Advances and Controversies in Cardiovascular Risk Prediction Promises




































- Slides: 37
Advances and Controversies in Cardiovascular Risk Prediction Promises, Pitfalls and Progress Peter Brindle General Practitioner R&D lead Bristol, N. Somerset and S. Glouc PCTs

Outline • Promises – Why do CVD risk estimation? – Background – Framingham • Pitfalls – How well to current methods perform? – Two studies • Progress – Four new risk scores – Where to next?

PROMISES

Why do CVD risk estimation? • To identify high risk individuals • Prioritise treatment - for individuals - for policy • Patient education

Background • Guidelines recommend preventive treatment in high risk patients • Population screening • Lifelong treatment. Or not.

The Framingham Heart Study • Data collection started in 1948 • Bi-annual follow up • First CVD risk equation: Truett et al. 1967 • > 20 groups of regression equations between 1967 and 2008 • Modified Anderson et al 1991 used in UK

Framingham - Anderson • Data collected 1968 -75 • 5573 men and women followed up for 12 years • Six regression equations published in 1991

Risk factors used to calculate the Anderson Framingham risk score -age and sex -diastolic and systolic BP -total: HDL cholesterol ratio -diabetes (Y/N) -cigarette smoking (Y/N) -LVH (Y/N) Absolute CVD Risk over 10 years

Different versions and coloured charts New Zealand cardiovascular risk prediction charts

Sheffield Tables

Joint British Societies 1998

Joint British Societies(2) 2004

PITFALLS

Getting it wrong Over-prediction means. . . People with little to gain may become patients, and the benefit to risk ratio of treatment becomes too small Under-prediction means… People with much to gain may not be offered preventive treatment

How well does Framingham perform? • Single UK population • One systematic review

Framingham in the Renfrew/Paisley study § 12, 300 men and women, aged 45 -64 and no evidence of cardiovascular disease at entry (1972 -76) § 10 -year follow up for cardiovascular disease mortality § Stratified by individual social class and area deprivation

Social deprivation 10 -year predicted versus observed CVD death rates by area deprivation and social class Social class Deprivation (Pred/Obs) Non-Manual 0. 69 Manual 0. 52 p= 0. 0005 Affluent 0. 64 Intermediate 0. 56 Deprived 0. 47 p= 0. 0017 for trend The Framingham risk score does not reflect the increased risk of people from deprived backgrounds relative to affluent people

Predicted over observed ratios ordered by background risk of test population

Issues with Framingham • • BP treatment Family History Deprivation Ethnicity Generalisability Statistical validity Face validity Improvements are needed

PROGRESS

SCORE Systematic Coronary Risk Evaluation 2003 • 205, 178 men and women from 12 European cohort studies • Used by “European guidelines on cardiovascular disease prevention in clinical practice”


SCORE – better than Framingham? SCORE BP treatment Family History Deprivation Ethnicity Generalisability Statistical validity Face validity No No ? Yes No

ASSIGN - ASSessing cardiovascular risk, using SIGN guidelines • Scottish Heart and Health Extended Cohort (SHHEC) • 6540 men, 6757 women • Classic risk factors plus – Deprivation – Family history • Shifts treatment towards the socially deprived compared to Framingham

ASSIGN – better than Framingham? SCORE ASSIGN BP treatment No No Family History No No Yes No ? Yes No Deprivation Ethnicity Generalisability Statistical validity Face validity

QRISK 1 and QRISK 2 • Electronic patient record • Cohort analysis based on large validated GP database (QResearch) • Contains individual patient level data • 15 year study period 1993 to 2008 • First diagnosis of CVD (including CVD death) • QRISK 1 – – § Deprivation Family History BMI On BP treatment NO Ethnicity

QRISK 1 - better than Framingham? BP treatment Family History Deprivation Ethnicity Generalisability Statistical validity Face validity SCORE ASSIGN QRISK 1 No No ? Yes No No Yes No ? Yes No Yes Yes Yes

QRISK 2 • • • Included ONS deaths linkage Included additional variables 2. 3 million people (>16 million person yrs) Self-assigned ethnicity Derivation (1. 5 million) and test cohorts

Model performance QRISK 2 vs Modified Framingham QRISK 2 Framingham R squared 43. 4% 38. 9% D statistic 1. 793 1. 632 R squared 38. 4% 34. 8% D statistic 1. 616 1. 495 Females Males

Age-standardised incidence of CVD by deprivation

Adjusted Hazard Ratios for CVD

QRISK 2 – better than Framingham? BP treatment Family History Deprivation Ethnicity Reproducibility Generalisability Statistical validity Face validity SCORE ASSIGN QRISK 1 QRISK 2 No No Yes ? Yes No No Yes ? Yes No Yes Yes Yes Yes

Where to next? • Generalisability? • Linkage – Census – Hospital data • Improved ethnicity recording

Summary • Promises – Why do CVD risk estimation? – Background – Framingham • Pitfalls – How well to current methods perform? – Two studies • Progress – Four new risk scores – Where to next? – linkage and statistics

CONCLUSION • The idea of risk assessment is well established • Existing methods flawed – but better than nothing • Electronic patient record + improving data sources = exciting prospects

Acknowledgements • British Regional Heart study team • Renfrew/Paisley study team • Shah Ebrahim • Tom Fahey • Andy Beswick • Julia Hippisley-Cox • John Robson • Carol Coupland • Yana Vinogradova • Aziz Sheikh • Rubin Minhas

CONCLUSION • The idea of risk assessment is well established • Existing methods flawed – but better than nothing • Electronic patient record + improving data sources = exciting prospects
 Cardiovascular disease risk factor
Cardiovascular disease risk factor Liquidity measures
Liquidity measures Sports in society issues and controversies
Sports in society issues and controversies Controversies in sport
Controversies in sport It is current controversies in clinical psychologist
It is current controversies in clinical psychologist Activist trade policy
Activist trade policy Controversies in nursing
Controversies in nursing Sports controversies
Sports controversies Sports controversies
Sports controversies Loans and advances in tally
Loans and advances in tally What is long term loans and advances
What is long term loans and advances Global oncology trends 2017 advances complexity and cost
Global oncology trends 2017 advances complexity and cost Axis powers
Axis powers Advances in technology during wwii
Advances in technology during wwii Chapter 9 intellectual development of infants
Chapter 9 intellectual development of infants Advances in real time rendering
Advances in real time rendering Advances in mri
Advances in mri Opto-electronic advances
Opto-electronic advances Recent advances in dental ceramics
Recent advances in dental ceramics Asset classification norms
Asset classification norms Advances in memory technology
Advances in memory technology Frontiern
Frontiern Baptismal promises
Baptismal promises Solemn promises
Solemn promises Promises of distributed database system
Promises of distributed database system Managing service promises
Managing service promises Old testament promises
Old testament promises Managing service promises
Managing service promises Desired and adequate service
Desired and adequate service Believing in god's promises
Believing in god's promises Faraj promises
Faraj promises Manifesto for head girl
Manifesto for head girl Security promises of the jvm
Security promises of the jvm Note receivable
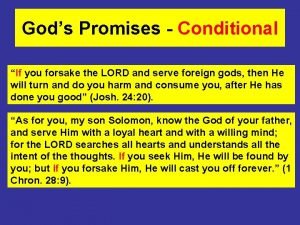
Note receivable Are god's promises conditional
Are god's promises conditional Promises of ddbms
Promises of ddbms Nothing formed against me shall stand song
Nothing formed against me shall stand song God's covenant
God's covenant