Case Presentation Marisa Glashow MS IV HPI 21
- Slides: 18
Case Presentation Marisa Glashow, MS IV
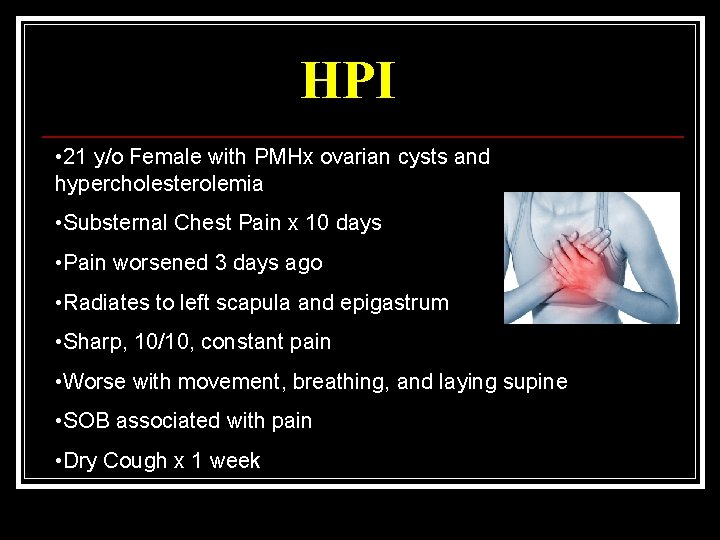
HPI • 21 y/o Female with PMHx ovarian cysts and hypercholesterolemia • Substernal Chest Pain x 10 days • Pain worsened 3 days ago • Radiates to left scapula and epigastrum • Sharp, 10/10, constant pain • Worse with movement, breathing, and laying supine • SOB associated with pain • Dry Cough x 1 week
HPI • Two days prior to onset of symptoms patient strained back • One week prior to onset of symptoms patient took two 6 hour car rides • Intentional 25 lb weight loss over past 18 months • Mild reflux • LMP 1 week prior to visit • Denies: • Fever/chills • Calf Pain • Nausea/Vomiting
Allergies • NKDA Medications • Lovaza • OCP PMHx • Ovarian Cysts, Hypercholesterolemia PSHx • Tonsillectomy Social Hx • + Tobacco 1 ppd x 4 years
Vital Signs • • • Temp 97. 7 F HR 111 RR 22 BP 130/66 Sp 02 99%, room air
Physical Exam General • No Acute Distress Respiratory • Rapid, shallow breaths • CTA bilaterally • No wheezes/rales/rhonchi Cardiac • +S 1/S 2 • Regular rate and rhythm • No murmurs/rubs/gallops
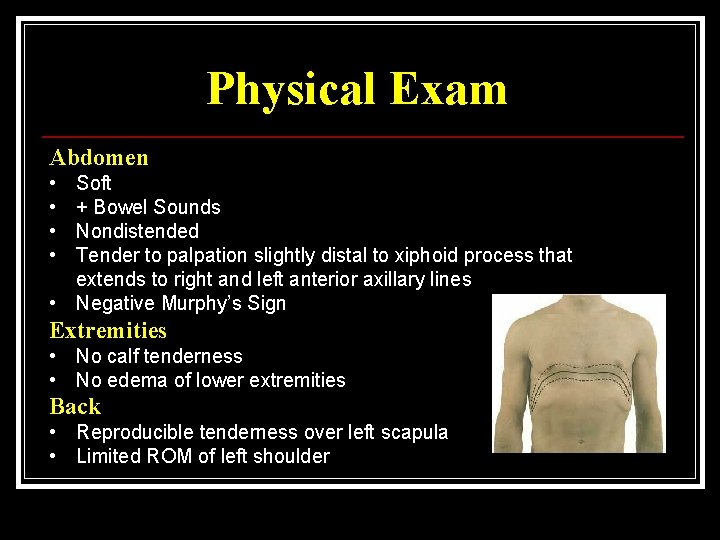
Physical Exam Abdomen • • Soft + Bowel Sounds Nondistended Tender to palpation slightly distal to xiphoid process that extends to right and left anterior axillary lines • Negative Murphy’s Sign Extremities • No calf tenderness • No edema of lower extremities Back • Reproducible tenderness over left scapula • Limited ROM of left shoulder
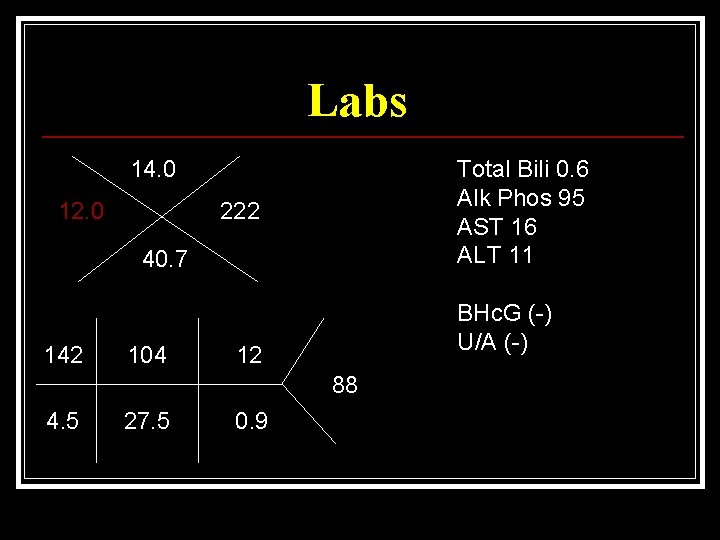
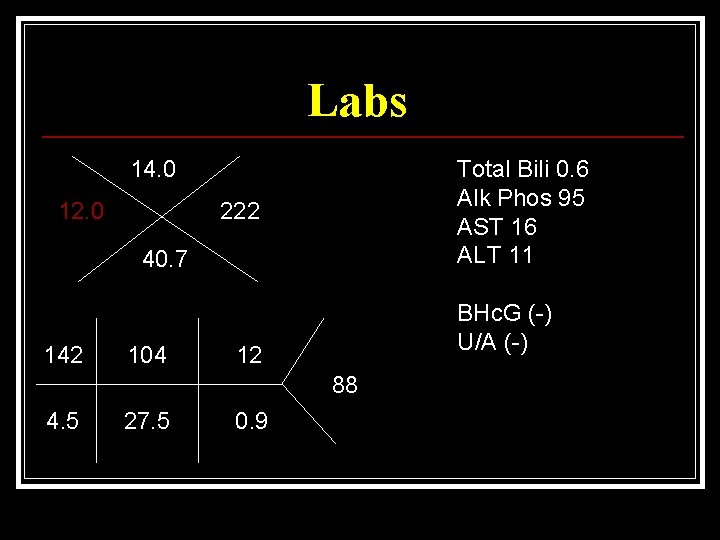
Labs 14. 0 12. 0 Total Bili 0. 6 Alk Phos 95 AST 16 ALT 11 222 40. 7 142 104 BHc. G (-) U/A (-) 12 88 4. 5 27. 5 0. 9
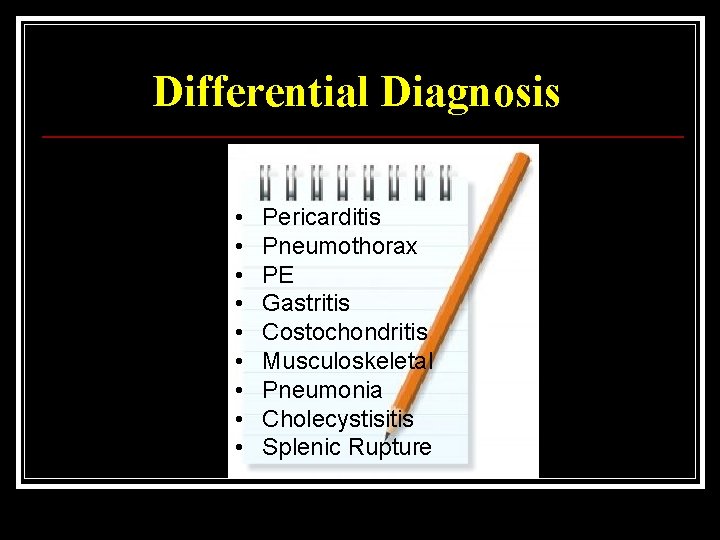
Differential Diagnosis • • • Pericarditis Pneumothorax PE Gastritis Costochondritis Musculoskeletal Pneumonia Cholecystisitis Splenic Rupture
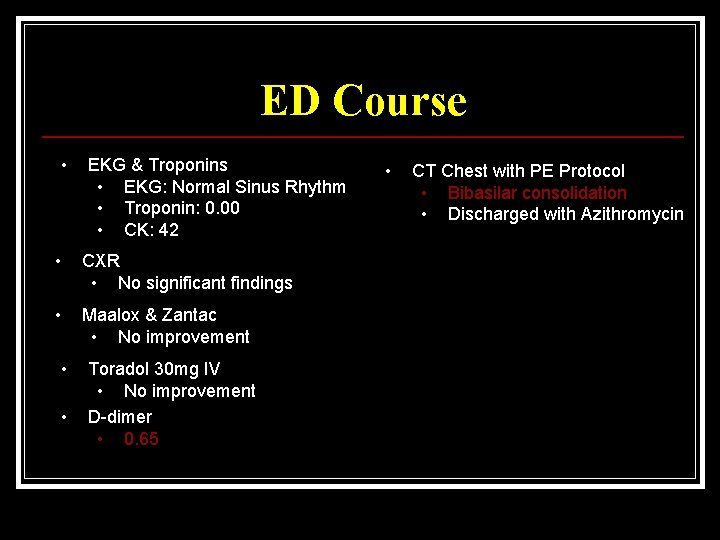
ED Course • EKG & Troponins • EKG: Normal Sinus Rhythm • Troponin: 0. 00 • CK: 42 • CXR • No significant findings • Maalox & Zantac • No improvement • • Toradol 30 mg IV • No improvement D-dimer • 0. 65 • CT Chest with PE Protocol • Bibasilar consolidation • Discharged with Azithromycin
Atypical Pneumonia • Most common organism is Mycoplasma pneumoniae • Symptoms: • • Chest Pain Headache Sore Throat Dry Cough Low-Grade Fever Fatigue Myalgias • Signs: • • Pulse-Temperature Dissociation No Signs of Consolidation • Diagnostic Studies: • PA & Lateral CXR-diffuse reticulonodular infiltrates with absent or minimal consolidation • First-Line Treatment: • Macrolides or Doxycycline
CXR vs. CT • Retrospective study determining the incidence of PNA diagnosis in the ED using thoracic CT after obtaining a negative or nondiagnostic CXR • Analyzed charts of 1057 patients diagnosed with PNA • 97 patients had both CXR and CT performed • 26 (27%) of patients had negative or non-diagnostic CXR, but CT showed infiltrate or consolidation consistent with PNA • CT has a higher sensitivity than CXR for diagnosing PNA • Concluded that future studies need to analyze radiographic diagnostic techniques used for PNA
CXR vs. CT • False Negative CXR more common: • • • dehydrated patient immunocompromised patient portable CXR done at bedside • Drawbacks to CT: • • • cost limited availability increased radiation exposure • Consider CT: • • empyema or effusion suspected immunocompromised patient underlying malignancy suspected diagnosis is unclear
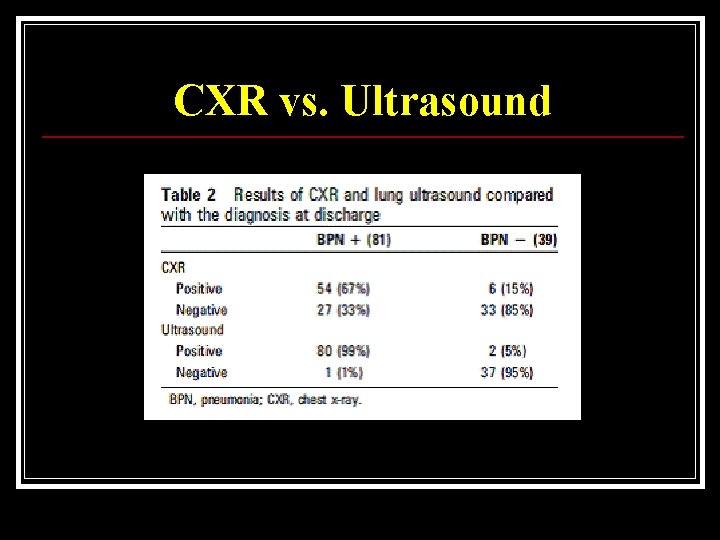
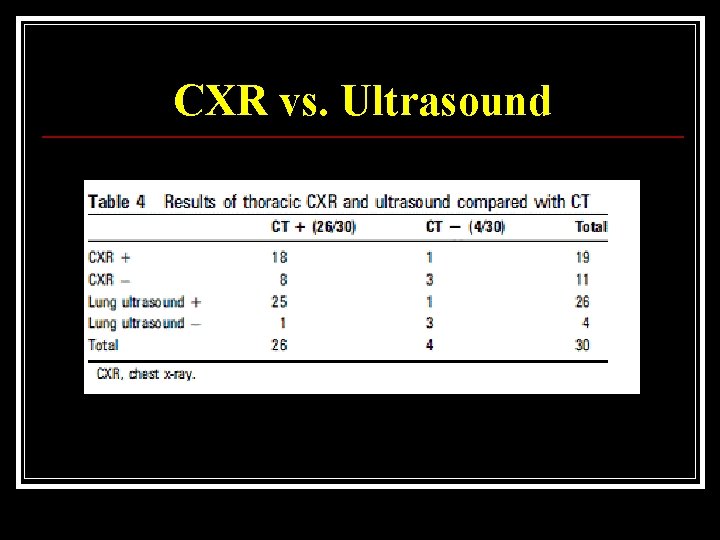
CXR vs. Ultrasound • Determine whethere is a difference in sensitivity, specificity, and likelihood ratios in the diagnosis of PNA with lung ultrasound vs. CXR • Subjects were 120 patients admitted to the hospital with communityacquired pneumonia • Ultrasound Exam: • Performed by one ED physician who was non-blinded to the subject’s clinical condition • Longitudinal and oblique views of the inferior and superior portions of the anterior and lateral chest • Two mid-posterior views • PA & Lateral CXR read by radiologist who was blinded to the subject’s clinical condition
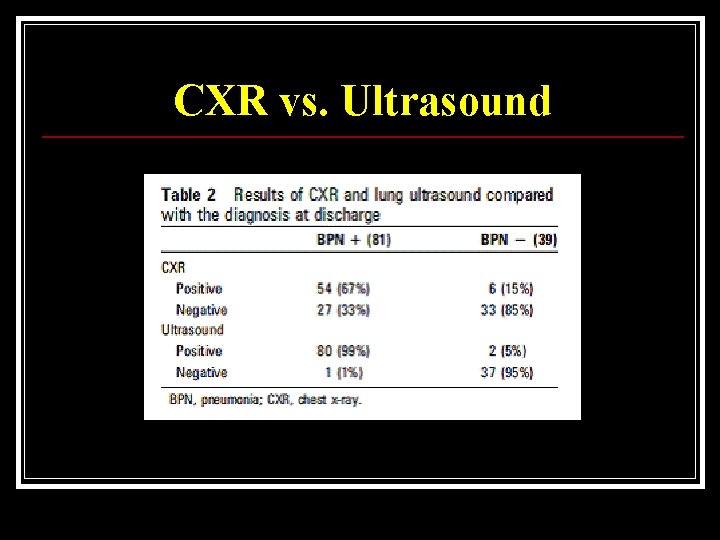
CXR vs. Ultrasound
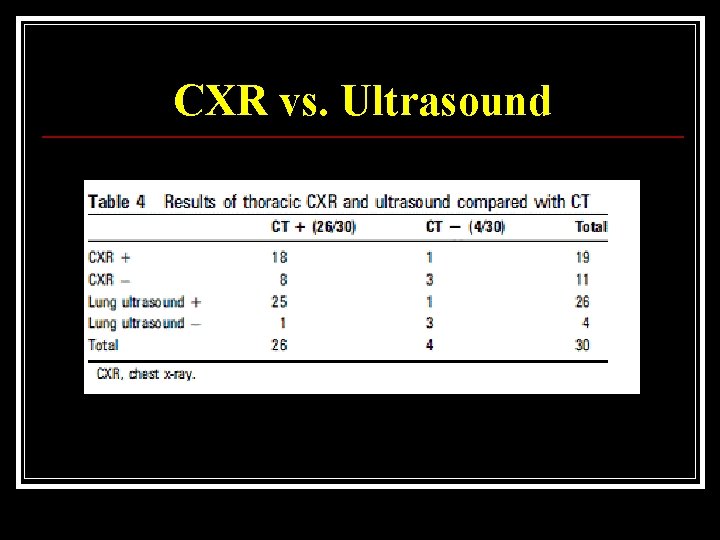
CXR vs. Ultrasound
Things to Remember… • Don’t forget to consider atypical pneumonia • When ruling out pneumonia, don’t forget that CXR can be falsely negative • Dehydrated patients • Immunocompromised patients • Ultrasound has a higher sensitivity than CXR for diagnosing pneumonia • CT continues to be the gold standard for diagnosing pneumonia
Bibliography Agabegi, Steven. Step-Up to Medicine. 2. Philadelphia: Lippincott Williams & Wilkins, 2008. Cortellaro, F. "Lung ultrasound is an accurate diagnostic tool of pneumonia in the emergency department. " Emergency Medicine Journal. 29. (2012): 19 -23. Goljan, Edward. Rapid Review: Pathology. 3. Philadelphia: Mosby Elsevier, 2010. Hayden, G. "Chest radiograph vs. computed tomography scan in the evaluation of pneumonia. " Journal of Emergency Medicine. 36. 3 (2009): 266 -270. Marrie, TJ. "A controlled trial of a critical pathway for treatment of community-acquired pneumonia. CAPITAL Study Investigators. Community-Acquired Pneumonia Intervention Trial Assessing Levofloxacin. . " JAMA. 283. 6 (2000): 749 -755.