Yoke Lim ST 3 Radiology Amandeep Kahlon ST


- Slides: 15
Yoke Lim ST 3 Radiology Amandeep Kahlon ST 2 Radiology Dr Appu Rudralingam Consultant Radiologist Dr Haider Alwan-Walker Consultant Radiologist Manchester Foundation Trust (Wythenshawe Hospital)
§ 44 years, Male § Presented with fatigue, long standing epigastric discomfort, haematemesis & melaena. § Previous pancreatitis, excessive alcohol intake (32 units/week) § Initial bloods § Hb 39, MCV 70, WCC 2. 6, Plt 187

INITIAL MANAGEMENT Figure 1 A & B: Normal oesophago-gastro-duodenoscopy (OGD) and colonoscopy.
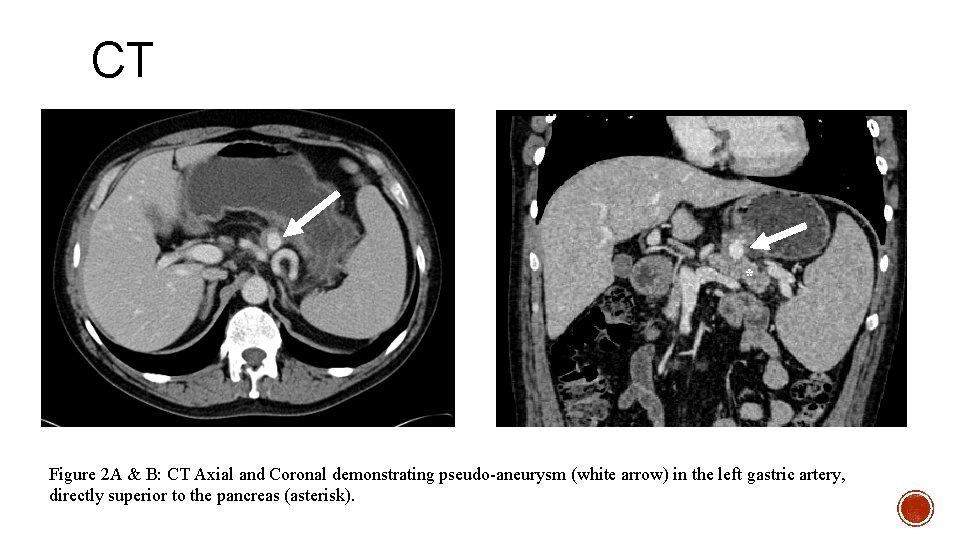
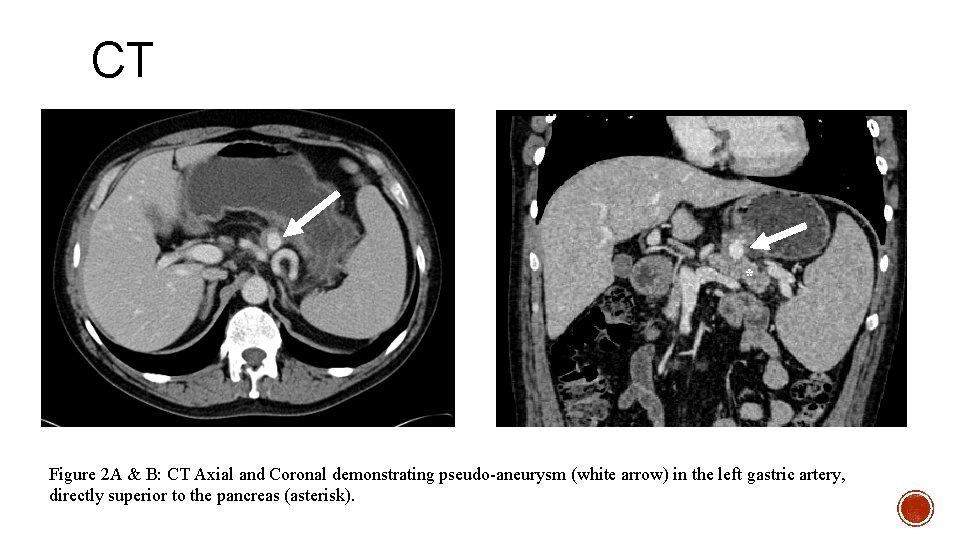
CT * Figure 2 A & B: CT Axial and Coronal demonstrating pseudo-aneurysm (white arrow) in the left gastric artery, directly superior to the pancreas (asterisk).
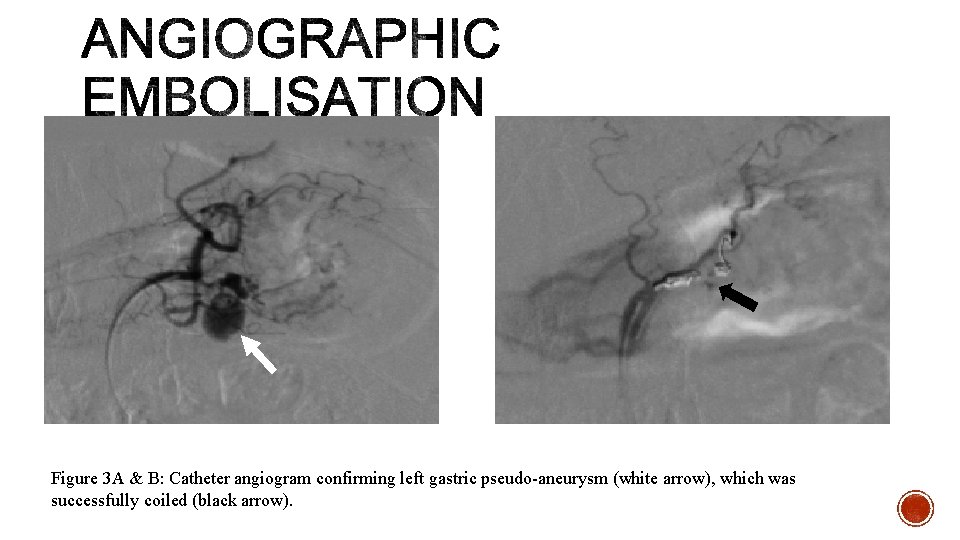
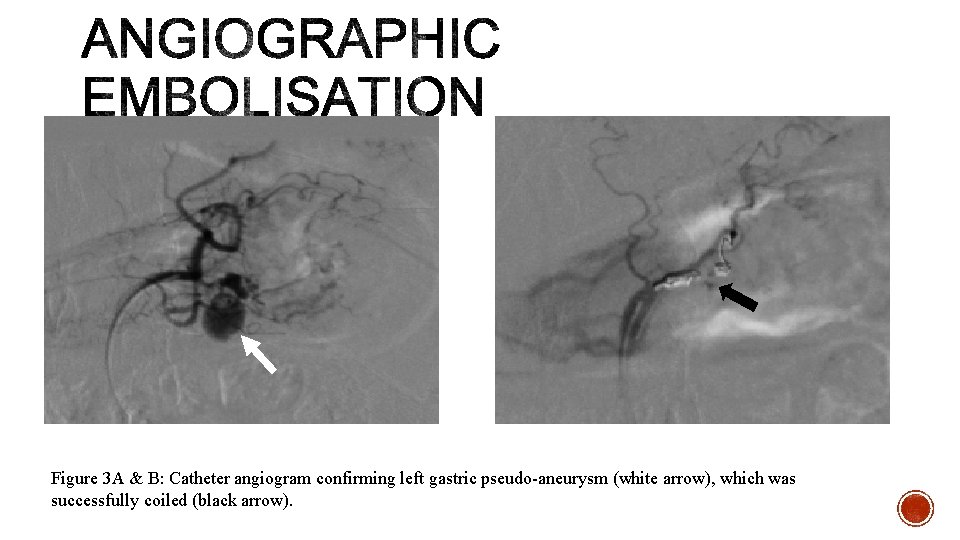
Figure 3 A & B: Catheter angiogram confirming left gastric pseudo-aneurysm (white arrow), which was successfully coiled (black arrow).
§ Despite embolization, he represented with a further episode of UGI bleed § Hb 51 § Normal OGD § Repeat CT angiogram
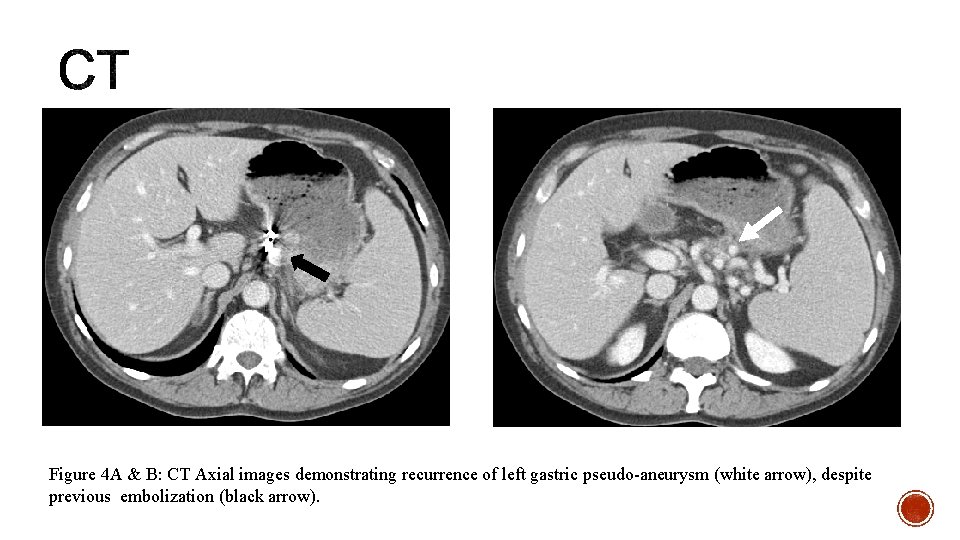
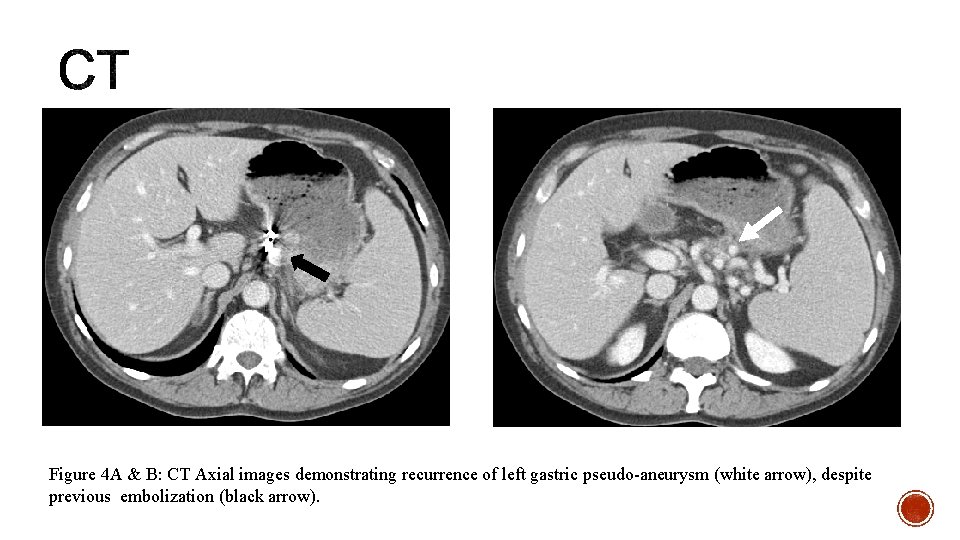
Figure 4 A & B: CT Axial images demonstrating recurrence of left gastric pseudo-aneurysm (white arrow), despite previous embolization (black arrow).
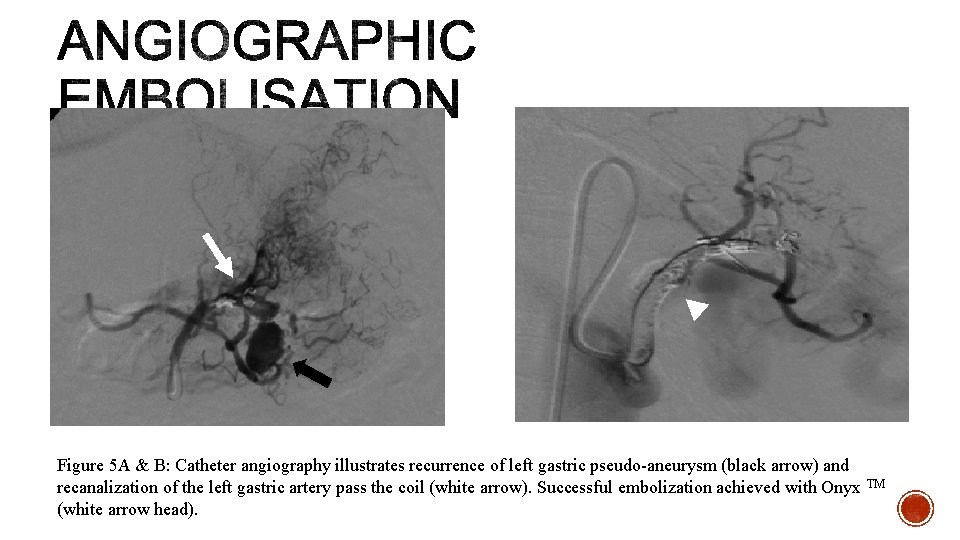
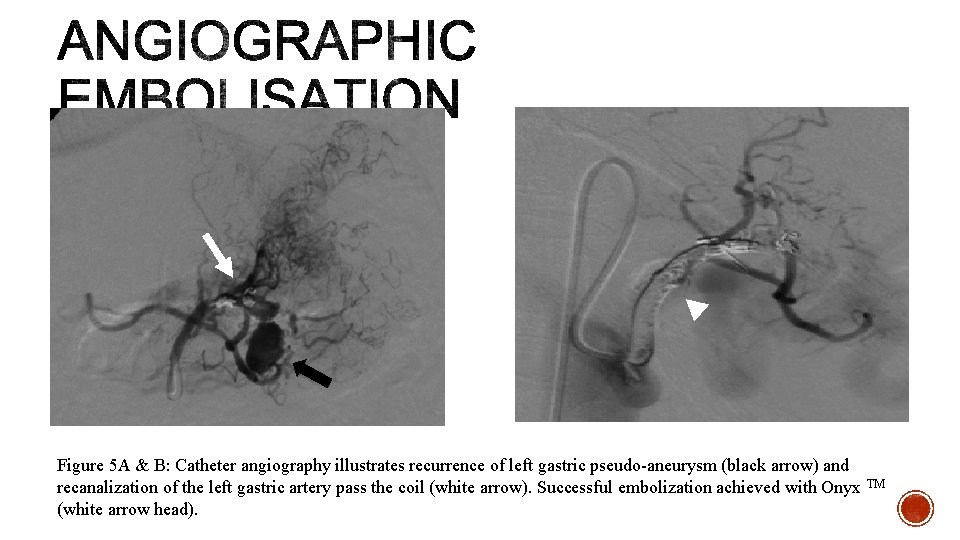
Figure 5 A & B: Catheter angiography illustrates recurrence of left gastric pseudo-aneurysm (black arrow) and recanalization of the left gastric artery pass the coil (white arrow). Successful embolization achieved with Onyx TM (white arrow head).
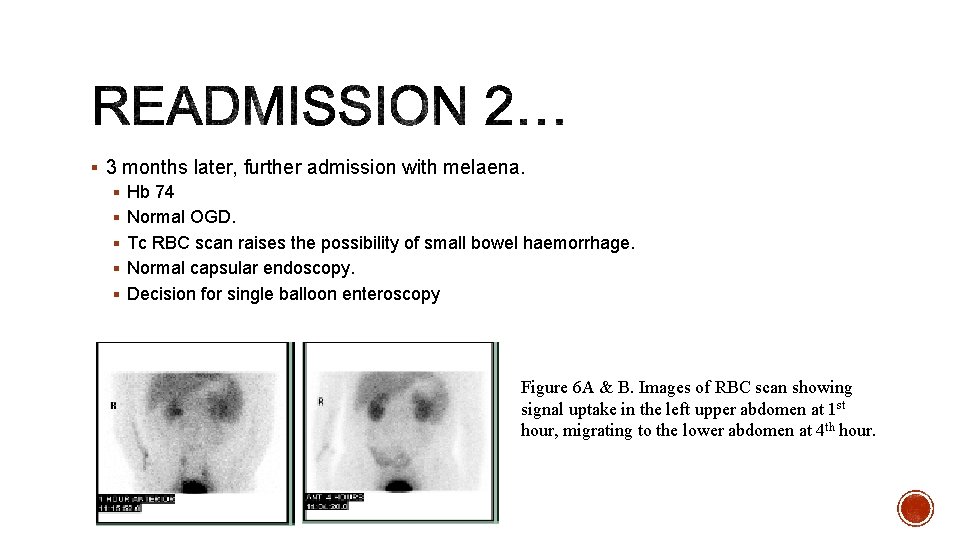
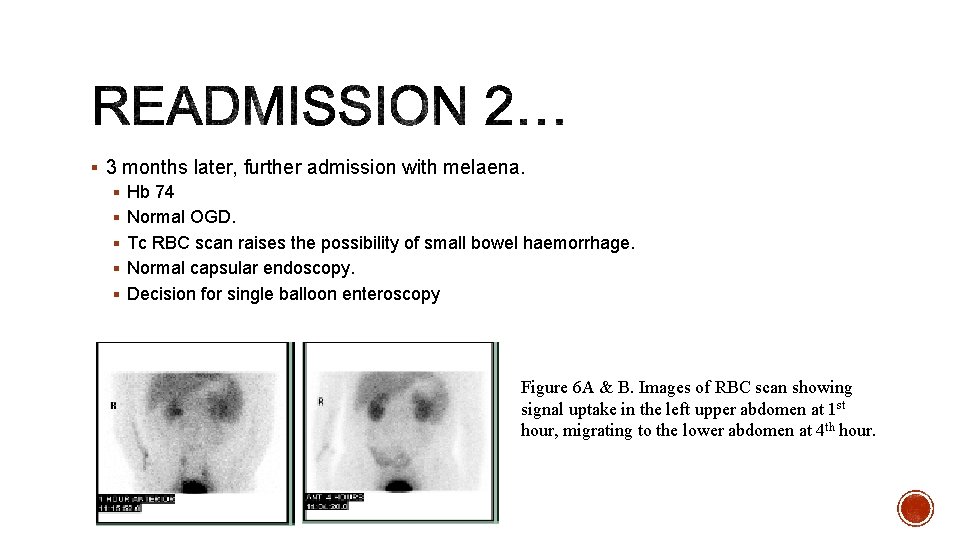
§ 3 months later, further admission with melaena. § Hb 74 § Normal OGD. § Tc RBC scan raises the possibility of small bowel haemorrhage. § Normal capsular endoscopy. § Decision for single balloon enteroscopy Figure 6 A & B. Images of RBC scan showing signal uptake in the left upper abdomen at 1 st hour, migrating to the lower abdomen at 4 th hour.
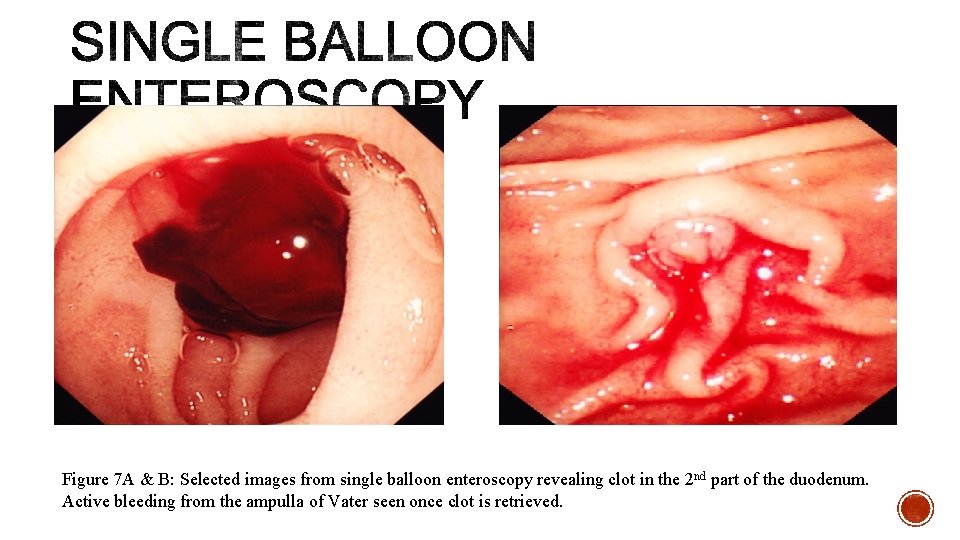
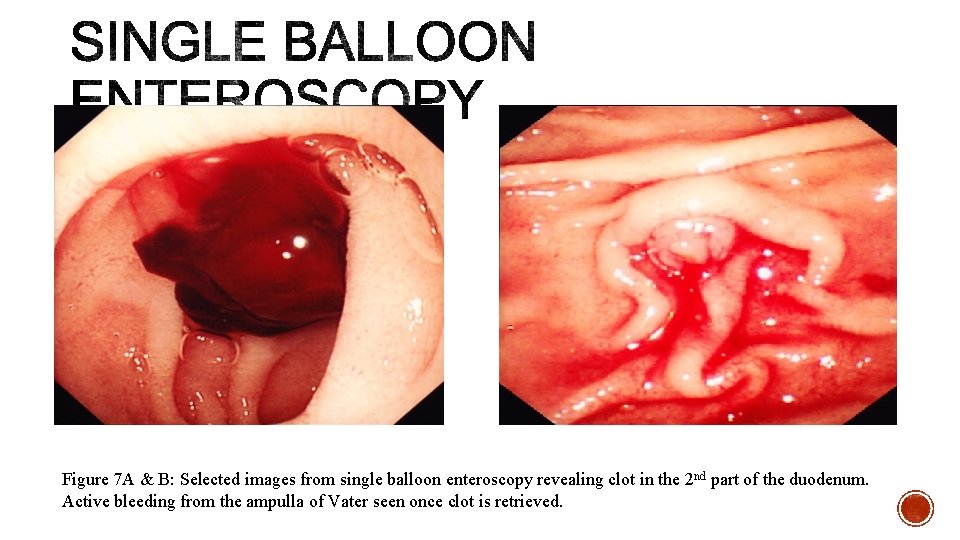
Figure 7 A & B: Selected images from single balloon enteroscopy revealing clot in the 2 nd part of the duodenum. Active bleeding from the ampulla of Vater seen once clot is retrieved.
§ Bleeding from ampulla of Vater § Causes § Chronic pancreatitis –pseudoaneurysm. § Vascular malformation § Pancreatic tumour § Iatrogenic § Source of pseudoaneurysm § Splenic (40%) § Gastroduodenal (30%) § Pancreaticoduodenal (20%)
§ Symptoms § Intermittent repetitive UGI bleed – difficult diagnosis § Melaena – most common § Haematemesis § Epigastric pain § Diagnosis § Clinical § Radiology § Cross sectional imaging § Angiography § Endoscopy § Bleeding from ampulla of Vater
§ Management § Interventional radiology § Angiographic embolization § Immediate success rate - > 60% § Recurrence rate – 30% § Surgery § Unsuccessful embolization § Success rate – 70 – 85% § Rebleeding rate – < 5%

1. Haemosuccus pancreaticus is a rare cause, but an important differential for UGI bleeding. 2. Challenging diagnosis due to its intermittent nature and obscure bleeding into the main pancreatic duct. 3. Endoscopy remains the gold standard, but radiology plays an essential role in diagnosis and management.
 Dr randeep kahlon
Dr randeep kahlon Ta'limning binar metodi
Ta'limning binar metodi Ta'lim vositalari turlari
Ta'lim vositalari turlari Ditaktika nima
Ditaktika nima Link 25 system
Link 25 system Poka yoke presentation
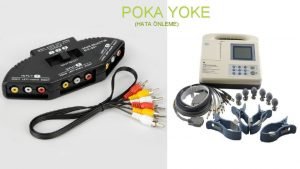
Poka yoke presentation Poka-yoke exemple
Poka-yoke exemple Kutzbach equation
Kutzbach equation Sipoc táblázat
Sipoc táblázat Take my yoke
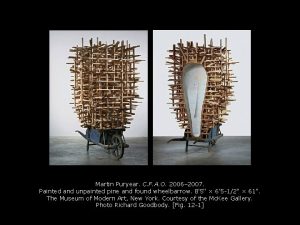
Take my yoke Ballplayer with three-part yoke and bird headdress
Ballplayer with three-part yoke and bird headdress Ballplayer with three-part yoke and bird headdress
Ballplayer with three-part yoke and bird headdress Act 4 scene 1 macbeth analysis
Act 4 scene 1 macbeth analysis Leanhuis
Leanhuis Elements of iso 9000:2000
Elements of iso 9000:2000 Poka yoke in tqm
Poka yoke in tqm