On the CUSP Stop CAUTI National Expansion Implementing

- Slides: 49
On the CUSP: Stop CAUTI National Expansion: Implementing CUSP to Eliminate Catheter-Associated Urinary Tract Infections (CAUTI) Project Initiation Call 1
Overview of Today’s Call • Welcome and introductions • Why this initiative is important: Overview of CAUTI • Comprehensive Unit-Based Safety Program (CUSP) • Project overview and data requirements – Expected outcomes – What it requires • What are the next steps 2
Project Goals • Reduce CAUTI rates in participating units by 25% – Appropriate placement – Appropriate continuance – Appropriate utilization • Improve patient safety culture on participating units 3
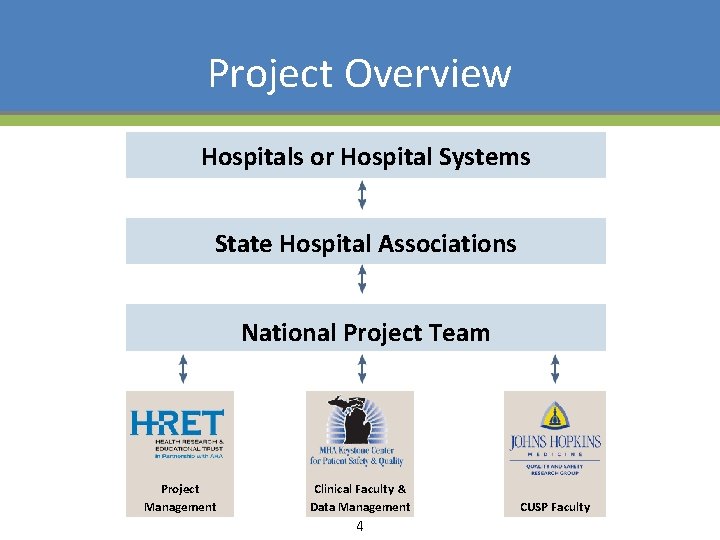
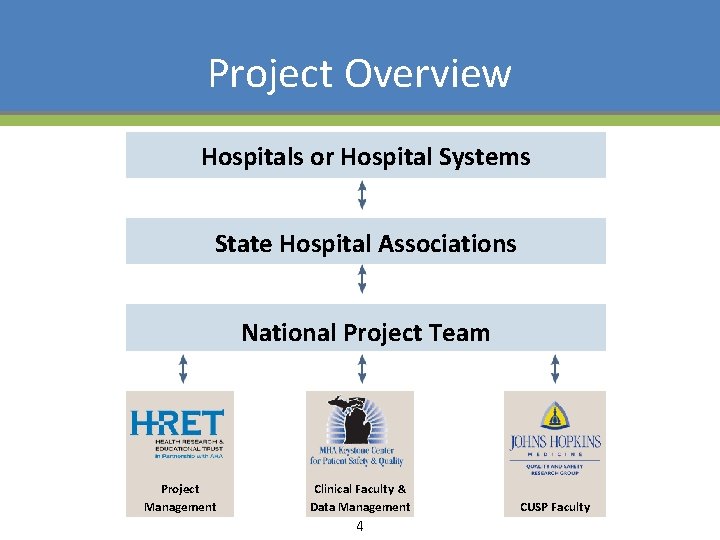
Project Overview Hospitals or Hospital Systems State Hospital Associations National Project Team Project Management Clinical Faculty & Data Management 4 CUSP Faculty
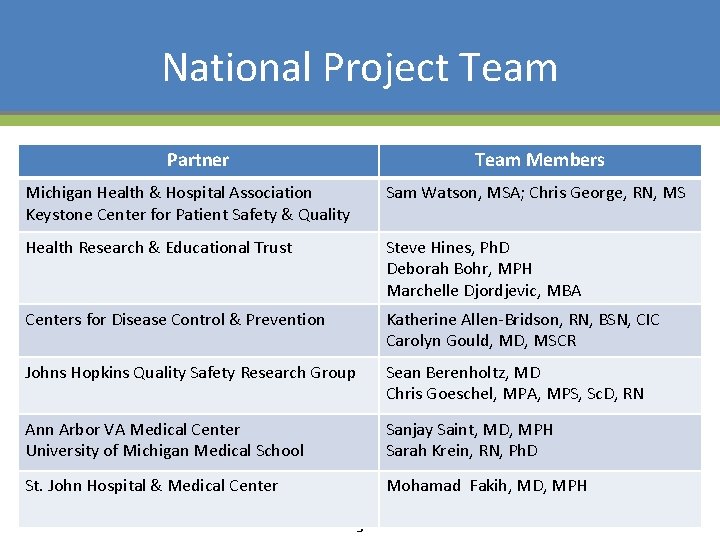
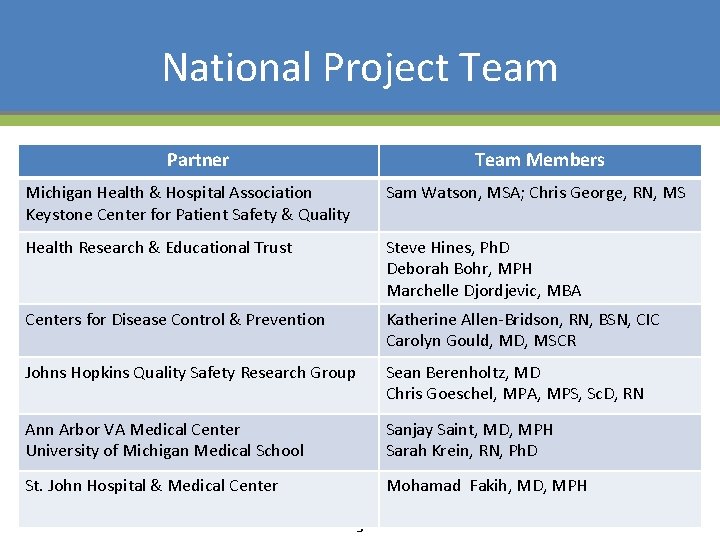
National Project Team Partner Team Members Michigan Health & Hospital Association Keystone Center for Patient Safety & Quality Sam Watson, MSA; Chris George, RN, MS Health Research & Educational Trust Steve Hines, Ph. D Deborah Bohr, MPH Marchelle Djordjevic, MBA Centers for Disease Control & Prevention Katherine Allen-Bridson, RN, BSN, CIC Carolyn Gould, MD, MSCR Johns Hopkins Quality Safety Research Group Sean Berenholtz, MD Chris Goeschel, MPA, MPS, Sc. D, RN Ann Arbor VA Medical Center University of Michigan Medical School Sanjay Saint, MD, MPH Sarah Krein, RN, Ph. D St. John Hospital & Medical Center Mohamad Fakih, MD, MPH 5
Healthcare-Associated Infections (HAI’s) • At least 20% of episodes are preventable; perhaps as much as 70% (Harbath et al. J Hosp Infect 2003) • Medicare no longer reimburses U. S. hospitals for the additional costs of certain infections • Preventive practices are variably used • The most common HAI is urinary tract infection 6
Urinary Catheter-Related Infection: Background • Urinary tract infection (UTI) causes ~ 40% of hospitalacquired infections • Most infections due to urinary catheters • Up to 25% of inpatients are catheterized • Leads to increased morbidity and costs 7
Clinical Manifestations of CAUTI • Clinical manifestations vary greatly • Asymptomatic bacteriuria overwhelming sepsis • Symptomatic UTI: – Lower abdominal, suprapubic, or flank pain – Systemic symptoms: nausea, vomiting, fever 8
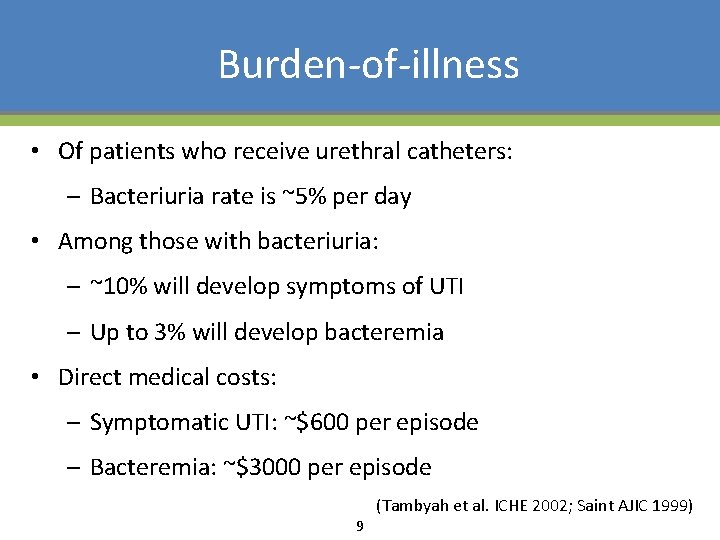
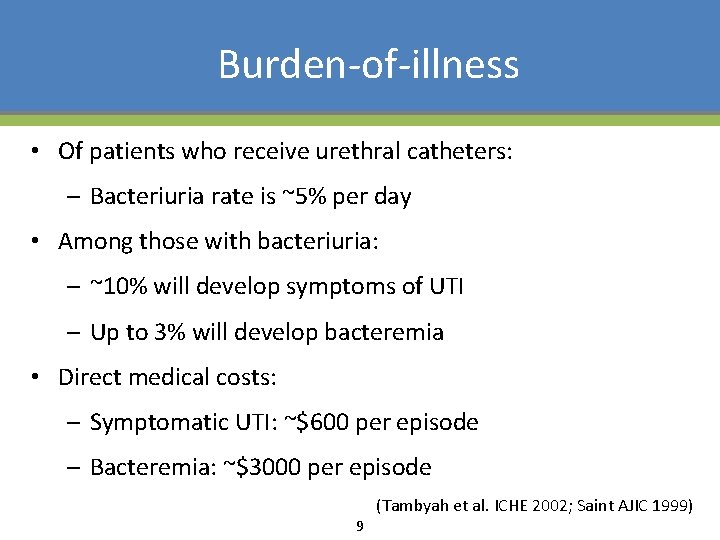
Burden-of-illness • Of patients who receive urethral catheters: – Bacteriuria rate is ~5% per day • Among those with bacteriuria: – ~10% will develop symptoms of UTI – Up to 3% will develop bacteremia • Direct medical costs: – Symptomatic UTI: ~$600 per episode – Bacteremia: ~$3000 per episode 9 (Tambyah et al. ICHE 2002; Saint AJIC 1999)
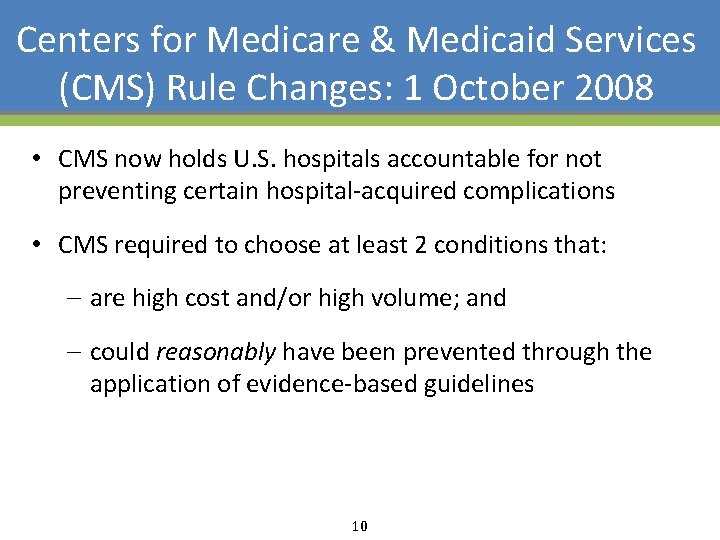
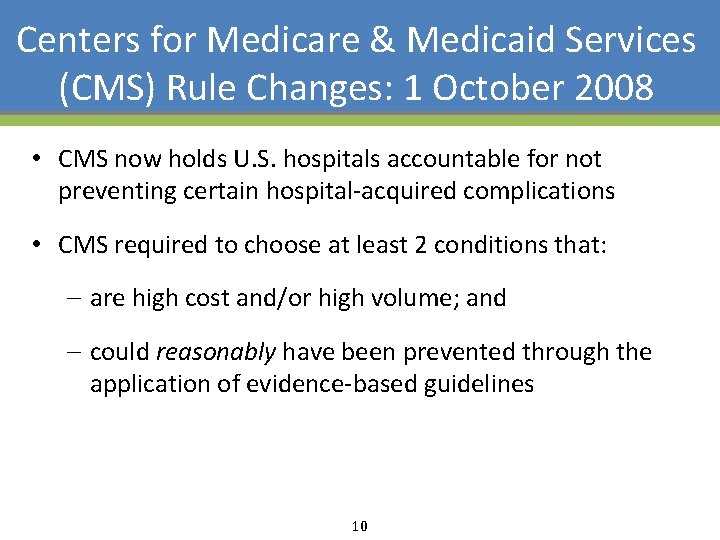
Centers for Medicare & Medicaid Services (CMS) Rule Changes: 1 October 2008 • CMS now holds U. S. hospitals accountable for not preventing certain hospital-acquired complications • CMS required to choose at least 2 conditions that: – are high cost and/or high volume; and – could reasonably have been prevented through the application of evidence-based guidelines 10
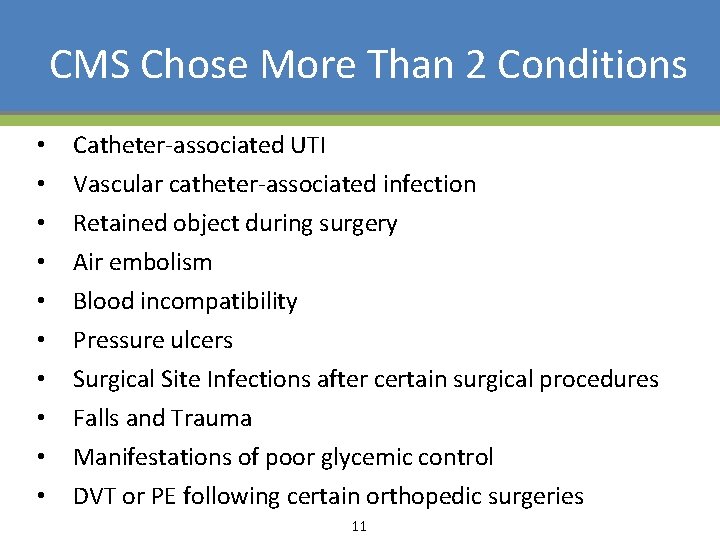
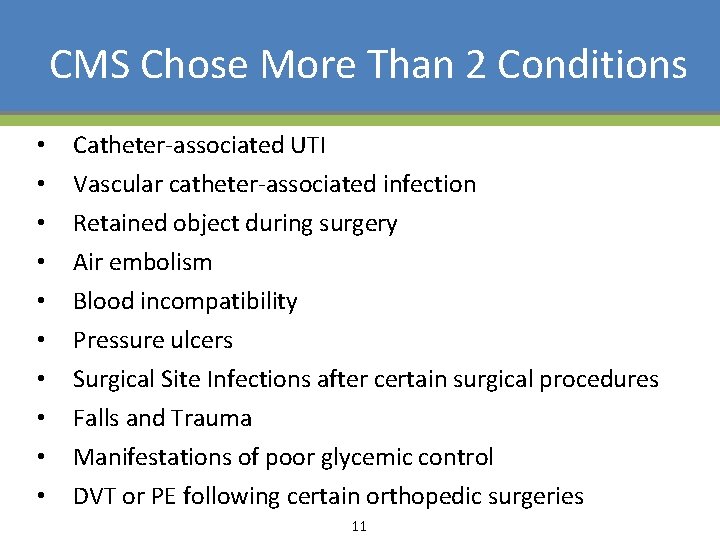
CMS Chose More Than 2 Conditions • • • Catheter-associated UTI Vascular catheter-associated infection Retained object during surgery Air embolism Blood incompatibility Pressure ulcers Surgical Site Infections after certain surgical procedures Falls and Trauma Manifestations of poor glycemic control DVT or PE following certain orthopedic surgeries 11
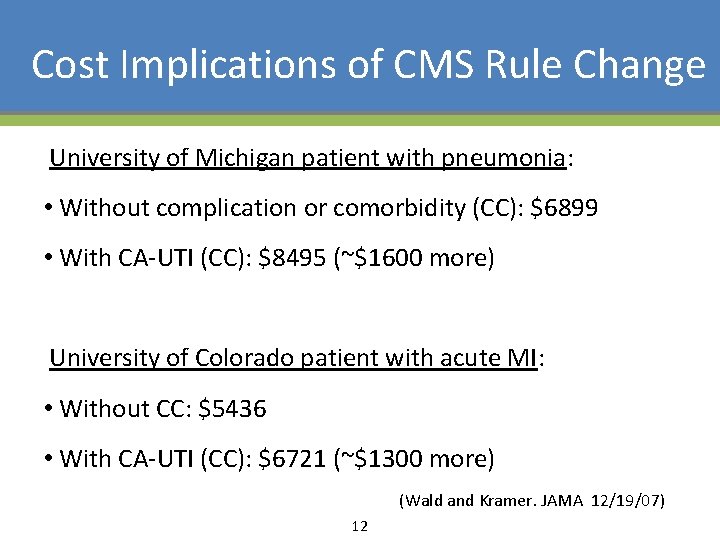
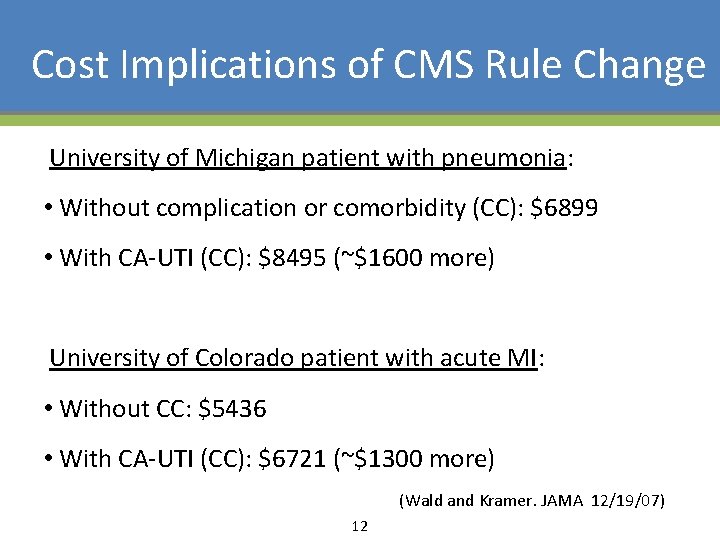
Cost Implications of CMS Rule Change University of Michigan patient with pneumonia: • Without complication or comorbidity (CC): $6899 • With CA-UTI (CC): $8495 (~$1600 more) University of Colorado patient with acute MI: • Without CC: $5436 • With CA-UTI (CC): $6721 (~$1300 more) (Wald and Kramer. JAMA 12/19/07) 12
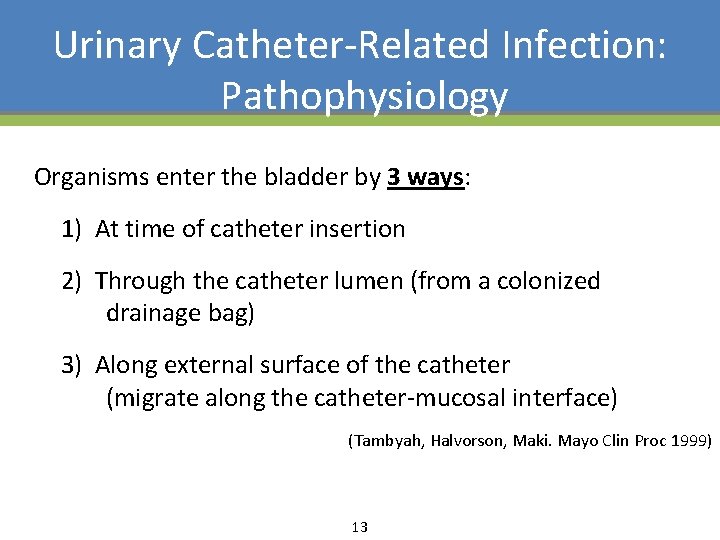
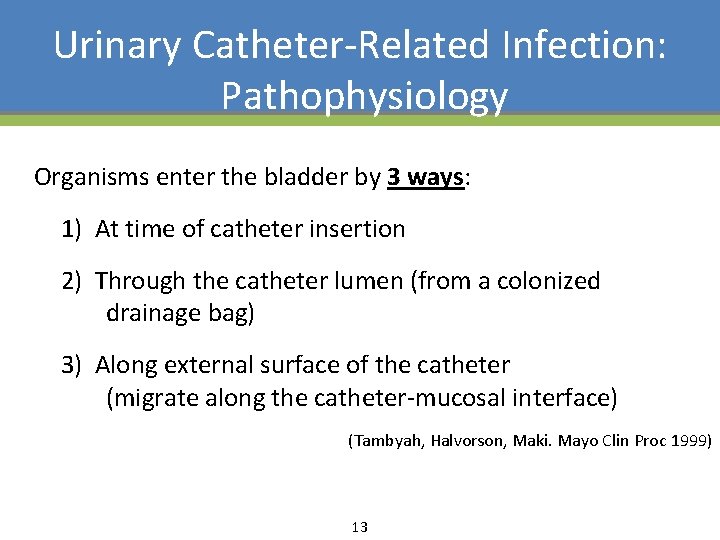
Urinary Catheter-Related Infection: Pathophysiology Organisms enter the bladder by 3 ways: 1) At time of catheter insertion 2) Through the catheter lumen (from a colonized drainage bag) 3) Along external surface of the catheter (migrate along the catheter-mucosal interface) (Tambyah, Halvorson, Maki. Mayo Clin Proc 1999) 13
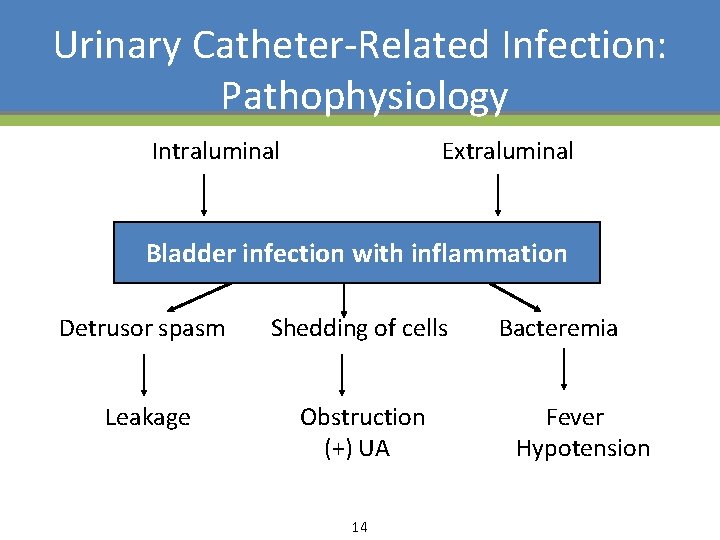
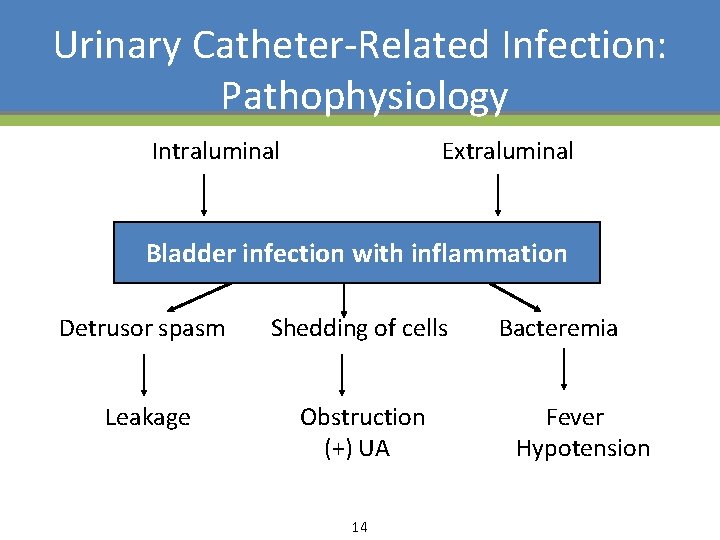
Urinary Catheter-Related Infection: Pathophysiology Intraluminal Extraluminal Bladder infection with inflammation Detrusor spasm Shedding of cells Bacteremia Leakage Obstruction (+) UA Fever Hypotension 14
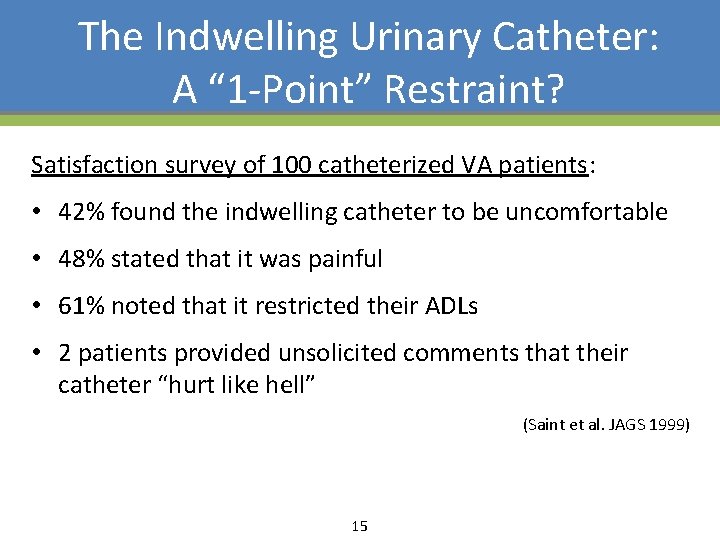
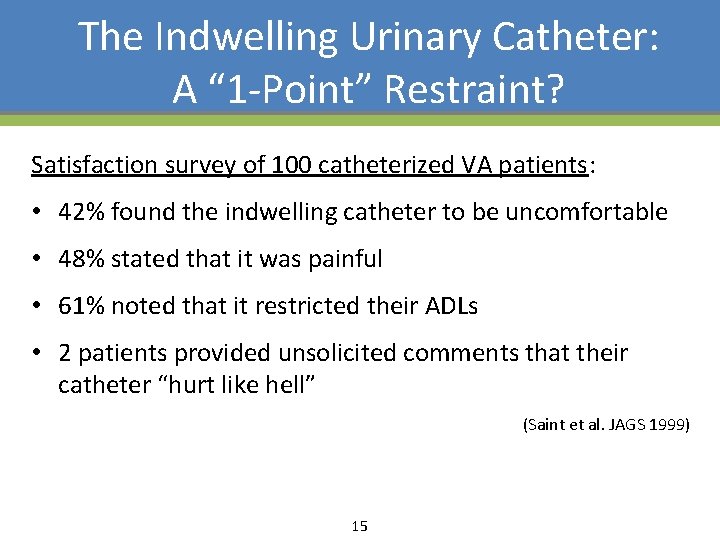
The Indwelling Urinary Catheter: A “ 1 -Point” Restraint? Satisfaction survey of 100 catheterized VA patients: • 42% found the indwelling catheter to be uncomfortable • 48% stated that it was painful • 61% noted that it restricted their ADLs • 2 patients provided unsolicited comments that their catheter “hurt like hell” (Saint et al. JAGS 1999) 15
Catheter-Associated Urinary Tract Infection • Background • Prevention 16
Prevention of Catheter- Associated UTI ü Make sure the catheter is indicated • Adhere to general infection control principles (eg, aseptic insertion, proper maintenance, hand hygiene, education, feedback) • Remove the catheter as soon as possible • Consider other methods of prevention 17
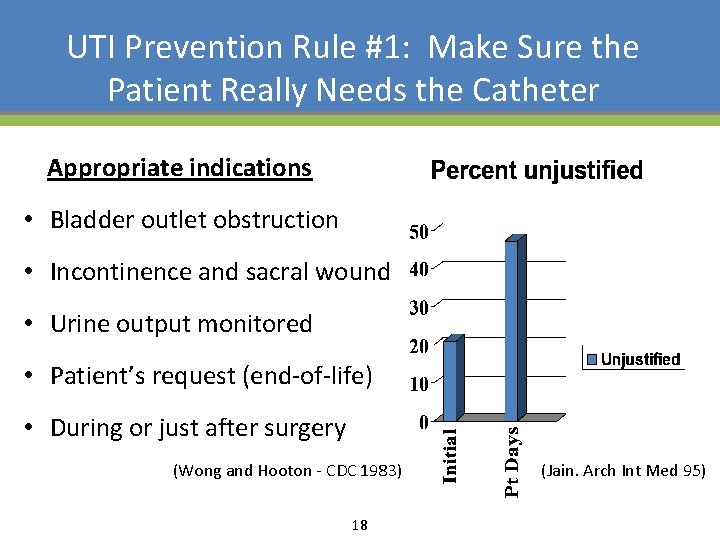
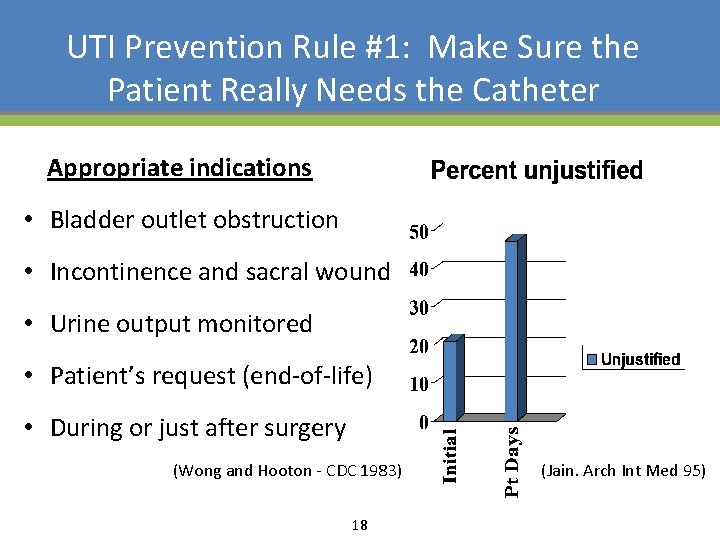
UTI Prevention Rule #1: Make Sure the Patient Really Needs the Catheter Appropriate indications • Bladder outlet obstruction • Incontinence and sacral wound • Urine output monitored • Patient’s request (end-of-life) • During or just after surgery (Wong and Hooton - CDC 1983) 18 (Jain. Arch Int Med 95)
Why are Catheters Used Inappropriately? • Perhaps physicians “forget” that their patient has a urinary catheter • We determined the extent to which doctors are aware which of their inpatients have catheters • Surveyed 56 medical teams at 4 sites (Saint S, Wiese J, Amory J, et al. Am J Med 2000) 19
One Reason Catheters Are Used Inappropriately (Saint S, Wiese J, Amory J, et al. Am J Med 2000) 20
Urinary Catheters Often Placed in the Emergency Department: A National U. S. Study • Catheters often inserted without clear indications and may remain in place for convenience rather than medical necessity • An Infection Control Nurse: “our other barrier is the Emergency Department and this is where most Foleys are placed. . Doctors forget to look under the sheets to say, ‘Oh yeah, there’s a Foley there’ and … the nurses aren’t going to take the initiative. . . ” Epid 2008) (Saint et al. Infect Cont Hosp 21
Prevention of Catheter- Associated UTI • Make sure the catheter is indicated ü Adhere to general infection control principles (e. g. , aseptic insertion, proper maintenance, hand hygiene, education, feedback) • Remove the catheter as soon as possible • Consider other methods of prevention 22
Use Proper Aseptic Technique for Catheter Insertion • NEJM Videos in Clinical Medicine: – Male Urethral Catheterization T. W. Thomsen and G. S. Setnik - 25 May, 2006 – Female Urethral Catheterization R. Ortega, L. Ng, P. Sekhar, and M. Song - 3 Apr, 2008 • Goal is to avoid contamination of the sterile catheter during the insertion process • Should not assume that the healthcare workers inserting urinary catheters know how to do so 23
Prevention of Catheter. Associated UTI • Make sure the catheter is indicated • Adhere to general infection control principles (eg, aseptic insertion, proper maintenance, hand hygiene, education, feedback) ü Remove the catheter as soon as possible • Consider other methods of prevention 24
Early Removal of Indwelling Catheters: Summary of the Evidence • 14 studies have evaluated urinary catheter reminders and stop-orders (written, computerized, nurse-initiated) – Significant reduction in catheter use – Significant reduction in infection – No evidence of harm (ie, re-insertion) (Meddings J et al. Clin Infect Dis 2010) 25
Prevention of Catheter. Associated UTI • Make sure the catheter is indicated • Adhere to general infection control principles (eg, aseptic insertion, proper maintenance, hand hygiene, education, feedback) • Remove the catheter as soon as possible ü Consider other methods of prevention 26
Other Methods for Preventing CAUTI • Alternatives to the indwelling catheter – Bladder ultrasound – Intermittent catheterization – Condom catheter 27
On the CUSP: Stop CAUTI Recent Guidelines on CAUTI Prevention 28

29
On the CUSP: Stop CAUTI http: //www. cdc. gov/hicpac/pdf/CAUTIguideline 2009 final. pdf 30
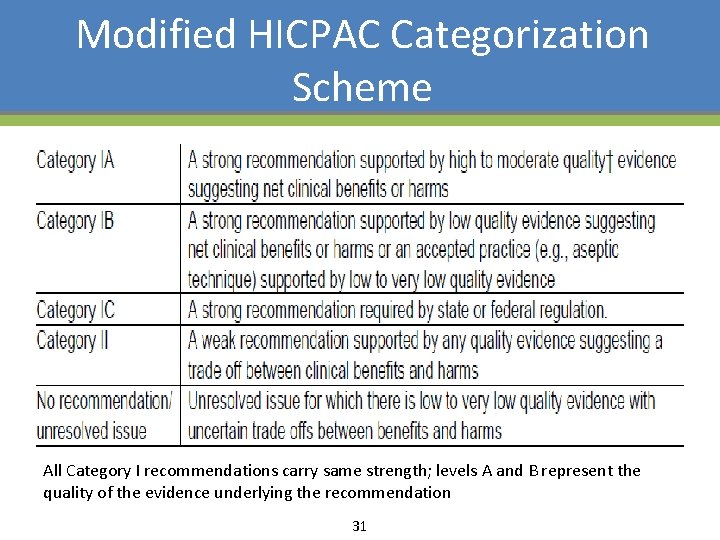
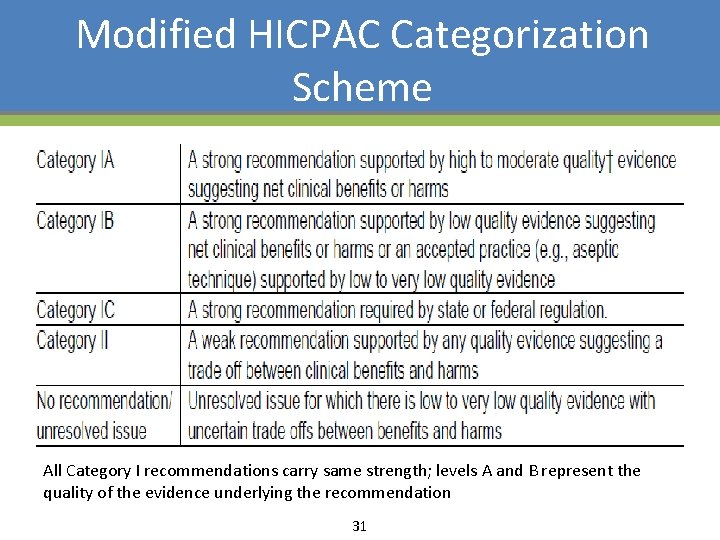
Modified HICPAC Categorization Scheme All Category I recommendations carry same strength; levels A and B represent the quality of the evidence underlying the recommendation 31
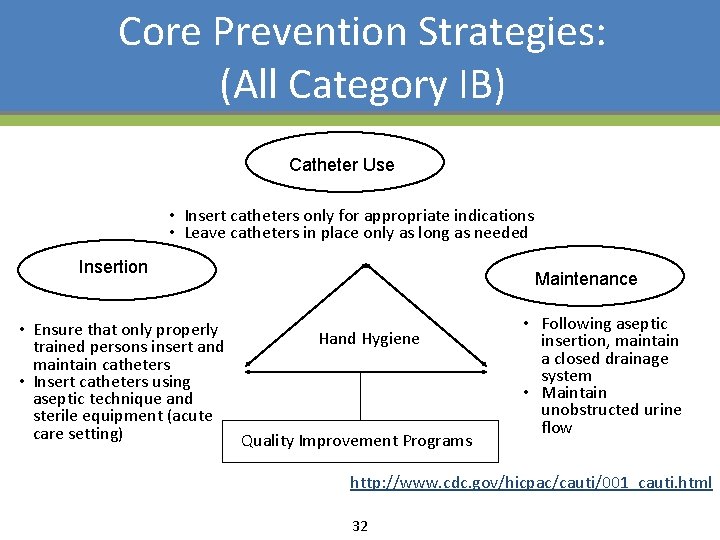
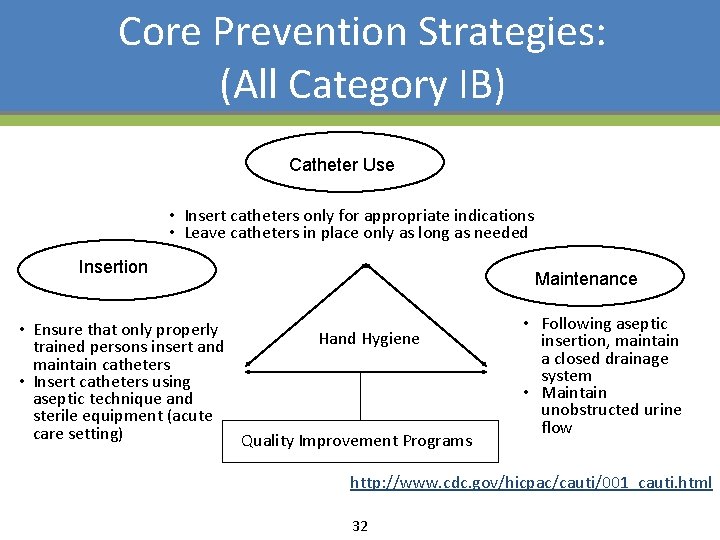
Core Prevention Strategies: (All Category IB) Catheter Use • Insert catheters only for appropriate indications • Leave catheters in place only as long as needed Insertion Maintenance • Ensure that only properly Hand Hygiene trained persons insert and maintain catheters • Insert catheters using aseptic technique and sterile equipment (acute care setting) Quality Improvement Programs • Following aseptic insertion, maintain a closed drainage system • Maintain unobstructed urine flow http: //www. cdc. gov/hicpac/cauti/001_cauti. html 32
On the CUSP: Stop CAUTI Comprehensive Unit-based Safety Program (CUSP) 33
The Michigan Keystone ICU Project saved over 1, 500 lives and $200 million by reducing health care associated infections. Office of Health Reform, Department of Health and Human Services 34
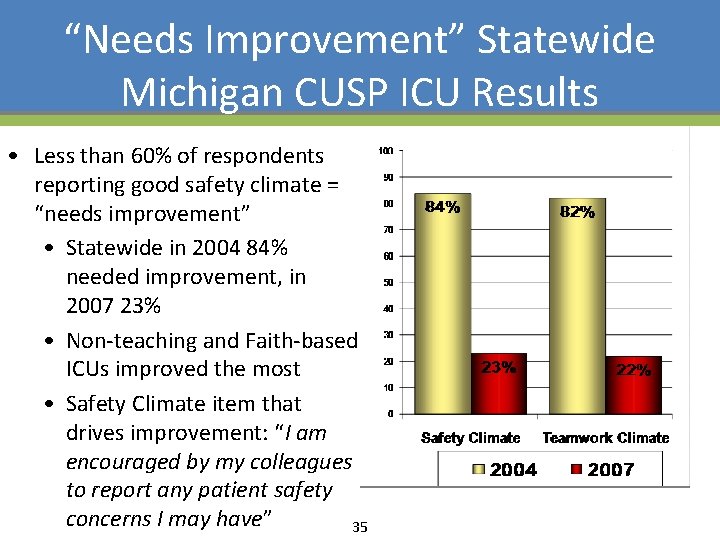
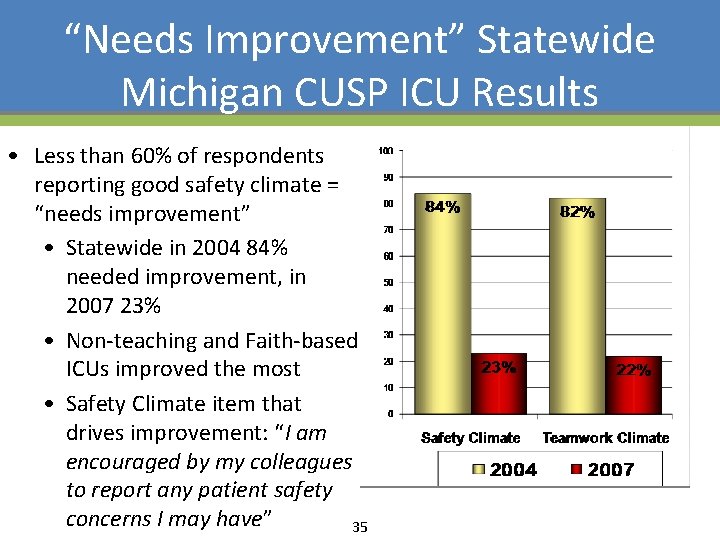
“Needs Improvement” Statewide Michigan CUSP ICU Results • Less than 60% of respondents reporting good safety climate = “needs improvement” • Statewide in 2004 84% needed improvement, in 2007 23% • Non-teaching and Faith-based ICUs improved the most • Safety Climate item that drives improvement: “I am encouraged by my colleagues to report any patient safety concerns I may have” 35
Pre CUSP Work • Create an ICU team – Nurse, physician, administrator, infection control, others – Assign a team leader • Measure Culture in your clinical unit (discuss with hospital association leader) • Work with hospital quality leader to have a senior executive assigned to your unit based team 36
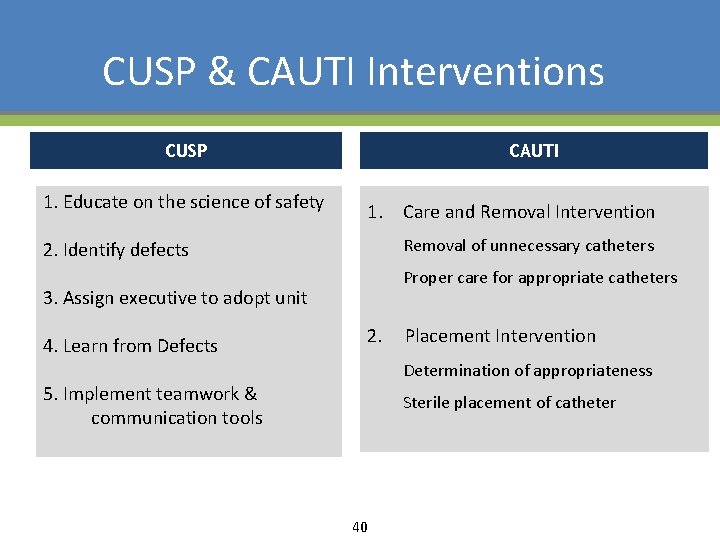
Comprehensive Unit-based Safety Program (CUSP) An Intervention to Learn from Mistakes and Improve Safety Culture 1. Educate staff on science of safety http: //www. safercare. net 2. Identify defects 3. Assign executive to adopt unit 4. Learn from one defect per quarter 5. Implement teamwork tools Timmel J, et al. Jt Comm J Qual Patient Saf 2010; 36: 252 -260. 37
Teamwork Tools • Call list • Daily Goals • AM briefing • Shadowing • Culture check up • TEAMSTepps 38
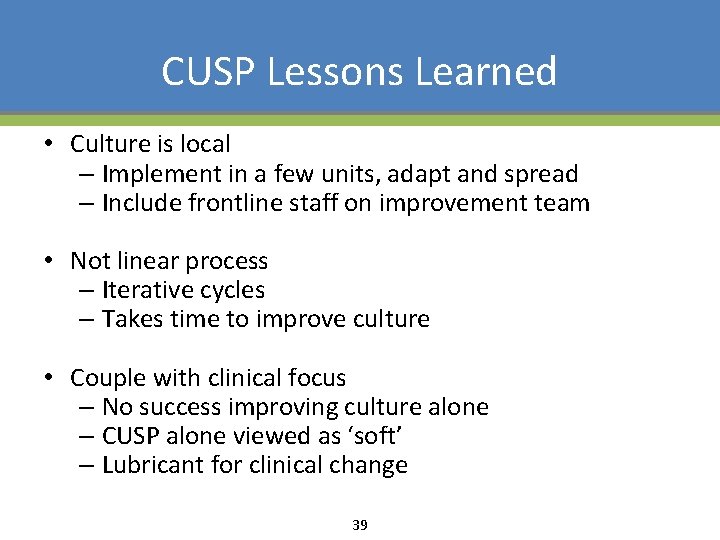
CUSP Lessons Learned • Culture is local – Implement in a few units, adapt and spread – Include frontline staff on improvement team • Not linear process – Iterative cycles – Takes time to improve culture • Couple with clinical focus – No success improving culture alone – CUSP alone viewed as ‘soft’ – Lubricant for clinical change 39
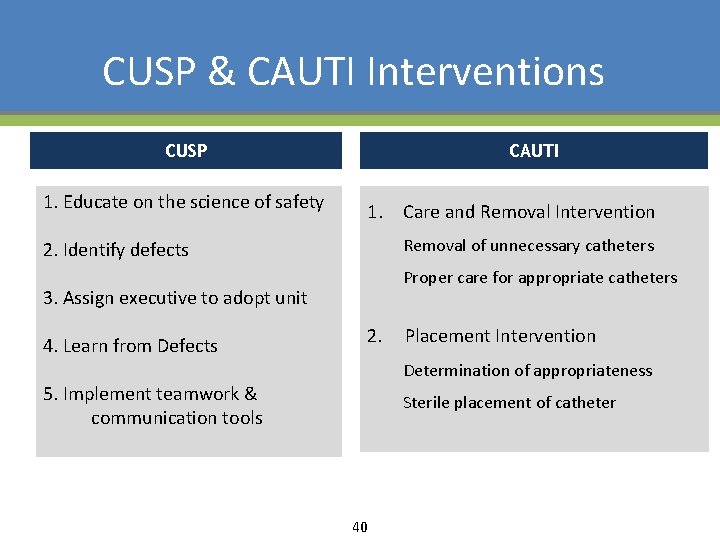
CUSP & CAUTI Interventions CUSP 1. Educate on the science of safety CAUTI 1. Care and Removal Intervention Removal of unnecessary catheters 2. Identify defects Proper care for appropriate catheters 3. Assign executive to adopt unit 4. Learn from Defects 2. Placement Intervention Determination of appropriateness 5. Implement teamwork & communication tools Sterile placement of catheter 40
Expected Benefits • Increased awareness of appropriate indications for indwelling urinary catheter use • Reduced use of indwelling urinary catheters • Improved caregiver accountability to assess need and trigger UC discontinuation when UC no longer necessary • Reduced risk of urethral trauma with reduction in utilization • Reduced patient discomfort 41
Expected Benefits • Reduction in bacteriuria • Reduction in symptomatic UTIs • Shortened Length of Stay • Decreased Cost per stay • Improved sensitivity to “patient dignity” 42
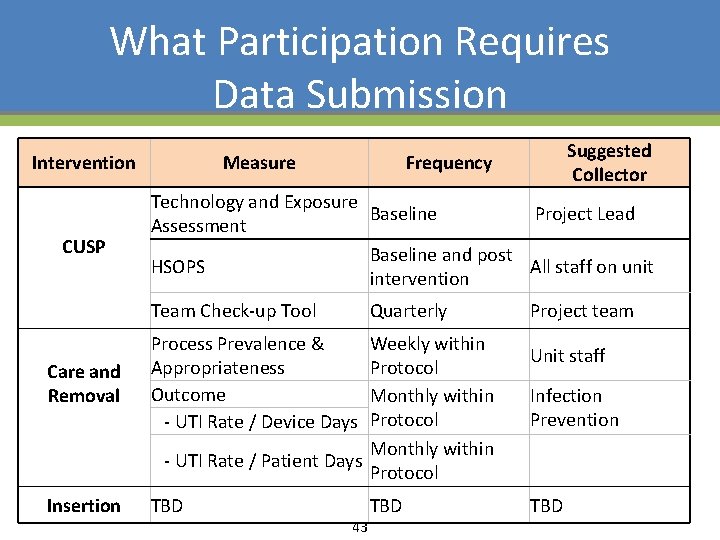
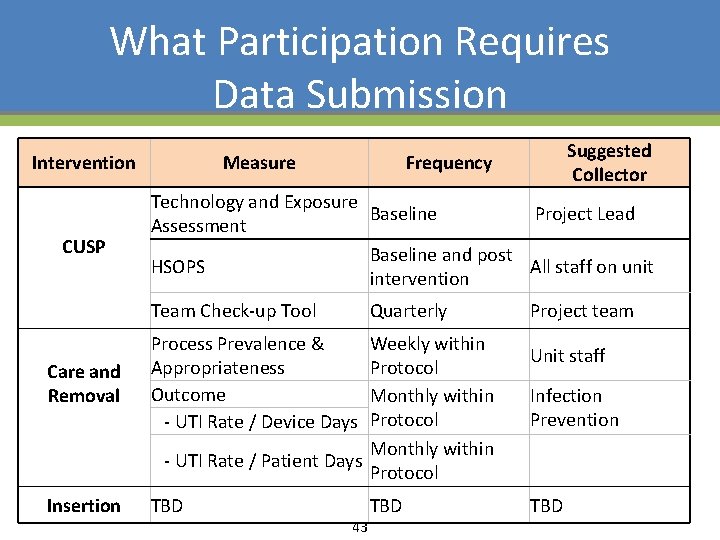
What Participation Requires Data Submission Intervention CUSP Measure Technology and Exposure Baseline Project Lead Assessment Baseline and post HSOPS All staff on unit intervention Team Check-up Tool Suggested Collector Frequency Quarterly Care and Removal Process Prevalence & Appropriateness Outcome - UTI Rate / Device Days Weekly within Protocol Monthly within - UTI Rate / Patient Days Protocol Insertion TBD 43 TBD Project team Unit staff Infection Prevention TBD
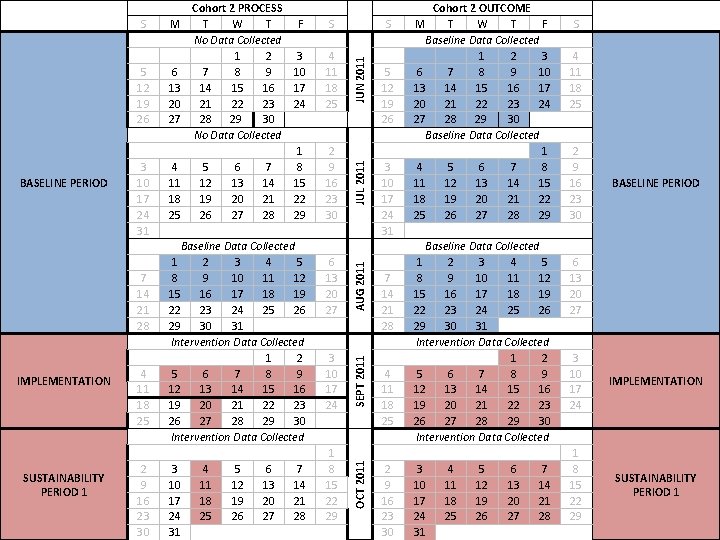
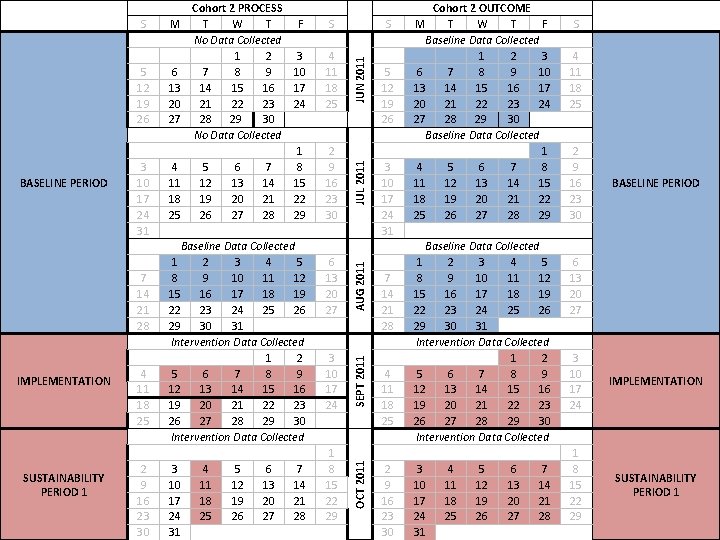
7 14 21 28 IMPLEMENTATION SUSTAINABILITY PERIOD 1 4 11 18 25 2 9 16 23 30 6 13 20 27 3 10 17 24 1 8 15 22 29 JUN 2011 JUL 2011 BASELINE PERIOD 3 10 17 24 31 4 11 18 25 AUG 2011 5 12 19 26 S SEPT 2011 S Cohort 2 PROCESS M T W T F No Data Collected 1 2 3 6 7 8 9 10 13 14 15 16 17 20 21 22 23 24 27 28 29 30 No Data Collected 1 4 5 6 7 8 11 12 13 14 15 18 19 20 21 22 25 26 27 28 29 Baseline Data Collected 1 2 3 4 5 8 9 10 11 12 15 16 17 18 19 22 23 24 25 26 29 30 31 Intervention Data Collected 1 2 5 6 7 8 9 12 13 14 15 16 19 20 21 22 23 26 27 28 29 30 Intervention Data Collected 3 4 5 6 7 10 11 12 13 14 17 18 19 20 21 24 25 26 27 28 31 OCT 2011 S 5 12 19 26 3 10 17 24 31 7 14 21 28 4 11 18 25 2 9 16 23 30 Cohort 2 OUTCOME M T W T F Baseline Data Collected 1 2 3 6 7 8 9 10 13 14 15 16 17 20 21 22 23 24 27 28 29 30 Baseline Data Collected 1 4 5 6 7 8 11 12 13 14 15 18 19 20 21 22 25 26 27 28 29 Baseline Data Collected 1 2 3 4 5 8 9 10 11 12 15 16 17 18 19 22 23 24 25 26 29 30 31 Intervention Data Collected 1 2 5 6 7 8 9 12 13 14 15 16 19 20 21 22 23 26 27 28 29 30 Intervention Data Collected 3 4 5 6 7 10 11 12 13 14 17 18 19 20 21 24 25 26 27 28 31 S 4 11 18 25 2 9 16 23 30 BASELINE PERIOD 6 13 20 27 3 10 17 24 1 8 15 22 29 IMPLEMENTATION SUSTAINABILITY PERIOD 1
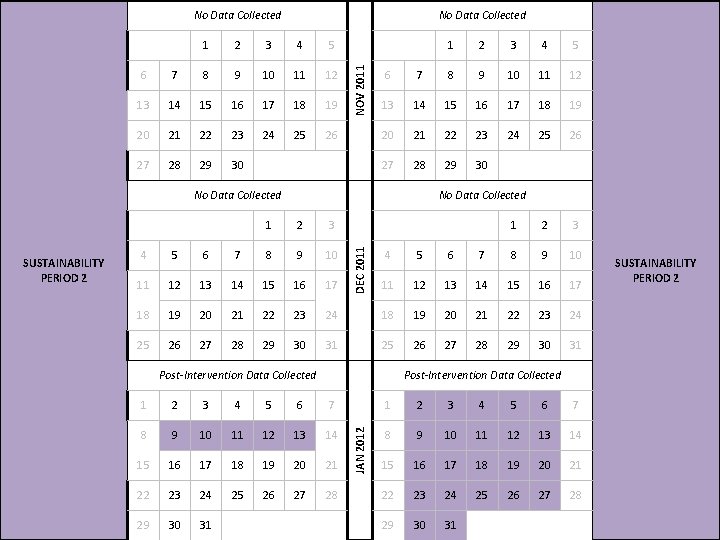
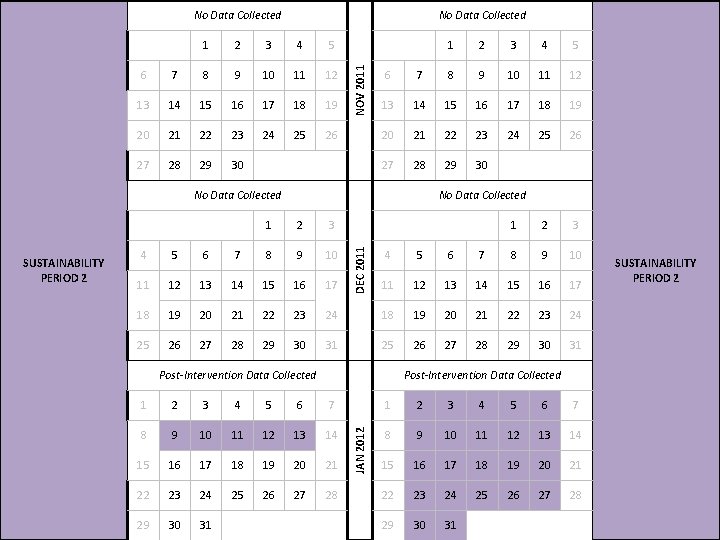
No Data Collected 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 NOV 2011 No Data Collected 3 4 5 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 No Data Collected 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 25 26 27 28 29 30 DEC 2011 1 2 3 5 6 7 8 9 10 11 12 13 14 15 16 17 24 18 19 20 21 22 23 24 31 25 26 27 28 29 30 31 Post-Intervention Data Collected SUSTAINABILITY PERIOD 2 Post-Intervention Data Collected 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 1 4 JAN 2012 SUSTAINABILITY PERIOD 2 2 6 No Data Collected 1 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 45
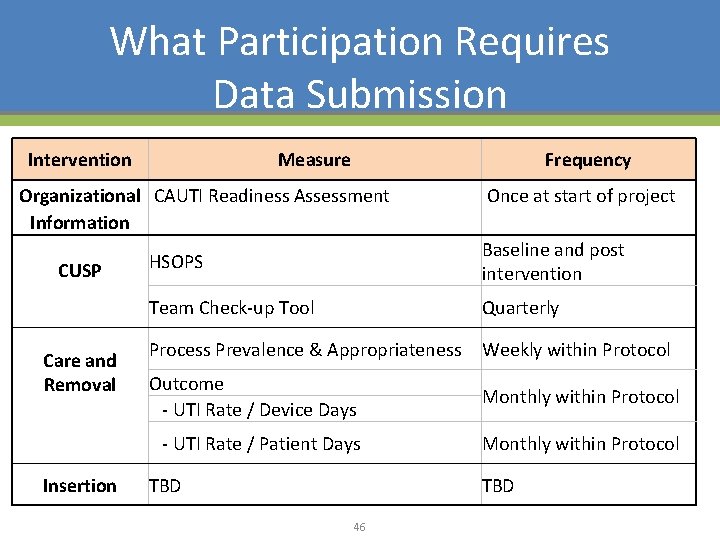
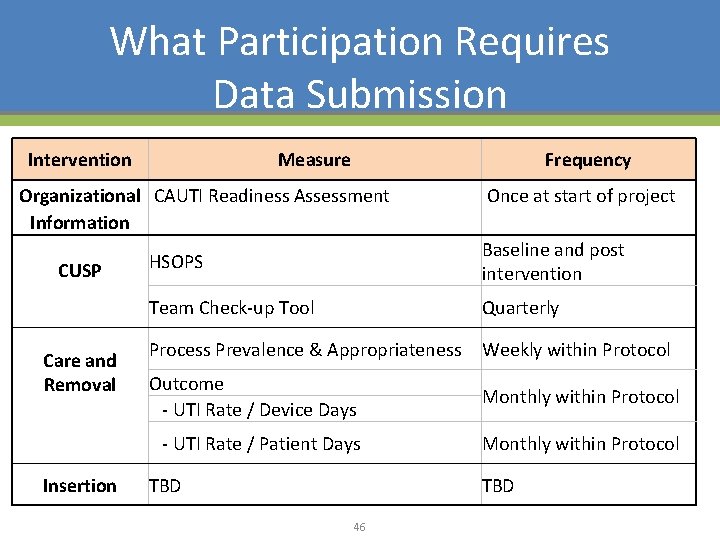
What Participation Requires Data Submission Intervention Measure Frequency Organizational CAUTI Readiness Assessment Information CUSP Care and Removal Insertion Once at start of project HSOPS Baseline and post intervention Team Check-up Tool Quarterly Process Prevalence & Appropriateness Weekly within Protocol Outcome - UTI Rate / Device Days Monthly within Protocol - UTI Rate / Patient Days Monthly within Protocol TBD 46
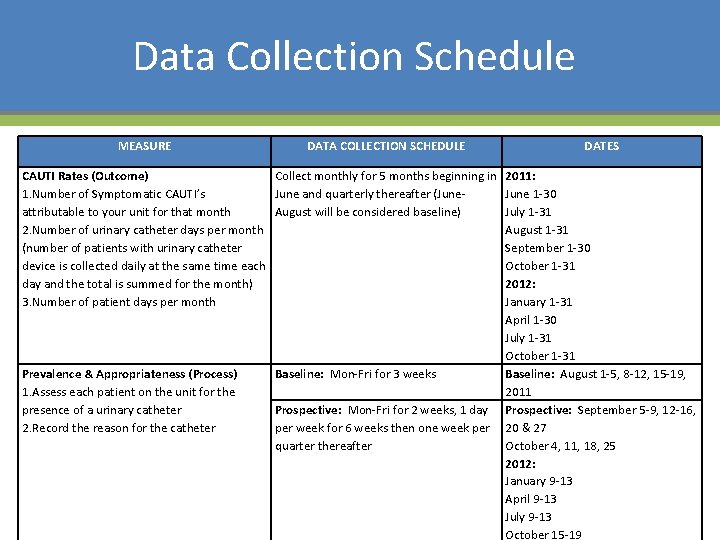
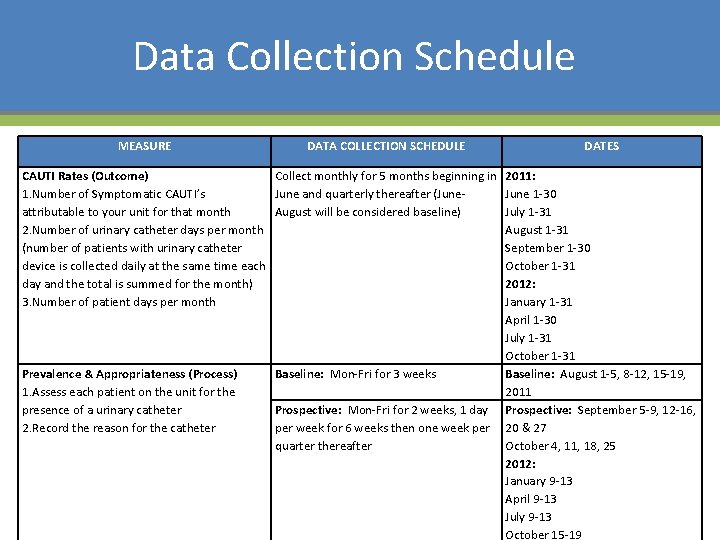
Data Collection Schedule MEASURE DATA COLLECTION SCHEDULE DATES CAUTI Rates (Outcome) Collect monthly for 5 months beginning in 2011: 1. Number of Symptomatic CAUTI’s June and quarterly thereafter (June 1 -30 attributable to your unit for that month August will be considered baseline) July 1 -31 2. Number of urinary catheter days per month August 1 -31 (number of patients with urinary catheter September 1 -30 device is collected daily at the same time each October 1 -31 day and the total is summed for the month) 2012: 3. Number of patient days per month January 1 -31 April 1 -30 July 1 -31 October 1 -31 Prevalence & Appropriateness (Process) Baseline: Mon-Fri for 3 weeks Baseline: August 1 -5, 8 -12, 15 -19, 1. Assess each patient on the unit for the 2011 presence of a urinary catheter Prospective: Mon-Fri for 2 weeks, 1 day Prospective: September 5 -9, 12 -16, 2. Record the reason for the catheter per week for 6 weeks then one week per 20 & 27 quarter thereafter October 4, 11, 18, 25 2012: January 9 -13 April 9 -13 July 9 -13 October 15 -19
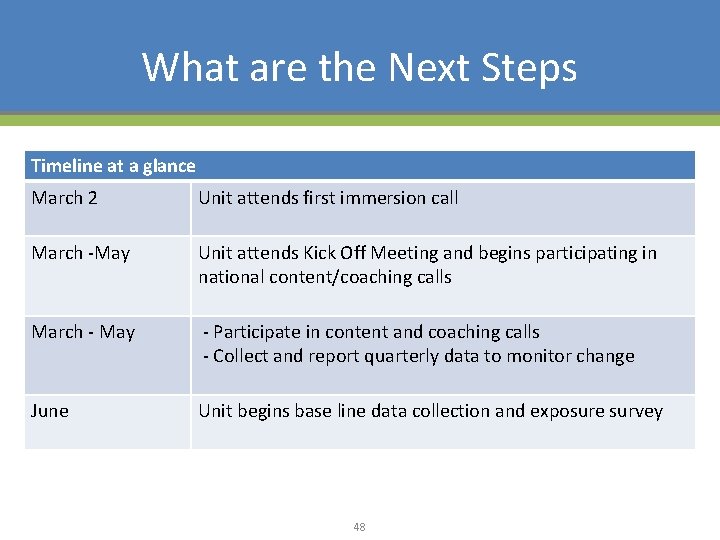
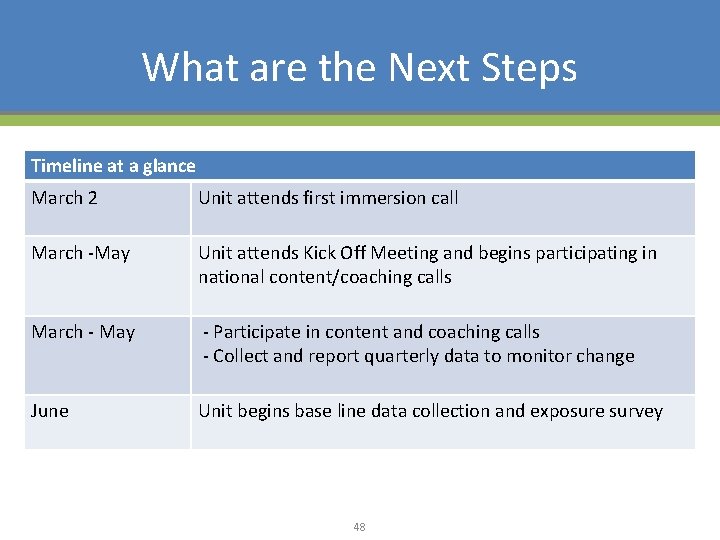
What are the Next Steps Timeline at a glance March 2 Unit attends first immersion call March -May Unit attends Kick Off Meeting and begins participating in national content/coaching calls March - May - Participate in content and coaching calls - Collect and report quarterly data to monitor change June Unit begins base line data collection and exposure survey 48
Questions • Content – Sam Watson, MHA Keystone – swatson@mha. org • Participation–Kristina Davis, HRET – kdavis@aha. org 49