Welcome and introductions David Smith Chief Officer for




- Slides: 36

Welcome and introductions David Smith, Chief Officer for Kingston CCG and Director of Health and Adult Services for Kingston Council
Update on Kingston CCG Dr Naz Jivani, Chair
Changes to the NHS • GPs taking over commissioning of hospital, community and mental health services from PCTs • National Commissioning Board to commission doctors, dentists, pharmacists and opticians • Health and Wellbeing boards established in each borough • Increased role for Healthwatch in engaging patients • Public health services transferred to councils and Public Health England
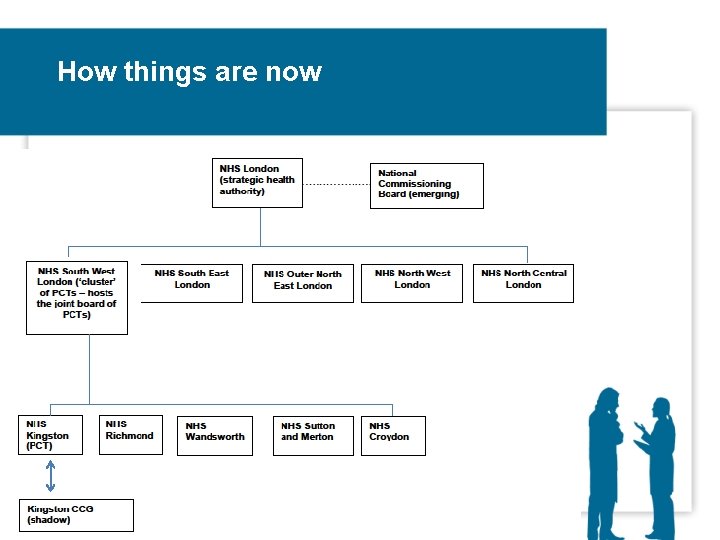
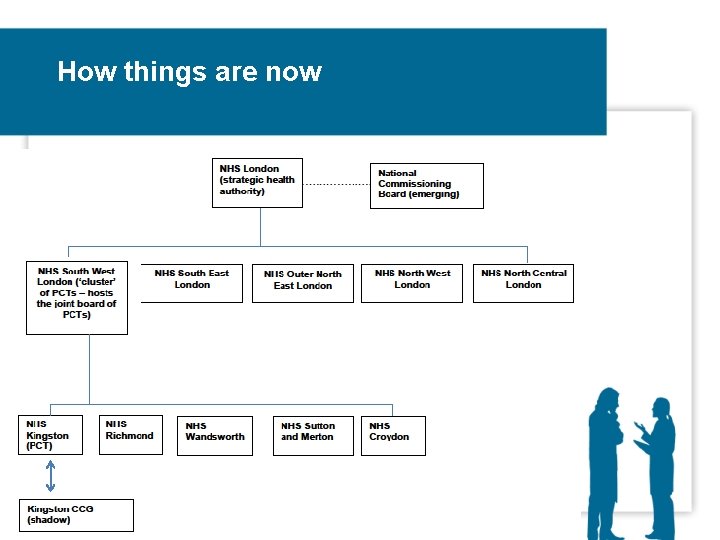
How things are now
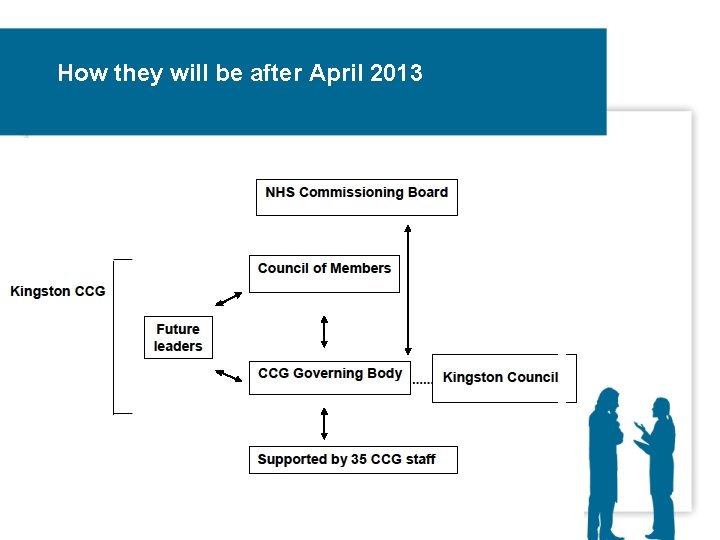
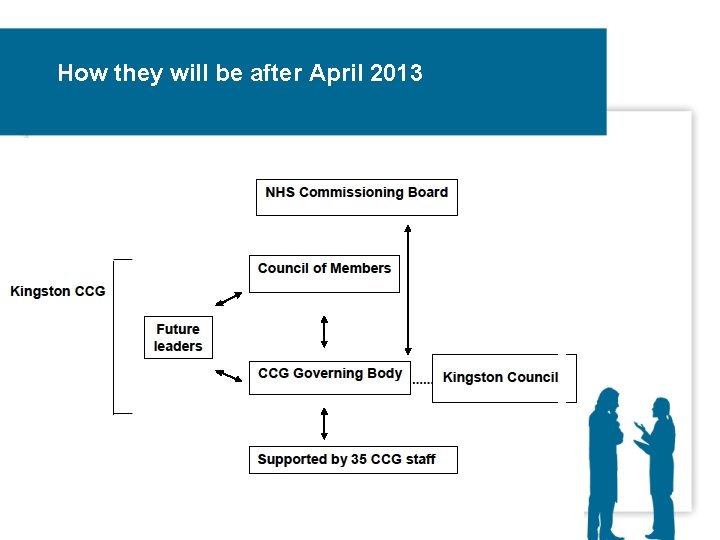
How they will be after April 2013
Developments in Kingston • Kingston CCG was given delegated responsibility for hospital, mental health and community services • One of three in London and 35 nationally to apply for ‘first wave’ authorisation • We now have an elected governing body and a unique Council of Members, representing all GPs • We also have a constitution and robust governance arrangements • Once approved the CCG will take over full responsibility from April 2013
What we have been doing • Kingston at Home was launched - a joint health and social care programme to support people to stay living in their own homes • Medicines management – working with GP practices to ensure patients get the right medicines for their condition • Urgent care – increasing options so patients can avoid a long wait in A&E
Other CCG priorities • Helping patients look after themselves - e. g. Kingston exercise programmes have decreased hypertension levels • Outpatients – ensuring patients are referred to the right place for the treatment they need • Contributing to the Better Services Better Value review. Public consultation begins soon.
Mental health improvements SW London engagement events were held to capture views Initial findings: • Agreement that changes are needed • Greater need for joint working between organisations • Proactive involvement of a wide range of voices • Clearer communications • More consistency of care • Quicker access/referral times What we’re already doing: • Tendering for new substance misuse and psychological therapies services • Working across SW London to act on patient feedback
Involving patients • We’re talking to patient reference groups, voluntary organisations and other stakeholders to make sure people can influence decision making ‘upstream’ • Engagement to be carried out before relevant board reports are submitted • This will involve proactive engagement using a range of routes • We’re proposing a regular patient forum and email network • Views reported to Integrated Committee Governance

Questions This is a work in progress – we need your ideas! Contact us e: communications@kpct. nhs. uk t: 020 8547 5557 www. kingstonccg. nhs. uk
Health and Wellbeing Strategy Dr Jonathan Hildebrand, Joint Director of Public Health
Why have a health and wellbeing strategy? • As part of changes to the NHS, Health and Wellbeing Boards are being set up • Kingston’s H&WBB has been meeting for two years • Members include representatives of the voluntary sector, Healthwatch, the CCG, councillors and officers • Chaired by the Leader of the Council • The H&WBB has a responsibility to produce a Health and Wellbeing Strategy
Why have a health and wellbeing strategy? • Strategy is based on the Joint Strategic Needs Assessment of the assets and needs of local people • Focuses on a small number of key areas where partnership working could make a major difference • Lays outcomes for agencies to work to achieve • Does not replace other agreed strategies • Once agreed, progress will be by the Board reviewed regularly
What’s in the strategy • Initial thinking from a board seminar • Draft discussed at H&WBB, Kingston CCG, now on CCG and council websites • Overview of Kingston and overall principles • Four main themes: 1. 2. 3. 4. Mental health Older people/long term conditions Socially excluded disadvantaged groups Children and young people
Mental health • High spend but outcomes do not reflect this Desired outcomes include: - Improved physical and mental health for people with MH problems - Co-ordination and support for people with MH problems in the community - Integration between specialist/primary care - Simple referral and care pathways for alcohol/drugs - Modernised care for older people
Older people and people with long-term conditions • Older people and people with long-term conditions are major users of services Desired outcomes include: - Improved information and advice - Empowerment of people with long term conditions - Addressing risk factors for long-term conditions - Improved local activities/support - Greater availability of rehabilitation
Addressing the needs of socially excluded and disadvantaged groups • There are wide variations in health within Kingston Desired outcomes include: - Reduce the gap in life expectancy for disadvantaged communities whilst improving outcomes for all - Engage and empower disadvantaged communities so that their lifestyle becomes more focused on health - Strengthen the involvement of disadvantaged groups in service redesign to avoid exclusion
Children and young people • Child health influences health in adulthood so action has long term benefits Desired outcomes include: - Good quality antenatal care/ screening - Achieve immunisation targets - Reduce childhood obesity - Increased provision for children with complex needs - Early identification and intervention behaviours with high risk
For discussion • Are there any key priorities for joint action that we have missed? • Of the four priorities identified, is there an order of importance? • Within the priorities are there outcomes we need to add? • Do you have any other comments about the strategy? • How can we maintain your involvement in the strategy in the future?

Kingston at Home Julia Gosden, Project Lead Pre-proposal ideas testing
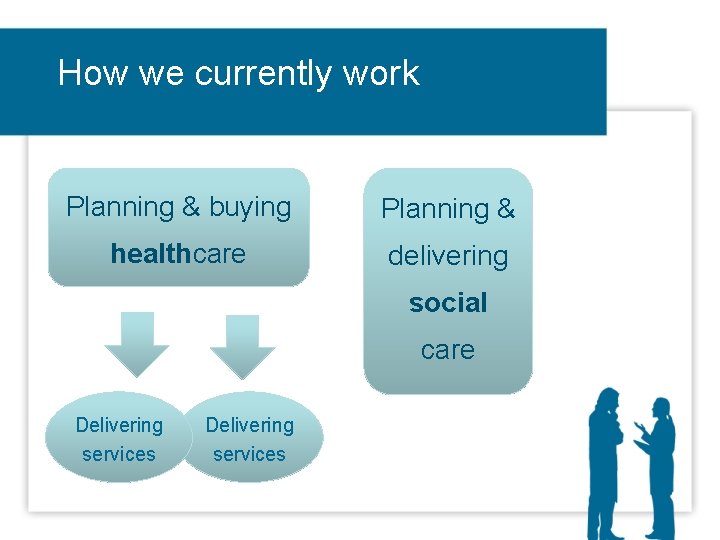
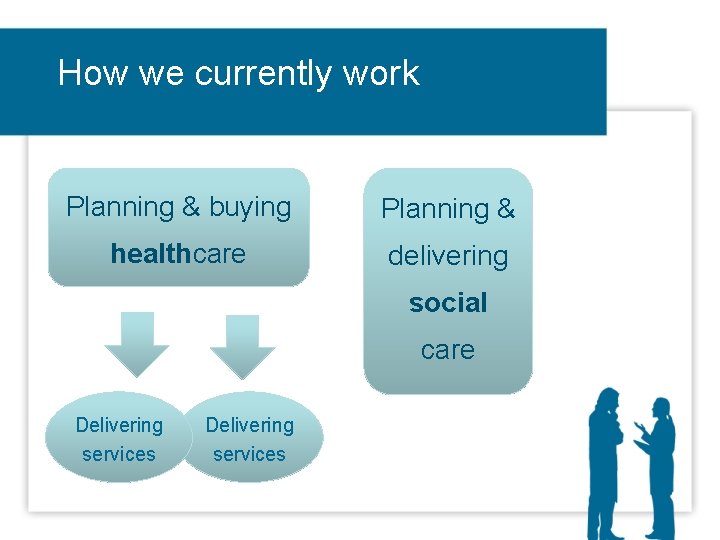
How we currently work Planning & buying Planning & healthcare delivering social care Delivering services
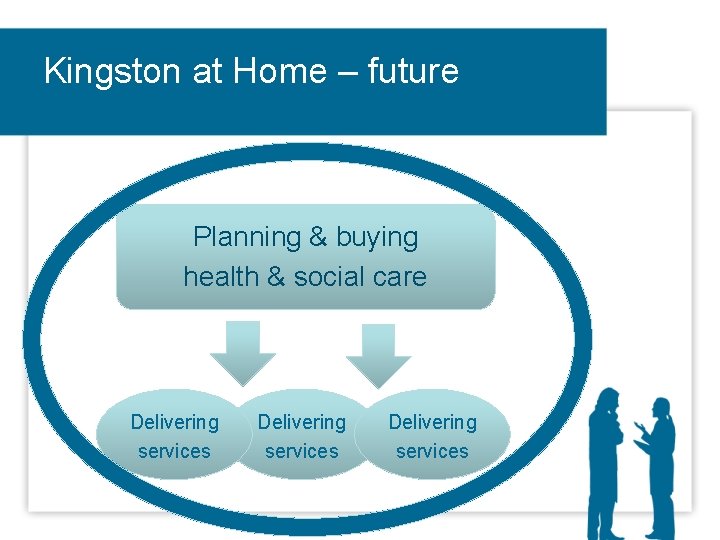
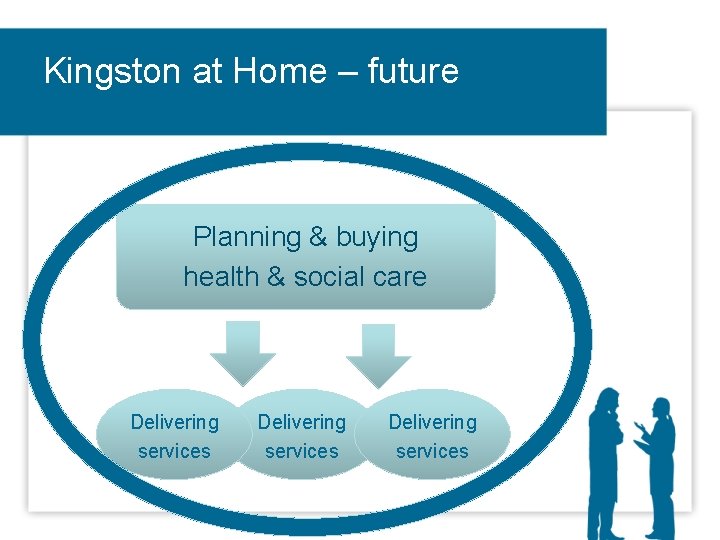
Kingston at Home – future Planning & buying health & social care Delivering services
Today’s focus Home & community care improvements - discuss ideas, so we can include your views as we develop proposals. Emphasis on increasing the amount of treatment, care & support that is provided at home.
Why we need to change People live longer (Kingston over 65 s – top 25% in England; 14% increase 2009 -18) 54% of spend on older people = residential care (Kingston - high referrals) Over 75 s form 34% of emergency admissions but their stay is longer - 56% of bed days Financial challenges - no change not an option
Evidence • We know people want more coordinated care that gives them control over their own health and helps them to live independently • Evidence from other areas demonstrates that this approach works – is better for patients and more cost effective
Kingston at Home – What? • More treatment at home • More community support & activities • Especially after an illness, accident or other incident to help people: ü Get better ü Stay well ü Remain independent
Kingston at Home – How? • Focus on rehabilitation & reablement = better value & better for patients • Transfer funding & resources • Join-up health, social & voluntary care services • Prevention of high-dependency
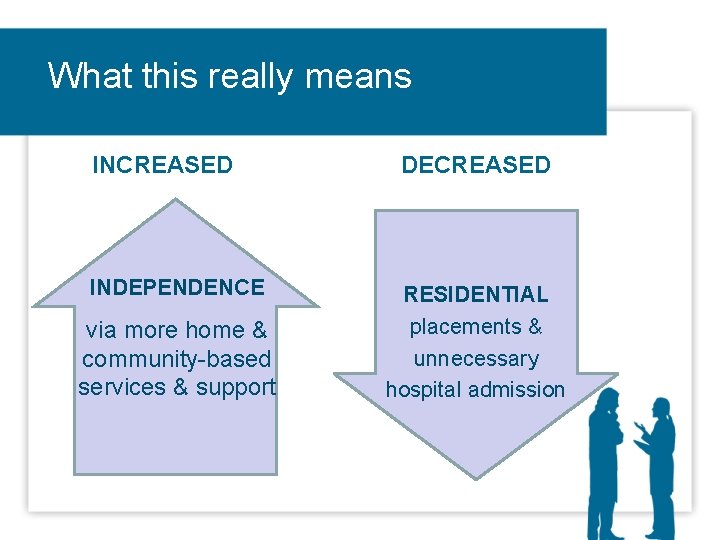
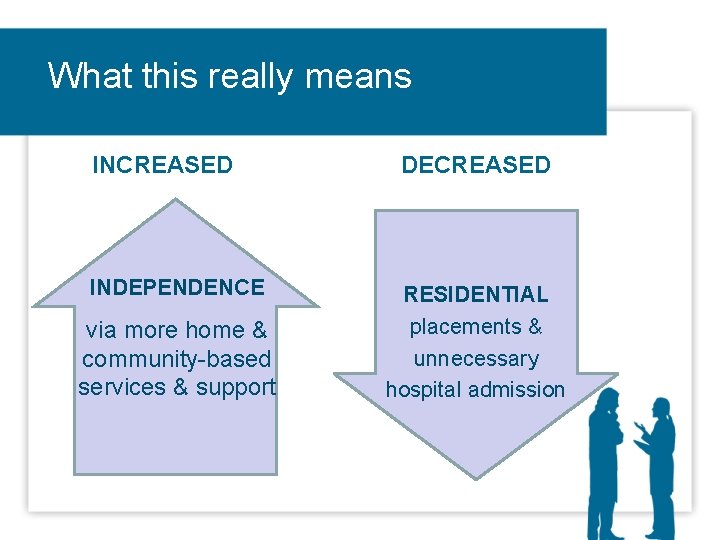
What this really means INCREASED INDEPENDENCE via more home & community-based services & support DECREASED RESIDENTIAL placements & unnecessary hospital admission
Some examples • Single point of access with quick referral response • Teams that are integrated across council and NHS • Multidisciplinary assessment/case management • Greater use of technology e. g. sensors and alarms
Some examples (continued) • Reduced discharge from hospital to residential care • Increased home based rehabilitation • Community beds for short term support • Social care personal budgets for service users
Kingston at Home – Future • More people-focused – asking, listening, informing others • Whole-person approach – all health, physical fitness, safety, emotional wellbeing & daily needs • Reduce hospital visits, length of stay, readmissions & referrals into long-term care

How can we best support people to stay living at home?
Questions • What do you think of our ‘joined-up’ vision to help support people at home rather than residential care or hospital? • What are the positives/negatives? • What types of care and support would your ideal home service include? • What factors should we bear in developing proposals? mind when
Feedback on this forum
Your feedback on this forum • What could be improved? • What did you think of the format/venue? • Do you support quarterly meetings? • If you would like us to meet with your patient group or organisation let us know Please note you can complete feedback forms that have been left on each chair, including any further questions, and we will respond to you.