Acute Urinary Retention Laura Oakley FY 1 Urology

- Slides: 26
Acute Urinary Retention Laura Oakley FY 1 Urology
Definition l Acute Urinary Retention refers to the inability to empty the bladder l Most common in men l Increasing incidence with increasing age
Case Study: History 1 l 67 yr old man l PC 1) Unable to pass urine l 2) Lower abdominal pain l
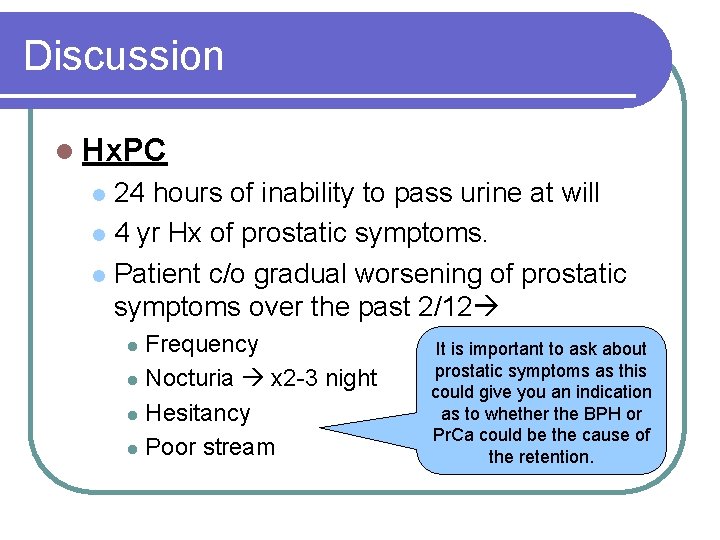
Case Study: History 2 l Hx. PC 24 hours of inability to pass urine at will l 4 yr Hx of prostatic symptoms. l Patient c/o gradual worsening of prostatic symptoms over the past 2/12 l Frequency l Nocturia x 2 -3 night l Hesitancy l Poor stream l
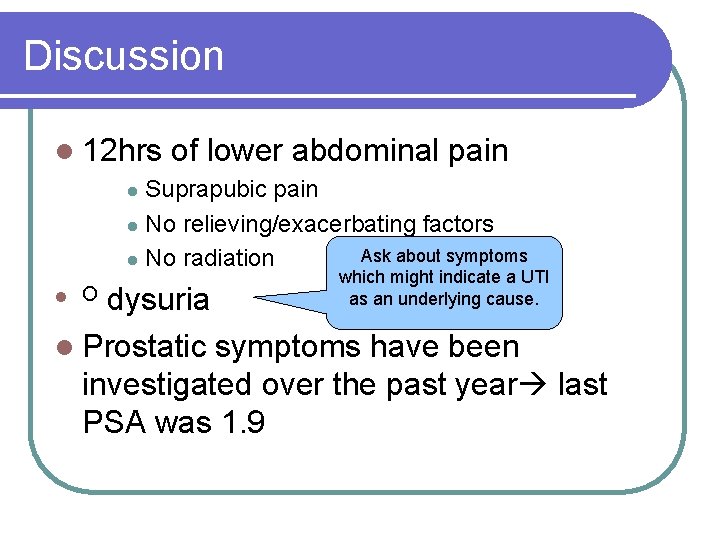
Case Study: History 3 l 12 hrs of lower abdominal pain Suprapubic pain l No relieving/exacerbating factors l No radiation l l No dysuria l Prostatic symptoms have been investigated over the past year last PSA was 1. 9
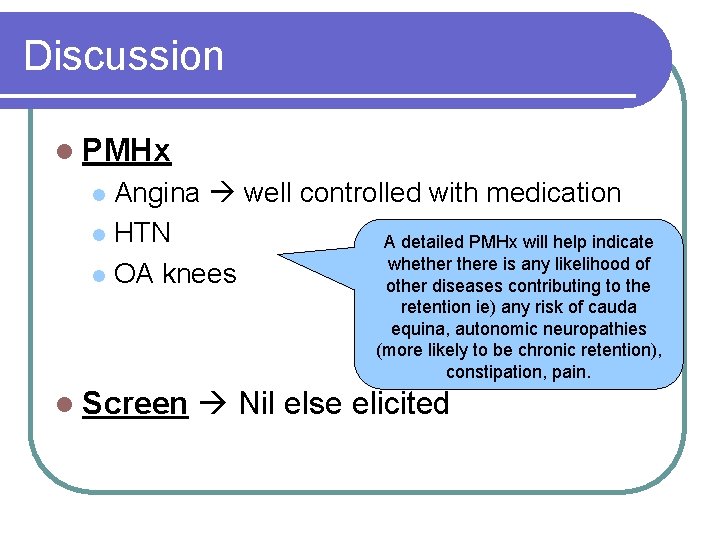
Case Study: History 4 l PMHx Angina well controlled with medication l HTN l OA knees l l Screen Nil else elicited
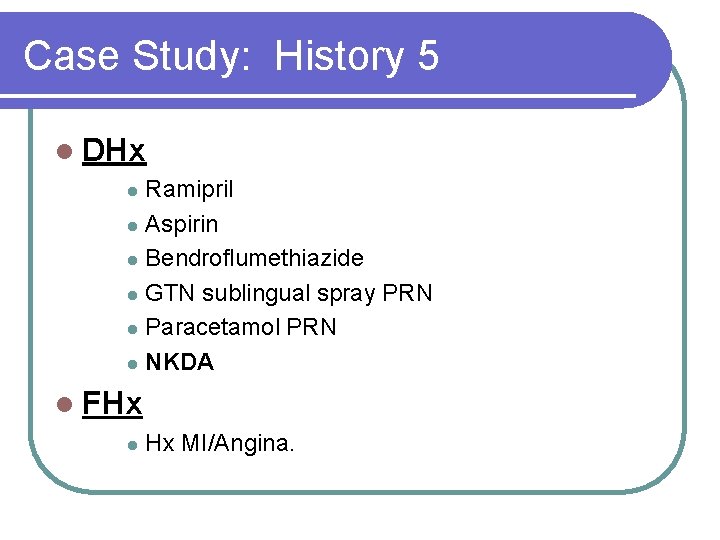
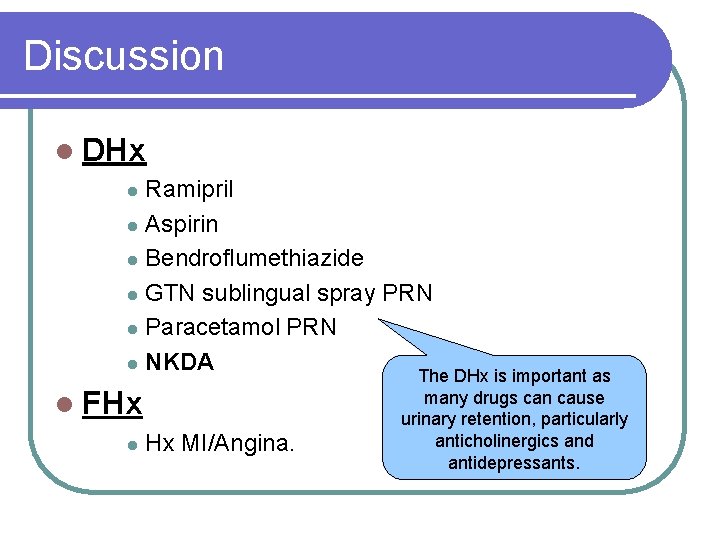
Case Study: History 5 l DHx Ramipril l Aspirin l Bendroflumethiazide l GTN sublingual spray PRN l Paracetamol PRN l NKDA l l FHx l Hx MI/Angina.
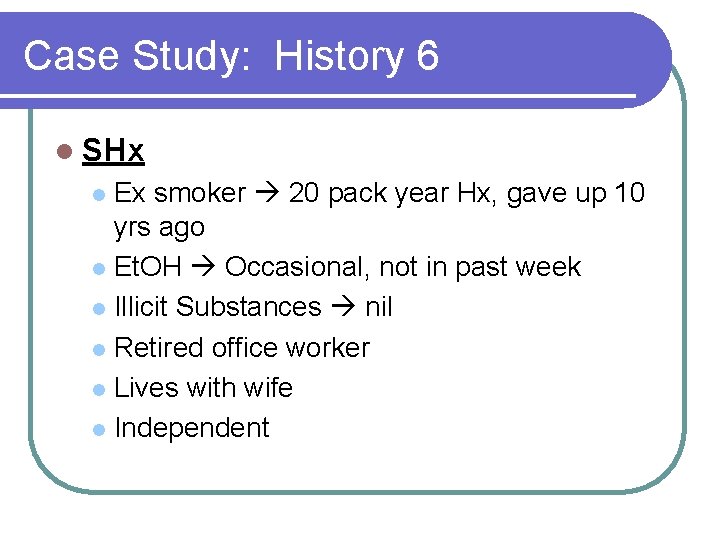
Case Study: History 6 l SHx Ex smoker 20 pack year Hx, gave up 10 yrs ago l Et. OH Occasional, not in past week l Illicit Substances nil l Retired office worker l Lives with wife l Independent l
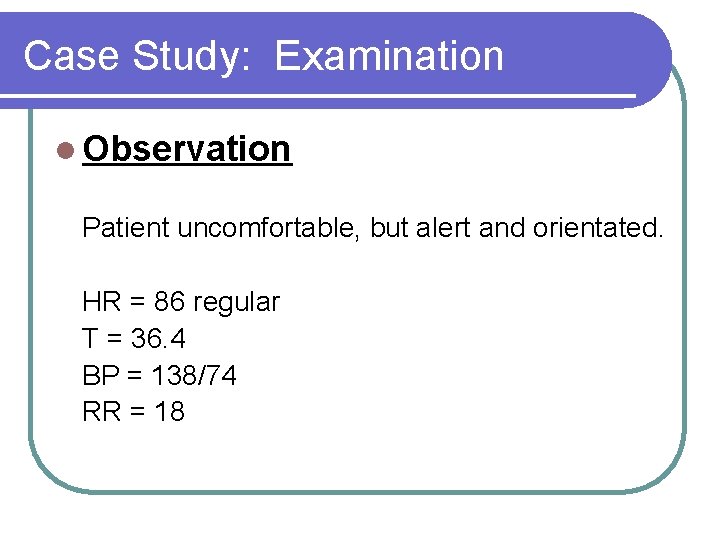
Case Study: Examination l Observation Patient uncomfortable, but alert and orientated. HR = 86 regular T = 36. 4 BP = 138/74 RR = 18
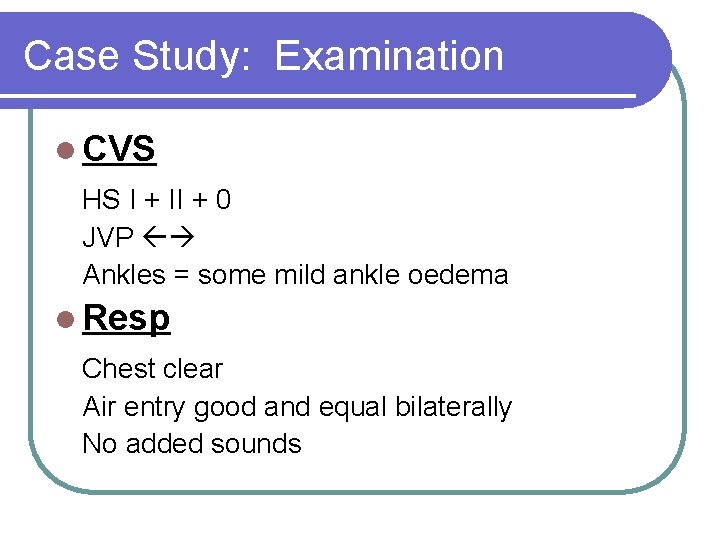
Case Study: Examination l CVS HS I + II + 0 JVP Ankles = some mild ankle oedema l Resp Chest clear Air entry good and equal bilaterally No added sounds
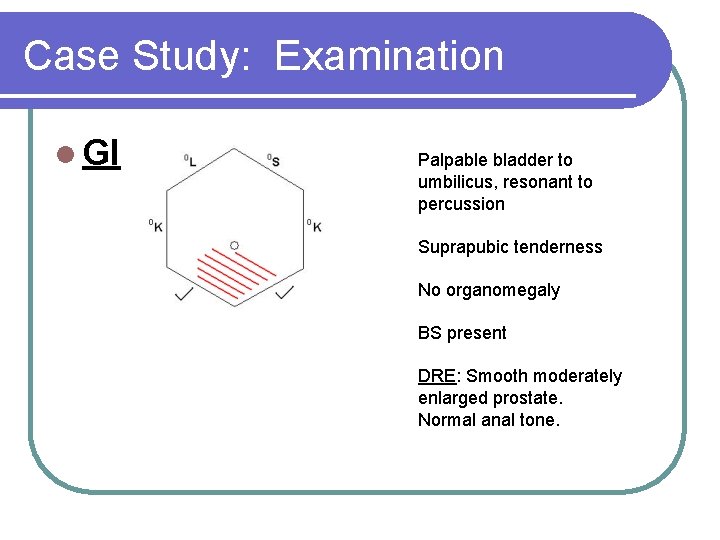
Case Study: Examination l GI Palpable bladder to umbilicus, resonant to percussion Suprapubic tenderness No organomegaly BS present DRE: Smooth moderately enlarged prostate. Normal anal tone.
Case Study: Examination l Neuro Power 5/5 Sensation N, perineal sensation normal Reflexes N Tone N l Bladder scan ~ 750 mls
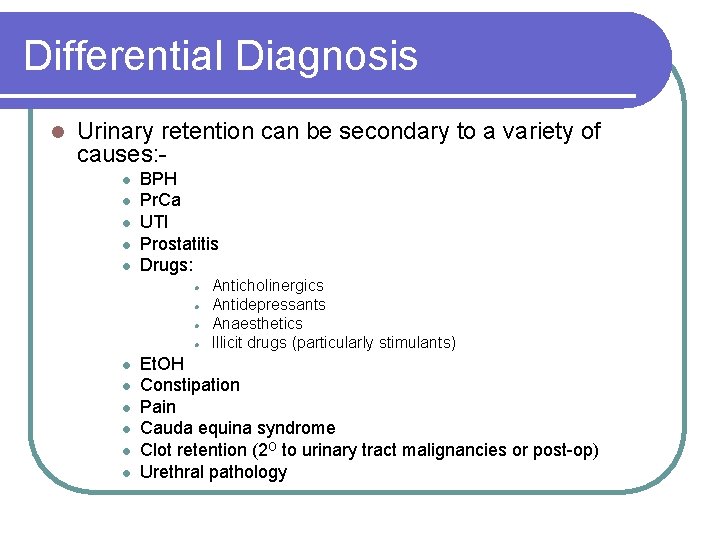
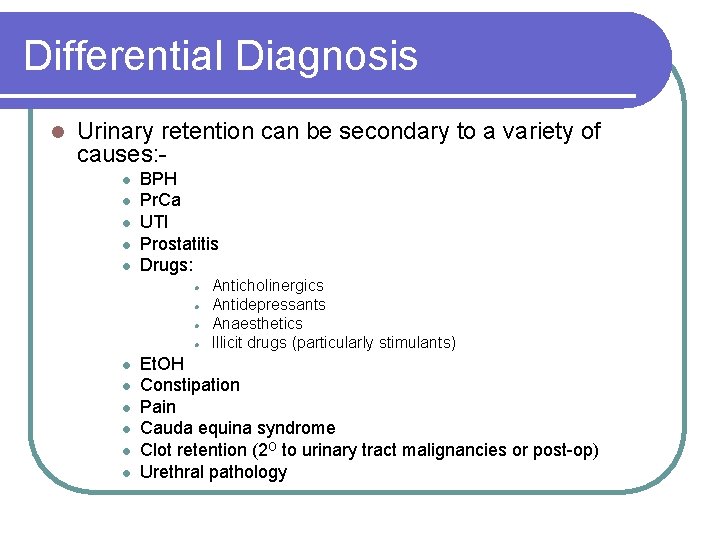
Differential Diagnosis l Urinary retention can be secondary to a variety of causes: l l l BPH Pr. Ca UTI Prostatitis Drugs: l l l l l Anticholinergics Antidepressants Anaesthetics Illicit drugs (particularly stimulants) Et. OH Constipation Pain Cauda equina syndrome Clot retention (2 O to urinary tract malignancies or post-op) Urethral pathology
Discussion l Points in the history can give us clues as to the cause of the individuals retention………
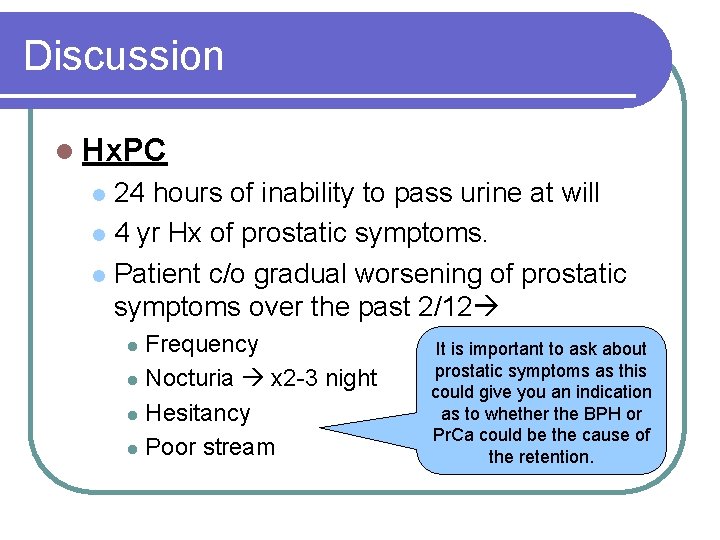
Discussion l Hx. PC 24 hours of inability to pass urine at will l 4 yr Hx of prostatic symptoms. l Patient c/o gradual worsening of prostatic symptoms over the past 2/12 l Frequency l Nocturia x 2 -3 night l Hesitancy l Poor stream l It is important to ask about prostatic symptoms as this could give you an indication as to whether the BPH or Pr. Ca could be the cause of the retention.
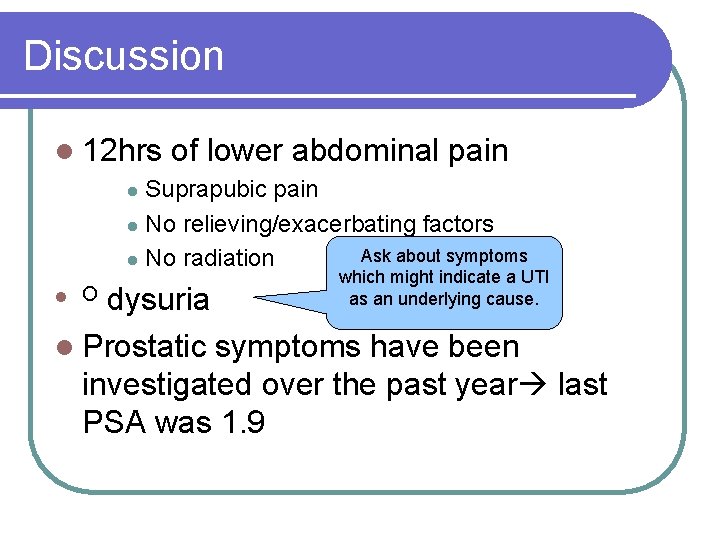
Discussion l 12 hrs of lower abdominal pain Suprapubic pain l No relieving/exacerbating factors Ask about symptoms l No radiation l which might indicate a UTI as an underlying cause. dysuria l Prostatic symptoms have been investigated over the past year last PSA was 1. 9 l O
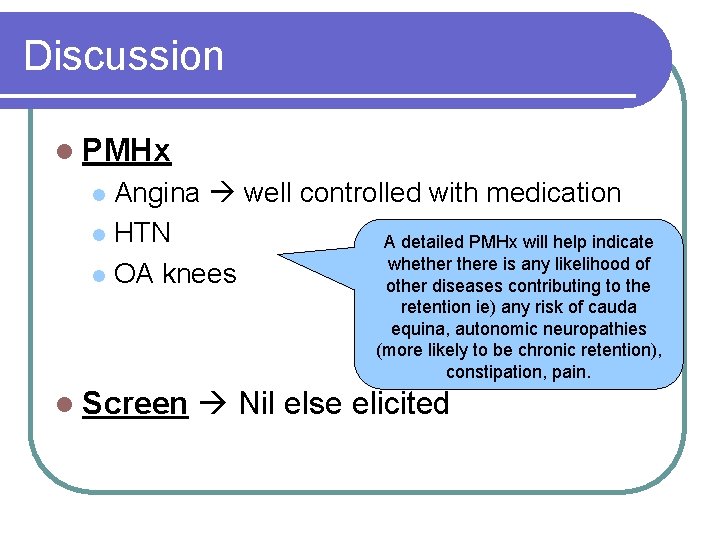
Discussion l PMHx Angina well controlled with medication l HTN A detailed PMHx will help indicate whethere is any likelihood of l OA knees other diseases contributing to the l retention ie) any risk of cauda equina, autonomic neuropathies (more likely to be chronic retention), constipation, pain. l Screen Nil else elicited
Discussion l DHx Ramipril l Aspirin l Bendroflumethiazide l GTN sublingual spray PRN l Paracetamol PRN l NKDA l l FHx l Hx MI/Angina. The DHx is important as many drugs can cause urinary retention, particularly anticholinergics and antidepressants.
Discussion l SHx Ex smoker 20 pack year Hx, gave up 10 yrs ago l Et. OH Occasional, not in past week l Illicit Substances nil l Retired office worker A good social history helps us to elicit l Lives with wife whether Et. OH consumption or drug abuse could have contributed to the l Independent development of retention. Be particularly l aware of this in cases involving younger men with no other likely cause.

Discussion l GI Palpable bladder to umbilicus, resonant to percussion Suprapubic tenderness No organomegaly Doing a DRE is essential, as it can identify: BPH (enlarged, smooth), malignant prostate (craggy, hard) and can also help to identify other causes such as cauda equina syndrome (reduced anal tone, saddle anaesthesia). BS present DRE: Smooth moderately enlarged prostate. Normal anal tone.
Investigations l Some basic preliminary investigations may help narrow down the cause……
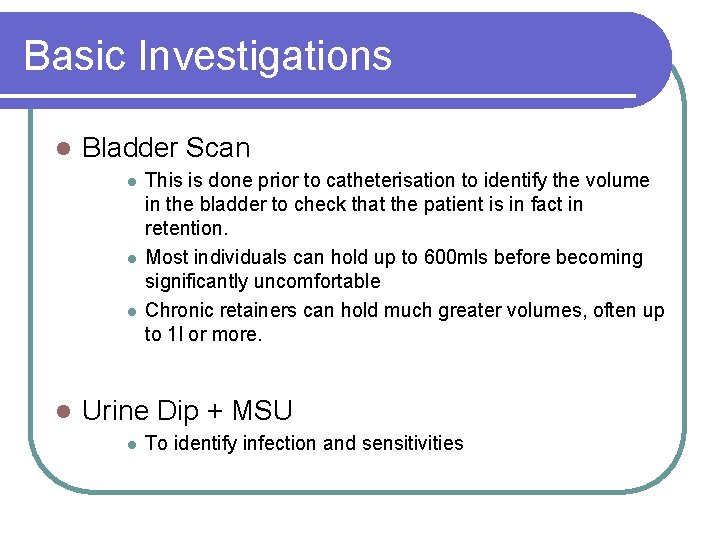
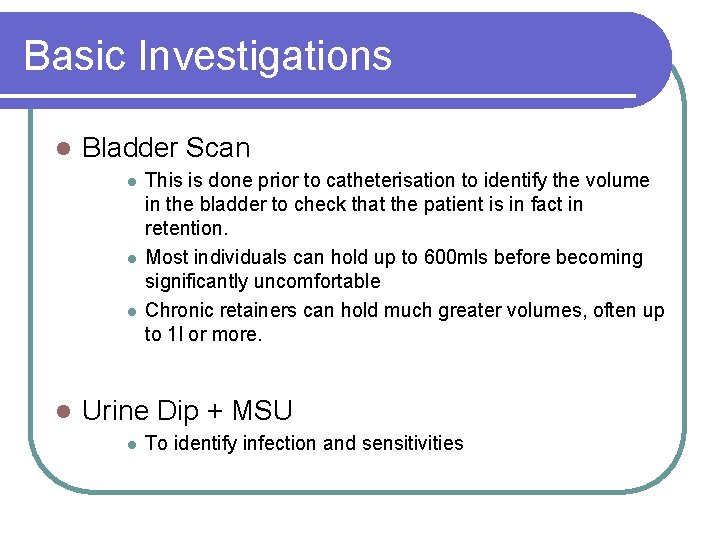
Basic Investigations l Bladder Scan l l This is done prior to catheterisation to identify the volume in the bladder to check that the patient is in fact in retention. Most individuals can hold up to 600 mls before becoming significantly uncomfortable Chronic retainers can hold much greater volumes, often up to 1 l or more. Urine Dip + MSU l To identify infection and sensitivities
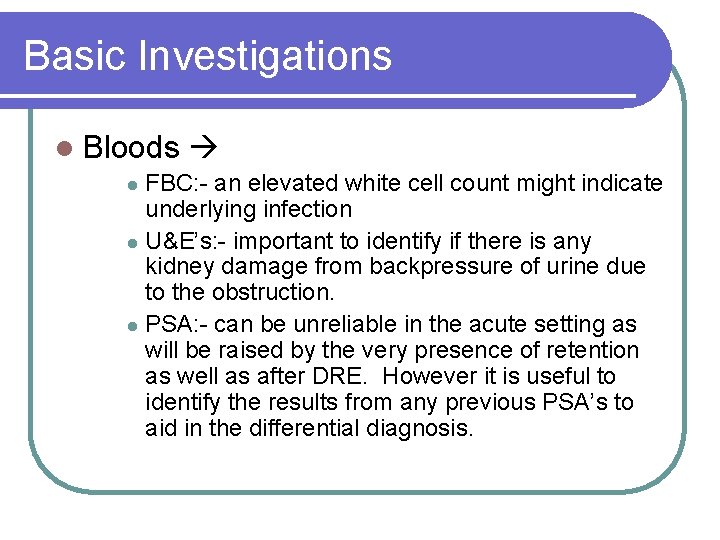
Basic Investigations l Bloods FBC: - an elevated white cell count might indicate underlying infection l U&E’s: - important to identify if there is any kidney damage from backpressure of urine due to the obstruction. l PSA: - can be unreliable in the acute setting as will be raised by the very presence of retention as well as after DRE. However it is useful to identify the results from any previous PSA’s to aid in the differential diagnosis. l
Treatment l Catheterise using aseptic technique and appropriate Abx cover l IM Gentamicin is the Abx of choice in this Trust. Record residual volume of urine l Monitor for diuresis occurs due to: l l Osmotic diuresis secondary to increased urea following retention Diuresis of retained salt and H 2 O Reduced concentration gradient in the Loop of Henlé after reduced flow rates in retention, which do not recover immediately after obstruction to the urinary tract is relieved.
Further Investigations and Treatment l Further treatment may include: l l l Abx for UTI’s and Prostitis Tamsulosin 400 micrograms OD for BPH TWOC (trial without catheter) following underlying cause being treated. l Further investigations may include: l l Prostate biopsy (suspicion of malignancy) Renal Tract US (hydronephrosis) MRI L-S spine (cauda equina syndrome) Surgery (ie TURP for BPH/Pr. Ca)
Summary l Acute retention is a common but easily treated condition l There a variety of common causes, most commonly BPH and UTI’s. l It is important to fully investigate these causes and treat accordingly to prevent permanent damage to the urinary tract and prevent recurrence.
 Laura oakley
Laura oakley Urinary retention
Urinary retention Purpose of catheterization
Purpose of catheterization Indica el reflexivo reciproco adecuado
Indica el reflexivo reciproco adecuado Usc
Usc Urology coding cheat sheet
Urology coding cheat sheet Rpug in urology
Rpug in urology Hymen
Hymen Dr donaldson urology
Dr donaldson urology Children urology
Children urology Ubc urology
Ubc urology Refhelp urology
Refhelp urology Urology match
Urology match Hidrocele y varicocele
Hidrocele y varicocele Pediatric urologist atlanta ga
Pediatric urologist atlanta ga Srmc urology
Srmc urology Urology match
Urology match Carlee oakley
Carlee oakley Toxin neutralization test
Toxin neutralization test Oakley fulthorpe procedure
Oakley fulthorpe procedure Luke geary mills oakley
Luke geary mills oakley The urinary system chapter 15
The urinary system chapter 15 Urinary system powerpoint
Urinary system powerpoint Diuretics classification
Diuretics classification Location of kidneys in humans
Location of kidneys in humans Chapter 25 urinary catheters
Chapter 25 urinary catheters Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures