Case n HPI 37 yo presents with 6





- Slides: 39
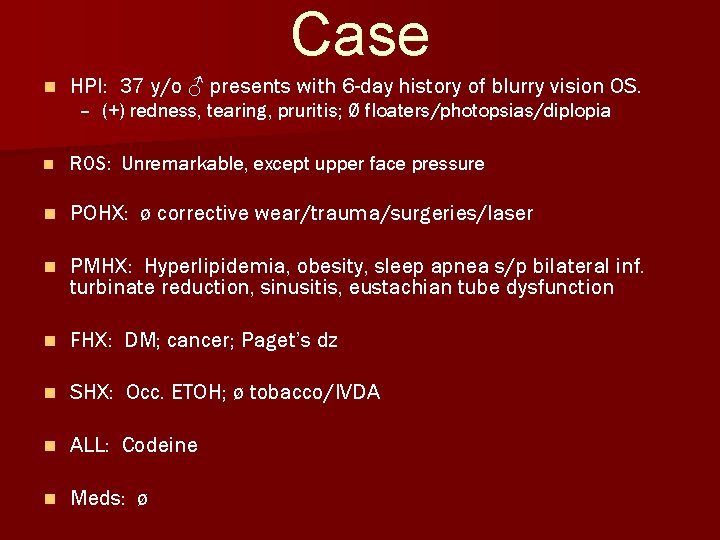
Case n HPI: 37 y/o ♂ presents with 6 -day history of blurry vision OS. – (+) redness, tearing, pruritis; Ø floaters/photopsias/diplopia n ROS: Unremarkable, except upper face pressure n POHX: ø corrective wear/trauma/surgeries/laser n PMHX: Hyperlipidemia, obesity, sleep apnea s/p bilateral inf. turbinate reduction, sinusitis, eustachian tube dysfunction n FHX: DM; cancer; Paget’s dz n SHX: Occ. ETOH; ø tobacco/IVDA n ALL: Codeine n Meds: ø
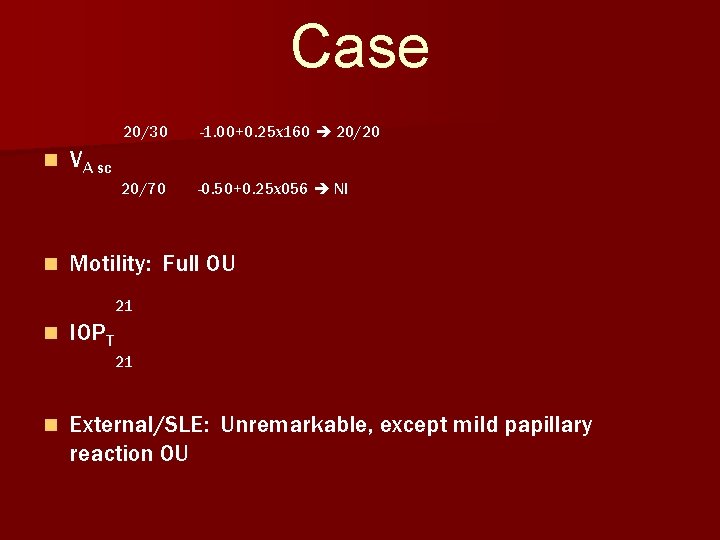
Case n n 20/30 -1. 00+0. 25 x 160 20/20 20/70 -0. 50+0. 25 x 056 NI VA sc Motility: Full OU 21 n IOPT 21 n External/SLE: Unremarkable, except mild papillary reaction OU



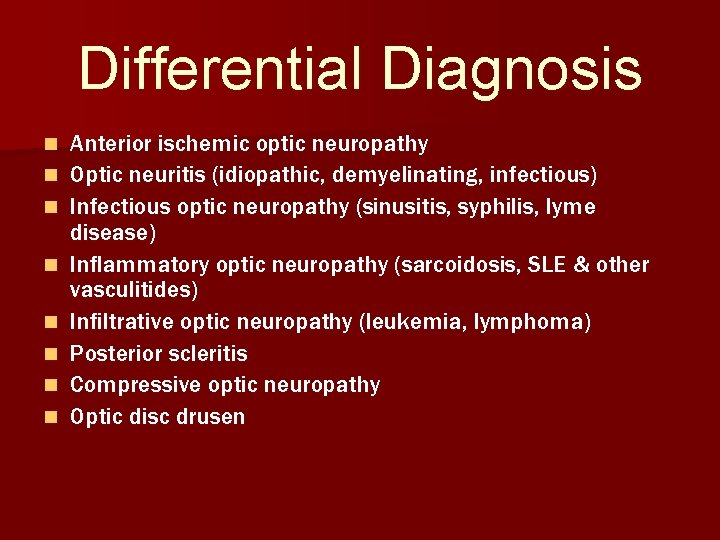
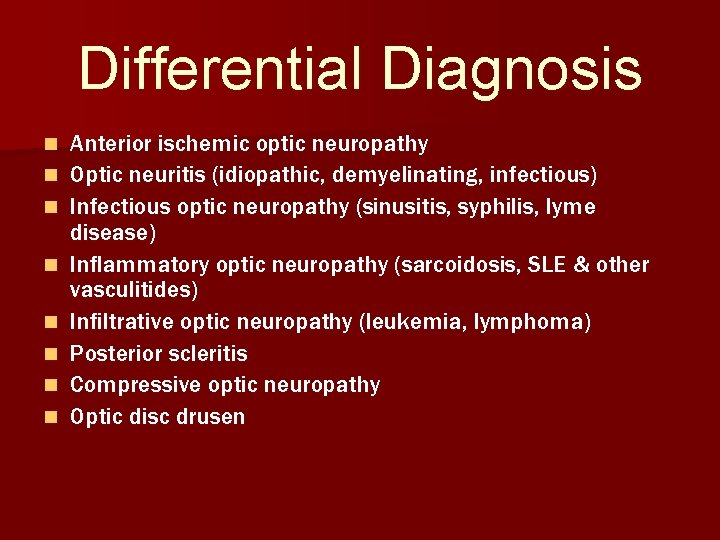
Differential Diagnosis n n n n Anterior ischemic optic neuropathy Optic neuritis (idiopathic, demyelinating, infectious) Infectious optic neuropathy (sinusitis, syphilis, lyme disease) Inflammatory optic neuropathy (sarcoidosis, SLE & other vasculitides) Infiltrative optic neuropathy (leukemia, lymphoma) Posterior scleritis Compressive optic neuropathy Optic disc drusen
More Information… n History & ocular exam n Humphrey visual field n Imaging
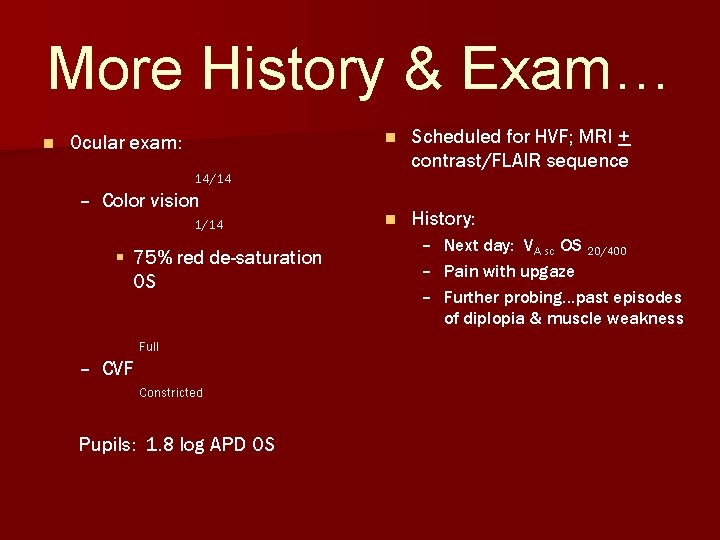
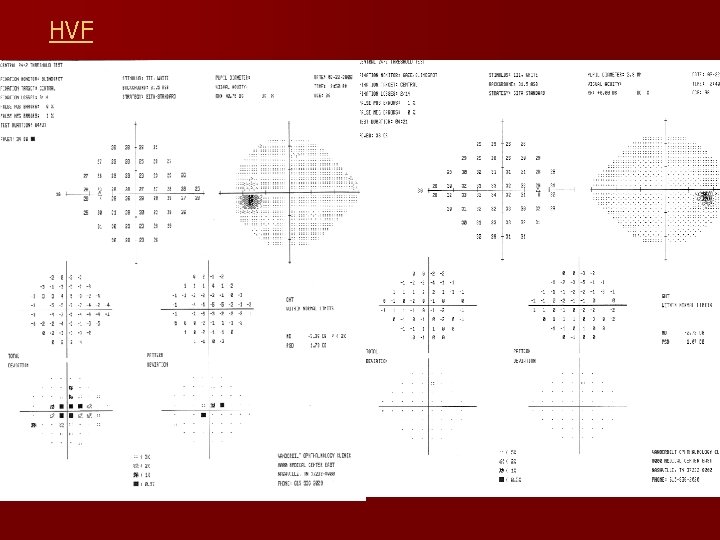
More History & Exam… n Ocular exam: n Scheduled for HVF; MRI + contrast/FLAIR sequence n History: 14/14 – Color vision 1/14 § 75% red de-saturation OS Full – CVF Constricted Pupils: 1. 8 log APD OS – Next day: VA sc OS 20/400 – Pain with upgaze – Further probing…past episodes of diplopia & muscle weakness
More Information… n History & ocular exam n Humphrey visual field n Imaging
More Information… n History & ocular exam n Humphrey visual field n Imaging

Imaging n MRI – Head discontinued/limited study § 1. 2 cm hyperintense FLAIR signal in the corpus callosum § Non-specific finding: inflammatory, infectious, demyelinating plaque, or neoplastic lesion
More Information… n History & ocular exam n Humphrey visual field n Imaging
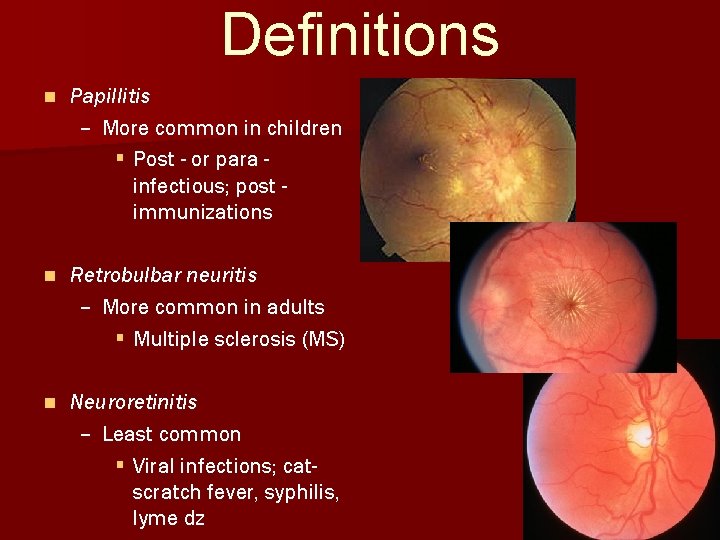
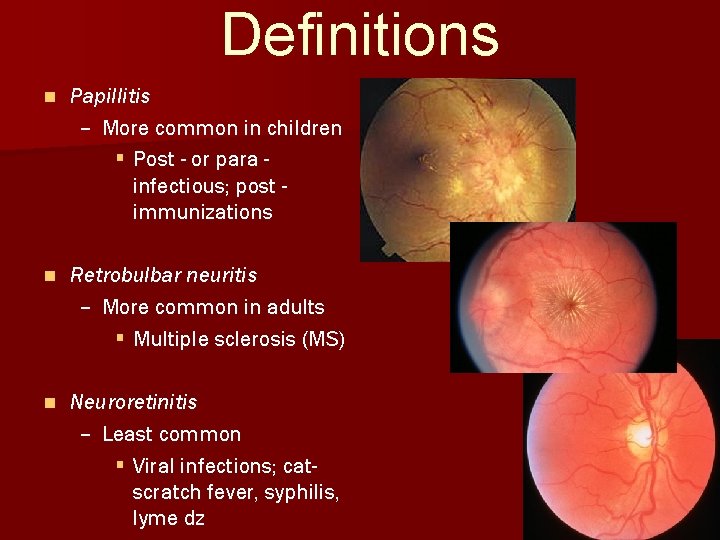
Definitions n Papillitis – More common in children § Post - or para infectious; post immunizations n Retrobulbar neuritis – More common in adults § Multiple sclerosis (MS) n Neuroretinitis – Least common § Viral infections; catscratch fever, syphilis, lyme dz

Epidemiology n Annual incidence: 5/100, 000 – Prevalence: 115/100, 000 n Age: 20 -50 yrs – ♀ mean age: 30. 2 (9 -55 yrs) – ♂ mean age: 31. 1 (16 -60 yrs) n More common in ♀ – ♀: ♂ 1. 8: 1 n Caucasians of northern European descent – Rare in Asians & Africans
n Demyelinating Diseases Isolated optic neuritis n Multiple sclerosis (MS) n Devic dz (neuromyelitis optica) n Schilder dz Isolated optic neuritis
Multiple Sclerosis n 70% of MS pts evidence of optic neuritis (ON) – 1 st manifestation in 20% n 1 st episode of ON & nrl brain MRI 16% develop MS within 5 yrs n 1 st episode of ON & ø signs of MS 50% with demyelinating lesions on brain MRI – risk of developing clinical definite MS (CDMS) within 5 -10 yrs n CDMS: 2 attacks > 24 hrs, separated > 1 month, separate parts of the CNS + abnormal neurologic exam
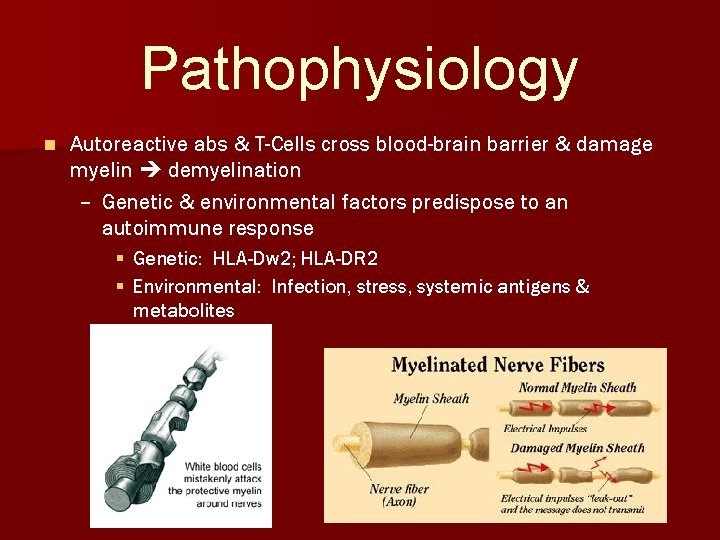
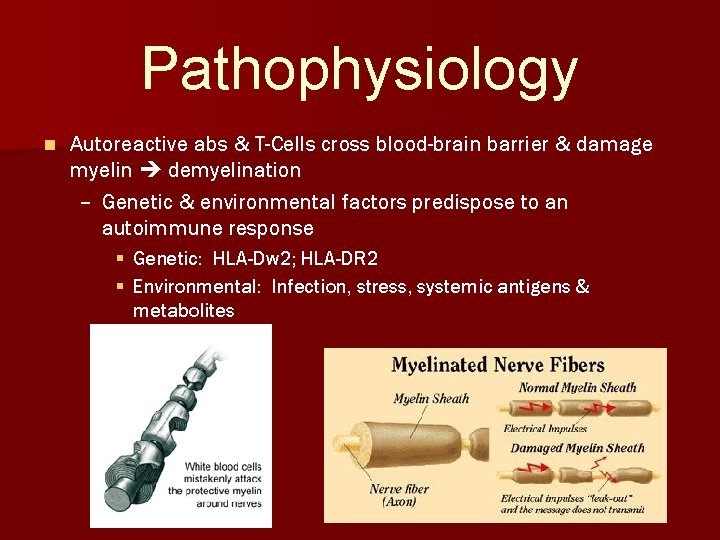
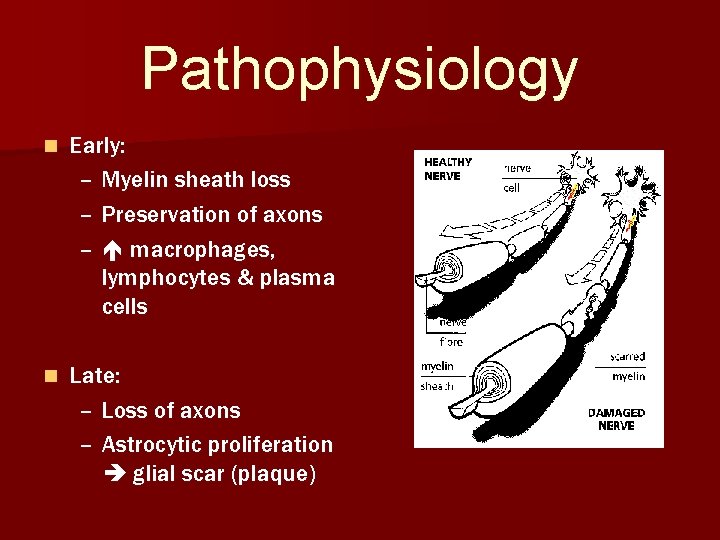
Pathophysiology n Autoreactive abs & T-Cells cross blood-brain barrier & damage myelin demyelination – Genetic & environmental factors predispose to an autoimmune response § Genetic: HLA-Dw 2; HLA-DR 2 § Environmental: Infection, stress, systemic antigens & metabolites
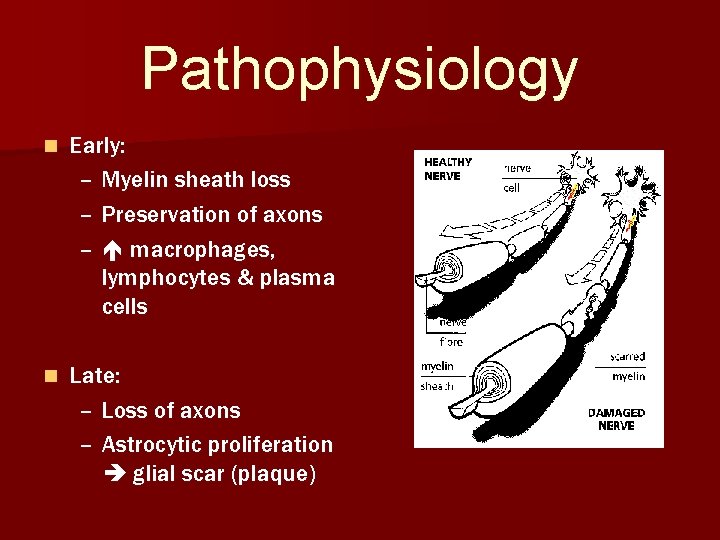
Pathophysiology n Early: – Myelin sheath loss – Preservation of axons – macrophages, lymphocytes & plasma cells n Late: – Loss of axons – Astrocytic proliferation glial scar (plaque)
Anatomy of Optic Neuritis n Optic nerve head: 45% n Retrobulbar: 61% n Intracanalicular: 34% n Intracranially (prechiasmatic): 5% n Chiasmatic: 2%
Clinical Symptoms n 70% unilateral n Retrobulbar pain (53 -88%) – Dull ache/sinus pain +/- globe tenderness – Esp. with EOM – Precedes visual symptoms n Subacute visual loss – Haze, cloud or dimness – Progresses over 2 -7 days § < 20/60: 52% § 20/70 -20/100: 48% § < 20/200: 38%
Clinical Symptoms n Obscuration of vision in bright light n Dyschromatopsia – ALWAYS present – vividness of saturated colors n Photopsias/phosphenes – Induced with horizontal EOM/loud noise
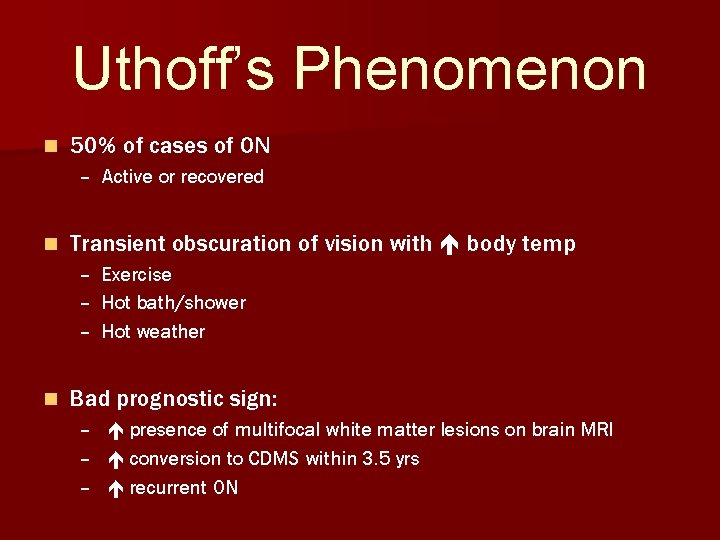
Uthoff’s Phenomenon n 50% of cases of ON – Active or recovered n Transient obscuration of vision with body temp – Exercise – Hot bath/shower – Hot weather n Bad prognostic sign: – presence of multifocal white matter lesions on brain MRI – conversion to CDMS within 3. 5 yrs – recurrent ON
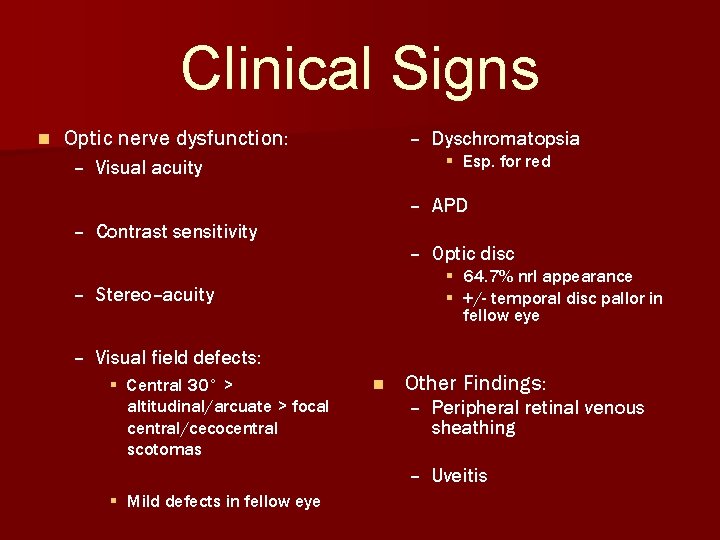
Clinical Signs n Optic nerve dysfunction: – Dyschromatopsia § Esp. for red – Visual acuity – APD – Contrast sensitivity – Optic disc § 64. 7% nrl appearance § +/- temporal disc pallor in fellow eye – Stereo–acuity – Visual field defects: § Central 30° > altitudinal/arcuate > focal central/cecocentral scotomas n Other Findings: – Peripheral retinal venous sheathing – Uveitis § Mild defects in fellow eye
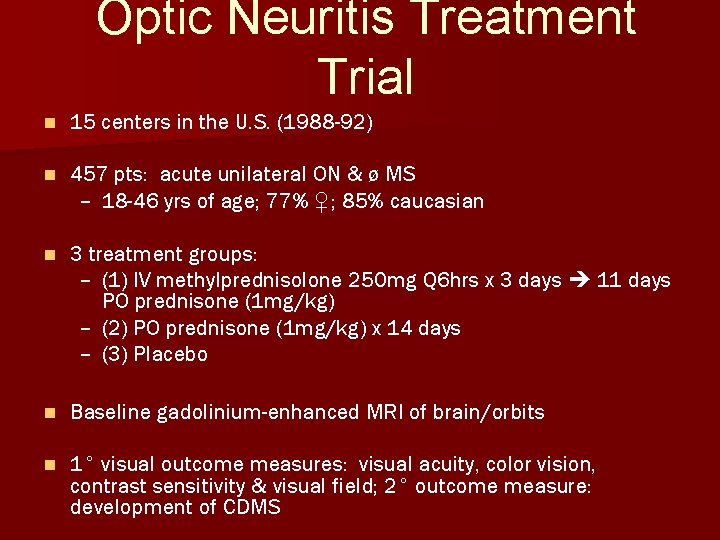
Optic Neuritis Treatment Trial n 15 centers in the U. S. (1988 -92) n 457 pts: acute unilateral ON & ø MS – 18 -46 yrs of age; 77% ♀; 85% caucasian n 3 treatment groups: – (1) IV methylprednisolone 250 mg Q 6 hrs x 3 days 11 days PO prednisone (1 mg/kg) – (2) PO prednisone (1 mg/kg) x 14 days – (3) Placebo n Baseline gadolinium-enhanced MRI of brain/orbits n 1° visual outcome measures: visual acuity, color vision, contrast sensitivity & visual field; 2° outcome measure: development of CDMS
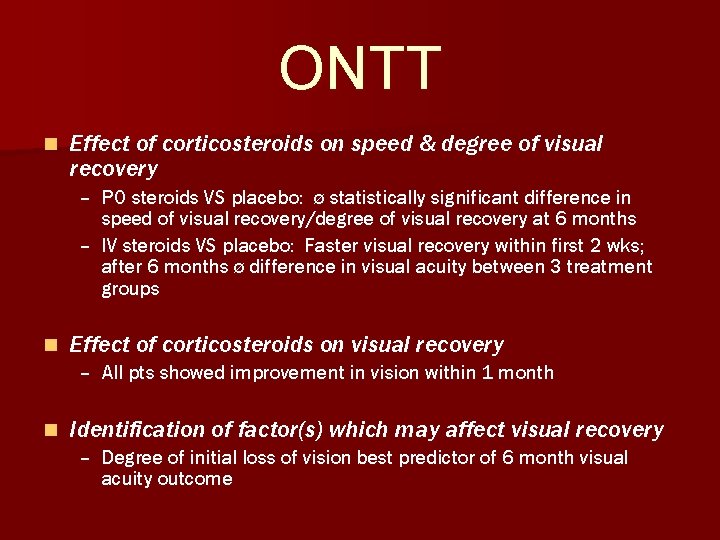
ONTT n Effect of corticosteroids on speed & degree of visual recovery – PO steroids VS placebo: ø statistically significant difference in speed of visual recovery/degree of visual recovery at 6 months – IV steroids VS placebo: Faster visual recovery within first 2 wks; after 6 months ø difference in visual acuity between 3 treatment groups n Effect of corticosteroids on visual recovery – All pts showed improvement in vision within 1 month n Identification of factor(s) which may affect visual recovery – Degree of initial loss of vision best predictor of 6 month visual acuity outcome
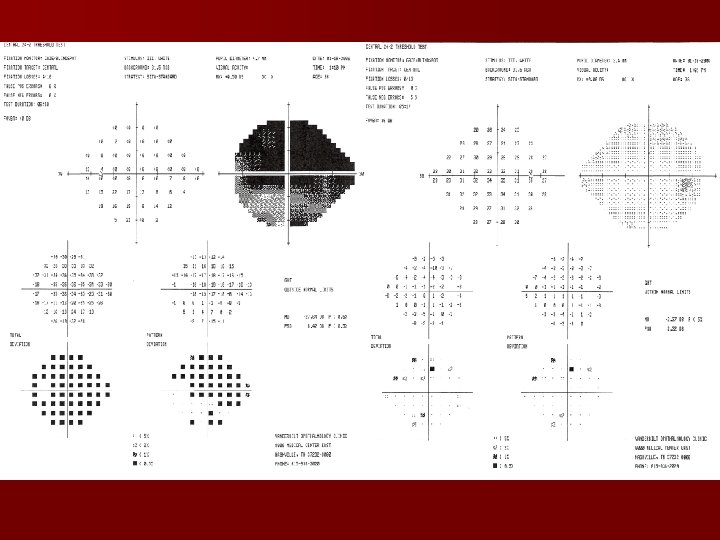
ONTT n Identification of side-effects of short-term use of corticosteroids – All pts reported sleep disturbances, mood changes, stomach upset, skin flushing & weight gain § IV steroid group: 1 case each of psychotic depression & acute pancreatitis n Visual Field Profile of pts with ON – Variable patterns § Chiasmal/retrochiasmal defects 76% with abnormal baseline MRI – 68. 8% of fellow eyes with mild, but abnormal VF
ONTT n Gadolinium - enhanced, T 2 -weighted brain/orbit MRI likelihood of developing CDMS – 5 -yr data, MS risk: § Ø lesions = 16% § 1 -2 lesions = 37% § > 3 lesions = 51% n Effects of corticosteroids on development of MS – IV steroids: risk of CDMS in pts with an abnormal MRI (> 2 white matter lesions) during first 2 yrs n Effect of corticosteroids on recurrent ON – PO steroids rate of recurrent ON § 30% of pts: > 1 new episode of ON in either eye by 2 nd yr; IV steroid group: 13%; placebo group: 16% § recurrence in pts subsequently diagnosed with MS
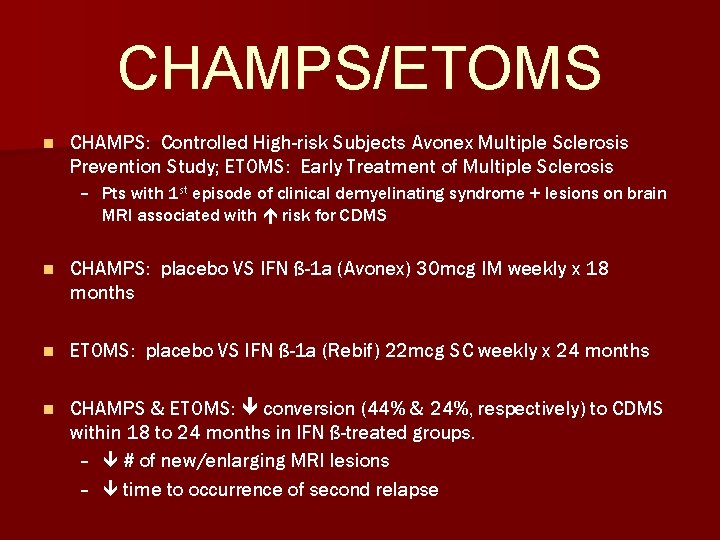
CHAMPS/ETOMS n CHAMPS: Controlled High-risk Subjects Avonex Multiple Sclerosis Prevention Study; ETOMS: Early Treatment of Multiple Sclerosis – Pts with 1 st episode of clinical demyelinating syndrome + lesions on brain MRI associated with risk for CDMS n CHAMPS: placebo VS IFN ß-1 a (Avonex) 30 mcg IM weekly x 18 months n ETOMS: placebo VS IFN ß-1 a (Rebif) 22 mcg SC weekly x 24 months n CHAMPS & ETOMS: conversion (44% & 24%, respectively) to CDMS within 18 to 24 months in IFN ß-treated groups. – # of new/enlarging MRI lesions – time to occurrence of second relapse
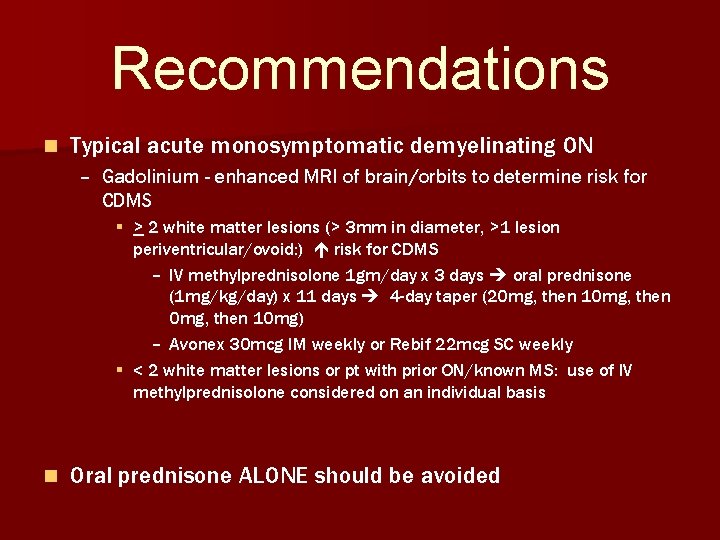
Recommendations n Typical acute monosymptomatic demyelinating ON – Gadolinium - enhanced MRI of brain/orbits to determine risk for CDMS § > 2 white matter lesions (> 3 mm in diameter, >1 lesion periventricular/ovoid: ) risk for CDMS – IV methylprednisolone 1 gm/day x 3 days oral prednisone (1 mg/kg/day) x 11 days 4 -day taper (20 mg, then 10 mg, then 10 mg) – Avonex 30 mcg IM weekly or Rebif 22 mcg SC weekly § < 2 white matter lesions or pt with prior ON/known MS: use of IV methylprednisolone considered on an individual basis n Oral prednisone ALONE should be avoided
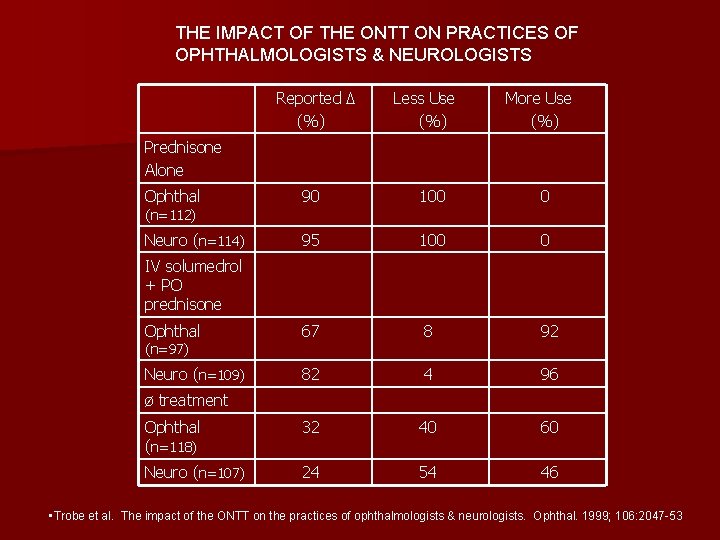
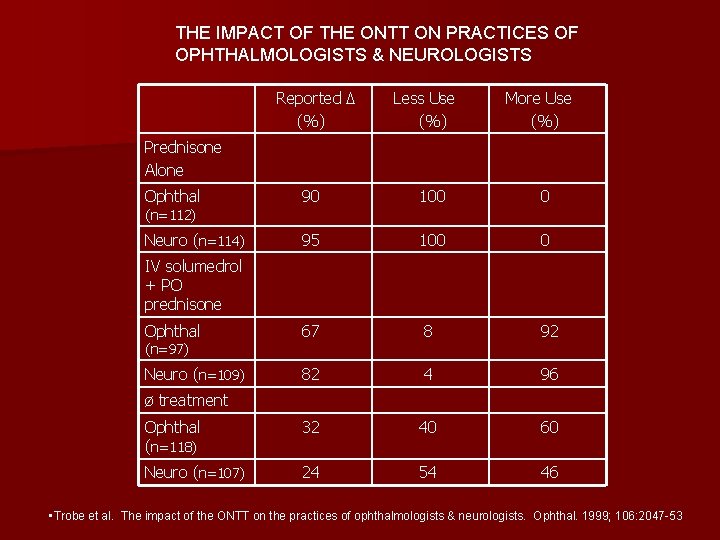
THE IMPACT OF THE ONTT ON PRACTICES OF OPHTHALMOLOGISTS & NEUROLOGISTS Reported Δ (%) Less Use (%) More Use (%) Prednisone Alone Ophthal 90 100 0 Neuro (n=114) 95 100 0 Ophthal 67 8 92 Neuro (n=109) 82 4 96 Ophthal (n=118) 32 40 60 Neuro (n=107) 24 54 46 (n=112) IV solumedrol + PO prednisone (n=97) ø treatment • Trobe et al. The impact of the ONTT on the practices of ophthalmologists & neurologists. Ophthal. 1999; 106: 2047 -53
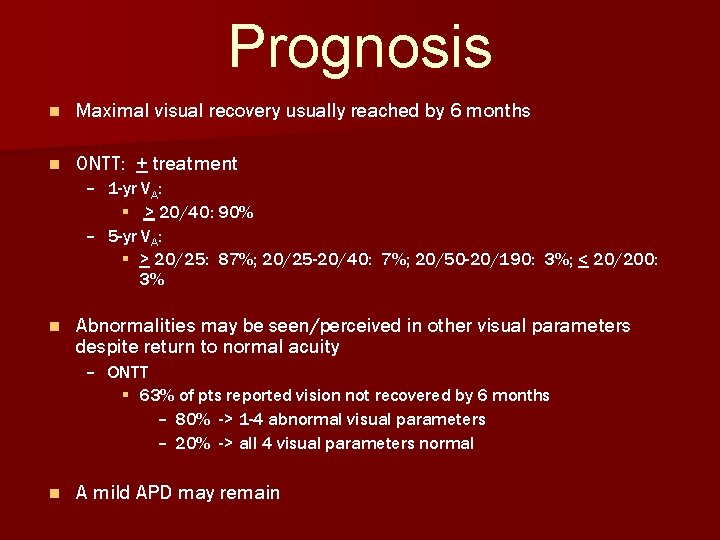
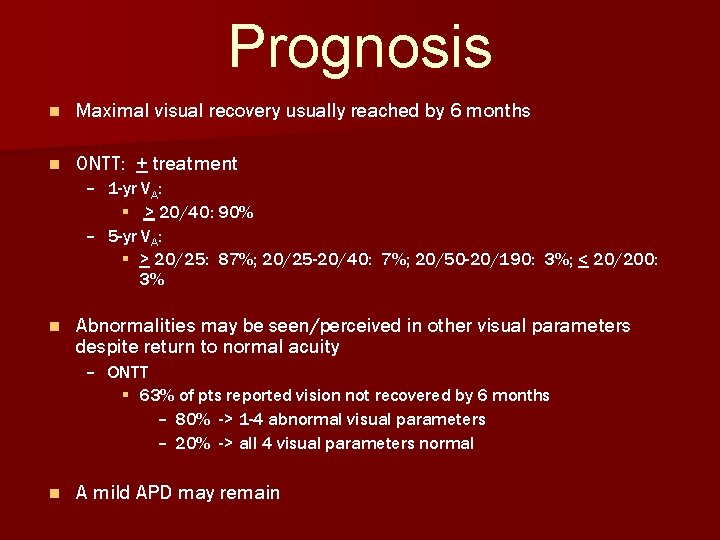
Prognosis n Maximal visual recovery usually reached by 6 months n ONTT: + treatment – 1 -yr VA: § > 20/40: 90% – 5 -yr VA: § > 20/25: 87%; 20/25 -20/40: 7%; 20/50 -20/190: 3%; < 20/200: 3% n Abnormalities may be seen/perceived in other visual parameters despite return to normal acuity – ONTT § 63% of pts reported vision not recovered by 6 months – 80% -> 1 -4 abnormal visual parameters – 20% -> all 4 visual parameters normal n A mild APD may remain
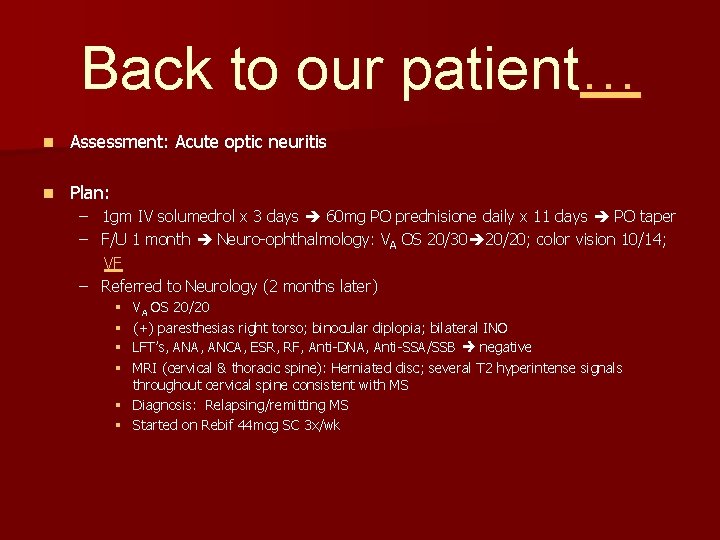
Back to our patient… n Assessment: Acute optic neuritis n Plan: – 1 gm IV solumedrol x 3 days 60 mg PO prednisione daily x 11 days PO taper – F/U 1 month Neuro-ophthalmology: VA OS 20/30 20/20; color vision 10/14; VF – Referred to Neurology (2 months later) VA OS 20/20 (+) paresthesias right torso; binocular diplopia; bilateral INO LFT’s, ANA, ANCA, ESR, RF, Anti-DNA, Anti-SSA/SSB negative MRI (cervical & thoracic spine): Herniated disc; several T 2 hyperintense signals throughout cervical spine consistent with MS § Diagnosis: Relapsing/remitting MS § Started on Rebif 44 mcg SC 3 x/wk § §
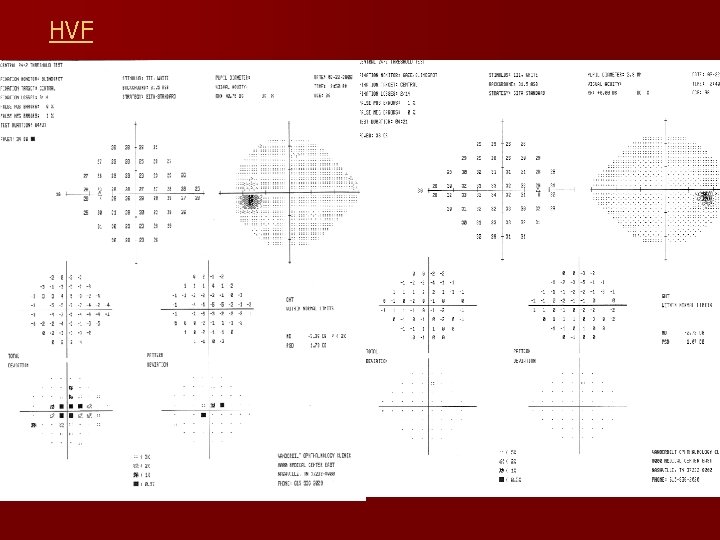
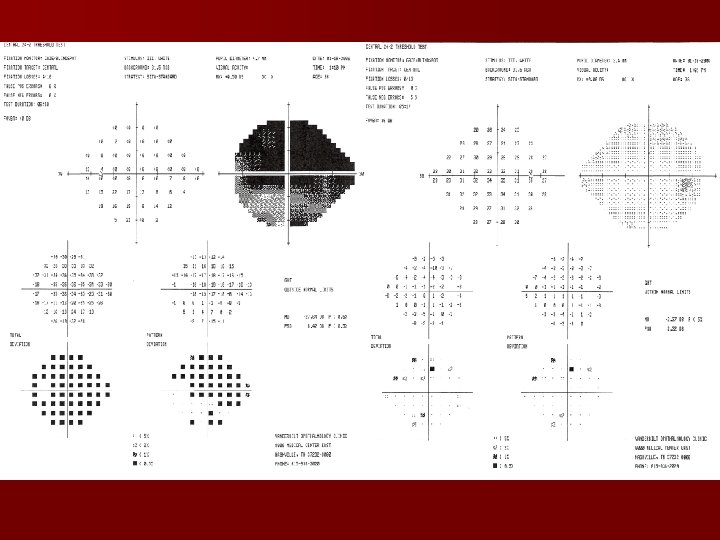
HVF
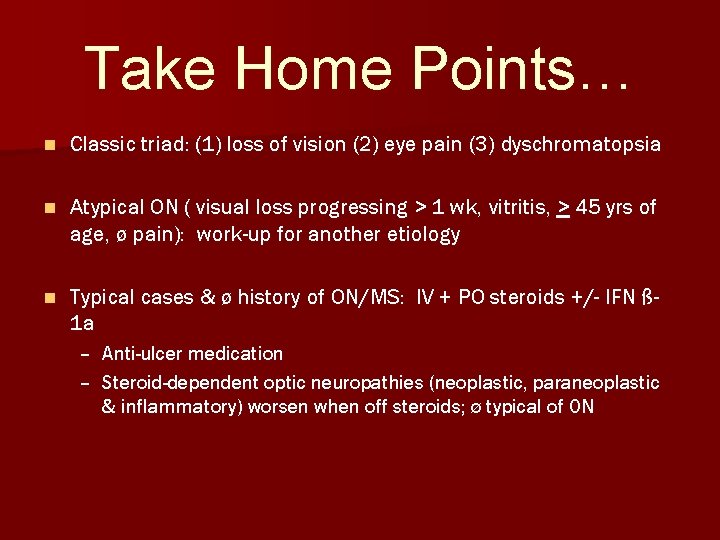
Take Home Points… n Classic triad: (1) loss of vision (2) eye pain (3) dyschromatopsia n Atypical ON ( visual loss progressing > 1 wk, vitritis, > 45 yrs of age, ø pain): work-up for another etiology n Typical cases & ø history of ON/MS: IV + PO steroids +/- IFN ß 1 a – Anti-ulcer medication – Steroid-dependent optic neuropathies (neoplastic, paraneoplastic & inflammatory) worsen when off steroids; ø typical of ON
Bibliography n n n n BCSC. Neuro-ophthalmology. AAO. 2004 -05 BCSC. Pathology. AAO. 2004 -05 Yanoff. Ophthalmology, 2 nd Ed. Mosby. 1263 -66 Kanski. Clinical Ophthalmology, 5 th Ed. Butterworth Heinemann. 601 -03. 2003 E-medicine: Optic Neuritis Beck RW, Cleary PA, Anderson MA, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. N Engl J Med. 1992; 326: 581– 8. Beck RW, Cleary PA, Backlund JC, et al. The course of visual recovery after optic neuritis: experience of the Optic Neuritis Treatment Trial. Ophthalmology. 1994; 101: 1771– 8. Arnold AC. Visual field defects in the Optic Neuritis Treatment Trial: central vs. peripheral, focal vs. global. Am J Ophthalmol. 1999; 128: 632– 4 Beck RW, Kupersmith MJ, Cleary PA, et al. Fellow eye abnormalities in acute unilateral optic neuritis: experience of the Optic Neuritis Treatment Trial. Ophthalmology. 1993; 100: 691– 8. Beck RW, Cleary PA, Trobe JD, et al. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. N Engl J Med. 1993; 329: 1764– 9. Cleary PA, Beck RW, Bourque LB, et al. Visual symptoms after optic neuritis: results from the Optic Neuritis Treatment Trial. J Neuroophthalmol. 1997; 17: 18– 28. Trobe JD, Sieving PC, Guire KE, et al. The impact of the Optic Neuritis Treatment Trial on the practices of ophthalmologists and neurologists. Ophthalmology. 1999; 106: 2047– 53. Jacobs LD, Beck RW, Simon JH, et al. Intramuscular interferon β-1 a therapy initiated during a first demyelinating event in multiple sclerosis. N Engl J Med. 2000; 343: 898– 904. n CHAMPS Study Group. Interferon β-1 a for optic neuritis patients at high risk for multiple sclerosis. Am J Ophthalmol. 2001; 132: 463– 71 n Comi G, Filippi M, Barkhof F, et al. Effect of early interferon treatment on conversion to definite multiple sclerosis: a randomized study. Lancet. 2001; 357: 1576– 82.