CAUTI Prevention Definition of CAUTI Urinary tract infection



- Slides: 22

CAUTI Prevention
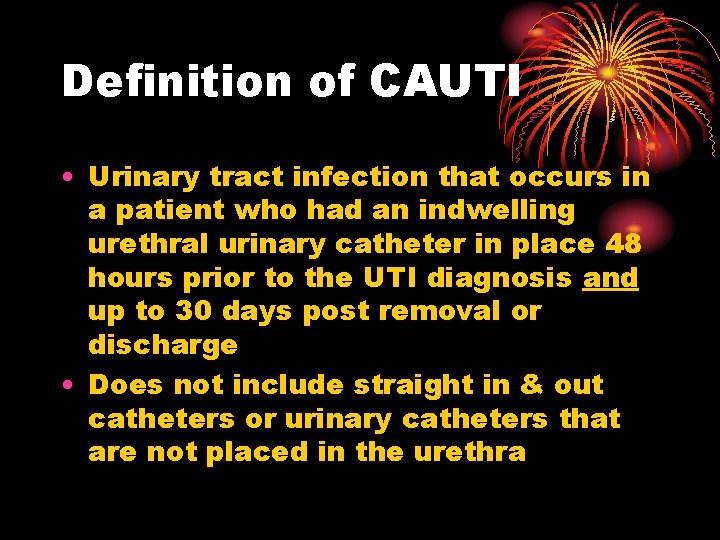
Definition of CAUTI • Urinary tract infection that occurs in a patient who had an indwelling urethral urinary catheter in place 48 hours prior to the UTI diagnosis and up to 30 days post removal or discharge • Does not include straight in & out catheters or urinary catheters that are not placed in the urethra
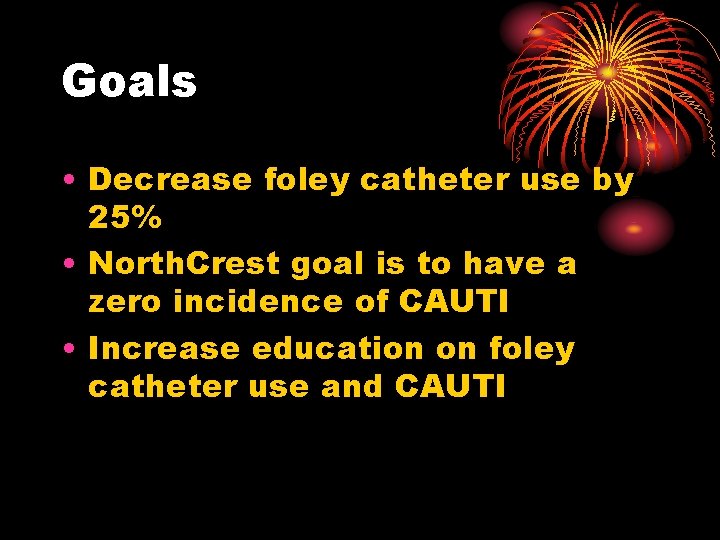
Goals • Decrease foley catheter use by 25% • North. Crest goal is to have a zero incidence of CAUTI • Increase education on foley catheter use and CAUTI
Background • Urinary Tract Infections (UTI’s) are the most common site of HAI’s • Most UTI’s (80%) are associated with urinary catheterization instrumentation • UTI’s lead to increased morbidity, mortality, LOS and cost
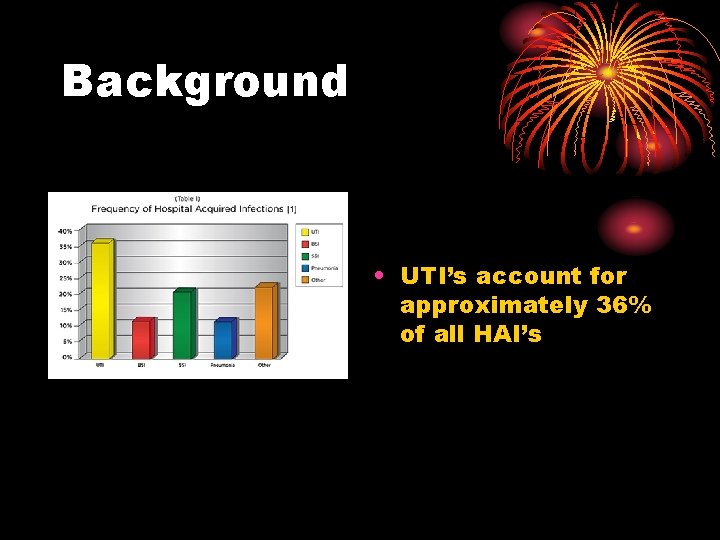
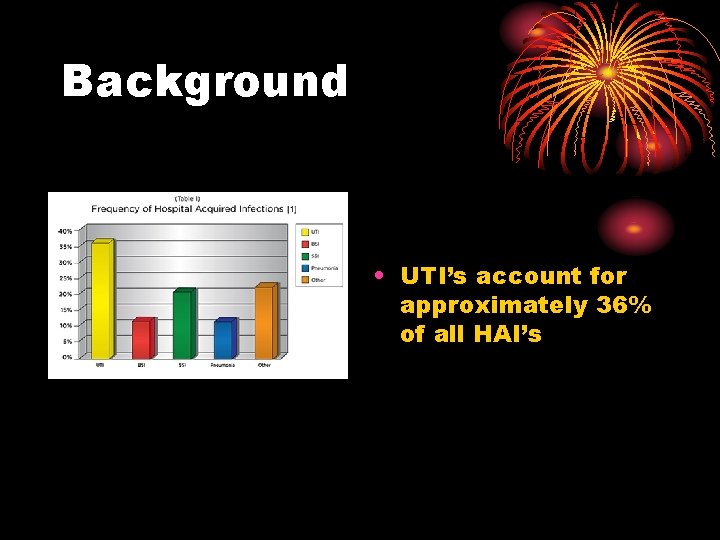
Background • UTI’s account for approximately 36% of all HAI’s
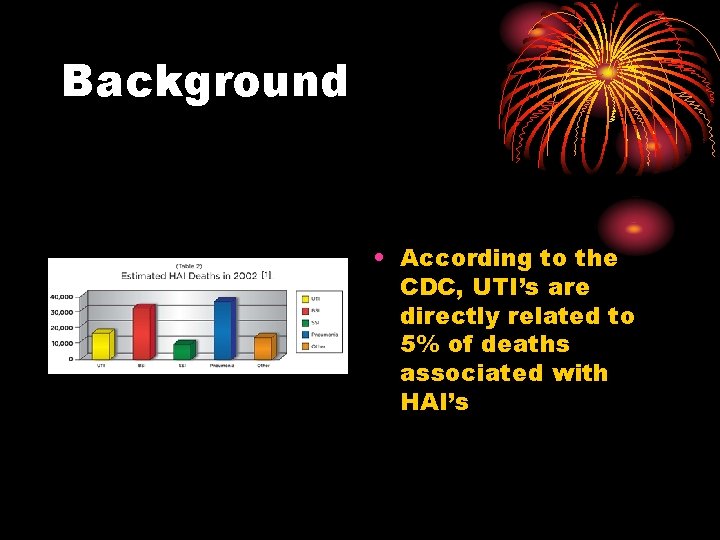
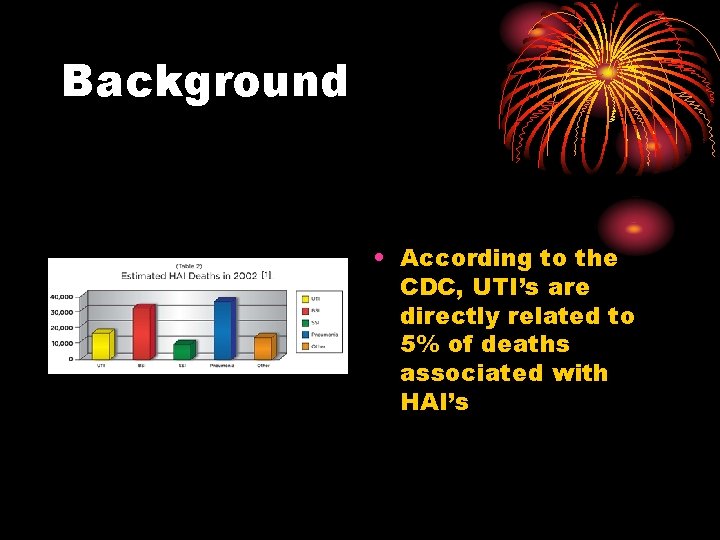
Background • According to the CDC, UTI’s are directly related to 5% of deaths associated with HAI’s
Eliminate CAUTI: One infection at a time • Appropriate Indications: Does this patient need the catheter? • Ensure patient meets appropriate indications for catheter use and document reason • Consider alternatives to indwelling urethral catheterization
Hand Hygiene: It starts with the hands • PRACTICE HAND HYGIENE and standard precautions • Sanitize hands thoroughly with an alcohol-based hand rub or soap and water before and after catheter insertion and manipulation

Insertion Technique: Pay attention to detail • Use sterile equipment including, sterile gloves, drape, sponges, and appropriate antiseptic solution • Use aseptic technique to insert catheter. If aseptic technique is broken, replace catheter and collection system aseptically with sterile equipment • Secure catheter to prevent movement and urethral traction
Catheter Maintenance: Keep it neat • Keep collection bag below level of the bladder at all times • Check tubing frequently for kinking • Keep drainage bag/tubing off the floor • Empty the collection bag every four hours or when ½ to 2/3 full • Maintain a closed-drainage system
Catheter Care: Keep it clean • Perform perineal care daily and after each bowel movement • Soap and water or perineal cleansing wipes will be utilized • Special care will be taken to remove fecal soiling from around the catheter by cleaning fecal material away from the urinary meatus
Catheter removal: Get it Out! • Assess patient every shift for catheter need • Take steps to remove catheter when patient no longer meets indications • Early removal of catheter using reminders or stop-order “stickers”
Indications for catheter use • Insert catheters only for appropriate indications • Management of acute urinary retention • Post-op bladder decompression for 48 hours • Surgery procedure • Monitoring urinary output in acutely ill patient
Indications for catheter use • Contamination of stage III or IV pressure ulcers with urine which has impeded healing, despite appropriate care for incontinence • Terminal illness or severe impairment which makes positioning or clothing changes uncomfortable, or which is associated with intractable pain • Other – MD clarification required
Alternatives • Alternatives to indwelling catheter • Bladder ultrasound • Intermittent catheterization • Condom catheter

Organisms enter the bladder by 3 ways: • At time of catheter insertion • Through the catheter lumen (from a colonized drainage bag) • Along external surface of the catheter (migrate along the catheter-mucosal interface)
Prevention • Use general infection control practices • Aseptic insertion • Proper maintenance • Hand hygiene • Nurse driven Catheter Removal Protocol • Education
Implementation of Evidence. Based Prevention Strategies • Make sure the catheter is indicated • Implement and promote alternatives to indwelling urinary catheterization • Perform hand hygiene in compliance with CDC • Provide education on proper insertion and maintenance • Limit insertion of catheters to trained personnel • Insert catheters using aseptic technique and sterile equipment
Implementation of Evidence. Based Prevention Strategies • Secure catheter to prevent movement and urethral traction • Maintain closed drainage system • Maintain unobstructed urine flow • Remove catheters with 48 hours following surgical procedure or document reason for extended use • Remove unnecessary catheters
Documentation • Accurate documentation on the Urinary Catheter Assessment in HMS • Document medical indications for placement • Insertion documentation (size of catheter used, patient response, amount & color or urine obtained, etc…) • Assess patient every shift for foley catheter removal – includes scoring indications for maintenance of foley • Discontinuation of urinary catheter documentation – includes Bladder scanner Clinical pathway documentation • New alert sticker in physician orders to remind physicians to discontinue foley catheters
Lessons Learned • Use evidenced-based, standardized, protocols and guidelines • Build redundancy into the process – new alert sticker placed in physician orders • Define and enforce accountability • Push accountability to the front line staff
Conclusions • CAUTI is a common and costly safety problem • Several practices appear to decrease CAUTI • Preventing CAUTI is a “team” effort
 Complicated uti symptoms
Complicated uti symptoms Complicated urinary tract infection
Complicated urinary tract infection Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Urised otc
Urised otc Bladder infection symptoms
Bladder infection symptoms Cauti prevention bundle checklist
Cauti prevention bundle checklist Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Urinary tract obstruction
Urinary tract obstruction Urinary bladder
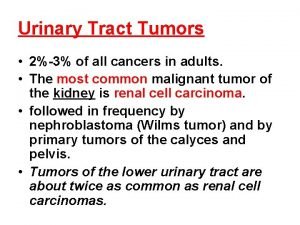
Urinary bladder Tumor in the urinary tract
Tumor in the urinary tract Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Lrti
Lrti Nursing management of reproductive tract infection
Nursing management of reproductive tract infection Pyramidal vs extrapyramidal tract
Pyramidal vs extrapyramidal tract Anterior spinothalamic tract
Anterior spinothalamic tract Stop cauti
Stop cauti Pico question for cauti
Pico question for cauti Puncture resistant container
Puncture resistant container Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 16 infection prevention and control
Chapter 16 infection prevention and control Define infection prevention chapter 5
Define infection prevention chapter 5 Infection control meaning
Infection control meaning