Viral HOST INTERACTIONS Dr Amita Arya Viral host
- Slides: 34
Viral HOST INTERACTIONS Dr. Amita Arya.
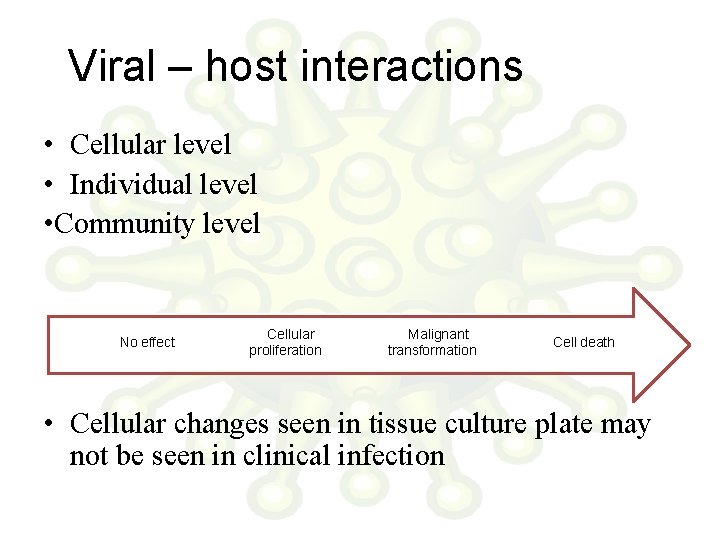
Viral – host interactions • Cellular level • Individual level • Community level No effect Cellular proliferation Malignant transformation Cell death • Cellular changes seen in tissue culture plate may not be seen in clinical infection
• Non structural proteins shut down the host protein & DNA synthesis • Large amount of Viral components change the cellular architecture of host cell • Toxic effects • Change in permeability of Host cell AUTOLYSIS • Formation of syncytium d/t fusion of adjacent cell membranes • Viral antigens will confer newer properties on host cell (cell adsorption, oncogenesis) • Changes in the host chromosome ( Measles, Mumps, Adenovirus, CMV & Varicella) • Inclusion bodies
Inclusion bodies • Structures with distinct size, shape , location and staining properties • Can be seen under light microscope after staining • May be seen in cytoplasm or nucleus • Generally acidophilic in nature – Pink in colour on staining with Giemsa or Eosin methylene blue stains • Some may be basophilic as well
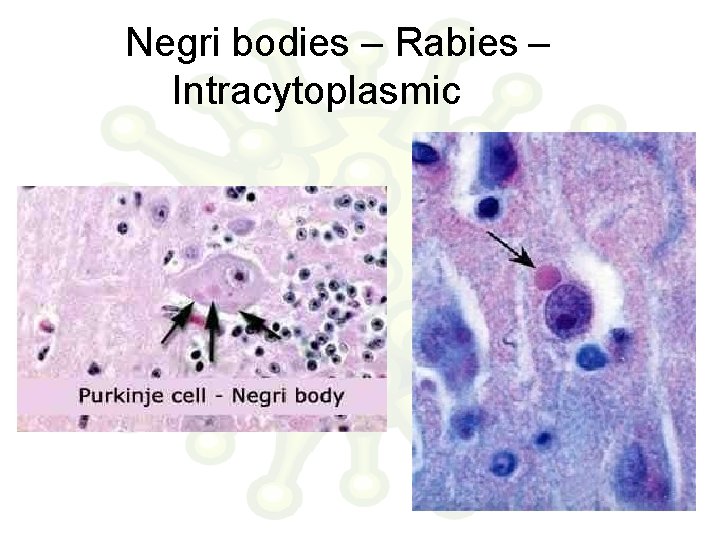
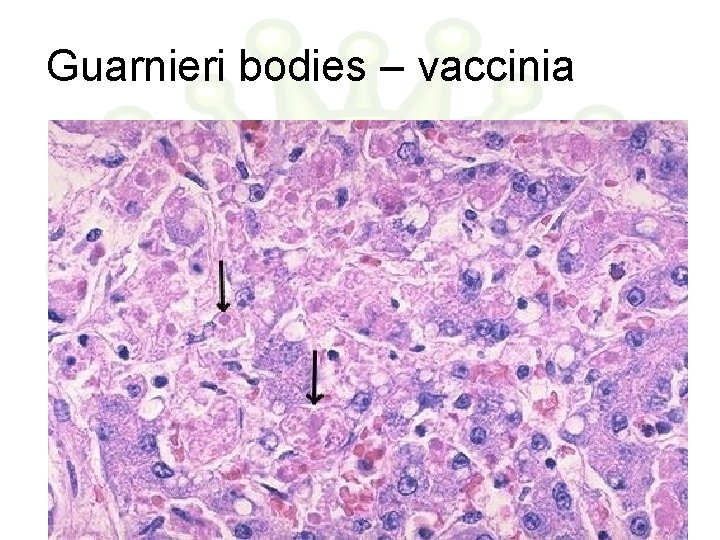
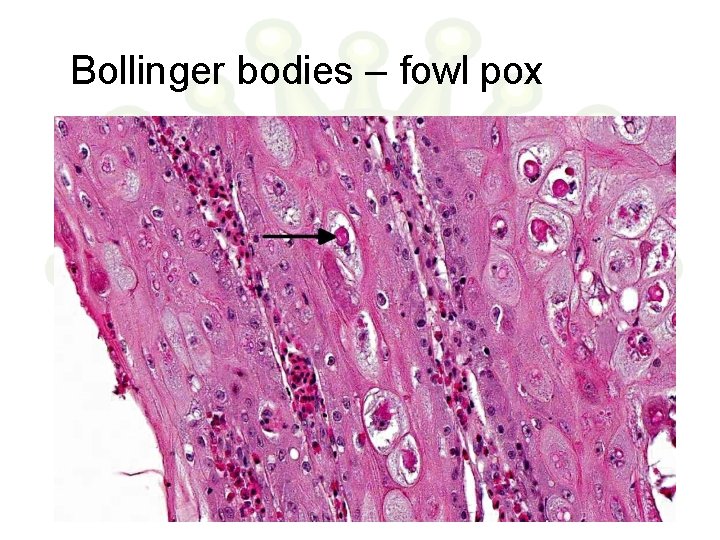
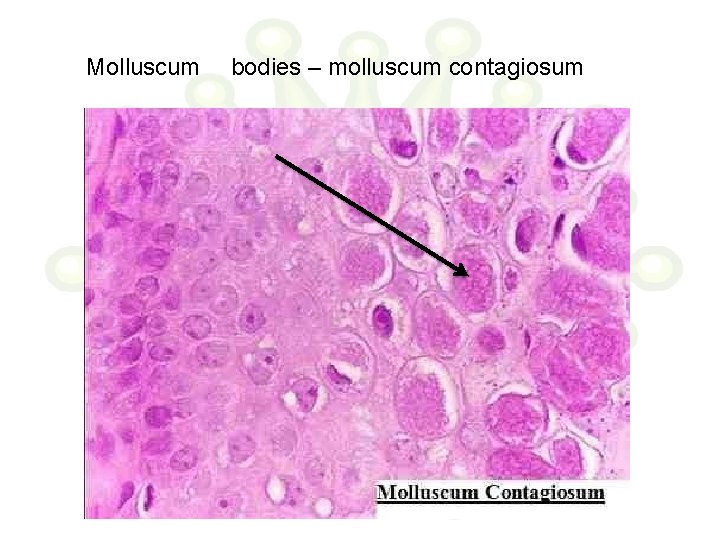
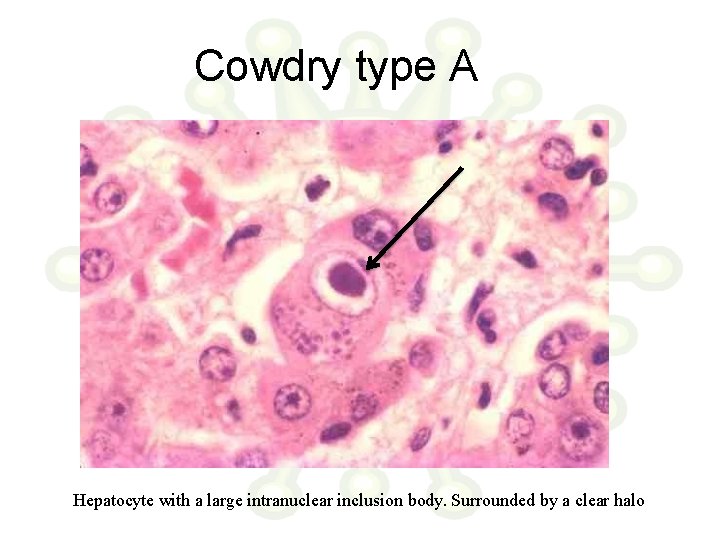
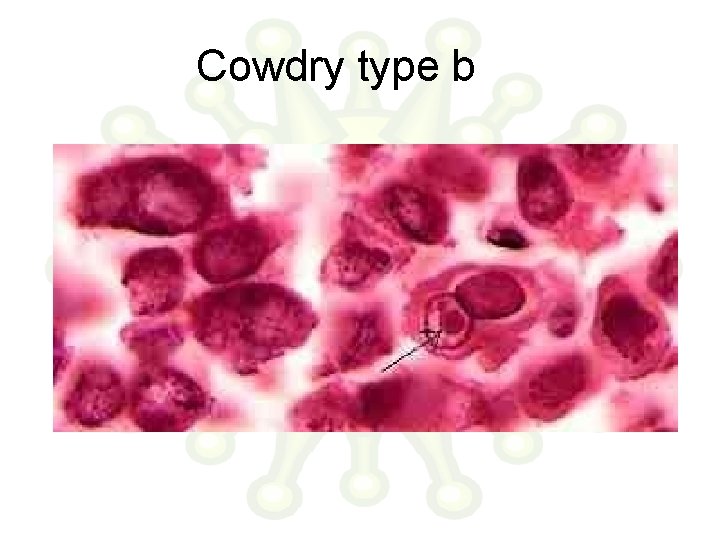
Inclusion bodies • Helps in diagnosis – Negri bodies – intra cytoplasmic inclusion – Rabies – Guarnieri bodies – vaccinia – Bollinger bodies – fowl pox – Molluscum bodies – molluscum contagiosum – Cowdry type A – Herpes virus , Yellow fever virus – Cowdry type B – Adeno virus, Polio virus • Inclusion bodies my be an aggregate of virions or collection of viral antigens or the degenerative changes produced by viral infection.
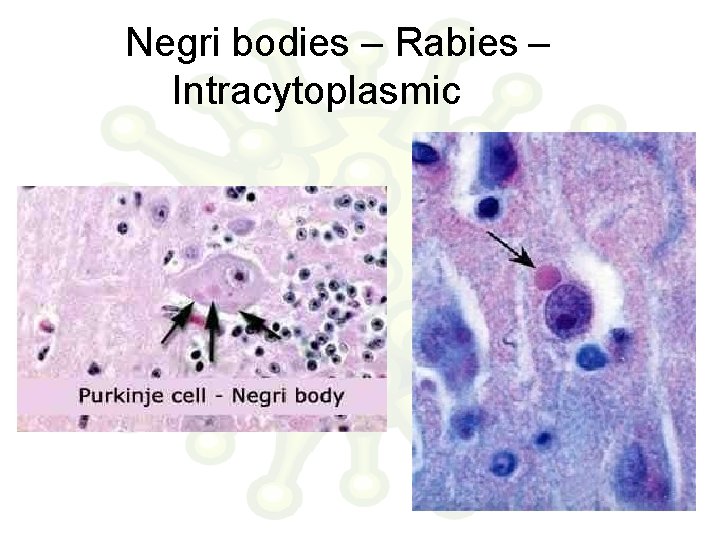
Negri bodies – Rabies – Intracytoplasmic
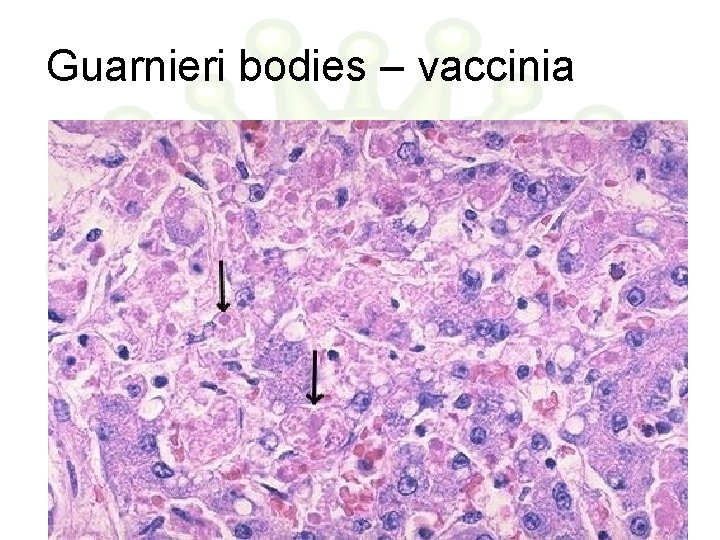
Guarnieri bodies – vaccinia
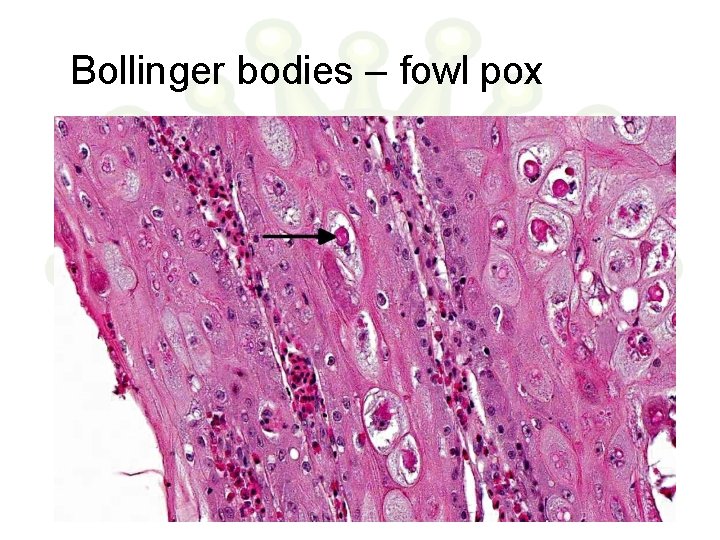
Bollinger bodies – fowl pox
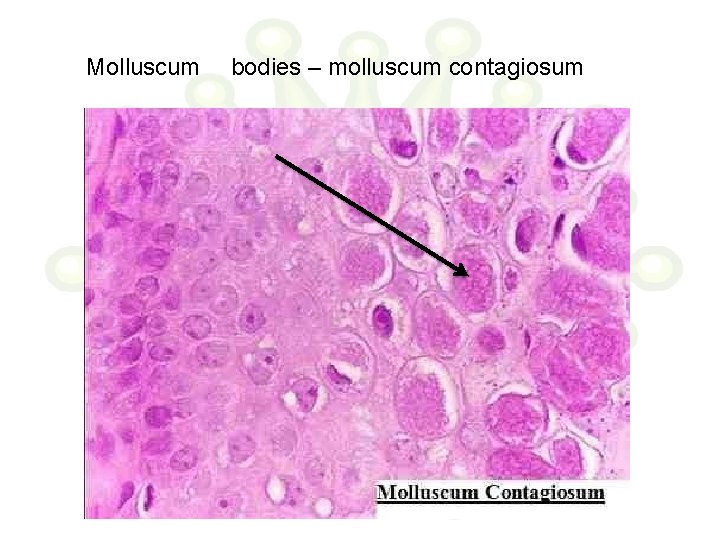
Molluscum bodies – molluscum contagiosum
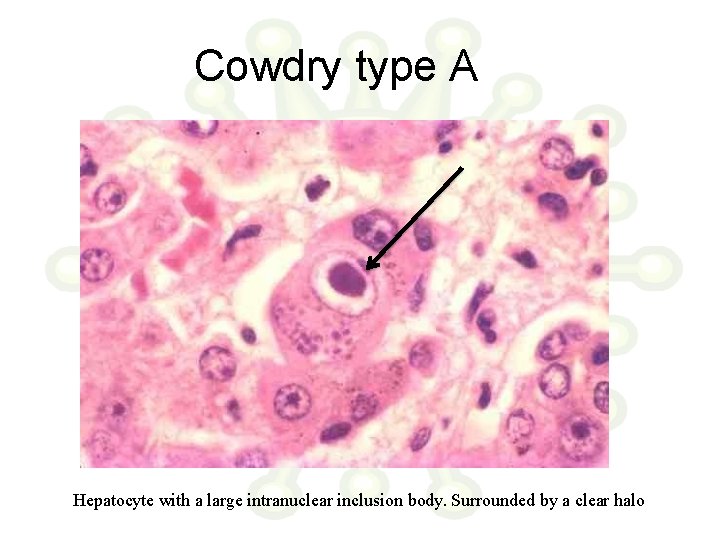
Cowdry type A Hepatocyte with a large intranuclear inclusion body. Surrounded by a clear halo
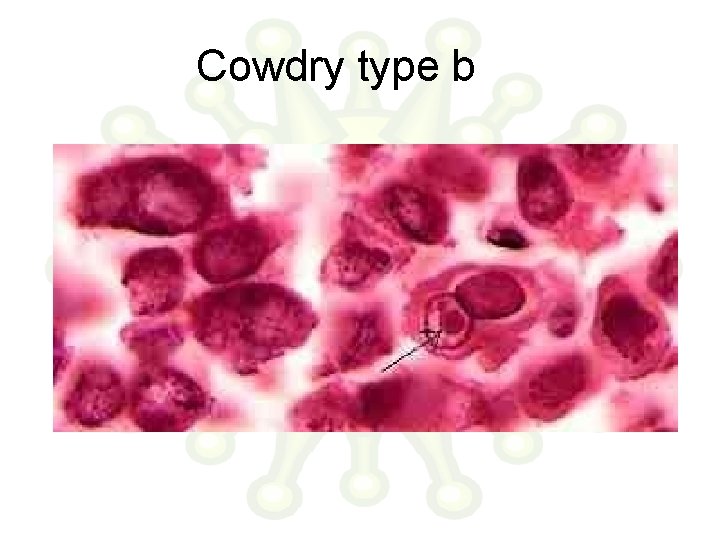
Cowdry type b
Pathogenesis of viral infection • Inapparent • Apparent – Acute – Subacute – Chronic • Latent • Persistent tolerant infections : Congenital / Neonatal infections • Oncogenic virus • HIV
Route of entry • Respiratory tract (Most common) – Multiply locally Blood/Lymph Extensive multiplication Disease. – Small pox, chicken pox – Influenza , Rhinovirus (stay in respiratory tract itself) • Alimentary tract – All enveloped viruses are destroyed by bile – Rhinovirus is inactivated by gastric juice – Enterovirus, adenovirus, reo virus, hepatitis virus – Some multiply in GIT and transported to target organs (eg. Polio virus) • Genital tract • Conjunctiva • Skin • Vertical transmission – Mother to baby
Route of entry • Skin – Produce few local lesions – Papilloma, vaccinia, cowpox & molluscum contagiosum. – Viruses can enter through break in skin – Abrasions – Papiloma virus – Insect bites – Arbovirus – Animal bites – Rabies – Injections – Hepatitis • Genital tract – Human immuno deficiency virus
Route of entry • Conjunctiva – Local disease – Adenovirus – Systemic disease – Measles • Vertical transmission – Mother to baby – May occur at any stage till birth – Usally leads to fetal death and abortion – Maldevelopment – Rubella and Cytomegalovirus – Many tumor virus spread via this route
Incubation period • Time taken for virus to spread from site of entry to the organs of viral multiplication and causation of disease. • Localized diseases : Shorter incubation period • Systemic diseases : Longer incubation period • Incubation period shorter when directly introduced into blood stream
Host response Depends on 1. Virulence of the infecting strain 2. Resistance of the host » Immunological • Humoral • Cell mediated immunity » Non specific • Interferon production • Body temperature • Age • Malnutrition
• Viral infection liberates – Surface antigens – Internal antigens – Non structural antigens • Early proteins – Humoral immunity • Ig. G Blood and Tissue • Ig. M • Ig. A Mucosal surface
Immunoglobulins on viruses • Prevents attachment of virus to cell • Enhances viral degradation • Prevents release of virions from infected cell Immunoglobulin + Complement Surface damage of enveloped virions Cytolysis of virus infected cells
Role of antibodies • Role of antibodies in viral infection is limited • Antibody to internal antigen Non neutralizing • Antibody to surface antigen varying neutralization • Some antibodies can paradoxically increase infectivity • May contribute to Pathogenicity • Antibody may result in – Complement dependent cell injury – Immune complex type tissue injury
Role of cmi • Plays a major role in viral infection • Helps in recovery from viral infection • Can cause tissue damage as well • Deficient CMI increase in Herpes, Pox, Measles • Most often an infection provides long lasting immunity
Non immunological responses Macrophages phagocytose virus in blood. Body temperature : > 39°C inhibits most virus Exception – Herpes simplex – fever blisters Hormones : Corticosteroids enhance viral infection. Due to depression of immune system & inhibition of interferon synthesis Malnutrition Age
Interferons • Family of host coded proteins • No direct action on virus • Acts on host cells to make them refractory o viral infection. • On exposure to interferon cells produce TIP (Translation Inhibition Protein) inhibits translation of viral m. RNA • Does not affect translation of host m. RNA • Interferons are species specific. • RNA viruses are better inducers of interferon production • Temperature of > 40°C induces interferon secretion • Steroids and increased O 2 tension decrease interferon synthesis • Synthesis starts in about 30 mins of induction and reaches peak by 6 -12 hours.
Interferons • α leucocytes • ß fibroblasts • Ɣ T-Lymphocytes • Inactivated by proteolytic enzymes • Resist 56°C – 60°C for 30 -60 mins • α & ß are resistant at p. H range of 2 -10 • Ɣ is labile at p. H of 2 • Non toxic • Poorly antigenic • Cannot be estimated by routine serological methods
Use of Interferons • Ideal candidate for prophylaxis and treatment – Non toxic – Non antigenic – Diffuses freely in the body – Wide spectrum of antiviral activity • Drawback species specific • Current use URTI, Warts, Herpetic keratitis & anticancer agent in lymphomas
Biological effects of interferons • Anti-Viral : resistance to infection • Anti –Microbial: Resistance to intracellular infections (Toxoplasma, Chlamydia, Malaria) • Cellular effects : Inhibition of cell growth and proliferation, Increased expression of MHC antigens on cell surface • Immunoregulatory : – Increases activity of Natural killer (NK) calls and T cells. – Activates cell destruction activity of macrophage – Moderates antibody formation – Activates suppressor T cells – Suppresses DTH
Lab diagnosis • Microscopy : Demonstration of virus by electron microscopy Demonstration of inclusion bodies Fluorescent antibody techniques • Demonstration of viral antigen: Possible when viral antigens are abundant in the lesion Precipitation in gel Immunofluorescence CIE RIA ELISA PCR
Lab diagnosis • Isolation of virus : • Need proper transport media at appropriate temperature • Processing to remove bacterial contaminants • Inoculation in eggs • Animal inoculation • Tissue culture Identified by Neutralization tests • Virus isolation has to be correlated with clinical history
Lab diagnosis • Serological diagnosis : • Rise in titre of antibodies during course of disease • Examine paired sera – Acute – Convalescent (10 -14 days later ) • When Ig. M alone is tested Single sample is enough – Neutralization test – Complement fixation – ELISA – Hemagglutination Inhibition
Immunoprophylaxis • Infection / vaccine Prolonged and effective immunity • Live vaccines more effective than killed vaccines • Successful Live vaccines – Small pox vaccine – Yellow fever vaccine – Polio Vaccine ( Sabin) • Killed vaccines prepared by inactivating viruses using Heat, Phenol, Formalin or BPL • Subunit vaccines – Hepatitis B
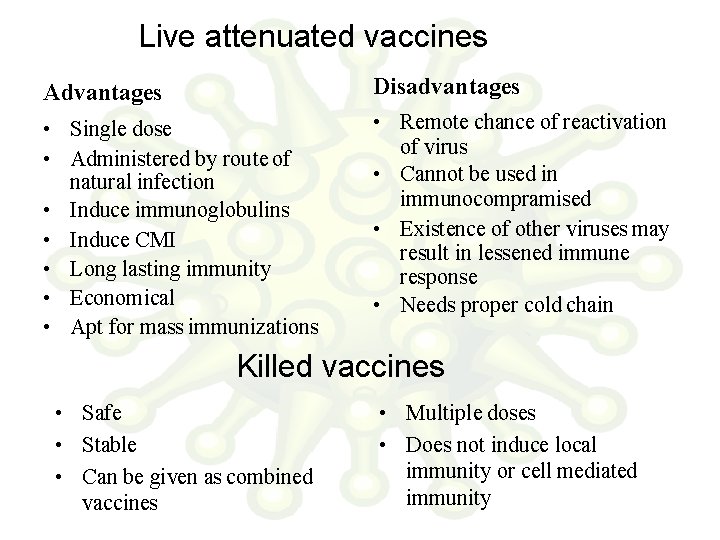
Live attenuated vaccines Advantages Disadvantages • Single dose • Administered by route of natural infection • Induce immunoglobulins • Induce CMI • Long lasting immunity • Economical • Apt for mass immunizations • Remote chance of reactivation of virus • Cannot be used in immunocompramised • Existence of other viruses may result in lessened immune response • Needs proper cold chain Killed vaccines • Safe • Stable • Can be given as combined vaccines • Multiple doses • Does not induce local immunity or cell mediated immunity
Chemoprophylaxis • Challenge Viruses are strictly intracellular , use host mechanisms for replication. Hence therapy would destroy host cell as well • Answer Selective inhibition of viral enzymes – Attachment – Transcription of viral nucleic acid – Translation – Replication – Viral assembly – Release
Antiviral agents • 1960 : First antiviral – Pox virus : Small pox eradicated by vaccination • 1962 : Idoxyuridine : Herpes Keratitis • 1970 : Acyclovir : effective in Herpes • Nucleoside analogues – Deoxyuridines • Idoxyuridine Herpetic keraitis • Trifluridine Less toxic • Bromovinyldeoxyuridine Herpes & Varicella – Adenine arabinoside • Herpetic keratitis • Herpes simplex • VZV – Acyclovir herpes – Ganciclovir Cytomegalovirus – Zidovudine HIV : inhibits viral reverse transcriptase
Antiviral agents • Protease inhibitors – Saquinavir – Ritonovir – Indinavir • Others – Amantidine – blocks cell penetration by influenza A but not by B&C
 Amita arya
Amita arya Amita mehta nasa
Amita mehta nasa Amita mission statement
Amita mission statement Amita dhanda
Amita dhanda Fmla tasc
Fmla tasc Amita prasad ias
Amita prasad ias Definitive host vs intermediate host
Definitive host vs intermediate host Arya kimia
Arya kimia Arya south asia 46m 14msinghtechcrunch
Arya south asia 46m 14msinghtechcrunch Ttp://work4unity.in/haicantik.html
Ttp://work4unity.in/haicantik.html Indo arya dan dravida
Indo arya dan dravida Arya overweight
Arya overweight @arya ia:http://work4unity.in/haicantik.html
@arya ia:http://work4unity.in/haicantik.html Opera arya
Opera arya Kitab suci agama budha adalah . . . *
Kitab suci agama budha adalah . . . * Arya overweight
Arya overweight Continuous bar major connector
Continuous bar major connector Bangsa arya
Bangsa arya Trplice
Trplice An acute highly contagious viral disease
An acute highly contagious viral disease Hepatitis viral
Hepatitis viral Viral receptors
Viral receptors Varicela variola
Varicela variola Vrus
Vrus Eline's viral
Eline's viral Viral gastroenteritis
Viral gastroenteritis Viral
Viral Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Viral life cycle
Viral life cycle Csf meningitis
Csf meningitis Streptococcus
Streptococcus Exocitose
Exocitose Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Section 24-1 viral structure and replication
Section 24-1 viral structure and replication Andrew lippman mit
Andrew lippman mit