Welcome Please place your phone on mute Safety


- Slides: 41

• Welcome! • Please place your phone on mute Safety Tools, Safety Coaching, and More! Ilana Cabrera, MSN, RN, CPNP, Clinical Practice Leader Christine Lutze, BSN, RN, Patient Safety Specialist With special guest Gena Melang, ADN, RN, CLC 1
Disclosure Information • There are no relevant financial relationships related to this presentation/program. • There is no sponsorship/commercial support of this presentation/program. • The content being presented will be fair, well-balanced, and evidence-based.
Objectives After today’s webinar, the learner will be able to: • Describe Solutions for Patient Safety • Identify safety tools, behaviors, and resources that help to facilitate a safe culture. 3
Solutions for Patient Safety (SPS) History • Eight Ohio children’s hospitals started SPS in 2009 to improve quality and reduce cost. • They instituted bundles (checklists) and high reliability concepts. • Within 2 years, they saw: § 60% fewer surgical site infections § 40% fewer adverse drug events § Savings of $11. 8 million in unnecessary costs 4
Solutions for Patient Safety • The SPS Network now includes more than 150 children’s hospitals across the country. • Over 50% of all U. S. pediatric admissions are in these hospitals. • Children’s Hospital of Wisconsin joined SPS in 2012. 5
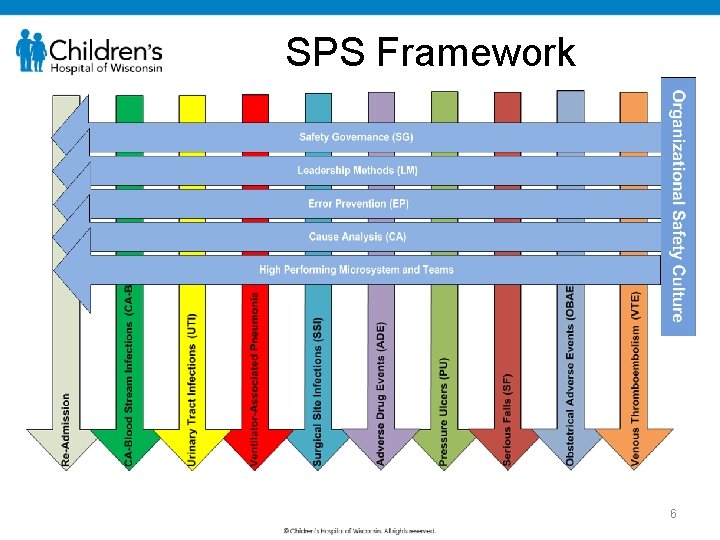
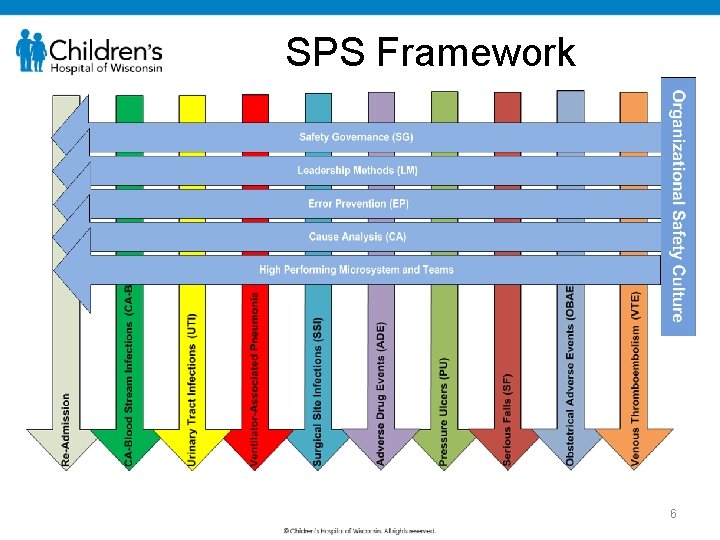
SPS Framework 6
SPS Principles • We will not compete on safety. • We will have transparency within the network. • All teach, all learn. • We act with a sense of urgency. • We focus on outcomes, learn through testing, and engage families and staff.
Patient and Family Perspective 1. Keep me safe. 2. Heal me. 3. Be nice to me. . in that order
Expected Safety Behaviors 1. Everyone makes a personal commitment to safety. 2. Everyone is accountable for clear and complete communication. 3. Everyone supports a questioning attitude.
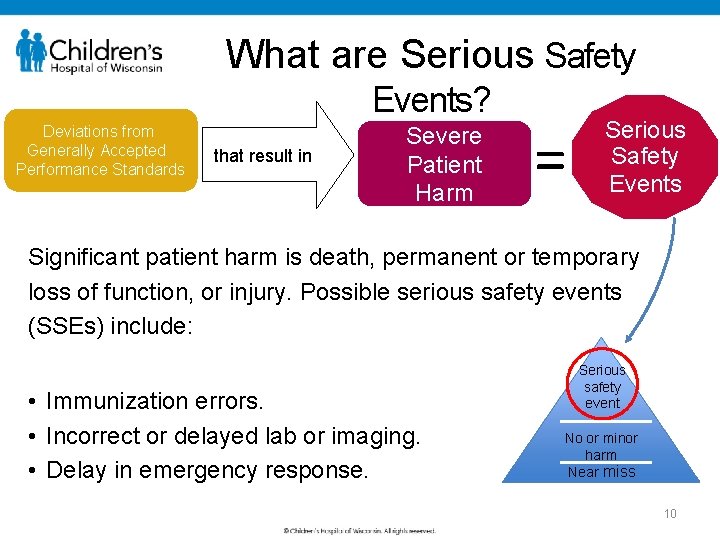
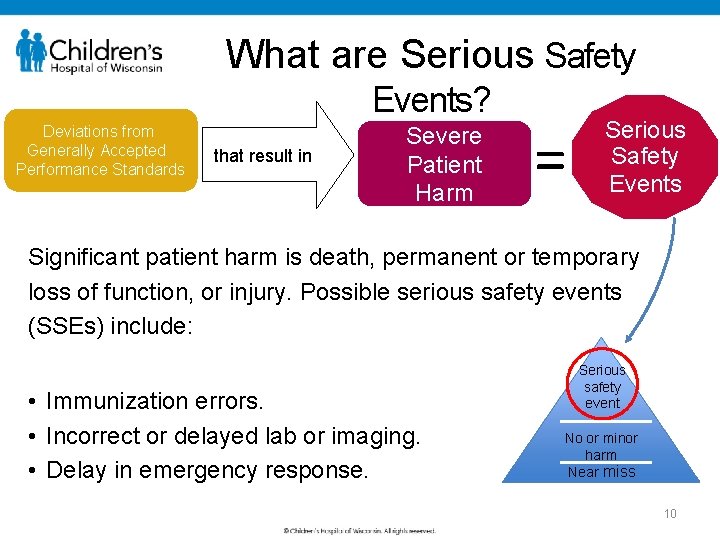
What are Serious Safety Events? Deviations from Generally Accepted Performance Standards that result in Severe Patient Harm = Serious Safety Events Significant patient harm is death, permanent or temporary loss of function, or injury. Possible serious safety events (SSEs) include: • Immunization errors. • Incorrect or delayed lab or imaging. • Delay in emergency response. Serious safety event No or minor harm Near miss 10
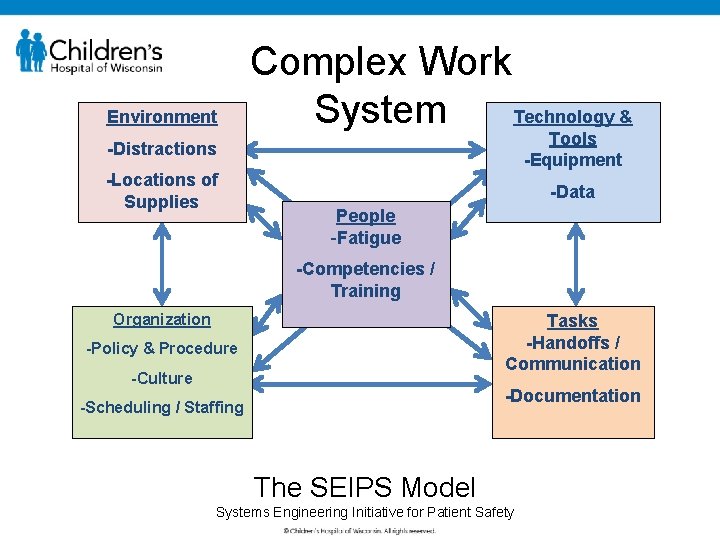
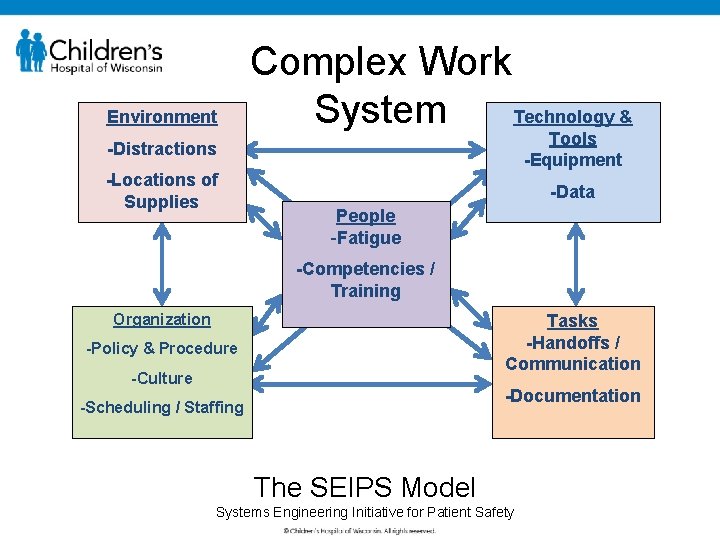
Environment Complex Work Technology & System Tools -Equipment -Distractions -Locations of Supplies -Data Significant vents or injuries People -Fatigue -Competencies / Training Organization Tasks -Handoffs / Communication -Policy & Procedure -Culture -Documentation -Scheduling / Staffing The SEIPS Model Systems Engineering Initiative for Patient Safety

Trained Safety Coaches 12 12
What is a Safety Coach? • Communicator • Educator • Role model • Observer • Storyteller • Change agent 13 13
The Safety Tools (endorsed by Solutions for Patient Safety) • AIDET • SBARR • Handoff • ARCC • Teach-Back • STAR 14 14
AIDET Use AIDET for communication with children, families, and staff: Acknowledge: Start with a smile. Greet them by name. Introduce: Tell the person who you are, your role, and your training. Duration: Describe how long it is going to take (for visit, results, etc). Explanation: Explain what you’re doing, why, and what happens next. Thank you: Thank children and families for allowing you to care for them. Thank staff for collaborating with you.
AIDET Example • Hello my name is Ilana, and I’ll be your provider today. I’m going to ask you a few more questions about how you fell. • After H&P complete: we are going to get an x-ray. Results usually take about 25 -30 minutes. We so appreciate your patience. What questions do you have? • Another example from a nursing perspective… 16
AIDET • Can be used as a framework that sets clear expectations and builds confidence. • It can be calming. • AIDET fosters effective communication with patients. • Elements of AIDET can be used in any order. 17
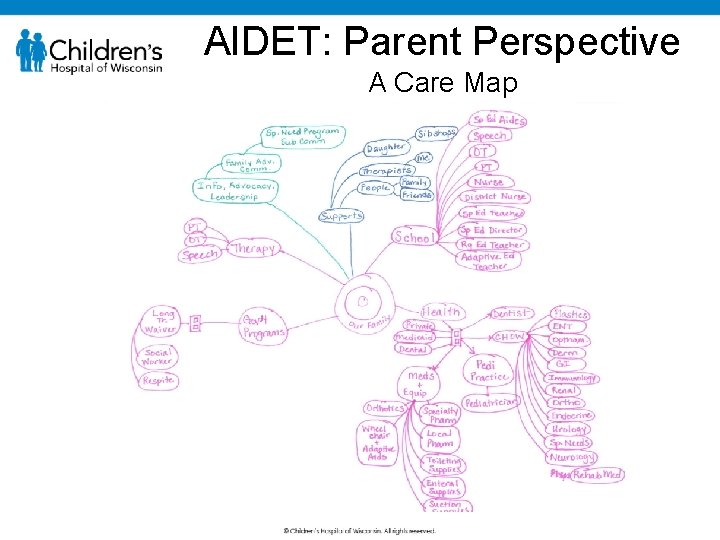
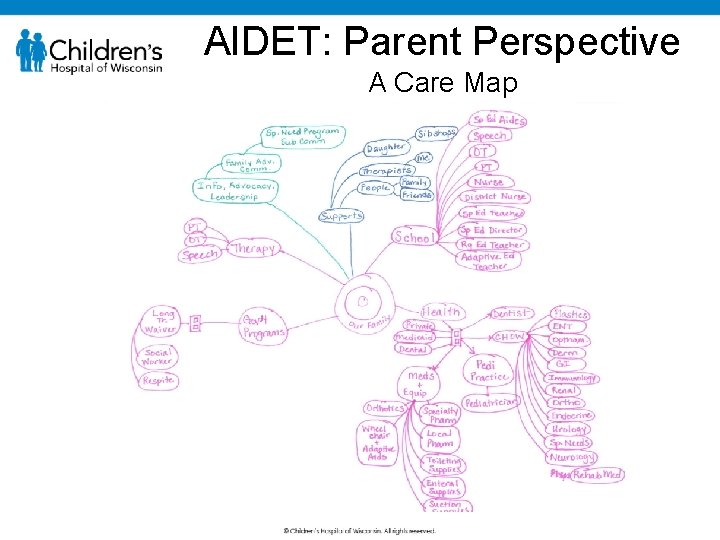
AIDET: Parent Perspective A Care Map
AIDET: Parent Perspective • It may decrease patient and parent anxiety, and may improve compliance • It prevents patients and families from becoming confused and frustrated throughout their visit and in turn increases patient satisfaction. 19
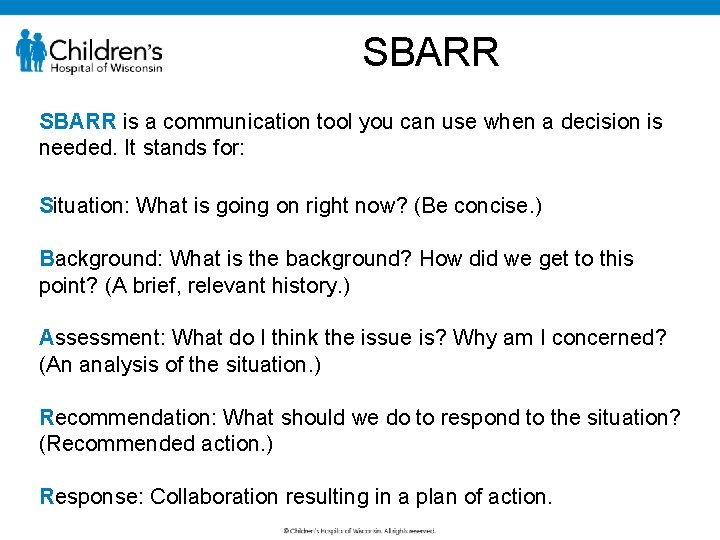
SBARR is a communication tool you can use when a decision is needed. It stands for: Situation: What is going on right now? (Be concise. ) Background: What is the background? How did we get to this point? (A brief, relevant history. ) Assessment: What do I think the issue is? Why am I concerned? (An analysis of the situation. ) Recommendation: What should we do to respond to the situation? (Recommended action. ) Response: Collaboration resulting in a plan of action.
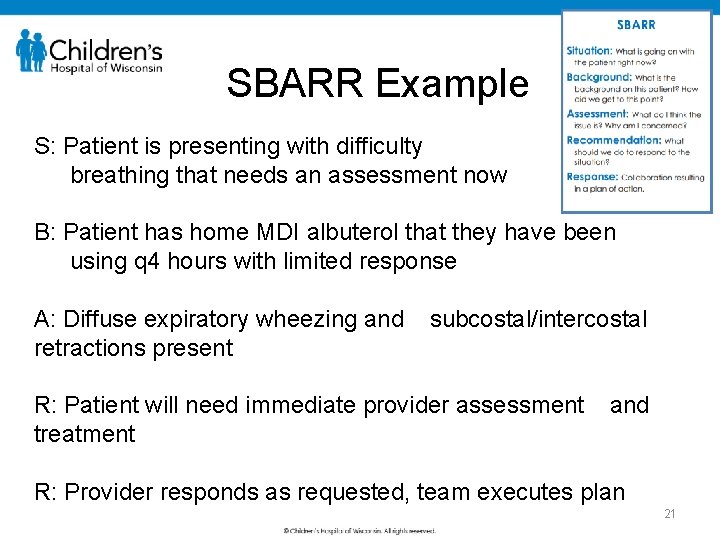
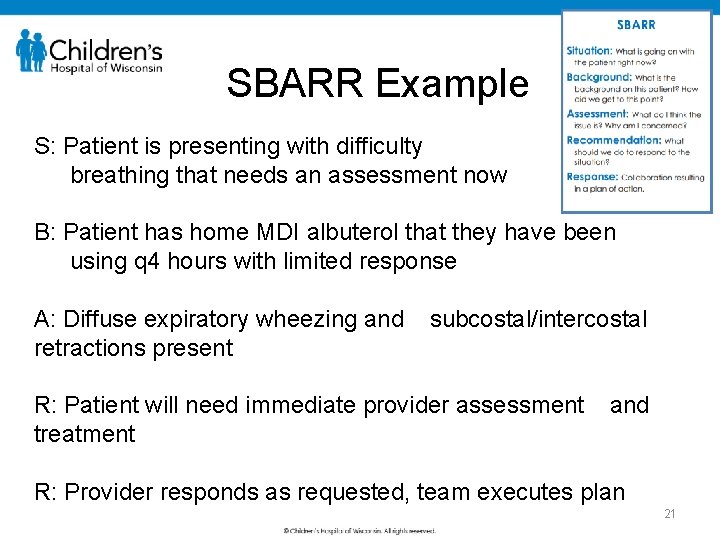
SBARR Example S: Patient is presenting with difficulty breathing that needs an assessment now B: Patient has home MDI albuterol that they have been using q 4 hours with limited response A: Diffuse expiratory wheezing and retractions present subcostal/intercostal R: Patient will need immediate provider assessment treatment and R: Provider responds as requested, team executes plan 21
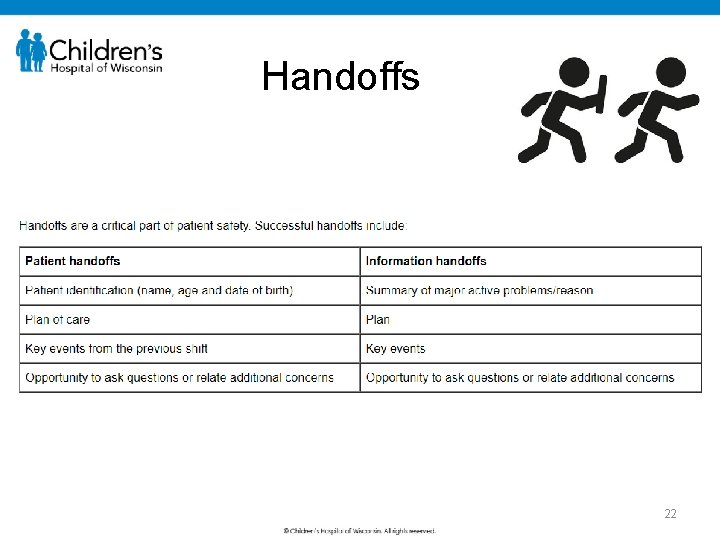
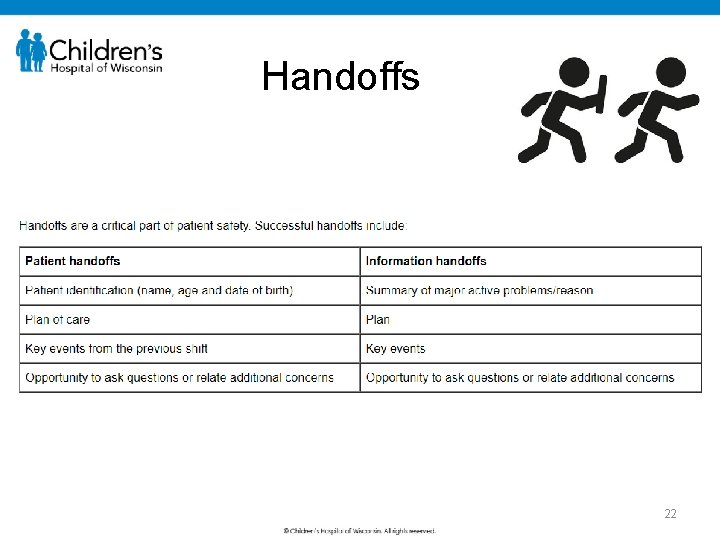
Handoffs 22
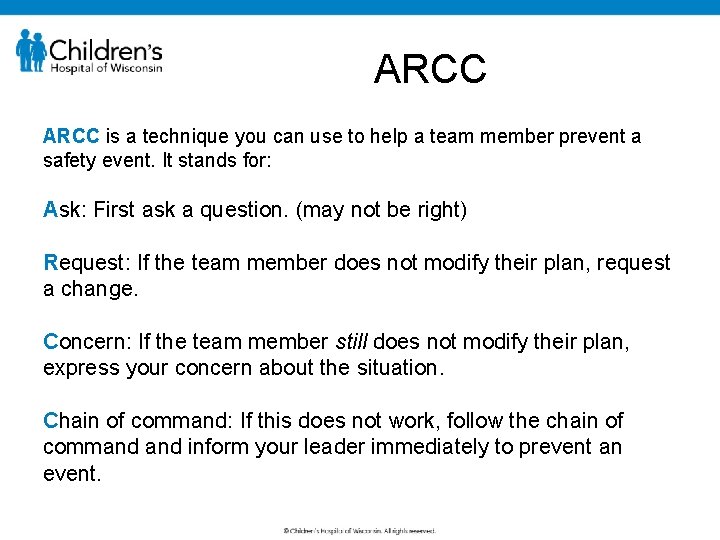
ARCC is a technique you can use to help a team member prevent a safety event. It stands for: Ask: First ask a question. (may not be right) Request: If the team member does not modify their plan, request a change. Concern: If the team member still does not modify their plan, express your concern about the situation. Chain of command: If this does not work, follow the chain of command inform your leader immediately to prevent an event.
ARCC Example The provider observes a staff member entering and exiting patient rooms without washing hands or using hand sanitizer. The provider shares her observation with the staff member and reminds the staff member to wash her hands upon entry and exit of patient rooms. “I’m concerned for your safety and the patient’s…Please don’t forget the importance of hand washing…” • Option A: success! No need to escalate • Option B: the provider notices no change in practice despite request. The provider can again discuss with staff member, hand them a prop such as hand sanitizer, or if all else fails, escalate safety concern to leader. 24
Teach-Back • Teach-back is using your own words to repeat directions or information you’ve just received. • We use teach-back when we check for understanding with patients and their families. • Using teach-back with co-workers serves the same purpose. • Think: closed loop communication!
Teach-Back: Ask and Encourage Clarifying Questions • Asking one or two clarifying questions reduces the chance of making an error by 2½ times. • Clarifying questions should be phrased in a positive way and in a manner that improves understanding.
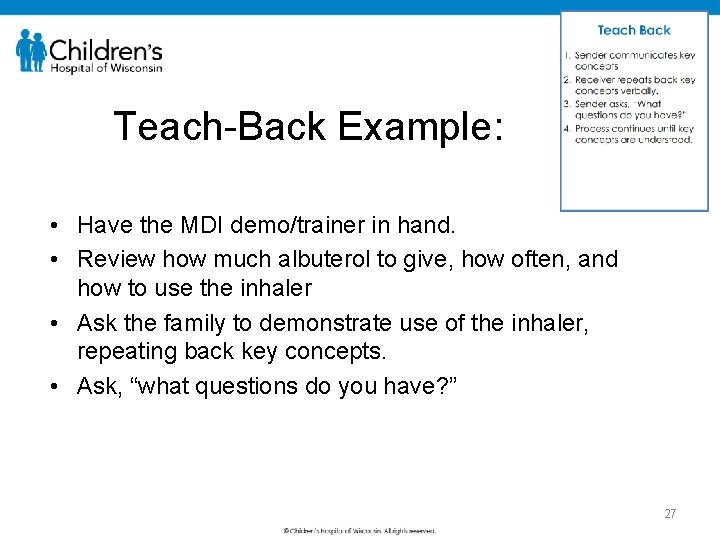
Teach-Back Example: • Have the MDI demo/trainer in hand. • Review how much albuterol to give, how often, and how to use the inhaler • Ask the family to demonstrate use of the inhaler, repeating back key concepts. • Ask, “what questions do you have? ” 27
STAR: Gena, Safety Coach STAR is a self-checking tool. Think of it as a mental time out that helps you focus on details. It stands for: Stop: Pause to focus your attention on the task at hand. Think: Understand what is to be done, plan your actions, and decide what you’ll do if the unexpected occurs. Act: Carry out the planned task. Review: Verify that you got the expected or desired results.
STAR takes just a couple of seconds. . . but it can reduce your chance of an error, mental slip, or lapse by more than 10 times when you are: • Distracted. • Fatigued. • Performing multiple tasks at once. • Under time pressure.
STAR can prevent this: “I grabbed the After Visit Summary for the child, stapled it, highlighted main points, and discharged him. Another staff member said that she printed an immunization report for a different patient and was unable to locate it. I checked my patient’s paperwork, and the immunization report was stapled to the last page of my patient’s After Visit Summary. I removed it and gave the After Visit Summary back to the correct family. ” 30
But wait, there’s more! • Safety concept of the month • Coaching • Good catches • Recognition • Monthly phone huddles 31
Safety Concept of the Month Example 32
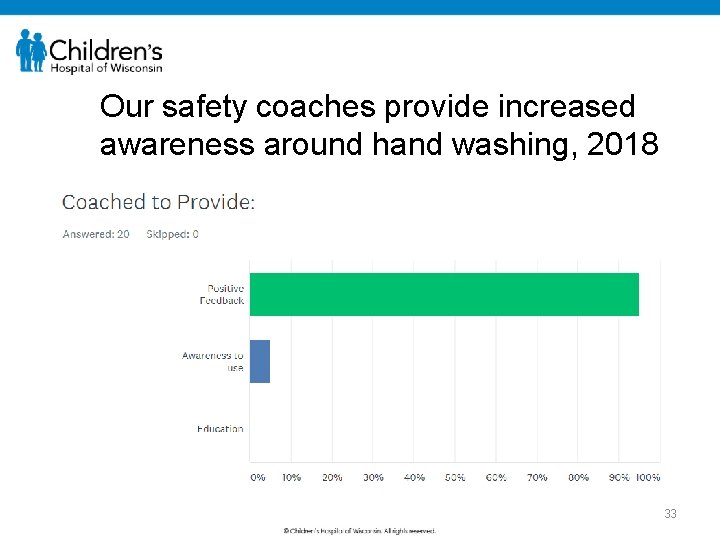
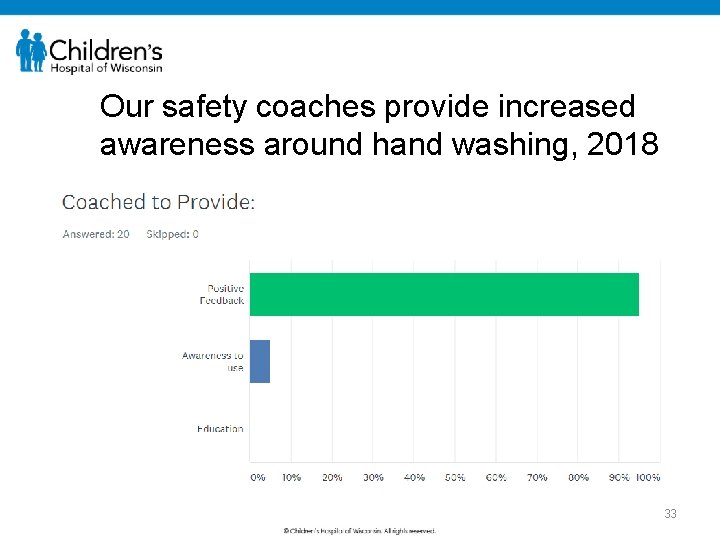
Our safety coaches provide increased awareness around hand washing, 2018 33
Good Catches We recognize good catches each month based on: • • Potential for harm Improvements made as a result of the event Customer appreciation Financial risk to the organization We provide appreciation & post as safety stories on our intranet
Good Catches “More than anything, this is what distinguished the great hospitals from the mediocre. They didn’t fail less. They rescued more. This in fact may be the real story of human and societal improvement. Risk is necessary. ” -Atul Gawande 35
Appreciation and Recognition Create a Culture of Teamwork 36
What Can We Expect? • If we adopt these safety tools, we will be 10 x less likely to experience a human error. • If everybody practices these behaviors, we can get to ZERO serious safety events. To get there, we must each act and believe that… Safety Starts with Me. 37
Safety Starts With Me I will make a personal commitment to safety. I am accountable for clear and complete communication. I support a questioning attitude.
We Are Committing To: • Demonstrating a personal and a team commitment to safety (200% accountability). • Being personally responsible for concise, accurate, clear, and timely verbal and written communications. • Questioning and welcoming being questioned.
If you are within CHW, please reach out to a safety coach or your leadership team with questions or concerns! For those outside of CHW, please contact us if you would like to learn more! 40 40
Thank You!
 Please mute yourself
Please mute yourself Please mute your microphone when not speaking
Please mute your microphone when not speaking Please mute your phone
Please mute your phone Please mute your phone
Please mute your phone Please keep your mic muted
Please keep your mic muted Please mute
Please mute Please mute yourself
Please mute yourself Triad polyamory
Triad polyamory Please turn off your cell phone in church
Please turn off your cell phone in church Please silence your phone
Please silence your phone Put your cell phone away
Put your cell phone away Cell phone energy transformation
Cell phone energy transformation Please write your phone
Please write your phone Please turn off your cell phone announcement
Please turn off your cell phone announcement Please extend your warm welcome
Please extend your warm welcome My blackboard tcc
My blackboard tcc Please switch off the phone
Please switch off the phone Please be quiet. i (try) to sleep
Please be quiet. i (try) to sleep Welcome mobile phone
Welcome mobile phone Selectively mute
Selectively mute Selective mute
Selective mute Pambasas
Pambasas Who wants to mute for a millionaire
Who wants to mute for a millionaire Mute yourselves
Mute yourselves Welcome please take a seat
Welcome please take a seat Welcome please sign in
Welcome please sign in Please place an order
Please place an order Welcome welcome this is our christmas story
Welcome welcome this is our christmas story Holy spirit thou art welcome in this place
Holy spirit thou art welcome in this place Millions billions trillions chart
Millions billions trillions chart A disturbance that transfers energy is called
A disturbance that transfers energy is called A wave is a disturbance that transfers energy
A wave is a disturbance that transfers energy Persuasion
Persuasion Piecewise problem solving
Piecewise problem solving Put your cell phone away
Put your cell phone away Signs your phone is hacked
Signs your phone is hacked Put your cell phone away
Put your cell phone away Give us your hungry your tired your poor
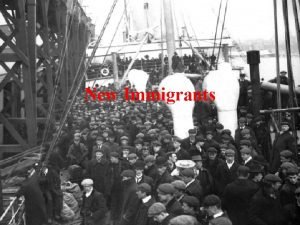
Give us your hungry your tired your poor Type in the chat box
Type in the chat box Please turn off your microphone
Please turn off your microphone Please come in and sit
Please come in and sit Please sit down and your seat belts
Please sit down and your seat belts