A COMPARATIVE ANALYSIS OF ANTIMULLERIAN HORMONE AND FOLLICLE








- Slides: 36
A COMPARATIVE ANALYSIS OF ANTI-MULLERIAN HORMONE AND FOLLICLE STIMULATING HORMONE IN ASSESSMENT OF OVARIAN RESERVE Dr. Kenneth Egwuda MBBS, PGA-ART(Lon), ESGE(Belg. ), FMAS, FWACS, FMC OG
Authors Egwuda, K. ; Onuh, SO. ; Ekwempu, CC. ; Shuaibu, SI. , Kamolideen, AA; Ojima, SC
AMH/FSH • A patient's ovarian reserve (OR) determines prognostic chances of fertility treatments and her treatment options • Best possible assessments of OR, therefore, represent a core issue in modern infertility care
OR • In human in-vitro fertilization (IVF), the identification of variables able to predict ovarian responsiveness to exogenous gonadotropins guides the clinician on individualizing treatment protocols, optimizing results and reducing complications
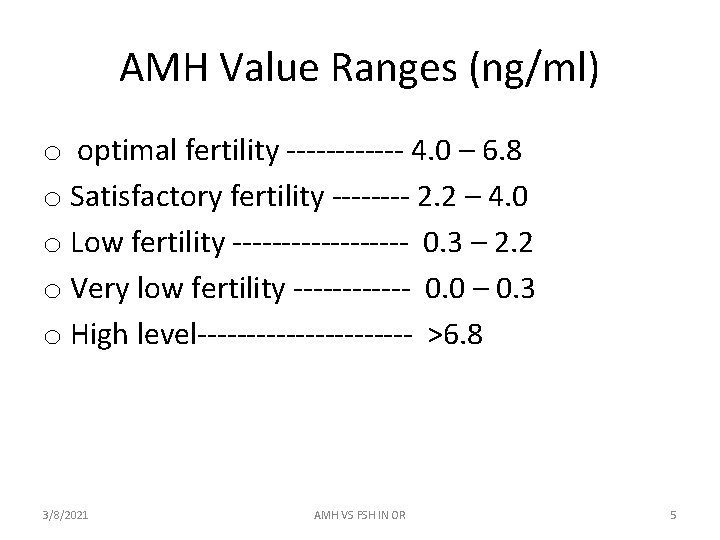
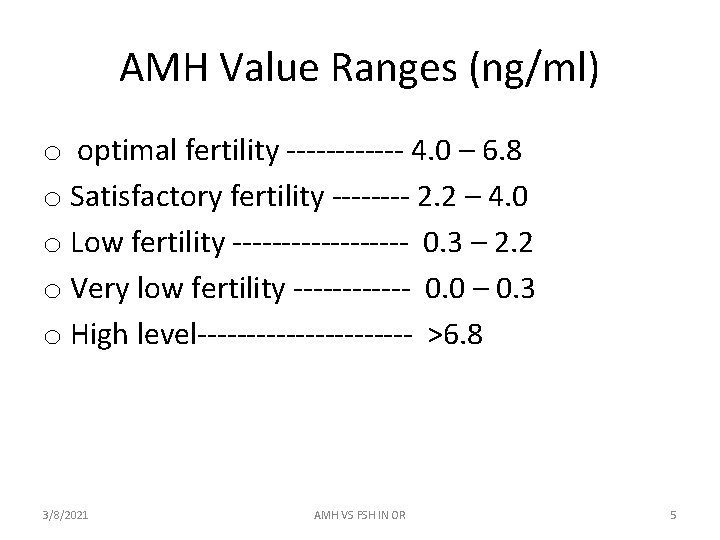
AMH Value Ranges (ng/ml) o optimal fertility ------ 4. 0 – 6. 8 o Satisfactory fertility ---- 2. 2 – 4. 0 o Low fertility --------- 0. 3 – 2. 2 o Very low fertility ------ 0. 0 – 0. 3 o High level----------- >6. 8 3/8/2021 AMH VS FSH IN OR 5
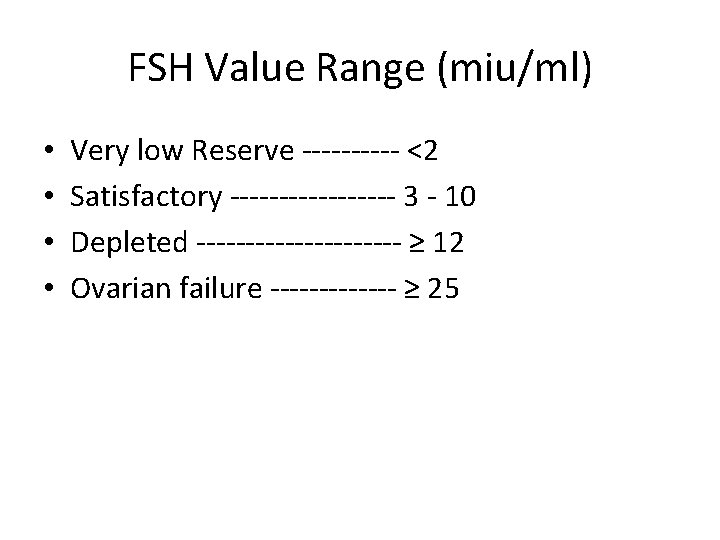
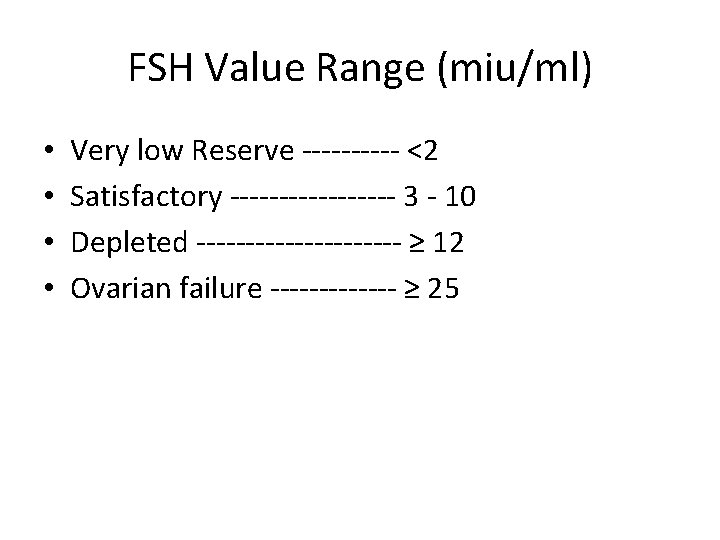
FSH Value Range (miu/ml) • • Very low Reserve ----- <2 Satisfactory --------- 3 - 10 Depleted ----------- ≥ 12 Ovarian failure ------- ≥ 25
objectives • To evaluate basal anti-müllerian hormone as compared to follicle stimulating hormone as a marker for ovarian reserve and responsiveness
Objective • To determine whether AMH is a better marker of ovarian reserve and responsiveness than FSH
Study Type • This was a hospital based study that was carried out in Fertile Aid Clinic, DEDA Hospital Abuja and a private hospital in Jos
Study Population • The study population comprised of clients who had the indication for In-vitro fertilization and Embryo Transfer (IVF-ET) or Assisted Reproductive Technology (ART), had been counselled, consented and scheduled for a treatment cycle
STUDY DESIGN • This was a cross-sectional and comparative study
INCLUSION CRITERIA • < 40 years, • having regular, menstrual cycles every 21– 35 days • having both ovaries present • no current or past diseases affecting ovaries, gonadotrophin, sex steroid secretion, clearance or excretion • they were also not on any form of hormonal therapy • their ovaries were adequately visualized at transvaginal ultrasound scanning
ETHICAL CONSIDERATION • This study was approved by the Research and Ethical Committees of the institution where it was conducted and the Federal Capital Development Authority. Informed consent was obtained from the clients before enrolment into the study. The laboratory analysis of baseline serum Anti-Mullerian Hormone was paid for by the researchers
methodology • Stored basal menstrual cycle day three serum samples of 112 women was evaluated for AMH and FSH and compared to the number of oocytes retrieved • A correlation analysis, ROC curve and analysis of variance were performed to determine the level of accuracy between AMH and FSH in predicting the ovarian reserve and responsiveness
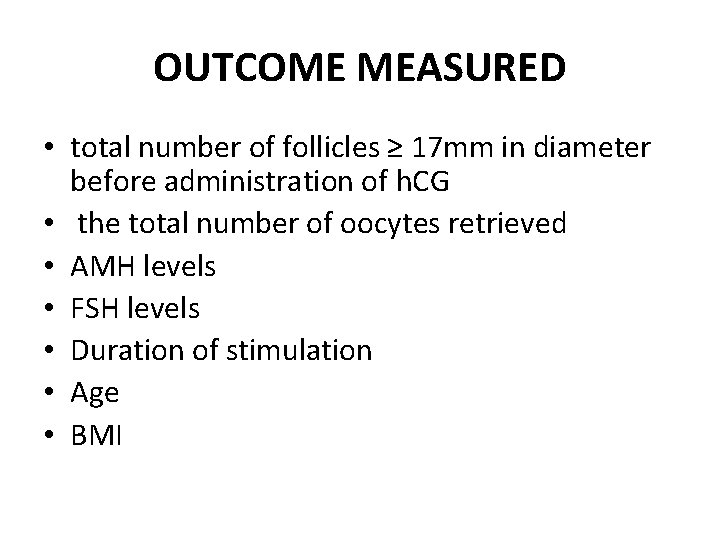
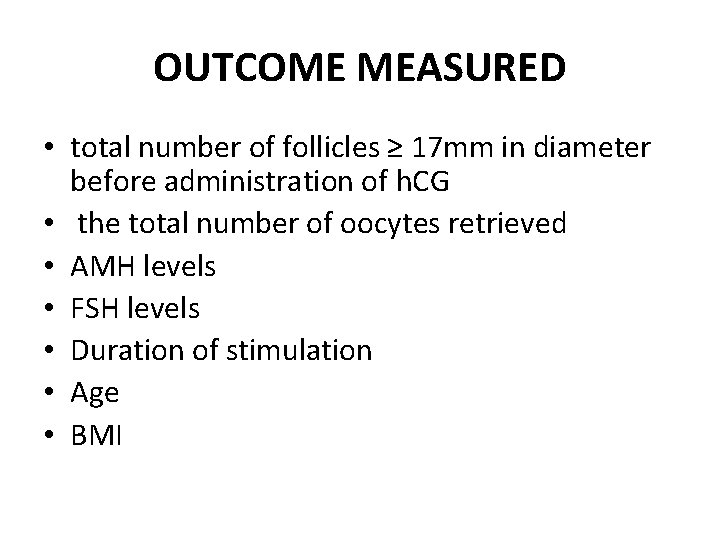
OUTCOME MEASURED • total number of follicles ≥ 17 mm in diameter before administration of h. CG • the total number of oocytes retrieved • AMH levels • FSH levels • Duration of stimulation • Age • BMI
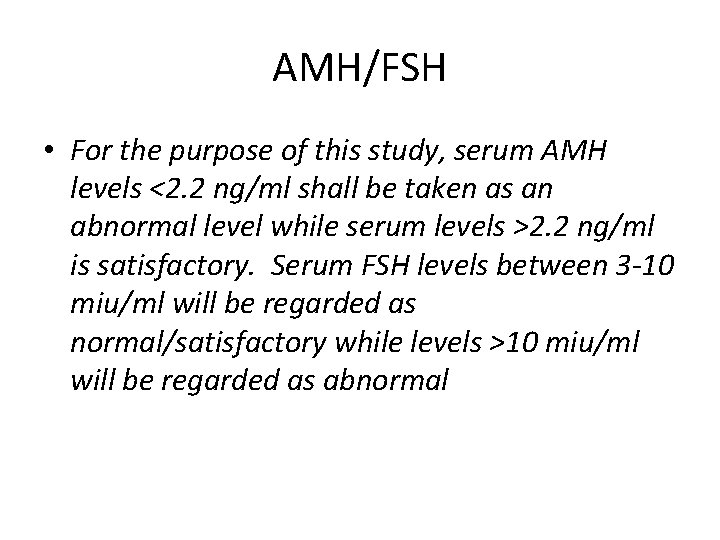
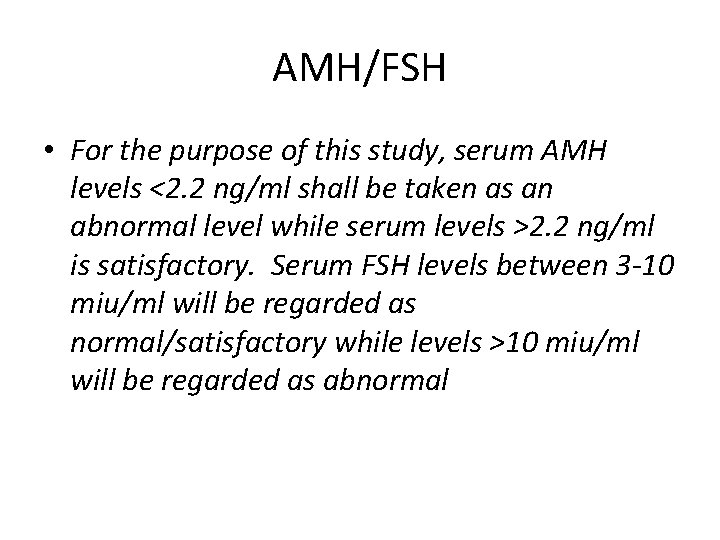
AMH/FSH • For the purpose of this study, serum AMH levels <2. 2 ng/ml shall be taken as an abnormal level while serum levels >2. 2 ng/ml is satisfactory. Serum FSH levels between 3 -10 miu/ml will be regarded as normal/satisfactory while levels >10 miu/ml will be regarded as abnormal
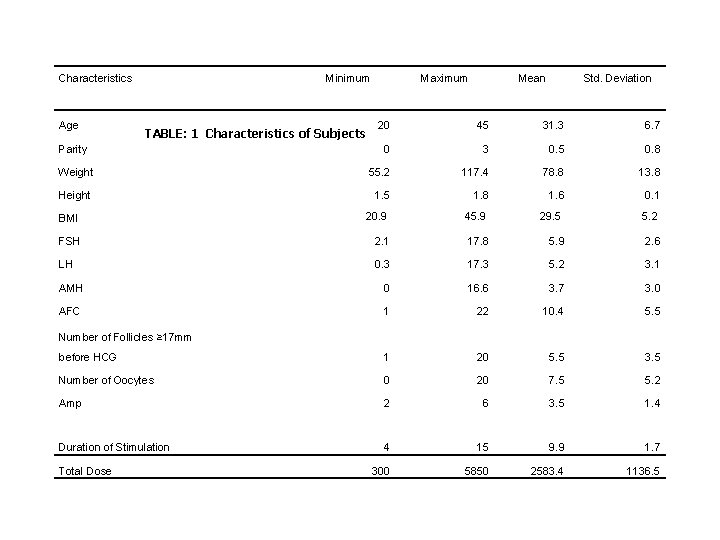
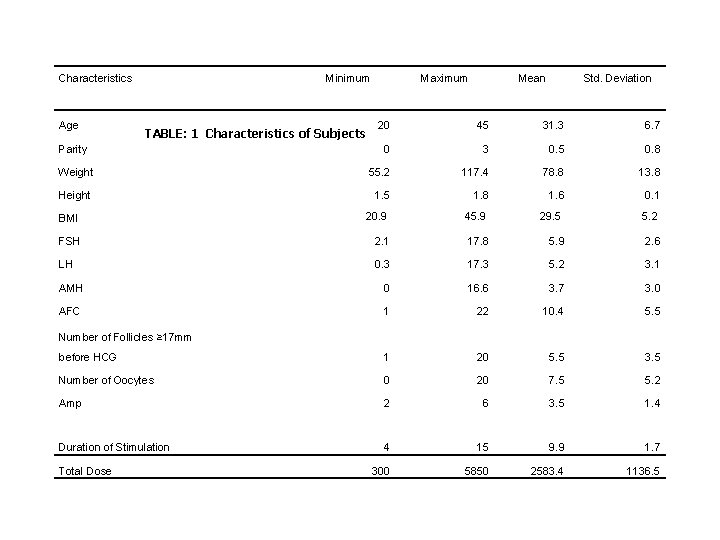
Characteristics Age Minimum Maximum Mean Std. Deviation 20 45 31. 3 6. 7 Parity 0 3 0. 5 0. 8 Weight 55. 2 117. 4 78. 8 13. 8 Height 1. 5 1. 8 1. 6 0. 1 BMI 20. 9 45. 9 29. 5 5. 2 FSH 2. 1 17. 8 5. 9 2. 6 LH 0. 3 17. 3 5. 2 3. 1 AMH 0 16. 6 3. 7 3. 0 AFC 1 22 10. 4 5. 5 before HCG 1 20 5. 5 3. 5 Number of Oocytes 0 20 7. 5 5. 2 Amp 2 6 3. 5 1. 4 Duration of Stimulation 4 15 9. 9 1. 7 Total Dose 300 5850 2583. 4 1136. 5 TABLE: 1 Characteristics of Subjects Number of Follicles ≥ 17 mm







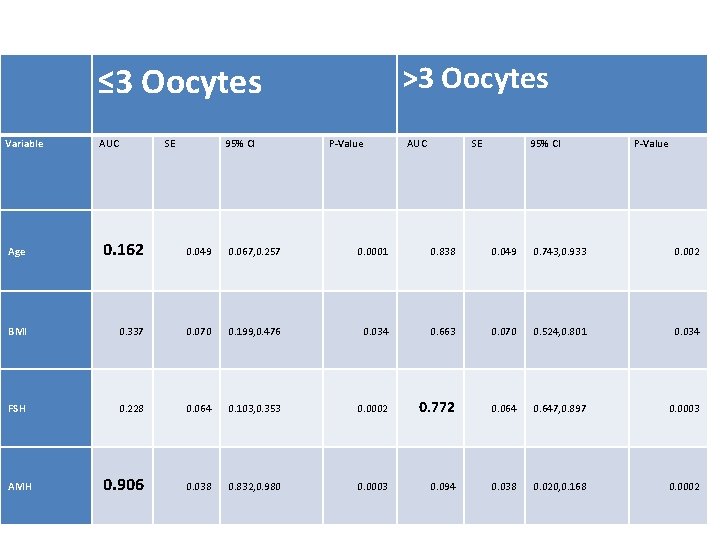
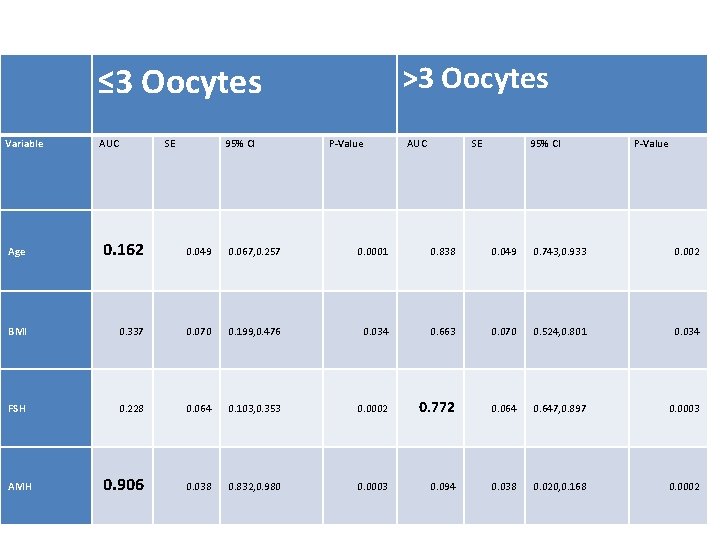
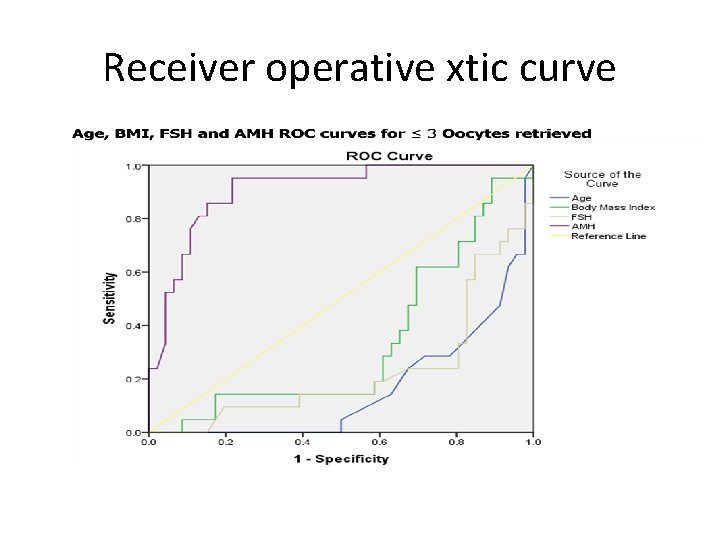
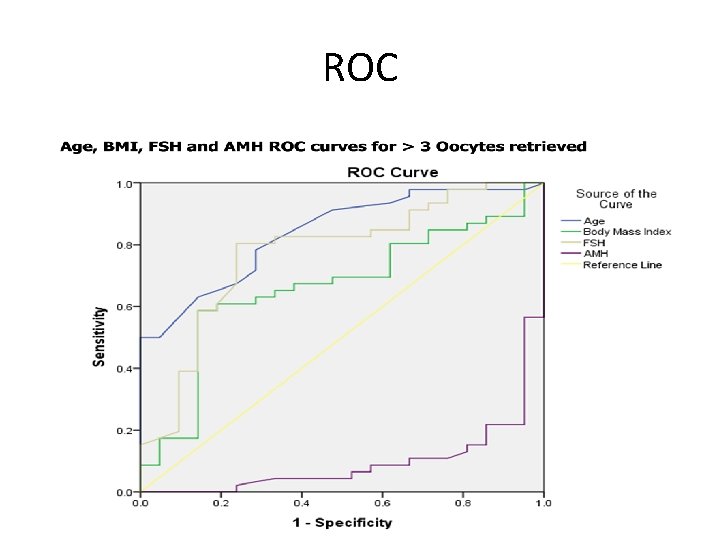
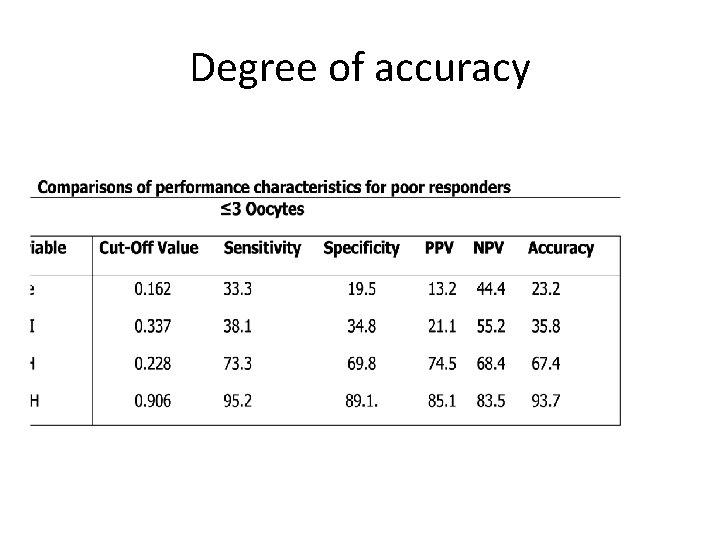
≤ 3 Oocytes Variable AUC SE 95% CI >3 Oocytes P-Value AUC SE 95% CI P-Value Age 0. 162 0. 049 0. 067, 0. 257 0. 0001 0. 838 0. 049 0. 743, 0. 933 0. 002 BMI 0. 337 0. 070 0. 199, 0. 476 0. 034 0. 663 0. 070 0. 524, 0. 801 0. 034 FSH 0. 228 0. 064 0. 103, 0. 353 0. 0002 0. 772 0. 064 0. 647, 0. 897 0. 0003 0. 906 0. 038 0. 832, 0. 980 0. 0003 0. 094 0. 038 0. 020, 0. 168 0. 0002 AMH
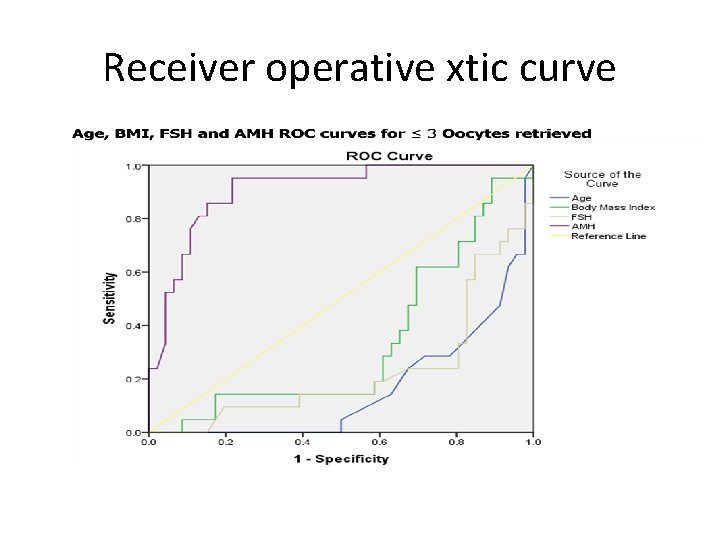
Receiver operative xtic curve
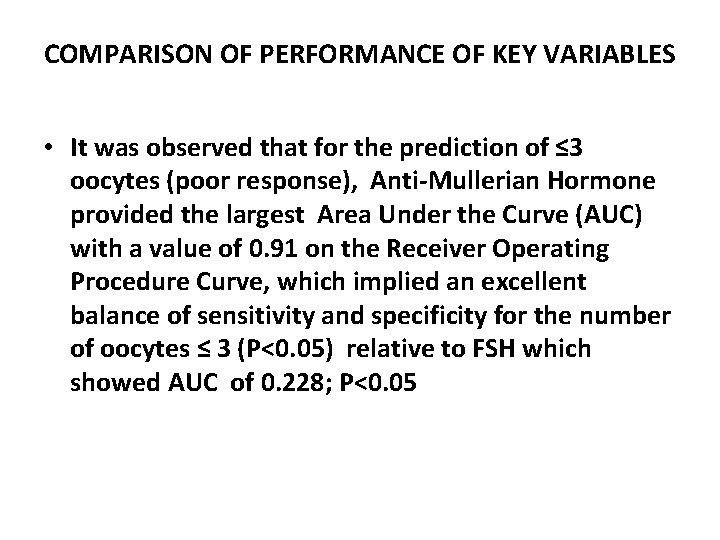
COMPARISON OF PERFORMANCE OF KEY VARIABLES • It was observed that for the prediction of ≤ 3 oocytes (poor response), Anti-Mullerian Hormone provided the largest Area Under the Curve (AUC) with a value of 0. 91 on the Receiver Operating Procedure Curve, which implied an excellent balance of sensitivity and specificity for the number of oocytes ≤ 3 (P<0. 05) relative to FSH which showed AUC of 0. 228; P<0. 05
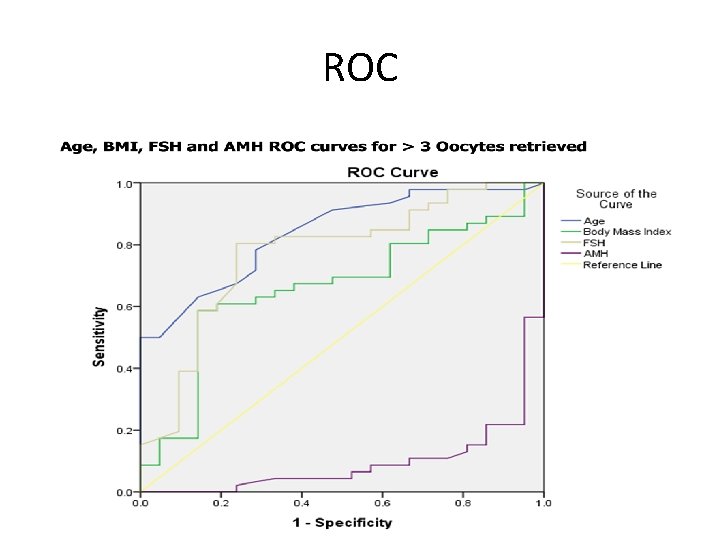
ROC
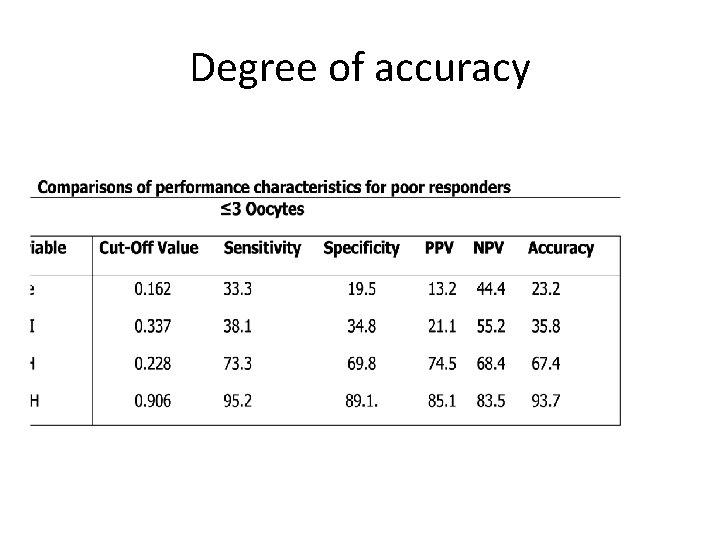
Degree of accuracy

AMH/FSH • FSH show a higher level of sensitivity for levels of Oocyte >3 oocytes retrieved. Interestingly, AMH showed a higher overall accuracy (82. 1%) even for normal responders
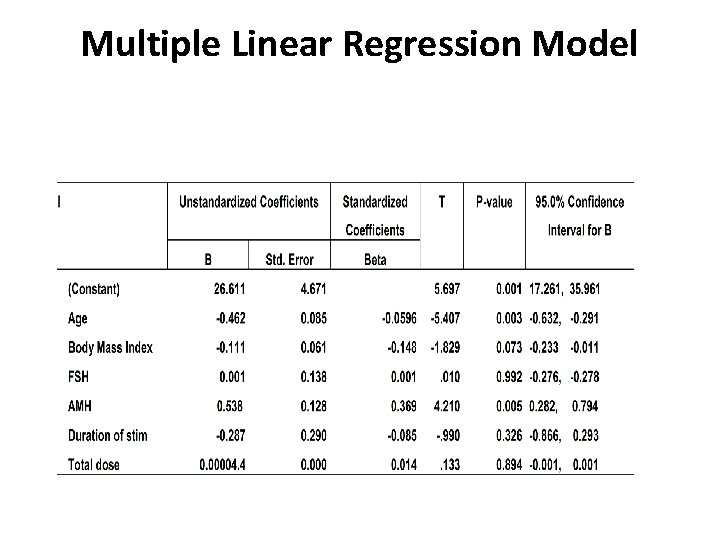
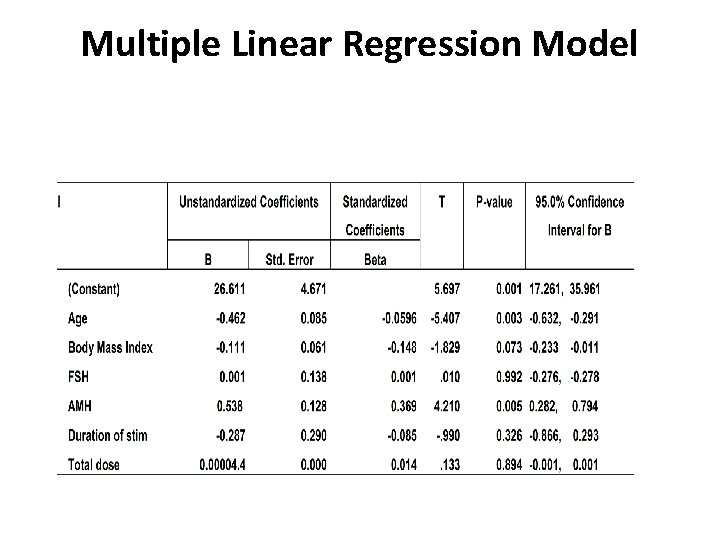
Multiple Linear Regression Model
model • A model developed based on the different variable that could predict the number of oocytes retrieved in an IVF treatment cycle. Though the model looks positive, AMH appeared to be the only significant predictor of the number of oocytes retrieved as compared to other independent variables including FSH. Anti. Mullerian Hormone was also seen to have the largest contribution (4. 210) to the model since it has the highest coefficient of 0. 538
conclusion • Conventional evaluation of ovarian reserve requires specific menstrual cycle day serum evaluation of oestradiol, FSH, and LH. The accuracy of these analytes may be decreased dramatically by exogenous hormone (gonadotropin-releasing hormone agonists, gonadotropin-releasing hormone antagonists, hormonal contraceptives), endogenous hormones (elevated oestradiol levels because of a functional ovarian cyst), and timing of sample acquisition
conclusion • studies have shown that AMH results are not influenced significantly by menstrual cycle day, oestradiol, contraceptives, or gonadotropinreleasing hormone agonists. Because AMH offers added convenience and its predictive value parallels or exceeds conventional analytes testing with FSH, age, and inhibin B, AMH appears to represent a compelling tool for the assessment of ovarian reserve. Use of AMH testing is likely to improve ovarian reserve assessment in infertile patients.
conclusion Thank you
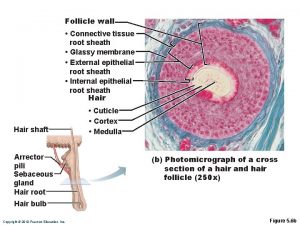
 Label the structures of the hair follicle
Label the structures of the hair follicle Vesicular (graafian) follicle
Vesicular (graafian) follicle Skin diagram labeled
Skin diagram labeled Empty hair follicle
Empty hair follicle Normal antral follicle count by age
Normal antral follicle count by age Layers of fallopian tube
Layers of fallopian tube Hair follicle definition forensics
Hair follicle definition forensics Hair follicle
Hair follicle Dominant follicle size
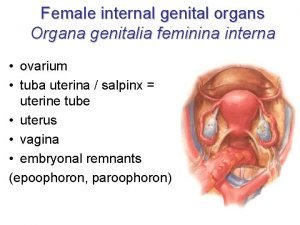
Dominant follicle size Organa genitalia feminina nedir
Organa genitalia feminina nedir Advanced bell stage ppt
Advanced bell stage ppt Ankylosis cementum
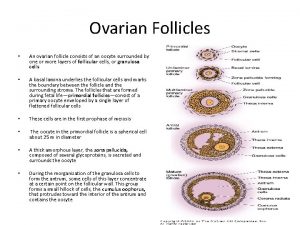
Ankylosis cementum Ovarian follicle
Ovarian follicle Anatomy of ovary slideshare
Anatomy of ovary slideshare Meissner’s corpuscles
Meissner’s corpuscles Follicular development diagram
Follicular development diagram Secondary follicle
Secondary follicle Uterus diagram
Uterus diagram Profase 1 meiosis
Profase 1 meiosis Lymphoid tissue in large intestine
Lymphoid tissue in large intestine Follicle atresia
Follicle atresia Draw a labelled diagram of a graafian follicle
Draw a labelled diagram of a graafian follicle Follicular adenoma
Follicular adenoma Unfair board game review
Unfair board game review Parathyroid gland image
Parathyroid gland image D
D Comparative form.
Comparative form. Function of antidiuretic hormone
Function of antidiuretic hormone Steroid hormones lipids
Steroid hormones lipids Thyroid hormone secretion
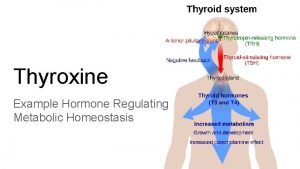
Thyroid hormone secretion Thyroid hormone secretion
Thyroid hormone secretion Hormone classification
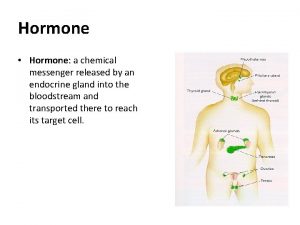
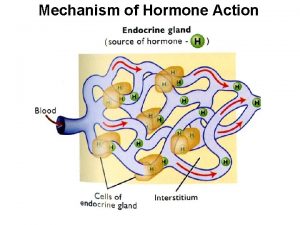
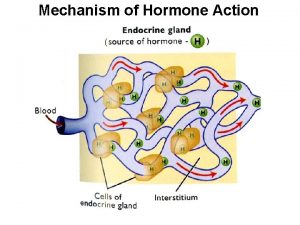
Hormone classification Reproductive physiology
Reproductive physiology Zygote
Zygote Hormone responsible for growth
Hormone responsible for growth Kako sportsko rekreativne aktivnosti deluju na nase hormone
Kako sportsko rekreativne aktivnosti deluju na nase hormone Major galactokinetic hormone
Major galactokinetic hormone