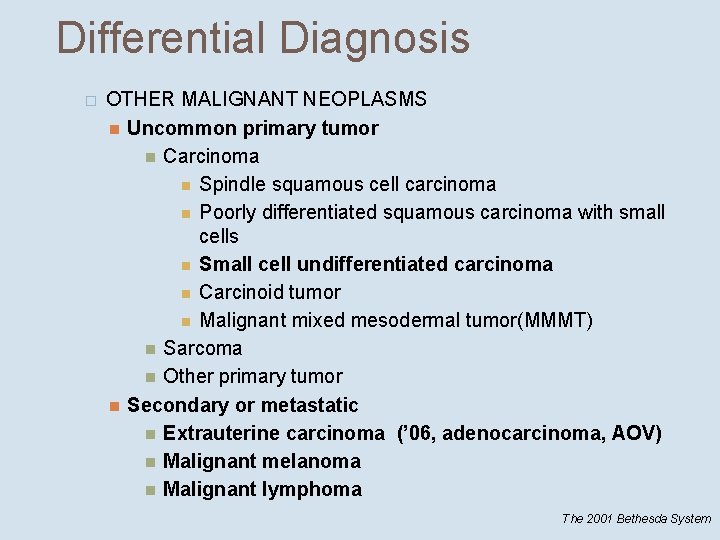
Differential Diagnosis � OTHER MALIGNANT NEOPLASMS Uncommon primary tumor Carcinoma Spindle squamous cell carcinoma Poorly differentiated squamous carcinoma with small cells Small cell undifferentiated carcinoma Carcinoid tumor Malignant mixed mesodermal tumor(MMMT) Sarcoma Other primary tumor Secondary or metastatic Extrauterine carcinoma (’ 06, adenocarcinoma, AOV) Malignant melanoma Malignant lymphoma The 2001 Bethesda System
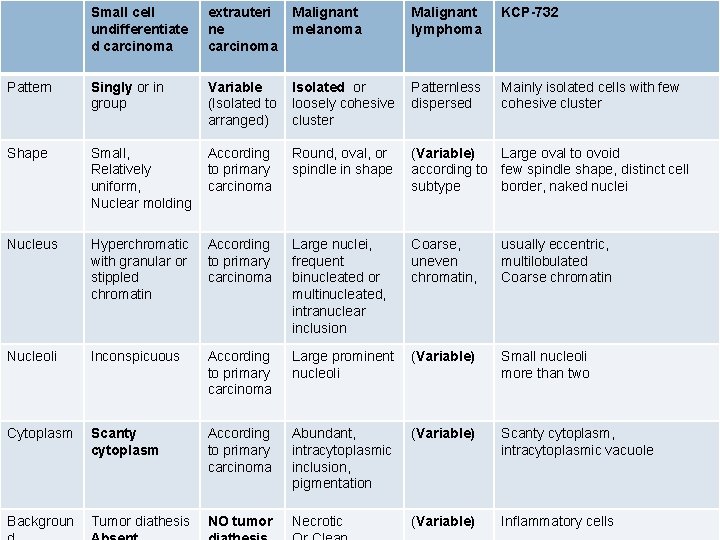
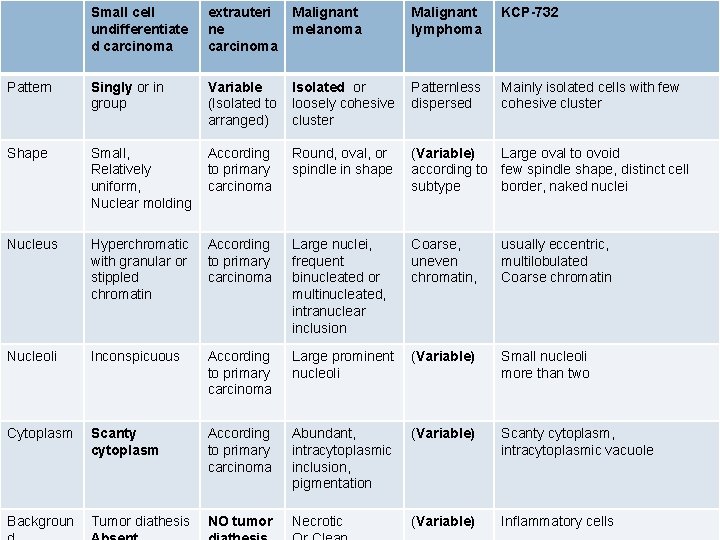
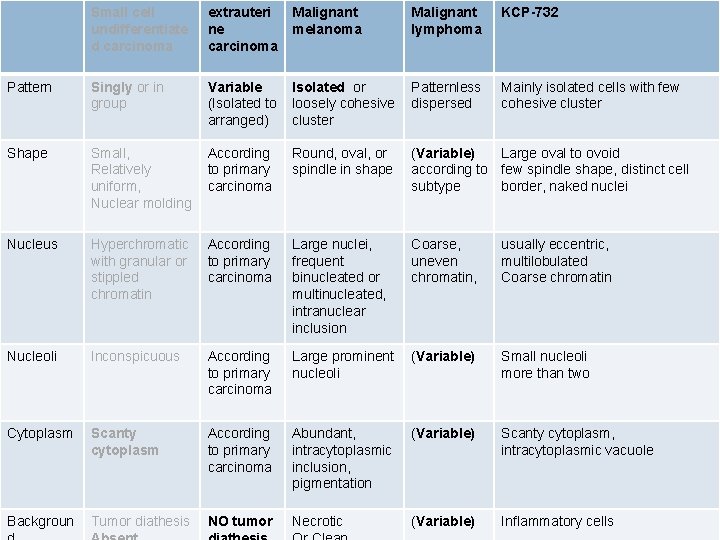
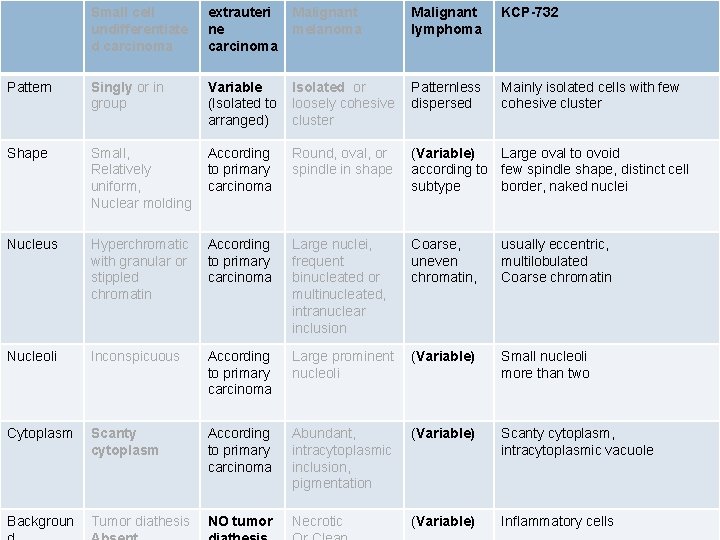
Small cell undifferentiate d carcinoma extrauteri ne carcinoma Malignant melanoma Malignant lymphoma KCP-732 Pattern Singly or in group Variable (Isolated to arranged) Isolated or loosely cohesive cluster Patternless dispersed Mainly isolated cells with few cohesive cluster Shape Small, Relatively uniform, Nuclear molding According to primary carcinoma Round, oval, or spindle in shape (Variable) Large oval to ovoid according to few spindle shape, distinct cell subtype border, naked nuclei Nucleus Hyperchromatic with granular or stippled chromatin According to primary carcinoma Large nuclei, frequent binucleated or multinucleated, intranuclear inclusion Coarse, uneven chromatin, usually eccentric, multilobulated Coarse chromatin Nucleoli Inconspicuous According to primary carcinoma Large prominent nucleoli (Variable) Small nucleoli more than two Cytoplasm Scanty cytoplasm According to primary carcinoma Abundant, intracytoplasmic inclusion, pigmentation (Variable) Scanty cytoplasm, intracytoplasmic vacuole Backgroun Tumor diathesis NO tumor Necrotic (Variable) Inflammatory cells
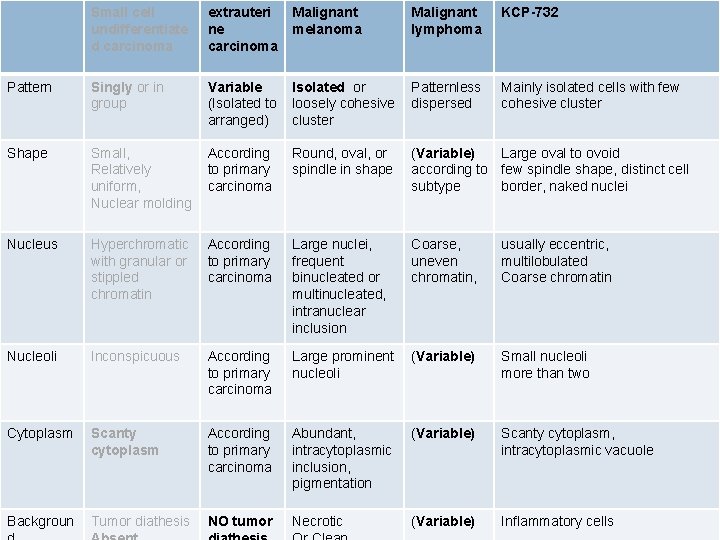
Small cell undifferentiate d carcinoma extrauteri ne carcinoma Malignant melanoma Malignant lymphoma KCP-732 Pattern Singly or in group Variable (Isolated to arranged) Isolated or loosely cohesive cluster Patternless dispersed Mainly isolated cells with few cohesive cluster Shape Small, Relatively uniform, Nuclear molding According to primary carcinoma Round, oval, or spindle in shape (Variable) Large oval to ovoid according to few spindle shape, distinct cell subtype border, naked nuclei Nucleus Hyperchromatic with granular or stippled chromatin According to primary carcinoma Large nuclei, frequent binucleated or multinucleated, intranuclear inclusion Coarse, uneven chromatin, usually eccentric, multilobulated Coarse chromatin Nucleoli Inconspicuous According to primary carcinoma Large prominent nucleoli (Variable) Small nucleoli more than two Cytoplasm Scanty cytoplasm According to primary carcinoma Abundant, intracytoplasmic inclusion, pigmentation (Variable) Scanty cytoplasm, intracytoplasmic vacuole Backgroun Tumor diathesis NO tumor Necrotic (Variable) Inflammatory cells
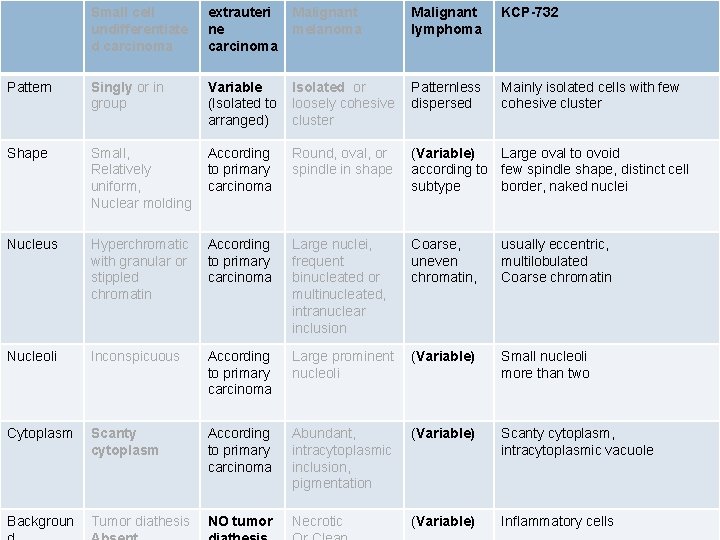
Small cell undifferentiate d carcinoma extrauteri ne carcinoma Malignant melanoma Malignant lymphoma KCP-732 Pattern Singly or in group Variable (Isolated to arranged) Isolated or loosely cohesive cluster Patternless dispersed Mainly isolated cells with few cohesive cluster Shape Small, Relatively uniform, Nuclear molding According to primary carcinoma Round, oval, or spindle in shape (Variable) Large oval to ovoid according to few spindle shape, distinct cell subtype border, naked nuclei Nucleus Hyperchromatic with granular or stippled chromatin According to primary carcinoma Large nuclei, frequent binucleated or multinucleated, intranuclear inclusion Coarse, uneven chromatin, usually eccentric, multilobulated Coarse chromatin Nucleoli Inconspicuous According to primary carcinoma Large prominent nucleoli (Variable) Small nucleoli more than two Cytoplasm Scanty cytoplasm According to primary carcinoma Abundant, intracytoplasmic inclusion, pigmentation (Variable) Scanty cytoplasm, intracytoplasmic vacuole Backgroun Tumor diathesis NO tumor Necrotic (Variable) Inflammatory cells
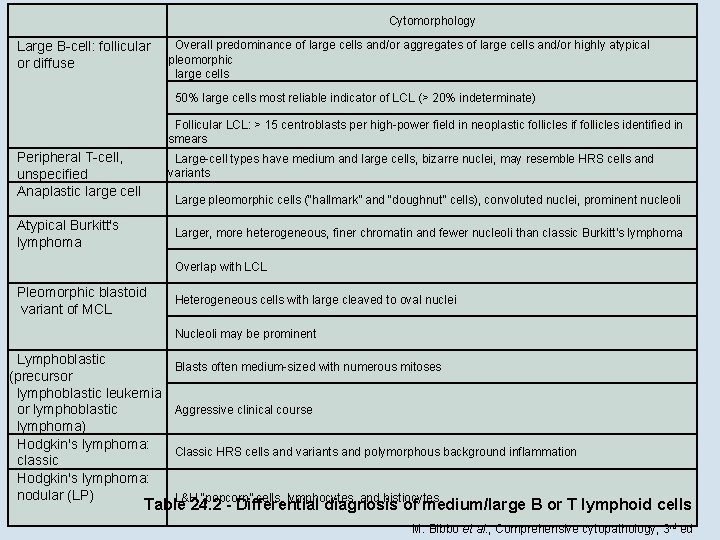
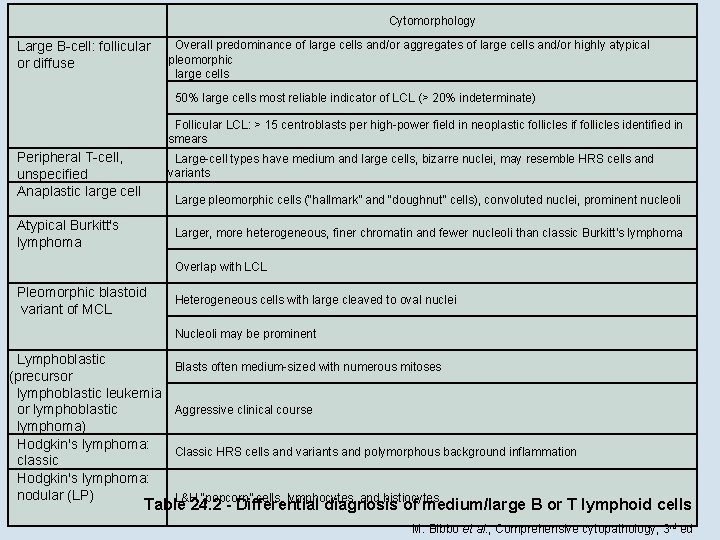
Cytomorphology Large B-cell: follicular or diffuse Overall predominance of large cells and/or aggregates of large cells and/or highly atypical pleomorphic large cells 50% large cells most reliable indicator of LCL (> 20% indeterminate) Follicular LCL: > 15 centroblasts per high-power field in neoplastic follicles if follicles identified in smears Peripheral T-cell, unspecified Anaplastic large cell Large-cell types have medium and large cells, bizarre nuclei, may resemble HRS cells and variants Large pleomorphic cells (“hallmark” and “doughnut” cells), convoluted nuclei, prominent nucleoli Atypical Burkitt's lymphoma Larger, more heterogeneous, finer chromatin and fewer nucleoli than classic Burkitt's lymphoma Overlap with LCL Pleomorphic blastoid variant of MCL Heterogeneous cells with large cleaved to oval nuclei Nucleoli may be prominent Lymphoblastic (precursor lymphoblastic leukemia or lymphoblastic lymphoma) Hodgkin's lymphoma: classic Hodgkin's lymphoma: nodular (LP) Blasts often medium-sized with numerous mitoses Aggressive clinical course Classic HRS cells and variants and polymorphous background inflammation L&H “popcorn” cells, lymphocytes, and histiocytes Table 24. 2 - Differential diagnosis of medium/large B or T lymphoid cells M. Bibbo et al. , Comprehensive cytopathology, 3 rd ed
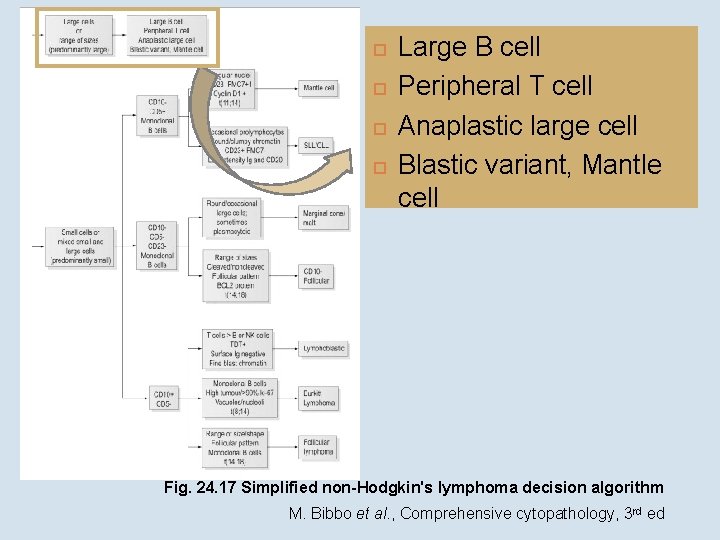
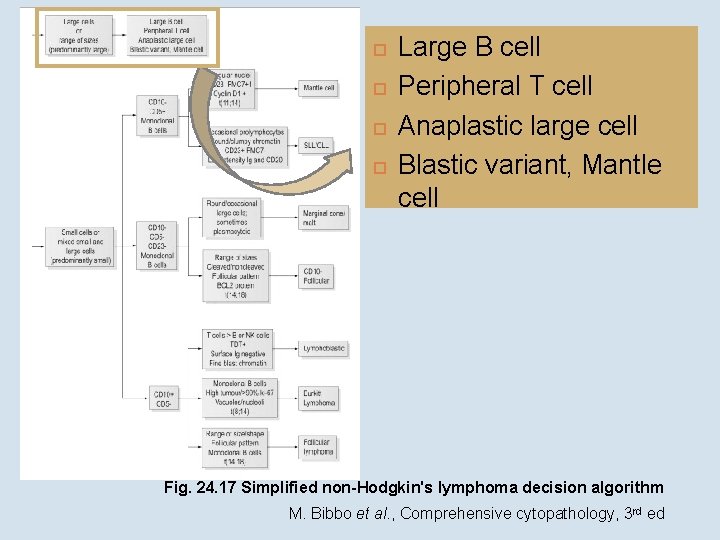
Large B cell Peripheral T cell Anaplastic large cell Blastic variant, Mantle cell Fig. 24. 17 Simplified non-Hodgkin's lymphoma decision algorithm M. Bibbo et al. , Comprehensive cytopathology, 3 rd ed
Large round centroblasts Nuclei are slightly irregular with several small nucleoli Cytoplasm is scanty and a few vacuoles - W. Gray et al. , Diagnostic cytopathology 3 rd ed
Diagnosis Malignant large cell lymphoma

 Cold opposite warm same
Cold opposite warm same Uterus ostia
Uterus ostia Ampulla anatomy ear
Ampulla anatomy ear Perirectal fascia
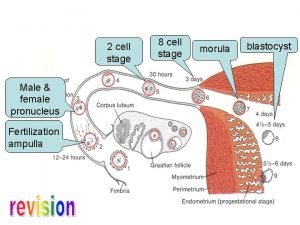
Perirectal fascia Fertilization ampulla
Fertilization ampulla Ligamentum pubocervicale
Ligamentum pubocervicale Ectocervix
Ectocervix Anteversion vs anteflexion
Anteversion vs anteflexion Hepatopancreatic ampulla.
Hepatopancreatic ampulla. Chemoreception
Chemoreception Starfish aboral view
Starfish aboral view Spiny skin
Spiny skin Sulcus salivarius
Sulcus salivarius Plica semilunaris large intestine
Plica semilunaris large intestine Adenocarcinoma
Adenocarcinoma Prostatic adenocarcinoma
Prostatic adenocarcinoma Adenocarcinoma
Adenocarcinoma Md frcpc definition
Md frcpc definition Adenocarcinoma
Adenocarcinoma Adenocarcinoma pancreatico
Adenocarcinoma pancreatico Signo del doble conducto
Signo del doble conducto Progesterone breakthrough bleeding
Progesterone breakthrough bleeding Adenocarcinoma
Adenocarcinoma