Perioperative Patient Assessment Microsoft Clipart Critical factors used








- Slides: 36
Perioperative Patient Assessment Microsoft Clipart
Critical factors used to determine pre-operative patient assessment • Patient is prepared Pre-operatively – Physiologic – Psychologic • Preparation should focus on : – – – Data collection (through patient assessment) Patient family teaching Emotional support Care plan for intra- and post-operative period Communication of information to the health care team (Surgeon, Anesthesiologist, Scrub Tech. etc. )
Planning • Begins with Patient Assessment • Desired outcomes: – That patient demonstrates knowledge of the procedure – Information should be provided to the patient during the Pre-operative phase during the assessment – Learning needs can only be assessed through an assessment process
Assessment • Physiologic: – – – – Medical Diagnosis Chronic Diseases Treatment (past and present) Medications (at home and present) Surgery to be performed Verification of the Surgical Site Any previous surgical procedures
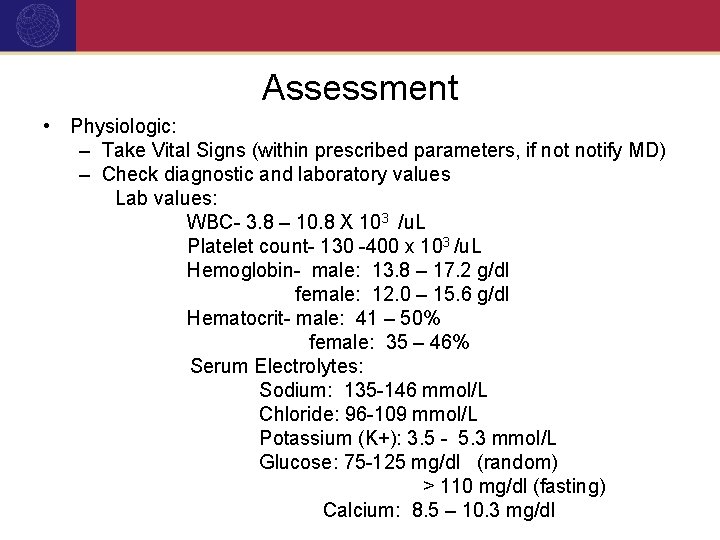
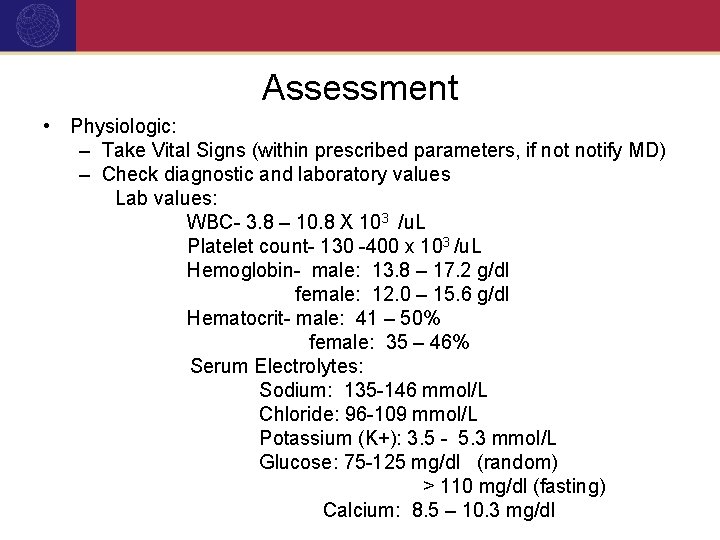
Assessment • Physiologic: – Take Vital Signs (within prescribed parameters, if notify MD) – Check diagnostic and laboratory values Lab values: WBC- 3. 8 – 10. 8 X 103 /u. L Platelet count- 130 -400 x 103 /u. L Hemoglobin- male: 13. 8 – 17. 2 g/dl female: 12. 0 – 15. 6 g/dl Hematocrit- male: 41 – 50% female: 35 – 46% Serum Electrolytes: Sodium: 135 -146 mmol/L Chloride: 96 -109 mmol/L Potassium (K+): 3. 5 - 5. 3 mmol/L Glucose: 75 -125 mg/dl (random) > 110 mg/dl (fasting) Calcium: 8. 5 – 10. 3 mg/dl
Assessment Lab values: PT (partial thromboplastin): 10 – 12. 5 sec PTT (Partial thromboplastin time): 20 -36 sec. Microsoft Clipart

Assessment Urinalysis Appearance: clear, yellow WBC: negative Specific gravity: 1. 001 – 1. 035 nitrite: negative PH: 4. 6 - 8. 0 WBC: < 5 high/power field Protein: negative RBC< 3 high power field Glucose: negative Renal epithelial cells: < 3/ hpf Reducing Substances: negative Squamous epithelial cells: none or few Ketones: negative Casts: none Bilirubin: negative Bacteria: none Occult Blood: negative Yeast: none WBC: negative
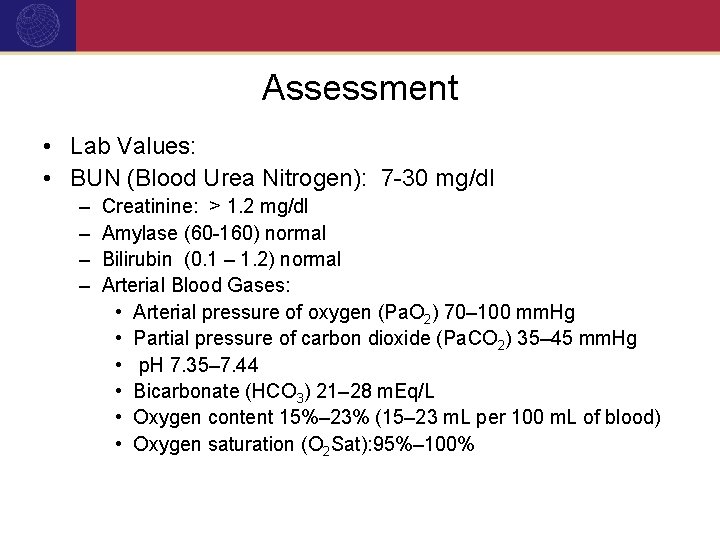
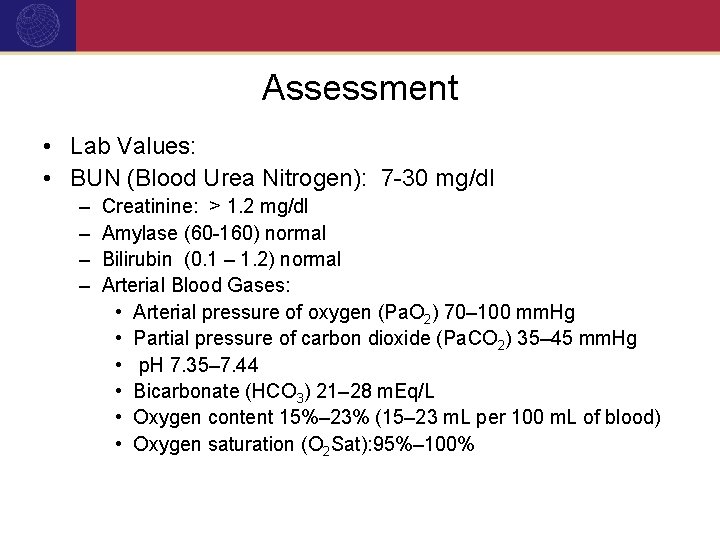
Assessment • Lab Values: • BUN (Blood Urea Nitrogen): 7 -30 mg/dl – – Creatinine: > 1. 2 mg/dl Amylase (60 -160) normal Bilirubin (0. 1 – 1. 2) normal Arterial Blood Gases: • Arterial pressure of oxygen (Pa. O 2) 70– 100 mm. Hg • Partial pressure of carbon dioxide (Pa. CO 2) 35– 45 mm. Hg • p. H 7. 35– 7. 44 • Bicarbonate (HCO 3) 21– 28 m. Eq/L • Oxygen content 15%– 23% (15– 23 m. L per 100 m. L of blood) • Oxygen saturation (O 2 Sat): 95%– 100%

Assessment – – – Age specific Substance Abuse (smoking, alcohol, drugs) Skin condition (color, rashes, lesions) Allergies- check for medication, food, latex? Nutritional status prior to surgery Previous reactions to anesthesia? IV, NG, foley or any drain present pre-op Check for NPO status Sensory impairments (hearing aids, contacts, glasses, dentures) Mobility impairment? Prosthetic devices Weight and height

Assessment • Diagnostic Tests: – – Chest X-ray EKG Diagnostic x-ray’s pertinent to surgical procedure Results of specific tests or studies specific to the planned procedure Microsoft Clipart
Assessment – Type and Crossmatch information/availability of replacement units of blood (if applicable) Microsoft Clipart – Check for completed History & Physical Versant Advantage, Inc. 2006
Assessment • IV drip started? ©Kendall Tyco, used by permission Microsoft Clipart
Assessment • Assess level of risk for DVT (general surgery patients have evidence of a 10 -40% increased chance of developing DVT and orthopedic patients have a 40 -60% chance of developing DVT) • Assess the following: – Is the patient elderly? – History of cancer? – Traveled recently? – Immobile while awaiting surgery? – Trauma patient? – Orthopedic patient?

Assessment • What type of case, and risk level as indicated: – If patient is < 40 years of age: no specific prophylaxis is taken – Patient 40 -60 years of age, moderate risk: LDUH (Low dose unit heparin) or LMWH (low molecular weight heparin) recommended and or compression stockings (TED) or pneumatic device (SCDSequential Compression Device) stockings – Patient > 60 years of age, high risk: LDUH or LMWH or SCD stockings – Multiple risk patients – ortho or trauma patients, utilize all of the above prevention measures. • SCD stockings are critical. ©Kendall Tyco, used by permission
Nursing Diagnosis • Most common: anxiety and deficit knowledge related to perioperative routines, surgical procedure or outcomes expectations – Due to: knowledge deficit, language barrier, communication ability, impaired mental capacity, lack of information – Nursing Interventions: appropriate to the cause of the patient knowledge deficit and learning deficit
Nursing Interventions to address knowledge deficit • • Confirm patient identification Verify surgical procedure and site Verify surgical consent Verify/confirm patient’s perception of the planned surgery Ask questions related to patients surgery Explain the surgical routine Explain the procedures that are to be followed post-op, upon discharge. • Provide appropriate information for the patient’s level of understanding/ability to comprehend, as well as medical questions to relate to surgeon • Request feedback regarding perioperative procedure
Nursing Diagnosis • Anxiety may range from mild to severe. – Signs and symptoms: increased B/P, increased heart rate – Maybe unable to focus or concentrate – May exhibit fear, but usually marked by apprehension • Anticipatory grieving due to possible changes in patient body image
Nursing Interventions for anxiety/fear of surgery • Listen! • Provide information as needed • Provide information to solicit information of anxiety or fear • Provide emotional support and reassurance to patient • Important to assess readiness to learn. Do not provide more information than the patient can assume
Nursing Diagnosis Intra-operative • Many nursing diagnosis may be related to injuries from positioning, transport, transfer, electrosurgical unit, equipment, x-ray, laser, sponges left in, and injury to chemical agents (ex. Prep solutions) • High risk for infection • Fluid/electrolyte imbalance • Impaired gas exchange related to anesthesia

Desired Patient Outcomes • In relation to knowledge deficit: is the patient will demonstrate knowledge of the psychological and physiologic responses to the surgery • In relation to anxiety and fear: will be lessened through knowledge and expression of feelings.

Criteria to Evaluate Outcomes • • • Confirm consent Describe sequence of events Express feelings of the surgical procedure Indicate knowledge of surgical procedure Confirm procedures upon discharge
Patient Advocacy • Verify patient identity • Verify correct surgical site/”time out” procedure (to be discussed at more depth in Periop Safety module) • Confirm patient identity – Verbally – Checking arm band – Unable to communicate- verify with family or authorized individual and chart review – Verify surgical procedure

Patient Family Teaching • Began at pre-admission workup • If patient can’t be involved, patient’s family then must be involved • Teaching must be appropriate to the patient’s/family’s ability and readiness to understand learn • Consideration of patients age is a must for teaching to be implemented
Patient Family Teaching • Plan additional time necessary when dealing elderly and children • Provide appropriate teaching materials • Provide age appropriate teaching, ie. Children under 7 years of age, may view illness/surgery as punishment • Provide children with the opportunity to touch and manipulate items such as anesthesia mask, dressing on bear/doll etc.
Patient Family Teaching • At minimum should include the following: – Procedure, time frame of, and outcome expectation – Specific post-op instructions (bath, shower, stair climbing, NPO status etc. ) – Explanation of Post-Op events (expected time in PACU, IV, NPO status- amount of time) – Post-op events: LOS, coughing and deep breathing, drains, catheters, pain control, expected time of discharge
Patient Family Teaching • Must be began in pre-operative area • Needs to be reinforced post-op (because of pre-op anxiety) • Provide pre-op emotional support and reassurance • Provide an attentive, caring attitude, touch, comfort and reassurance
Communication of Data to Surgical Team Members • Communicate information to all surgical team members to provide continuity of care. • Documentation of findings and verbal communication is a must to provide ongoing care • Documentation may be stand alone forms or part of the integrated Perioperative Record. • Documentation must include at the minimum: – Pre – Intra – Postoperative periods
AORN Recommended Standards and Practices for Documentation of Perioperative Care • Recommended Practice I: “The patient’s record should reflect the patient’s plan of care including assessment, diagnosis, outcome identification, planning, implementation and evaluation”

AORN Recommended Standards and Practices for Documentation of Perioperative Care • Recommended Practice II: “Policies and procedures for documenting perioperative nursing care should be written, reviewed periodically, revised as necessary and readily available within the practice setting”
AORN Recommended Standards and Practices for Documentation of Perioperative Care • Should include but not limited to the following: – – – – Operative Record Pre-Operative Perioperative Checklist Nurse’s notes Flow charts Care plans Implant records Laser logs
View Cine Med “Perioperative Patient Assessment” Video Microsoft Clipart
Patient Assessment Scenario • An 82 year old male arrives to the Pre-Op Holding Area. His wife makes you aware that he has dementia/Alzheimer's. You note that he is confused as to place and time, but calls his wife by name. He is scheduled for a Cholecystectomy with possible common bile duct exploration. He has a peripheral IV in his right forearm with 800 cc of NS. You note the following after reviewing the patient’s chart:
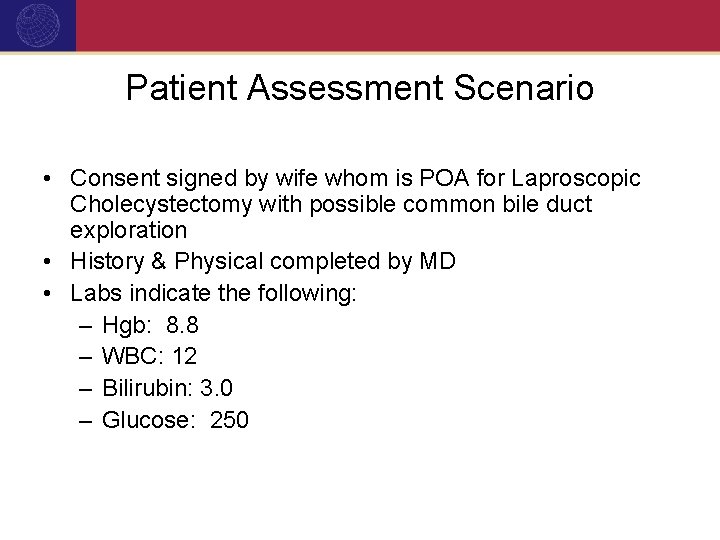
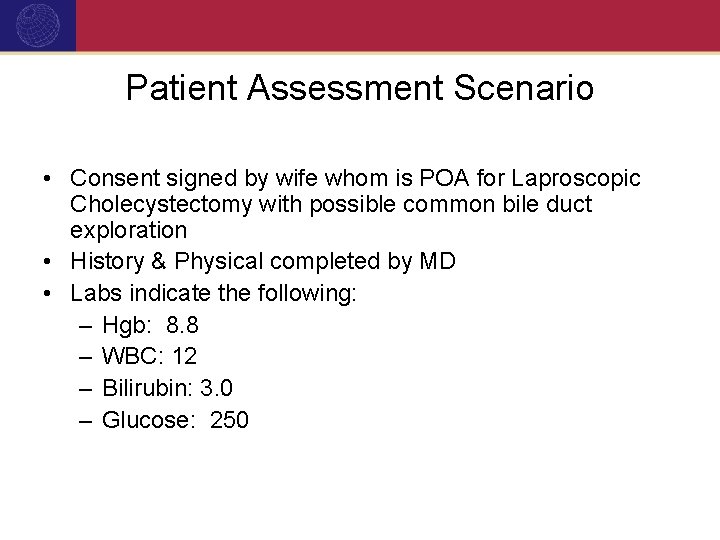
Patient Assessment Scenario • Consent signed by wife whom is POA for Laproscopic Cholecystectomy with possible common bile duct exploration • History & Physical completed by MD • Labs indicate the following: – Hgb: 8. 8 – WBC: 12 – Bilirubin: 3. 0 – Glucose: 250
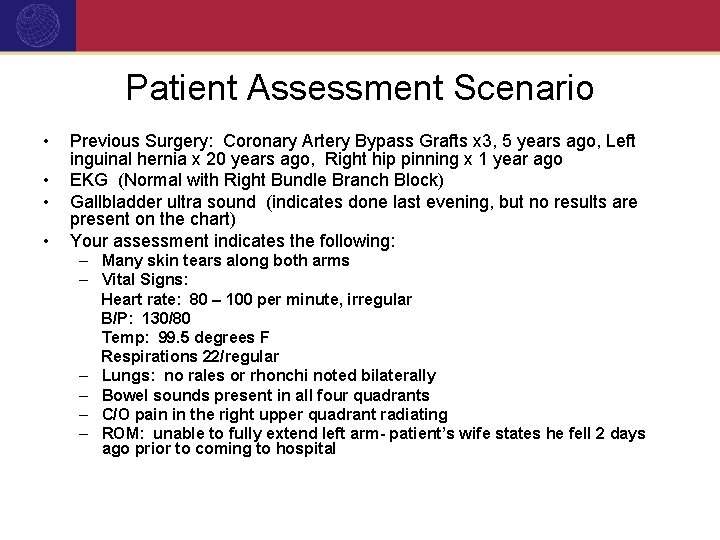
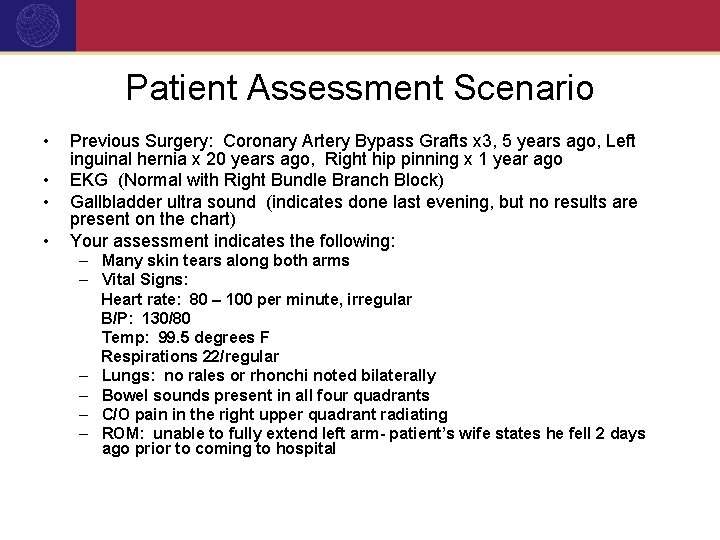
Patient Assessment Scenario • • Previous Surgery: Coronary Artery Bypass Grafts x 3, 5 years ago, Left inguinal hernia x 20 years ago, Right hip pinning x 1 year ago EKG (Normal with Right Bundle Branch Block) Gallbladder ultra sound (indicates done last evening, but no results are present on the chart) Your assessment indicates the following: – Many skin tears along both arms – Vital Signs: Heart rate: 80 – 100 per minute, irregular B/P: 130/80 Temp: 99. 5 degrees F Respirations 22/regular – Lungs: no rales or rhonchi noted bilaterally – Bowel sounds present in all four quadrants – C/O pain in the right upper quadrant radiating – ROM: unable to fully extend left arm- patient’s wife states he fell 2 days ago prior to coming to hospital
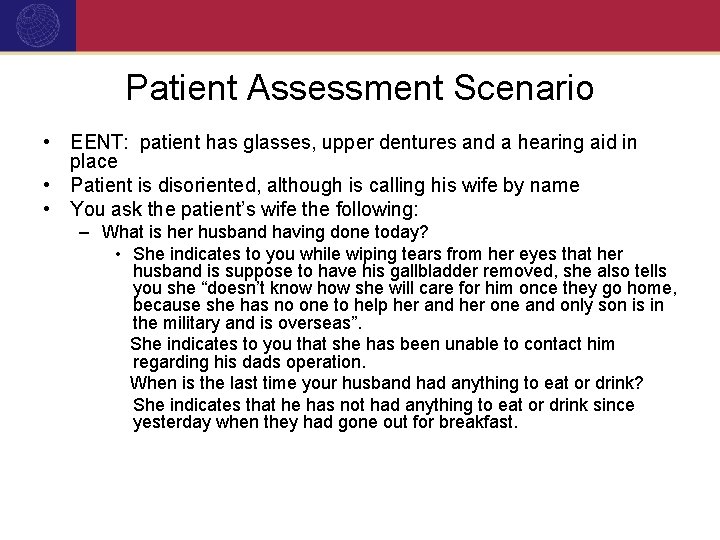
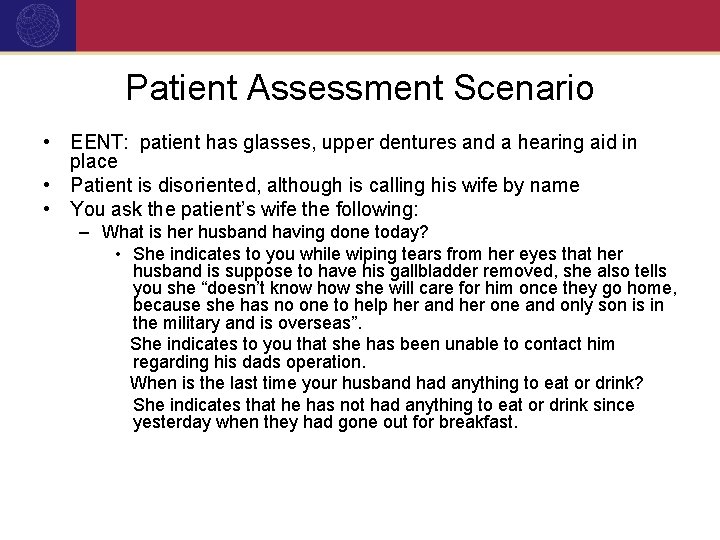
Patient Assessment Scenario • EENT: patient has glasses, upper dentures and a hearing aid in place • Patient is disoriented, although is calling his wife by name • You ask the patient’s wife the following: – What is her husband having done today? • She indicates to you while wiping tears from her eyes that her husband is suppose to have his gallbladder removed, she also tells you she “doesn’t know how she will care for him once they go home, because she has no one to help her and her one and only son is in the military and is overseas”. She indicates to you that she has been unable to contact him regarding his dads operation. When is the last time your husband had anything to eat or drink? She indicates that he has not had anything to eat or drink since yesterday when they had gone out for breakfast.
Patient Assessment Scenario • What nursing diagnosis do you determine from your Pre-Operative assessment? • What if anything should you report to the MD and how soon? • What should the surgical team be notified of if anything? • What are your nursing interventions in the Pre. Operative/Holding Area? • What are your outcome goals?
 Patient assessment clipart
Patient assessment clipart Phases of perioperative nursing
Phases of perioperative nursing Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Semi critical
Semi critical Abiotic factors clipart
Abiotic factors clipart Performance based assessment clipart
Performance based assessment clipart Patient 2 patient
Patient 2 patient Perioperative definition
Perioperative definition Perioperative nursing case study
Perioperative nursing case study Ccs perioperative guidelines
Ccs perioperative guidelines Preoperative nursing definition
Preoperative nursing definition Compare non-critical readers with critical readers.
Compare non-critical readers with critical readers. Factors of care patients can expect
Factors of care patients can expect First aid patient assessment
First aid patient assessment Emr patient assessment
Emr patient assessment Kleinman and campbell patient explanatory assessment model
Kleinman and campbell patient explanatory assessment model Opqrst sample
Opqrst sample Chapter 9: patient assessment worksheet answers
Chapter 9: patient assessment worksheet answers Bmat tool
Bmat tool Assessment of patient
Assessment of patient Microsoft project critical path tutorial
Microsoft project critical path tutorial The method used for transferring a patient depends on
The method used for transferring a patient depends on Nursing positions supine
Nursing positions supine Entrepreneurial venture
Entrepreneurial venture Chapter 6 feasibility study
Chapter 6 feasibility study Contoh critical incident asn
Contoh critical incident asn Halpern critical thinking assessment
Halpern critical thinking assessment Which modifier is used to control access to critical code
Which modifier is used to control access to critical code Microsoft official academic course microsoft word 2016
Microsoft official academic course microsoft word 2016 Microsoft official academic course microsoft excel 2016
Microsoft official academic course microsoft excel 2016 Edge startwarren theverge
Edge startwarren theverge Microsoft excel merupakan program aplikasi yang disebut
Microsoft excel merupakan program aplikasi yang disebut Microsoft official academic course microsoft word 2016
Microsoft official academic course microsoft word 2016 Site and situation factors
Site and situation factors Abiotic and biotic
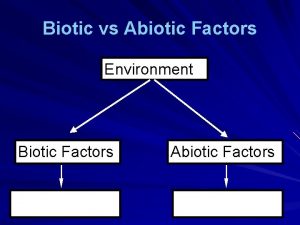
Abiotic and biotic Abiotic vs biotic factors
Abiotic vs biotic factors Abiotic factors and biotic factors
Abiotic factors and biotic factors