ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM APRDRG Payment

- Slides: 56
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM APR-DRG Payment System Implementation February 6, 2014 - DRAFT
TABLE OF CONTENTS Section 1 » Overview of DRG Payment Model Section 2 » AHCCCS Guiding Principles and Considerations Section 3 » New DRG System Pricing Formulas Section 5 » DRG Pricing Model Section 6 » Policy Issues Section 7 » Hemophilia and Blood Clotting Factors Section 8 » Documentation and Coding Improvement Page 2
OVERVIEW OF DRG PAYMENT MODELS
OVERVIEW OF DRG MODELS » DRG models generally pay a fixed amount, which is known in advance, on a “per discharge” basis, and based on the patient’s DRG assignment » DRG Patient Classifications Systems, or “Groupers”, assign each patient discharge to a DRG, based on the patient’s diagnoses, surgical procedures performed, age, gender, birth weight and discharge status » Each DRG has a relative weight factor, which recognizes the differences in resource requirements based on patient’s assigned DRG Page 4
OVERVIEW OF DRG MODELS » Payment is generally determined by multiplying a hospital’s “base rate” by the assigned DRG’s relative weight factor » An “outlier” payment provision is typically incorporated to provide additional payments where the base DRG amount is not appropriate – generally cases with extraordinarily high costs » Payment models are also commonly modified to affect payment for specialty services or providers, including behavioral health, rehabilitation, neonatal, pediatric and others Page 5
OVERVIEW OF DRG MODELS » There are two DRG grouper models that are broadly used by public and commercial payers for classifying patients into DRGs › All Patient Refined DRGs (APR-DRGs) › Medicare Severity DRGs (MS-DRGs) » While a number of state Medicaid programs rely on MS-DRGs for DRG payment models, the APR-DRG groper is considered to be a superior model for payments targeted to the Medicaid (i. e. , non-aged) population Page 6
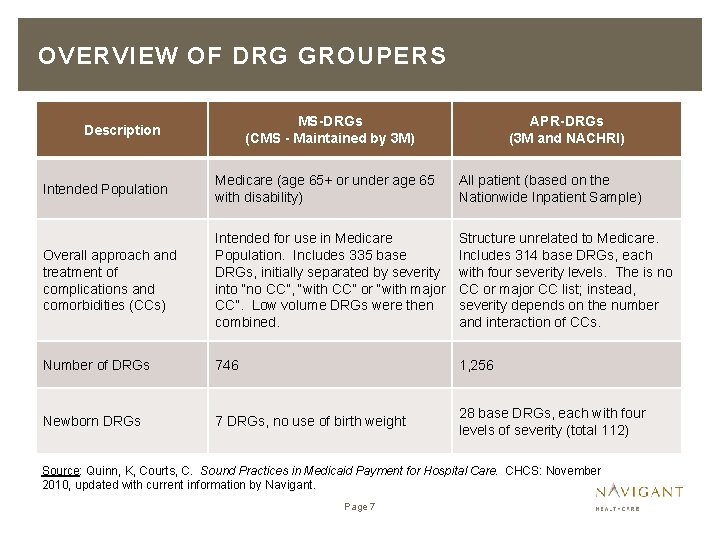
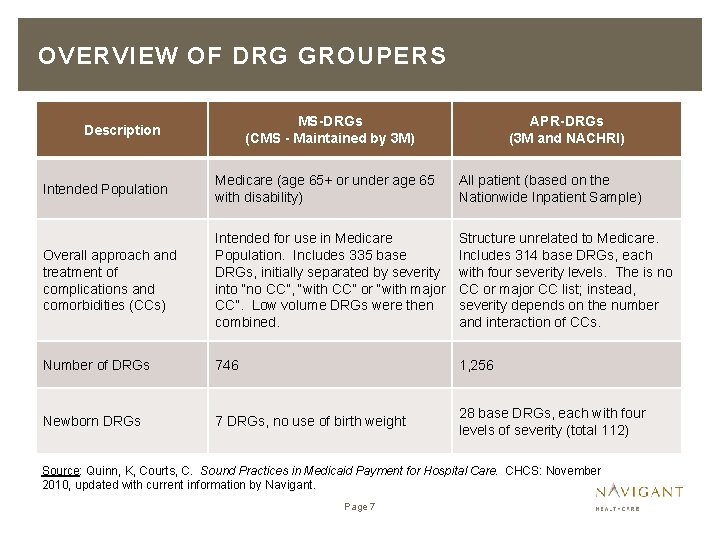
OVERVIEW OF DRG GROUPERS MS-DRGs (CMS - Maintained by 3 M) Description APR-DRGs (3 M and NACHRI) Intended Population Medicare (age 65+ or under age 65 with disability) All patient (based on the Nationwide Inpatient Sample) Overall approach and treatment of complications and comorbidities (CCs) Intended for use in Medicare Population. Includes 335 base DRGs, initially separated by severity into “no CC”, “with CC” or “with major CC”. Low volume DRGs were then combined. Structure unrelated to Medicare. Includes 314 base DRGs, each with four severity levels. The is no CC or major CC list; instead, severity depends on the number and interaction of CCs. Number of DRGs 746 1, 256 Newborn DRGs 7 DRGs, no use of birth weight 28 base DRGs, each with four levels of severity (total 112) Source: Quinn, K, Courts, C. Sound Practices in Medicaid Payment for Hospital Care. CHCS: November 2010, updated with current information by Navigant. Page 7
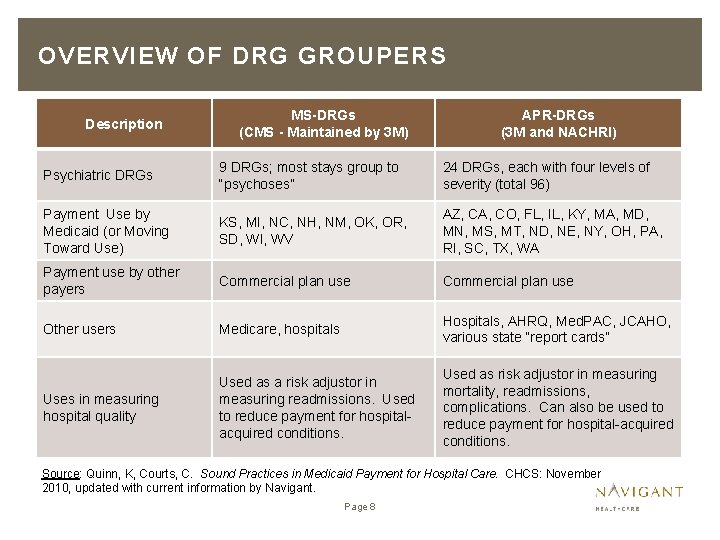
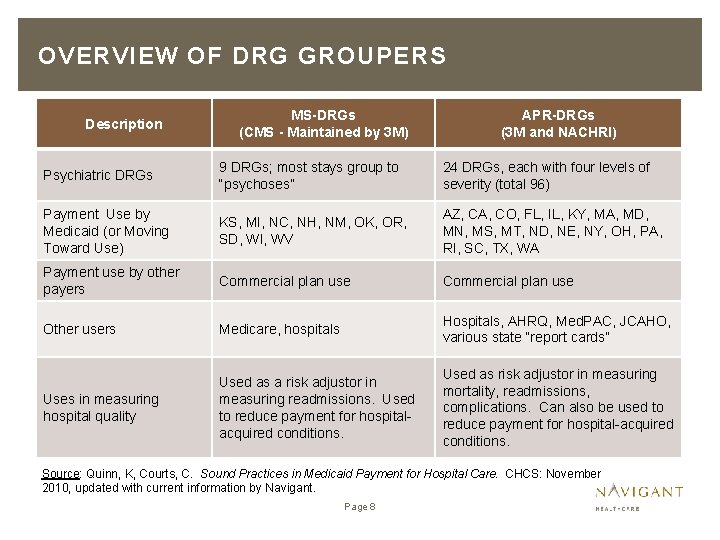
OVERVIEW OF DRG GROUPERS Description MS-DRGs (CMS - Maintained by 3 M) APR-DRGs (3 M and NACHRI) Psychiatric DRGs 9 DRGs; most stays group to “psychoses” 24 DRGs, each with four levels of severity (total 96) Payment Use by Medicaid (or Moving Toward Use) KS, MI, NC, NH, NM, OK, OR, SD, WI, WV AZ, CA, CO, FL, IL, KY, MA, MD, MN, MS, MT, ND, NE, NY, OH, PA, RI, SC, TX, WA Payment use by other payers Commercial plan use Other users Medicare, hospitals Hospitals, AHRQ, Med. PAC, JCAHO, various state “report cards” Uses in measuring hospital quality Used as a risk adjustor in measuring readmissions. Used to reduce payment for hospitalacquired conditions. Used as risk adjustor in measuring mortality, readmissions, complications. Can also be used to reduce payment for hospital-acquired conditions. Source: Quinn, K, Courts, C. Sound Practices in Medicaid Payment for Hospital Care. CHCS: November 2010, updated with current information by Navigant. Page 8
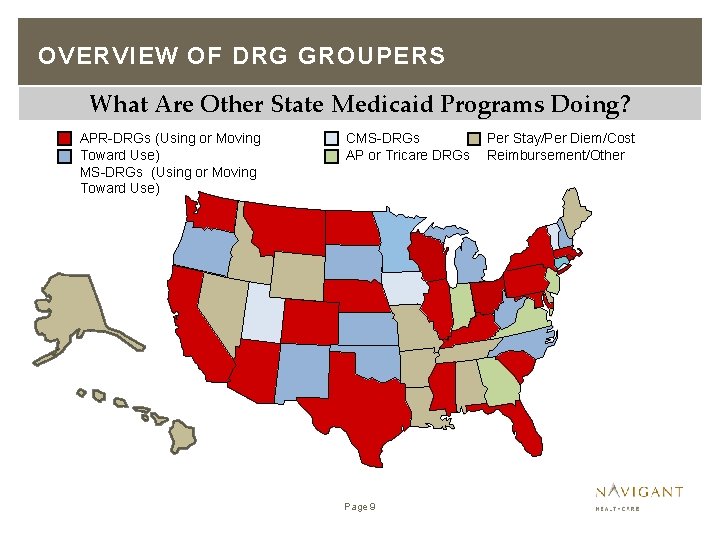
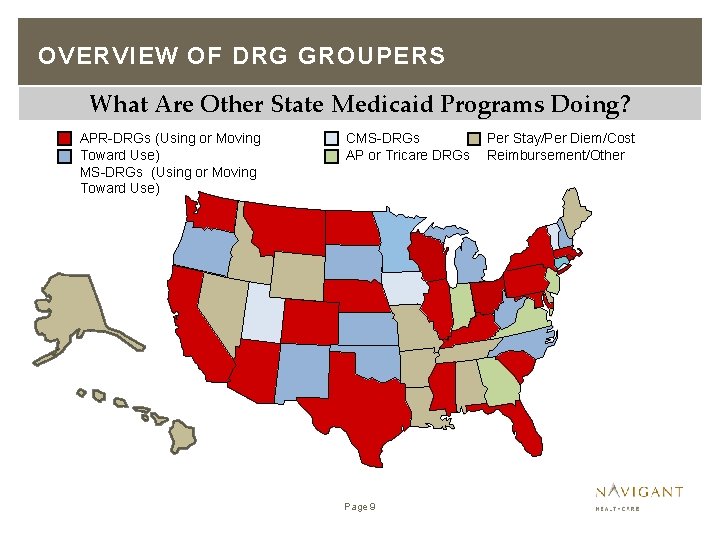
OVERVIEW OF DRG GROUPERS What Are Other State Medicaid Programs Doing? APR-DRGs (Using or Moving Toward Use) MS-DRGs (Using or Moving Toward Use) CMS-DRGs AP or Tricare DRGs Page 9 Per Stay/Per Diem/Cost Reimbursement/Other
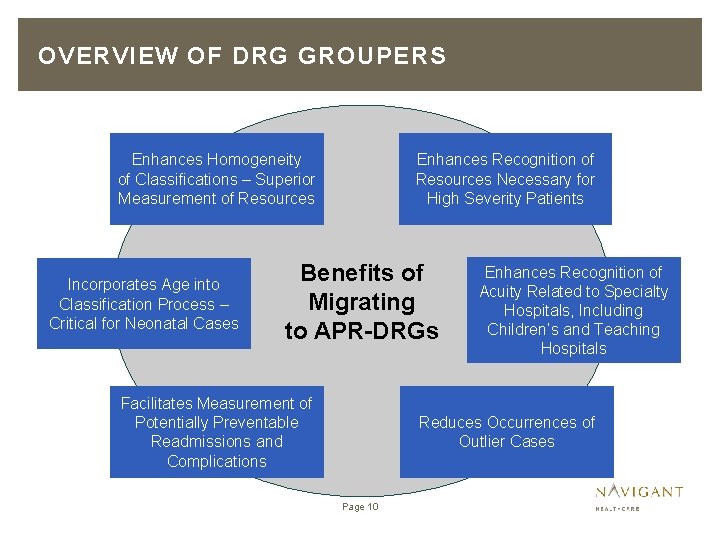
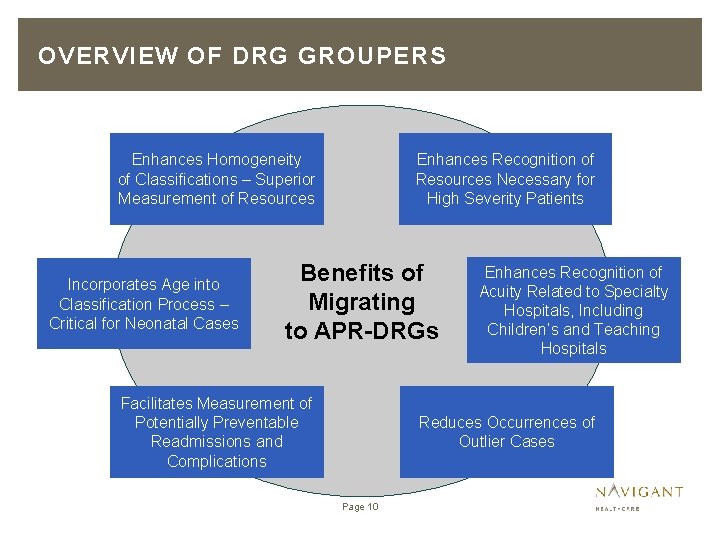
OVERVIEW OF DRG GROUPERS Enhances Homogeneity of Classifications – Superior Measurement of Resources Incorporates Age into Classification Process – Critical for Neonatal Cases Enhances Recognition of Resources Necessary for High Severity Patients Benefits of Migrating to APR-DRGs Facilitates Measurement of Potentially Preventable Readmissions and Complications Enhances Recognition of Acuity Related to Specialty Hospitals, Including Children’s and Teaching Hospitals Reduces Occurrences of Outlier Cases Page 10
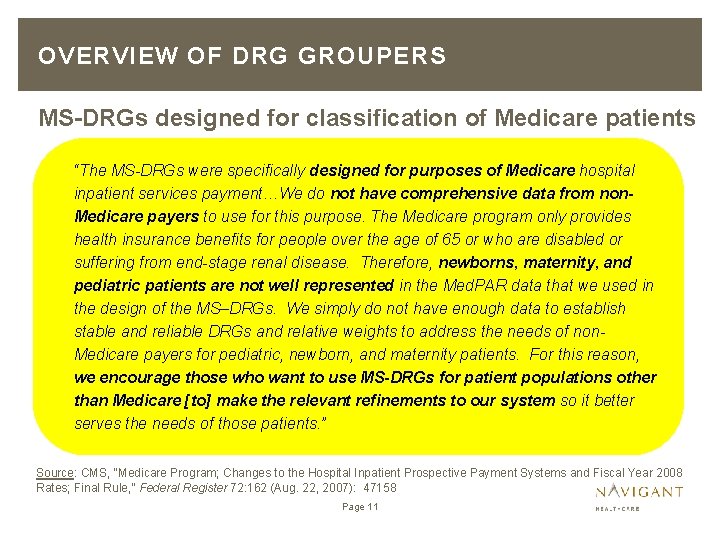
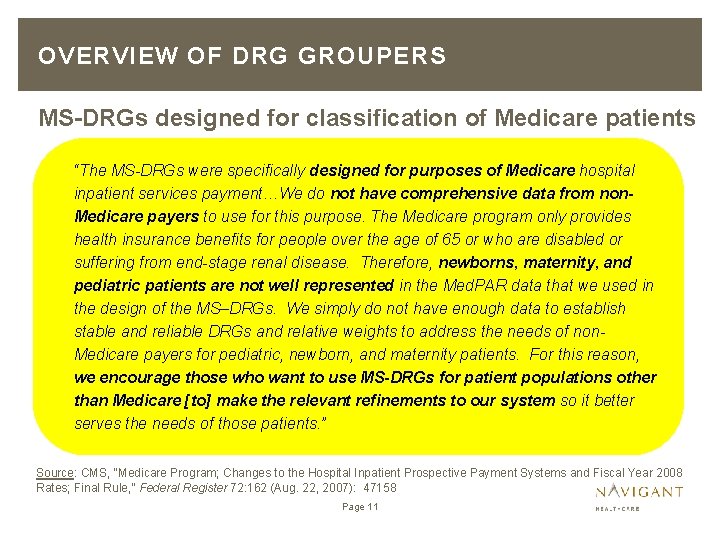
OVERVIEW OF DRG GROUPERS MS-DRGs designed for classification of Medicare patients … “The MS-DRGs were specifically designed for purposes of Medicare hospital inpatient services payment…We do not have comprehensive data from non. Medicare payers to use for this purpose. The Medicare program only provides health insurance benefits for people over the age of 65 or who are disabled or suffering from end-stage renal disease. Therefore, newborns, maternity, and pediatric patients are not well represented in the Med. PAR data that we used in the design of the MS–DRGs. We simply do not have enough data to establish stable and reliable DRGs and relative weights to address the needs of non. Medicare payers for pediatric, newborn, and maternity patients. For this reason, we encourage those who want to use MS-DRGs for patient populations other than Medicare [to] make the relevant refinements to our system so it better serves the needs of those patients. ” Source: CMS, “Medicare Program; Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Year 2008 Rates; Final Rule, ” Federal Register 72: 162 (Aug. 22, 2007): 47158 Page 11
GUIDING PRINCIPLES AND CONSIDERATIONS FOR DESIGN AND IMPLEMENTATION BY AHCCCS
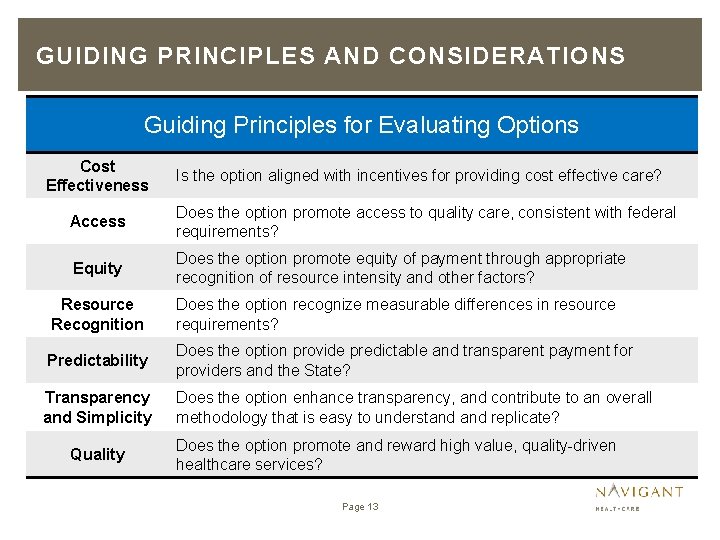
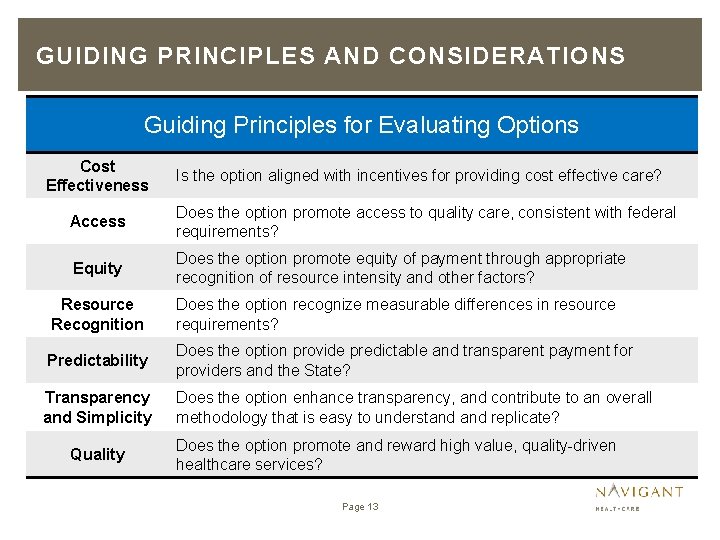
GUIDING PRINCIPLES AND CONSIDERATIONS Guiding Principles for Evaluating Options Cost Effectiveness Is the option aligned with incentives for providing cost effective care? Access Does the option promote access to quality care, consistent with federal requirements? Equity Does the option promote equity of payment through appropriate recognition of resource intensity and other factors? Resource Recognition Does the option recognize measurable differences in resource requirements? Predictability Does the option provide predictable and transparent payment for providers and the State? Transparency and Simplicity Does the option enhance transparency, and contribute to an overall methodology that is easy to understand replicate? Quality Does the option promote and reward high value, quality-driven healthcare services? Page 13
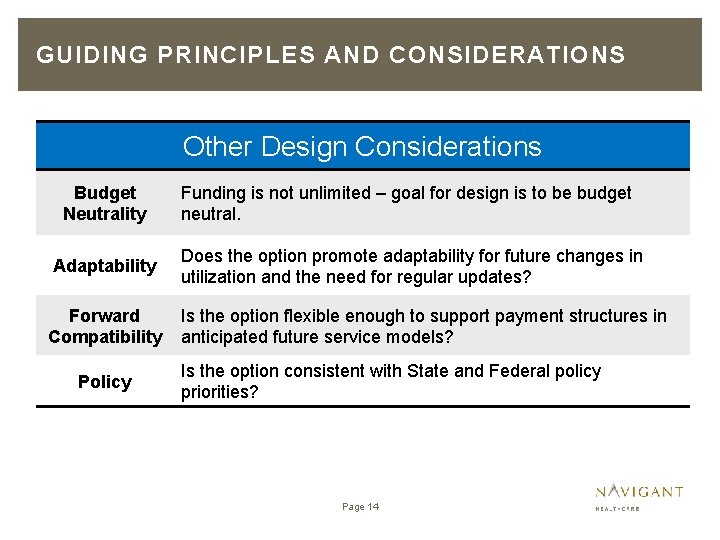
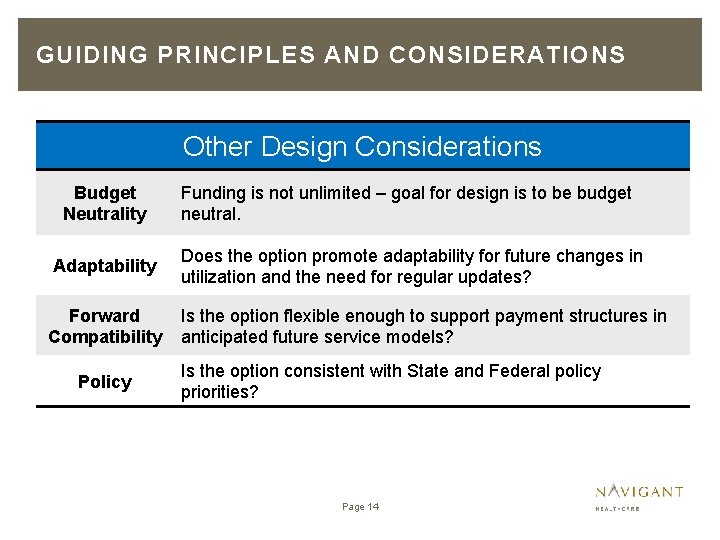
GUIDING PRINCIPLES AND CONSIDERATIONS Other Design Considerations Budget Neutrality Adaptability Forward Compatibility Policy Funding is not unlimited – goal for design is to be budget neutral. Does the option promote adaptability for future changes in utilization and the need for regular updates? Is the option flexible enough to support payment structures in anticipated future service models? Is the option consistent with State and Federal policy priorities? Page 14
NEW DRG SYSTEM PRICING FORMULAS
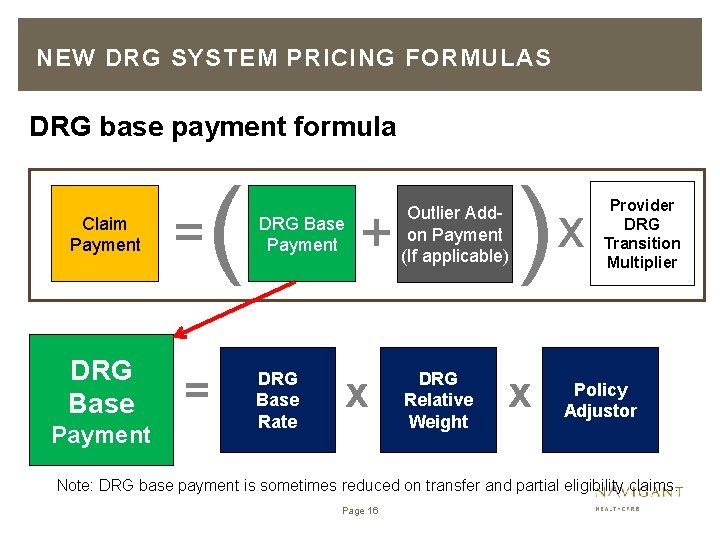
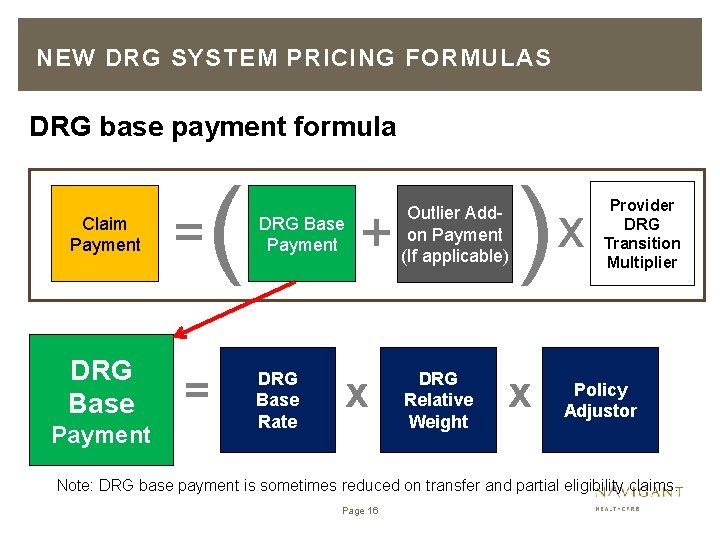
NEW DRG SYSTEM PRICING FORMULAS DRG base payment formula Claim Payment DRG Base Payment = ( = DRG Base Payment DRG Base Rate + x Outlier Addon Payment (If applicable) DRG Relative Weight ) x x Provider DRG Transition Multiplier Policy Adjustor Note: DRG base payment is sometimes reduced on transfer and partial eligibility claims. Page 16
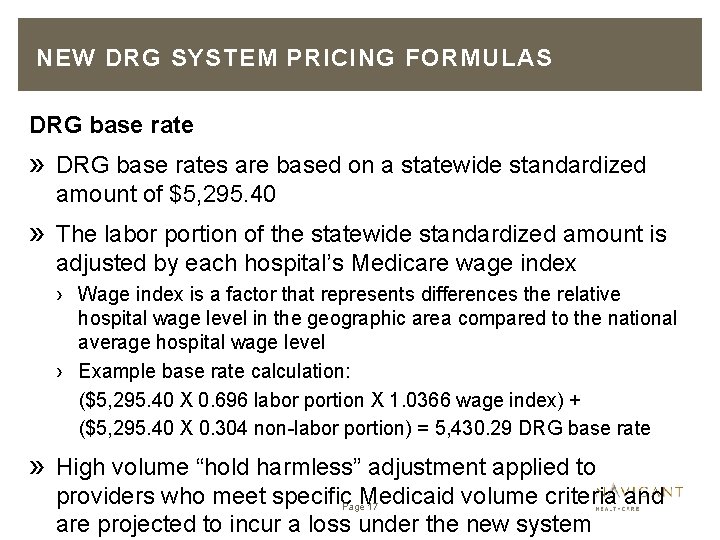
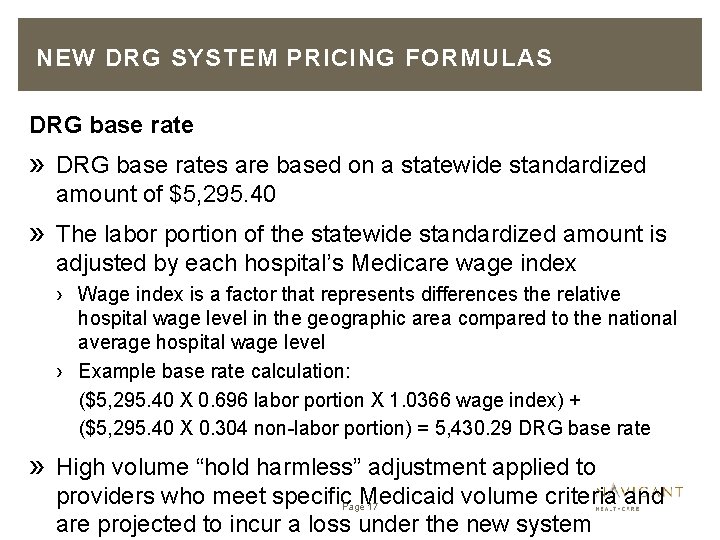
NEW DRG SYSTEM PRICING FORMULAS DRG base rate » DRG base rates are based on a statewide standardized amount of $5, 295. 40 » The labor portion of the statewide standardized amount is adjusted by each hospital’s Medicare wage index › Wage index is a factor that represents differences the relative hospital wage level in the geographic area compared to the national average hospital wage level › Example base rate calculation: ($5, 295. 40 X 0. 696 labor portion X 1. 0366 wage index) + ($5, 295. 40 X 0. 304 non-labor portion) = 5, 430. 29 DRG base rate » High volume “hold harmless” adjustment applied to providers who meet specific. Page. Medicaid volume criteria and 17 are projected to incur a loss under the new system
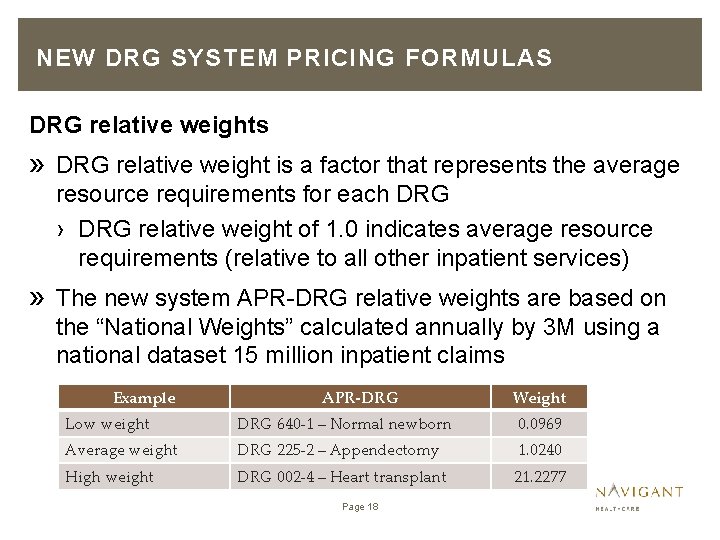
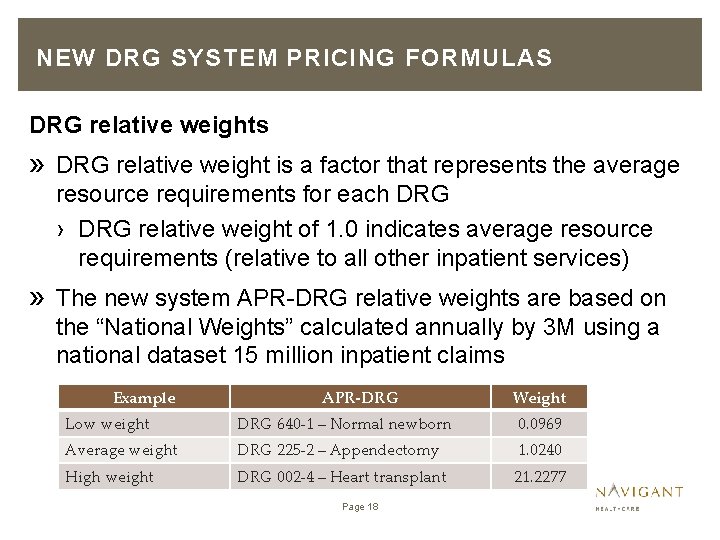
NEW DRG SYSTEM PRICING FORMULAS DRG relative weights » DRG relative weight is a factor that represents the average resource requirements for each DRG › DRG relative weight of 1. 0 indicates average resource requirements (relative to all other inpatient services) » The new system APR-DRG relative weights are based on the “National Weights” calculated annually by 3 M using a national dataset 15 million inpatient claims Example APR-DRG Weight Low weight DRG 640 -1 – Normal newborn 0. 0969 Average weight DRG 225 -2 – Appendectomy 1. 0240 High weight DRG 002 -4 – Heart transplant 21. 2277 Page 18
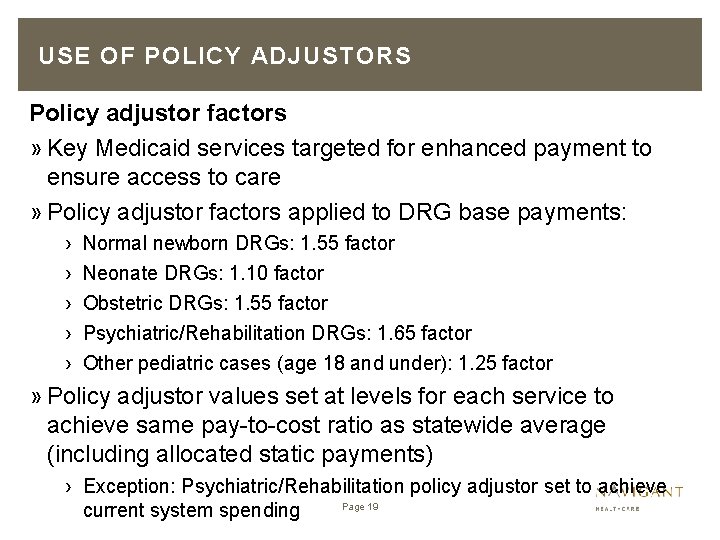
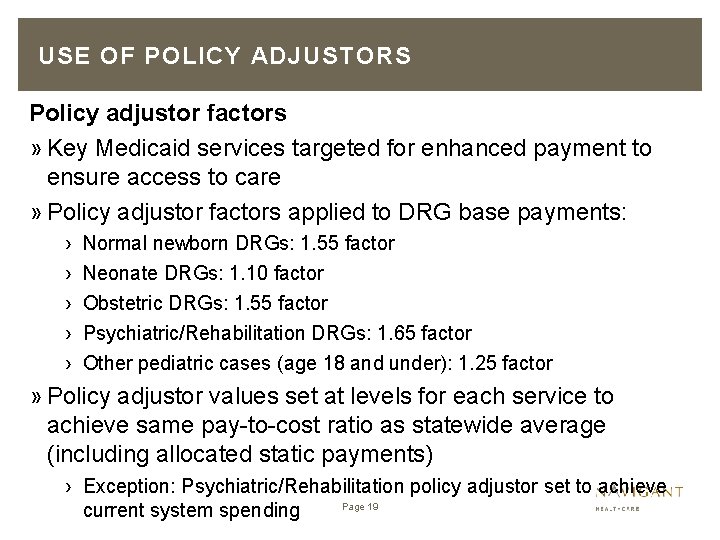
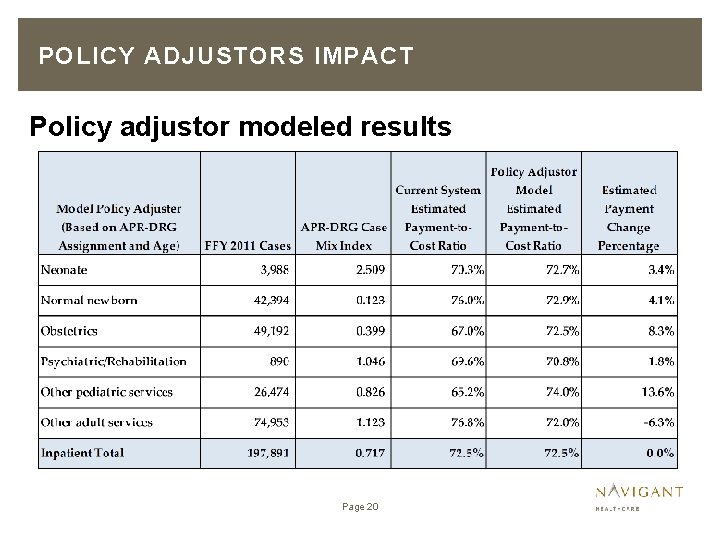
USE OF POLICY ADJUSTORS Policy adjustor factors » Key Medicaid services targeted for enhanced payment to ensure access to care » Policy adjustor factors applied to DRG base payments: › › › Normal newborn DRGs: 1. 55 factor Neonate DRGs: 1. 10 factor Obstetric DRGs: 1. 55 factor Psychiatric/Rehabilitation DRGs: 1. 65 factor Other pediatric cases (age 18 and under): 1. 25 factor » Policy adjustor values set at levels for each service to achieve same pay-to-cost ratio as statewide average (including allocated static payments) › Exception: Psychiatric/Rehabilitation policy adjustor set to achieve Page 19 current system spending
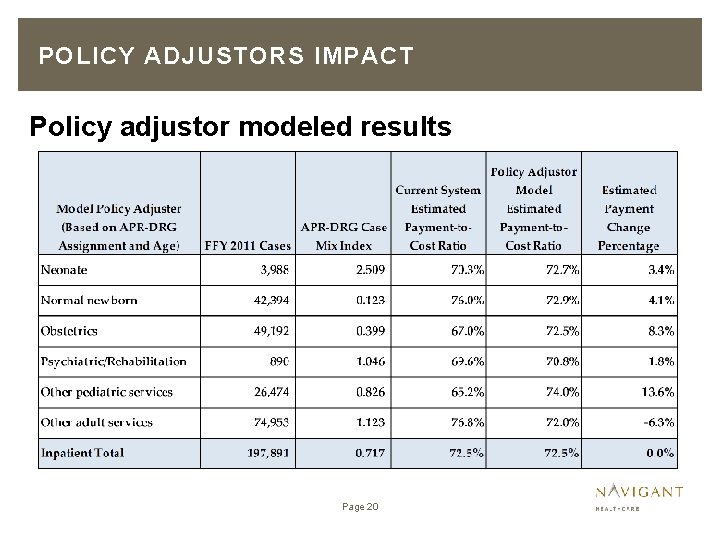
POLICY ADJUSTORS IMPACT Policy adjustor modeled results Page 20
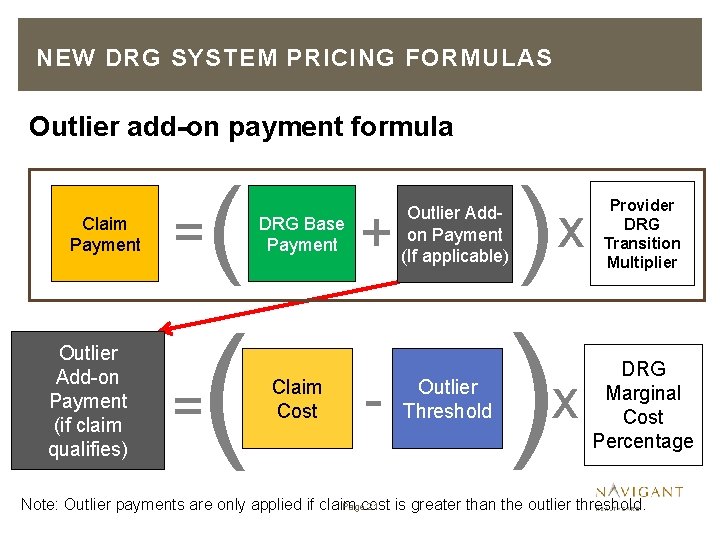
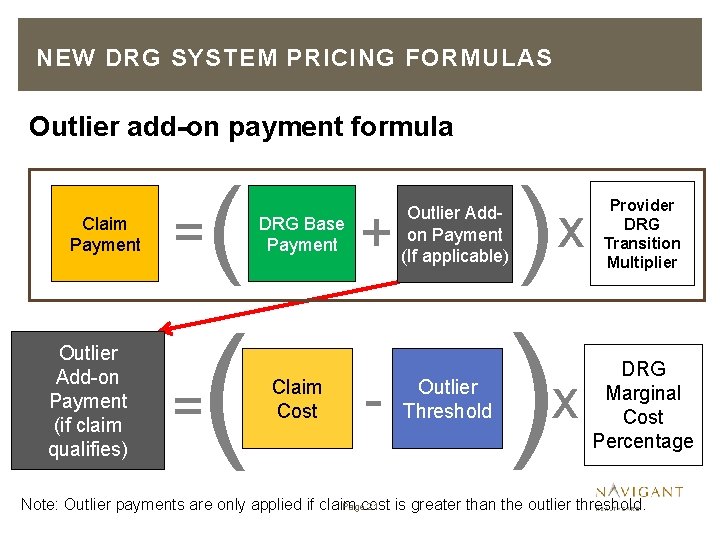
NEW DRG SYSTEM PRICING FORMULAS Outlier add-on payment formula Claim Payment Outlier Add-on Payment (if claim qualifies) = ( ( = DRG Base Payment Claim Cost + - Outlier Addon Payment (If applicable) Outlier Threshold ) ) x x Provider DRG Transition Multiplier DRG Marginal Cost Percentage Pagecost 21 Note: Outlier payments are only applied if claim is greater than the outlier threshold.
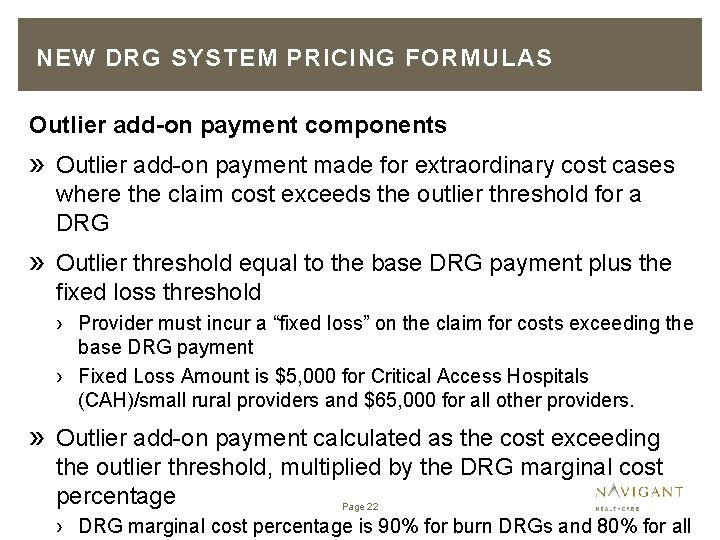
NEW DRG SYSTEM PRICING FORMULAS Outlier add-on payment components » Outlier add-on payment made for extraordinary cost cases where the claim cost exceeds the outlier threshold for a DRG » Outlier threshold equal to the base DRG payment plus the fixed loss threshold › Provider must incur a “fixed loss” on the claim for costs exceeding the base DRG payment › Fixed Loss Amount is $5, 000 for Critical Access Hospitals (CAH)/small rural providers and $65, 000 for all other providers. » Outlier add-on payment calculated as the cost exceeding the outlier threshold, multiplied by the DRG marginal cost percentage Page 22 › DRG marginal cost percentage is 90% for burn DRGs and 80% for all
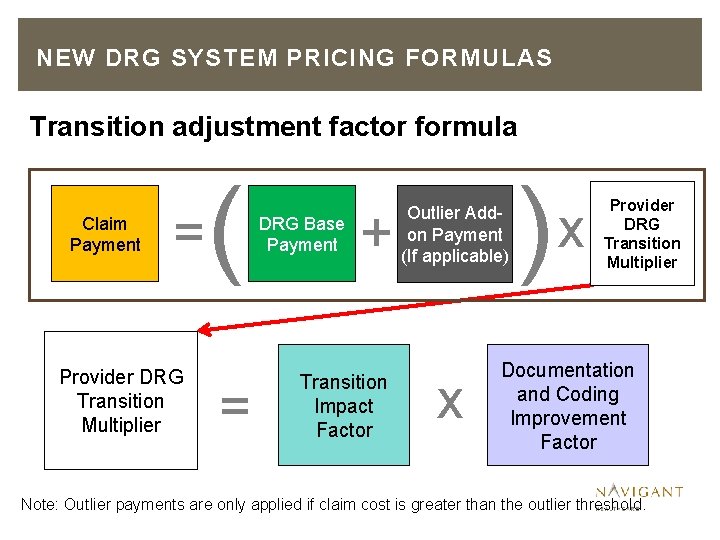
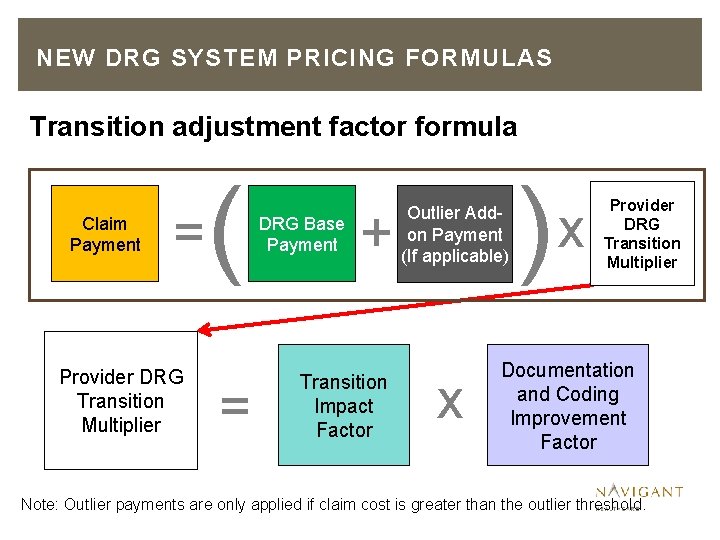
NEW DRG SYSTEM PRICING FORMULAS Transition adjustment factor formula Claim Payment = Provider DRG Transition Multiplier ( = DRG Base Payment + Transition Impact Factor Outlier Addon Payment (If applicable) x Provider DRG Transition Multiplier Documentation and Coding Improvement Factor Note: Outlier payments are only applied if claim cost is greater than the outlier threshold.
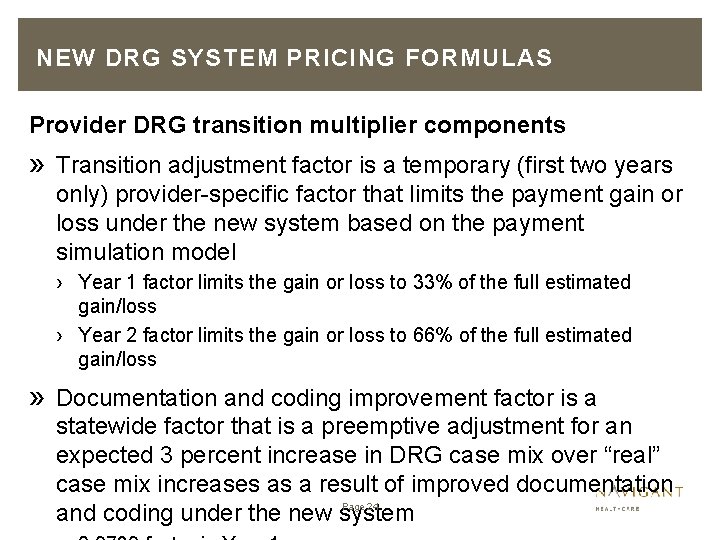
NEW DRG SYSTEM PRICING FORMULAS Provider DRG transition multiplier components » Transition adjustment factor is a temporary (first two years only) provider-specific factor that limits the payment gain or loss under the new system based on the payment simulation model › Year 1 factor limits the gain or loss to 33% of the full estimated gain/loss › Year 2 factor limits the gain or loss to 66% of the full estimated gain/loss » Documentation and coding improvement factor is a statewide factor that is a preemptive adjustment for an expected 3 percent increase in DRG case mix over “real” case mix increases as a result of improved documentation Page 24 and coding under the new system
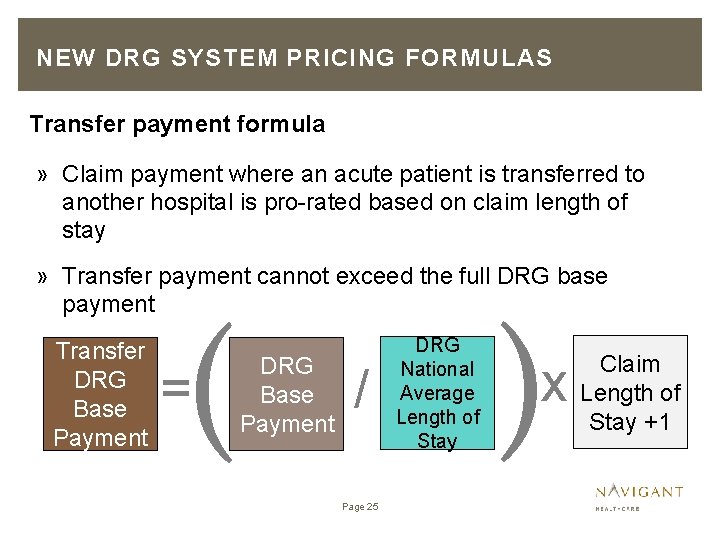
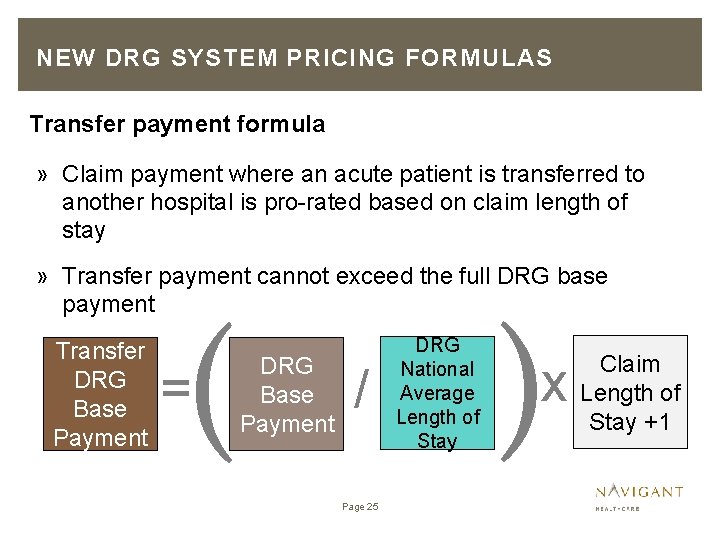
NEW DRG SYSTEM PRICING FORMULAS Transfer payment formula » Claim payment where an acute patient is transferred to another hospital is pro-rated based on claim length of stay » Transfer payment cannot exceed the full DRG base payment Transfer DRG Base Payment ( = DRG Base Payment / Page 25 DRG National Average Length of Stay ) x Claim Length of Stay +1
AHCCCS DRG PRICING MODEL
AHCCCS DRG PRICING MODEL New system DRG payment simulation » DRG pricing model simulates payments under the new DRG system, including the DRG base payment, outlier payment and policy adjusters, using historical claims data » Model used to establish what the DRG base rates can be given all other payment methodology parameters, while maintaining budget neutrality » Model also compares simulated payments under the new system to payments under the current system and estimated provider costs, at the following levels: › Provider level › Service line level › System aggregate Page 27
AHCCCS DRG PRICING MODEL Standardized amount determination » DRG pricing model is based on FFY 2011 Arizona Medicaid FFS claims and managed care encounter data and Medicare cost report data for in-state providers and critical out-of-state providers » Funding pool for determination of budget neutrality is based on FFY 2011 model claim/encounter total reported payments, with reductions applied to reflect payment rate/methodology changes since 2011 » DRG base rates “solved for” to be budget neutral to current system payments › DRG base rates result in aggregate simulated DRG Page 28 payments that are approximately equal to FFY 2011
POLICY ISSUES
POLICY ISSUES – ENROLLMENT CHANGE DURING HOSPITAL STAY » Recipient may change payers during a single hospital stay, while maintaining Medicaid eligibility throughout entire stay » This may occur under a variety of scenarios including › Enrollment change from fee-for-service to managed care plan › Enrollment change from managed care plan to fee-for-service › Enrollment change between managed care plans within the same program › Enrollment change between managed care plans in different programs, for example moving from an Acute MCO to the Arizona Long Term Care System (ALTCS) » Services paid via DRG method will be paid by the payer to which the recipient is enrolled at the date of discharge » Providers to submit a claim to the appropriate payer Page 30
POLICY ISSUES – MEDICARE PART A BENEFITS EXHAUSTED » In the event recipient exhausts Medicare Part A benefits during a single hospital stay, providers must submit a second claim for the Medicaid covered portion of the stay » A full DRG payment will be paid for the Medicaid claim Page 31
POLICY ISSUES – ADMINISTRATIVE DAYS » AHCCCS may offer reimbursement for Medicaid recipients occupying a bed while not in need of care › These days are referred to as administrative days » Administrative days must be prior authorized by AHCCCS » Administrative days will be reimbursed using a negotiated per diem rate » Reimbursement for administrative days will be separate from DRG reimbursement for acute care services and provider must bill such days on a separate claim Page 32
POLICY ISSUES – INTERIM CLAIMS » A recipient may be in the hospital for an extended period of time » If patient stay exceeds a 29 day period, hospitals may submit interim claims related to the patient stay in increments of 30 days » Interim claims will be reimbursed under a per diem rate of $500 per day » Hospitals must submit a final claim associated with the patient stay upon the patient’s discharge – all previously submitted interim claims will be voided and final claim will be paid Page 33
POLICY ISSUES – RECIPIENT GAINS ELIGIBILITY AFTER ADMISSION » A recipient may be ineligible for Medicaid upon admission, however, may become eligible for Medicaid during the hospital stay » Providers will be reimbursed for the Medicaid covered days of the hospital stay › The DRG payment designed to cover the full hospital will be prorated based on the number of Medicaid covered days › This prorated payment to providers will not exceed the full DRG payment Page 34 » Only claims with dates of service where the recipient is an
POLICY ISSUES – RECIPIENT LOSES ELIGIBILITY PRIOR TO DISCHARGE » A recipient may be eligible for Medicaid upon admission, however, may lose eligibility for Medicaid prior to being discharged » Providers will be reimbursed for the Medicaid covered days of the hospital stay › The DRG payment designed to cover the full hospital will be prorated based on the number of Medicaid covered days › This prorated payment to providers will not exceed the full DRG payment Page 35 » Only claims with dates of service where the recipient is an
POLICY ISSUES – SAME DAY ADMISSION AND DISCHARGE » A recipient may be admitted and discharged on the same day » Inpatient claims with a date of admission matching the date of the discharge will be paid under the reimbursement policy that is currently in place for AHCCCS, with one exception. » Maternity and nursery claims will be reimbursed under the AHCCCS Outpatient Hospital Fees Schedule Methodology (OPFS) Page 36
POLICY ISSUES – HEALTH CARE ACQUIRED CONDITIONS (HCAC’S) » For claims paid via DRG methodology, AHCCCS will utilize DRG assignment to determine payment reductions in cases of health care acquired conditions » A present on admission (POA) indicator will continue to be required on all inpatient claims as the HCAC payment reduction policy only applies if the HCAC condition(s) were acquired in the hospital after admission » Under the DRG methodology, two DRGs will be assigned to every claim (“pre-HCAC” and “post-HCAC”). The DRG will the lower relative weight will be used to price the claim. Page 37
POLICY ISSUES – READMISSION POLICY » A recipient may be readmitted to a hospital after receiving a service or treatment » For claims paid under DRG methodology, the Administration will identify certain readmission cases and conduct a medical review to determine if the readmission was preventable by the hospital » The following criteria will prompt a medical review › Recipient is readmitted to the same hospital within 72 hours, and › The base DRG assignment on the readmission claim must match the base DRG assignment on the initial Page 38 claim, and
POLICY ISSUES – READMISSION POLICY » Claims which meet the criteria described, will be pended for medical review » The payment associated with the readmission claim will be held until the completion of the medical review process » If the claim is determined to have been preventable by the hospital, the payment associated with the readmission claim will be disallowed » Alternatively, if upon the medical review it is determined the hospital would not have been able to prevent the readmission, the claim will be paid under DRG methodology Page 39
PRICING EXAMPLES
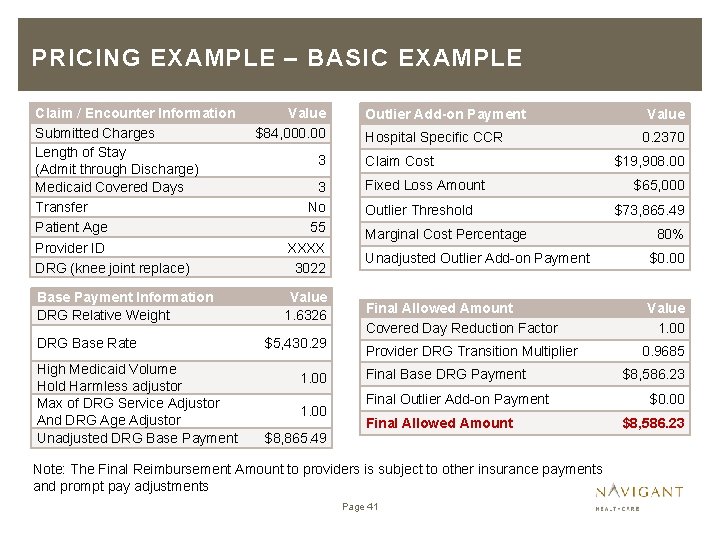
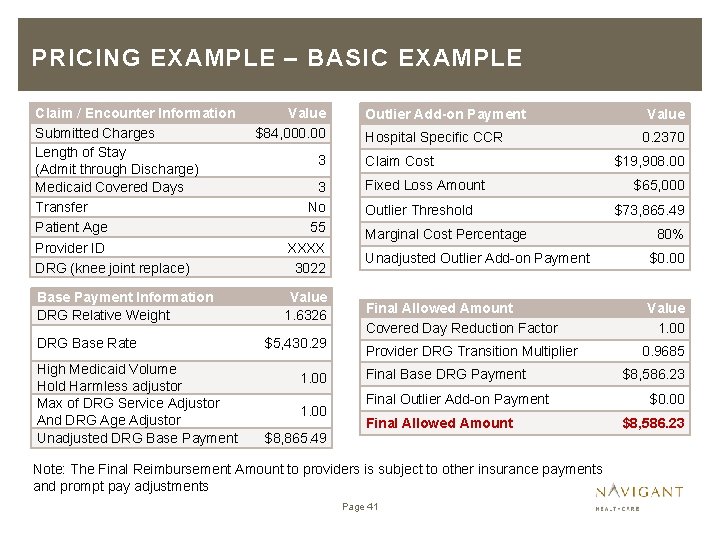
PRICING EXAMPLE – BASIC EXAMPLE Claim / Encounter Information Submitted Charges Length of Stay (Admit through Discharge) Medicaid Covered Days Transfer Patient Age Provider ID DRG (knee joint replace) Base Payment Information DRG Relative Weight DRG Base Rate High Medicaid Volume Hold Harmless adjustor Max of DRG Service Adjustor And DRG Age Adjustor Unadjusted DRG Base Payment Value $84, 000. 00 3 3 No 55 XXXX 3022 Value 1. 6326 $5, 430. 29 1. 00 $8, 865. 49 Outlier Add-on Payment Hospital Specific CCR Claim Cost Fixed Loss Amount Outlier Threshold Marginal Cost Percentage Value 0. 2370 $19, 908. 00 $65, 000 $73, 865. 49 80% Unadjusted Outlier Add-on Payment $0. 00 Final Allowed Amount Covered Day Reduction Factor Value 1. 00 Provider DRG Transition Multiplier Final Base DRG Payment Final Outlier Add-on Payment Final Allowed Amount Note: The Final Reimbursement Amount to providers is subject to other insurance payments and prompt pay adjustments Page 41 0. 9685 $8, 586. 23 $0. 00 $8, 586. 23
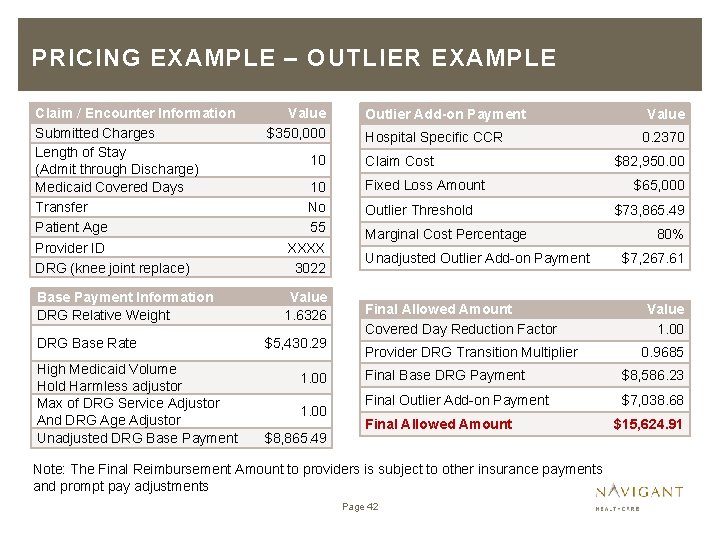
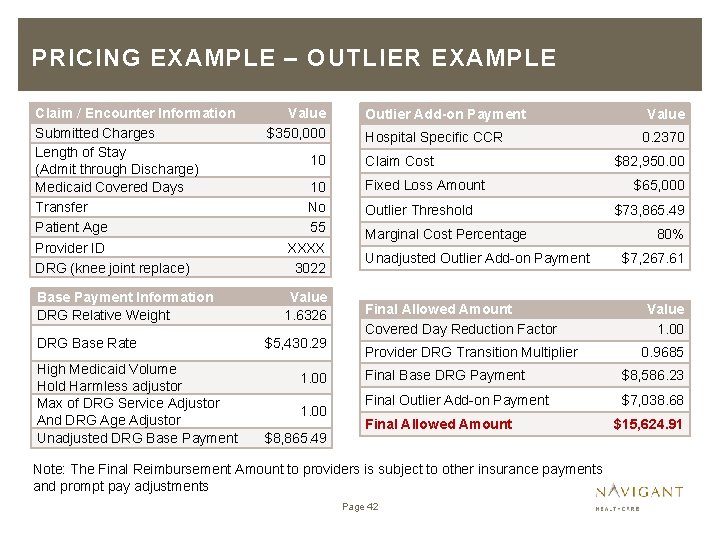
PRICING EXAMPLE – OUTLIER EXAMPLE Claim / Encounter Information Submitted Charges Length of Stay (Admit through Discharge) Medicaid Covered Days Transfer Patient Age Provider ID DRG (knee joint replace) Base Payment Information DRG Relative Weight DRG Base Rate High Medicaid Volume Hold Harmless adjustor Max of DRG Service Adjustor And DRG Age Adjustor Unadjusted DRG Base Payment Value $350, 000 10 10 No 55 XXXX 3022 Value 1. 6326 $5, 430. 29 1. 00 $8, 865. 49 Outlier Add-on Payment Hospital Specific CCR Claim Cost Fixed Loss Amount Outlier Threshold Marginal Cost Percentage Unadjusted Outlier Add-on Payment Final Allowed Amount Covered Day Reduction Factor Provider DRG Transition Multiplier Value 0. 2370 $82, 950. 00 $65, 000 $73, 865. 49 80% $7, 267. 61 Value 1. 00 0. 9685 Final Base DRG Payment $8, 586. 23 Final Outlier Add-on Payment $7, 038. 68 Final Allowed Amount Note: The Final Reimbursement Amount to providers is subject to other insurance payments and prompt pay adjustments Page 42 $15, 624. 91
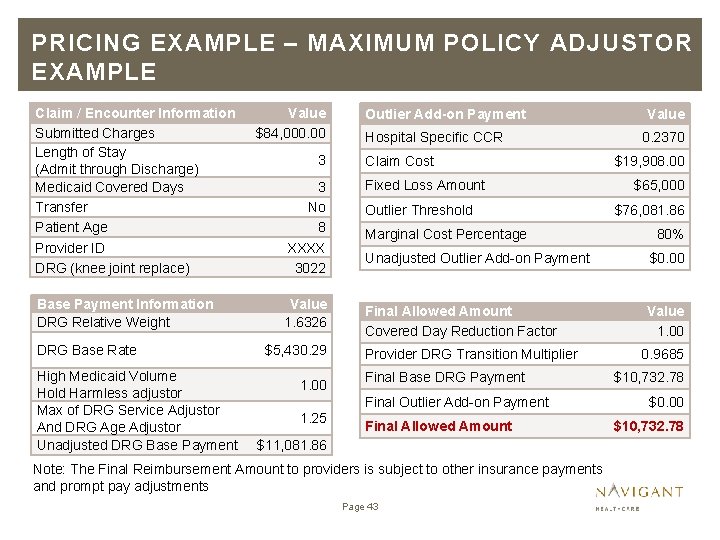
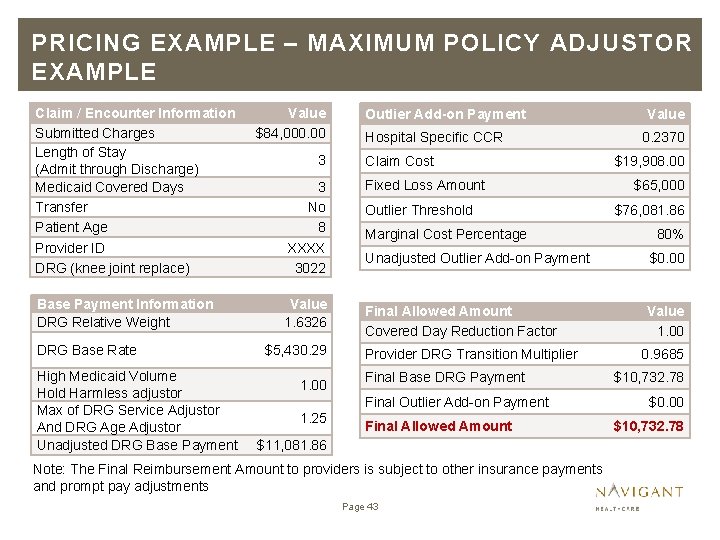
PRICING EXAMPLE – MAXIMUM POLICY ADJUSTOR EXAMPLE Claim / Encounter Information Submitted Charges Length of Stay (Admit through Discharge) Medicaid Covered Days Transfer Patient Age Provider ID DRG (knee joint replace) Base Payment Information DRG Relative Weight DRG Base Rate High Medicaid Volume Hold Harmless adjustor Max of DRG Service Adjustor And DRG Age Adjustor Unadjusted DRG Base Payment Value $84, 000. 00 3 3 No 8 XXXX 3022 Value 1. 6326 $5, 430. 29 1. 00 Outlier Add-on Payment Hospital Specific CCR Claim Cost Fixed Loss Amount Outlier Threshold Marginal Cost Percentage 0. 2370 $19, 908. 00 $65, 000 $76, 081. 86 80% Unadjusted Outlier Add-on Payment $0. 00 Final Allowed Amount Covered Day Reduction Factor Value 1. 00 Provider DRG Transition Multiplier Final Base DRG Payment Final Outlier Add-on Payment 1. 25 Value Final Allowed Amount $11, 081. 86 Note: The Final Reimbursement Amount to providers is subject to other insurance payments and prompt pay adjustments Page 43 0. 9685 $10, 732. 78 $0. 00 $10, 732. 78
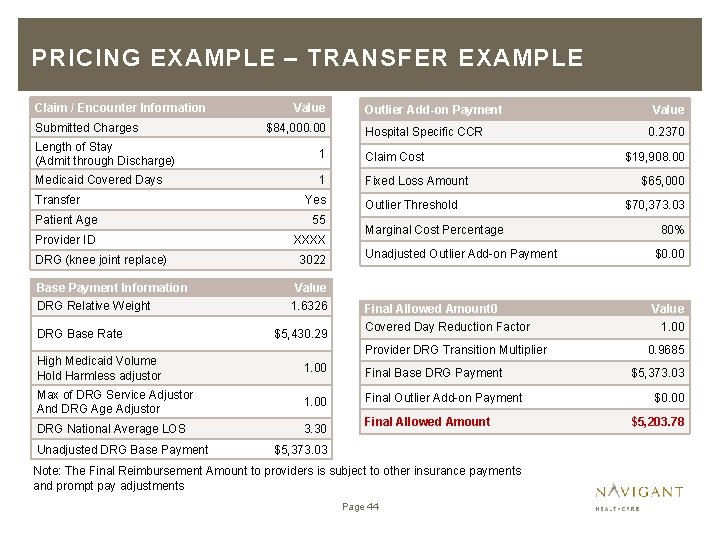
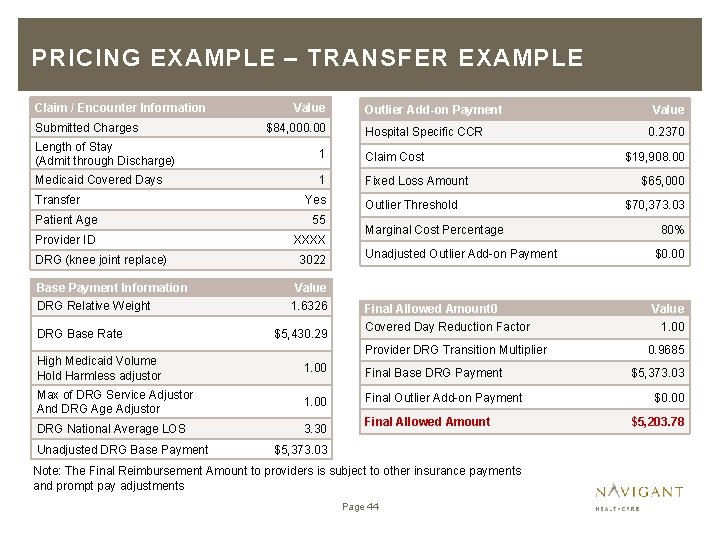
PRICING EXAMPLE – TRANSFER EXAMPLE Claim / Encounter Information Submitted Charges Value $84, 000. 00 Outlier Add-on Payment Hospital Specific CCR Length of Stay (Admit through Discharge) 1 Claim Cost Medicaid Covered Days 1 Fixed Loss Amount Transfer Yes Patient Age 55 Provider ID XXXX DRG (knee joint replace) Base Payment Information DRG Relative Weight DRG Base Rate 3022 Outlier Threshold Marginal Cost Percentage 0. 2370 $19, 908. 00 $65, 000 $70, 373. 03 80% Unadjusted Outlier Add-on Payment $0. 00 Final Allowed Amount 0 Value 1. 6326 $5, 430. 29 Covered Day Reduction Factor Provider DRG Transition Multiplier High Medicaid Volume Hold Harmless adjustor 1. 00 Final Base DRG Payment Max of DRG Service Adjustor And DRG Age Adjustor 1. 00 Final Outlier Add-on Payment DRG National Average LOS 3. 30 Unadjusted DRG Base Payment Value Final Allowed Amount $5, 373. 03 Note: The Final Reimbursement Amount to providers is subject to other insurance payments and prompt pay adjustments Page 44 1. 00 0. 9685 $5, 373. 03 $0. 00 $5, 203. 78
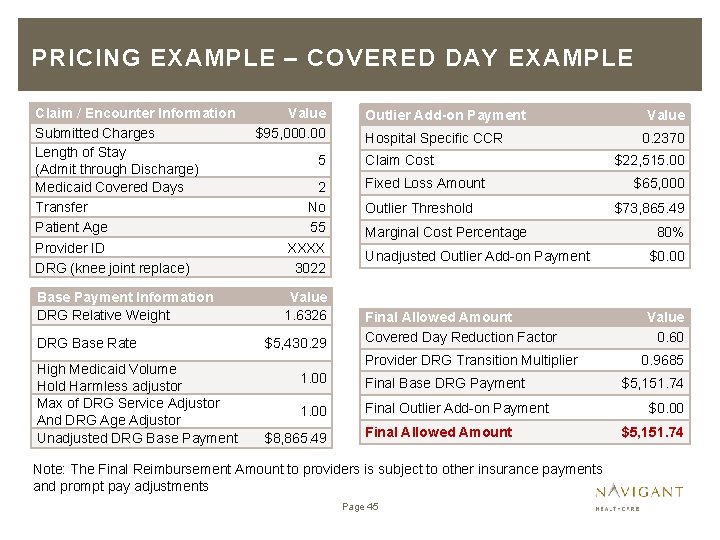
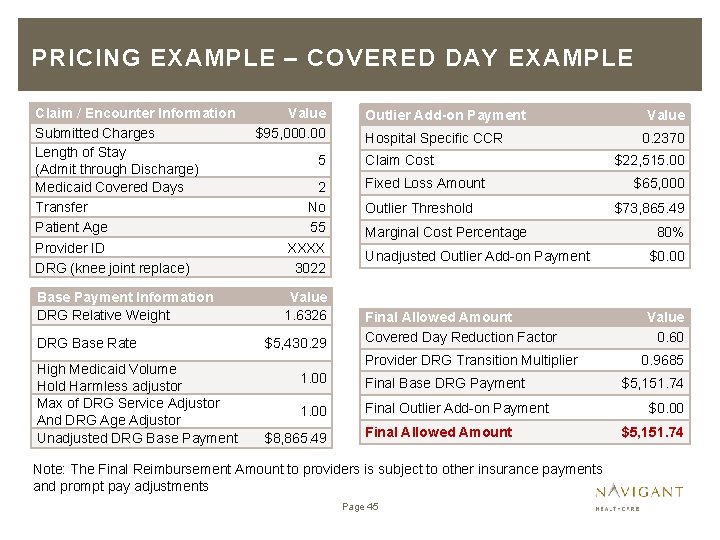
PRICING EXAMPLE – COVERED DAY EXAMPLE Claim / Encounter Information Submitted Charges Length of Stay (Admit through Discharge) Medicaid Covered Days Transfer Patient Age Provider ID DRG (knee joint replace) Base Payment Information DRG Relative Weight DRG Base Rate High Medicaid Volume Hold Harmless adjustor Max of DRG Service Adjustor And DRG Age Adjustor Unadjusted DRG Base Payment Value $95, 000. 00 5 2 No 55 XXXX 3022 Value 1. 6326 $5, 430. 29 Outlier Add-on Payment Hospital Specific CCR Claim Cost Fixed Loss Amount Outlier Threshold Marginal Cost Percentage 0. 2370 $22, 515. 00 $65, 000 $73, 865. 49 80% Unadjusted Outlier Add-on Payment $0. 00 Final Allowed Amount Covered Day Reduction Factor Value 0. 60 Provider DRG Transition Multiplier 1. 00 Final Base DRG Payment 1. 00 Final Outlier Add-on Payment $8, 865. 49 Value Final Allowed Amount Note: The Final Reimbursement Amount to providers is subject to other insurance payments and prompt pay adjustments Page 45 0. 9685 $5, 151. 74 $0. 00 $5, 151. 74
PRICING EXAMPLE – REASONS FOR COVERED DAYS ADJUSTMENT » Recipient is enrolled in the Federal Emergency Services Program (FES) » Recipient gains Medicaid eligibility after admission into the hospital » Recipient loses Medicaid eligibility after admission and before discharge
PRICING EXAMPLE – FINAL REIMBURSEMENT AMOUNT » The Final Reimbursement Amount will be calculated as: » Final Reimbursement Amount = Final Allowed Amount - Other Insurance Payment + / - Prompt Pay Adjustment Note: The current prompt pay policy (slow pay penalties and quick pay discounts) will continue to apply.
DOCUMENTATION AND CODING IMPROVEMENT
DOCUMENTATION AND CODING IMPROVEMENT The Need for a Documentation and Coding Adjustment: » » » » Documentation and Coding Improvement (DCI) is necessary, and as such are expected to be made by providers as an appropriate response to the coding requirements under the APR-DRG model Because the same level of coding rigor was not required for payment purposes under the legacy per diem model, AHCCCS expects that case mix will increase as a result of DCI coding once the system is implemented – beyond actual increases in acuity To maintain budget neutrality, it will be necessary to incorporate an adjustment to offset increases in case mix after implementation AHCCCS expects that actual. Page payments, in the aggregate, will 49 be greater than simulated amounts, and as such, resulting
DOCUMENTATION AND CODING IMPROVEMENT Preemptive adjustment » Up-front 3 percent adjustment for expected Documentation and Coding Improvement (DCI) › Simulate a 3% casemix increase and determine an adjustment factor (“DCI Factor”) that would be necessary to maintain budget neutrality › Claim allowed amounts (including the base DRG payment, outlier payment or transfer payment) will be reduced by the DCI factor › With a 3% casemix increase, the DCI factor is 0. 974 Page 50
DOCUMENTATION AND CODING IMPROVEMENT DCI measurement » Periodically (and based on the availability and completeness of data) AHCCCS will measure actual increases or decreases in case mix attributable to DCI – or “Casemix Differential” » Based on measurement › AHCCCS intends to set the DCI Factor for the next year based on actual measured Casemix Differential › If measured Casemix Differential is significantly different (more than 1 percentage point higher or lower) from the initial 3% assumption, further adjust the DCI Factor for the next year to prospectively correct for the previous year(s) Page 51

DOCUMENTATION AND CODING IMPROVEMENT DCI measurement (continued) » Measure actual increases in acuity using Medicare’s MSDRG grouper and Medicare relative weights – › Assumes that measuring actual changes in casemix using MSDRGs is a reasonable proxy for measuring actual change in acuity › Assumes that hospitals have already responded to documentation and coding standards needed for payment under MS-DRGs » Measure increases in acuity using APR-DRG grouper and relative weights using the same encounters » The Casemix Differential is the difference between MSDRG and APR-DRG casemix increases – › For example, for the same 12 month period, if MS-DRG casemix increases 1%, and APR-DRG casemix increases 4%, the Casemix Differential – the amount attributable to DCI – is 3 percentage Page 52 points
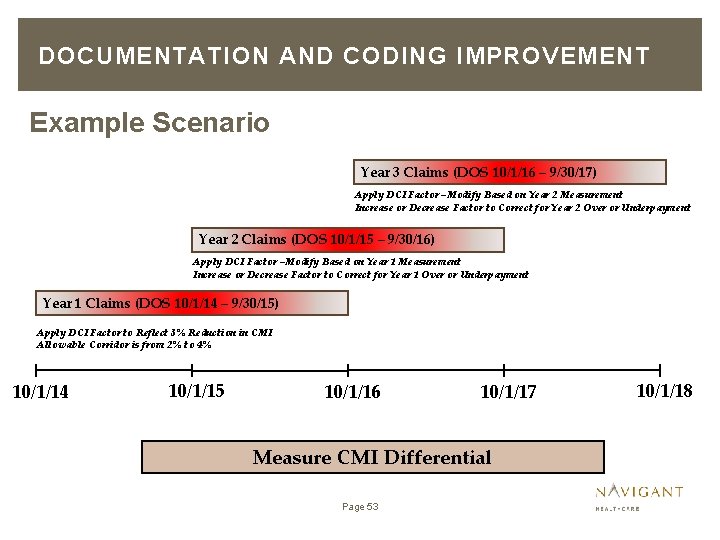
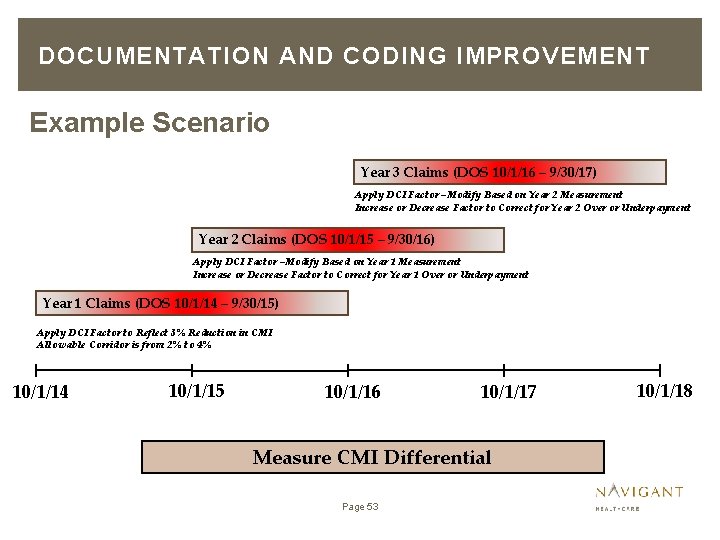
DOCUMENTATION AND CODING IMPROVEMENT Example Scenario Year 3 Claims (DOS 10/1/16 – 9/30/17) Apply DCI Factor –Modify Based on Year 2 Measurement Increase or Decrease Factor to Correct for Year 2 Over or Underpayment Year 2 Claims (DOS 10/1/15 – 9/30/16) Apply DCI Factor –Modify Based on Year 1 Measurement Increase or Decrease Factor to Correct for Year 1 Over or Underpayment Year 1 Claims (DOS 10/1/14 – 9/30/15) Apply DCI Factor to Reflect 3% Reduction in CMI Allowable Corridor is from 2% to 4% 10/1/14 10/1/15 10/1/16 10/1/17 Measure CMI Differential Page 53 10/1/18
DOCUMENTATION AND CODING IMPROVEMENT Example 10/1/15 CMI differential measurement » AHCCCS intends to measure CMI Differential using available Year 1 encounters. » Set Year 2 DCI Factor to be equal to measured Year 1 CMI Differential » Adjust Year 2 DCI Factor to correct for Year 1 overpayment or underpayment: › If measured Year 1 CMI Differential is within allowable corridor, make no adjustment › If measured Year 1 CMI Differential exceeds 4%, increase Year 2 DCI Factor by the difference between actual measured and 4% › If measured Year 1 CMI Differential is less than 2%, decrease Year 2 Page 54 DCI Factor by the difference between actual measured and 2%
DOCUMENTATION AND CODING IMPROVEMENT Example 10/1/16 CMI differential measurement » AHCCCS intends to measure CMI Differential using available Year 2 encounters › Alternatively use available encounters with DOS between 10/1/14 and date of measurement » Set Year 3 DCI Factor to be equal to measured Year 2 CMI Differential » Adjust Year 3 DCI Factor to correct for Year 2 overpayment or underpayment: › › If measured Year 2 CMI Differential is within allowable corridor, make no adjustment If measured Year 2 CMI Differential exceeds Year 2 DCI factor by more than 1 percentage point, increase Year 3 DCI Factor by the Page 55 difference
DOCUMENTATION AND CODING IMPROVEMENT Example 10/1/17 CMI differential measurement » » Rebase System Go Live – new rates become effective Begin rebasing process 9 -12 months prior to go live date Use most current 12 months of complete encounter data Based on results of previous analyses, determine need for additional DCI adjustments for 10/1/17, and going forward. Page 56
 Containment theory criminology
Containment theory criminology Arizona fare payment
Arizona fare payment What is altcs
What is altcs Arizona long term care system (altcs)
Arizona long term care system (altcs) Alice cost containment
Alice cost containment Accent cost containment solutions
Accent cost containment solutions Medical cost containment
Medical cost containment Cost containment definition
Cost containment definition Pacportal tim
Pacportal tim Job wr53 at nw fab
Job wr53 at nw fab Primary secondary tertiary care
Primary secondary tertiary care Perimeter fire containment systems
Perimeter fire containment systems Care value base health and social care
Care value base health and social care Health and social component 3
Health and social component 3 Arizona criminal justice information system
Arizona criminal justice information system Health insurance premium payment program ny
Health insurance premium payment program ny Objectives of health care delivery system
Objectives of health care delivery system Secondary care definition
Secondary care definition Introduction of health care delivery system
Introduction of health care delivery system Health care system definition
Health care system definition What was the policy of containment
What was the policy of containment Nato def apush
Nato def apush Containment of communism cloze notes
Containment of communism cloze notes Oil spill containment methods
Oil spill containment methods Jav worms
Jav worms On the resemblance and containment of documents
On the resemblance and containment of documents Java containment hierarchy
Java containment hierarchy Father of containment
Father of containment Where is the deadman on a fiberglass tank
Where is the deadman on a fiberglass tank Ischial containment socket
Ischial containment socket Interim containment action meaning
Interim containment action meaning Earthen berm
Earthen berm Opw india
Opw india With the order reversed perversely crossword clue
With the order reversed perversely crossword clue Maximum containment laboratory
Maximum containment laboratory Containment definition cold war
Containment definition cold war Fluid containment solutions
Fluid containment solutions Strengths of differential association theory
Strengths of differential association theory Containment soviet
Containment soviet Containment action planning
Containment action planning Containment
Containment Containment theory
Containment theory Containment politikk
Containment politikk Containment eradication
Containment eradication Cost accumulation and cost assignment
Cost accumulation and cost assignment Cost accumulation and cost assignment
Cost accumulation and cost assignment Manufacturing cost vs non manufacturing cost
Manufacturing cost vs non manufacturing cost Job costing vs process costing examples
Job costing vs process costing examples Whats financial leverage
Whats financial leverage Manufacturing cost vs non manufacturing cost
Manufacturing cost vs non manufacturing cost Cost pools
Cost pools Manufacturing cost vs non manufacturing cost
Manufacturing cost vs non manufacturing cost Standard cost variance
Standard cost variance Book value of debt
Book value of debt What is a period cost on the income statement
What is a period cost on the income statement Cost control and cost reduction difference
Cost control and cost reduction difference Definition of standard costing
Definition of standard costing