Chapter 9 Patient Assessment National EMS Education Standard



- Slides: 59
Chapter 9: Patient Assessment
National EMS Education Standard Competencies (1 of 5) Assessment Use scene information and simple patient assessment findings to identify and manage immediate life threats and injuries within the scope and practice of the emergency medical responder (EMR).
National EMS Education Standard Competencies (2 of 5) Scene Size-Up • Scene safety • Scene management – Impact of the environment on patient care – Addressing hazards – Violence – Need for additional or specialized resources – Standard precautions
National EMS Education Standard Competencies (3 of 5) Primary Assessment • Primary assessment for all patient situations – Level of consciousness – ABCs – Identifying life threats – Assessment of vital functions • Begin interventions needed to preserve life
National EMS Education Standard Competencies (4 of 5) History Taking • Determine the chief complaint • Mechanism of injury (MOI)/nature of illness (NOI) • Associated signs and symptoms
National EMS Education Standard Competencies (5 of 5) Secondary Assessment • Performing a rapid full-body scan • Focused assessment of pain • Assessment of vital signs Reassessment • How and when to reassess patients
Introduction (1 of 2) • EMRs are the first trained emergency medical services (EMS) providers at many emergency scenes. • Patient assessment sequence – Perform a scene size-up. – Perform a primary assessment. – Obtain the patient’s medical history. – Perform a secondary assessment. – Perform a reassessment.
Introduction (2 of 2) • The skills and knowledge presented in this chapter follow an assessment-based care model. – The treatment rendered is based on the patient’s symptoms. – Assessment-based care requires you to conduct a careful and thorough evaluation.
Patient Assessment Sequence • The patient assessment sequence provides a framework so that you can – Safely approach an emergency scene – Determine the need for additional help – Examine the patient to determine if injuries or illnesses are present – Obtain the patient’s medical history – Report the results to other EMS personnel
Scene Size-Up (1 of 8) • General overview of the incident and its surroundings • Review dispatch information. – Location of the incident – Main problem or type of incident – Number of people involved – Safety issues at the scene
Scene Size-Up (2 of 8) • Review dispatch information. (cont’d) – Other factors can affect your actions: • Time of day • Day of the week • Weather conditions – Mentally prepare for other situations you may find when you arrive on the scene. – If you come across a medical emergency, contact dispatch using your two-way radio.
Scene Size-Up (3 of 8) • Ensure scene safety. – Park your vehicle so that it helps secure the scene and minimizes traffic blockage. © Dale A. Stork/Shutterstock. – Scan the scene and determine the: • Extent of the incident • Possible number of people injured • Presence of possible hazards
Scene Size-Up (4 of 8) • Ensure scene safety. (cont’d) – Visible hazards include • Crash or crime scene • Fallen electrical wires • Traffic • Spilled gasoline • Unstable buildings or surfaces • Weather • Crowds
Scene Size-Up (5 of 8) • Ensure scene safety. (cont’d) – Invisible hazards include • Electricity • Biologic hazards • Hazardous materials • Poisonous fumes – If a scene is unsafe, keep people away until specially trained teams arrive.
Scene Size-Up (6 of 8) • Determine the MOI or NOI. – Look for clues that may indicate how the accident happened. – Ask the patient, family members, or bystanders for additional information. – Do not rule out any injury without conducting a full-body physical assessment.
Scene Size-Up (7 of 8) • Take standard precautions. – Always have gloves readily available. – Consider whether the use of additional protection may be necessary. – Wash your hands thoroughly after contact with a patient or contaminated materials.
Scene Size-Up (8 of 8) • Determine the number of patients. – Call for additional assistance if you think you will need help. – It may be necessary to perform triage. • Consider additional resources, including Law enforcement personnel – Fire department units – Utility company personnel – Wrecker operators
Primary Assessment (1 of 9) • The purpose of the primary assessment is to identify life threats to the patient. • Form a general impression. – Note the patient’s sex and approximate age. – Determine whether the patient has experienced trauma or illness. – Determine the patient’s level of consciousness.
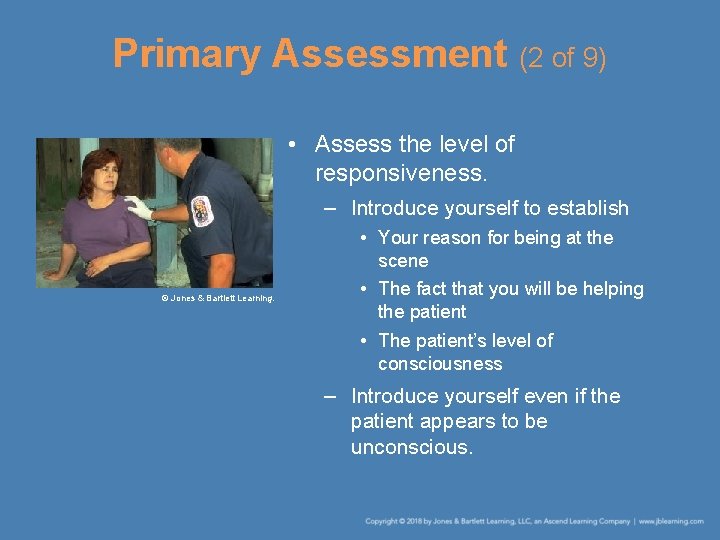
Primary Assessment (2 of 9) • Assess the level of responsiveness. – Introduce yourself to establish © Jones & Bartlett Learning. • Your reason for being at the scene • The fact that you will be helping the patient • The patient’s level of consciousness – Introduce yourself even if the patient appears to be unconscious.
Primary Assessment (3 of 9) • Assess the level of responsiveness. (cont’d) – Use the AVPU scale. • Alert • Verbal • Pain • Unresponsive
Primary Assessment (4 of 9) • Perform a rapid exam. – Assess the airway. • If the patient is alert and able to answer questions, the airway is open. • In an unconscious patient, you must open the airway. • Inspect the airway foreign bodies or secretions. • Clear the airway as needed. • You may need to insert an airway adjunct.
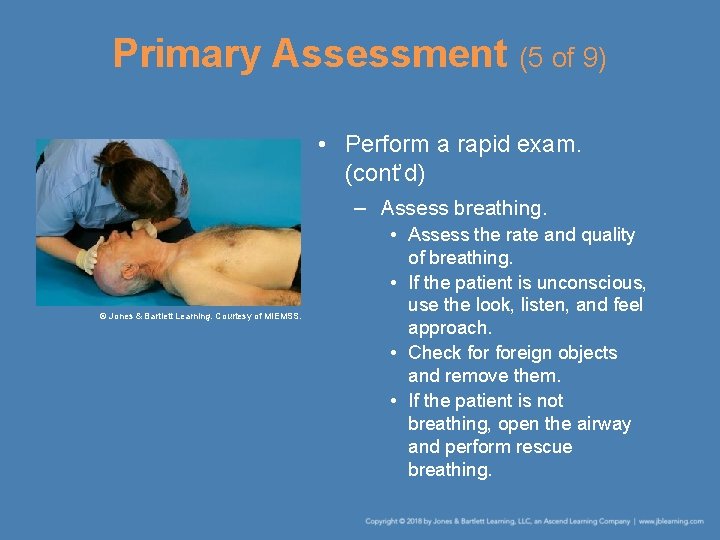
Primary Assessment (5 of 9) • Perform a rapid exam. (cont’d) – Assess breathing. © Jones & Bartlett Learning. Courtesy of MIEMSS. • Assess the rate and quality of breathing. • If the patient is unconscious, use the look, listen, and feel approach. • Check foreign objects and remove them. • If the patient is not breathing, open the airway and perform rescue breathing.
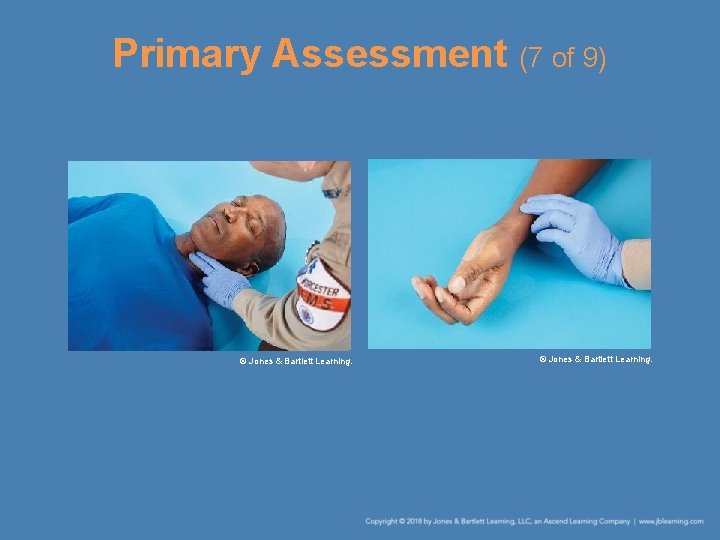
Primary Assessment (6 of 9) • Perform a rapid exam. (cont’d) – Assess circulation. • If the patient is unconscious, check a carotid pulse. • If the patient is conscious, assess the radial pulse. • Check the patient for severe external bleeding. • Assess the patient’s skin color and temperature.
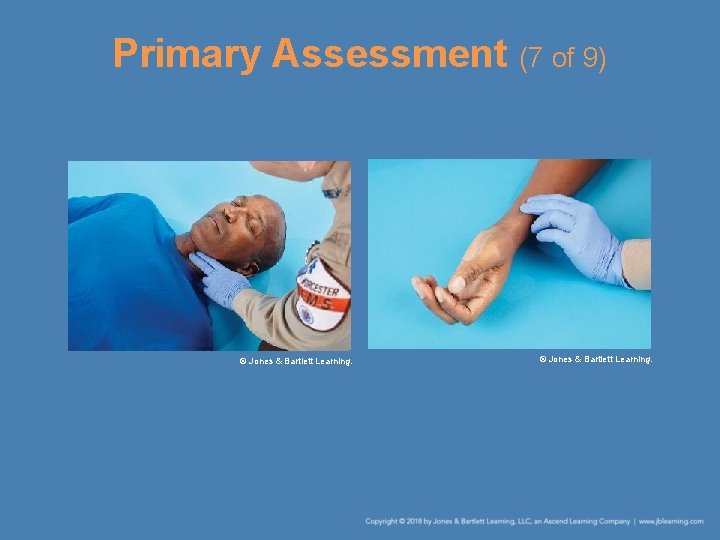
Primary Assessment (7 of 9) © Jones & Bartlett Learning.
Primary Assessment (8 of 9) • Perform a rapid exam. (cont’d) – Descriptions of skin color: • Pale—whitish, indicating decreased circulation to that part of the body or to all of the body • Flushed—reddish, indicating excess circulation to that part of the body • Blue—cyanotic, indicating lack of oxygen and possible airway problems • Yellow—indicating liver problems • Normal
Primary Assessment (9 of 9) • Update responding EMS units. – Elements of the report: • Age and sex of the patient • Chief complaint • Level of responsiveness • Status of airway, breathing, and circulation – Try to perform all four steps of the primary assessment quickly as you make contact with the patient.
History Taking (1 of 4) • Investigate the chief complaint. – Do not allow a conscious patient’s comments to distract you. – Purposes of obtaining a history is to • Gather a systematic account of past medical conditions, illnesses, and injuries. • Determine the events leading up to the present medical situation. • Determine the signs and symptoms of the current condition.

History Taking (2 of 4) • Investigate the chief complaint. (cont’d) – Question the patient in a clear and systematic manner. – Learn the relevant facts, including • Serious injuries, illnesses, or surgeries • Prescription medicines • Over-the-counter (OTC) medicines and herbal medicines • Allergies to any medicines, foods, or seasonal allergens
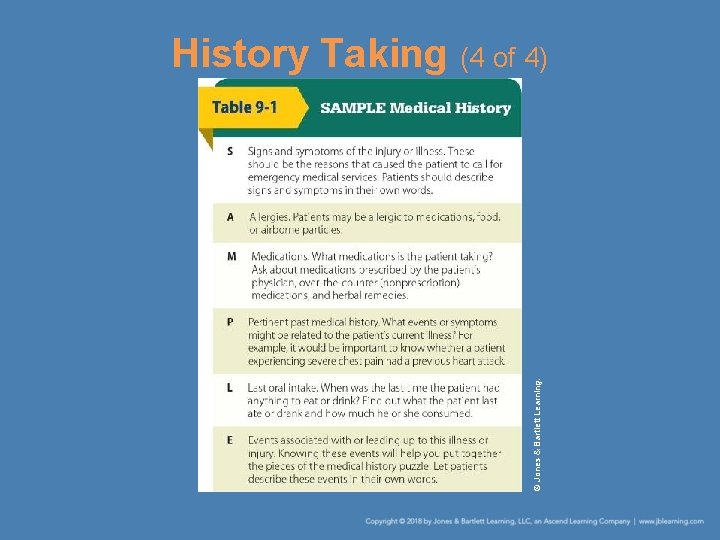
History Taking (3 of 4) • Obtain a SAMPLE history. – Provides a framework to ask further questions of the patient – Ask the patient one question at a time. – Listen carefully and use good eye contact. – If the patient is unconscious or senile, a family member or friend may be able to help. – Communicate this information to other EMS personnel.
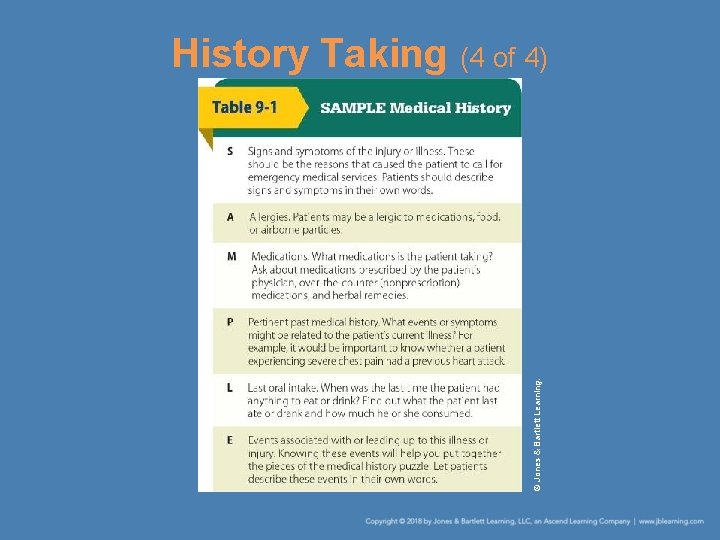
© Jones & Bartlett Learning. History Taking (4 of 4)
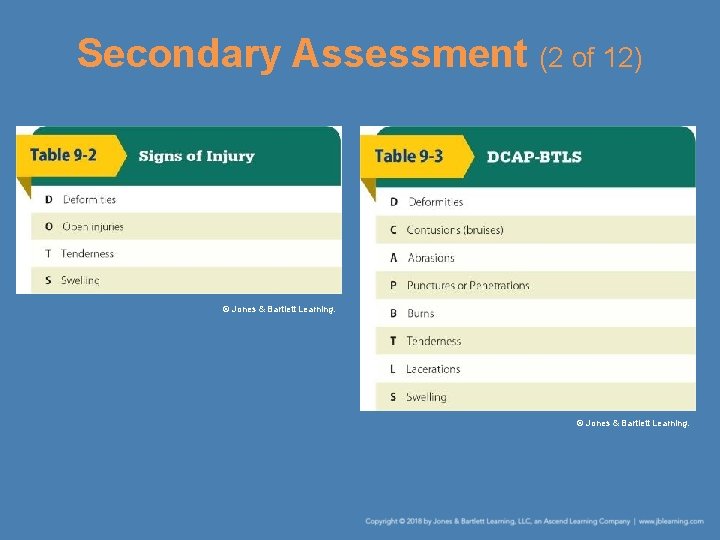
Secondary Assessment (1 of 12) • The secondary assessment is done to assess non–life-threatening conditions. • The physical examination helps you locate and begin initial management of signs and symptoms of illness or injury. – A sign is something about the patient you can see or feel for yourself. – A symptom is something the patient tells you about his or her condition.
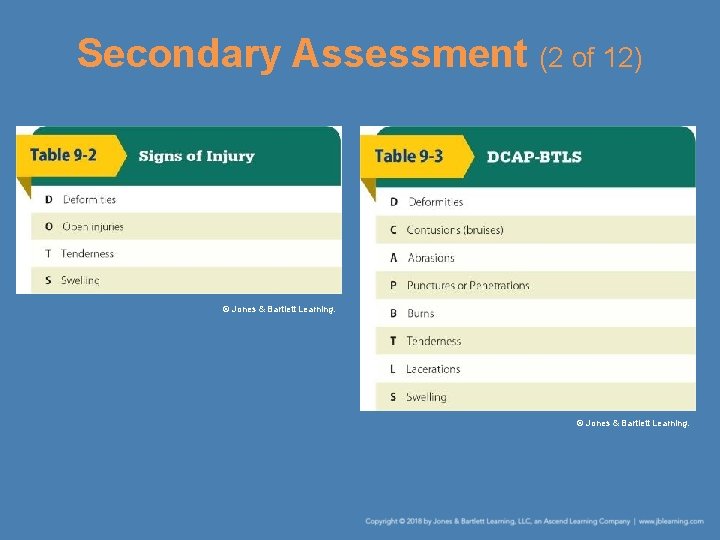
Secondary Assessment (2 of 12) © Jones & Bartlett Learning.
Secondary Assessment (3 of 12) • Secondary assessment of the entire body – Can be done whether the patient is conscious or unconscious. – Assume that all unconscious, injured patients have spinal injuries. – Stabilize the head and spine to minimize movement during the patient examination. – Follow the steps in Skill Drill 9 -1 to perform a full-body assessment.
Secondary Assessment (4 of 12) • Exam of a specific area of the body – Performed on patients who have sustained nonsignificant MOIs or on responsive medical patients – Based on the chief complaint – Focuses your attention on the immediate problem
Secondary Assessment (5 of 12) • Assess vital signs. – Respiration • The normal adult resting respiratory rate is 12 to 20 breaths per minute. • Count the patient’s breath for 1 minute. • Check the breathing rate and quality. – Pulse • Indicates the speed and force of the heartbeat • Take the radial pulse of a conscious patient.
Secondary Assessment (6 of 12) • Assess vital signs. (cont’d) – Pulse (cont’d) • Take the carotid pulse of an unconscious patient. • When examining an infant, use the brachial pulse. • In a normal adult, the resting pulse rate is 60 to 100 beats per minute. • Determine the rhythm and the quality. – Capillary refill • Ability of the circulatory system to return blood to the capillary vessels
Secondary Assessment (7 of 12) • Assess vital signs. (cont’d) – Capillary refill (cont’d) • Squeeze the patient’s nail bed firmly between your thumb and forefinger until the nail bed looks pale. • Release the pressure and count 2 seconds. • The patient’s nail bed should return to pink in this time, indicating a normal capillary refill.
Secondary Assessment (8 of 12) • Assess vital signs. (cont’d) – Blood pressure • Systolic pressure is the force exerted on the walls of the arteries as the heart contracts. • Diastolic pressure is the arterial pressure during the relaxation phase of the heart. • Hypertension exists when the blood pressure remains greater than 140/90 mm Hg. • Check blood pressure by palpation (feeling) or auscultation (listening).
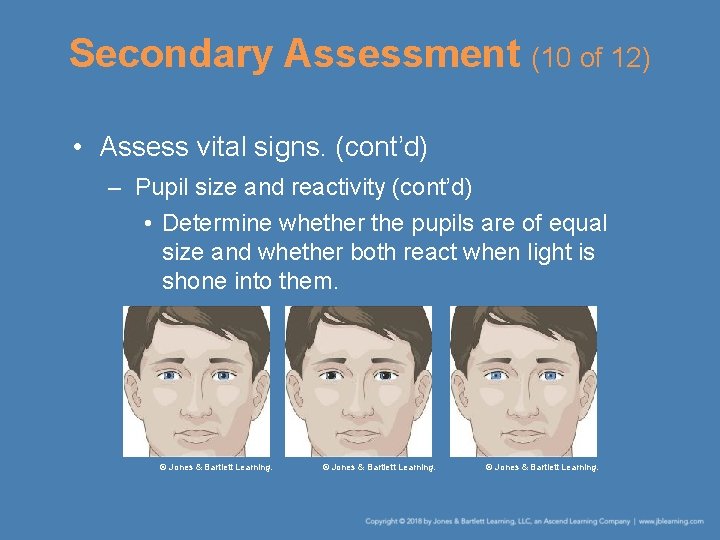
Secondary Assessment (9 of 12) • Assess vital signs. (cont’d) – Skin condition • Check for skin color, temperature, and moisture. • Normal body temperature is 98. 6 F (37 C). • Normal skin conditions are described as warm, pink, and dry. – Pupil size and reactivity • Examine each eye to detect signs of head injury, stroke, or drug overdose.
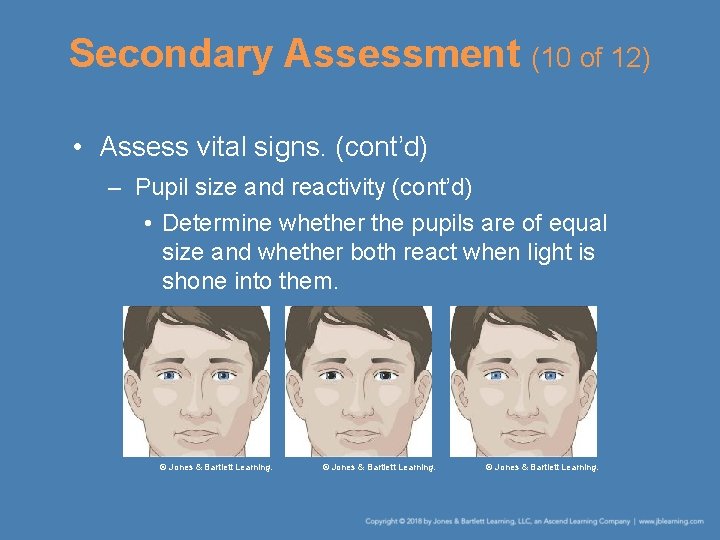
Secondary Assessment (10 of 12) • Assess vital signs. (cont’d) – Pupil size and reactivity (cont’d) • Determine whether the pupils are of equal size and whether both react when light is shone into them. © Jones & Bartlett Learning.
Secondary Assessment (11 of 12) • Assess vital signs. (cont’d) – Pupil size and reactivity (cont’d) • Pupils of unequal size can indicate a stroke or injury to the brain. • Pupils may remain constricted in a person who is taking narcotics. • Dilated pupils indicate a relaxed or unconscious state.
Secondary Assessment (12 of 12) • Assess vital signs. (cont’d) – Level of responsiveness • Observe and note any changes that occur between the time of your arrival and the time you turn over the patient’s care to higher-level personnel. • Use the AVPU scale.
Reassessment (1 of 5) • If you need to continue to care for the patient, some parts of the patient assessment need to be repeated. • Repeat the primary assessment. – Recheck the patient’s level of responsiveness and ABCs. – Continue to maintain an open airway and to monitor breathing and pulse for rate and quality.

Reassessment (2 of 5) • Reassess vital signs. – Observe the patient’s skin color and temperature. – Reassess the patient’s blood pressure. • Reassess the chief complaint. • Recheck the effectiveness of treatment. – If the patient’s status changes, determine whether you need to alter your care.
Reassessment (3 of 5) • Identify and treat changes in the patient’s condition. • Reassess the patient. – Reassess a stable patient every 15 minutes. – If the patient is unstable, repeat the reassessment every 5 minutes.

Reassessment (4 of 5) • Provide a hand-off report, including: – Age and sex of the patient – History of the incident – Patient’s chief complaint – Patient’s level of responsiveness – How you found the patient – Status of the vital signs – Results of the secondary patient assessment
Reassessment (5 of 5) • Provide a hand-off report, including: (cont’d) – Any pertinent medical conditions (using the SAMPLE format) – Any interventions provided and how the patient responded
A Word About Medical and Trauma Patients (1 of 2) • Patients can generally be classified into two main categories: – Those who have a sudden illness – Those who sustain trauma • The patient assessment sequence can be used to examine patients who have experienced illnesses, trauma, or both.
A Word About Medical and Trauma Patients (2 of 2) • When examining medical patients, follow the basic assessment sequence. • When caring for a trauma patient, perform the secondary assessment before taking the medical history. • Always avoid jumping to conclusions.
Summary (1 of 4) • A complete patient assessment consists of five steps: perform a scene size-up, perform a primary assessment, obtain a patient’s medical history, perform a secondary assessment, and provide reassessment. • The scene size-up is a general overview of the incident and its surroundings.
Summary (2 of 4) • During the primary assessment, determine and correct any life-threatening conditions. The steps of the primary assessment are to form a general impression of the patient, assess responsiveness, and perform a rapid scan that consists of checking and correcting problems with the patient’s airway, breathing, and circulation. Finally, update responding EMS units.
Summary (3 of 4) • A medical history provides a systematic account of the patient’s past medical conditions, illnesses, and injuries to determine the signs and symptoms of the current condition. • The secondary assessment of the patient consists of a secondary assessment of the entire body used to assess non-lifethreatening conditions.
Summary (4 of 4) • If the patient is stable, repeat the vital signs every 15 minutes. If the patient is unstable, repeat the vital signs every 5 minutes. • Provide a concise and accurate hand-off report to EMS personnel.
Review 1. Which of the following steps might be performed during the scene size-up? A. Assessing vital signs using appropriate monitoring devices B. Forming a general impression of the patient C. Notifying dispatch to send fire personnel D. Performing a full-body scan
Review Answer: C. notifying dispatch to send fire personnel
Review 2. The goal of the primary assessment is to A. quickly diagnose the patient’s condition. B. determine the need to perform a full-body assessment. C. determine the number of patients. D. identify and treat life threats.
Review Answer: D. identify and treat life threats.
Review 3. After performing a primary assessment and treating any immediate life threats, you should next A. determine the priority of patient care and transport. B. reassess the patient. C. recheck your interventions. D. promptly transport the patient to the closest hospital.
Review Answer: A. determine the priority of patient care and transport.
 National ems standards
National ems standards National quality standard assessment and rating instrument
National quality standard assessment and rating instrument Chapter 9 patient assessment worksheet answers
Chapter 9 patient assessment worksheet answers National ems advisory council
National ems advisory council Patient 2 patient
Patient 2 patient Chapter 9 patient education and health promotion
Chapter 9 patient education and health promotion Ems grade 9 term 3 case study
Ems grade 9 term 3 case study National patient safety goals 2012
National patient safety goals 2012 Patient safety incident policy
Patient safety incident policy National patient safety goal 6
National patient safety goal 6 National patient safety goal 6
National patient safety goal 6 National patient safety goals 2017
National patient safety goals 2017 2013 hospital national patient safety goals
2013 hospital national patient safety goals National patient safety framework
National patient safety framework National safety goal 6
National safety goal 6 First aid patient assessment
First aid patient assessment Emr patient assessment
Emr patient assessment Kleinman and campbell patient explanatory assessment model
Kleinman and campbell patient explanatory assessment model Secondary assessment
Secondary assessment Critical clipart
Critical clipart Banner mobility assessment tool
Banner mobility assessment tool Assessment of patient
Assessment of patient Introduction to ems systems chapter 1
Introduction to ems systems chapter 1 Ems systems chapter 1
Ems systems chapter 1 Personalized patient education
Personalized patient education éducation du patient définition
éducation du patient définition Patient handout template
Patient handout template Krames on demand patient education
Krames on demand patient education Krames living well with diabetes
Krames living well with diabetes Pre operative care
Pre operative care X-plain patient education
X-plain patient education Standard error for mean
Standard error for mean Definition of home language
Definition of home language Standard cost is predetermined cost
Standard cost is predetermined cost Standard kandungan dan standard pembelajaran
Standard kandungan dan standard pembelajaran 6 key priorities in health
6 key priorities in health National building information modeling standard
National building information modeling standard National standard 1
National standard 1 Nfpa 1600 standard
Nfpa 1600 standard National standard medication chart
National standard medication chart National standard for user applied labelling
National standard for user applied labelling National healthy housing standard
National healthy housing standard Nfpa business continuity
Nfpa business continuity Universal principles
Universal principles National unification and the national state
National unification and the national state Chapter 10 chemical reactions
Chapter 10 chemical reactions Chapter 11 chapter assessment stoichiometry answer key
Chapter 11 chapter assessment stoichiometry answer key Chapter 9 chapter assessment chemical reactions
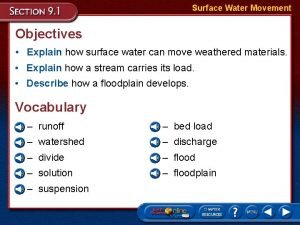
Chapter 9 chapter assessment chemical reactions Chapter 9 surface water answer key
Chapter 9 surface water answer key Chapter 2 chapter assessment representing motion
Chapter 2 chapter assessment representing motion Chapter 1 chapter assessment the central science
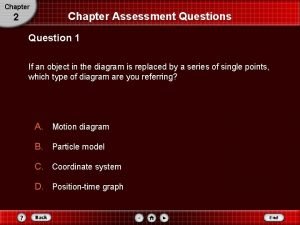
Chapter 1 chapter assessment the central science Chapter 2 chapter assessment
Chapter 2 chapter assessment Ionic compound properties
Ionic compound properties Chapter 7 chapter assessment ionic compounds and metals
Chapter 7 chapter assessment ionic compounds and metals National youth assessment study
National youth assessment study Pnac police
Pnac police National center for credibility assessment
National center for credibility assessment National center for credibility assessment
National center for credibility assessment Cm research
Cm research National center for credibility assessment
National center for credibility assessment