Blood and Blood Products Whole Blood n Contents
Blood and Blood Products
Whole Blood n Contents – RBC’s – WBC’s – Platelets – Plasma – Clotting factors
Whole Blood n Indications – Acute loss of whole blood
Packed Cells n Contents – RBC’s – 20% Plasma n Indications – Replace O 2 carrying capacity with less volume – Severe anemia, slow blood loss, CHF
Granulocytes n Contents – WBC’s – 20% Plasma n Indications – Life-threatening decreases in WBC count
Platelets n Contents – Platelets – WBC’s – Plasma n Indications – Low platelet counts
Plasma n Contents – Clotting factors – Fibrinogen – Prothrombin – Albumin – Globulins
Plasma n Indications – Clotting factor deficiency – Volume expansion
Plasma Protein Fraction n Contents – 5% Albumin/Globin in saline n Indications – Expand volume in burns – Hemorrhage – Hypoproteinemia
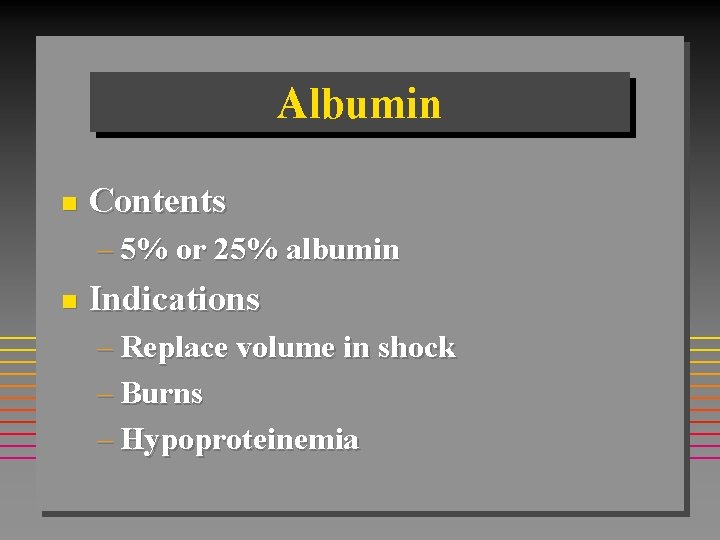
Albumin n Contents – 5% or 25% albumin n Indications – Replace volume in shock – Burns – Hypoproteinemia
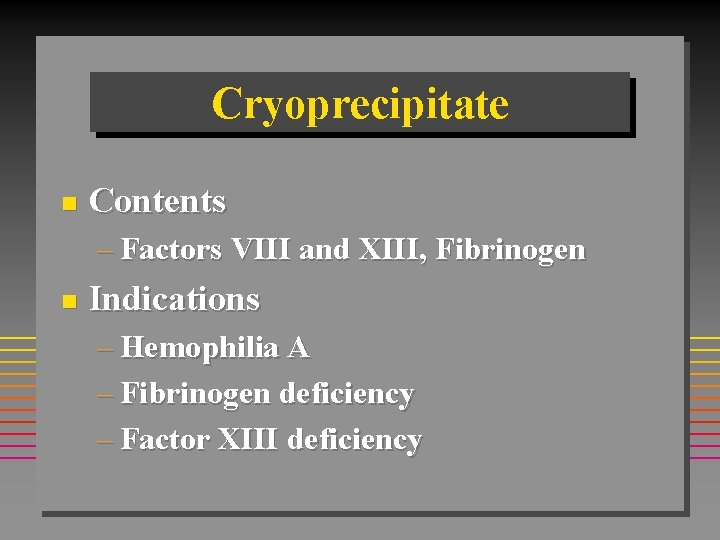
Cryoprecipitate n Contents – Factors VIII and XIII, Fibrinogen n Indications – Hemophilia A – Fibrinogen deficiency – Factor XIII deficiency
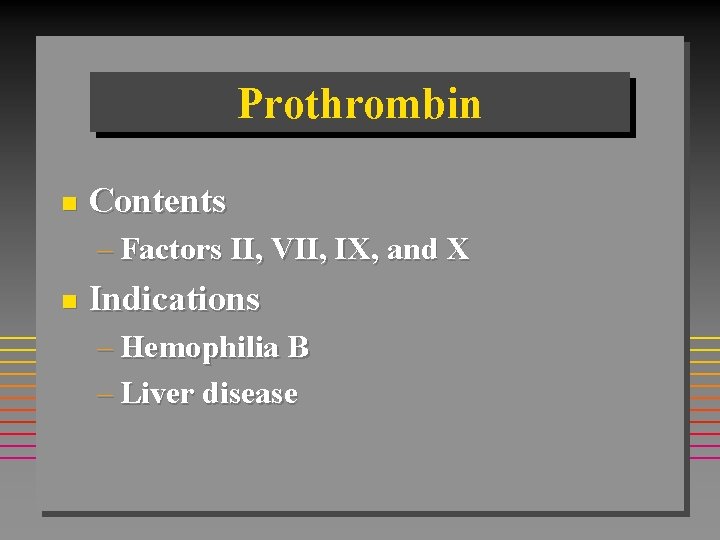
Prothrombin n Contents – Factors II, VII, IX, and X n Indications – Hemophilia B – Liver disease
Blood Transfusion
Blood Transfusion n Blood must be typed prior to administration
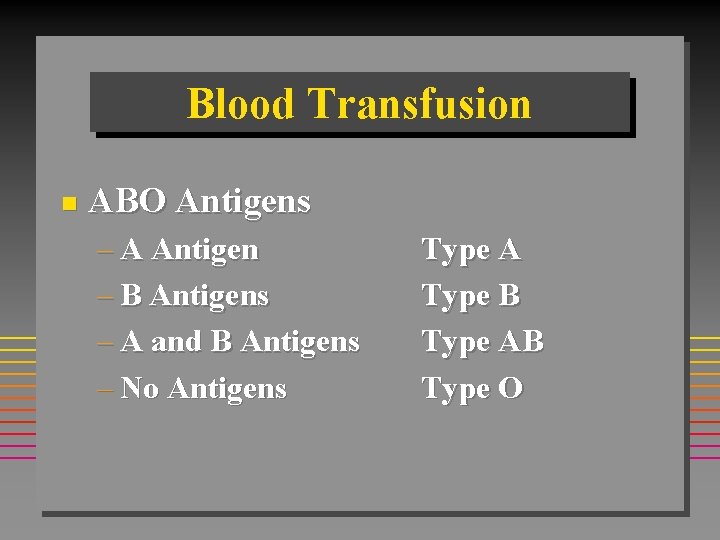
Blood Transfusion n ABO Antigens – A Antigen – B Antigens – A and B Antigens – No Antigens Type A Type B Type AB Type O
Blood Transfusions n Plasma Antibodies Agglutinate (Clump) Cells of other Types
Blood Transfusions n Type A = B Antibodies – (Clumps B or AB) n Type B = A Antibodies – (Clumps A or AB)
Blood Transfusions n Type AB = No Antibodies – (Clumps Nothing) n Type O = A and B Antibodies – (Clumps everything except O)
Blood Transfusions O Negative = Universal Donor n AB Positive = Universal Recipient n
Blood Transfusions n Rh Factor – 85% of Population » Rh Positive – 15% of Population » Rh Negative
Blood Transfusions Rh Negative patients produce Rh antibodies only if exposed to Rh Positive blood
Blood Transfusions n Erythroblastosis Fetalis – Rh Negative mother exposed to Rh Positive fetal blood during delivery – Mother produces Rh Antibodies – Antibodies cross placenta during subsequent pregnancy – Fetal blood hemolyses
Blood Transfusions n Erythroblastosis Fetalis – Prevented by administration of Rhogam to mother
Transfusion Complications
Fever Most common reaction n Donor WBC incompatabilities n Antipyretics n
Allergic Reactions n Signs/Symptoms – Itching – Uticaria – Chills – Fever – Facial edema – Wheezing – Anaphylactic shock
Allergic Reactions n Management – Oxygen – IV fluids – Epinephrine – Antihistamines
Hemolytic Reaction n Signs/Symptoms – – – – – Chills, fever Low back pain Headache Chest pain Dyspnea Cyanosis Restlessness, anxiety Hypotension Red urine
Hemolytic Reaction n Management – Stop transfusion – Treat shock – Volume replacement – Mannitol
Volume Overload n Signs/Symptoms – Cough – Chest pain – Dyspnea – Distended neck veins – Rales – Frothy sputum
Volume Overload n Management – Slow infusion – Diuretics – Vasodilators
Transfusion Complications n Coagulation Disturbances – Platelet/Clotting factor deterioration n Citrate Intoxication – Hypocalcemia – Metabolic Alkalosis n Hyperkalemia – RBC’s Lyse/Release K+
Transfusion Complications n Acid/Base Imbalances – Banked blood gradually acidifies n Poor tissue Oxygenation – Loss of 2, 3 DPG
Transfusion Complications n Hypothermia – Inadequate warming during transfusion n Viral Hepatitis – Risk rises with each unit
Blood Transfusion IV catheter 18 g or larger n No fluid other than saline n – D 5 W lyses RBC’s – LR contains calcium/triggers clotting Two persons confirm ABO/Rh n Blood filter in administration set n
Blood Transfusion n Infusion pumps – Excessive pressure can cause hemolysis Rewarming above 380 C can cause hemolysis n Never add medications directly n
- Slides: 36