ARRHYTHMIAS DANNY HAYWOOD FY 1 INTRO Conduction system




- Slides: 42
ARRHYTHMIAS DANNY HAYWOOD FY 1
INTRO • • • Conduction system of heart Symptoms/signs Investigations Tachy vs Bradyarrhythmias • Different types • Management • Tachyarrhythmias • Broad vs narrow • Types of each • Management of each • Summary • Some example ECGs

SYMPTOMS/SIGNS • • Syncope Dizziness Palpitations Heart Failure Chest pain Sudden death No symptoms

INVESTIGATIONS • Bedside • ECG • Bloods • TFTs, U+E, FBC, Troponins • Imaging • Echo, CXR • Special tests • Holter monitor

ARRHYTHMIAS • Bradyarrhythmias vs Tachyarrhythmias • Brady • HR < 60 bpm • Tachy • HR > 100 bpm
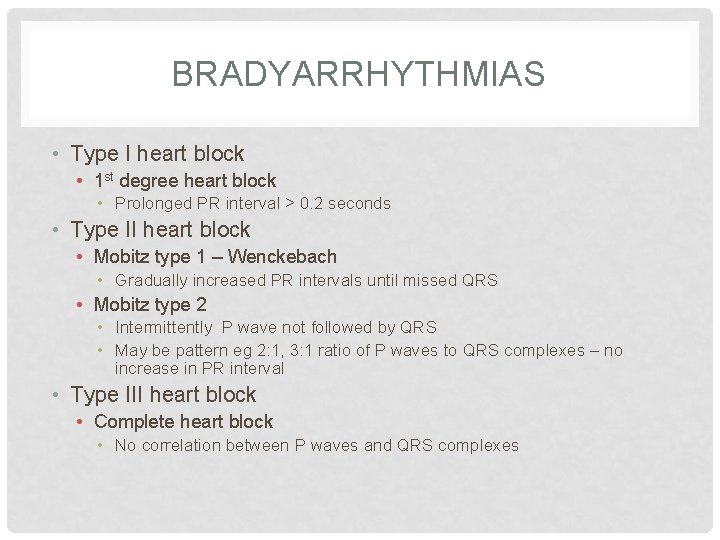
BRADYARRHYTHMIAS • Type I heart block • 1 st degree heart block • Prolonged PR interval > 0. 2 seconds • Type II heart block • Mobitz type 1 – Wenckebach • Gradually increased PR intervals until missed QRS • Mobitz type 2 • Intermittently P wave not followed by QRS • May be pattern eg 2: 1, 3: 1 ratio of P waves to QRS complexes – no increase in PR interval • Type III heart block • Complete heart block • No correlation between P waves and QRS complexes
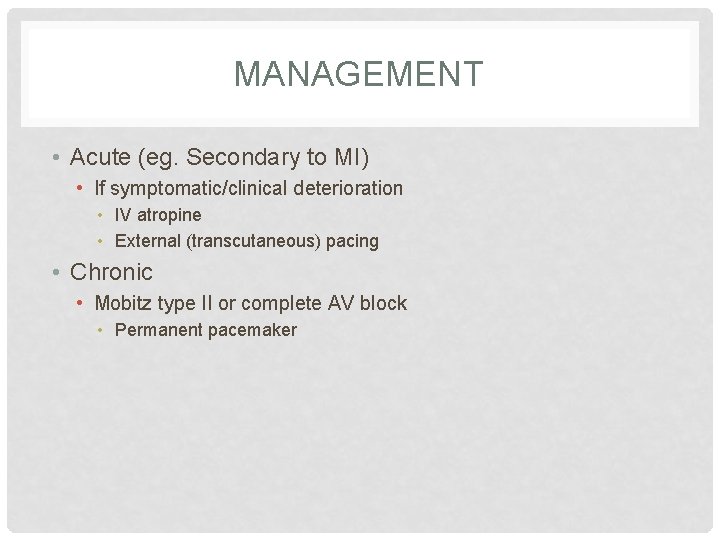
MANAGEMENT • Acute (eg. Secondary to MI) • If symptomatic/clinical deterioration • IV atropine • External (transcutaneous) pacing • Chronic • Mobitz type II or complete AV block • Permanent pacemaker
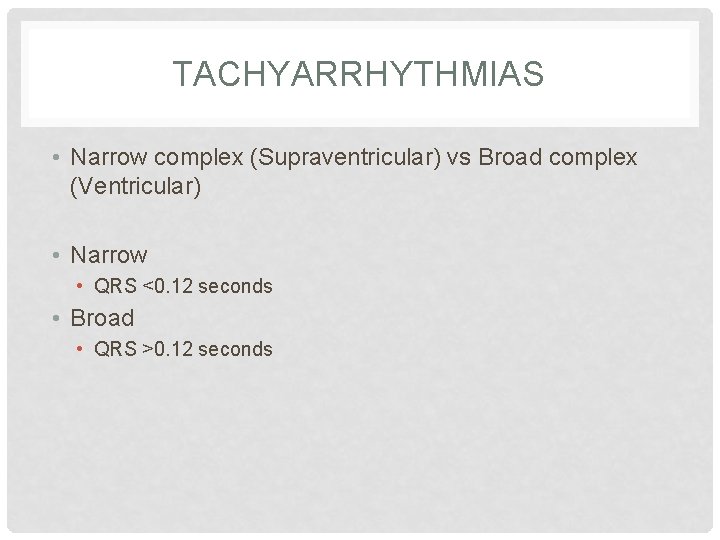
TACHYARRHYTHMIAS • Narrow complex (Supraventricular) vs Broad complex (Ventricular) • Narrow • QRS <0. 12 seconds • Broad • QRS >0. 12 seconds
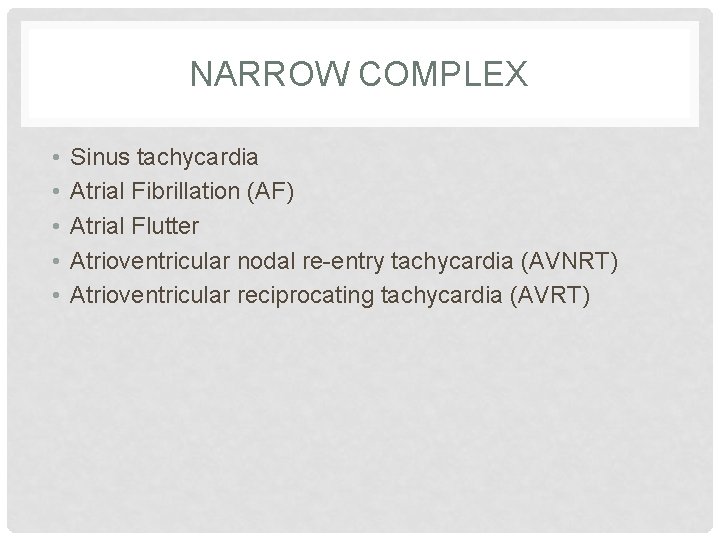
NARROW COMPLEX • • • Sinus tachycardia Atrial Fibrillation (AF) Atrial Flutter Atrioventricular nodal re-entry tachycardia (AVNRT) Atrioventricular reciprocating tachycardia (AVRT)
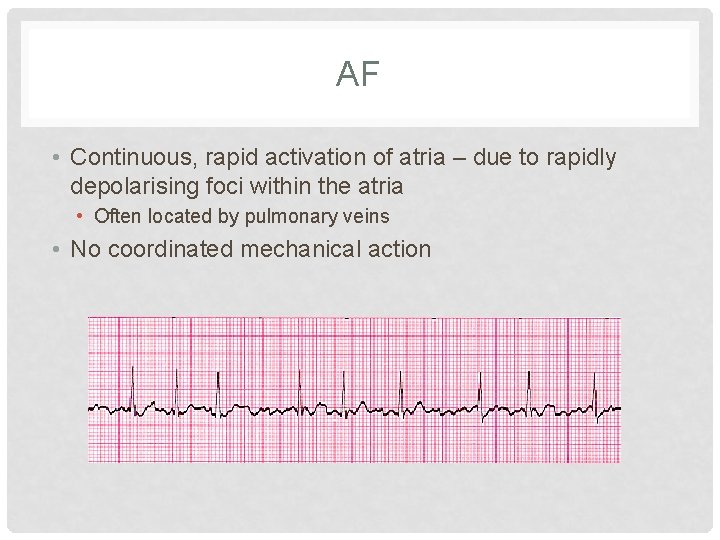
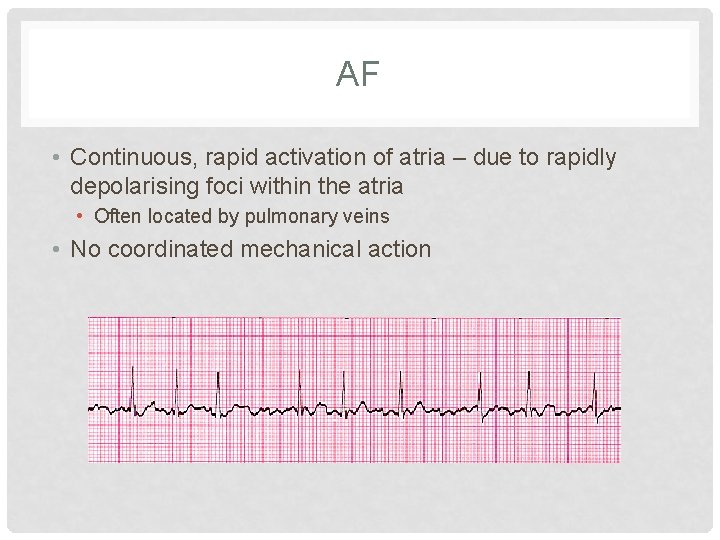
AF • Continuous, rapid activation of atria – due to rapidly depolarising foci within the atria • Often located by pulmonary veins • No coordinated mechanical action
AF – CAUSES • ATRIAL Ph. IB • • • A – Alcohol T – Thyroid disease R – Rheumatic heart disease I – Ischaemic heart disease A – Atrial myxoma L – Lung pathology (pneumonia, PE) • Ph – Pheochromocytoma • I – Idiopathic • B – Blood pressure (hypertension)
AF - MANAGEMENT • Conservative • Alcohol cessation • Lifestyle factors (diet/exercise/smoking) • Medical • Treat underlying cause • Rate control vs rhythm control • Interventional • Catheter ablation
RATE CONTROL • Older age, permanent AF • Bisoprolol/verapamil and Warfarin (CHADSVASc)
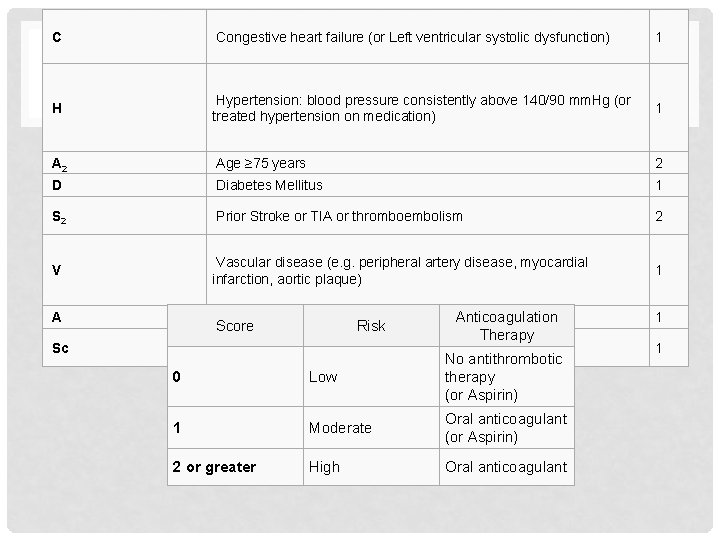
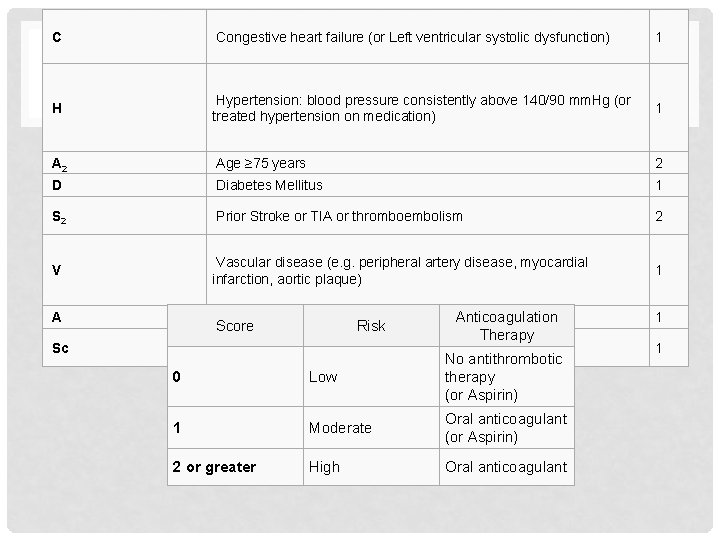
C Congestive heart failure (or Left ventricular systolic dysfunction) 1 CHADSVASC H Hypertension: blood pressure consistently above 140/90 mm. Hg (or treated hypertension on medication) 1 A 2 Age ≥ 75 years 2 D Diabetes Mellitus 1 S 2 Prior Stroke or TIA or thromboembolism 2 V Vascular disease (e. g. peripheral artery disease, myocardial infarction, aortic plaque) 1 A Age 65– 74 years Sc Sex category (i. e. female gender) Score Risk Anticoagulation Therapy 0 Low No antithrombotic therapy (or Aspirin) 1 Moderate Oral anticoagulant (or Aspirin) 2 or greater High Oral anticoagulant 1 1
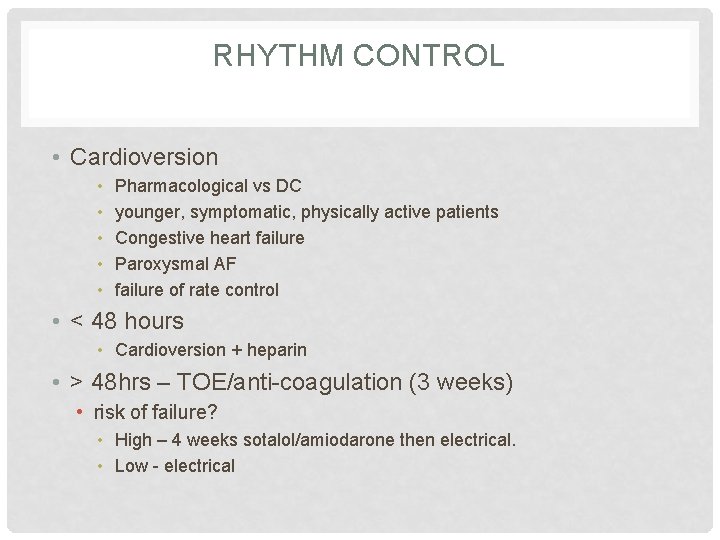
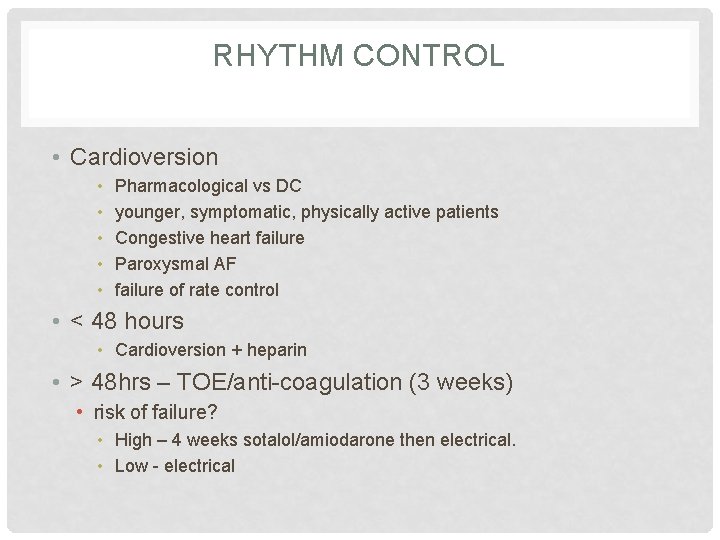
RHYTHM CONTROL • Cardioversion • • • Pharmacological vs DC younger, symptomatic, physically active patients Congestive heart failure Paroxysmal AF failure of rate control • < 48 hours • Cardioversion + heparin • > 48 hrs – TOE/anti-coagulation (3 weeks) • risk of failure? • High – 4 weeks sotalol/amiodarone then electrical. • Low - electrical
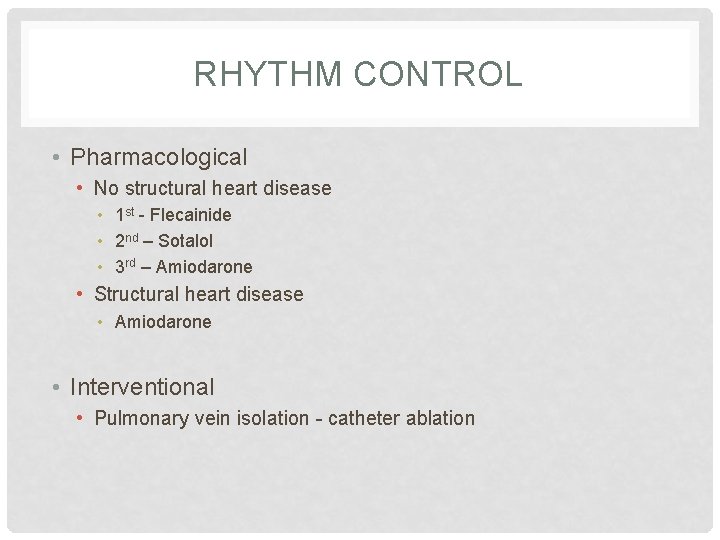
RHYTHM CONTROL • Pharmacological • No structural heart disease • 1 st - Flecainide • 2 nd – Sotalol • 3 rd – Amiodarone • Structural heart disease • Amiodarone • Interventional • Pulmonary vein isolation - catheter ablation
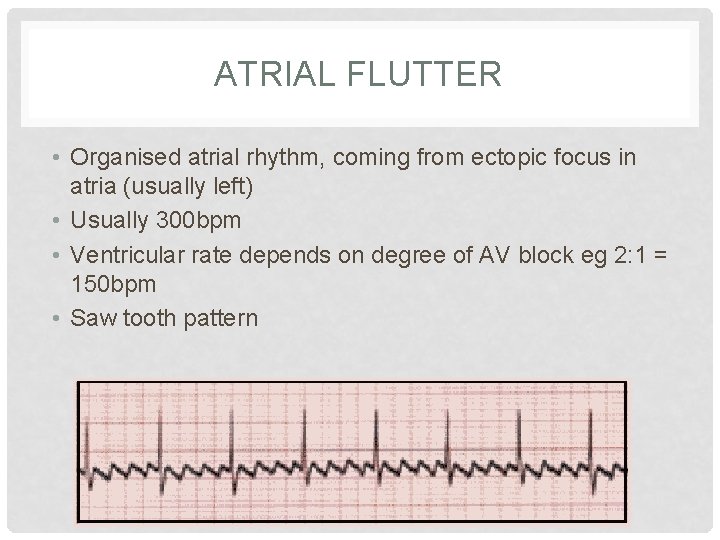
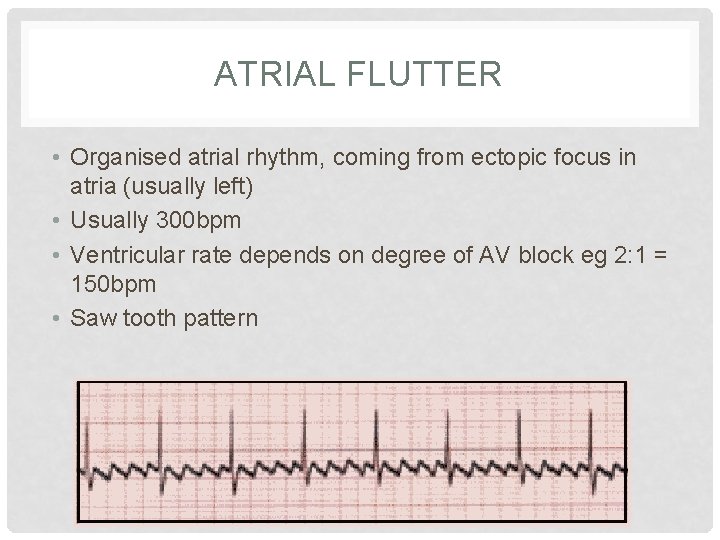
ATRIAL FLUTTER • Organised atrial rhythm, coming from ectopic focus in atria (usually left) • Usually 300 bpm • Ventricular rate depends on degree of AV block eg 2: 1 = 150 bpm • Saw tooth pattern
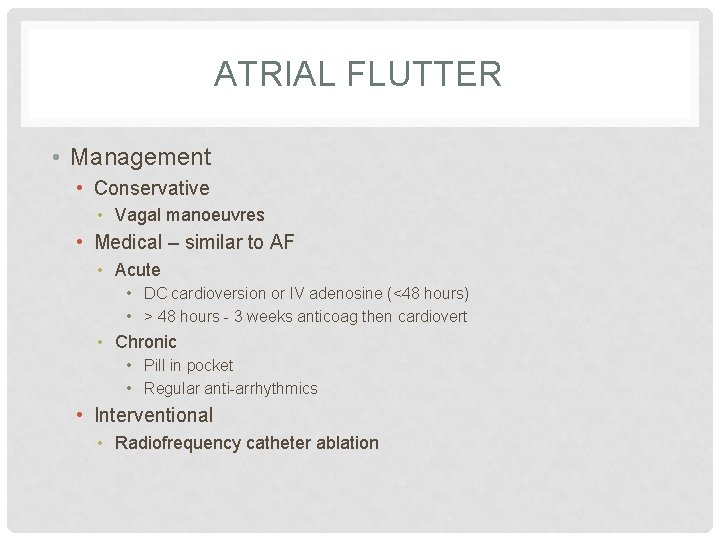
ATRIAL FLUTTER • Management • Conservative • Vagal manoeuvres • Medical – similar to AF • Acute • DC cardioversion or IV adenosine (<48 hours) • > 48 hours - 3 weeks anticoag then cardiovert • Chronic • Pill in pocket • Regular anti-arrhythmics • Interventional • Radiofrequency catheter ablation
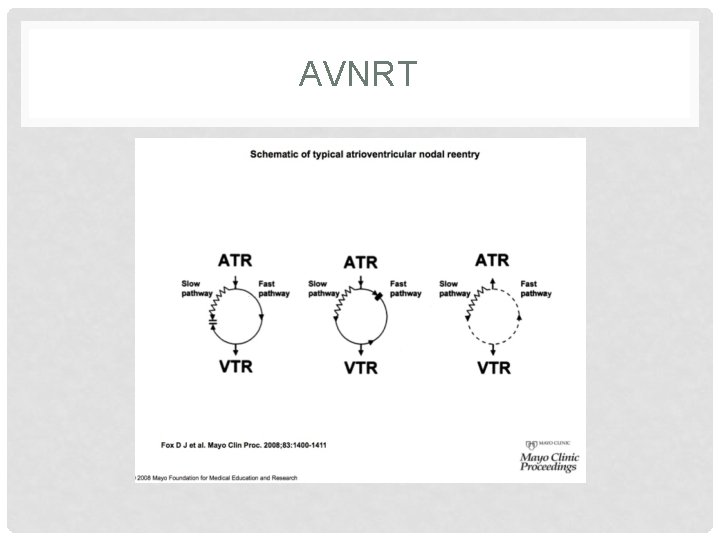
AVNRT • 2 pathways within the AV node 1) short refractory period + slow conduction 2) long refractory period + fast conduction • Normally conducts through fast pathway • If premature atrial beat, fast pathway still refractory (long refractory period) therefore travels down slow pathway and back up the fast pathway.
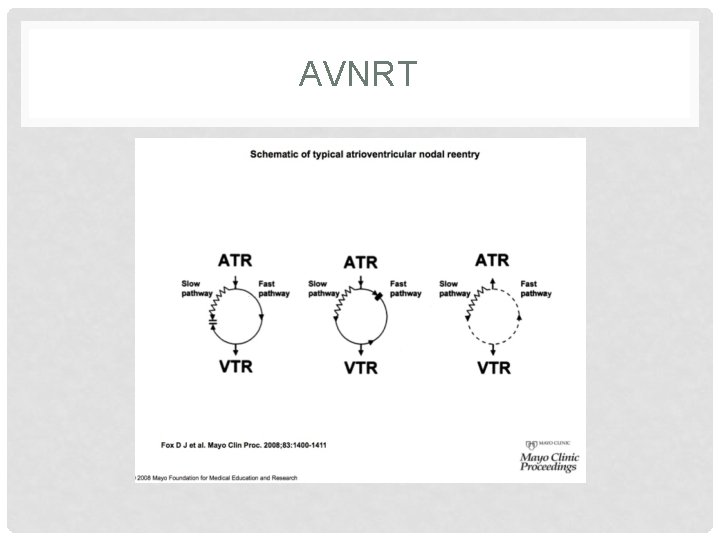
AVNRT
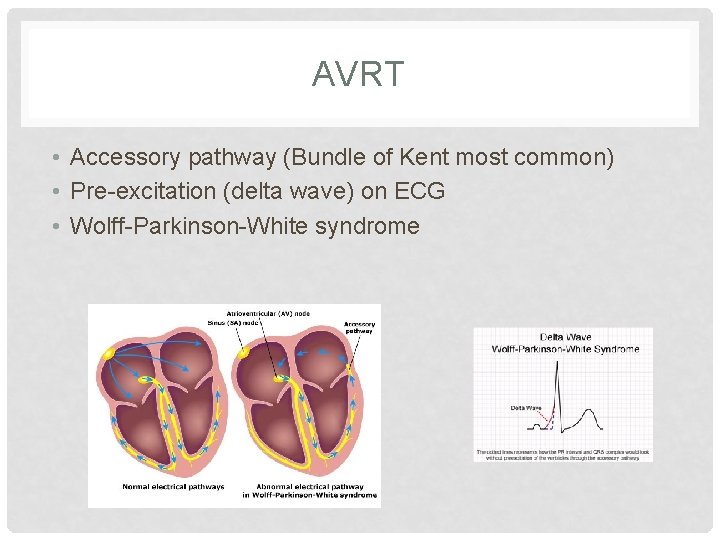
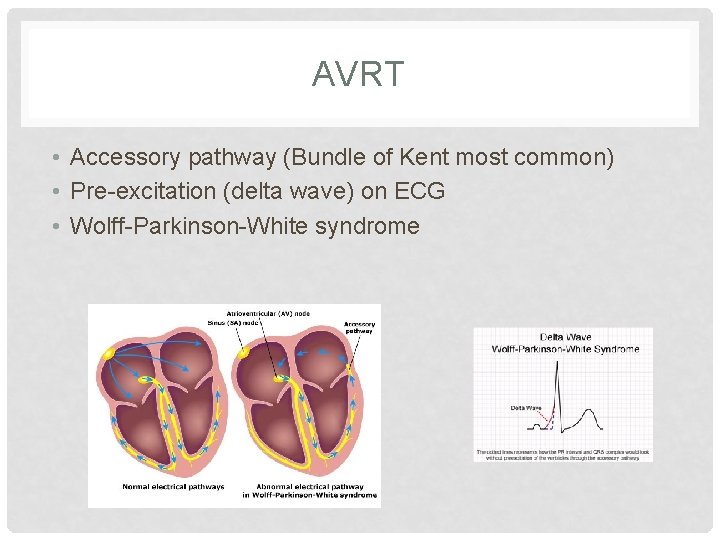
AVRT • Accessory pathway (Bundle of Kent most common) • Pre-excitation (delta wave) on ECG • Wolff-Parkinson-White syndrome
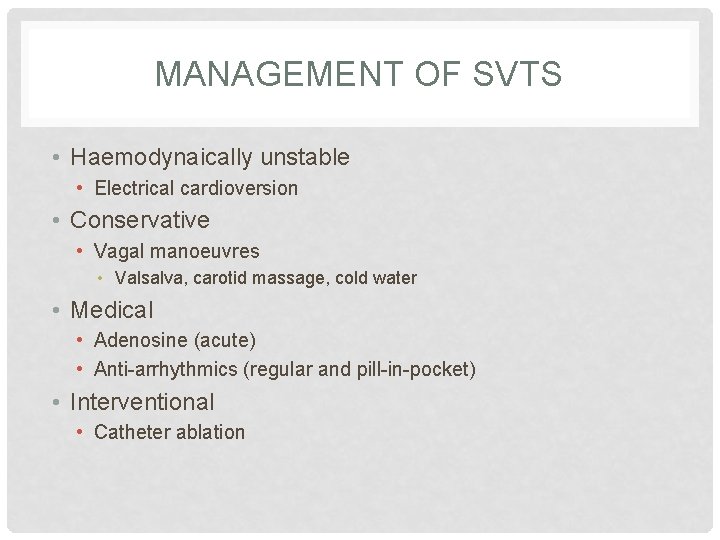
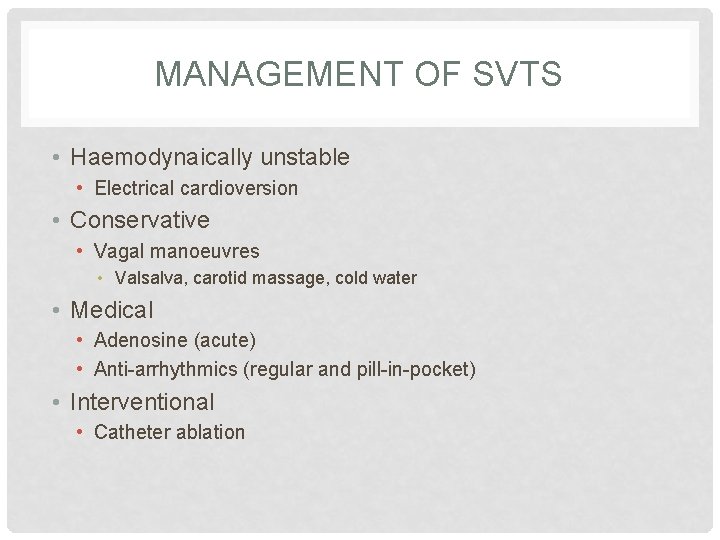
MANAGEMENT OF SVTS • Haemodynaically unstable • Electrical cardioversion • Conservative • Vagal manoeuvres • Valsalva, carotid massage, cold water • Medical • Adenosine (acute) • Anti-arrhythmics (regular and pill-in-pocket) • Interventional • Catheter ablation
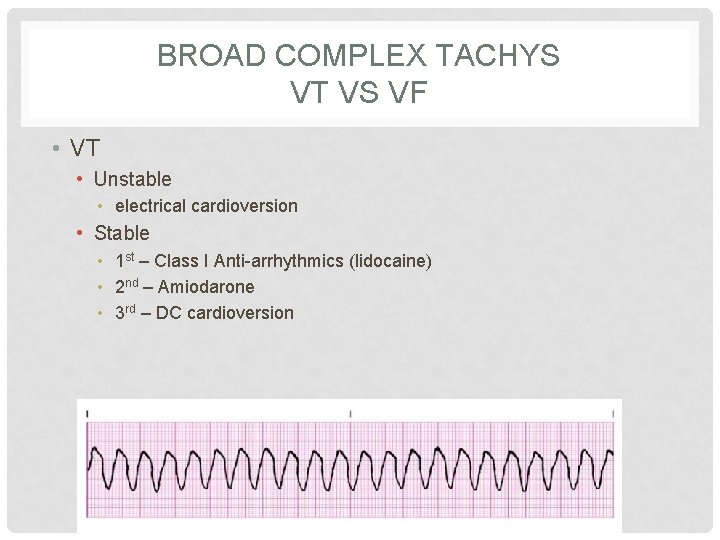
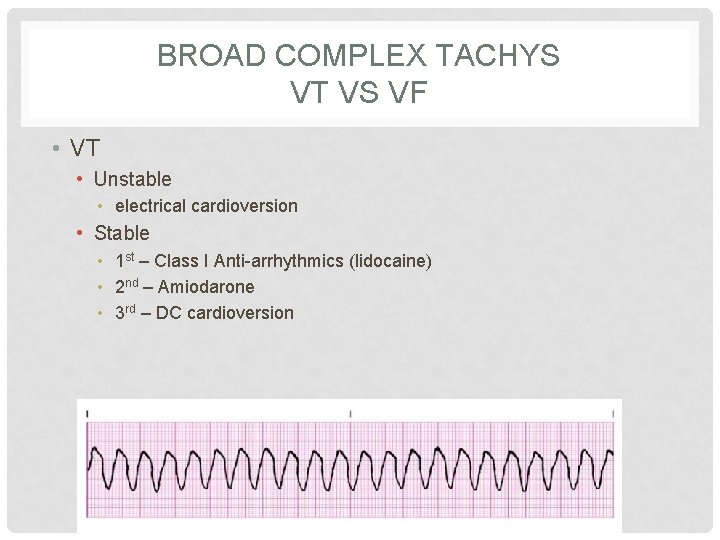
BROAD COMPLEX TACHYS VT VS VF • VT • Unstable • electrical cardioversion • Stable • 1 st – Class I Anti-arrhythmics (lidocaine) • 2 nd – Amiodarone • 3 rd – DC cardioversion
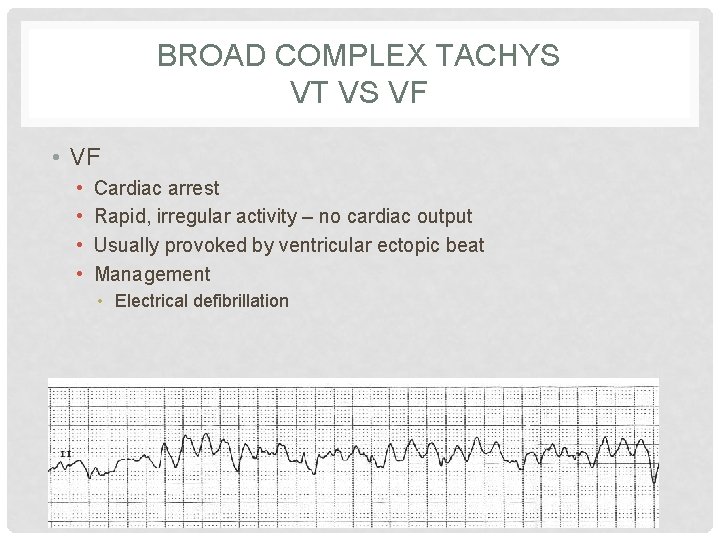
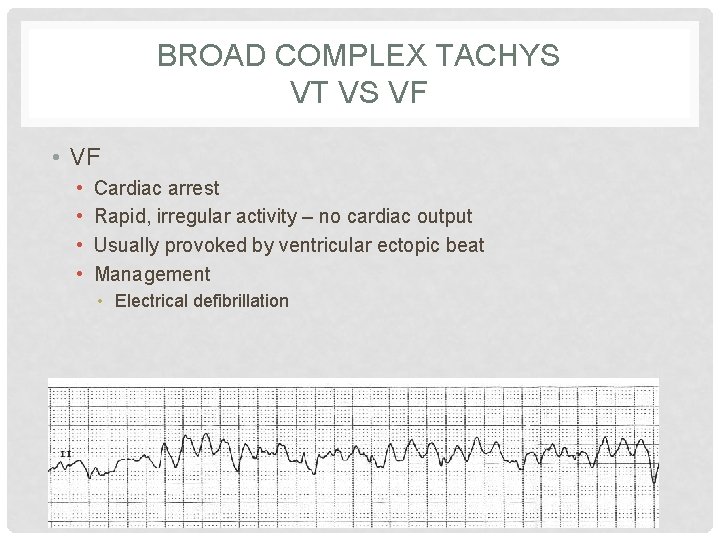
BROAD COMPLEX TACHYS VT VS VF • • Cardiac arrest Rapid, irregular activity – no cardiac output Usually provoked by ventricular ectopic beat Management • Electrical defibrillation
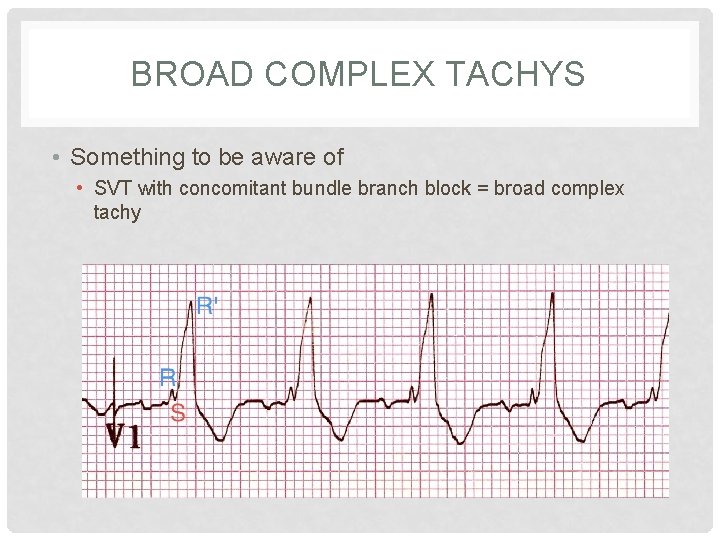
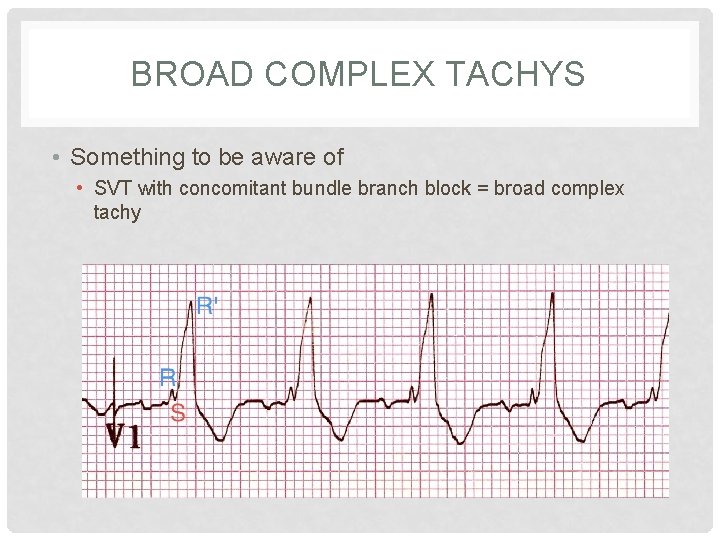
BROAD COMPLEX TACHYS • Something to be aware of • SVT with concomitant bundle branch block = broad complex tachy

SUMMARY • Brady vs tachy • Brady • • Sinus Brady 1 st degree heart block Mobitz I & II Complete • Tachy • Narrow • Sinus tachy, AF, Flutter, AVNRT, AVRT • Broad • VT, VF, • Remember causes of AF
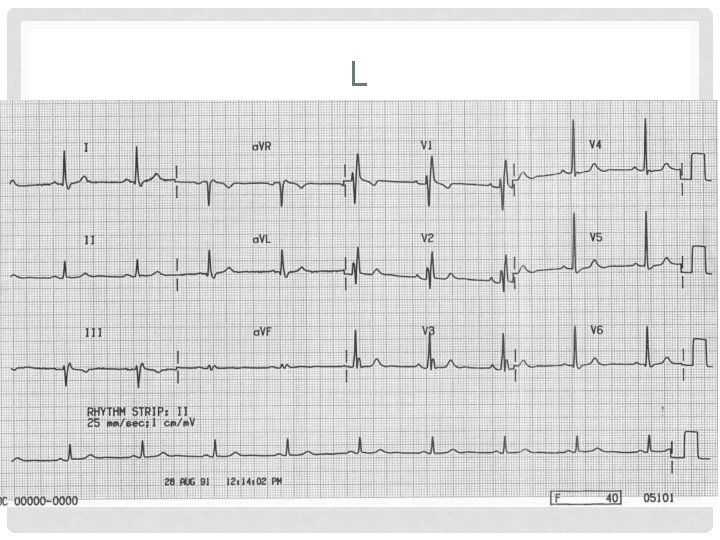
ECGS – TEST YOURSELF
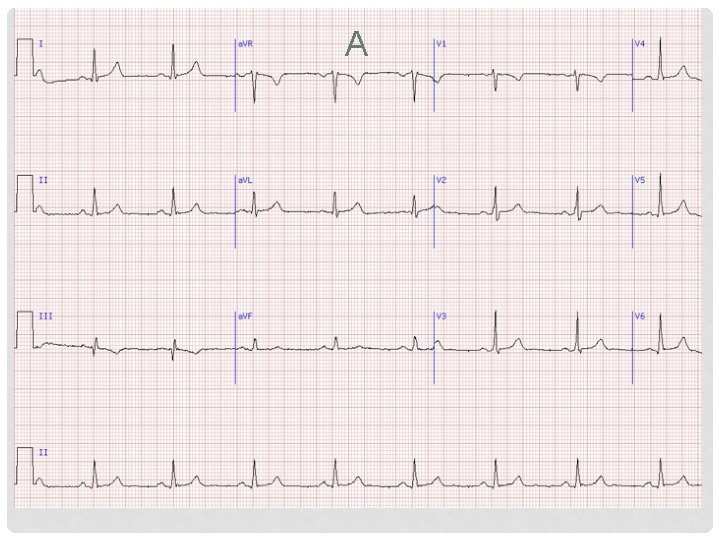
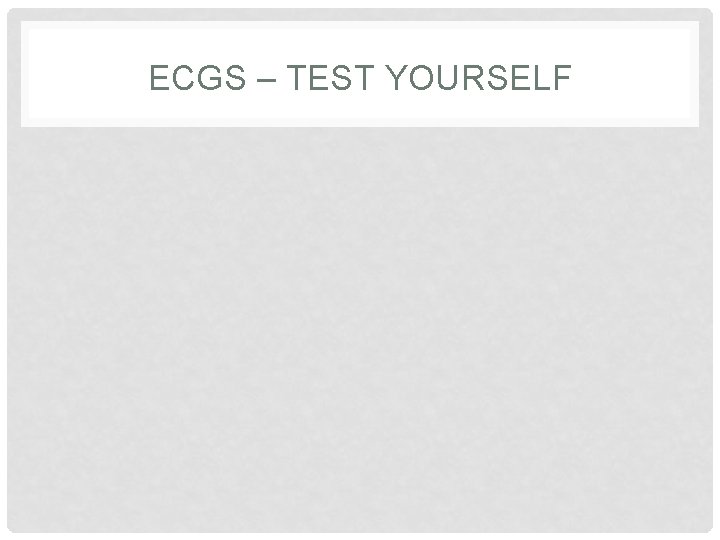
A
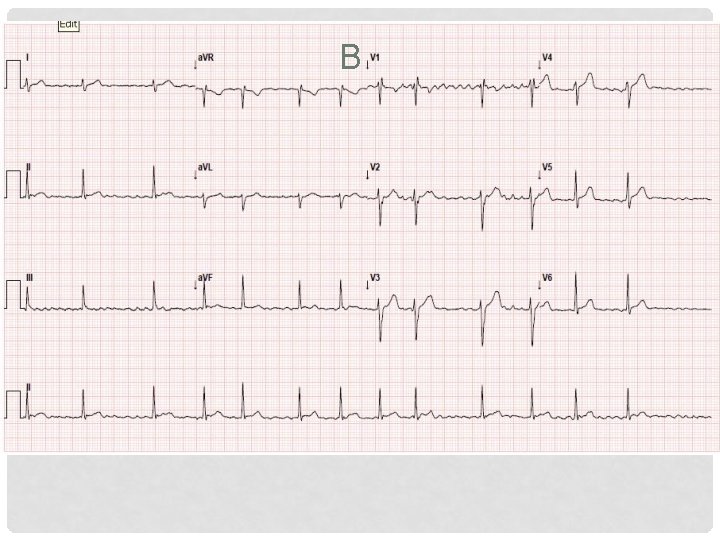
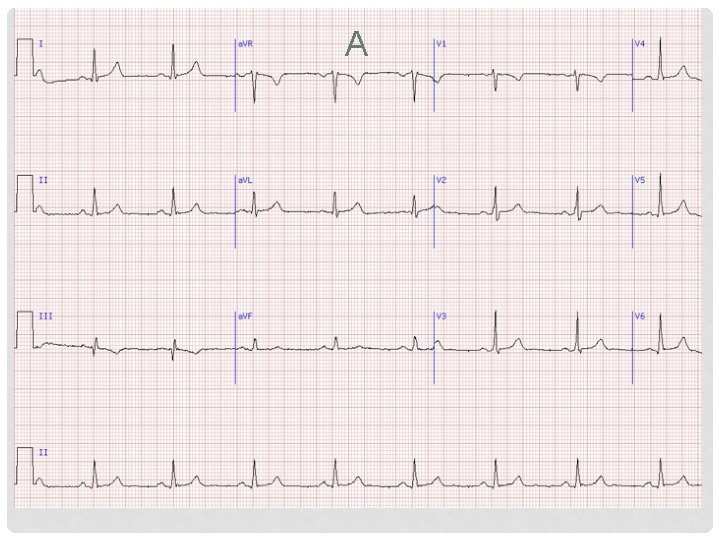
B
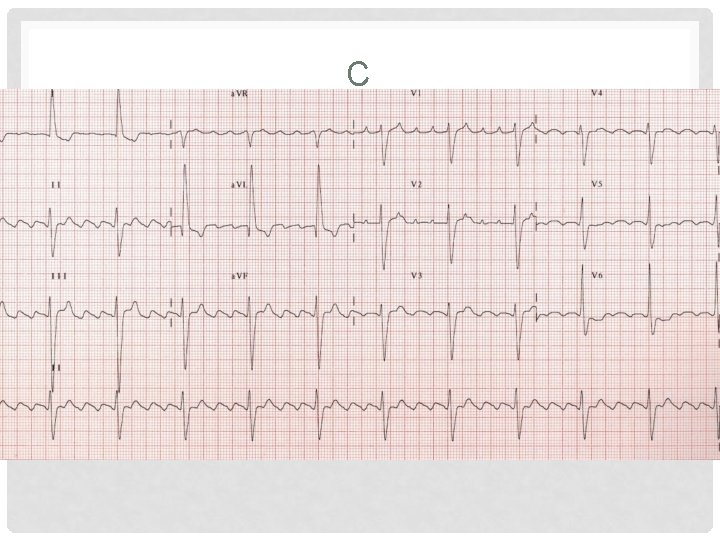
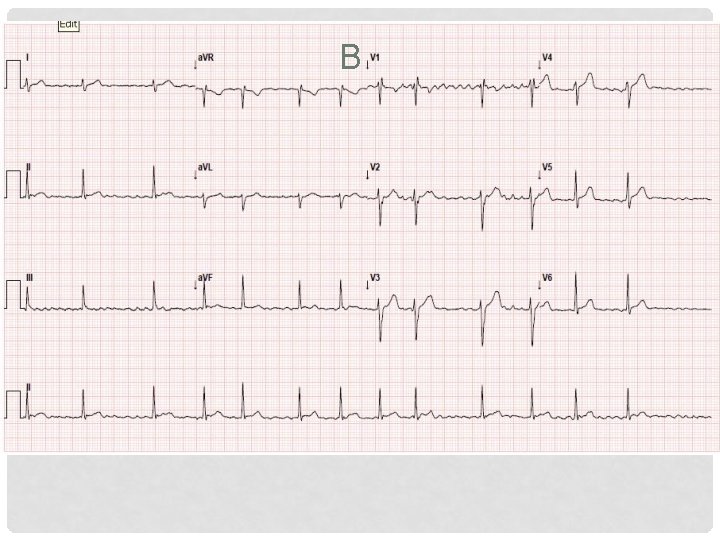
C
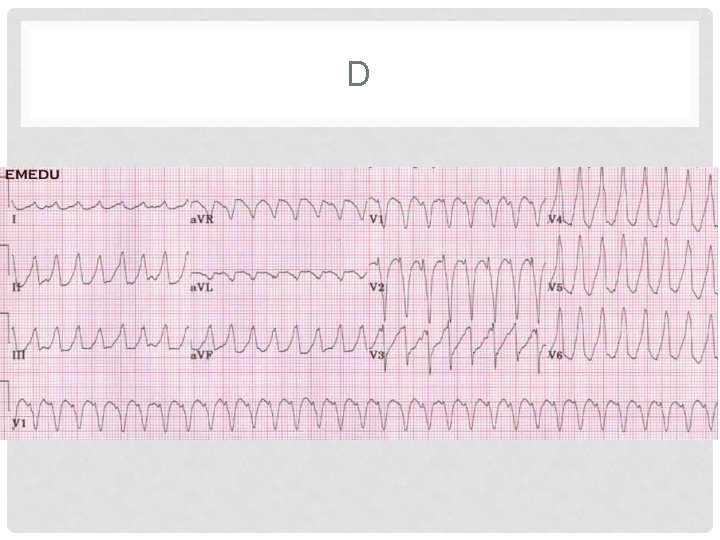
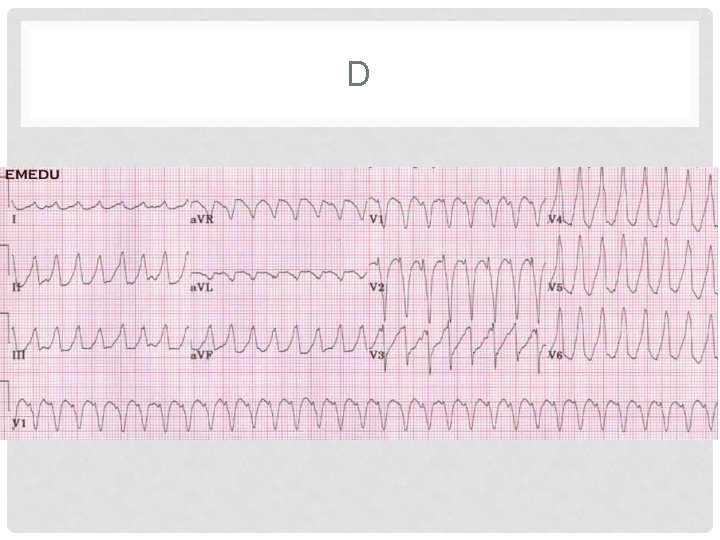
D
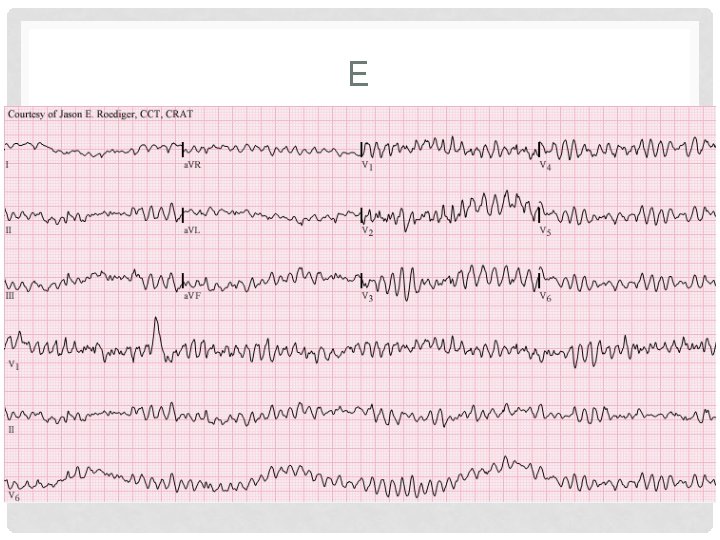
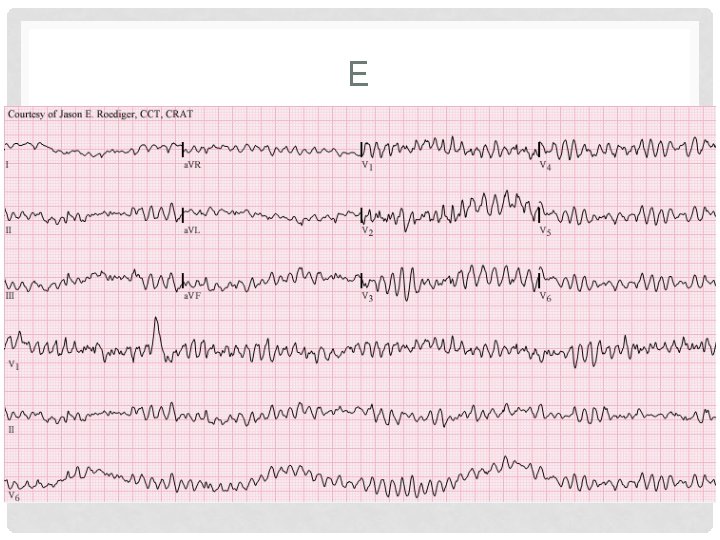
E
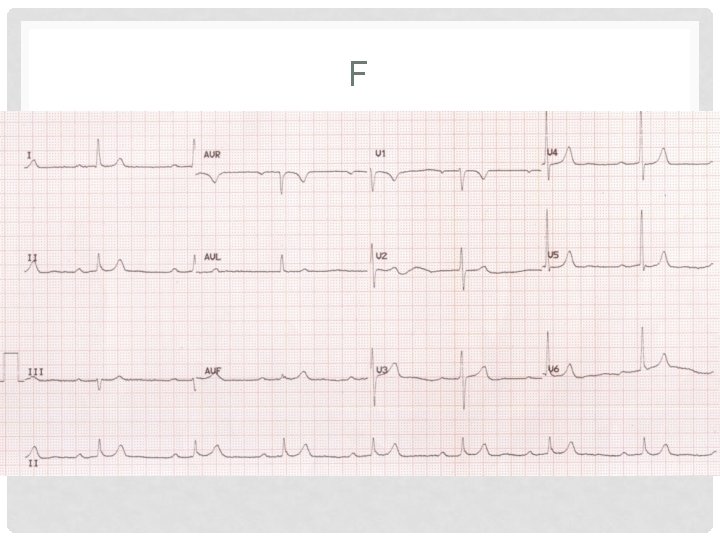
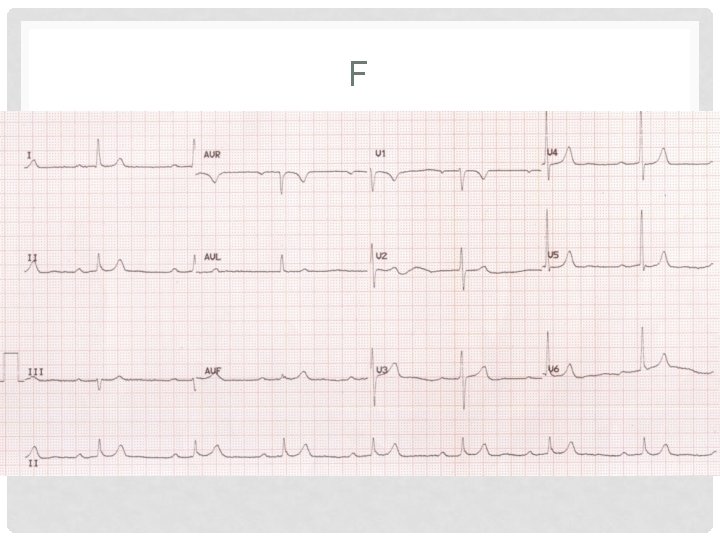
F
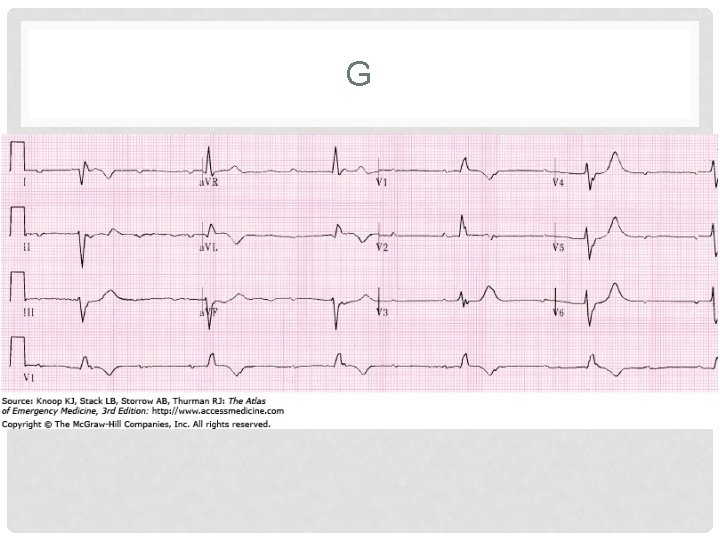
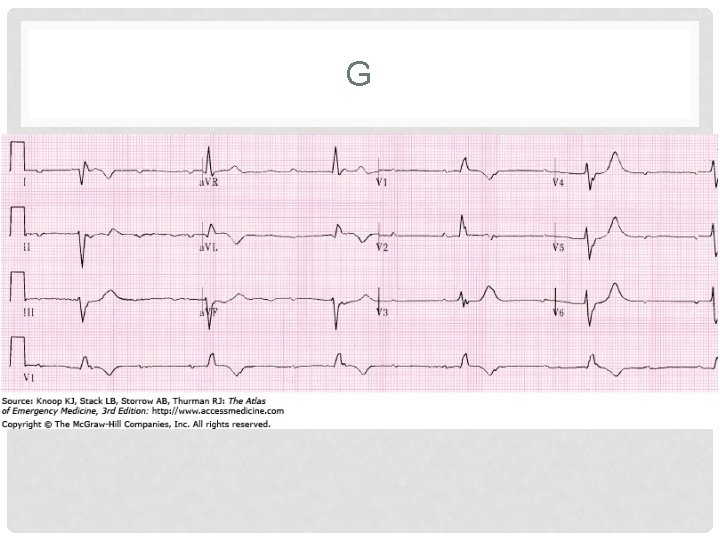
G
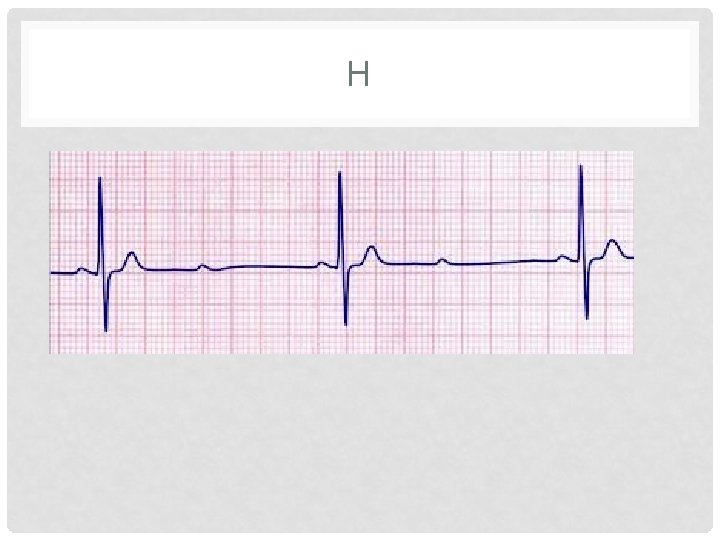
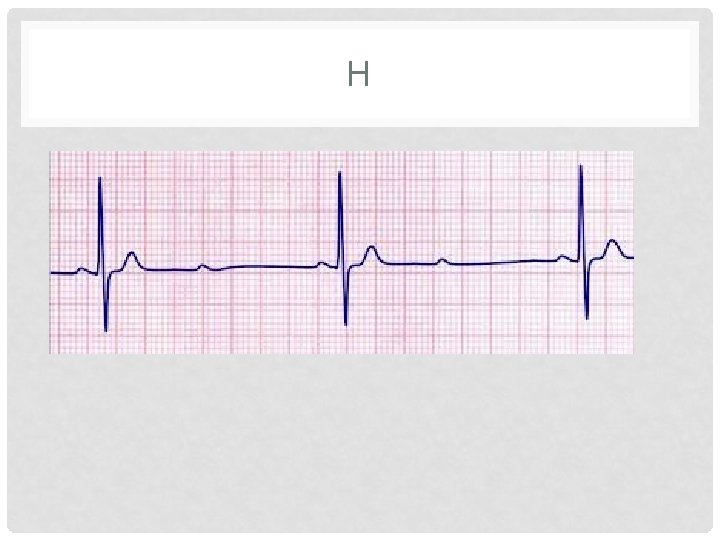
H
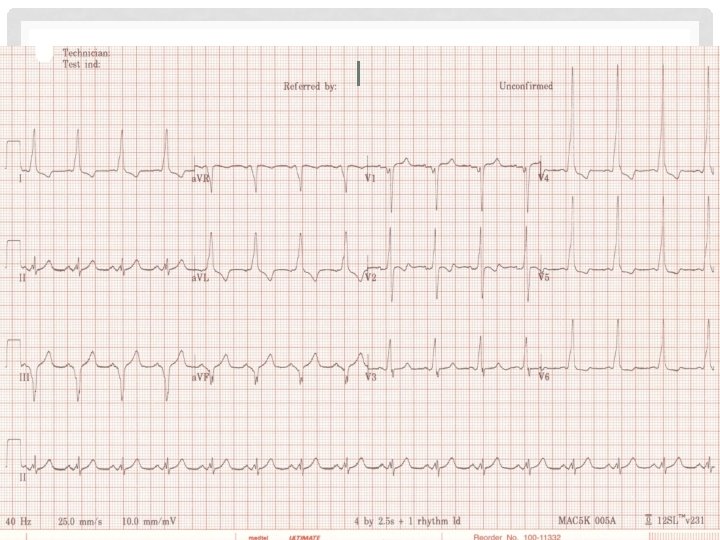
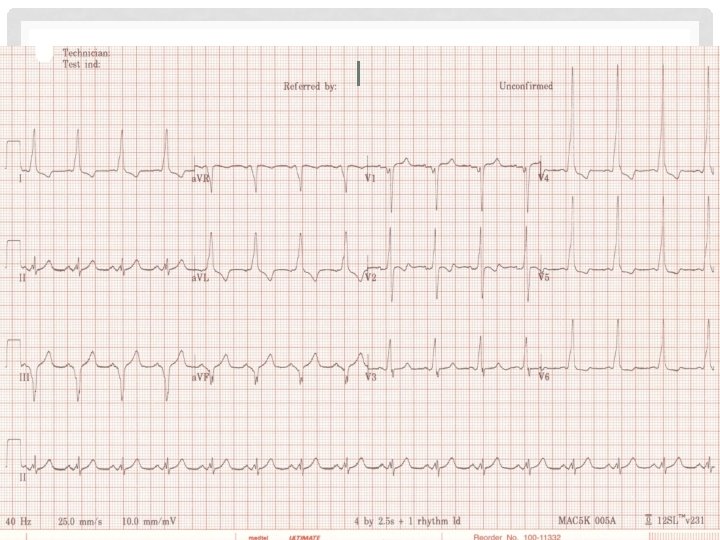
I
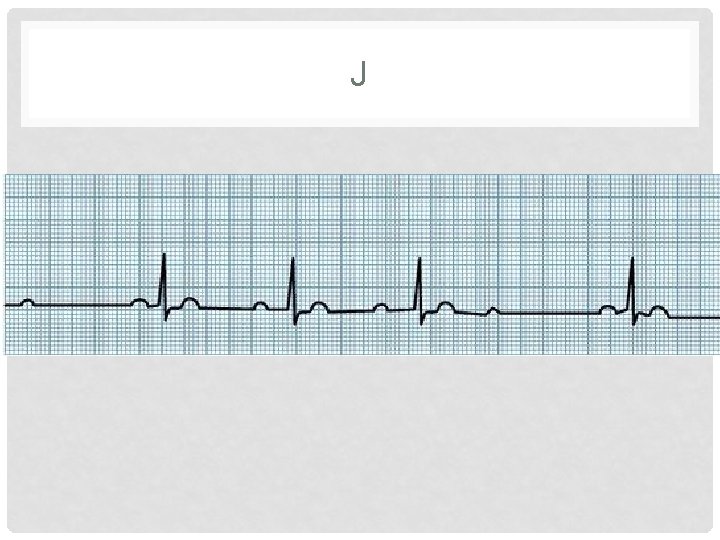
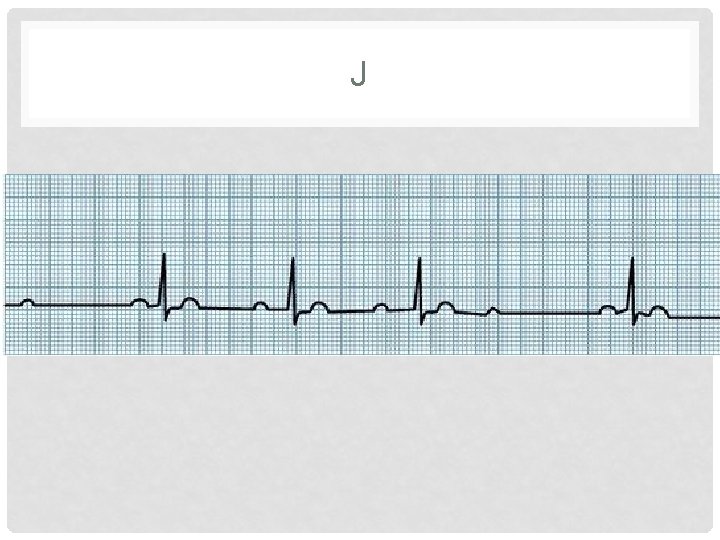
J
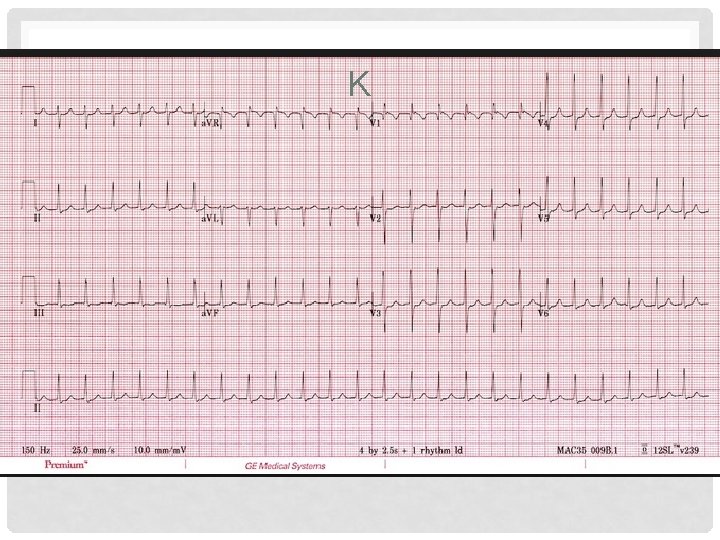
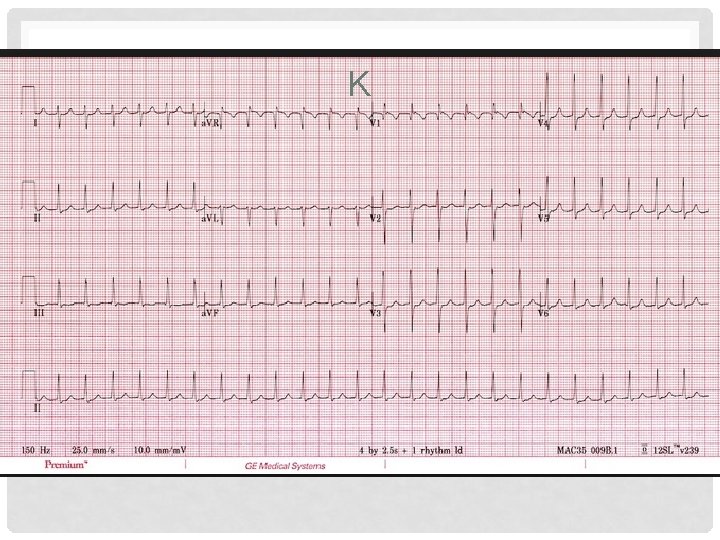
K
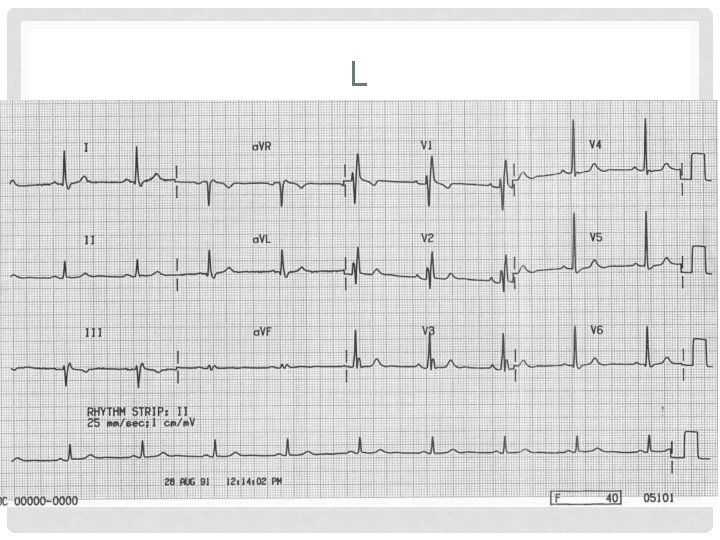
L
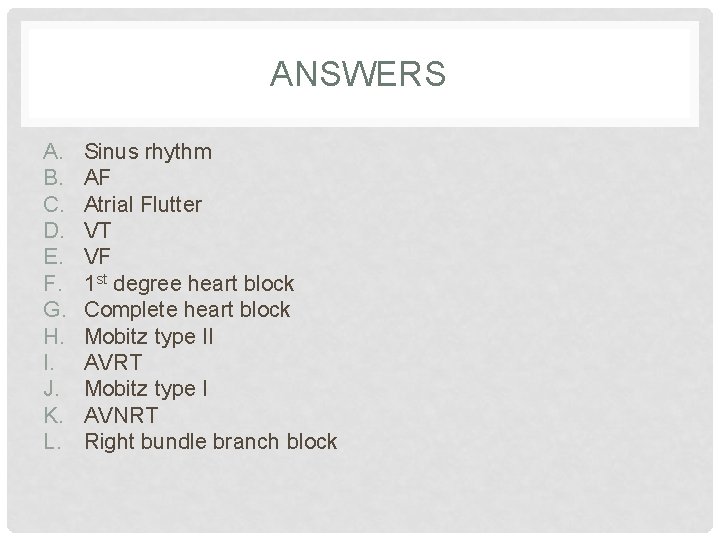
ANSWERS A. B. C. D. E. F. G. H. I. J. K. L. Sinus rhythm AF Atrial Flutter VT VF 1 st degree heart block Complete heart block Mobitz type II AVRT Mobitz type I AVNRT Right bundle branch block
REFERENCES • All images and ECGs borrowed gratefully from google images • Kumar & Clarke: Clinical Medicine 7 th Ed • NICE guidelines: AF (CG 36)
 Haywood ho
Haywood ho Sonja harris haywood md
Sonja harris haywood md Haywood academy staff
Haywood academy staff Labor unions apush
Labor unions apush Figure 11-6 arteries
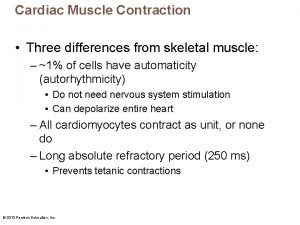
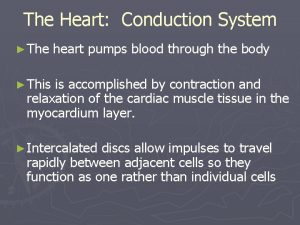
Figure 11-6 arteries Label the components of the conduction system.
Label the components of the conduction system. Factors affecting cardiac output
Factors affecting cardiac output Intrinsic cardiac conduction system
Intrinsic cardiac conduction system Apetm heart sounds
Apetm heart sounds The conduction system
The conduction system The conduction system
The conduction system The conduction system
The conduction system The conduction system
The conduction system The conduction system
The conduction system Conduction system of heart
Conduction system of heart Conduction system of the heart
Conduction system of the heart The conduction system
The conduction system The conduction system
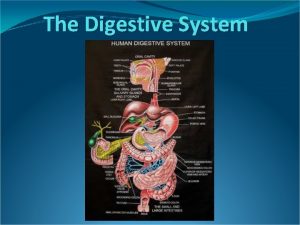
The conduction system Human digestive system introduction
Human digestive system introduction The digestive system introduction
The digestive system introduction Arc system intro
Arc system intro Solar system intro
Solar system intro Danny amato
Danny amato Danny and melinda
Danny and melinda Sofia calltorp
Sofia calltorp Is danny elfman married
Is danny elfman married Eric sun facebook
Eric sun facebook Danny elfman school
Danny elfman school Danny delcambre
Danny delcambre Sullivan search engine
Sullivan search engine Danny brazzale
Danny brazzale Amida raigo triptych
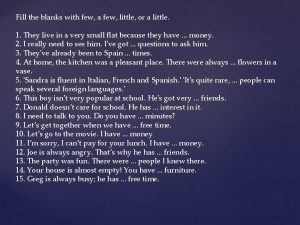
Amida raigo triptych Danny is my best friend. i know _____ so well. *
Danny is my best friend. i know _____ so well. * Danny mather warrington
Danny mather warrington Ma favorite danny defoe
Ma favorite danny defoe Transmitis
Transmitis Danny townsend massachusetts
Danny townsend massachusetts Danny hendler
Danny hendler Danny van noort
Danny van noort Danny panisko
Danny panisko Danny fae
Danny fae Danny summer wife
Danny summer wife The somebody danny santiago
The somebody danny santiago