Circulating portion of the extracellular fluid 25 of
- Slides: 29
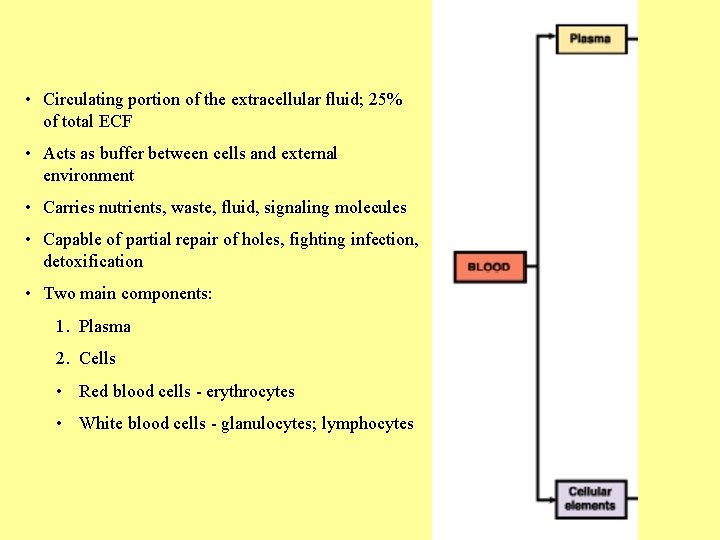
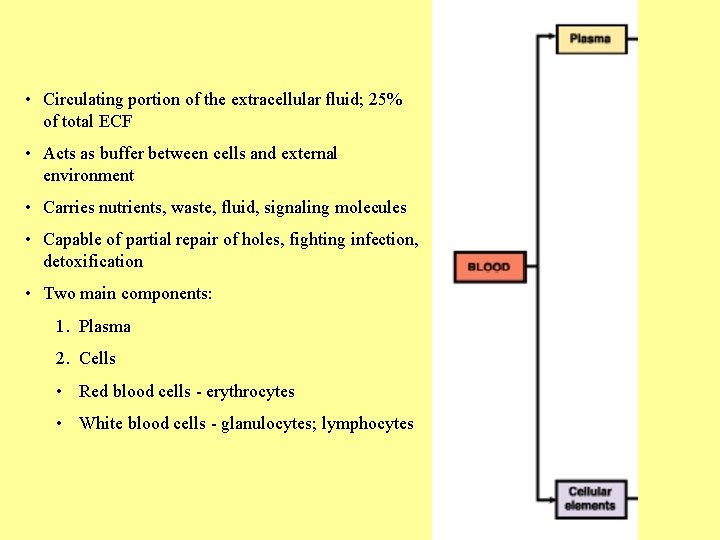
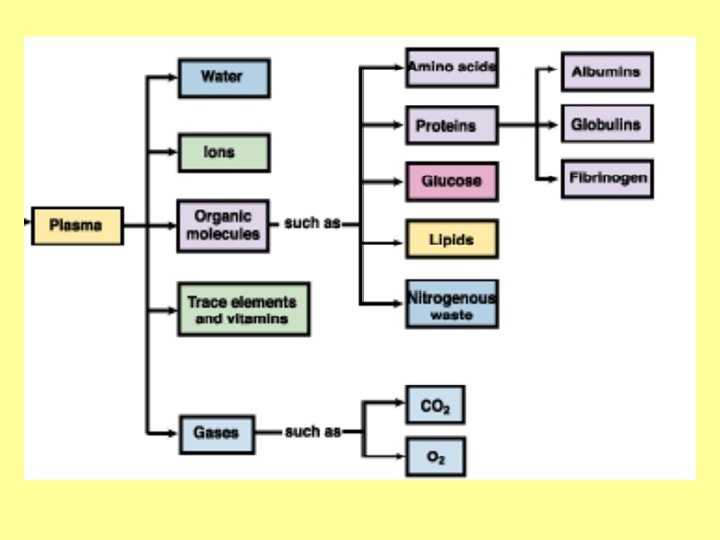
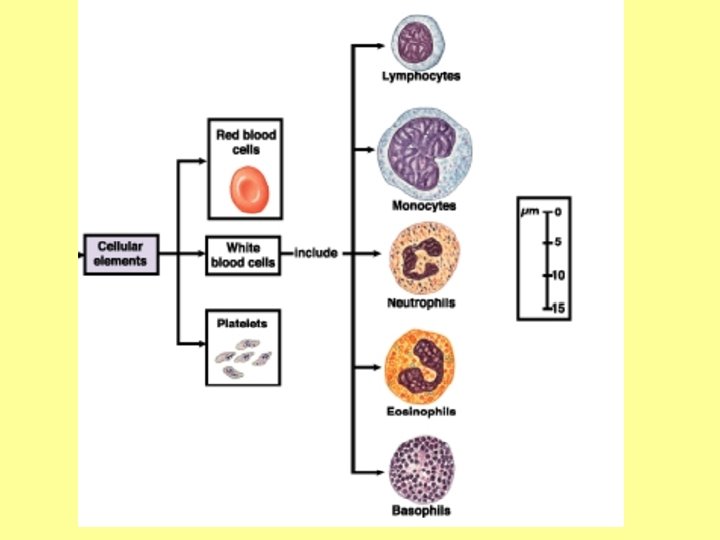
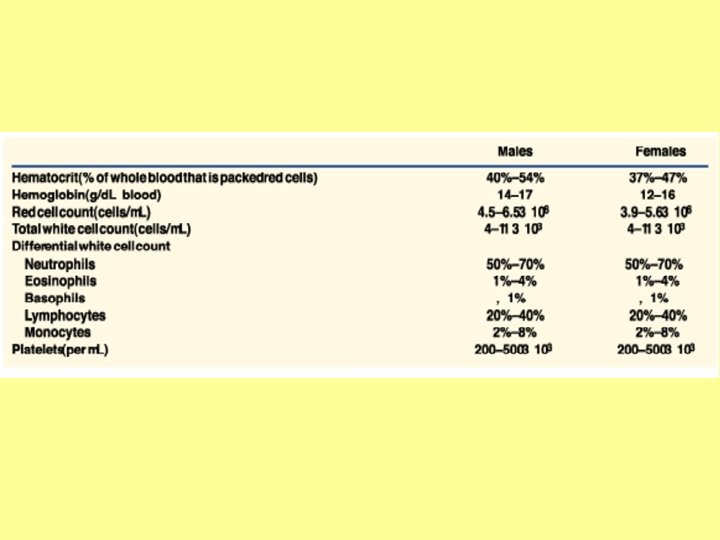
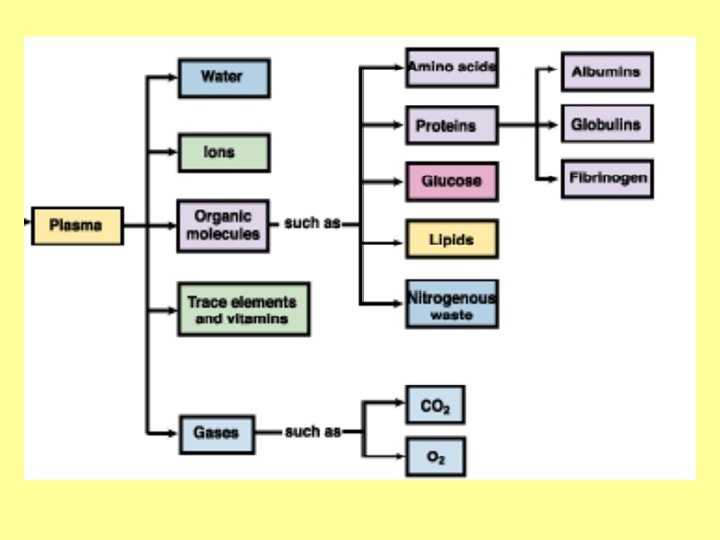
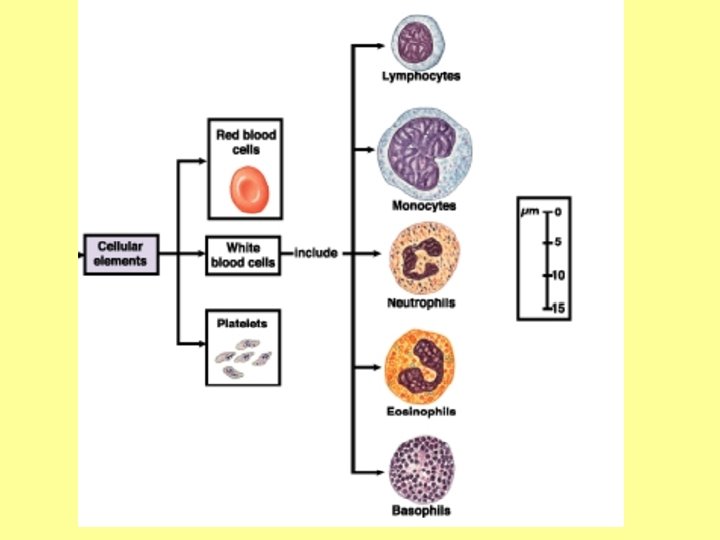
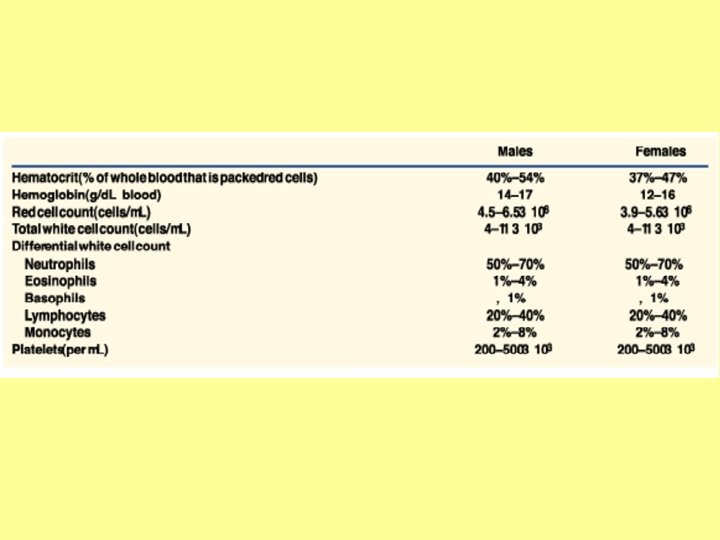
• Circulating portion of the extracellular fluid; 25% of total ECF • Acts as buffer between cells and external environment • Carries nutrients, waste, fluid, signaling molecules • Capable of partial repair of holes, fighting infection, detoxification • Two main components: 1. Plasma 2. Cells • Red blood cells - erythrocytes • White blood cells - glanulocytes; lymphocytes
What do you know? • When referring to a mixture of gasses, we say that each gas has its own partial pressure. What does this mean? • What is the percentage of O 2 in the air that we breathe? What is the percentage in the air on top of Mt. Everest? • What effects do the following have on O 2 binding to hemoglobin? • Temperature increase • Increase in altitude + additional 2, 3 DPG • Increased H+ concentration
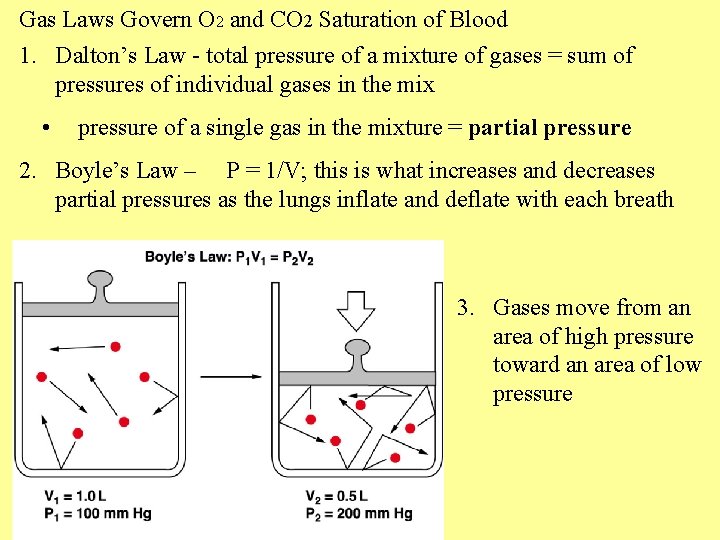
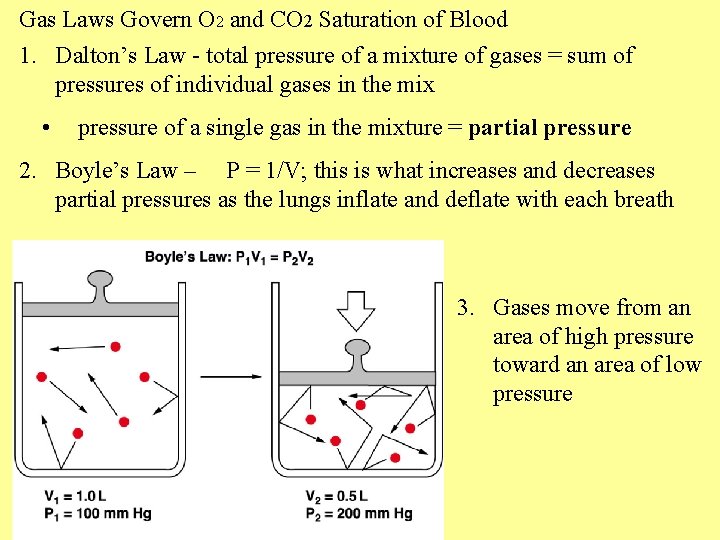
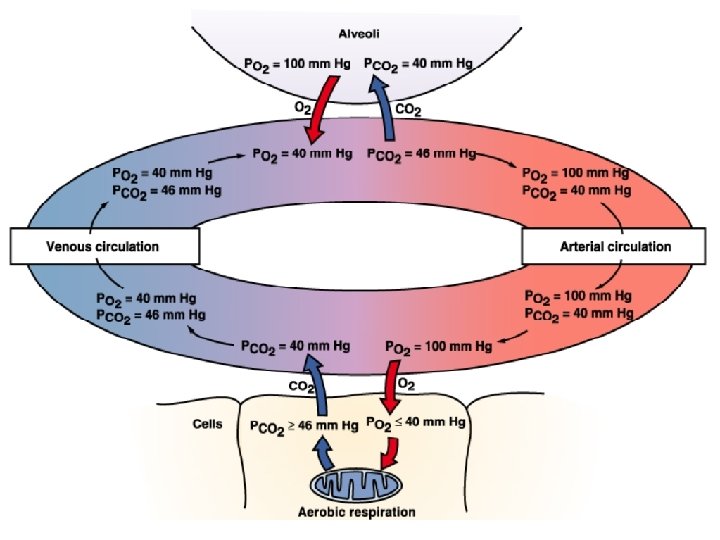
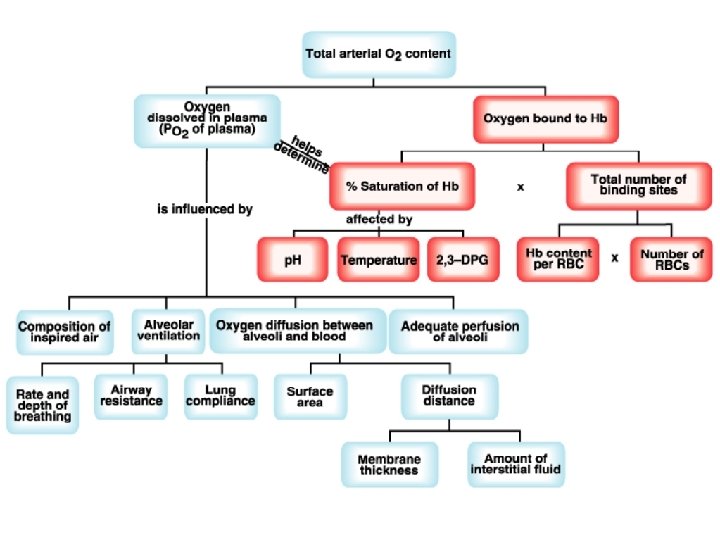
Gas Laws Govern O 2 and CO 2 Saturation of Blood 1. Dalton’s Law - total pressure of a mixture of gases = sum of pressures of individual gases in the mix • pressure of a single gas in the mixture = partial pressure 2. Boyle’s Law – P = 1/V; this is what increases and decreases partial pressures as the lungs inflate and deflate with each breath 3. Gases move from an area of high pressure toward an area of low pressure
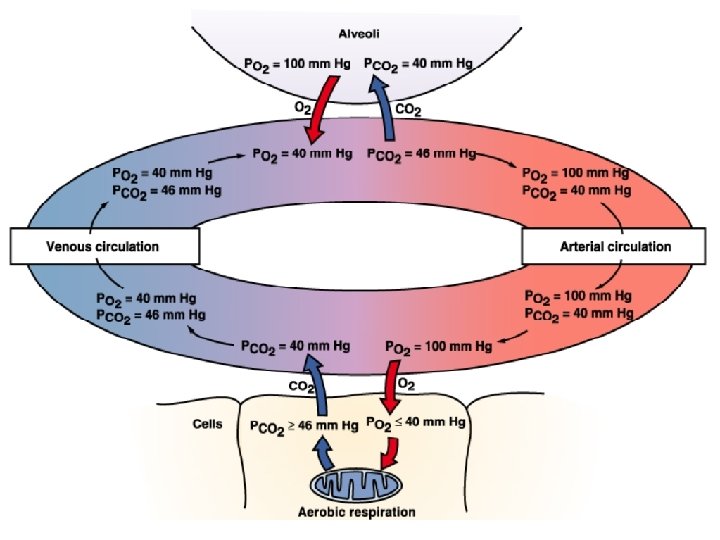
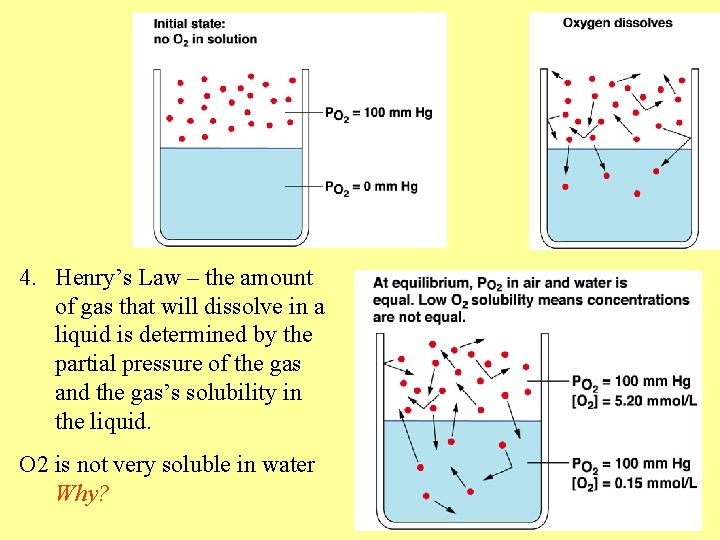
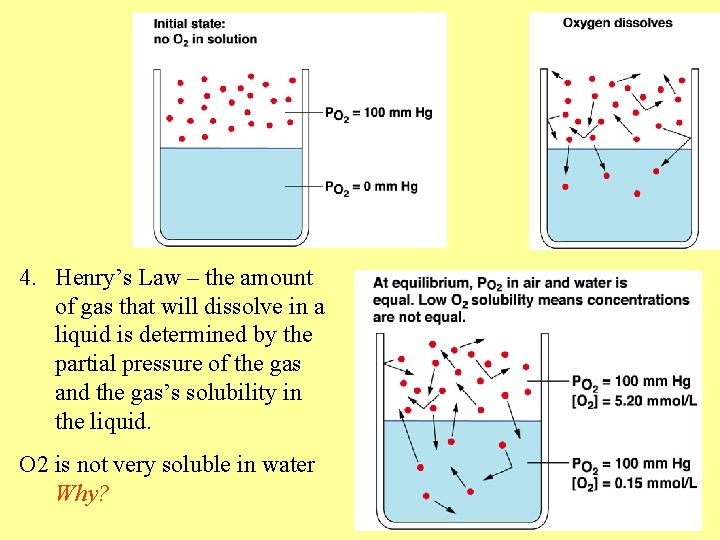
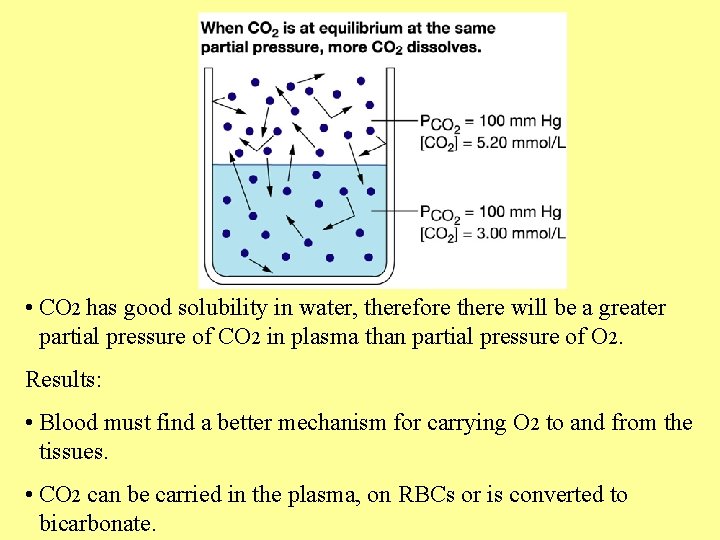
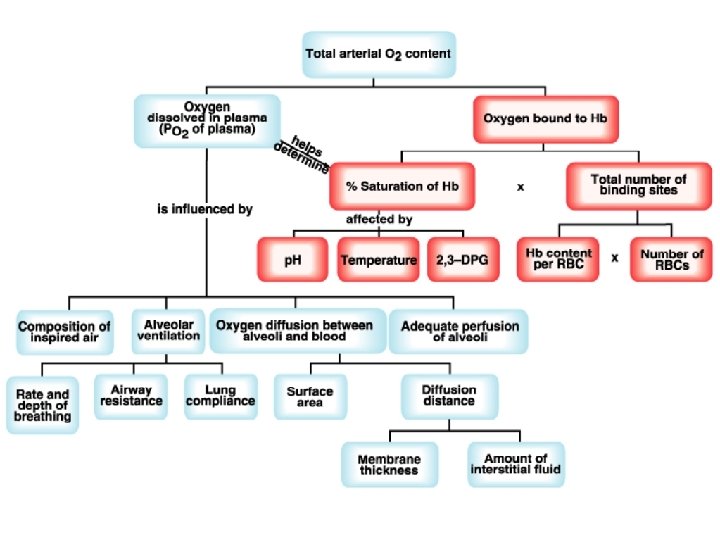
4. Henry’s Law – the amount of gas that will dissolve in a liquid is determined by the partial pressure of the gas and the gas’s solubility in the liquid. O 2 is not very soluble in water Why?
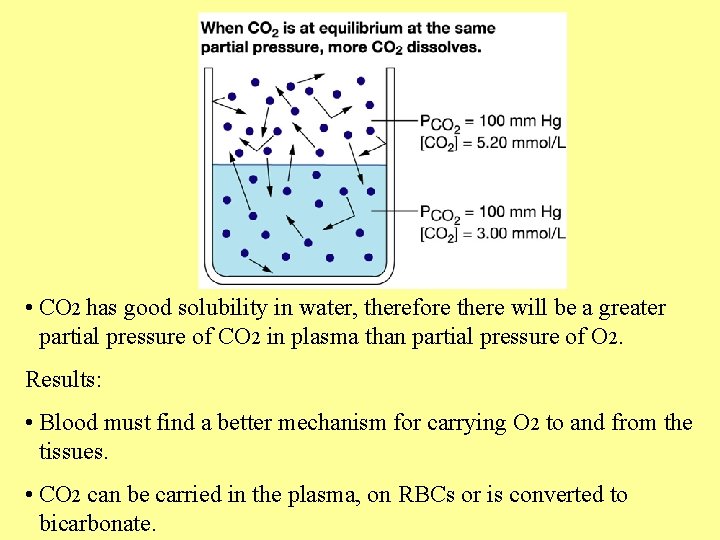
• CO 2 has good solubility in water, therefore there will be a greater partial pressure of CO 2 in plasma than partial pressure of O 2. Results: • Blood must find a better mechanism for carrying O 2 to and from the tissues. • CO 2 can be carried in the plasma, on RBCs or is converted to bicarbonate.
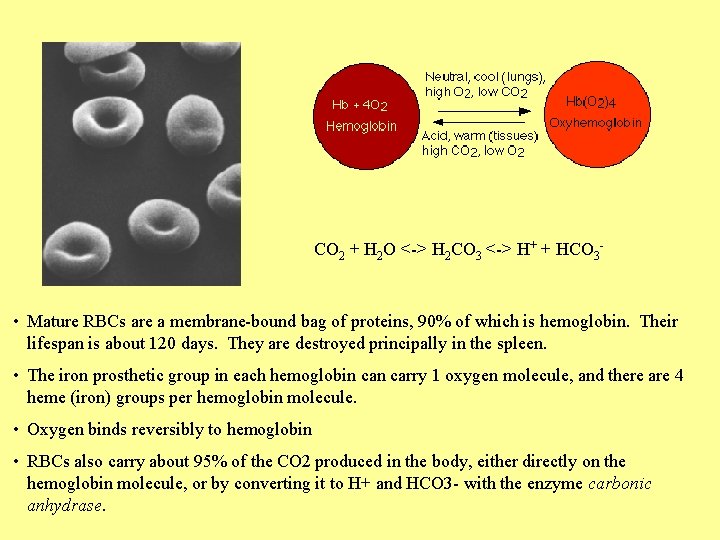
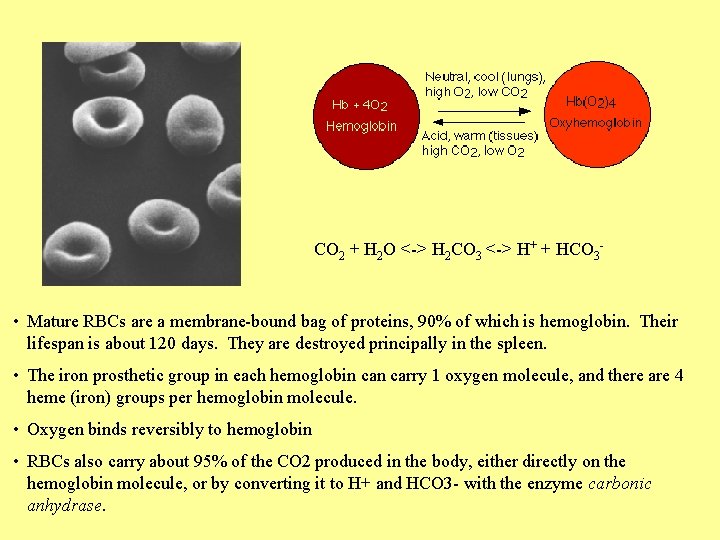
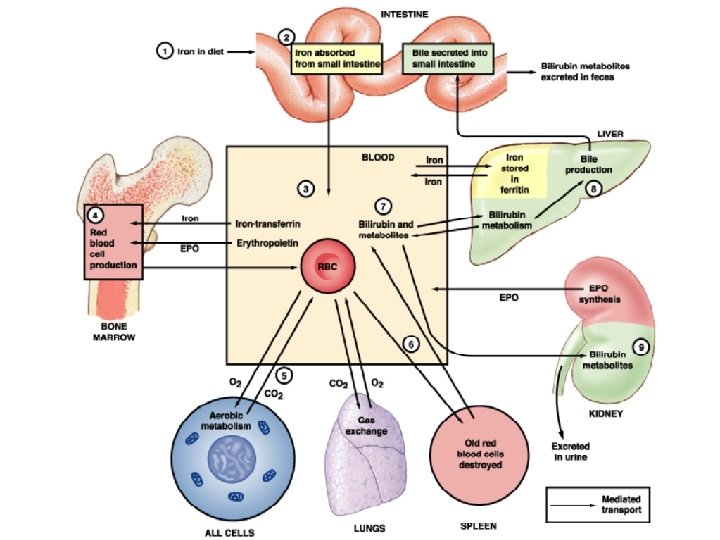
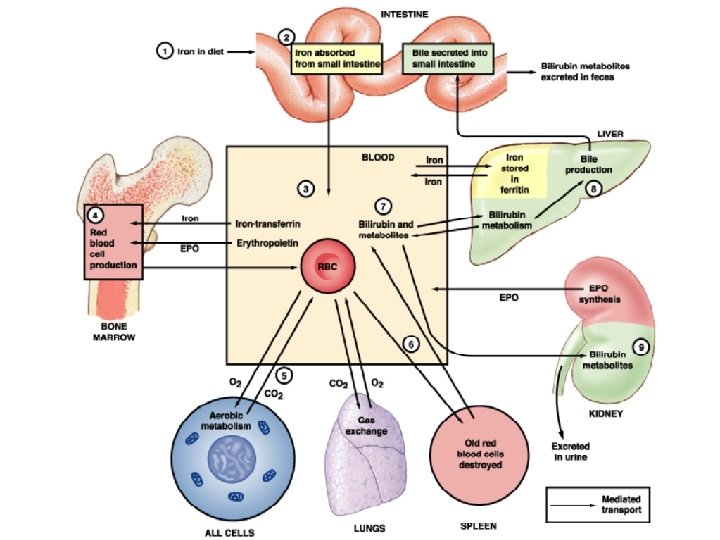
CO 2 + H 2 O <-> H 2 CO 3 <-> H+ + HCO 3 - • Mature RBCs are a membrane-bound bag of proteins, 90% of which is hemoglobin. Their lifespan is about 120 days. They are destroyed principally in the spleen. • The iron prosthetic group in each hemoglobin carry 1 oxygen molecule, and there are 4 heme (iron) groups per hemoglobin molecule. • Oxygen binds reversibly to hemoglobin • RBCs also carry about 95% of the CO 2 produced in the body, either directly on the hemoglobin molecule, or by converting it to H+ and HCO 3 - with the enzyme carbonic anhydrase.
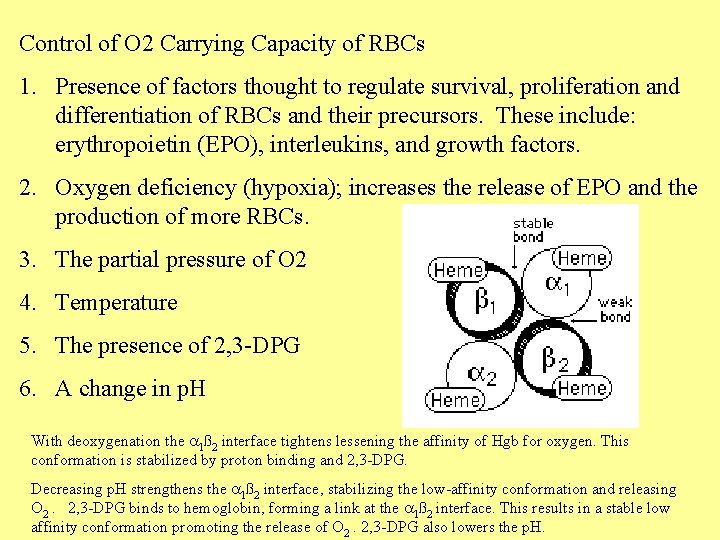
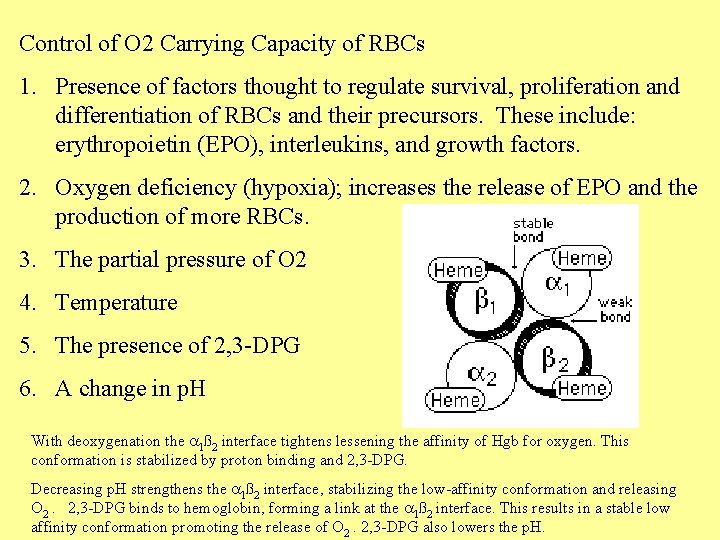
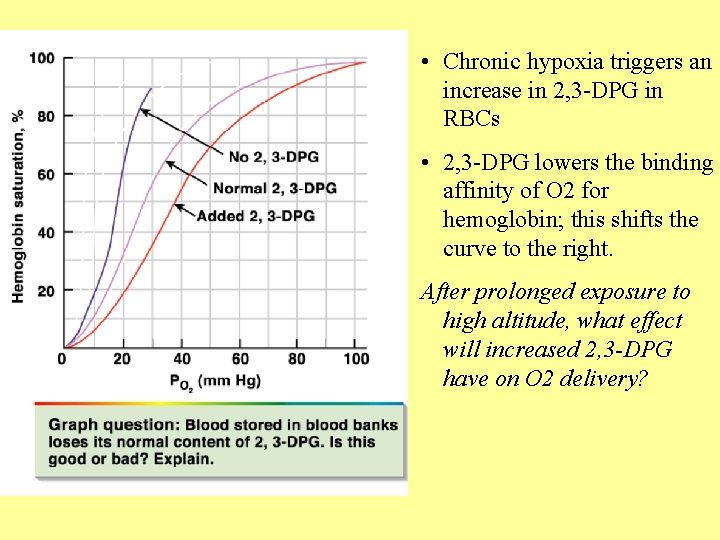
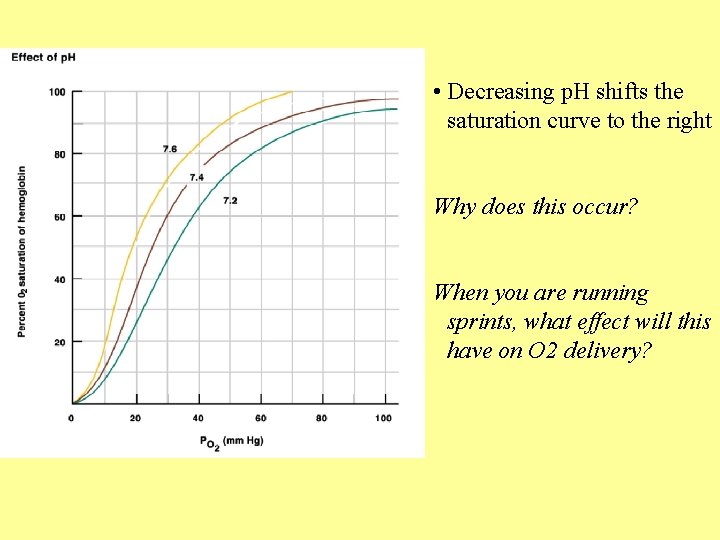
Control of O 2 Carrying Capacity of RBCs 1. Presence of factors thought to regulate survival, proliferation and differentiation of RBCs and their precursors. These include: erythropoietin (EPO), interleukins, and growth factors. 2. Oxygen deficiency (hypoxia); increases the release of EPO and the production of more RBCs. 3. The partial pressure of O 2 4. Temperature 5. The presence of 2, 3 -DPG 6. A change in p. H With deoxygenation the a 1ß 2 interface tightens lessening the affinity of Hgb for oxygen. This conformation is stabilized by proton binding and 2, 3 -DPG. Decreasing p. H strengthens the a 1ß 2 interface, stabilizing the low-affinity conformation and releasing O 2. 2, 3 -DPG binds to hemoglobin, forming a link at the a 1ß 2 interface. This results in a stable low affinity conformation promoting the release of O 2. 2, 3 -DPG also lowers the p. H.
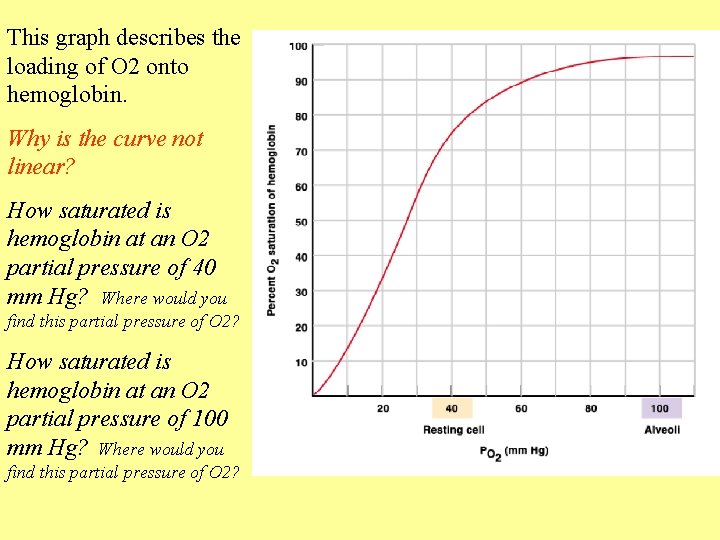
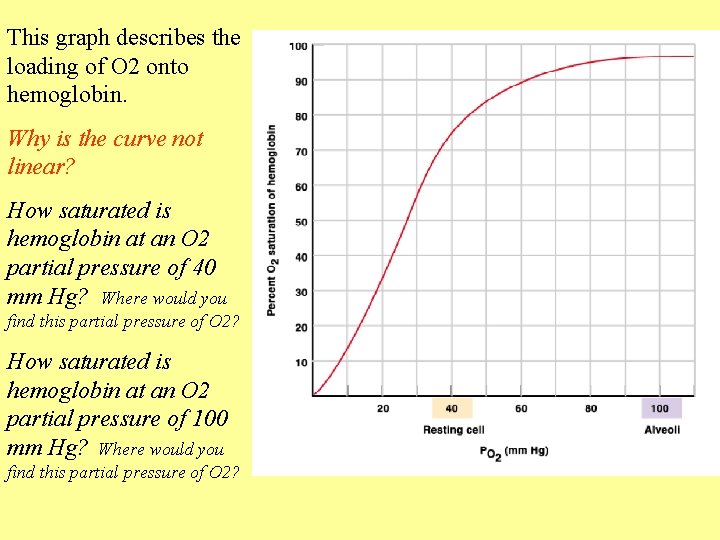
This graph describes the loading of O 2 onto hemoglobin. Why is the curve not linear? How saturated is hemoglobin at an O 2 partial pressure of 40 mm Hg? Where would you find this partial pressure of O 2? How saturated is hemoglobin at an O 2 partial pressure of 100 mm Hg? Where would you find this partial pressure of O 2?
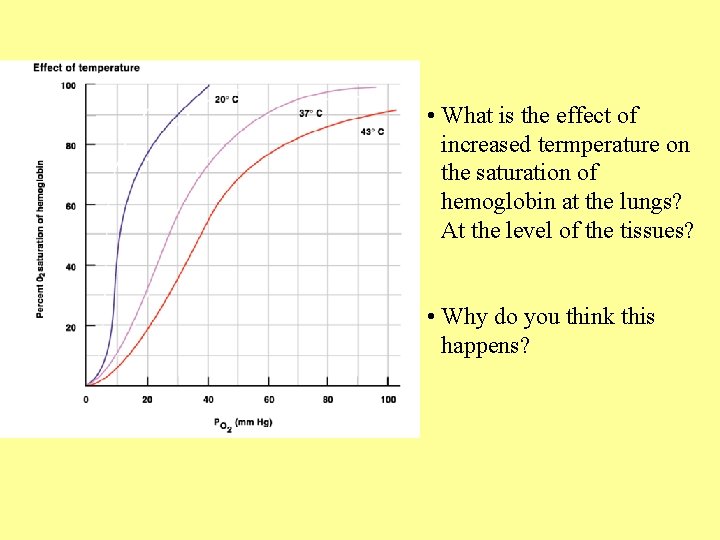
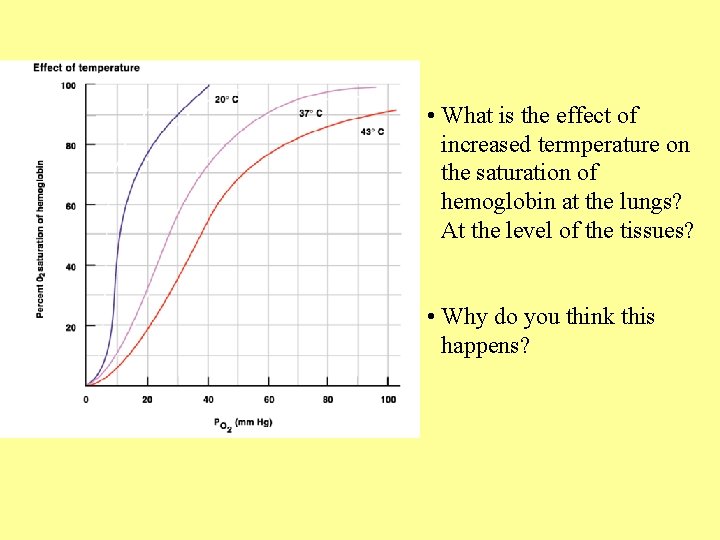
• What is the effect of increased termperature on the saturation of hemoglobin at the lungs? At the level of the tissues? • Why do you think this happens?
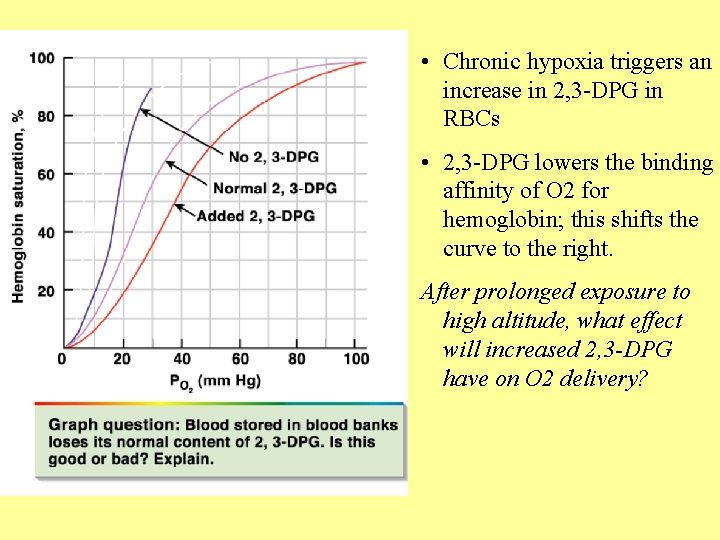
• Chronic hypoxia triggers an increase in 2, 3 -DPG in RBCs • 2, 3 -DPG lowers the binding affinity of O 2 for hemoglobin; this shifts the curve to the right. After prolonged exposure to high altitude, what effect will increased 2, 3 -DPG have on O 2 delivery?
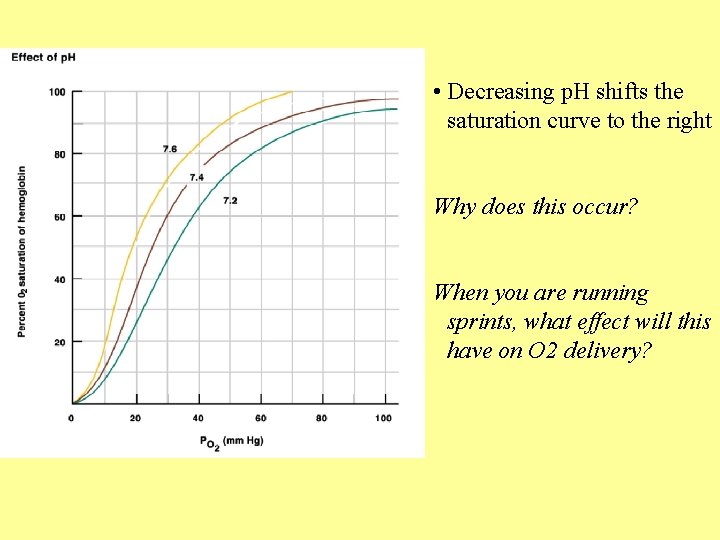
• Decreasing p. H shifts the saturation curve to the right Why does this occur? When you are running sprints, what effect will this have on O 2 delivery?
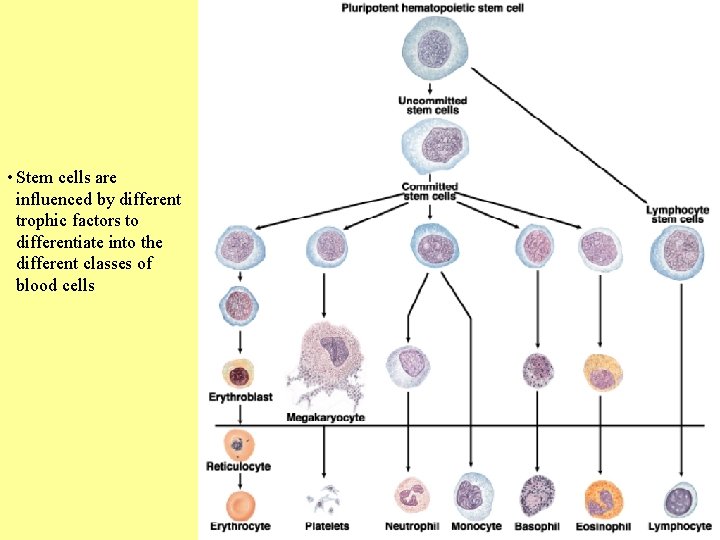
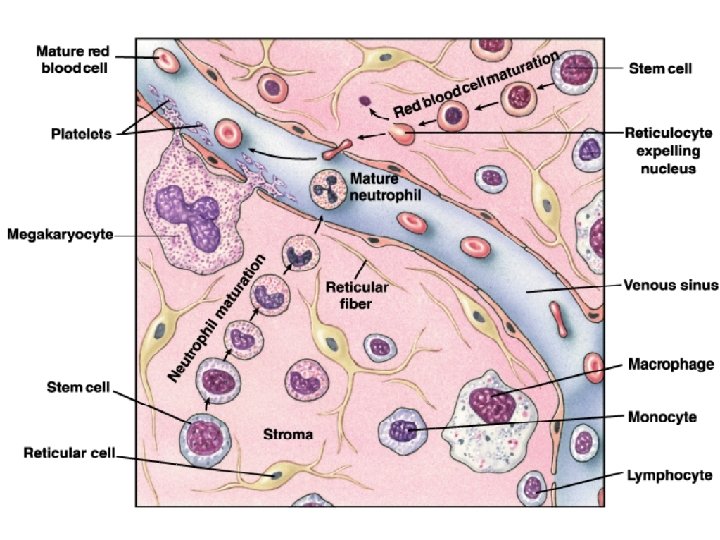
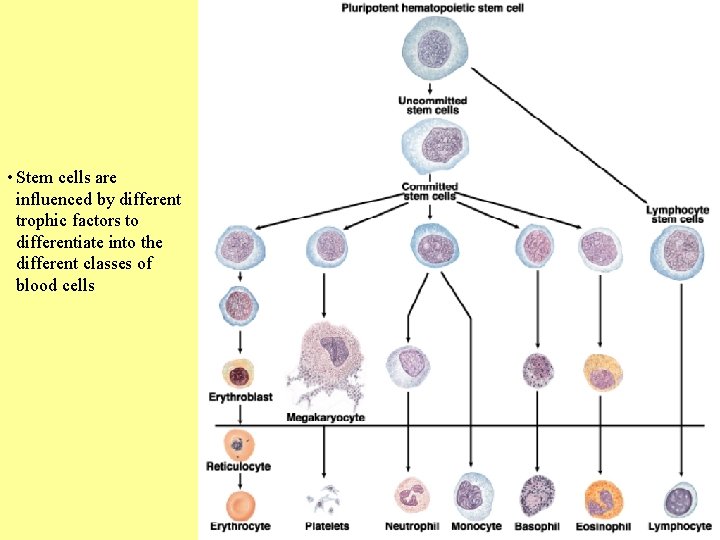
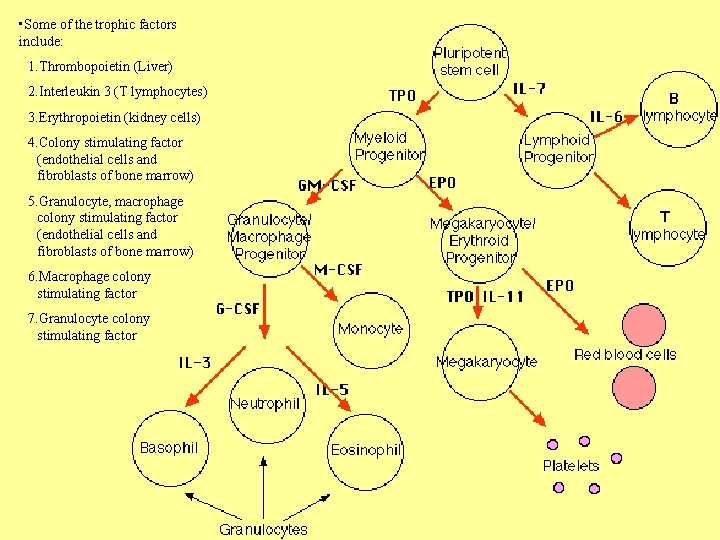
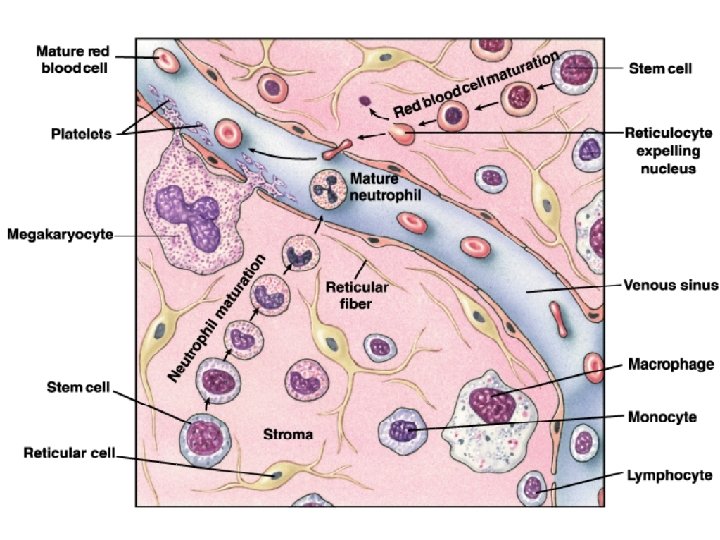
• Stem cells are influenced by different trophic factors to differentiate into the different classes of blood cells
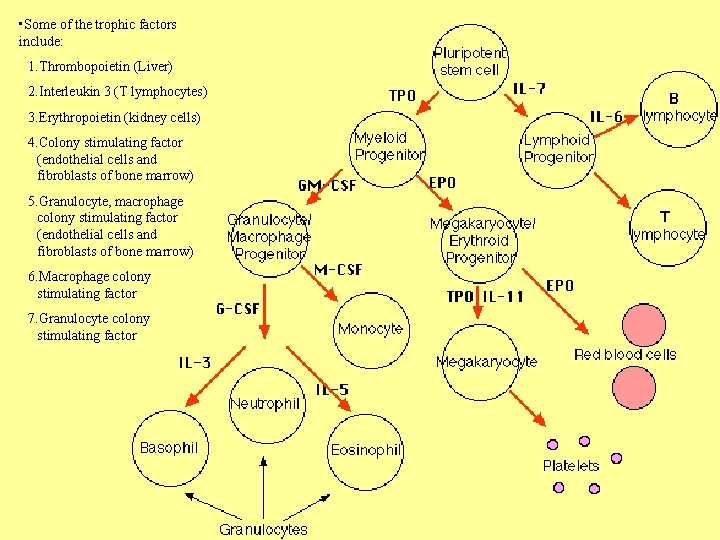
• Some of the trophic factors include: 1. Thrombopoietin (Liver) 2. Interleukin 3 (T lymphocytes) 3. Erythropoietin (kidney cells) 4. Colony stimulating factor (endothelial cells and fibroblasts of bone marrow) 5. Granulocyte, macrophage colony stimulating factor (endothelial cells and fibroblasts of bone marrow) 6. Macrophage colony stimulating factor 7. Granulocyte colony stimulating factor
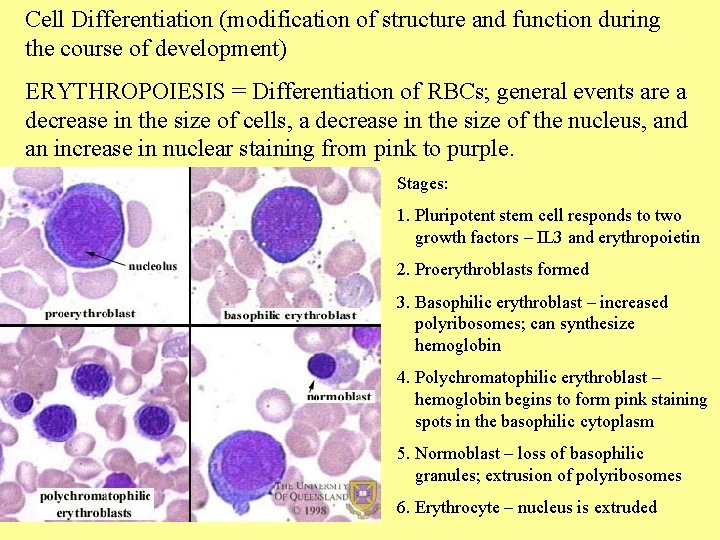
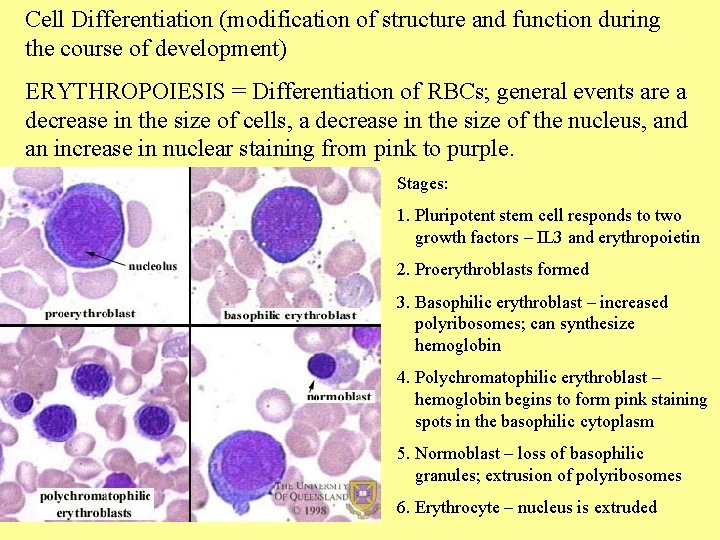
Cell Differentiation (modification of structure and function during the course of development) ERYTHROPOIESIS = Differentiation of RBCs; general events are a decrease in the size of cells, a decrease in the size of the nucleus, and an increase in nuclear staining from pink to purple. Stages: 1. Pluripotent stem cell responds to two growth factors – IL 3 and erythropoietin 2. Proerythroblasts formed 3. Basophilic erythroblast – increased polyribosomes; can synthesize hemoglobin 4. Polychromatophilic erythroblast – hemoglobin begins to form pink staining spots in the basophilic cytoplasm 5. Normoblast – loss of basophilic granules; extrusion of polyribosomes 6. Erythrocyte – nucleus is extruded
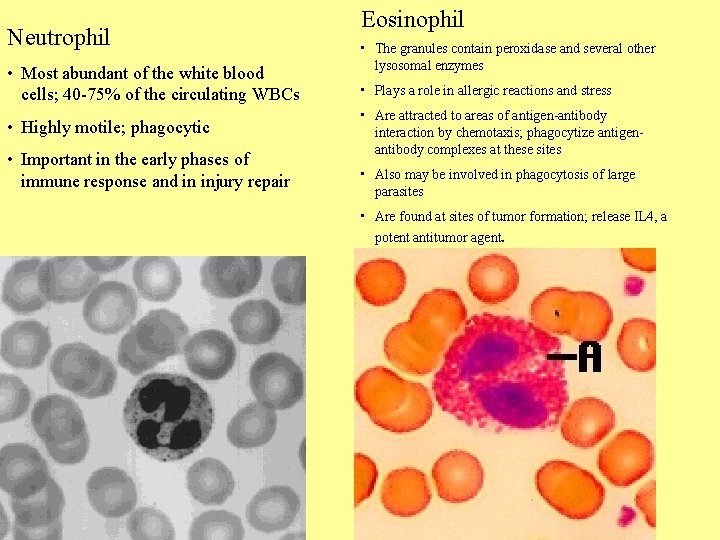
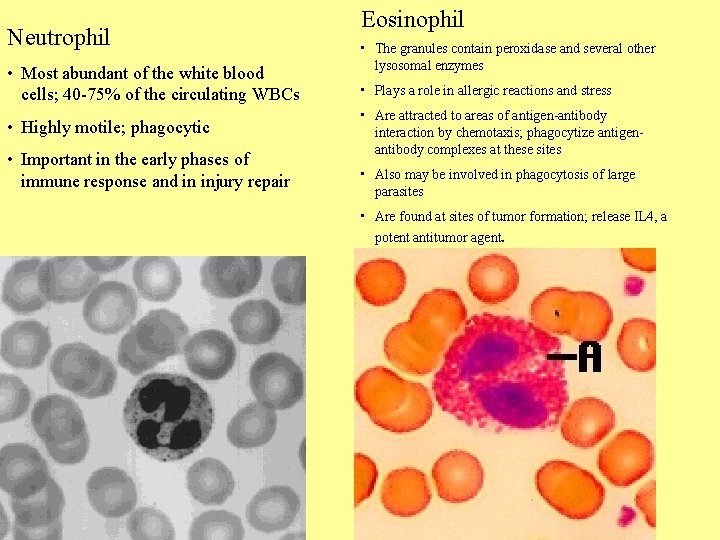
Neutrophil • Most abundant of the white blood cells; 40 -75% of the circulating WBCs • Highly motile; phagocytic • Important in the early phases of immune response and in injury repair Eosinophil • The granules contain peroxidase and several other lysosomal enzymes • Plays a role in allergic reactions and stress • Are attracted to areas of antigen-antibody interaction by chemotaxis; phagocytize antigenantibody complexes at these sites • Also may be involved in phagocytosis of large parasites • Are found at sites of tumor formation; release IL 4, a potent antitumor agent.
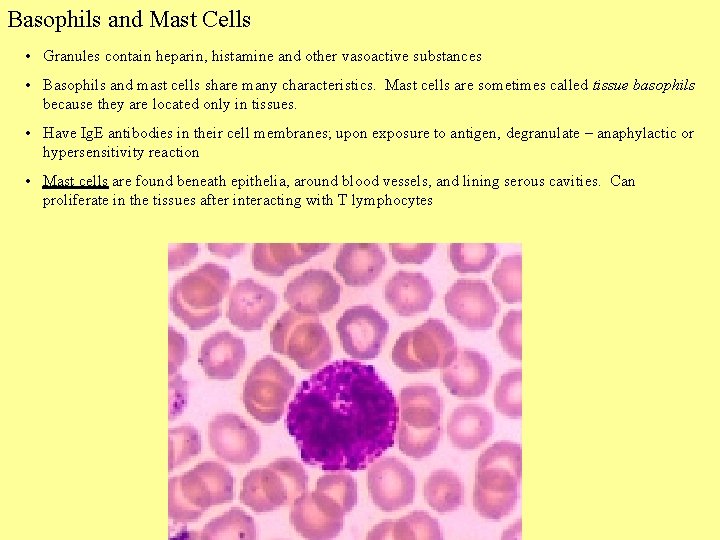
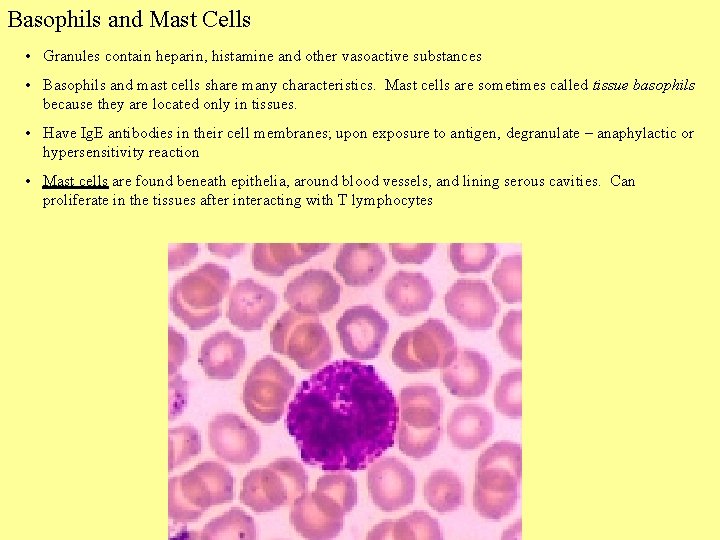
Basophils and Mast Cells • Granules contain heparin, histamine and other vasoactive substances • Basophils and mast cells share many characteristics. Mast cells are sometimes called tissue basophils because they are located only in tissues. • Have Ig. E antibodies in their cell membranes; upon exposure to antigen, degranulate – anaphylactic or hypersensitivity reaction • Mast cells are found beneath epithelia, around blood vessels, and lining serous cavities. Can proliferate in the tissues after interacting with T lymphocytes
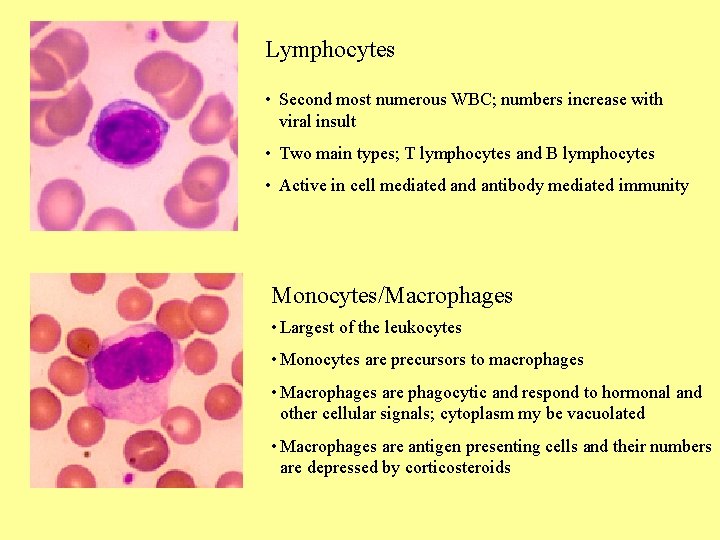
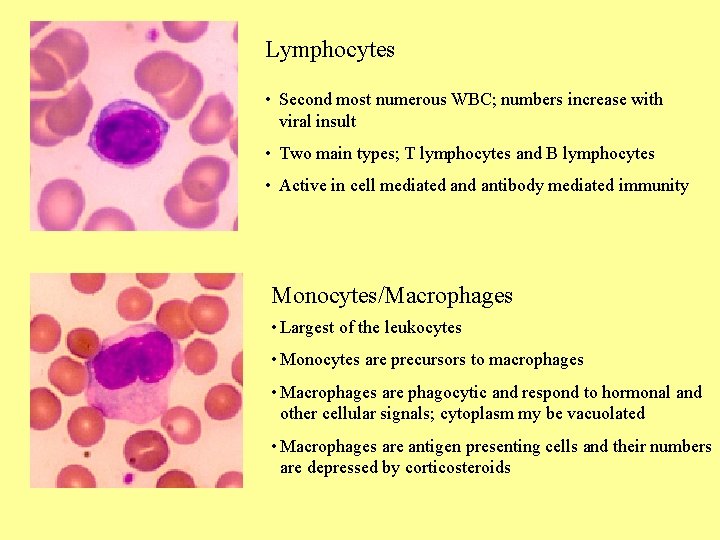
Lymphocytes • Second most numerous WBC; numbers increase with viral insult • Two main types; T lymphocytes and B lymphocytes • Active in cell mediated antibody mediated immunity Monocytes/Macrophages • Largest of the leukocytes • Monocytes are precursors to macrophages • Macrophages are phagocytic and respond to hormonal and other cellular signals; cytoplasm my be vacuolated • Macrophages are antigen presenting cells and their numbers are depressed by corticosteroids
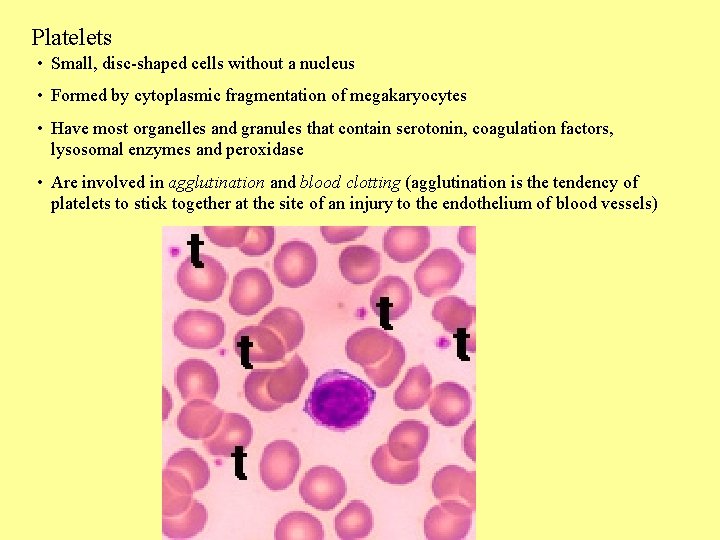
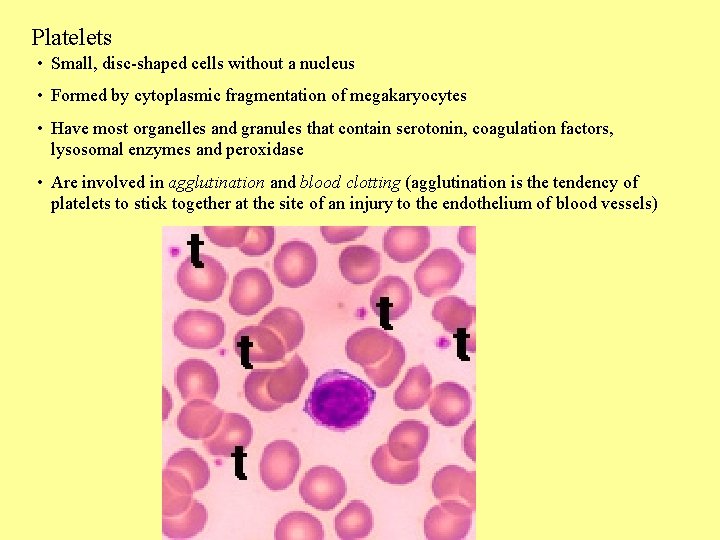
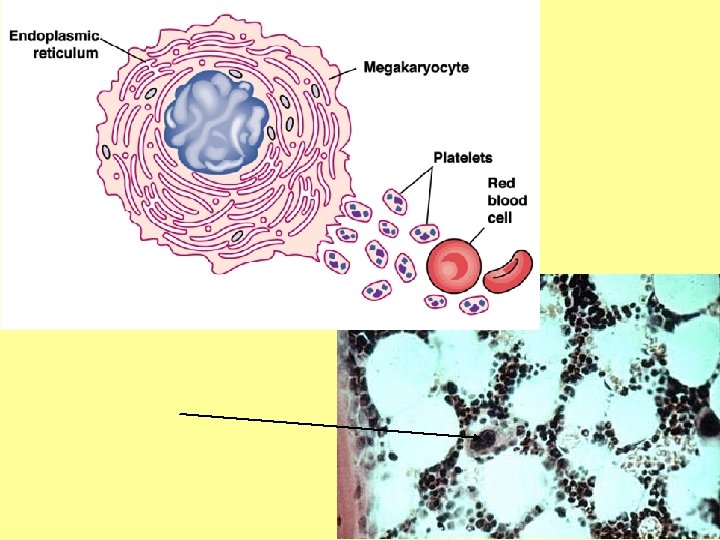
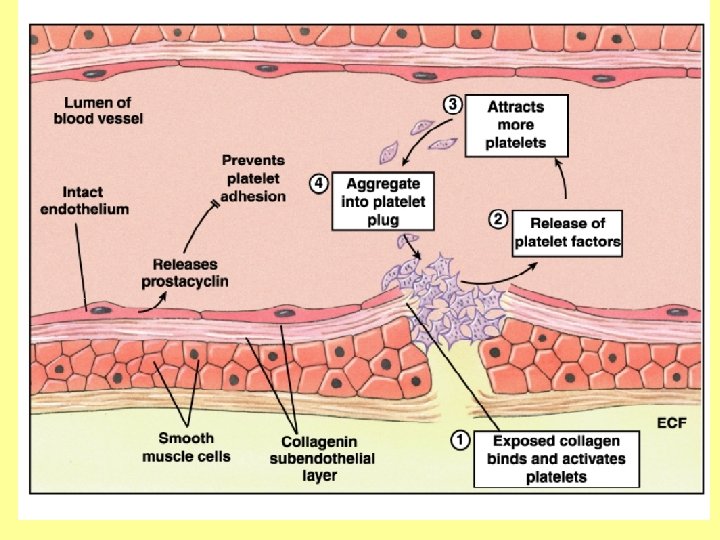
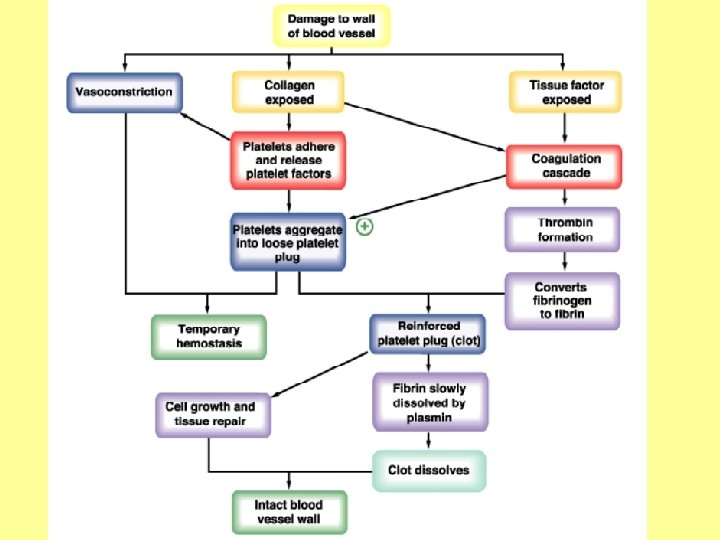
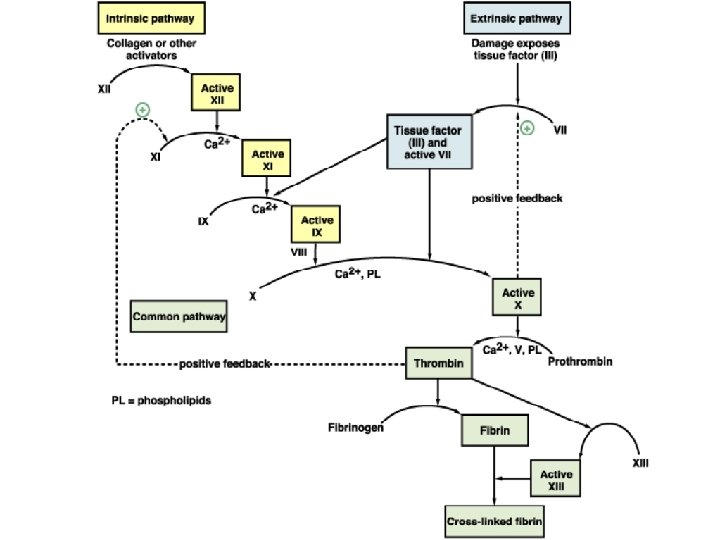
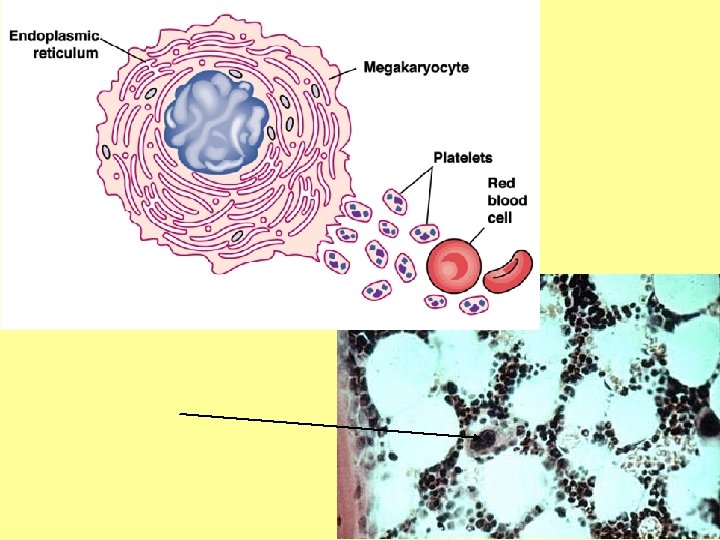
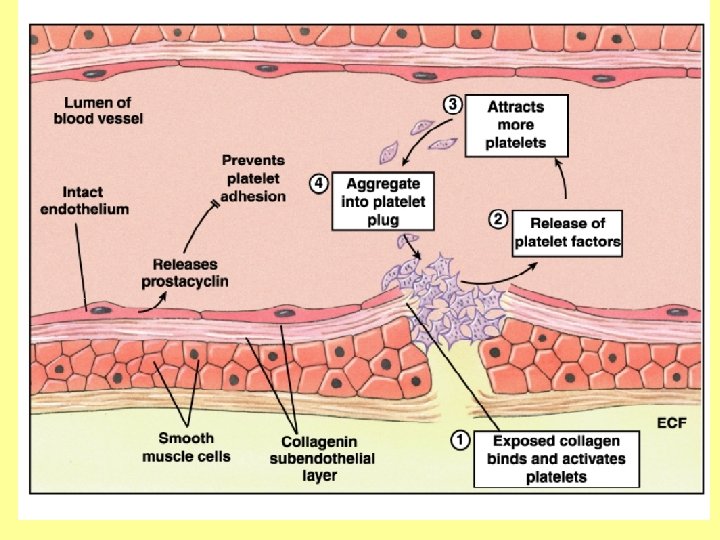
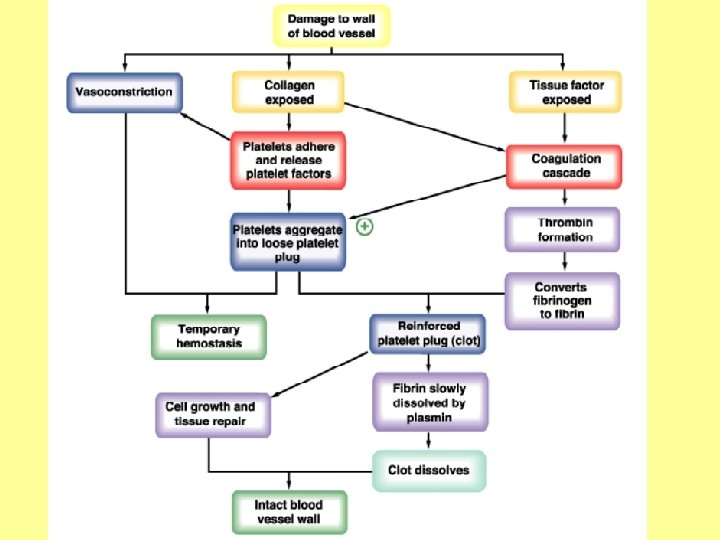
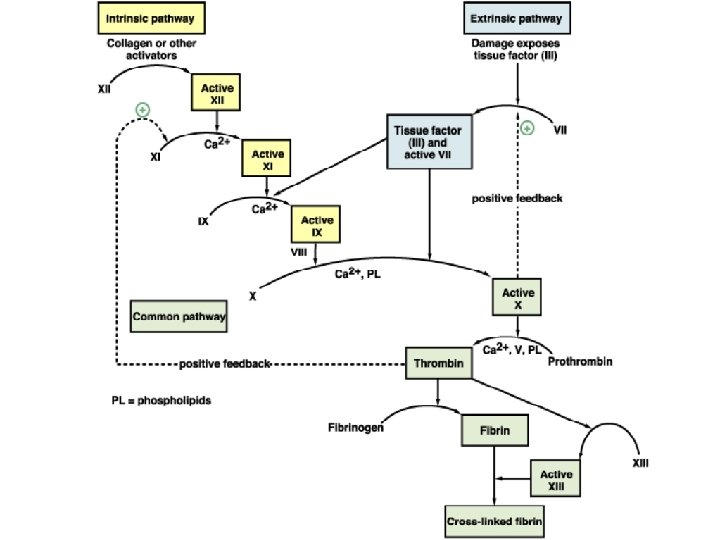
Platelets • Small, disc-shaped cells without a nucleus • Formed by cytoplasmic fragmentation of megakaryocytes • Have most organelles and granules that contain serotonin, coagulation factors, lysosomal enzymes and peroxidase • Are involved in agglutination and blood clotting (agglutination is the tendency of platelets to stick together at the site of an injury to the endothelium of blood vessels)
 Interstitial vs intracellular
Interstitial vs intracellular Is synovial fluid extracellular fluid
Is synovial fluid extracellular fluid Extracellular fluid and interstitial fluid
Extracellular fluid and interstitial fluid Fluid compartments in the body
Fluid compartments in the body Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Extracellular fluid composition
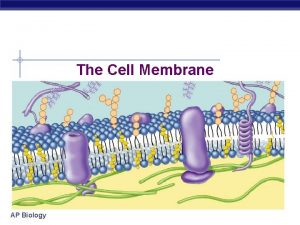
Extracellular fluid composition Struktur dasar membran sel
Struktur dasar membran sel Extracellular fluid contains
Extracellular fluid contains Intracellular and extracellular
Intracellular and extracellular Extracellular fluid
Extracellular fluid Yellowish liquid part of the blood
Yellowish liquid part of the blood Fluid portion of blood
Fluid portion of blood Principal cells
Principal cells Bone content
Bone content Circulating dental assistant
Circulating dental assistant What is effective circulating volume
What is effective circulating volume Role of scrub nurse
Role of scrub nurse Equipment used for crystallization
Equipment used for crystallization What is effective circulating volume
What is effective circulating volume Single phase dual converter waveform
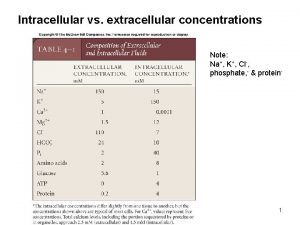
Single phase dual converter waveform Intracellular k concentration
Intracellular k concentration Nature reviews immunology
Nature reviews immunology Extracellular signal
Extracellular signal Deuteromycotes
Deuteromycotes Basement membrane structure
Basement membrane structure Major intra and extracellular electrolytes
Major intra and extracellular electrolytes Adipose loose connective tissue function
Adipose loose connective tissue function Extracellular digestion
Extracellular digestion Extracellular signal regulated kinase
Extracellular signal regulated kinase Neutrophil extracellular traps
Neutrophil extracellular traps