Child protection in the ED Child Protection and
- Slides: 30
Child protection in the ED Child Protection and Wellbeing Identify, Consult, Respond 1
Learning objectives • Recognise red flags for child protection and wellbeing concerns. • Know how to get help for vulnerable families. • Know how the NSW Health Child Wellbeing Unit can assist you. • Know how and when to make a Mandatory Report – and what to do next. 2
Facts and figures • In the 10 years to 2013, 83 children from 75 families died at the hands of a family member. • In 17 families, the child had been seen in an Emergency Department in the year before their death. • In many cases, a Mandatory Report had been made. The message is clear: Making a Mandatory Report is not enough. 3
Cases: video 1 4
Cases: video 2 5
Cases: video 3 6
Red flags: general Parents who abuse their children can also appear to be loving and caring. Don’t take the presentation at face value • delayed presentation • inappropriate behaviour/interactions from the child or carer • inconsistent or implausible history • bruising • frequent presentations • domestic & family violence • multiple concerning presentations in the e. MR
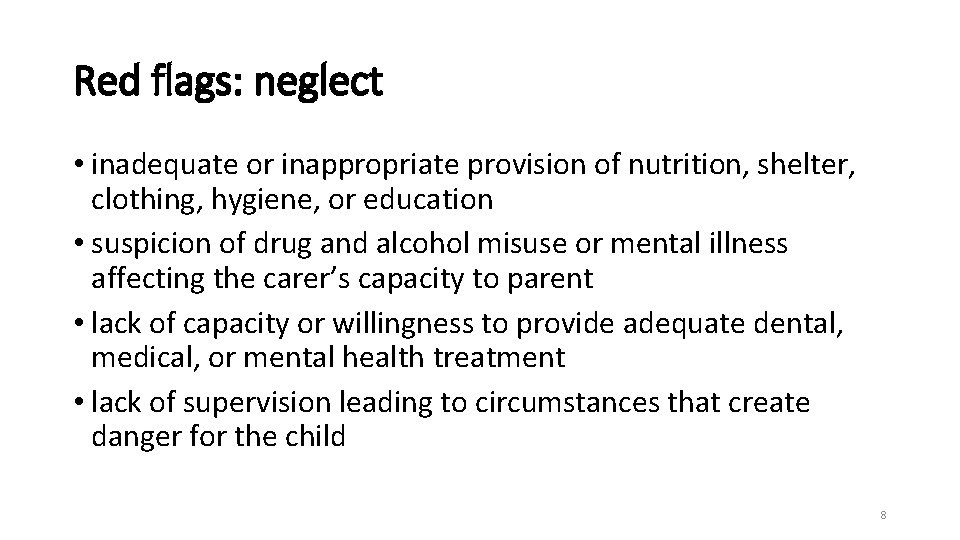
Red flags: neglect • inadequate or inappropriate provision of nutrition, shelter, clothing, hygiene, or education • suspicion of drug and alcohol misuse or mental illness affecting the carer’s capacity to parent • lack of capacity or willingness to provide adequate dental, medical, or mental health treatment • lack of supervision leading to circumstances that create danger for the child 8
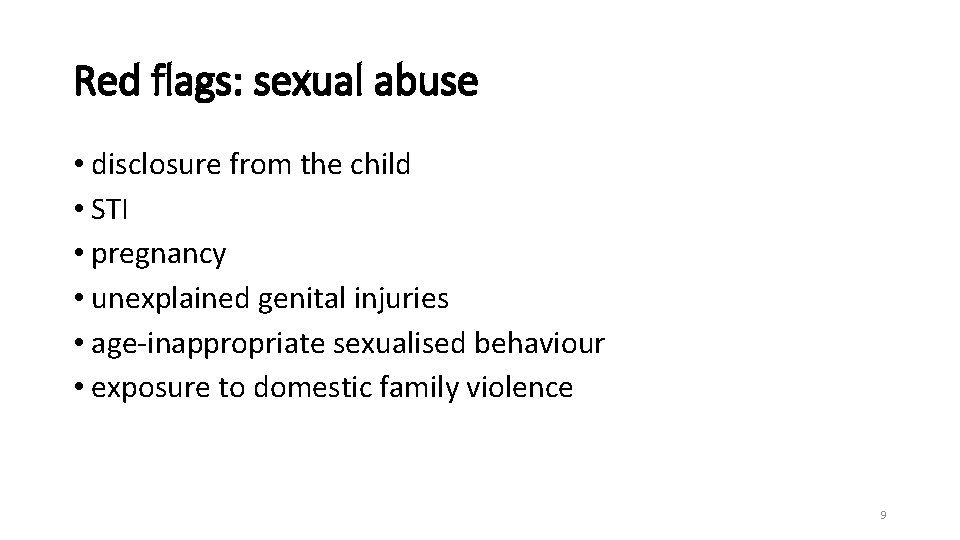
Red flags: sexual abuse • disclosure from the child • STI • pregnancy • unexplained genital injuries • age-inappropriate sexualised behaviour • exposure to domestic family violence 9
Wrap your head around this: The child or young person at risk may not be in the ED in front of you. 10
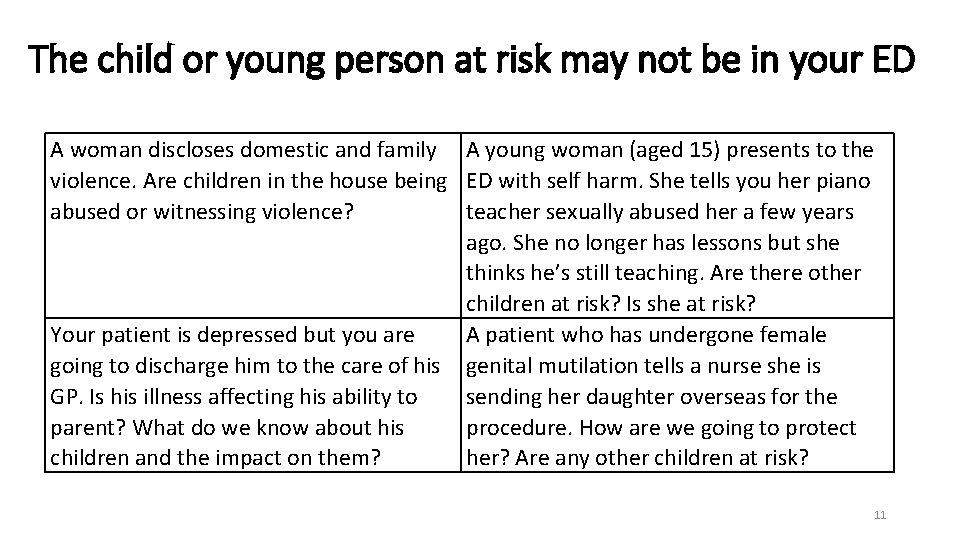
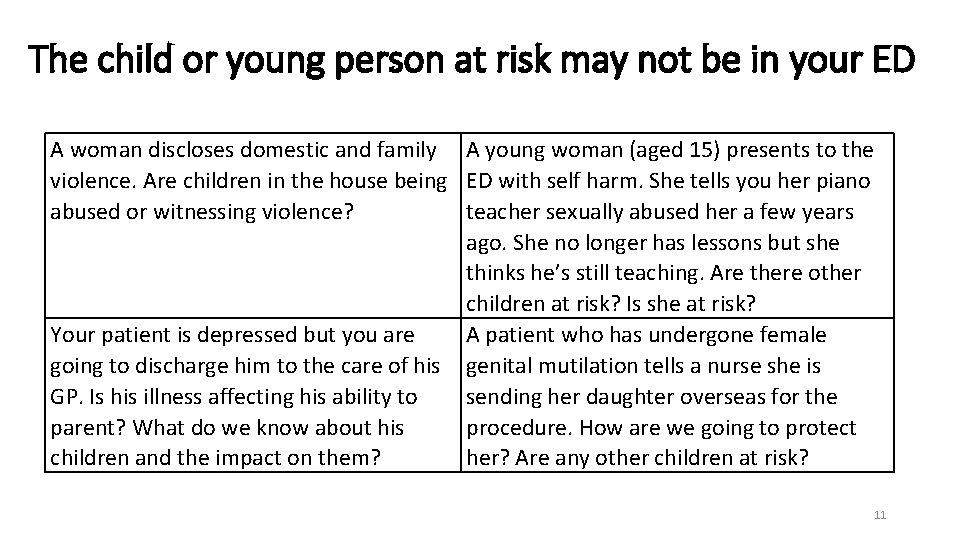
The child or young person at risk may not be in your ED A woman discloses domestic and family A young woman (aged 15) presents to the violence. Are children in the house being ED with self harm. She tells you her piano abused or witnessing violence? teacher sexually abused her a few years ago. She no longer has lessons but she thinks he’s still teaching. Are there other children at risk? Is she at risk? Your patient is depressed but you are A patient who has undergone female going to discharge him to the care of his genital mutilation tells a nurse she is GP. Is his illness affecting his ability to sending her daughter overseas for the parent? What do we know about his procedure. How are we going to protect children and the impact on them? her? Are any other children at risk? 11
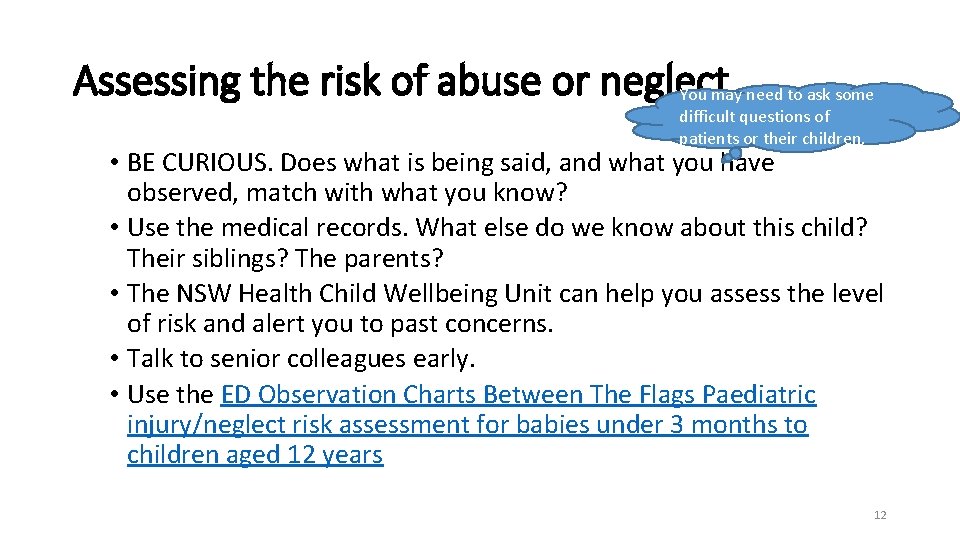
Assessing the risk of abuse or neglect You may need to ask some difficult questions of patients or their children. • BE CURIOUS. Does what is being said, and what you have observed, match with what you know? • Use the medical records. What else do we know about this child? Their siblings? The parents? • The NSW Health Child Wellbeing Unit can help you assess the level of risk and alert you to past concerns. • Talk to senior colleagues early. • Use the ED Observation Charts Between The Flags Paediatric injury/neglect risk assessment for babies under 3 months to children aged 12 years 12
Options: where can you turn for help? 13
You are worried about a child’s safety or wellbeing: can you ask the GP for more information? or child and family health nurse, school, daycare, preschool, other treating clinicians (eg psychologists or drug and alcohol counsellors) etc
Can you ask the family’s GP for more information? Yes: safety and care coordination trump confidentiality. Chapter 16 A of the NSW Children and Young Persons (Care and Protection) Act 1998 allows information sharing here without consent. • This can be verbally or in writing. • A record of any information exchange must be made in e. MR or your local documentation system.
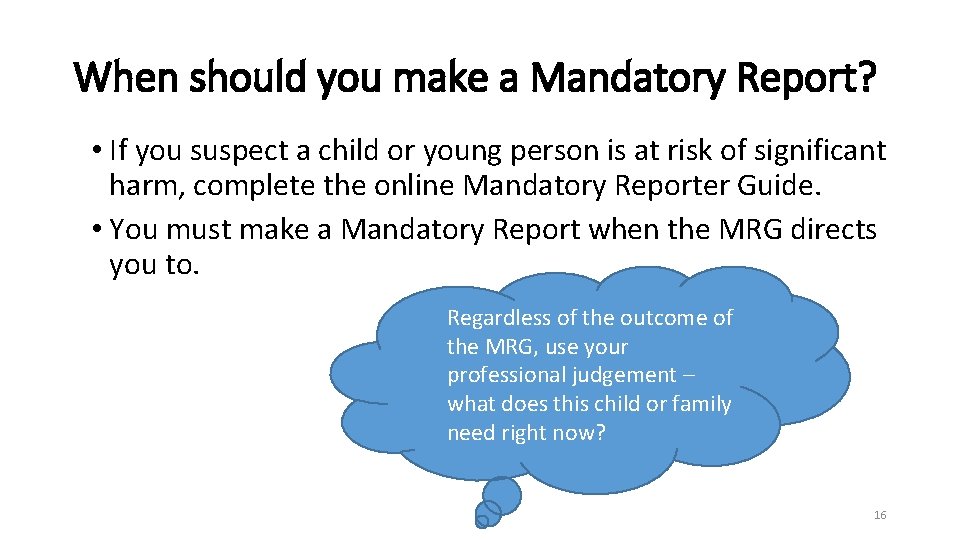
When should you make a Mandatory Report? • If you suspect a child or young person is at risk of significant harm, complete the online Mandatory Reporter Guide. • You must make a Mandatory Report when the MRG directs you to. Regardless of the outcome of the MRG, use your professional judgement – what does this child or family need right now? 16
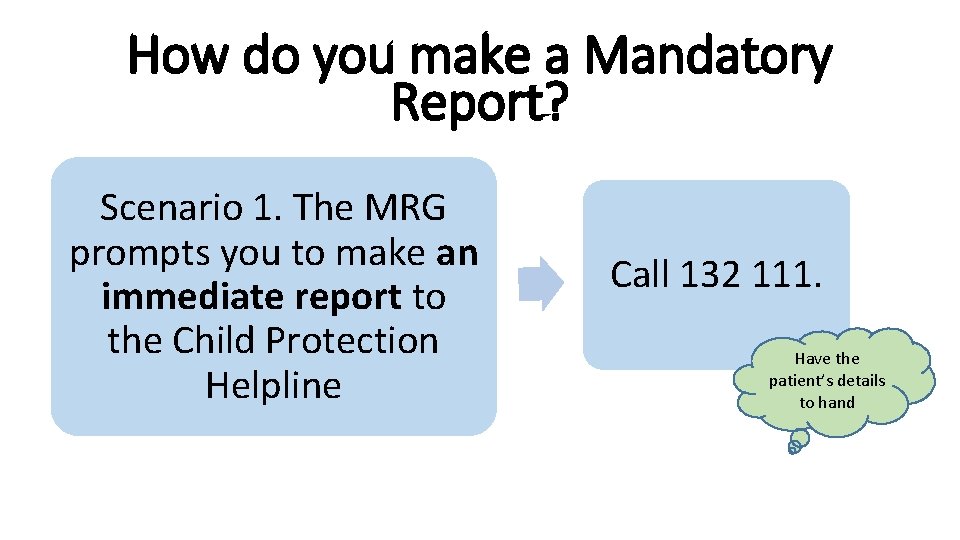
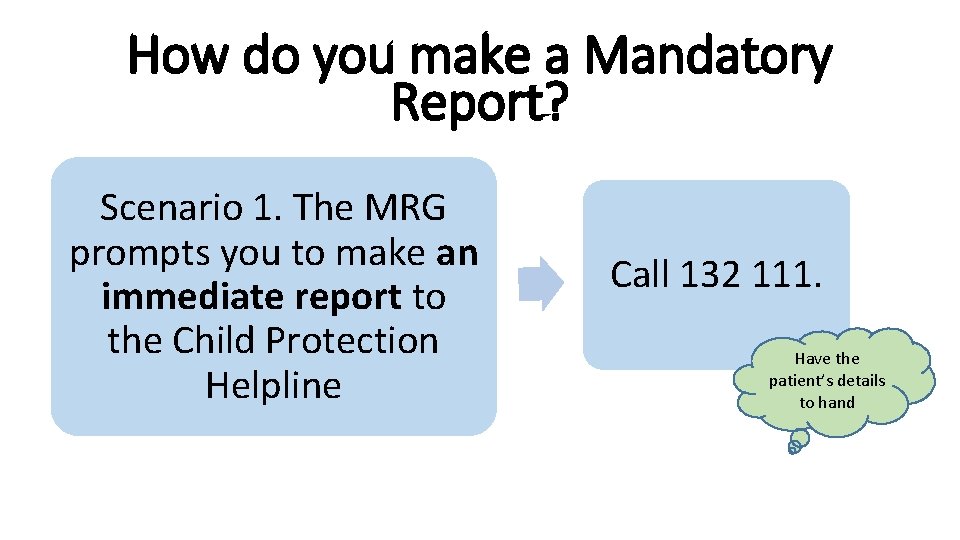
How do you make a Mandatory Report? Scenario 1. The MRG prompts you to make an immediate report to the Child Protection Helpline Call 132 111. Have the patient’s details to hand
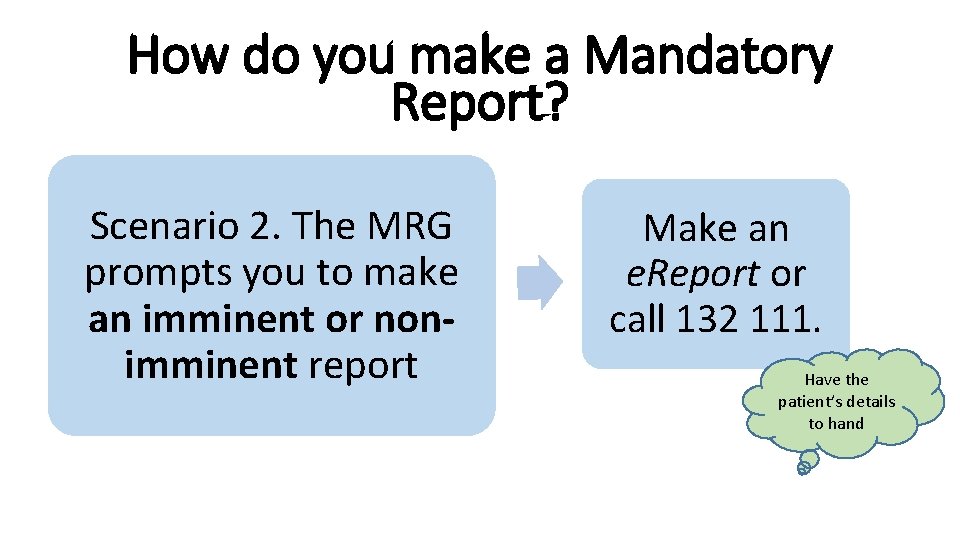
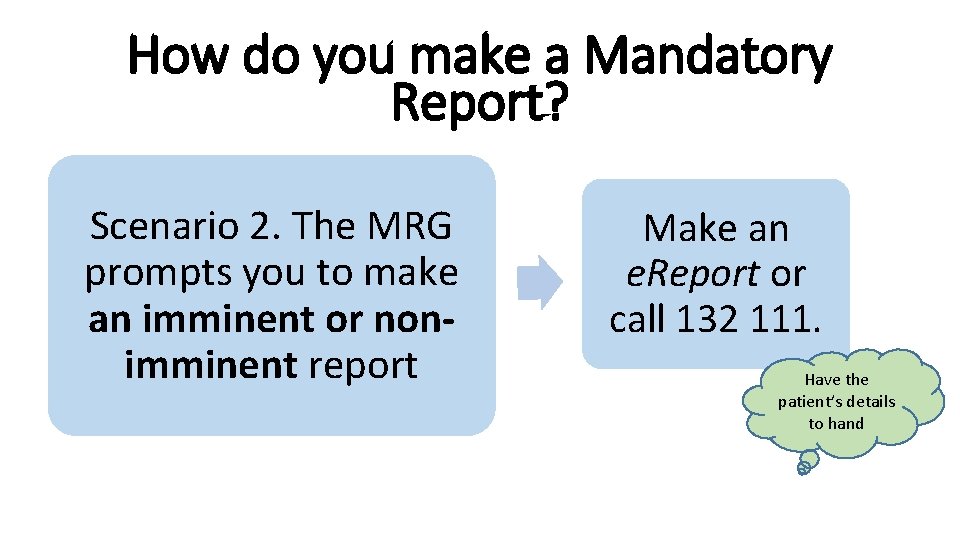
How do you make a Mandatory Report? Scenario 2. The MRG prompts you to make an imminent or nonimminent report Make an e. Report or call 132 111. Have the patient’s details to hand
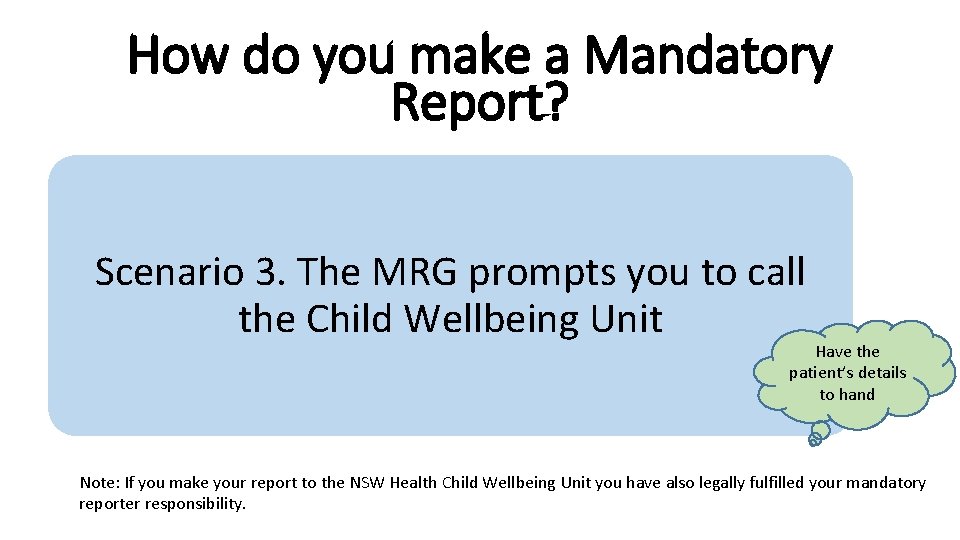
How do you make a Mandatory Report? Scenario 3. The MRG prompts you to call the Child Wellbeing Unit Have the patient’s details to hand Note: If you make your report to the NSW Health Child Wellbeing Unit you have also legally fulfilled your mandatory reporter responsibility.
How do you make a Mandatory Report? Scenario 4. The MRG prompts you to continue care What are you going to do next?
What happens after a Mandatory Report? This short video outlines what happens after you hang up the phone. Always continue to offer a service to the child, young person and their family and/or consider additional referrals. 21
NSW Health Child Wellbeing Unit – how can it help? This short video explains the role of CWU. 22
Sexual Assault Services – how can they help? Every LHD has a 24 -h Sexual Assault Service. This short video outlines its functions. Call your SAS for advice as soon as you suspect sexual abuse. 23
What next? • What are you going to do to ensure the child or young person’s safety right now? • What does this family need right now? • What are you going to do to look after yourself? 24
Key elements of a good response to child protection concerns • Take a really good history and document it thoroughly. • Don’t be afraid to ask the key questions. • Get information from other sources. • Use the Mandatory Reporter Guide (MRG). Always ask yourself what the hospital needs to do right now to keep this child safe or to address any identified risk factors. 25
Tips for raising child protection and wellbeing concerns with carers • Seek help from senior staff, medical, nursing or social worker • Be honest • Explain why you are worried 26
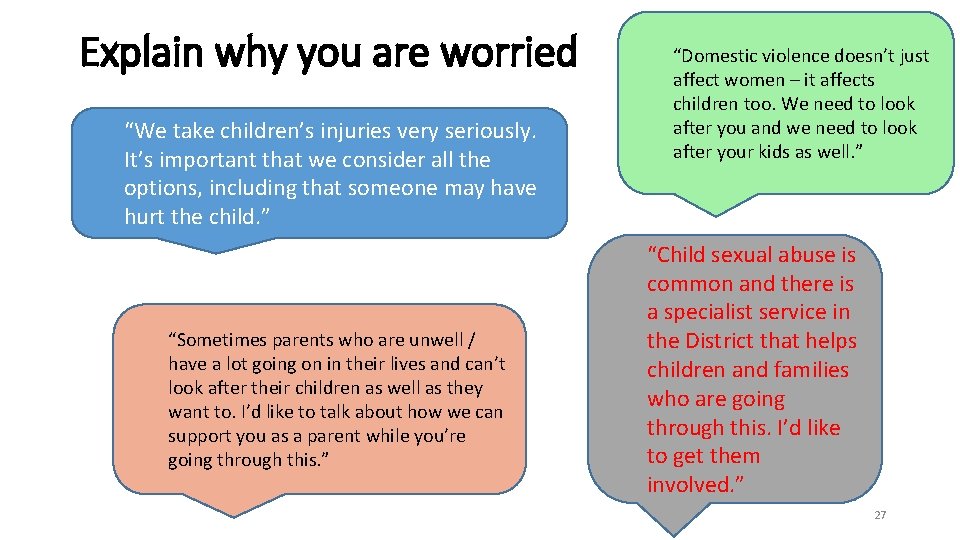
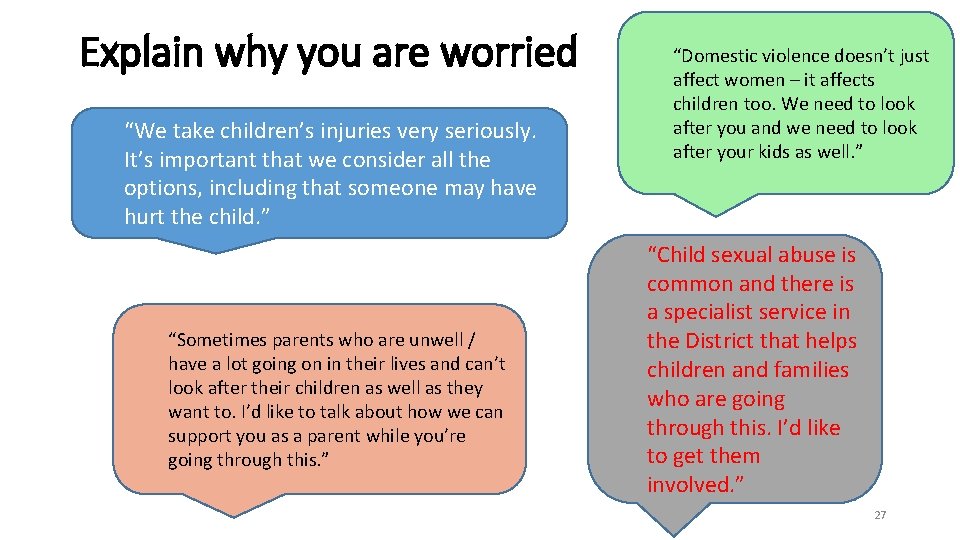
Explain why you are worried “We take children’s injuries very seriously. It’s important that we consider all the options, including that someone may have hurt the child. ” “Sometimes parents who are unwell / have a lot going on in their lives and can’t look after their children as well as they want to. I’d like to talk about how we can support you as a parent while you’re going through this. ” “Domestic violence doesn’t just affect women – it affects children too. We need to look after you and we need to look after your kids as well. ” “Child sexual abuse is common and there is a specialist service in the District that helps children and families who are going through this. I’d like to get them involved. ” 27
Tips for raising child protection and wellbeing concerns with carers (continued) • Allow parents to vent. It’s okay for them to express their distress and disbelief. • Be clear about the next steps eg ortho consult, Mandatory Report • If the carer removes the child from the ED, escalate your response: alert a senior staff member and make a Mandatory Report or update your Report. Remember: ED staff are very good at delivering bad news. 28
Conclusions: Identify, Consult, Respond IDENTIFY: • Considering a child or young person’s safety, welfare and wellbeing is an important part of every consultation. • A child or young person at risk may not be in the Department – think outside the hospital walls. What’s going on within the family or household? CONSULT: • Know where to consult for further assessments and/or referrals as required. RESPOND: • Make the most of every opportunity to improve the safety, welfare and wellbeing of these children/young people. • Mandatory reporting is only one part of your Health response. 29
Questions? Identify Consult Respond 30
 Safeguarding and child protection the essentials
Safeguarding and child protection the essentials Child care and protection
Child care and protection Child protection and toy safety act
Child protection and toy safety act Child care and protection act 3 of 2015
Child care and protection act 3 of 2015 Courage child protection
Courage child protection Types of child protection
Types of child protection Child marriage definition
Child marriage definition Child protection case management tools
Child protection case management tools Types of child protection
Types of child protection Professional curiosity examples
Professional curiosity examples Community based child protection mechanisms
Community based child protection mechanisms Child protection training materials
Child protection training materials Child protection awareness training
Child protection awareness training Child protection minimum standards
Child protection minimum standards Child protection policy
Child protection policy Child protection policy
Child protection policy Child protection reform amendment act 2017
Child protection reform amendment act 2017 Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Glasgow thang điểm
Glasgow thang điểm Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù