1 Dr zohreh lavasani Ultra S onograph 48

- Slides: 46
1
Dr. zohreh lavasani Ultra S onograph 48 y In Assisted Reproducti on Obstetrics & Gynecology Department ARASH HOSPITAL l. Ian Tur-Kaspa and laurel Stadtmauer 2
3 • 1 Ultra Sonography In Assisted Reproduction INTRODUCTION 1) Ultrasound of the OVARY 2) Ultrasound of the UTERUS 3) Ultrasound of the FALLOPIAN TUBES 2 4) Ultrasound -guided IVF PROCEDURES (OR, ET) 5) Ultrasound For THE DIAGNOSIS AND TREATMENT OF ART COMPLICATIONS AND OUTCOME • CONCLUSIONS
4 Ultra Sonography In Assisted Reproduction INTRODUCTION
5 INTRODUCTION • Can we imagine assisted reproductive technique (ART) today without imaging? • Ultrasound has become the most widely used and important tool in the diagnosis and treatment of infertility. • When a patient presents with the complaint of infertility, ultrasound evaluation is one of the first steps in the evaluation of infertility.
6 INTRODUCTION • This initial ultrasound exam will immediately affect the management of the patient. • It allows us to diagnose adnexal pathology such as polycystic ovarian syndrome (PCOS), endometrioma, or other ovarian cysts, as well as hydrosalpinges. • Measuring the antral follicle count (AFC) is one of the best predictors for estimating ovarian reserve.
7 INTRODUCTION • Congenital uterine anomalies, fibroids, as well as intracavitary abnormalities may be diagnosed in the uterus. • This will be for monitoring of follicular development and endometrial response as well as ultrasound guidance for oocyte retrieval and embryo transfer (ET). • Three-dimensional (3 D) ultrasound allows better imaging as well as more accurate volume rendering.
8 INTRODUCTION • It has become a gold standard for the diagnosis of uterine anomalies and may assist in more accurate follicular monitoring measurements. • Doppler modalities of ultrasound allow identification of the direction and magnitude of blood flow and calculation of velocity.
9 Ultra Sonography In Assisted Reproduction 1 ) Ultrasound of the OVARY EVALUATION OF THE INFERTILE WOMAN AND ART ONITORING
10 1 - ULTRASOUND OF THE OVARY • Primordial follicles consist of the oocyte with a thin layer of granulosa and stromal cells, which cannot be seen on ultrasound. • The gonadotropin-dependent stage can be visualized on ultrasound. • As a follicle grows, it develops follicular fluid, which can be seen by ultrasound.
11 1 - ULTRASOUND OF THE OVARY • Antral follicles are visible and measure from 2 to 10 mm and represent the pool of follicles that may be recruited in the follicular phase for ovulation. • These follicles reach a diameter of mm 17 -24 prior to ovulation. • Ovarian flow velocity tends to increase at immediately after ovulation.
12 1 - ULTRASOUND OF THE OVARY • After ovulation a corpus luteum (CL) is frequently seen during the secretory phase of the cycle. • It is well vascularized and may have the appearance of a "ring of fire" from the vascularity as seen by power Doppler. • A normal CL has a variety of sonographic appearances.
13 1 - ULTRASOUND OF THE OVARY • Most commonly, the CL appears as a round anechoic intra ovarian or exophytic ovarian cystic mass with a homogeneous, thick, moderately echogenic wall, which may be highly vascular with a low-resistance arterial waveform.
14 1 - ULTRASOUND OF THE OVARY • CL blood flow is characterized by low impedance and high flow pattern. • Hemorrhage into a CL can create a sonographic pattern of internal echoes similar to a hemorrhagic follicular cyst and rupture of the cyst can result in hemorrhage or clot surrounding the ovary or within the peritoneal cavity.
15 1 - ULTRASOUND OF THE OVARY Ovarian Reserve
16 Ovarian Reserve • Age has a significant impact on follicle number and oocyte quality, given the women were born with a fixed number of oocytes. • The peak number of five million primordial follicles occurs prior to birth at about 20 weeks gestation, and decrease throughout life mainly by atresia.
17 Ovarian Reserve • At birth there about one million oocytes, and at puberty approximately 250, 000 oocytes. • The exponential loss of follicles accelerates at 37 -38 years (only about 25000), and leads to full depletion of the oocytes up to menopause at average of 51 years. • Retrieval of 10 -100 of oocytes with multiple IVF cycles does not seem to significantly affect this agerelated follicular loss.
18 Ovarian Reserve • Blood tests for estimating ovarian reserve include day 3 FSH and estradiol (E 2) levels as well as anti. Mullerian hormone (AMH) and inhibin B. • With ultrasound, the ovarian reserve can be assessed by measuring antral follicle counts (AFC) with or without the ovarian volumes.
19 Ovarian Reserve • AFCs are typically made by counting the number of follicles measuring 2 -10 mm in both ovaries and can be estimated by 2 D or 3 D ultrasound. • 3 D AFC is more reproducible and accurate but the method is less standardized and 3 D technology may not be freely available for all reproductive endocrinologists.
20 Ovarian Reserve • AFC of >12 is mandatory for the definition of polycystic ovaries. • Both AFC and AMH predict similarly ovarian reserve and the response to treatment, but ultrasound is the only method so far that allows a direct assessment of each ovary separately.
21 Ovarian Reserve • Pretreatment AFC and AMH were found to be the most significant predictors of the number of oocytes retrieved especially for low and high responders in multiple studies. • On the other hand, ovarian volume, vascularity, and perfusion had no significant value in predicting poor ovarian response and are inferior to AFC.
22 Ovarian Reserve • The hypothesis that aneuploidy is negatively associated with the quantity of oocytes in the ovary is poorly supported by studies showing decreased AFC in women with spontaneous abortions after IVF. • In many women with low AFC, especially at a young age, there is a decrease in quantity but not in quality of the oocytes.
23 1 - ULTRASOUND OF THE OVARY Ovarian Cysts
24 Ovarian Cysts • Ultrasound is the best method for evaluating the ovaries for cysts, and it is a mandatory step in the initial evaluation of the infertile woman. • The most common ovarian cysts seen in infertility patients are simple functional cysts, hemorrhagic cysts, endometrioma, and dermoid cysts.
25 Ovarian Cysts • Functional cysts are the most common cystic masses seen in the reproductive age group. • These cysts tend to stay less than 3 -8 cm in diameter and regress after 1 -2 cycles. • They are usually either follicular cysts or luteal cysts. • If they are small « 3 cm» and not hormonally active, they do not need to be treated before ART.
26 Ovarian Cysts • However, patients with large simple ovarian cysts may have lower response to stimulation and ovarian cyst aspiration under ultrasound guidance, with local or IV sedation, immediately prior to ovarian stimulation, has been shown to be beneficial. • An endometrioma is also a common finding in the In fertile patient and is a sign of the presence of endometriosis in other areas.
27 Ovarian Cysts • The typical endometrioma is a unilocular cyst with homogeneous low-level internal echogenicity (ground glass echogenicity) of the cyst fluid. • With respect to endometrioma, a correct diagnosis is important for infertility with possible need for ART. • Transvaginal ultrasonography is the imaging of choice to differentiate ovarian endometrioma from other adnexal masses.
28 Ovarian Cysts • IVF outcome in women with a diagnosis of ovarian endometriosis has been reduced pregnancy rates (PRs) after IVF. • Intervention studies investigating the effectiveness of laparoscopic removal of ovarian endometriosis as a tool to improve subsequent IVF results show mainly negative results.
29 Ovarian Cysts • Several reports showed that the outcome of IVF in patients previously submitted to laparoscopic stripping of endometrioma was similar to that of endometriosis-free controls. • A more recent meta-analysis showed that the outcome of IVF was similar in patients with in situ ovarian endometrioma as in endometriosis-free women and that removing endometrioma was not harmful.
30 Ovarian Cysts • If an endometrioma is seen during oocyte retrieval, it should not be aspirated as there is a high risk of ovarian infection. • Surgery pre-IVF should be considered in cases of follicle inaccessibility due to the size or position of the endometrioma.
31 Ovarian Cysts • Dermoid cysts can present as solid hyperechoic heterogeneous masses with a mixed pattern of solid and cystic areas. • They may contain calcifications, fat and hair. • They should be removed prior to IVF if they are causing pain or if there is a question of malignancy. • Puncture during oocyte retrieval should be avoided due to high risk of peritonitis.
32 1 - ULTRASOUND OF THE OVARY P oly Cystic Ovary (PCO )
33 Polycystic. Ovary (PCO) • Current data suggest that polycystic ovaries detected by TVS may be found in approximately 75% of women with a clinical diagnosis of PCOS. • However, it is not a rule that all women with polycystic ovaries will demonstrate the clinical and biochemical features of PCOS, oligomenorrhea, and/or hyperandrogenism، Polycystic ovaries per se, even without PCOS, constitute a risk factor for the development of (OHSS).
34 Polycystic. Ovary (PCO) • Transvaginal ultrasound (TVS) is a highly sensitivity method for identification of PCO and the transvaginal definition is based on the presence of >12 small follicles in a single ovary. • Comparisons between transabdominal and transvaginal ultrasound do not find significant differences in the detection rate of PCO.
35 Polycystic. Ovary (PCO) • The 3 D ultrasound and the use of color and pulsed Doppler ultrasound showing increased ovarian blood flow are techniques that further. • other imaging modality, such as (MRI) for the visualization of the ovaries are needed for the diagnosis of PCO, and should not be used as routine examination.
36 Polycystic. Ovary (PCO) • Polycystic ovaries can be established when at least one ovary demonstrates an ovarian volume of greater than 10 cm 3 or 12 or more follicles measuring 2 -9 mm in diameter (small antral follicles) arranged peripherally with a dense core of ovarian stroma. • The presence of a single polycystic ovary is sufficient to provide the diagnosis.
37 1 - ULTRASOUND OF THE OVARY Ultrasound Monitoring of Ovarian Stimulation 2 D and 3 D Sono. AVC
38 2 D and 3 D Sono. AVC • A linear relationship between follicle size and E 2 levels. • Monitoring with serial ultrasound and serum E 2 is an imperative step to reduce the risks of OHSS and multiple births. • Follicle size in 2 D is best estimated by calculating the mean of the maximum follicular diameter in three planes, but is more commonly done in two planes.
39 2 D and 3 D Sono. AVC • Follicular growth of 1 -3 mm per day is expected once the dominant follicle(s) measure greater than 12 mm. • Measuring baseline (AFC) on day 2 -3 of the cycle, before beginning ovarian stimulation, is an excellent tool to predict the ovarian response. • This can be done by 2 D or 3 D ultrasound, with or without Sono AVc.
40 2 D and 3 D Sono. AVC • A new automated ultrasound application, sonographybased Automated Volume Calculation (Sono AVC, GE medical systems) was developed to be used for follicular monitoring during controlled ovarian hyper stimulation. • The lower size limit of follicles that Sono AVC can detect is 1 -2 mm. The technique involves 3 D manipulation.
41 2 D and 3 D Sono. AVC • First, the multi planar view is used to ensure that the ovary is centrally placed and the render mode is selected to generate a 3 D volume of interest box. At this point Sono. AVC is implemented. • The individual follicles identified are then displayed with a specific color and shown together with their dimensions and relative sizes. • Post-processing is required in almost all cases to manually identify those antral follicles that have been missed in the initial automated analysis and these are easily added.
42 2 D and 3 D Sono. AVC • The total number of follicles is recorded together with the mean diameter of each follicle calculated using the relaxed sphere technique. • The volume calculation is based on a voxel count within the identified hyperechoic structure and represents a true measure of follicular volume regardless of its shape.
43 2 D and 3 D Sono. AVC • There have been studies verifying the Sono AVC technique. • Deutch et al. using an ultrasound phantom showed <0. 02 ml error comparing the spheres of known volume with a hyperechoic matrix. • Rousian et al. showed that the Sono. A VC system underestimated the volume by a mean difference of -0. 63 ml in their study, which used larger volumes of spheres than the previous study.
44 2 D and 3 D Sono. AVC • All published studies looking at correlation between the number and size of follicles in stimulated ovaries have demonstrated an excellent correlation between Sono AVC and true follicle volume showing the accuracy system for the stimulated ovary. • There is also a relationship between the follicular volume calculation and final oocyte maturation and likelihood of collecting mature eggs.
45 2 D and 3 D Sono. AVC • The advantages of Sono. A VC may be a time decrease during the ultrasound as the ovarian volumes are saved and less discomfort for the patients. • They found reduced time saving off our minutes per case after including the post-processing time. • It may also be possible to visualize the cumulus oophorus in the ovarian follicle prior to aspiration and this correlates with the number of retrieved mature oocytes.

 Zohreh zahedi
Zohreh zahedi Ab-700 ultra glide
Ab-700 ultra glide Ultra i infradźwięki
Ultra i infradźwięki Nu skin facial cleansing bar
Nu skin facial cleansing bar Feminax ultra alternative
Feminax ultra alternative Ultra vires acts of corporation
Ultra vires acts of corporation Tim koleti
Tim koleti Prefix ultra examples
Prefix ultra examples Ultra pure switch
Ultra pure switch Distancia percorrida
Distancia percorrida Ultra long duration balloon
Ultra long duration balloon Ultra violet germicidal irradiation
Ultra violet germicidal irradiation Scare repairex
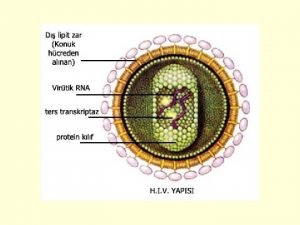
Scare repairex Vidas hiv duo ultra package insert
Vidas hiv duo ultra package insert Ultra reiz
Ultra reiz Ilimb ultra
Ilimb ultra Tt ab700
Tt ab700 Doctrine of ultra vires
Doctrine of ultra vires Nokia
Nokia Ultra vires acts of corporation
Ultra vires acts of corporation 4.jenerasyon vidas hıv duo ultra testi güvenilir mi
4.jenerasyon vidas hıv duo ultra testi güvenilir mi Ultra vires meaning
Ultra vires meaning Ultra structure of plant cell
Ultra structure of plant cell Ultra testing & research laboratory
Ultra testing & research laboratory Ultra cold
Ultra cold Feminax ultra boots
Feminax ultra boots K&s maxum ultra
K&s maxum ultra Pesquisa por imagens
Pesquisa por imagens Fungsi nukleus
Fungsi nukleus The watsons go to birmingham brown bomber
The watsons go to birmingham brown bomber Humalog mix 25 cálculo de dosis
Humalog mix 25 cálculo de dosis Linear mechanical motion
Linear mechanical motion Acn telus
Acn telus Jitter transfer function
Jitter transfer function Ultra posse nemo obligatur
Ultra posse nemo obligatur Ultra low emission burner
Ultra low emission burner Insulina glargina dosis
Insulina glargina dosis Ultra pure vodka concentrate
Ultra pure vodka concentrate Ultra eser elementler
Ultra eser elementler Analisis swot ultra milk
Analisis swot ultra milk Pio mode 4
Pio mode 4 Digital foil enhancement
Digital foil enhancement Seps/o medical term
Seps/o medical term Standard cost model
Standard cost model Great plains ultra till
Great plains ultra till Pigpen cipher
Pigpen cipher Ultra thin bonded wearing course
Ultra thin bonded wearing course