55 Year Old Female with Familial Hypercholesterolemia Case

- Slides: 29
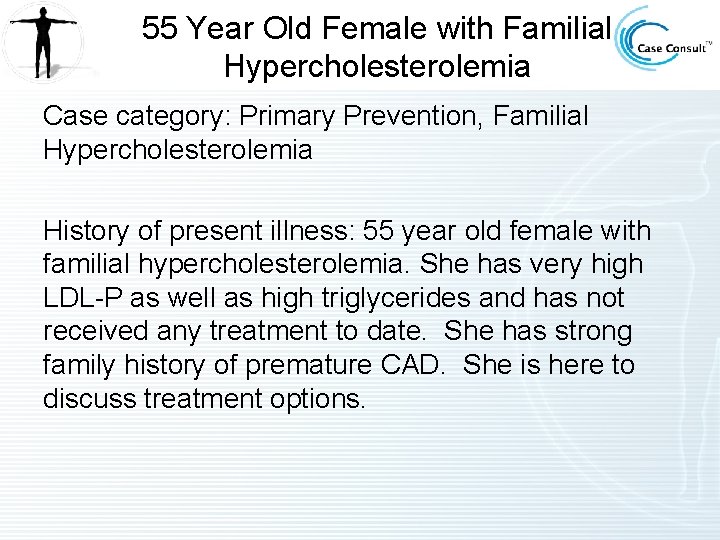
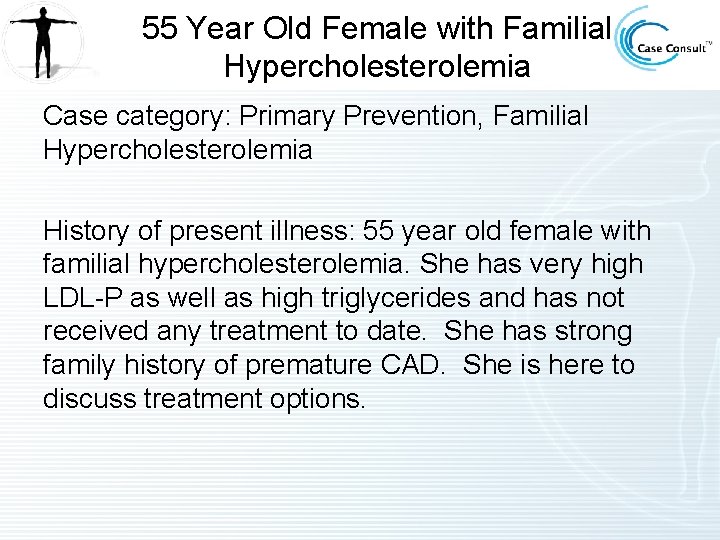
55 Year Old Female with Familial Hypercholesterolemia Case category: Primary Prevention, Familial Hypercholesterolemia History of present illness: 55 year old female with familial hypercholesterolemia. She has very high LDL-P as well as high triglycerides and has not received any treatment to date. She has strong family history of premature CAD. She is here to discuss treatment options.
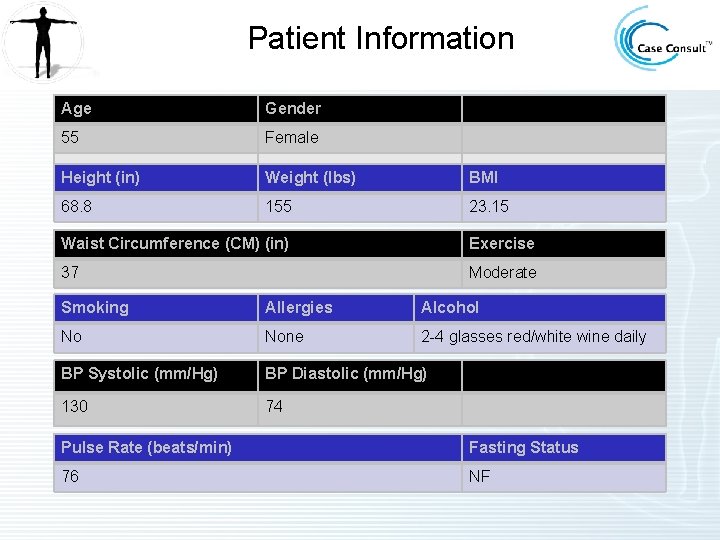
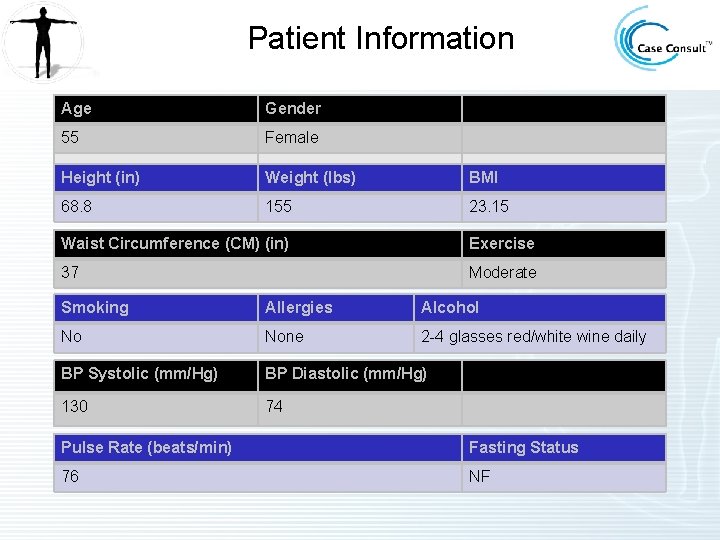
Patient Information Age Gender 55 Female Height (in) Weight (lbs) BMI 68. 8 155 23. 15 Waist Circumference (CM) (in) Exercise 37 Moderate Smoking Allergies Alcohol No None 2 -4 glasses red/white wine daily BP Systolic (mm/Hg) BP Diastolic (mm/Hg) 130 74 Pulse Rate (beats/min) Fasting Status 76 NF
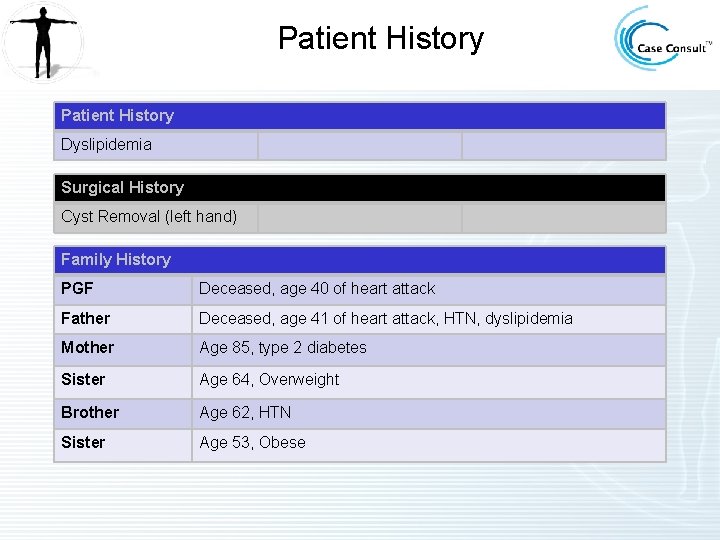
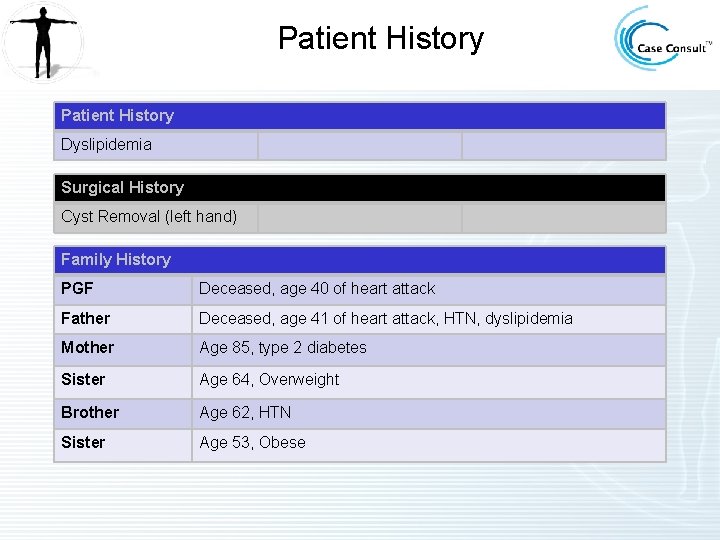
Patient History Dyslipidemia Surgical History Cyst Removal (left hand) Family History PGF Deceased, age 40 of heart attack Father Deceased, age 41 of heart attack, HTN, dyslipidemia Mother Age 85, type 2 diabetes Sister Age 64, Overweight Brother Age 62, HTN Sister Age 53, Obese
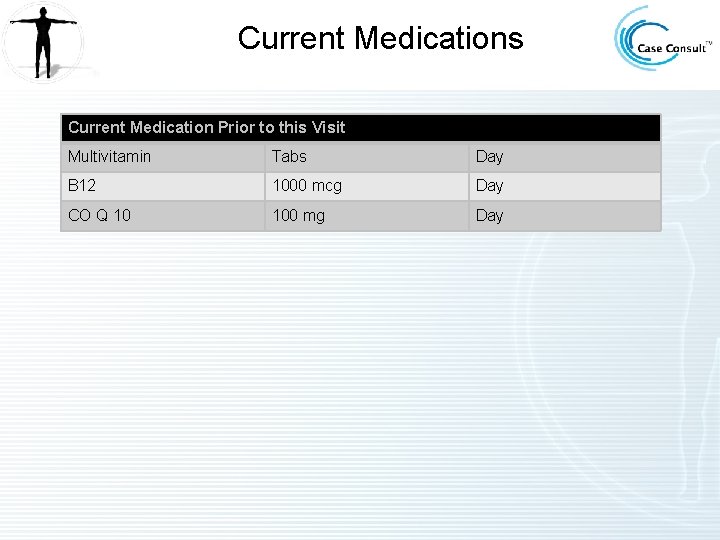
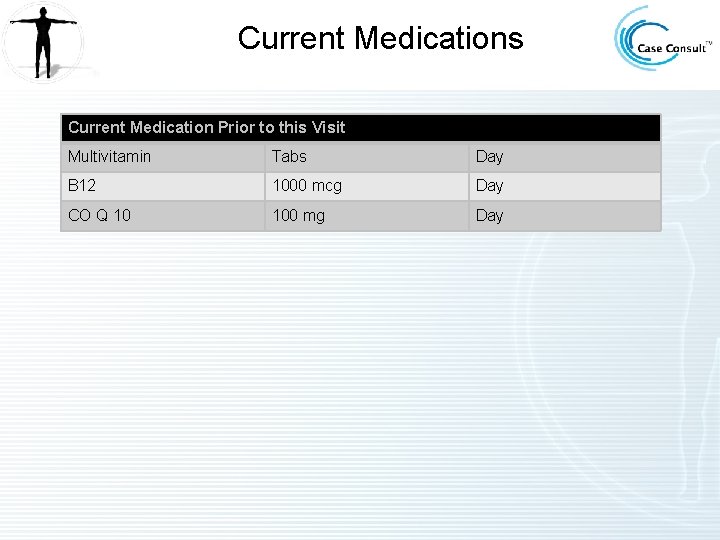
Current Medications Current Medication Prior to this Visit Multivitamin Tabs Day B 12 1000 mcg Day CO Q 10 100 mg Day
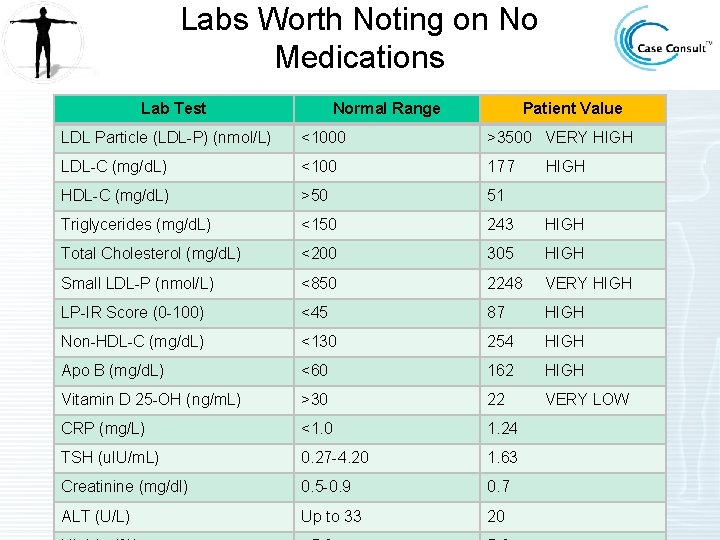
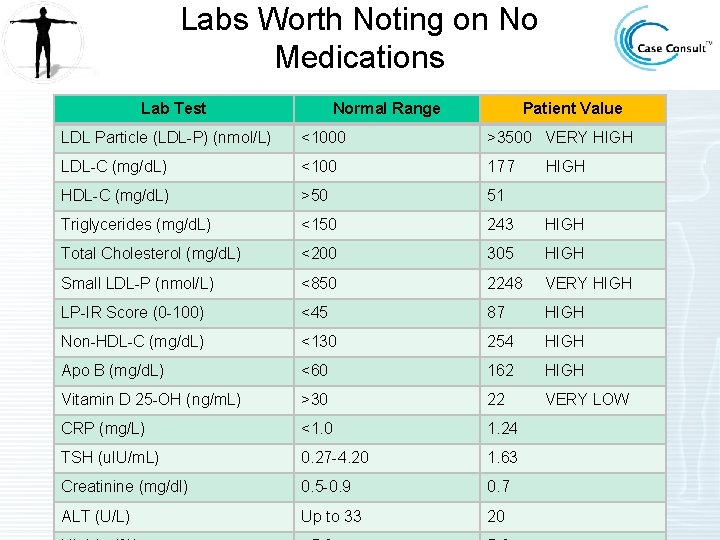
Labs Worth Noting on No Medications Lab Test Normal Range Patient Value LDL Particle (LDL-P) (nmol/L) <1000 >3500 VERY HIGH LDL-C (mg/d. L) <100 177 HDL-C (mg/d. L) >50 51 Triglycerides (mg/d. L) <150 243 HIGH Total Cholesterol (mg/d. L) <200 305 HIGH Small LDL-P (nmol/L) <850 2248 VERY HIGH LP-IR Score (0 -100) <45 87 HIGH Non-HDL-C (mg/d. L) <130 254 HIGH Apo B (mg/d. L) <60 162 HIGH Vitamin D 25 -OH (ng/m. L) >30 22 VERY LOW CRP (mg/L) <1. 0 1. 24 TSH (u. IU/m. L) 0. 27 -4. 20 1. 63 Creatinine (mg/dl) 0. 5 -0. 9 0. 7 ALT (U/L) Up to 33 20 HIGH
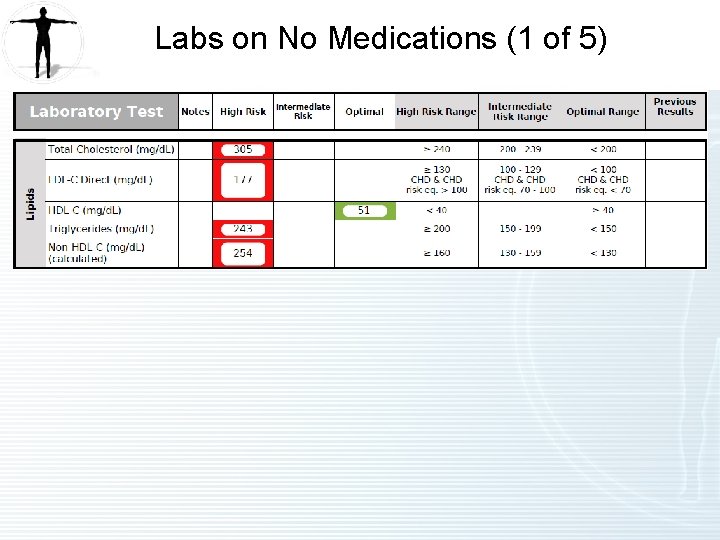
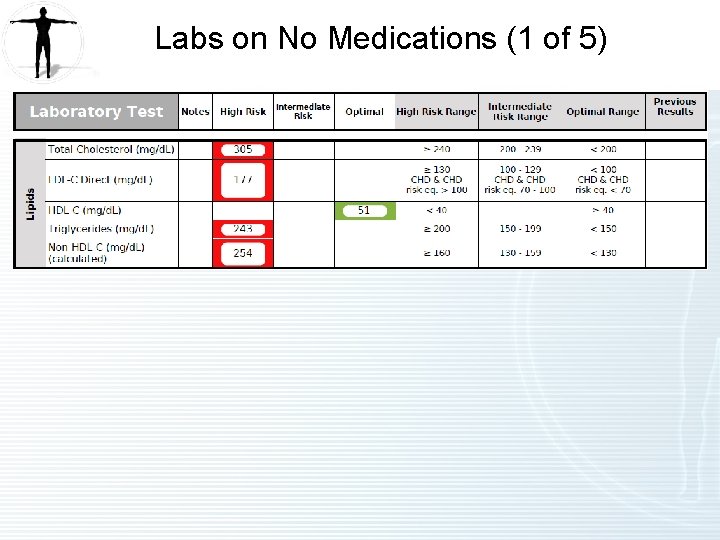
Labs on No Medications (1 of 5)
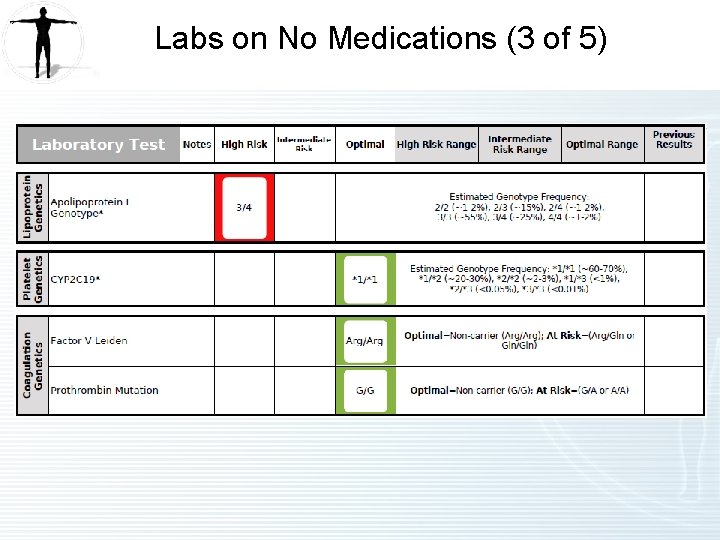
Labs on No Medications (2 of 5)
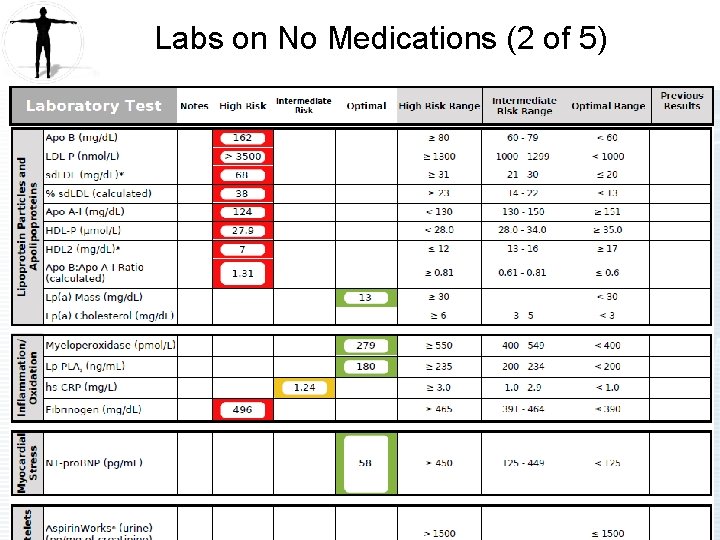
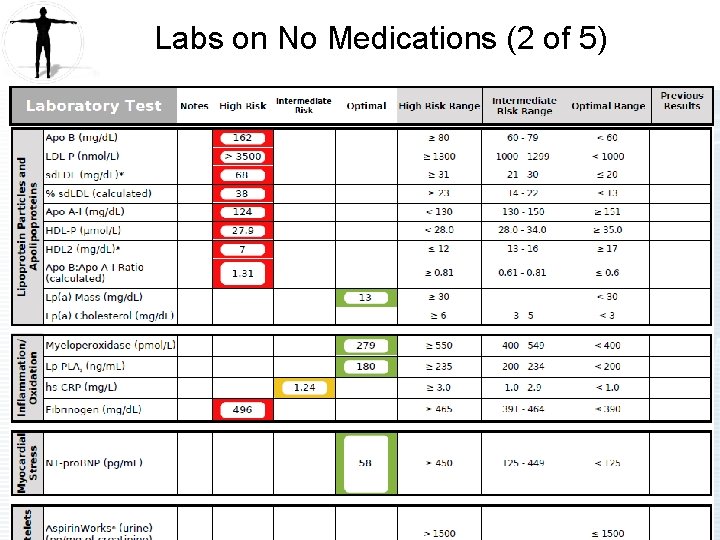
Labs on No Medications (3 of 5)
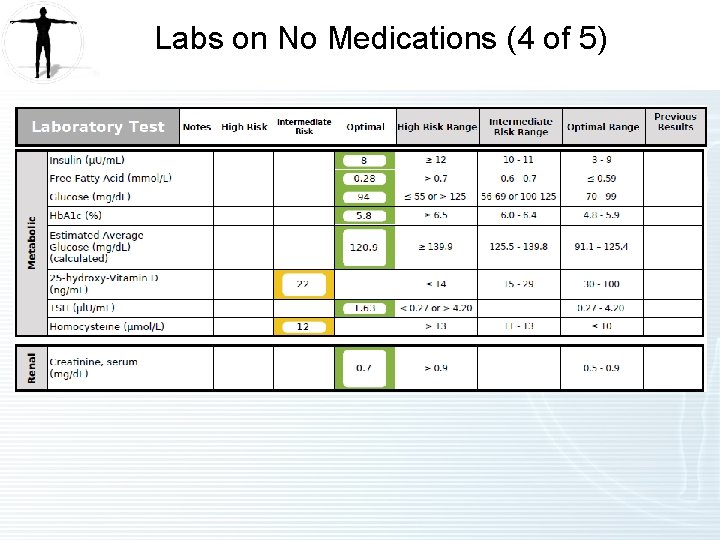
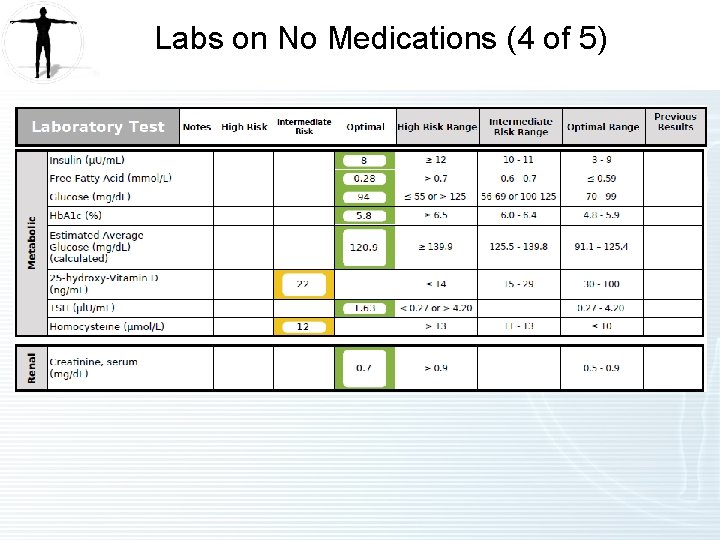
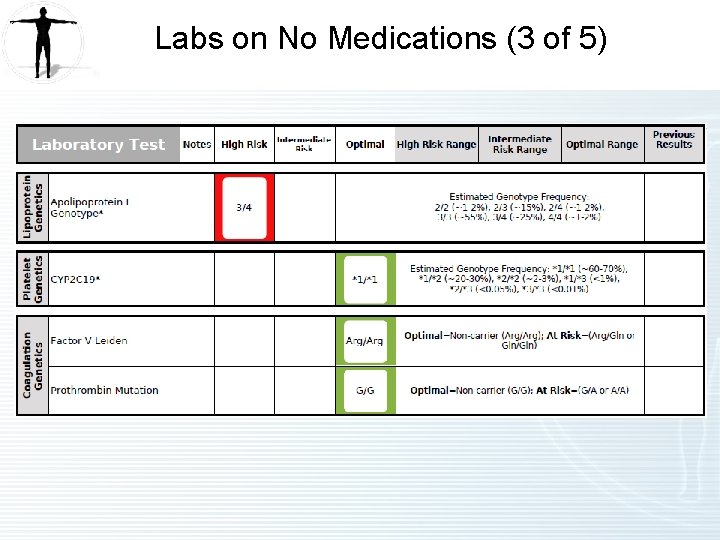
Labs on No Medications (4 of 5)
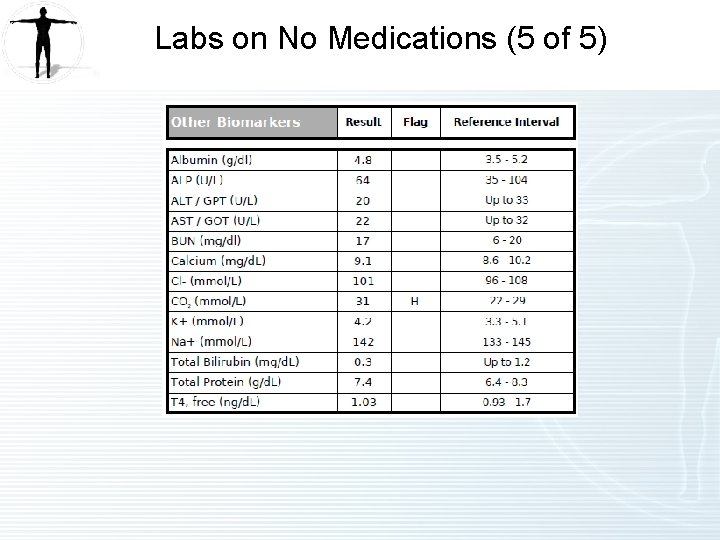
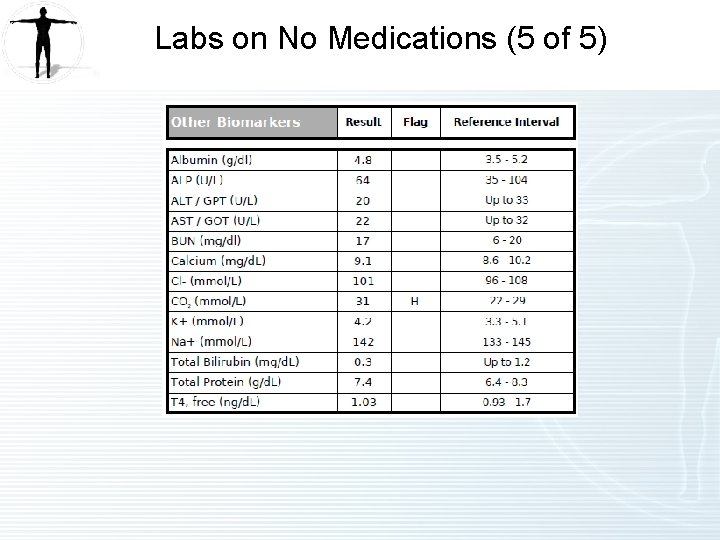
Labs on No Medications (5 of 5)
NMR Lipo. Profile • Insert NMR Lipoprofile 06072011 CC 55 Insert
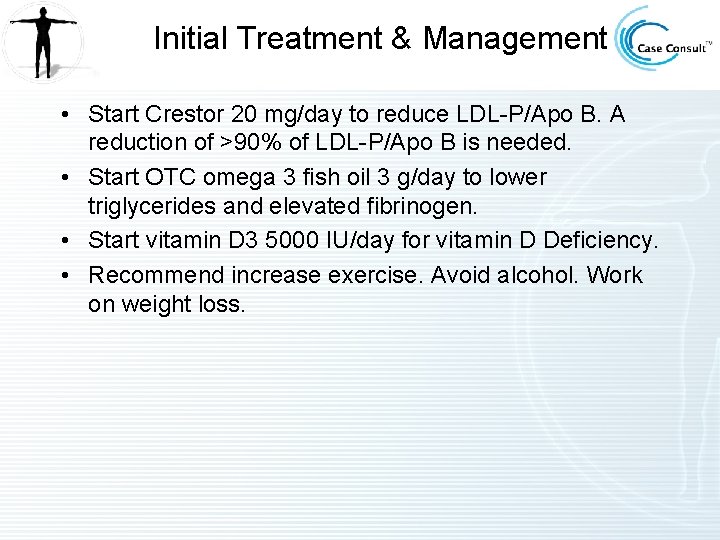
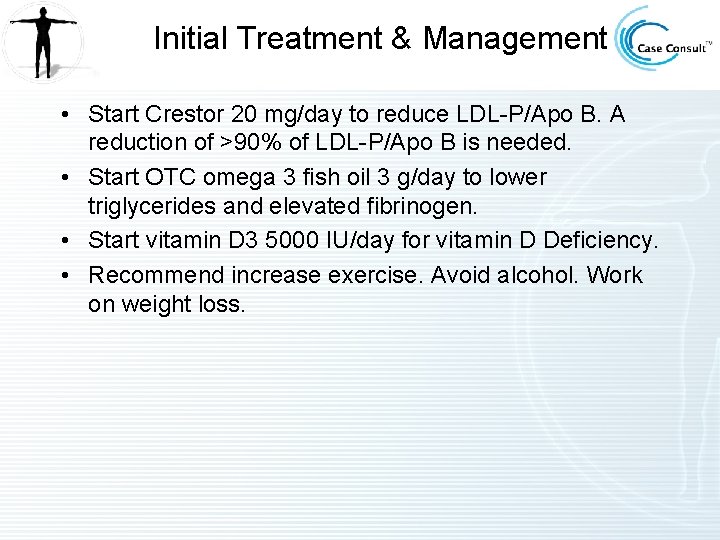
Initial Treatment & Management • Start Crestor 20 mg/day to reduce LDL-P/Apo B. A reduction of >90% of LDL-P/Apo B is needed. • Start OTC omega 3 fish oil 3 g/day to lower triglycerides and elevated fibrinogen. • Start vitamin D 3 5000 IU/day for vitamin D Deficiency. • Recommend increase exercise. Avoid alcohol. Work on weight loss.
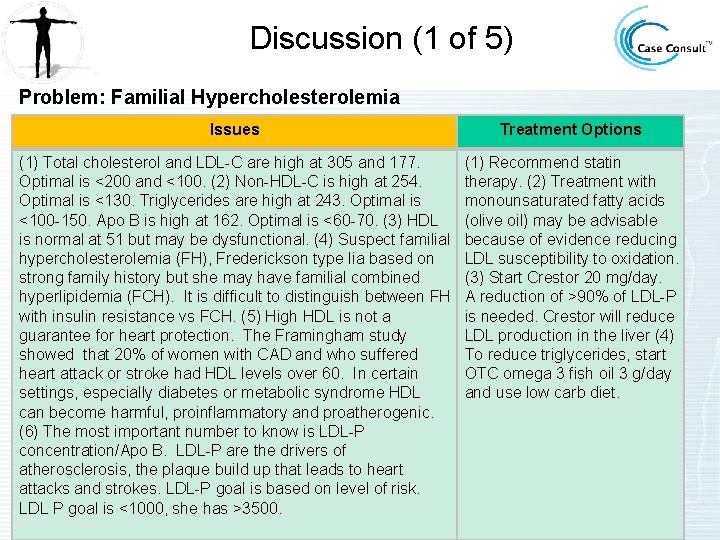
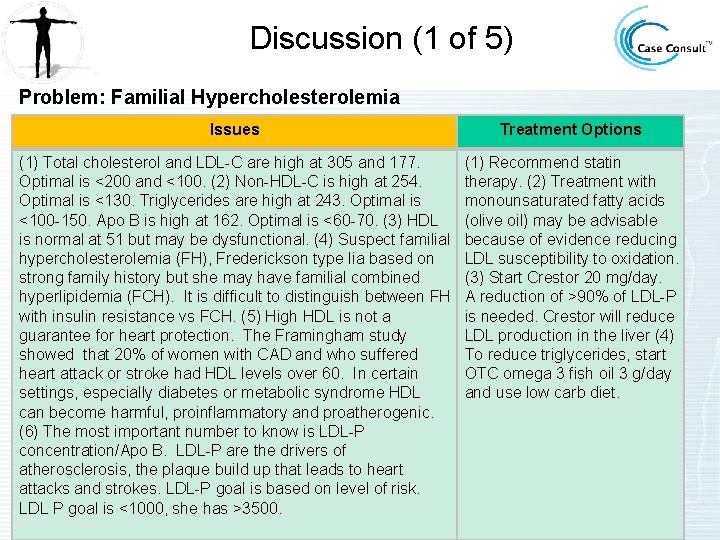
Discussion (1 of 5) Problem: Familial Hypercholesterolemia Issues Treatment Options (1) Total cholesterol and LDL-C are high at 305 and 177. Optimal is <200 and <100. (2) Non-HDL-C is high at 254. Optimal is <130. Triglycerides are high at 243. Optimal is <100 -150. Apo B is high at 162. Optimal is <60 -70. (3) HDL is normal at 51 but may be dysfunctional. (4) Suspect familial hypercholesterolemia (FH), Frederickson type Iia based on strong family history but she may have familial combined hyperlipidemia (FCH). It is difficult to distinguish between FH with insulin resistance vs FCH. (5) High HDL is not a guarantee for heart protection. The Framingham study showed that 20% of women with CAD and who suffered heart attack or stroke had HDL levels over 60. In certain settings, especially diabetes or metabolic syndrome HDL can become harmful, proinflammatory and proatherogenic. (6) The most important number to know is LDL-P concentration/Apo B. LDL-P are the drivers of atherosclerosis, the plaque build up that leads to heart attacks and strokes. LDL-P goal is based on level of risk. LDL P goal is <1000, she has >3500. (1) Recommend statin therapy. (2) Treatment with monounsaturated fatty acids (olive oil) may be advisable because of evidence reducing LDL susceptibility to oxidation. (3) Start Crestor 20 mg/day. A reduction of >90% of LDL-P is needed. Crestor will reduce LDL production in the liver (4) To reduce triglycerides, start OTC omega 3 fish oil 3 g/day and use low carb diet.
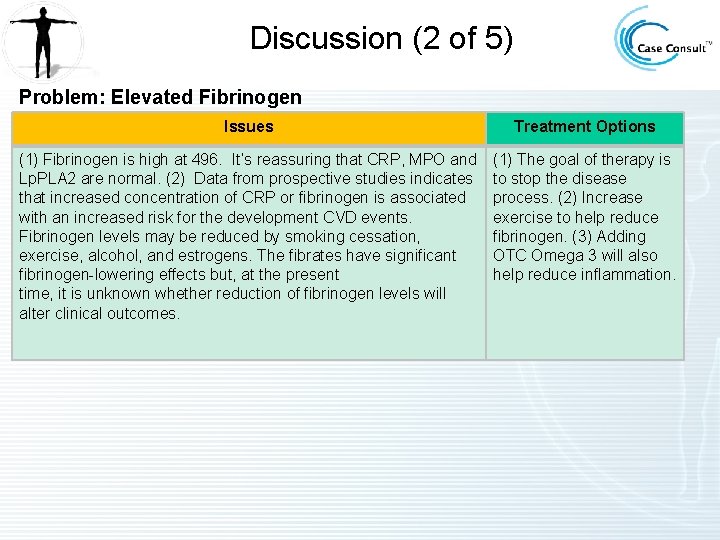
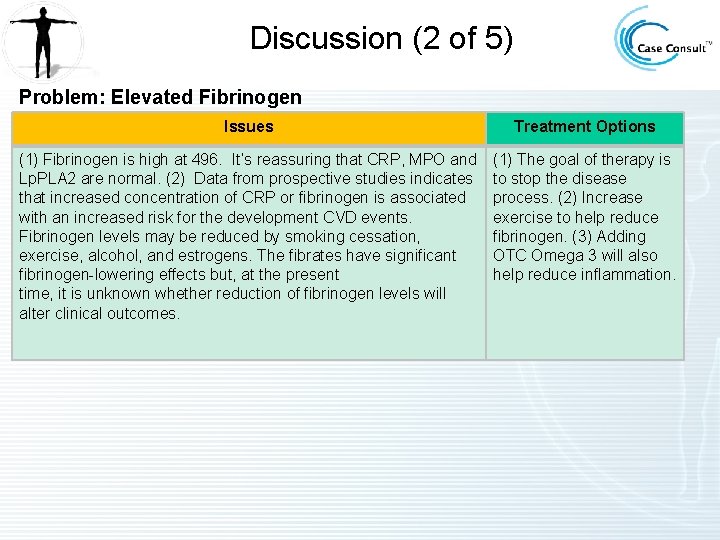
Discussion (2 of 5) Problem: Elevated Fibrinogen Issues Treatment Options (1) Fibrinogen is high at 496. It’s reassuring that CRP, MPO and Lp. PLA 2 are normal. (2) Data from prospective studies indicates that increased concentration of CRP or fibrinogen is associated with an increased risk for the development CVD events. Fibrinogen levels may be reduced by smoking cessation, exercise, alcohol, and estrogens. The fibrates have significant fibrinogen-lowering effects but, at the present time, it is unknown whether reduction of fibrinogen levels will alter clinical outcomes. (1) The goal of therapy is to stop the disease process. (2) Increase exercise to help reduce fibrinogen. (3) Adding OTC Omega 3 will also help reduce inflammation.
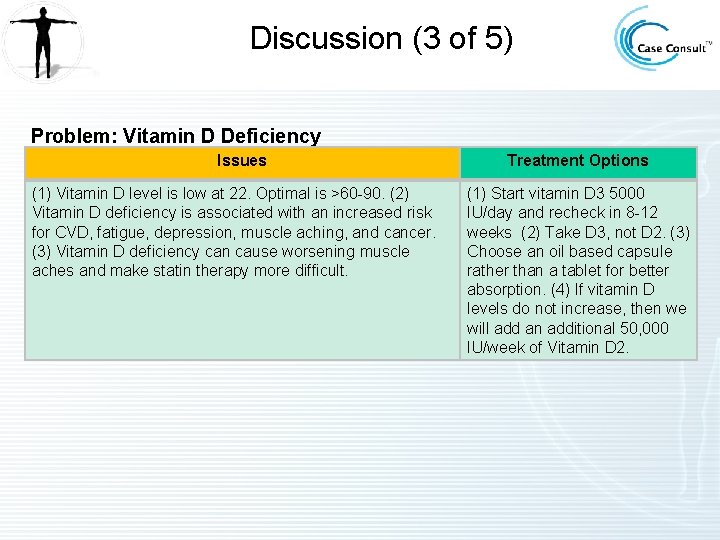
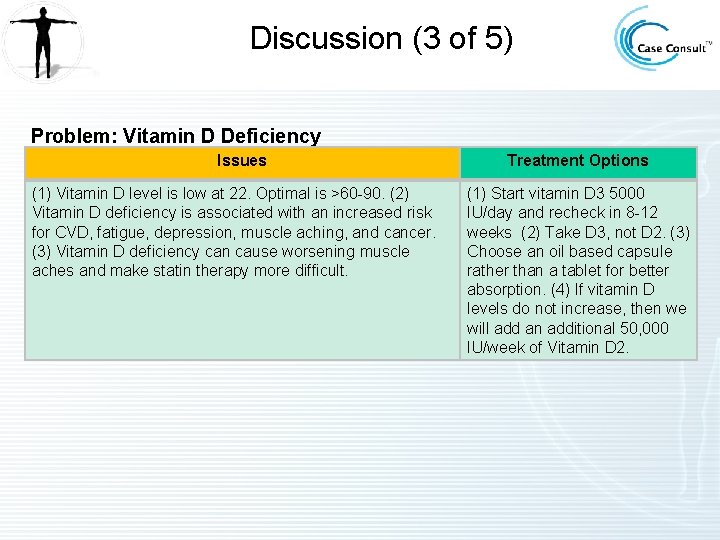
Discussion (3 of 5) Problem: Vitamin D Deficiency Issues (1) Vitamin D level is low at 22. Optimal is >60 -90. (2) Vitamin D deficiency is associated with an increased risk for CVD, fatigue, depression, muscle aching, and cancer. (3) Vitamin D deficiency can cause worsening muscle aches and make statin therapy more difficult. Treatment Options (1) Start vitamin D 3 5000 IU/day and recheck in 8 -12 weeks (2) Take D 3, not D 2. (3) Choose an oil based capsule rather than a tablet for better absorption. (4) If vitamin D levels do not increase, then we will add an additional 50, 000 IU/week of Vitamin D 2.
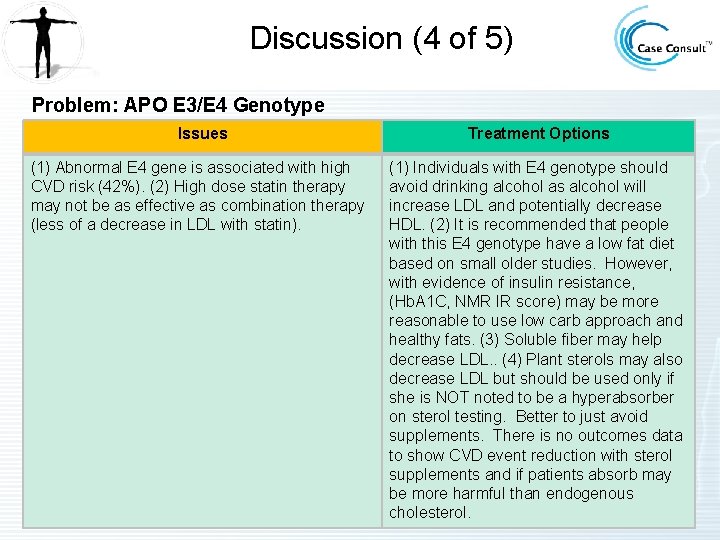
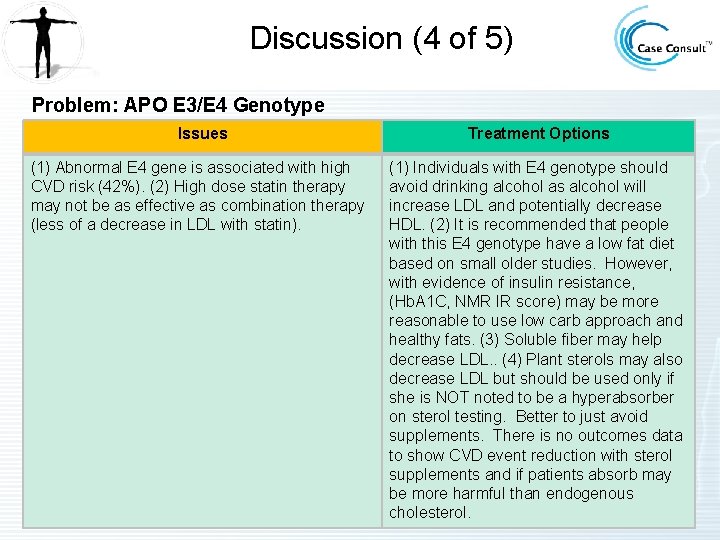
Discussion (4 of 5) Problem: APO E 3/E 4 Genotype Issues (1) Abnormal E 4 gene is associated with high CVD risk (42%). (2) High dose statin therapy may not be as effective as combination therapy (less of a decrease in LDL with statin). Treatment Options (1) Individuals with E 4 genotype should avoid drinking alcohol as alcohol will increase LDL and potentially decrease HDL. (2) It is recommended that people with this E 4 genotype have a low fat diet based on small older studies. However, with evidence of insulin resistance, (Hb. A 1 C, NMR IR score) may be more reasonable to use low carb approach and healthy fats. (3) Soluble fiber may help decrease LDL. . (4) Plant sterols may also decrease LDL but should be used only if she is NOT noted to be a hyperabsorber on sterol testing. Better to just avoid supplements. There is no outcomes data to show CVD event reduction with sterol supplements and if patients absorb may be more harmful than endogenous cholesterol.
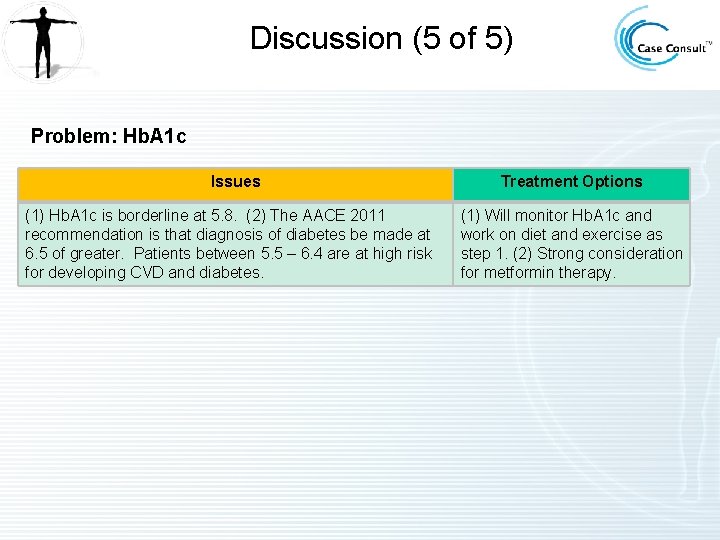
Discussion (5 of 5) Problem: Hb. A 1 c Issues (1) Hb. A 1 c is borderline at 5. 8. (2) The AACE 2011 recommendation is that diagnosis of diabetes be made at 6. 5 of greater. Patients between 5. 5 – 6. 4 are at high risk for developing CVD and diabetes. Treatment Options (1) Will monitor Hb. A 1 c and work on diet and exercise as step 1. (2) Strong consideration for metformin therapy.
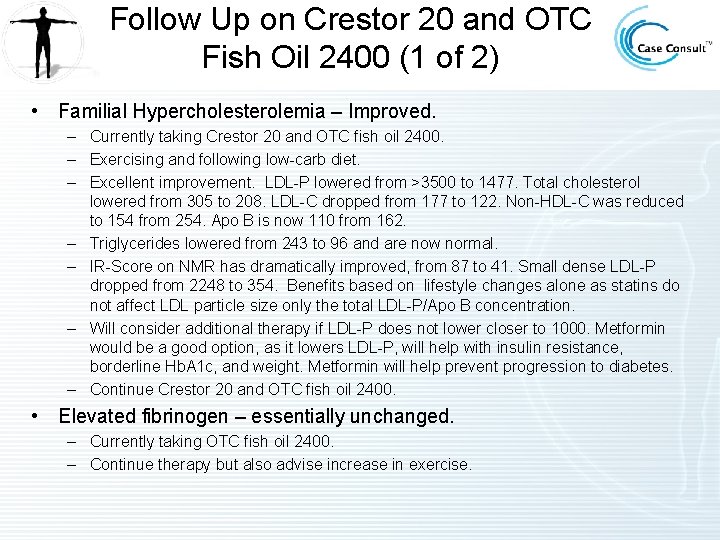
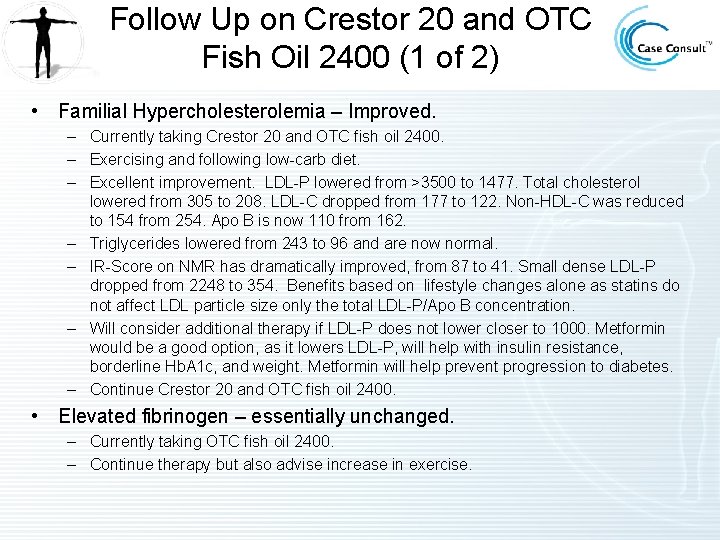
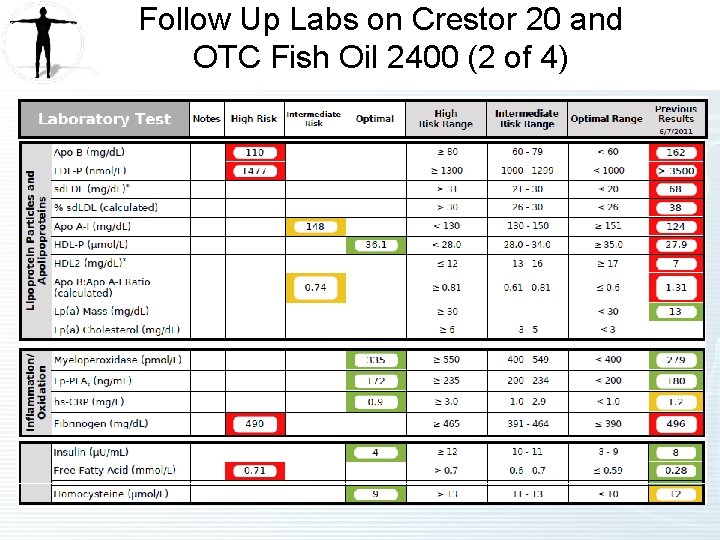
Follow Up on Crestor 20 and OTC Fish Oil 2400 (1 of 2) • Familial Hypercholesterolemia – Improved. – Currently taking Crestor 20 and OTC fish oil 2400. – Exercising and following low-carb diet. – Excellent improvement. LDL-P lowered from >3500 to 1477. Total cholesterol lowered from 305 to 208. LDL-C dropped from 177 to 122. Non-HDL-C was reduced to 154 from 254. Apo B is now 110 from 162. – Triglycerides lowered from 243 to 96 and are now normal. – IR-Score on NMR has dramatically improved, from 87 to 41. Small dense LDL-P dropped from 2248 to 354. Benefits based on lifestyle changes alone as statins do not affect LDL particle size only the total LDL-P/Apo B concentration. – Will consider additional therapy if LDL-P does not lower closer to 1000. Metformin would be a good option, as it lowers LDL-P, will help with insulin resistance, borderline Hb. A 1 c, and weight. Metformin will help prevent progression to diabetes. – Continue Crestor 20 and OTC fish oil 2400. • Elevated fibrinogen – essentially unchanged. – Currently taking OTC fish oil 2400. – Continue therapy but also advise increase in exercise.
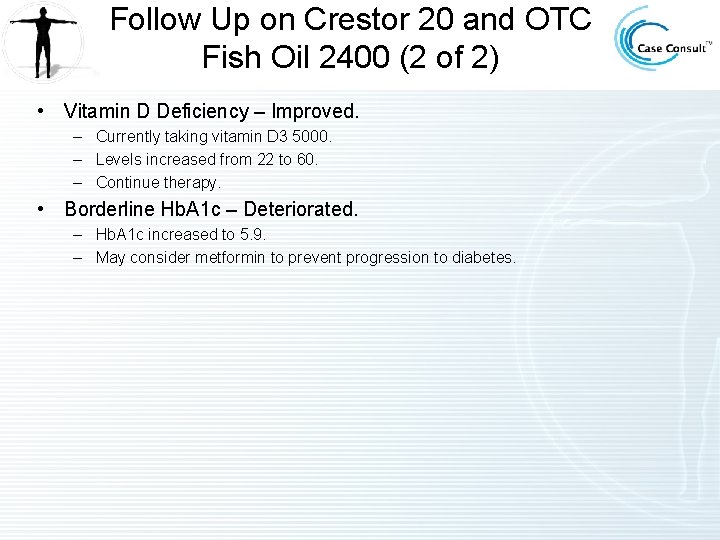
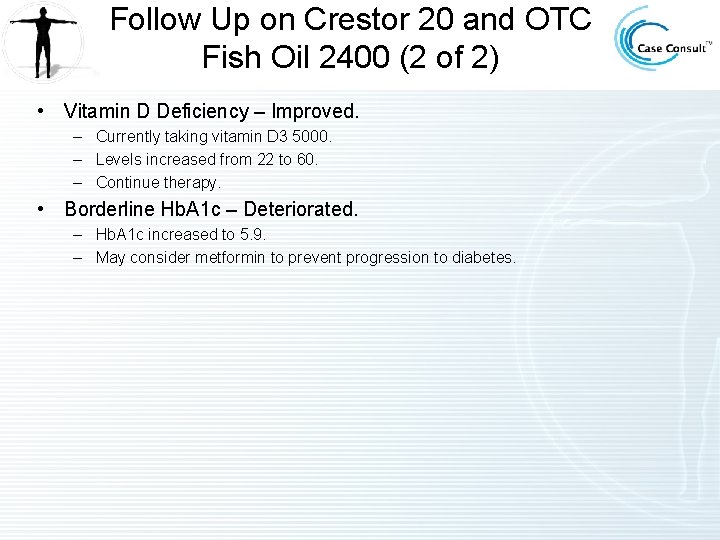
Follow Up on Crestor 20 and OTC Fish Oil 2400 (2 of 2) • Vitamin D Deficiency – Improved. – Currently taking vitamin D 3 5000. – Levels increased from 22 to 60. – Continue therapy. • Borderline Hb. A 1 c – Deteriorated. – Hb. A 1 c increased to 5. 9. – May consider metformin to prevent progression to diabetes.
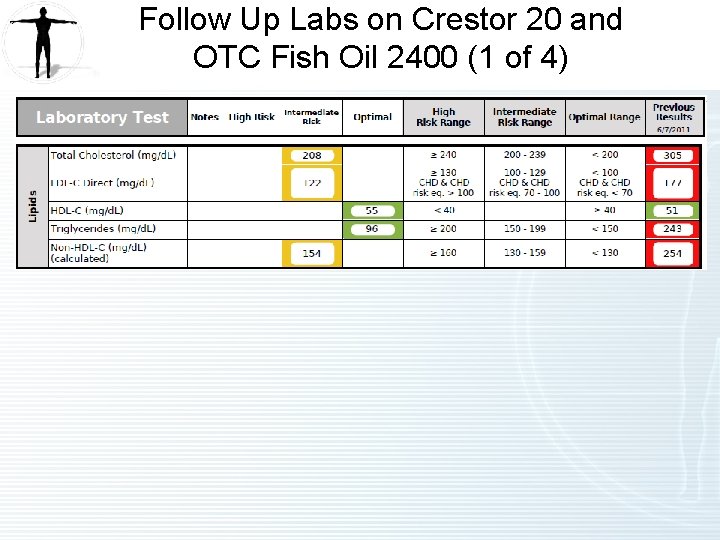
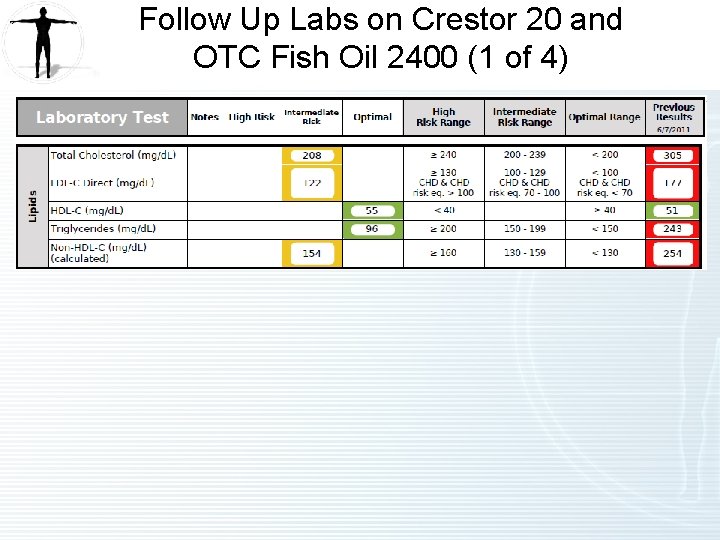
Follow Up Labs on Crestor 20 and OTC Fish Oil 2400 (1 of 4)
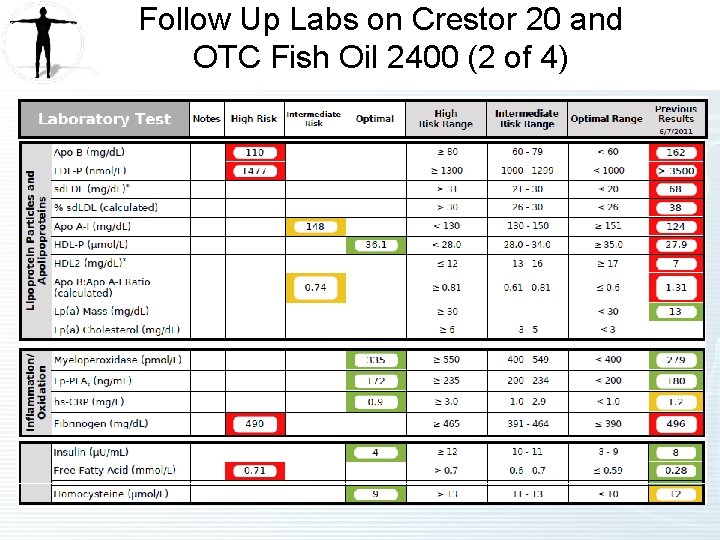
Follow Up Labs on Crestor 20 and OTC Fish Oil 2400 (2 of 4)
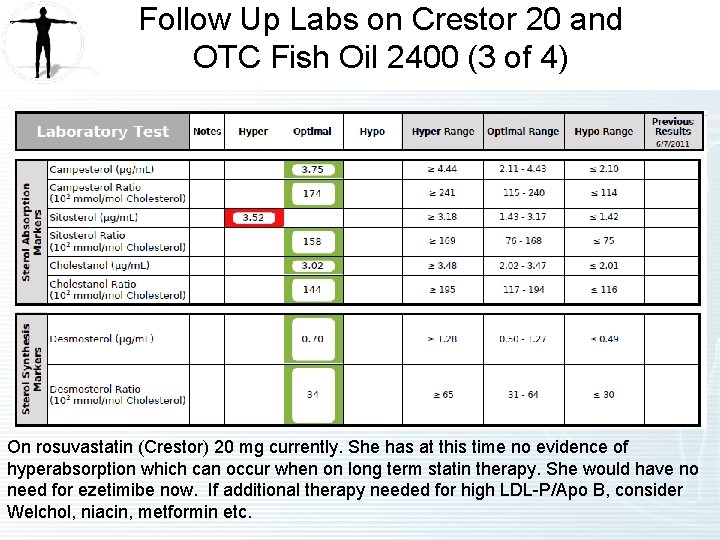
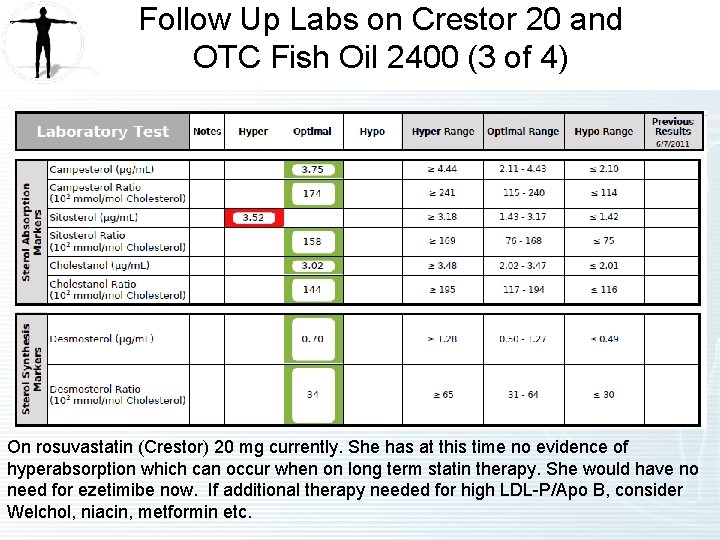
Follow Up Labs on Crestor 20 and OTC Fish Oil 2400 (3 of 4) On rosuvastatin (Crestor) 20 mg currently. She has at this time no evidence of hyperabsorption which can occur when on long term statin therapy. She would have no need for ezetimibe now. If additional therapy needed for high LDL-P/Apo B, consider Welchol, niacin, metformin etc.
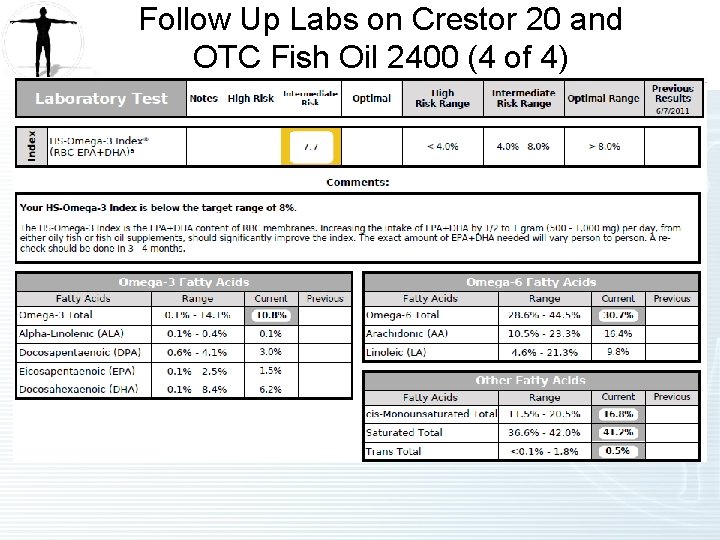
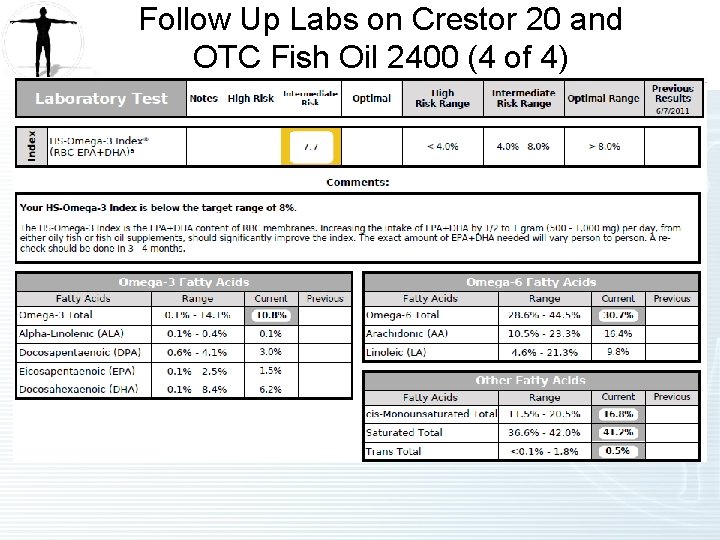
Follow Up Labs on Crestor 20 and OTC Fish Oil 2400 (4 of 4)
NMR Lipo. Profile • Insert NMR Lipoprofile 10112011 CC 55 Insert
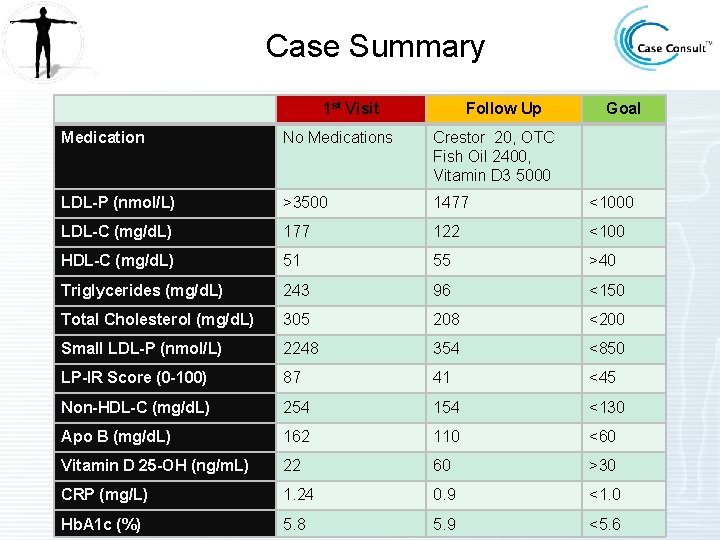
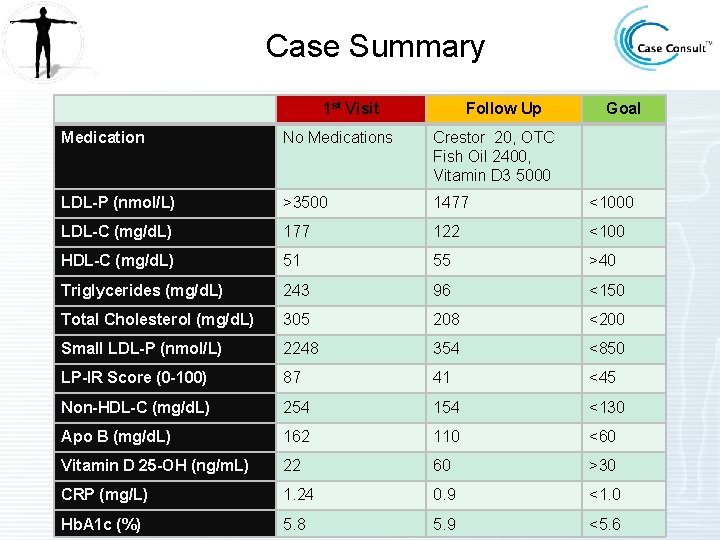
Case Summary 1 st Visit Follow Up Goal Medication No Medications Crestor 20, OTC Fish Oil 2400, Vitamin D 3 5000 LDL-P (nmol/L) >3500 1477 <1000 LDL-C (mg/d. L) 177 122 <100 HDL-C (mg/d. L) 51 55 >40 Triglycerides (mg/d. L) 243 96 <150 Total Cholesterol (mg/d. L) 305 208 <200 Small LDL-P (nmol/L) 2248 354 <850 LP-IR Score (0 -100) 87 41 <45 Non-HDL-C (mg/d. L) 254 154 <130 Apo B (mg/d. L) 162 110 <60 Vitamin D 25 -OH (ng/m. L) 22 60 >30 CRP (mg/L) 1. 24 0. 9 <1. 0 Hb. A 1 c (%) 5. 8 5. 9 <5. 6
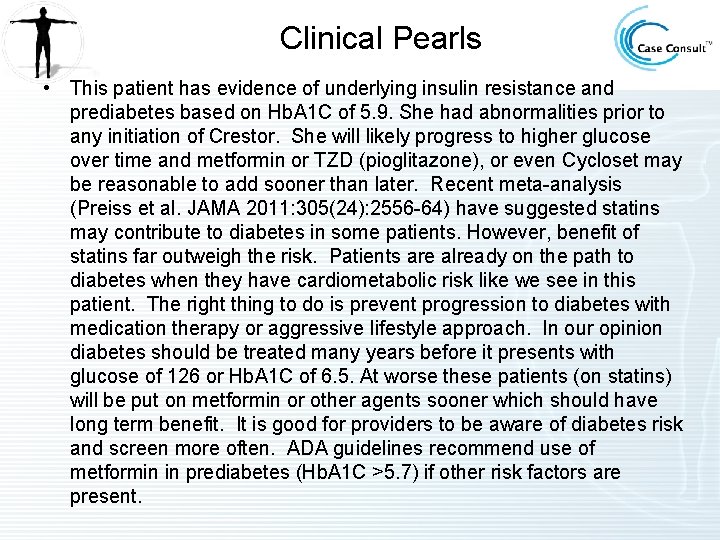
Clinical Pearls • This patient has evidence of underlying insulin resistance and prediabetes based on Hb. A 1 C of 5. 9. She had abnormalities prior to any initiation of Crestor. She will likely progress to higher glucose over time and metformin or TZD (pioglitazone), or even Cycloset may be reasonable to add sooner than later. Recent meta-analysis (Preiss et al. JAMA 2011: 305(24): 2556 -64) have suggested statins may contribute to diabetes in some patients. However, benefit of statins far outweigh the risk. Patients are already on the path to diabetes when they have cardiometabolic risk like we see in this patient. The right thing to do is prevent progression to diabetes with medication therapy or aggressive lifestyle approach. In our opinion diabetes should be treated many years before it presents with glucose of 126 or Hb. A 1 C of 6. 5. At worse these patients (on statins) will be put on metformin or other agents sooner which should have long term benefit. It is good for providers to be aware of diabetes risk and screen more often. ADA guidelines recommend use of metformin in prediabetes (Hb. A 1 C >5. 7) if other risk factors are present.

References (1 of 2) Familial Hypercholesterolemia • • Cromwell WC, Otvos JD, Keyes MJ, et al. LDL particle number and risk of future cardiovascular disease in the Framingham offspring study – implications for LDL management. J Clin Lipidol. 2007 Dec; 1(6): 583 -92. Nicholls SJ, Ballantyne CM, Barter PJ, et al. Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med. 2011 Dec 1; 365(22): 2078 -87. Roth EM, Bays HE, Forker AD, et al. Prescription omega-3 fatty acid as an adjunct to fenofibrate therapy in hypertriglyceridemic subjects. J Cardiovasc Pharmacol. Jul 10 2009. Brunzell JD, Davidson M, Furberg CD, et al. Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care. 2008 Apr; 31(4): 811 -22. Elevated Fibrinogen • Eriksson M, Egberg N, Wamala S, et al. Relationship between plasma fibrinogen and coronary heart disease in women. Arterioscler Thromb Vasc Biol. 1999 Jan; 19(1): 67 -72. .
References (2 of 2) Vitamin D Deficiency • • • Dobnig H, Pilz S, Scharnagl H, et al. Independent association of low serum 25 -hydroxyvitamin d and 1, 25 -dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008; 168(12): 1340 -1349. Giovannucci E, Liu Y, Hollis B, Rimm E. 25 -hydroxyvitamin d and risk of myocardial infarction in men. Arch Intern Med. 2008; 168(11): 1174 -1180. Michos E and Blumenthal R. Vitamin D Supplementation and Cardiovascular Disease Risk. Circulation. 2007; 115(7): 827 -828. Hathcock J, Shao A, Vieth R, et al. Risk assessment for vitamin D. Am J Clin Nutr. 2007; 85: 6 -18. Holick M. Vitamin D Deficiency. N Engl J Med. 2007; 357: 266 -81. APO E 3/E 4 Genotype • Ballantyne C, Herd JA, Stein E, et al. Apolipoprotein E genotypes and response of plasma lipids and progression-regression of coronary atherosclerosis to lipid-lowering drug therapy. J Am Coll Cardiol. 2000; 36: 1572 -8. Borderline Hb. A 1 C • • • ADA Standards of Medical Care in Diabetes - 2012. Diabetes Care. Jan 2012 35(1)11 -63. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002 Feb 7; 346(6): 393 -403. Nathan DM, Davidson M, De. Fronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. A consensus statement from the American Diabetes Association. Diabetes Care. 2007; 30: 753 -759.
 A 26 year old female presents
A 26 year old female presents Familial down syndrome
Familial down syndrome Mild hypercalcemia
Mild hypercalcemia Dr pattan casper wy
Dr pattan casper wy Monoploidy
Monoploidy Familial hypocalciuric hypercalcemia
Familial hypocalciuric hypercalcemia Edward syndrome
Edward syndrome Familial hypertriglyceridemia
Familial hypertriglyceridemia Danette format familial
Danette format familial Communauté universelle
Communauté universelle Familial roots
Familial roots Best case worst case average case
Best case worst case average case Year 6 leavers poem for teacher
Year 6 leavers poem for teacher Normal bpm for women
Normal bpm for women The great gatsby activities
The great gatsby activities 42 year old woman
42 year old woman Plep b
Plep b Average height of a 3 year old in centimeters
Average height of a 3 year old in centimeters 9-year-old physical development
9-year-old physical development Long lasting hyphen
Long lasting hyphen Average weight for 8-year-old boy
Average weight for 8-year-old boy Weight for a 11 year old
Weight for a 11 year old 9-year-old physical development
9-year-old physical development Brigance screening scoring
Brigance screening scoring Brigance calculator
Brigance calculator One year old marcus turns away in disgust
One year old marcus turns away in disgust Adhd in 3 year old
Adhd in 3 year old Five year old tammy mistakenly believes that her short
Five year old tammy mistakenly believes that her short Josef a high school student tells his therapist
Josef a high school student tells his therapist 54 year old tree trimming accident
54 year old tree trimming accident