Yoke Lim ST 3 Radiology Dr Appu Rudralingam

- Slides: 16
Yoke Lim ST 3 Radiology Dr Appu Rudralingam Consultant Radiologist Dr Haider Alwan-Walker Consultant Radiologist Manchester Foundation Trust (Wythenshawe Hospital)
§ 44 years, Male § Presented with fatigue, long standing epigastric discomfort, haematemesis & melaena. § Previous pancreatitis, excessive alcohol intake (32 units/week) § Initial bloods § Hb 39, MCV 70, WCC 2. 6, Plt 187
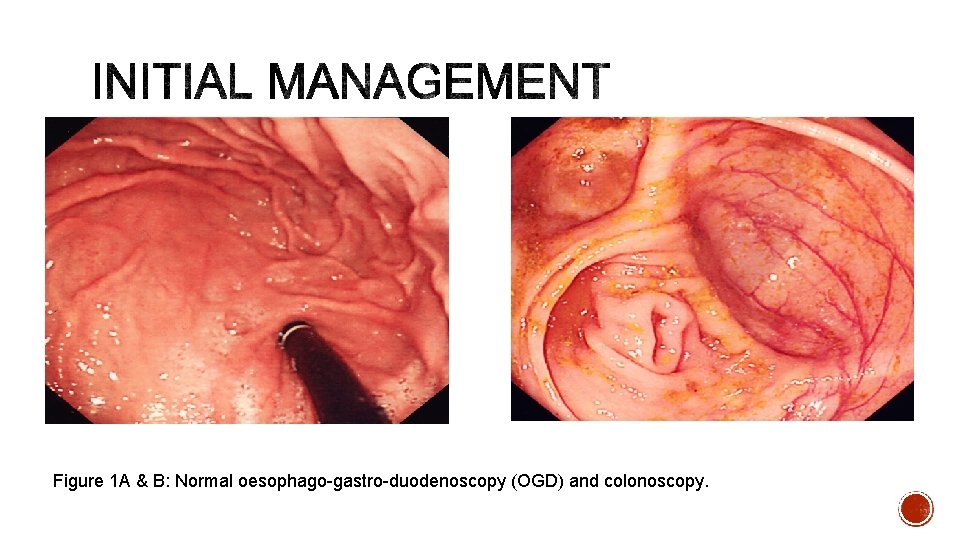
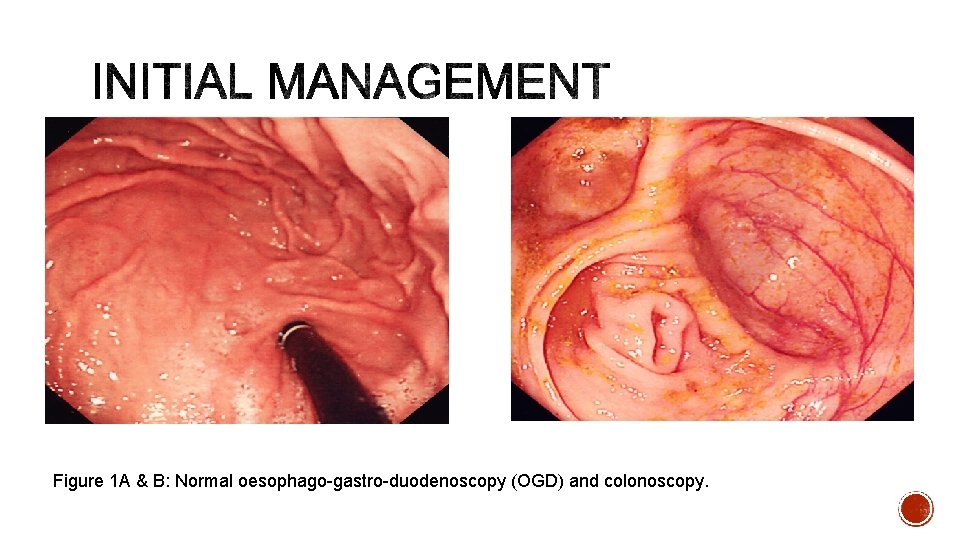
Figure 1 A & B: Normal oesophago-gastro-duodenoscopy (OGD) and colonoscopy.
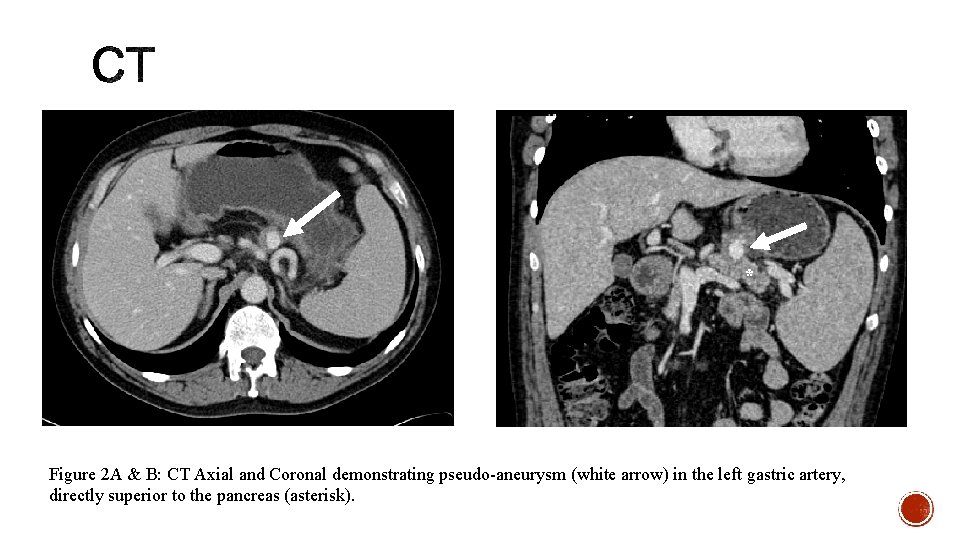
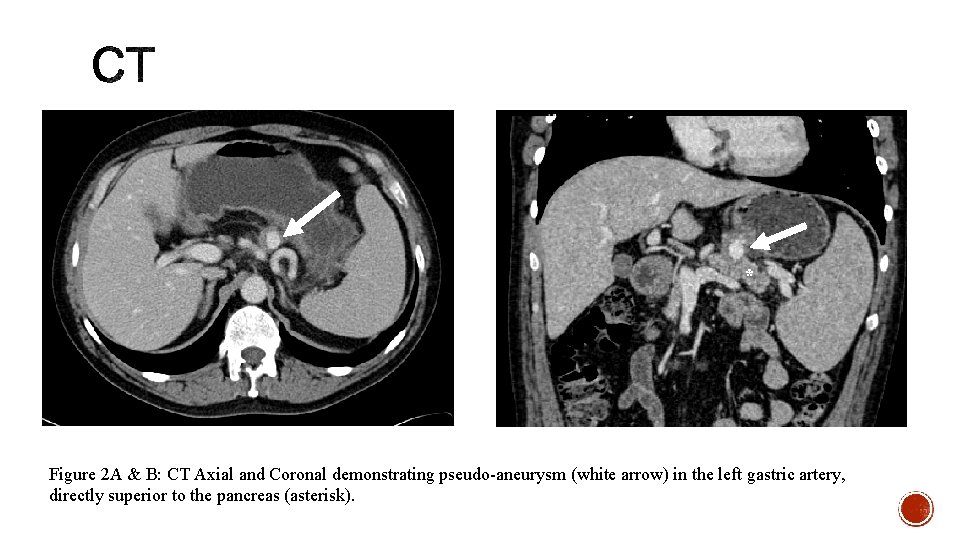
* Figure 2 A & B: CT Axial and Coronal demonstrating pseudo-aneurysm (white arrow) in the left gastric artery, directly superior to the pancreas (asterisk).
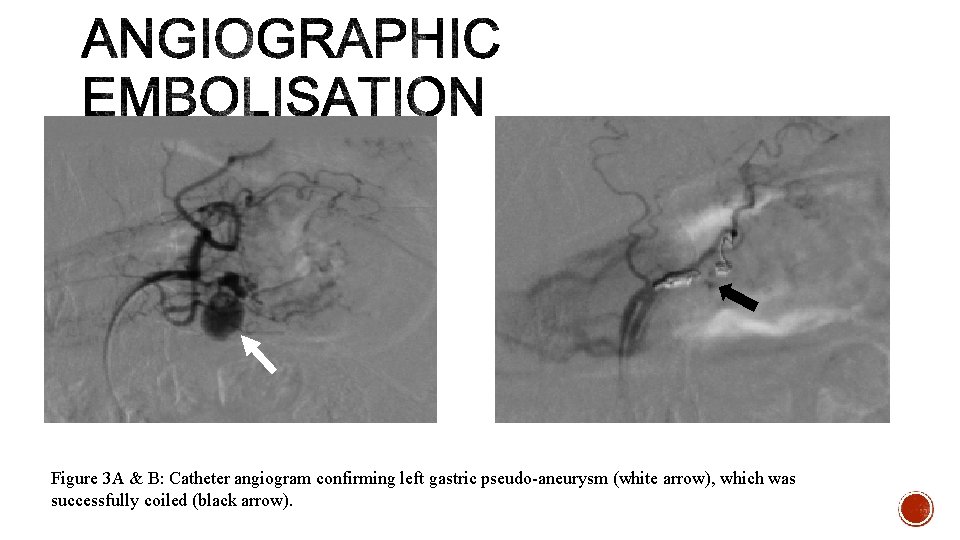
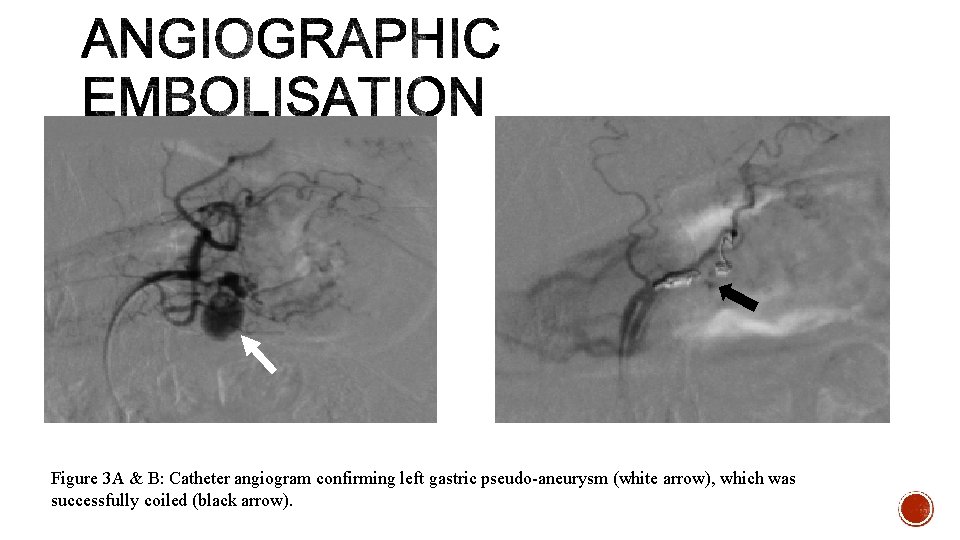
Figure 3 A & B: Catheter angiogram confirming left gastric pseudo-aneurysm (white arrow), which was successfully coiled (black arrow).
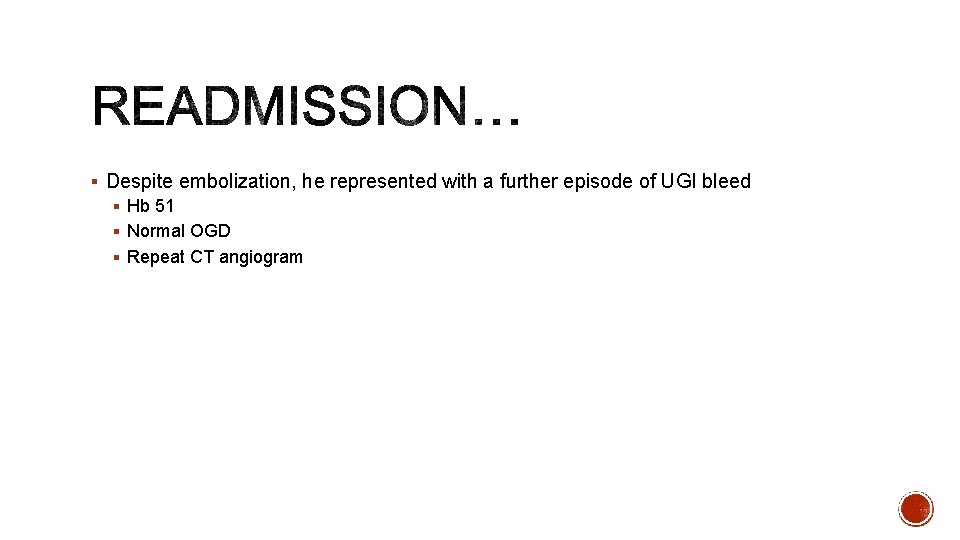
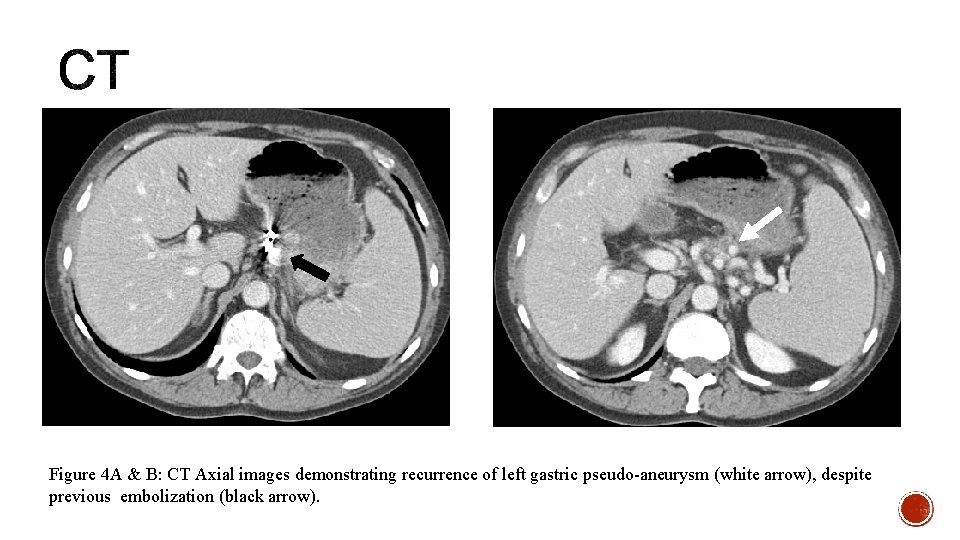
§ Despite embolization, he represented with a further episode of UGI bleed § Hb 51 § Normal OGD § Repeat CT angiogram
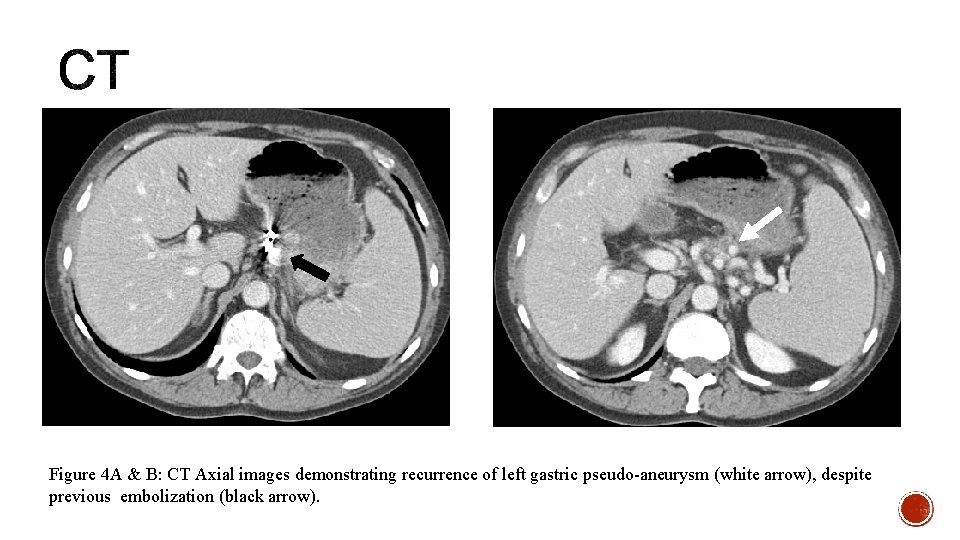
Figure 4 A & B: CT Axial images demonstrating recurrence of left gastric pseudo-aneurysm (white arrow), despite previous embolization (black arrow).
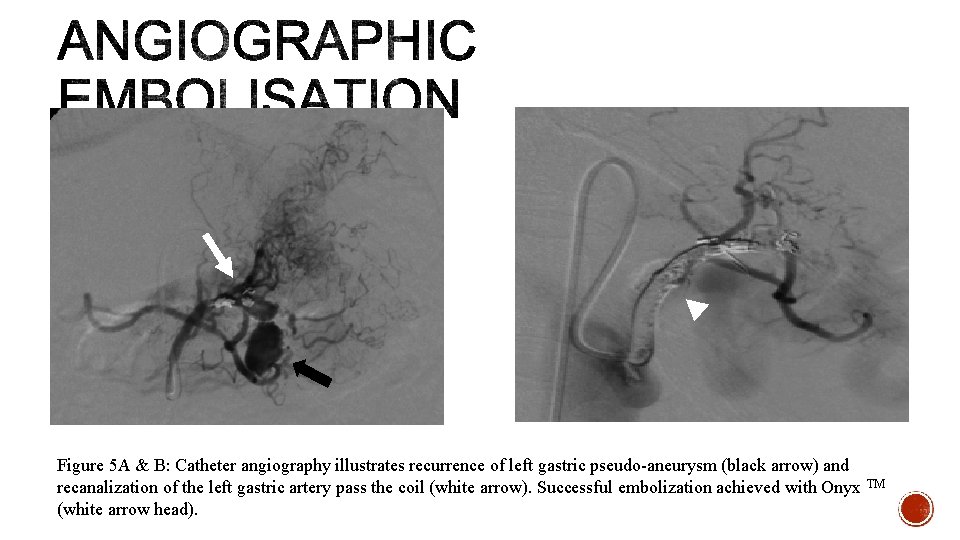
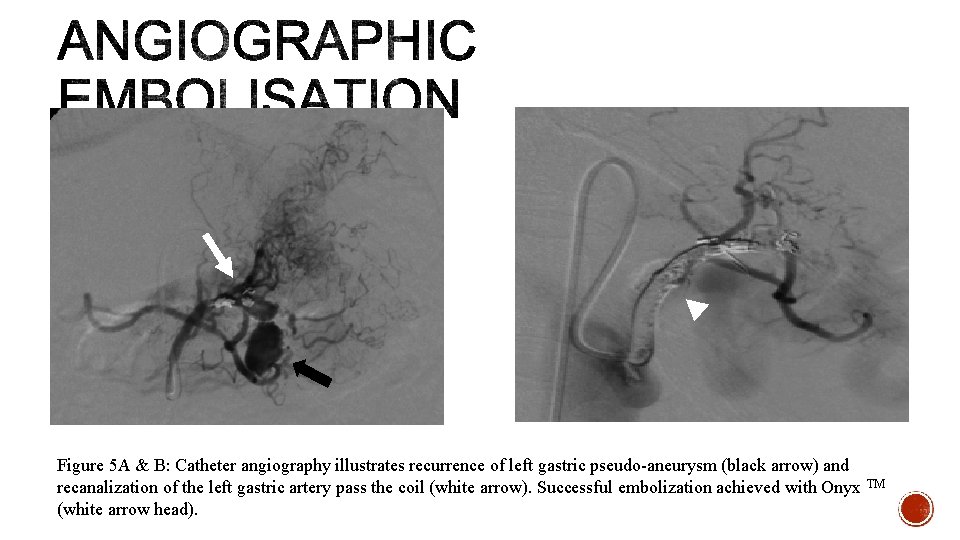
Figure 5 A & B: Catheter angiography illustrates recurrence of left gastric pseudo-aneurysm (black arrow) and recanalization of the left gastric artery pass the coil (white arrow). Successful embolization achieved with Onyx TM (white arrow head).
§ 3 months later, further admission with melaena. § Hb 74 § Normal OGD. § Tc RBC scan raises the possibility of small bowel haemorrhage. § Normal capsular endoscopy. § Decision for single balloon enteroscopy
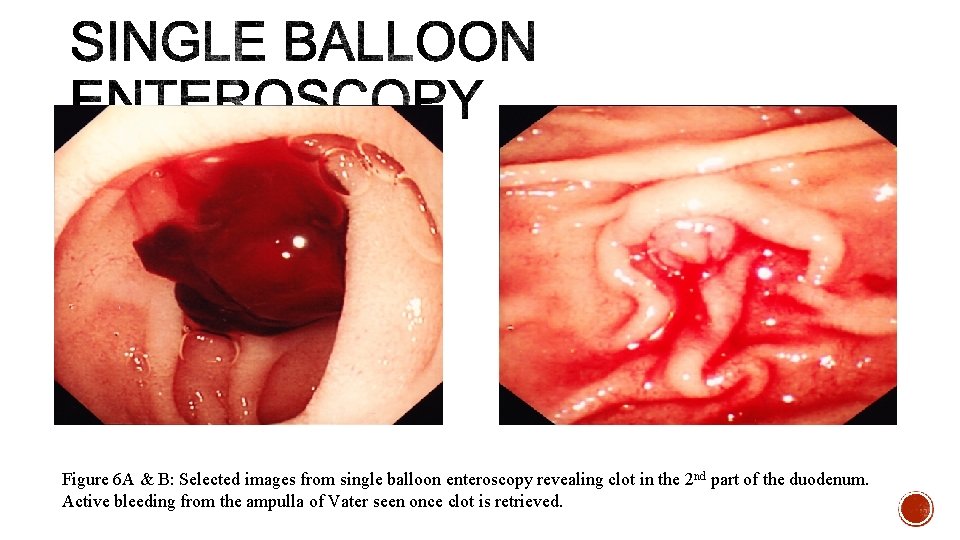
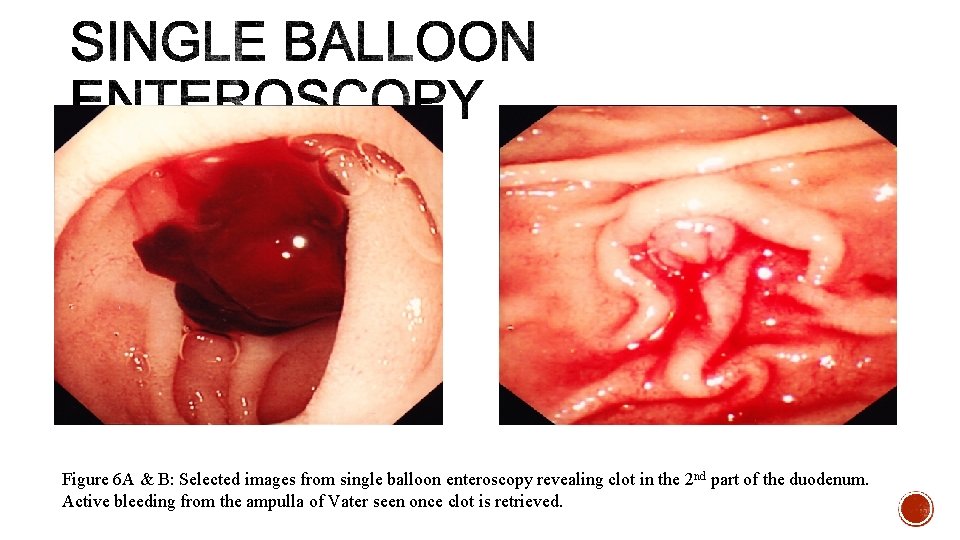
Figure 6 A & B: Selected images from single balloon enteroscopy revealing clot in the 2 nd part of the duodenum. Active bleeding from the ampulla of Vater seen once clot is retrieved.

§ Rare cause of UGI bleeding. § Bleeding from ampulla of Vater § Causes § Chronic pancreatitis – formation of pseudoaneurysm. § Vascular malformation § Pancreatic tumour § Iatrogenic/ trauma § Source of pseudoaneurysm § Splenic (40%) § Gastroduodenal (30%) § Pancreaticoduodenal (20%) § Gastric (5%) § Hepatic (2%)
§ Symptoms § Intermittent repetitive UGI bleed – difficult diagnosis § Melaena – most common § Haematemesis § Epigastric pain § Diagnosis § Clinical § Radiology § Cross sectional imaging § Cause § Acute bleeding § Angiography § Pseudoaneurysm § Endoscopy § Bleeding from ampulla of Vater § Rule out other causes of UGI bleeding
§ Management § Interventional radiology § Angiographic embolization § Immediate success rate - > 60% § Recurrence rate – 30% § Complication - ischaemia § Surgery § Unsuccessful embolization, uncontrolled haemorrhage § Other surgical indications – pseudocyst, abscess, obstructive jaundice, GO obstruction § Success rate – 70 – 85% § Rebleeding rate – < 5%
1. Haemosuccus pancreaticus is a rare cause, but an important differential for UGI bleeding. 2. Challenging diagnosis due to its intermittent nature and obscure bleeding into the main pancreatic duct. 3. Endoscopy remains the gold standard, but radiology plays an essential role in diagnosis and management.
§ Rahul Kothari et al. Hemosuccus pancreaticus: a rare cause of gastrointestinal bleeding. Ann Gastroenterol 2012; 25(4): 1 -3 § Ashwin Rammohan et al. Hemosuccus Pancreaticus: 15 -Year Experience in a Tertiary Care GI Bleed Centre. ISRN Radiology 2013
 Appu kile
Appu kile Kendriya vidyalaya lesson plan
Kendriya vidyalaya lesson plan Alwan walker
Alwan walker Appu the elephant likes guavas very much
Appu the elephant likes guavas very much Talim vositalari bu
Talim vositalari bu Buyuk didaktika tarjimasi
Buyuk didaktika tarjimasi Ananaviy talim metodlari
Ananaviy talim metodlari Corporate wars wall of influence
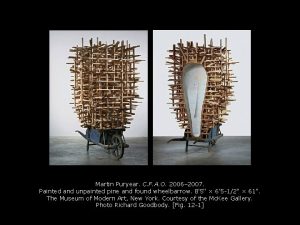
Corporate wars wall of influence Olafur eliasson the weather project
Olafur eliasson the weather project Macbeth act 4 scene 2
Macbeth act 4 scene 2 Sipoc táblázat
Sipoc táblázat Leanhuis
Leanhuis Definition of just in time
Definition of just in time Scotch yoke mechanism is the inversion of
Scotch yoke mechanism is the inversion of Poka yoke
Poka yoke Poka yoke in tqm
Poka yoke in tqm Yoke lamination
Yoke lamination