TREATMENT OPTIONS FOR DVT PE IN THE POSTOP
- Slides: 31
TREATMENT OPTIONS FOR DVT & PE IN THE POST-OP PERIOD Isabella Mor August 2004
INTRODUCTION n Post-op incidence of DVT varies with type of surgery: q q q n n n 3 -51% with general abdominal surgery 35% with trauma 45 -60% in hip replacement Pulmonary embolus accounts for 3% surgical inpatient deaths 24% of 5477 surgical patients in an autopsy series Mortality 2 – 30% Tai et al(1999)BJS
CASE STUDY n n n Mrs JN, 43 yo Laparoscopic panproctocolectomy for UC Lithotomy position SC heparin on induction No SCDs Long procedure
n Day 3 post op: q q Sudden onset SOB Hypoxia and tachypnoea Tachycardia L calf pain
n ECG
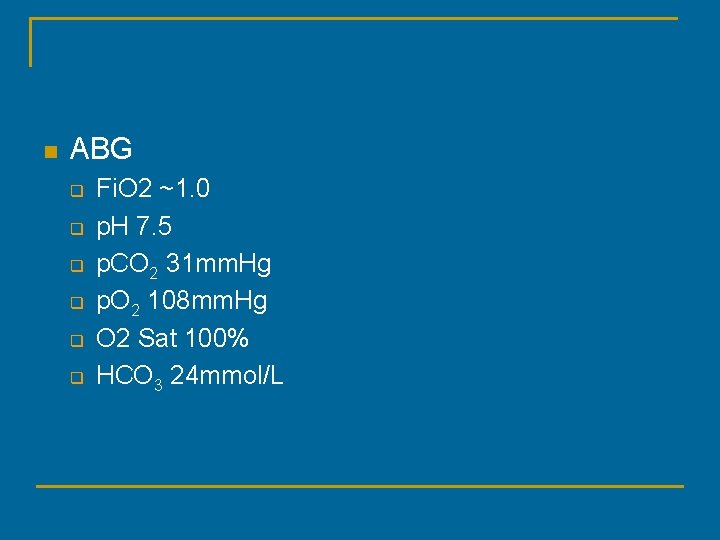
n ABG q q q Fi. O 2 ~1. 0 p. H 7. 5 p. CO 2 31 mm. Hg p. O 2 108 mm. Hg O 2 Sat 100% HCO 3 24 mmol/L
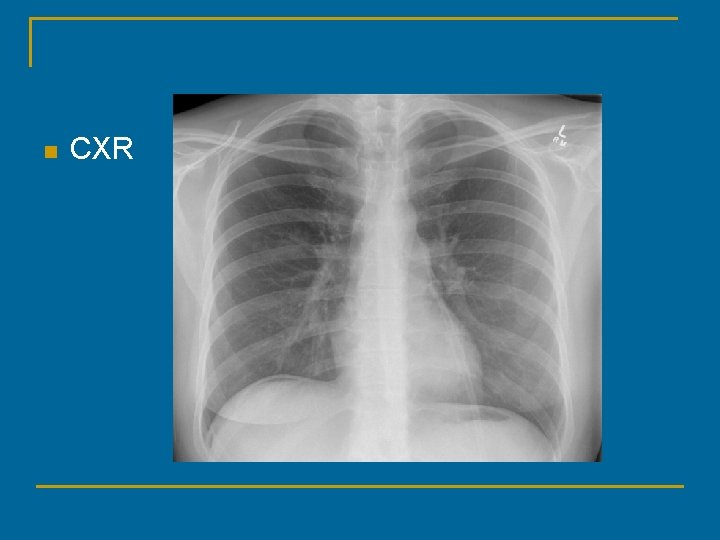
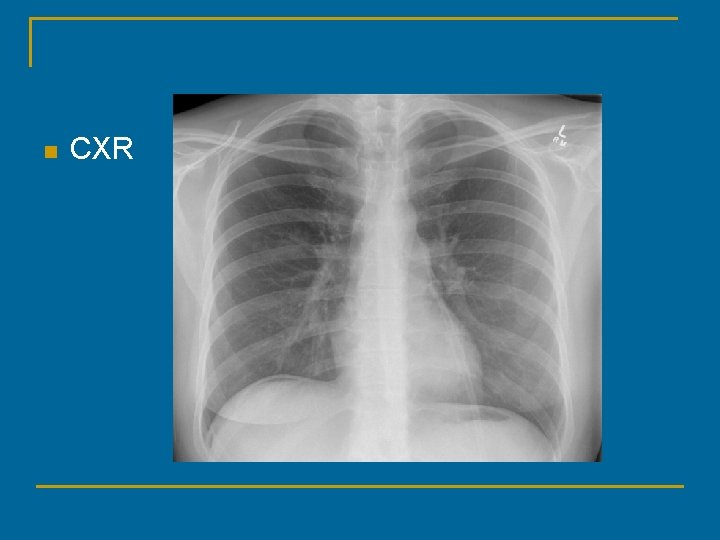
n CXR
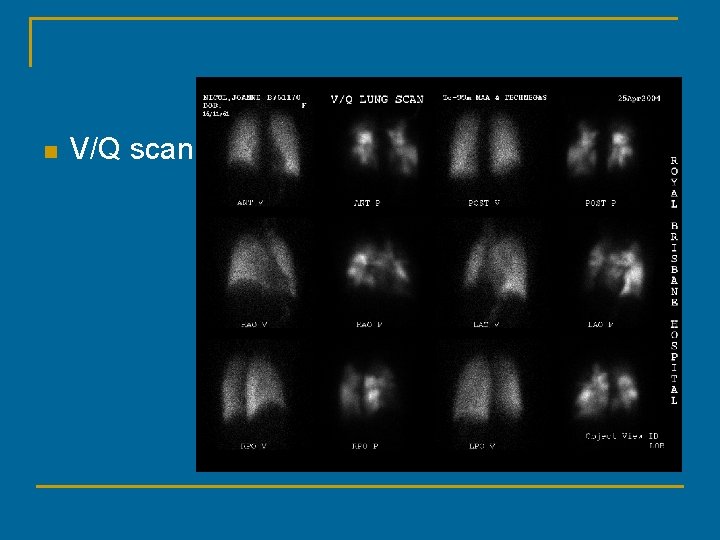
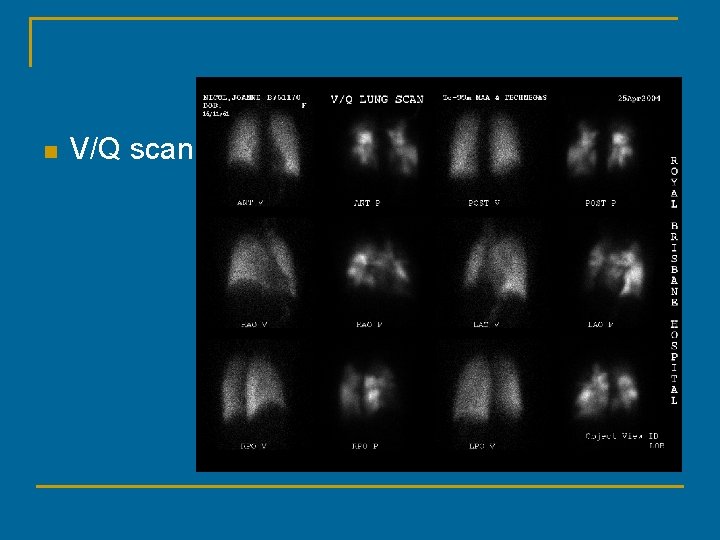
n V/Q scan
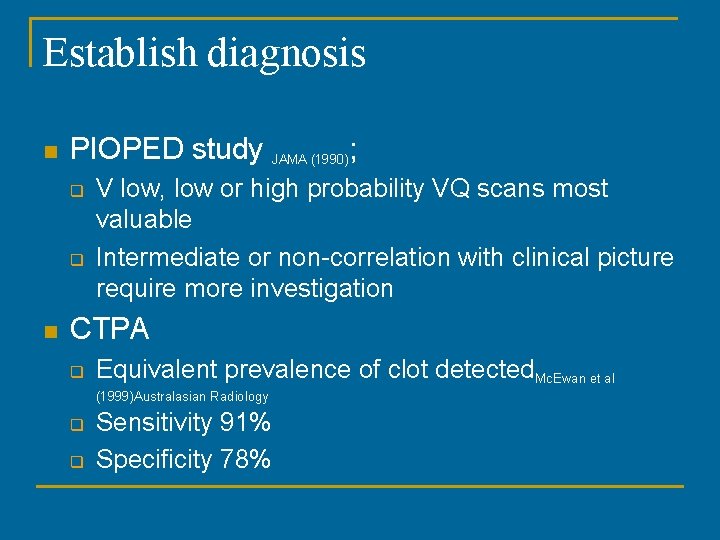
Establish diagnosis n PIOPED study JAMA (1990); q q n V low, low or high probability VQ scans most valuable Intermediate or non-correlation with clinical picture require more investigation CTPA q Equivalent prevalence of clot detected. Mc. Ewan et al (1999)Australasian Radiology q q Sensitivity 91% Specificity 78%
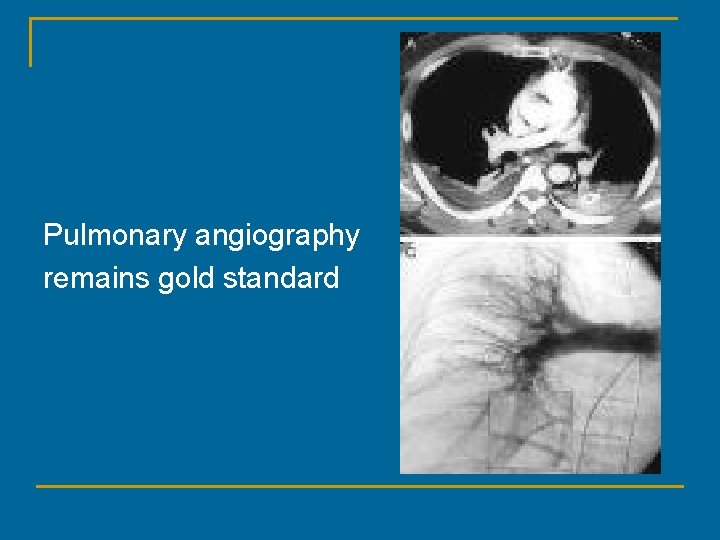
Pulmonary angiography remains gold standard
n Duplex ultrasound of lower limb veins q q Source of 90% PE Independent indication for treatment >95% sensitive 98% specific
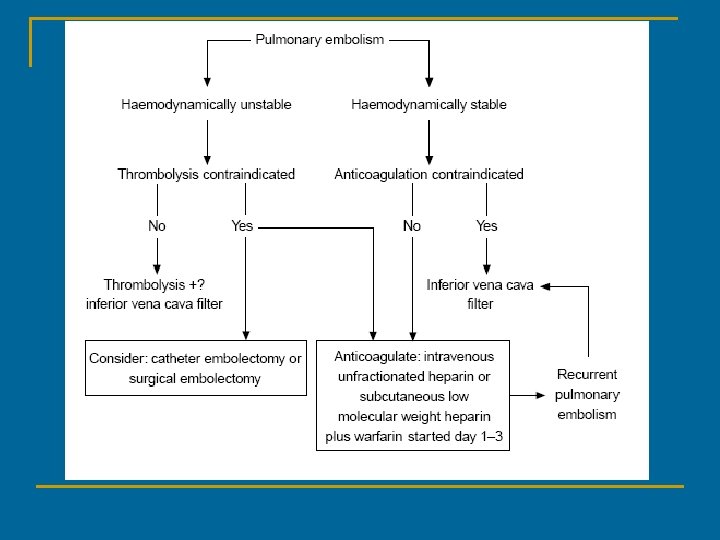
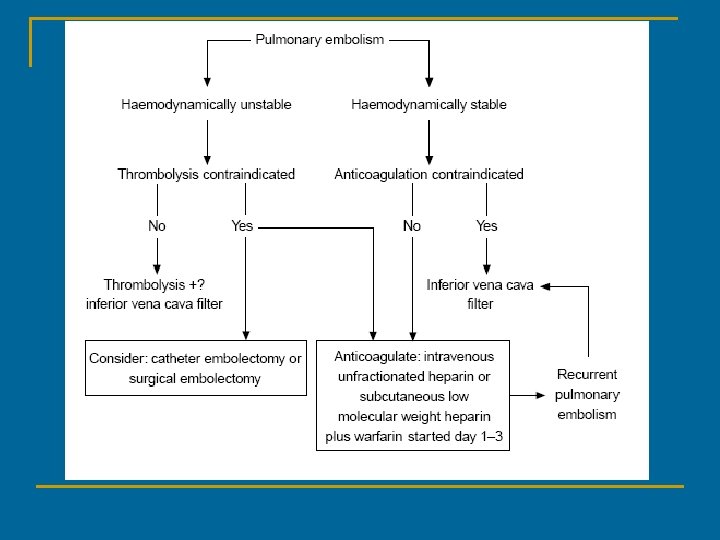
Initial Management n n n Depends on size of embolus and patient’s underlying cardiorespiratory comorbidities Oxygen +/- mechanical ventilation Analgesia for pleuritic pain, avoid opioids IV fluid / inotropic support CVP monitoring & maintenance of high RA pressures
Anticoagulation n n Standard therapy Reduce risk of further PE, does not treat existing clot Allows endogenous thrombolysis High clinical suspicion, start treatment immediately
Heparin n Unfractionated heparin q q q n Infusion or BD dosing to prolong APTT 1. 5 -2. 5 times normal Ability to “turn on & off” Completely reversible with protamine LMWH q q Lower risk of thrombotic & haemorrhagic complications Baglin (2001)Clinical Medicine Suitable for outpatient management
Warfarin n n Start within 3/7 of commencing treatment Paradoxical hypercoagulability in 1 st 24 hr Standard protocol for anticoagulation Target INR 2. 5 q Lowest thromboembolic recurrence & bleeding Baglin(2001) Clinical Medicine
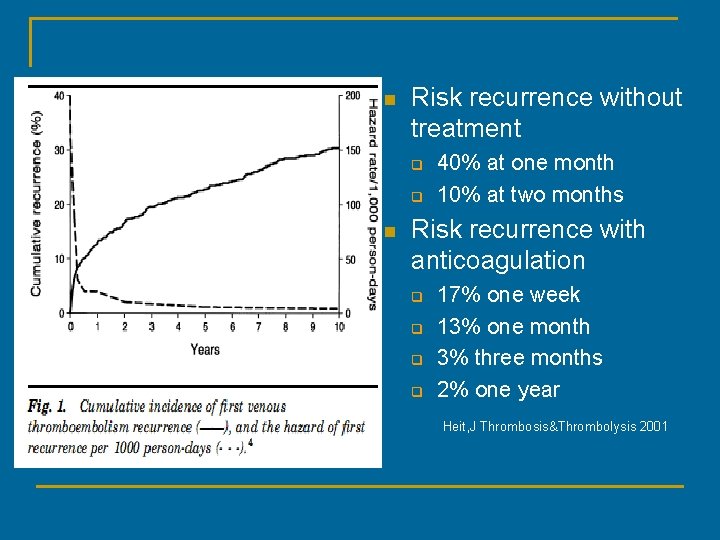
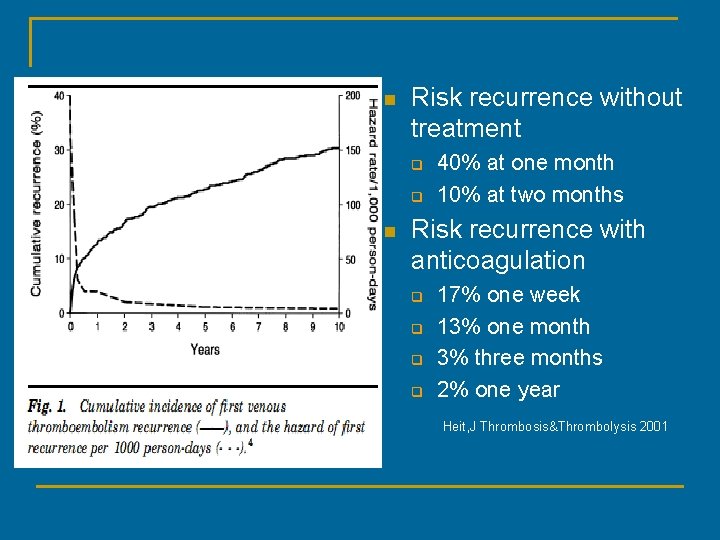
n Risk recurrence without treatment q q n 40% at one month 10% at two months Risk recurrence with anticoagulation q q 17% one week 13% one month 3% three months 2% one year Heit, J Thrombosis&Thrombolysis 2001
Duration of treatment n Research committee of the British Thoracic Society Lancet(1992) q Post-op cohort treatment failure and recurrence was 3% with anticoagulation for 4 weeks or 3 months
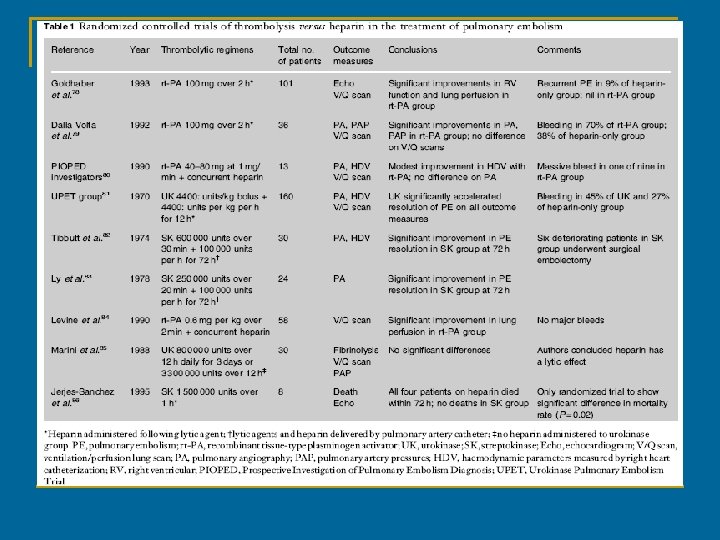
Thrombolysis n n n Massive PE Haemodynamic instability Agents: q Streptokinase, urokinase, r-TPA
Thrombolysis n Advantages: q q q n Early improvement in haemodynamic measures Effective in established clot Valve preservation Disadvantages: q q No evidence of long term benefit Four fold increased risk of bleeding Baglin(2001)Clinical Medicine
Thrombolysis n Regional administration q n No improvement in clot resolution TPA + pulmonary endothelium antibody Ding etal(2003)Circulation q q q Monoclonal antibody developed from membrane proteins of pulmonary vascular endothelium of rats In vivo biodistribution showed the ab & it’s conjugate urokinase rapidly and specifically accumulated in lung Compared in rats with pulmonary, hepatic and lower limb emboli n n Efficient thrombolysis in pulmonary model with no change to plasma fibrinogen or bleeding time No thrombolysis induced in the other 2 models
Caval Filter n n Aim to prevent PE Absolute indications: q q n Absolute contraindication to anticoagulation Failure of anticoagulation Relative indications: q q Thrombolysis Proximal free floating thrombus
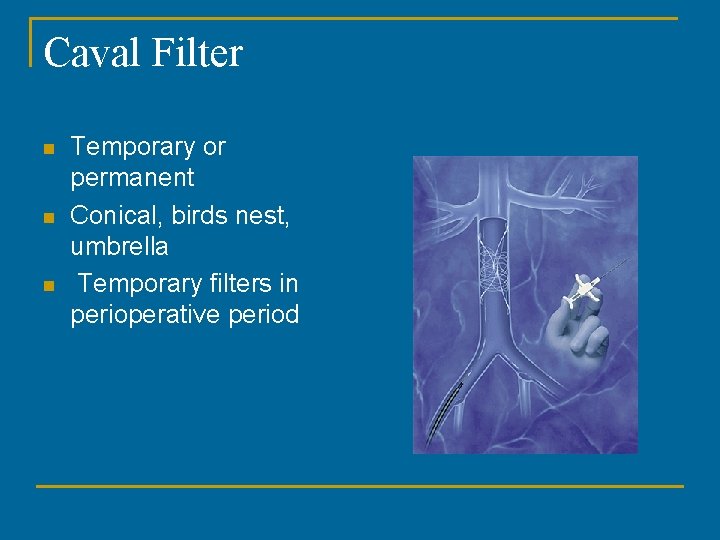
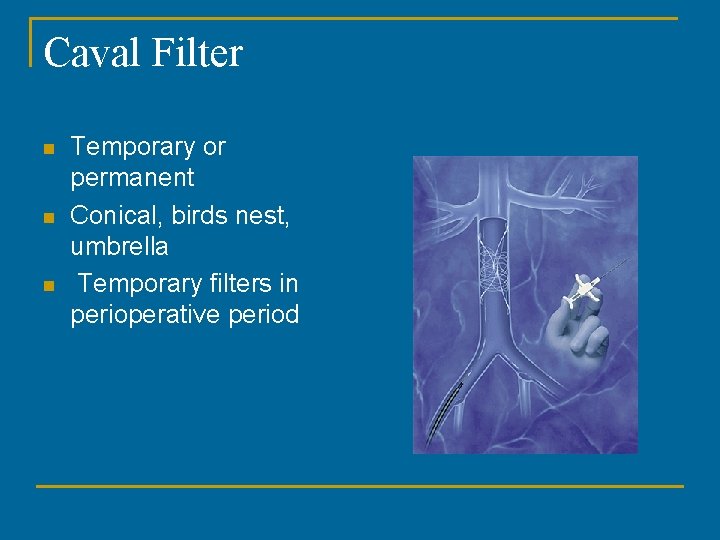
Caval Filter n n n Temporary or permanent Conical, birds nest, umbrella Temporary filters in perioperative period
Caval Filter n Risks/Complications q q q Filter migration Filter embolism Caval perforation Recurrent DVT/caval obstruction Postphlebitic syndrome Structural failure
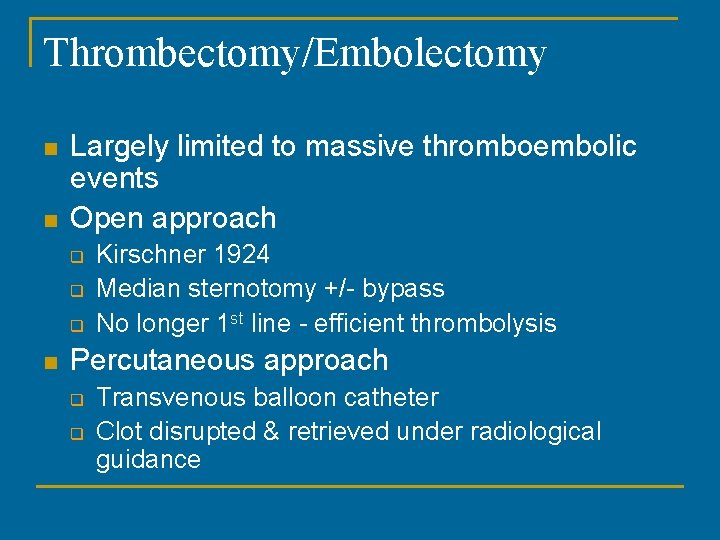
Thrombectomy/Embolectomy n n Largely limited to massive thromboembolic events Open approach q q q n Kirschner 1924 Median sternotomy +/- bypass No longer 1 st line - efficient thrombolysis Percutaneous approach q q Transvenous balloon catheter Clot disrupted & retrieved under radiological guidance
Prevention n n Incidence of VTE in post op period underestimated (due to admission/treatment elsewhere) Screening, eg duplex ultrasound lower limb veins not cost effective
Non-pharmacological prevention n Early ambulation Elastic stockings Intermittent pneumatic compression devices
Pharmacological prevention n Low dose unfractionated heparin Low molecular weight heparin Duration q q Should be started pre-op Optimum duration not known
Summary n n PE is a potentially fatal complication of surgery 3% surgical inpatient deaths Anticoagulation mainstay of treatment Prevention is better than cure
References n n n n Baglin, T. Evidence-based Management of Deep Vein Thrombosis and Pulmonary Embolus Clinical Medicine 2001; 1(6): 438 -40 British Thoracic Society Research Committee Optimum Duration of Anticoagulation for DVT & PE Lancet 1992; 340(8824): 873 -6 Ding, BS. , Zhou, YJ. , Chen, XY. , Zhang, J. , Zhang, PX. , Sun, ZY. , Tan, XY. & Liu, JN. , Lung Endothelium Targeting for Pulmonary Embolism and Thombolysis Circulation 2003; 108(23): 2892 -8 Heit, JA. , Perioperative Management of the Chronically Anticoagulated Patient Journal of Thrombosis and Thrombolysis 2001; 12(1): 81 -87 Kaboli, P. , Henderson, M. & White, R. , DVT Prophylaxis and Anticoagulation in the Surgical Patient The Medical Clinics of North America 2003; 87: 77 -110 Mc. Ewan, L. , Gandhi, M. , Anderson, J. & Manthey, K. , Can CT Pulmonary Angiography Replace Ventilation-Perfusion Scans as a First Line Investigation for Pulmonary Emboli? Australasian Radiology 1999; 43: 311 -314 PIOPED study results published Journal of the American Medical Association 1990; 263: 2753 -9 Tai, NRM. , Atwal, AS. & Hamilton, G. , Modern Management of Pulmonary Embolism British Journal of Surgery 1999; 86(7): 853 -868