1 Q l Postop Endophthalmitis after CE l
![1 Q l Post-op Endophthalmitis after CE l Acute = Within [time frame] l 1 Q l Post-op Endophthalmitis after CE l Acute = Within [time frame] l](https://slidetodoc.com/presentation_image_h/331265715c2e21043fc5dd723d2c0293/image-1.jpg)







































- Slides: 167
![1 Q l Postop Endophthalmitis after CE l Acute Within time frame l 1 Q l Post-op Endophthalmitis after CE l Acute = Within [time frame] l](https://slidetodoc.com/presentation_image_h/331265715c2e21043fc5dd723d2c0293/image-1.jpg)
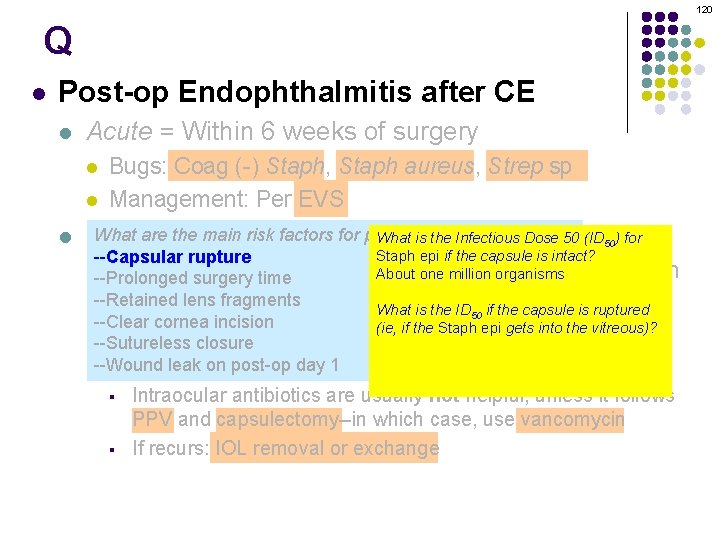
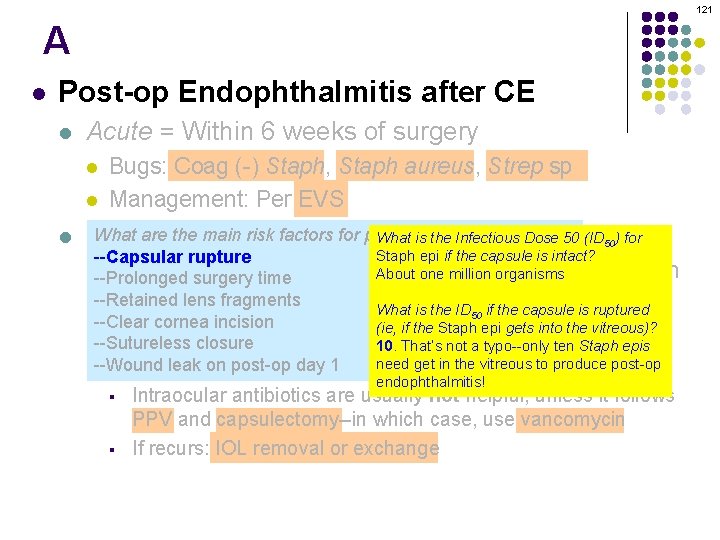
1 Q l Post-op Endophthalmitis after CE l Acute = Within [time frame] l l l (Cataract extraction) Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than [time frame] e
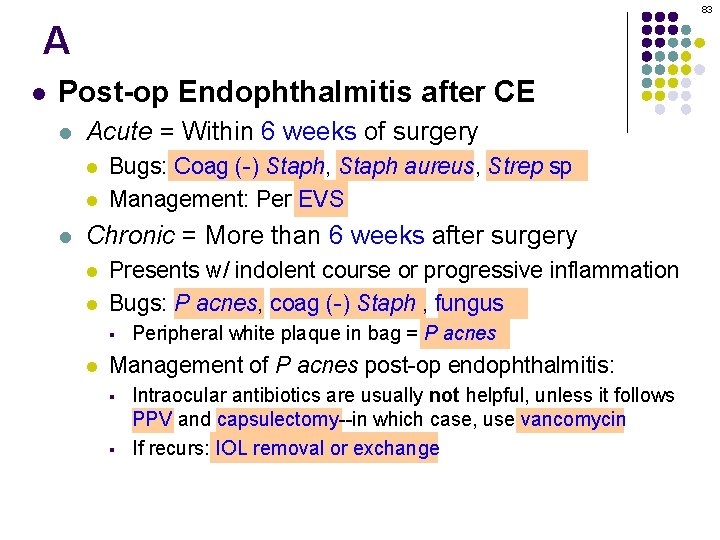
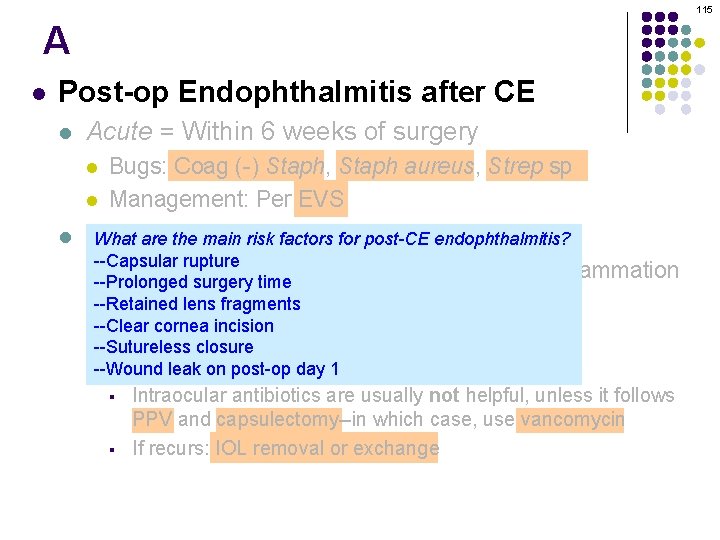
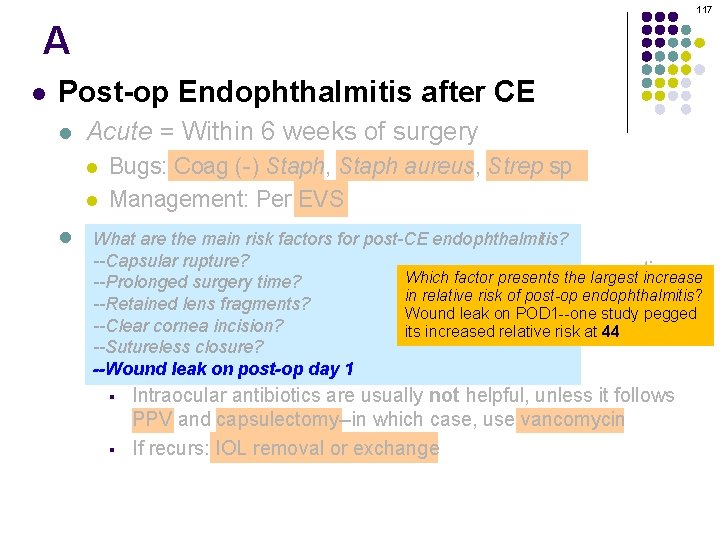
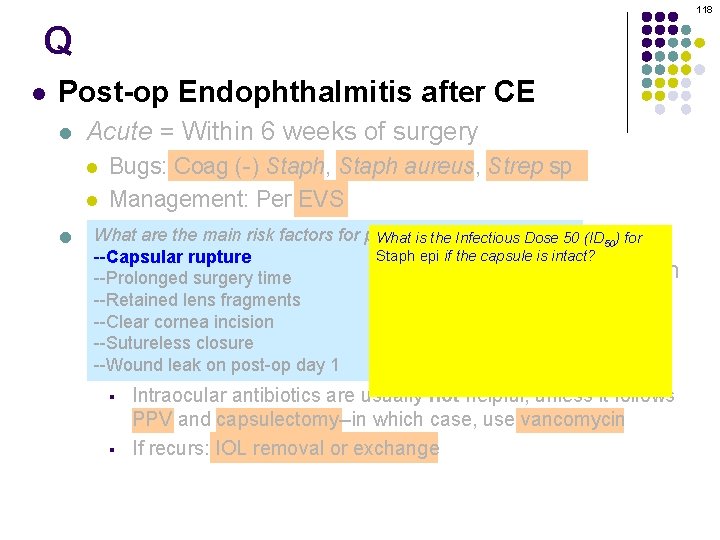
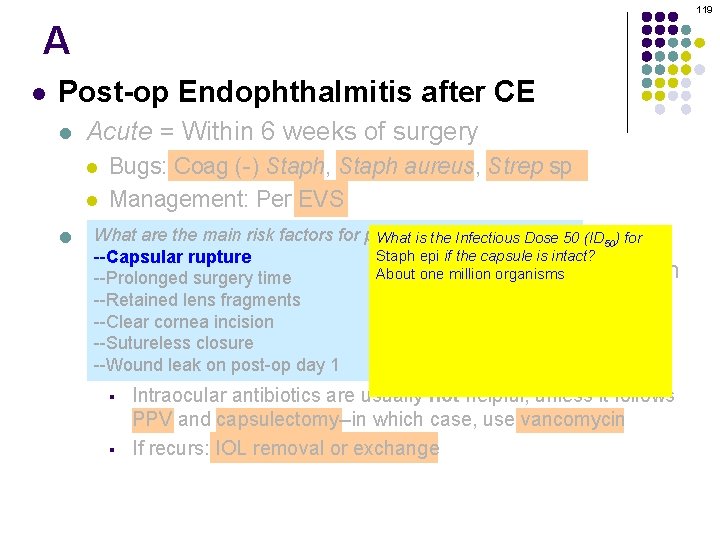
2 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery
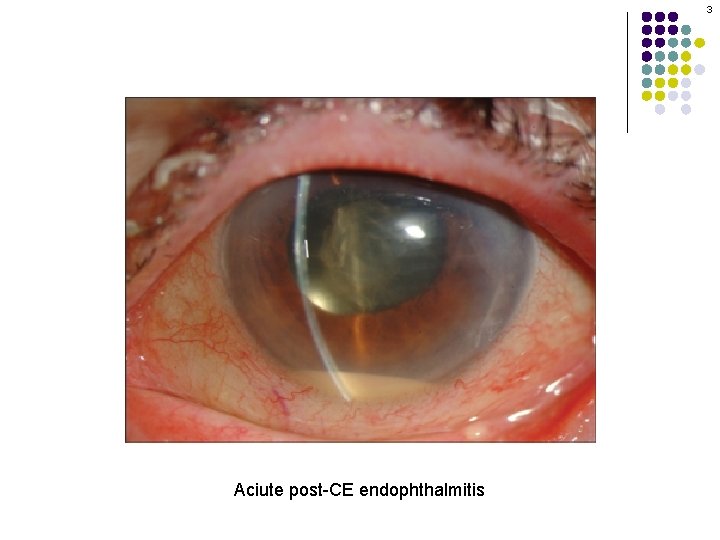
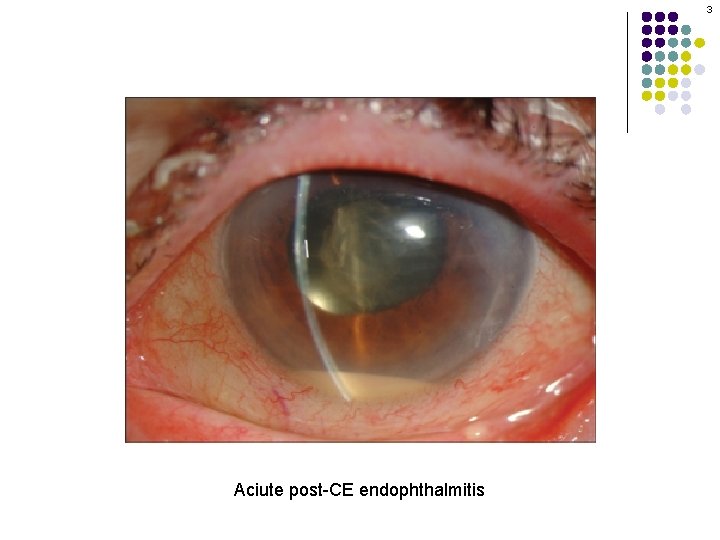
3 Aciute post-CE endophthalmitis
4 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Is post-op CE endophthalmitis more likely to occur in right eyes, or left? Right What proportion of post-CE endophthalmitis cases occur in right eyes? Estimates run as high as 86%! Why should it be more common in right eyes? It’s probably because most surgeons are right-handed, and therefore they place the main surgical wound OD at the inferior aspect of the cornea. Thus, this wound is in contact with the tear lake, meaning pathogens swimming therein have ready access to it. This increases the likelihood of pathogens entering the eye.
5 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Is post-op CE endophthalmitis more likely to occur in right eyes, or left? Right What proportion of post-CE endophthalmitis cases occur in right eyes? Estimates run as high as 86%! Why should it be more common in right eyes? It’s probably because most surgeons are right-handed, and therefore they place the main surgical wound OD at the inferior aspect of the cornea. Thus, this wound is in contact with the tear lake, meaning pathogens swimming therein have ready access to it. This increases the likelihood of pathogens entering the eye.
6 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Is post-op CE endophthalmitis more likely to occur in right eyes, or left? Right What proportion of post-CE endophthalmitis cases occur in right eyes? Estimates run as high as 86%! Why should it be more common in right eyes? It’s probably because most surgeons are right-handed, and therefore they place the main surgical wound OD at the inferior aspect of the cornea. Thus, this wound is in contact with the tear lake, meaning pathogens swimming therein have ready access to it. This increases the likelihood of pathogens entering the eye.
7 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Is post-op CE endophthalmitis more likely to occur in right eyes, or left? Right What proportion of post-CE endophthalmitis cases occur in right eyes? Estimates run as high as 86%! Why should it be more common in right eyes? It’s probably because most surgeons are right-handed, and therefore they place the main surgical wound OD at the inferior aspect of the cornea. Thus, this wound is in contact with the tear lake, meaning pathogens swimming therein have ready access to it. This increases the likelihood of pathogens entering the eye.

8 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Is post-op CE endophthalmitis more likely to occur in right eyes, or left? Right What proportion of post-CE endophthalmitis cases occur in right eyes? Estimates run as high as 86%! Why should it be more common in right eyes? It’s probably because most surgeons are right-handed, and therefore they place the main surgical wound OD at the inferior aspect of the cornea. Thus, this wound is in contact with the tear lake, meaning pathogens swimming therein have ready access to it. This increases the likelihood of pathogens entering the eye.
9 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Is post-op CE endophthalmitis more likely to occur in right eyes, or left? Right What proportion of post-CE endophthalmitis cases occur in right eyes? Estimates run as high as 86%! Why should it be more common in right eyes? It’s probably because most surgeons are right-handed, and therefore they place the main surgical wound OD at the inferior aspect of the cornea. Thus, this wound is in contact with the tear lake, meaning pathogens swimming therein have ready access to it. This increases the likelihood of pathogens entering the eye.
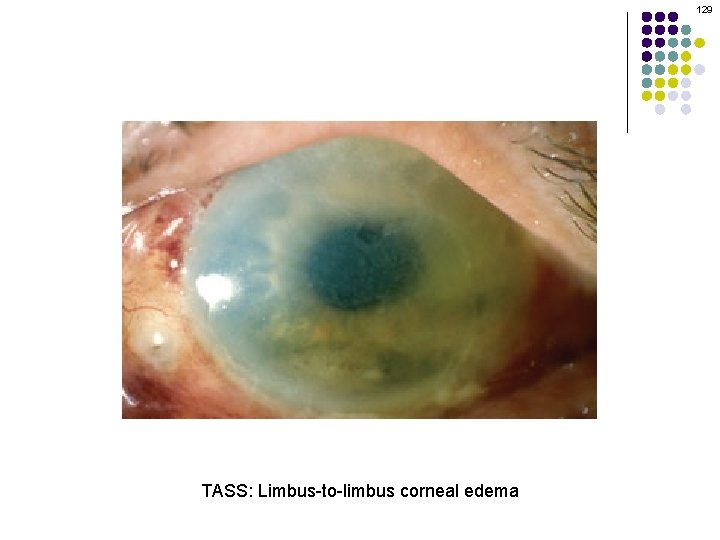
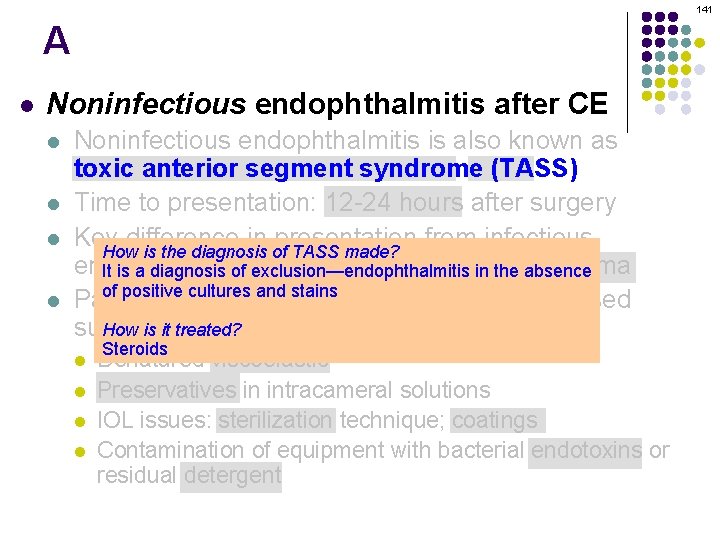
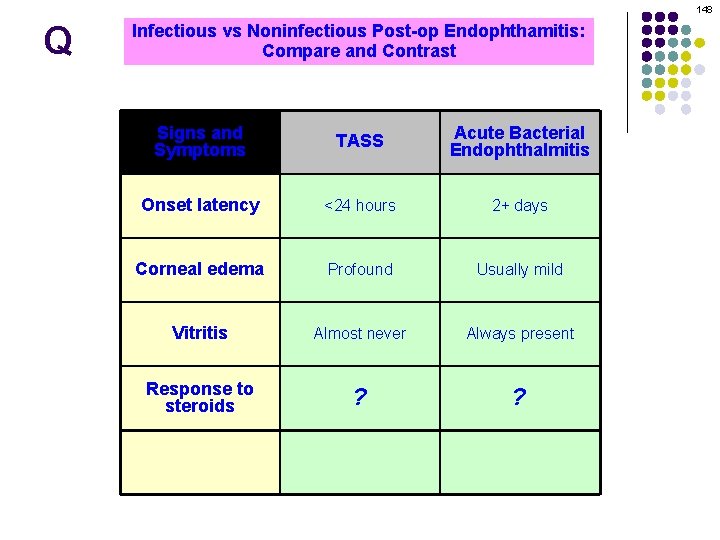
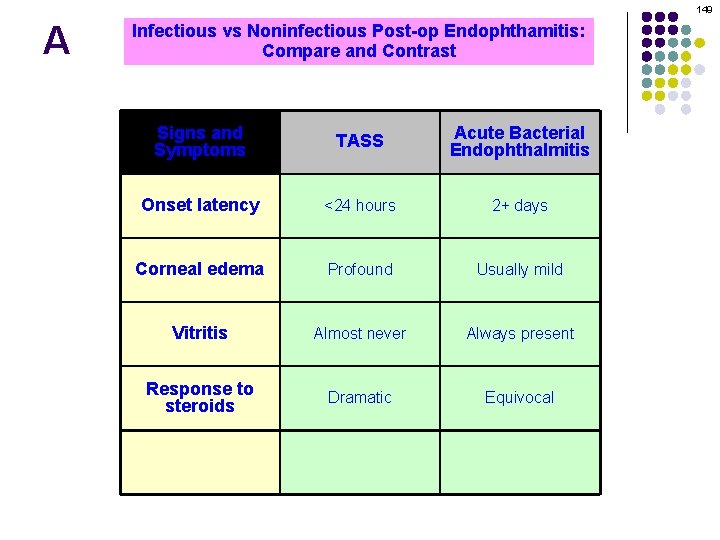
10 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)

11 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)
12 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)
13 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)
14 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)
15 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)
16 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)
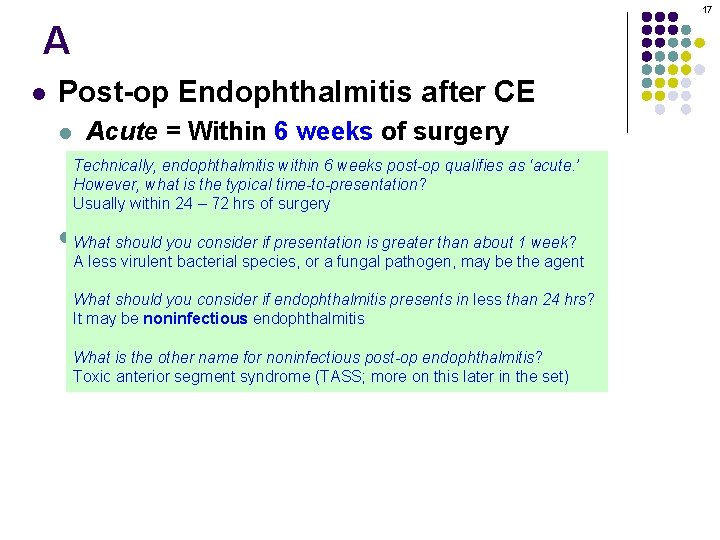
17 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Technically, within 6 weeks qualifies as ‘acute. ’ l Bugs: endophthalmitis Coag (-) Staph, Staphpost-op aureus, Strep sp However, what is the typical time-to-presentation? l Management: EVS Usually within 24 – 72 hrs Per of surgery l What Chronic =consider Moreif than 6 weeks surgery should you presentation is greaterafter than about 1 week? A less virulent bacterial species, or a fungal pathogen, may be the agent l Presents w/ indolent course or progressive What should you consider if endophthalmitis presents in less than 24 hrs? It may be noninfectious endophthalmitis What is the other name for noninfectious post-op endophthalmitis? Toxic anterior segment syndrome (TASS; more on this later in the set)
18 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P. acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

19 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P. acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
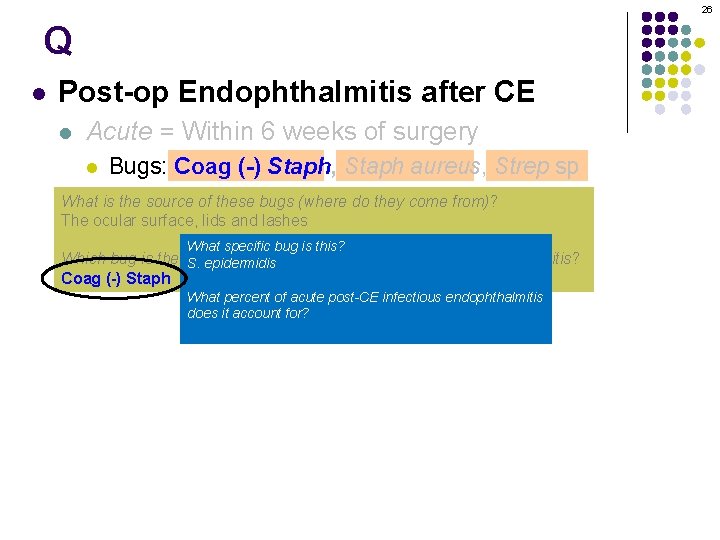
20 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic = More than 6 weeks after surgery Which bug is the most common cause of acute post-CE endophthalmitis? l (-) Presents w/ indolent course or progressive inflammation Coag Staph
21 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic = More than 6 weeks after surgery Which bug is the most common cause of acute post-CE endophthalmitis? l (-) Presents w/ indolent course or progressive inflammation Coag Staph
22 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic = More than 6 weeks after surgery Which bug is the most common cause of acute post-CE endophthalmitis? l (-) Presents w/ indolent course or progressive inflammation Coag Staph
23 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic = More than 6 weeks after surgery Which bug is the most common cause of acute post-CE endophthalmitis? l (-) Presents w/ indolent course or progressive inflammation Coag Staph

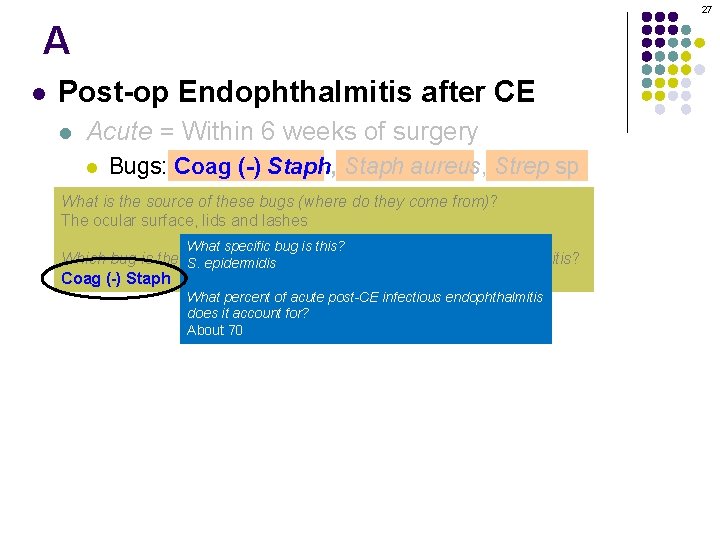
24 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic =What More than 6 weeks after surgery specific bug is this? Which bug is the most common cause of acute post-CE endophthalmitis? S. epidermidis l Presents w/ indolent course or progressive inflammation, Coag (-) Staph fungus What percent of acute post-CE infectious endophthalmitis does it account for? About 70
25 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic =What More than 6 weeks after surgery specific bug is this? Which bug is the most common cause of acute post-CE endophthalmitis? S. epidermidis l Presents w/ indolent course or progressive inflammation, Coag (-) Staph fungus What percent of acute post-CE infectious endophthalmitis does it account for? About 70
26 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic =What More than 6 weeks after surgery specific bug is this? Which bug is the most common cause of acute post-CE endophthalmitis? S. epidermidis l Presents w/ indolent course or progressive inflammation, Coag (-) Staph fungus What percent of acute post-CE infectious endophthalmitis does it account for? About 70
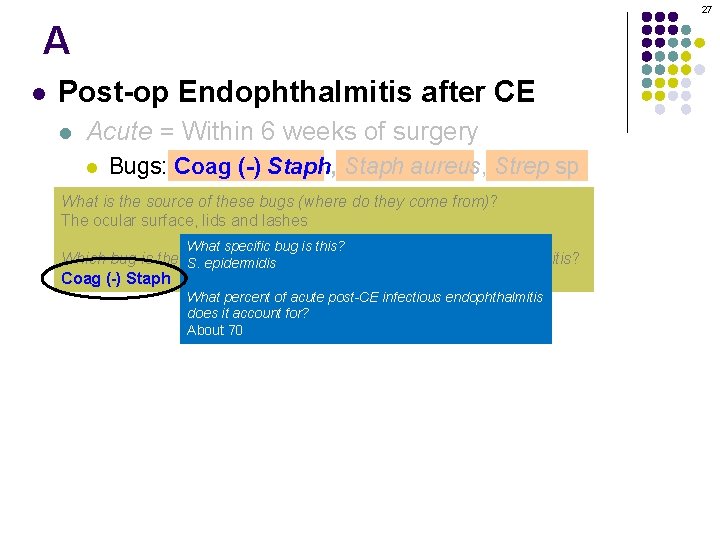
27 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery Bugs: Coag (-) Staph, Staph aureus, Strep sp What the source of these Per bugs EVS (where do they come from)? l is. Management: l The ocular surface, lids and lashes l Chronic =What More than 6 weeks after surgery specific bug is this? Which bug is the most common cause of acute post-CE endophthalmitis? S. epidermidis l Presents w/ indolent course or progressive inflammation, Coag (-) Staph fungus What percent of acute post-CE infectious endophthalmitis does it account for? About 70
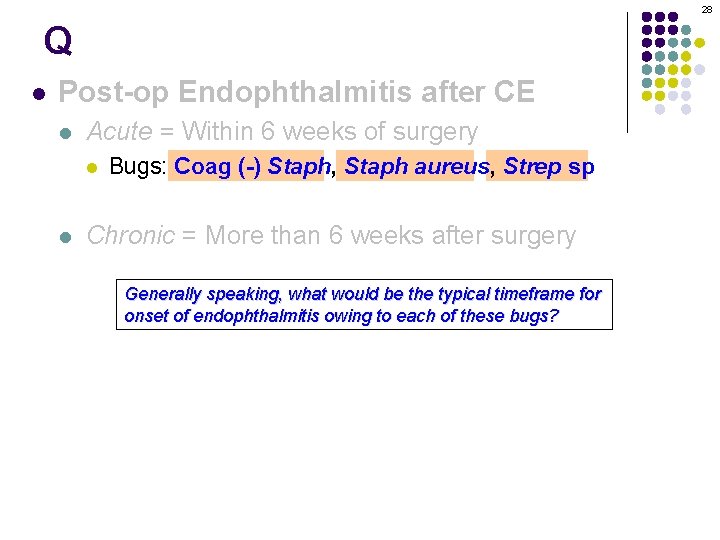
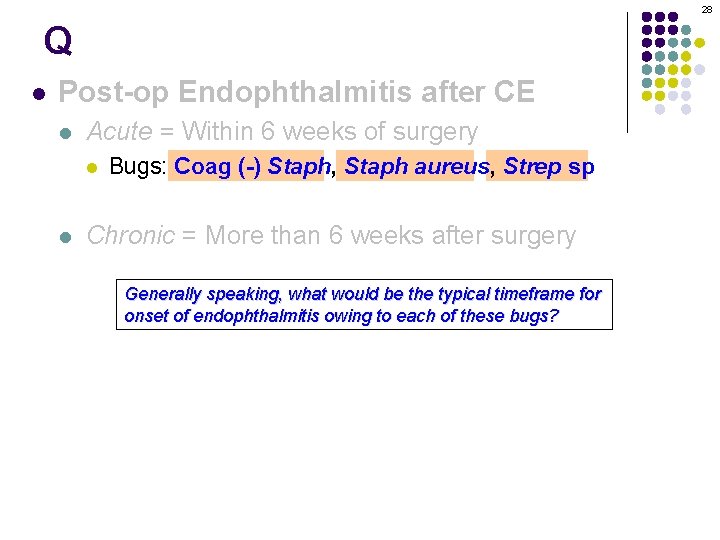
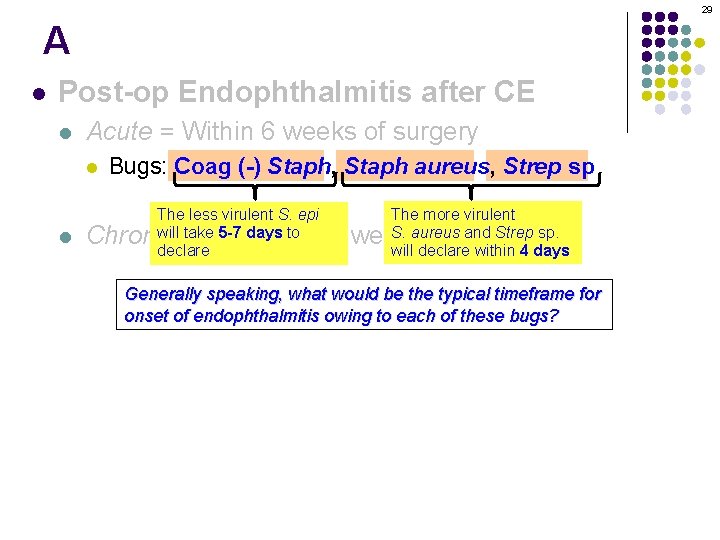
28 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Generally speaking, what would be the typical timeframe for Bugs: P. acnes, coag (-) Staph , fungus onset of endophthalmitis owing to each of these bugs? § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
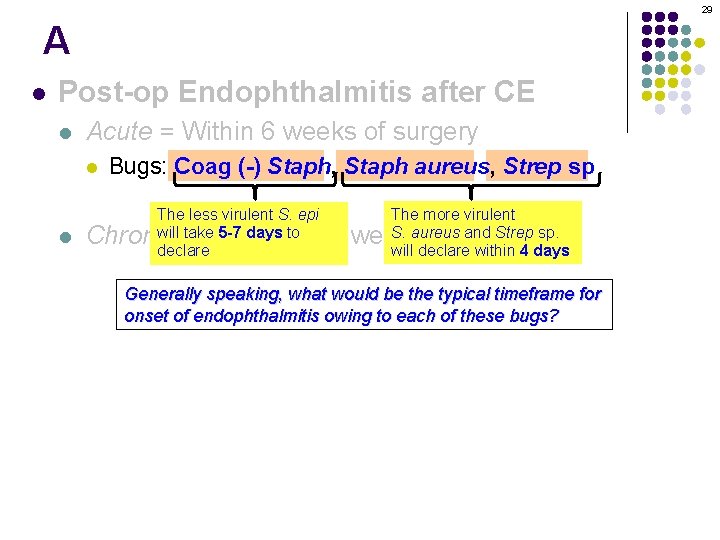
29 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS The less virulent S. epi will take 5 -7 days to declare The more virulent S. aureus and Strep sp. will declare within 4 days Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Generally speaking, what would be the typical timeframe for Bugs: P. acnes, coag (-) Staph , fungus onset of endophthalmitis owing to each of these bugs? § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
30 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp study (abb. ) Management: Per EVS Chronic = More than 6 weeks after surgery
31 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgerye
32 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1)…what is the role of PPV? § Peripheral white plaque in bag = P. acnes 2)…how effective are systemic antibiotics? l Management: In evaluating PPV efficacy, what was it compared to? PPV vs intravitreal antibiotics § Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

33 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1)…what is the role of PPV? § Peripheral white plaque in bag = P. acnes 2)…how effective are systemic antibiotics? l Management: In evaluating PPV efficacy, what was it compared to? PPV vs intravitreal antibiotics § Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
34 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of… [surgical procedure] § Peripheral 2)) How effective are… white plaque in bag = P. acnes l Management: In evaluating PPV efficacy, what was it compared to? PPV vs intravitreal antibiotics § Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

35 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral whiteantibiotics? plaque in bag = P. acnes (pars plana vitrectomy) 2) How effective are…systemic l Management: In evaluating PPV efficacy, what was it compared to? PPV vs intravitreal antibiotics § Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
36 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are… l Management: In evaluating PPV efficacy, what was it compared to? PPV vs intravitreal antibiotics § Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
37 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral whiteantibiotics? plaque in bag = P. acnes 2) How effective are…systemic l Management: In evaluating PPV efficacy, what was it compared to? PPV vs intravitreal antibiotics § Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
38 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral whiteantibiotics? plaque in bag = P. acnes 2) How effective are…systemic l Management: In evaluating PPV, what was it compared to? PPV vs intravitreal antibiotics § Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
39 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral whiteantibiotics? plaque in bag = P. acnes 2) How effective are…systemic l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually § § not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
40 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral whiteantibiotics? plaque in bag = P. acnes 2) How effective are…systemic l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually PPV and subtotal capsulectomy not helpful, unless it follows What did the study show with respect to PPV efficacy? Did it improve visual outcomes? Depends—if VA was LP or worse at presentation, PPV. § Use vancomycin 1 mg, either invisual the outcome vitreouswas or better in thewith bag However, if VA was better than LP, there was no difference between the PPV and § If recurs: Total capsulectomy with IOL removal or exchange intravitreal-antibiotics-only groups with respect to final visual outcome.
41 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral whiteantibiotics? plaque in bag = P. acnes 2) How effective are…systemic l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually PPV and subtotal capsulectomy not helpful, unless it follows What did the study show with respect to PPV efficacy? Did it improve visual outcomes? Depends—if VA was LP or worse at presentation, PPV. § Use vancomycin 1 mg, either invisual the outcome vitreouswas or better in thewith bag However, if VA was better than LP, there was no difference between the PPV and § If recurs: Total capsulectomy with IOL removal or exchange intravitreal-antibiotics-only groups with respect to final visual outcome.
42 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral whiteantibiotics? plaque in bag = P. acnes 2) How effective are…systemic l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually PPV and subtotal capsulectomy not helpful, unless it follows What did the study show with respect to PPV efficacy? Did it improve visual outcomes? Depends—if VA was LP or worse at presentation, PPV. § Use vancomycin 1 mg, either invisual the outcome vitreouswas or better in thewith bag However, if VA was better than LP, there was no difference between the PPV and § If recurs: Total capsulectomy with IOL removal or exchange intravitreal-antibiotics-only groups with respect to final visual outcome.

43 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy IV improve final visual outcome IV antibioticsdid didnot improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag § If recurs: Total capsulectomy with IOL removal or exchange
44 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy Intravenous antibiotics did not improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag § If recurs: Total capsulectomy with IOL removal or exchange
45 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy Intravenous antibiotics did not improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag Why was this conclusion controversial? § Ifused recurs: Total capsulectomy IOL. The removal exchange The antibiotics in the EVS were ceftazidime and with amikacin EVS wasor criticized for the choice of Ceftaz over vancomycin , which has better coverage of Gram+ cocci. Because of this, the effectiveness of IV abx remains an open question for many clinicians.

46 Q/A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy Intravenous antibiotics did not improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag Why was this conclusion controversial? § Ifused recurs: Total capsulectomy IOL. The removal exchange The antibiotics in the EVS were ceftazidime and with amikacin EVS wasor criticized for the choice of Ceftaz over vancomycin , which has better coverage of Gram+ cocci. Because of this, the effectiveness of IV abx remains an open question for many clinicians.

47 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy Intravenous antibiotics did not improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag Why was this conclusion controversial? § Ifused recurs: Total capsulectomy IOL. The removal exchange The antibiotics in the EVS were ceftazidime and with amikacin EVS wasor criticized for the choice of Ceftaz over vancomycin , which has better coverage of Gram+ cocci. Because of this, the effectiveness of IV abx remains an open question for many clinicians.

48 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy Intravenous antibiotics did not improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag Why was this conclusion controversial? § Ifused recurs: Total capsulectomy IOL. The removal exchange The antibiotics in the EVS were ceftazidime and with amikacin EVS wasor criticized for the choice of Ceftaz over vancomycin , which has better coverage of Gram+ cocci. Because of this, the effectiveness of IV abx remains an open question for many clinicians.
49 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy Intravenous antibiotics did not improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag Why was this conclusion controversial? § Ifused recurs: Total capsulectomy IOL. The removal exchange The antibiotics in the EVS were ceftazidime and with amikacin EVS wasor criticized for the choice of Ceftaz over vancomycin , which has better coverage of Gram+ cocci. Because of this, the effectiveness of IV abx remains an open question for many clinicians.
50 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery What l does EVS stand for? Endophthalmitis Vitrectomy Study l Presents w/ indolent course or progressive inflammation What questions did the EVS seek to answer? With respect to the. P. management of acute(-) post-CE infectious endophthalmitis: l Bugs: acnes, coag Staph , fungus 1) What is the role of…PPV? § Peripheral white plaque in bag = P. acnes 2) How effective are…systemic antibiotics? l Management: In evaluating PPV, what was it compared to? Intravitreal § antibiotics Intravitreal antibiotics are usually not helpful, unless it follows What did the PPV study and show subtotal with respect to systemic antibiotics and visual outcome? capsulectomy Intravenous antibiotics did not improve final visual outcome § Use vancomycin 1 mg, either in the vitreous or in the bag Why was this conclusion controversial? § Ifused recurs: Total capsulectomy IOL. The removal exchange The antibiotics in the EVS were ceftazidime and with amikacin EVS wasor criticized for the choice of Ceftaz over vancomycin , which has better coverage of Gram+ cocci. Because of this, the effectiveness of IV abx remains an open question for many clinicians.
51 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Alpatient s/p CE 6 months prior presents with endophthalmitis. Should EVS findings dictate management? l Presents w/ indolent course or progressive inflammation Not necessarily. The EVS addressed endophthalmitis developing within 6 weeks of CE, so extrapolation thisacnes, situation coag would constitute ‘off label use’ l Bugs: to. P. (-) Staph , fungus § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
52 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Alpatient s/p CE 6 months prior presents with endophthalmitis. Should EVS findings dictate management? l Presents w/ indolent course or progressive inflammation Not necessarily. The EVS addressed endophthalmitis developing within 6 weeks of CE, so extrapolation thisacnes, situation coag would constitute ‘off label use. ’ l Bugs: to. P. (-) Staph , fungus § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

53 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Alpatient s/p CE 6 months prior presents with endophthalmitis. Should EVS findings dictate management? l Presents w/ indolent course or progressive inflammation Not necessarily. The EVS addressed endophthalmitis developing within 6 weeks of CE, so extrapolation thisacnes, situation coag would constitute ‘off label use. ’ l Bugs: to. P. (-) Staph , fungus § Peripheral white plaque in bag = P. acnes A patient s/p trab 3 weeks prior presents with endophthalmitis. Should EVS findings Management: dictatelmanagement? Again, not The EVS addressed after CE. unless As in theit previous § necessarily. Intravitreal antibiotics are endophthalmitis usually not helpful, follows scenario, to extrapolate to this situation may not be justified or appropriate § § PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
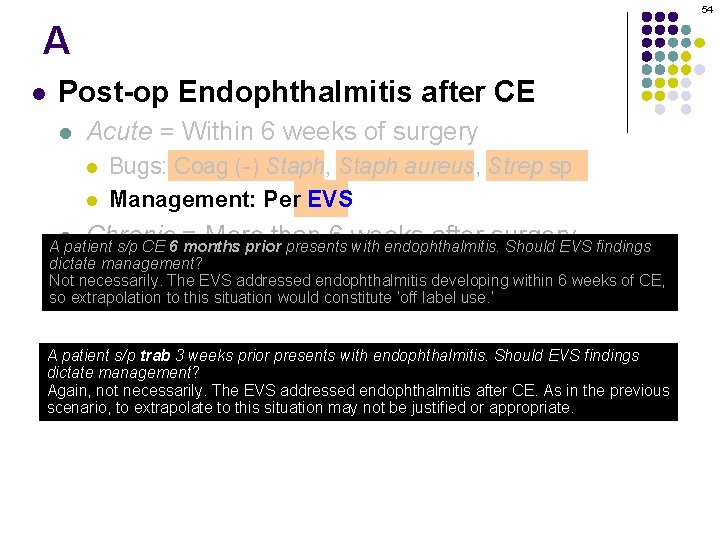
54 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery Alpatient s/p CE 6 months prior presents with endophthalmitis. Should EVS findings dictate management? l Presents w/ indolent course or progressive inflammation Not necessarily. The EVS addressed endophthalmitis developing within 6 weeks of CE, so extrapolation thisacnes, situation coag would constitute ‘off label use. ’ l Bugs: to. P. (-) Staph , fungus § Peripheral white plaque in bag = P. acnes A patient s/p trab 3 weeks prior presents with endophthalmitis. Should EVS findings Management: dictatelmanagement? Again, not The EVS addressed after CE. unless As in theit previous § necessarily. Intravitreal antibiotics are endophthalmitis usually not helpful, follows scenario, to extrapolate to this situation may not be justified or appropriate. § § PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

55 l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation (No question—proceed when ready)
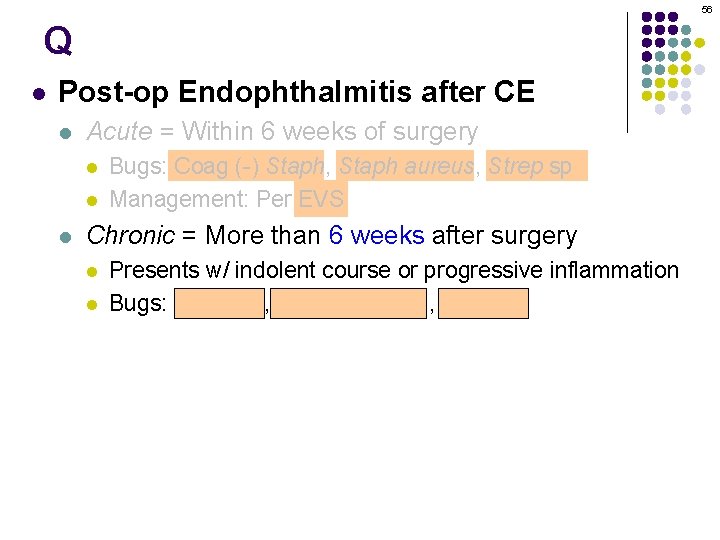
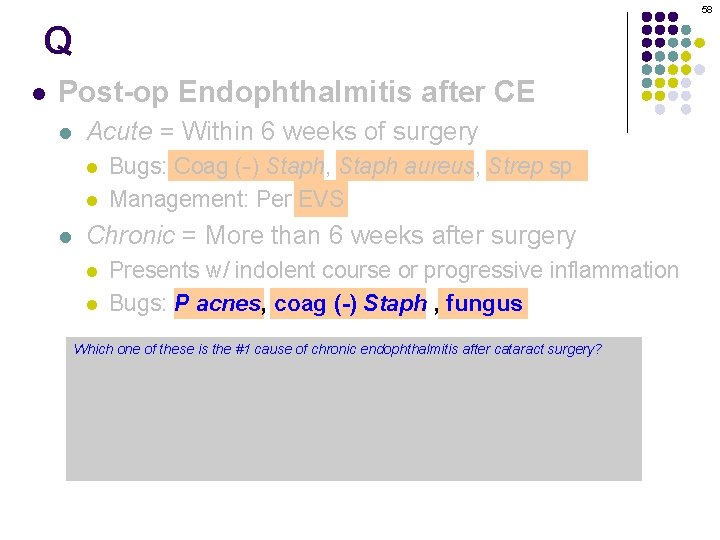
56 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P. acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

57 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P. acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
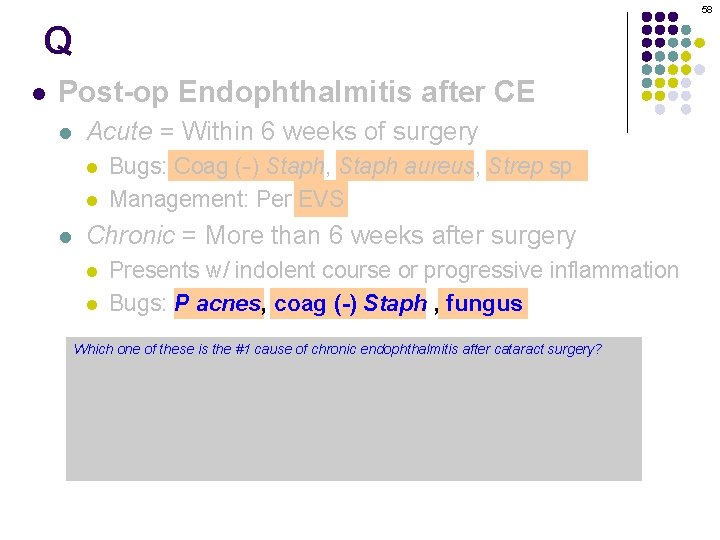
58 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Which one of these is the #1 cause of chronic endophthalmitis after cataract surgery? Pl acnes Management: § Intravitreal antibiotics are usually helpful, Microbiologically speaking, how is the bacterium P acnes not classified? It is an anaerobic, Gram(+), pleomorphic rod PPV and subtotal capsulectomy Is it part the normal ocular/periocular § of. Use vancomycin 1 mg, microbial eitherflora? in the Yes § unless it follows vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
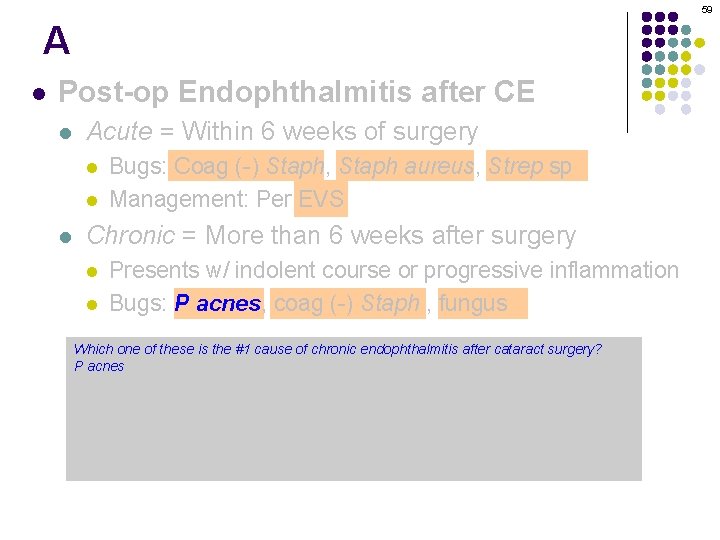
59 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Which one of these is the #1 cause of chronic endophthalmitis after cataract surgery? Pl acnes Management: § Intravitreal antibiotics are usually helpful, Microbiologically speaking, how is the bacterium P acnes not classified? It is an anaerobic, Gram(+), pleomorphic rod PPV and subtotal capsulectomy Is it part the normal ocular/periocular § of. Use vancomycin 1 mg, microbial eitherflora? in the Yes § unless it follows vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
60 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Which one of these is the #1 cause of chronic endophthalmitis after cataract surgery? Pl acnes Management: § Intravitreal antibiotics are usually helpful, Microbiologically speaking, how is the bacterium P acnes not classified? It is an anaerobic, Gram(+), pleomorphic rod PPV and subtotal capsulectomy Is it part the normal ocular/periocular § of. Use vancomycin 1 mg, microbial eitherflora? in the Yes § unless it follows vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
61 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Which one of these is the #1 cause of chronic endophthalmitis after cataract surgery? Pl acnes Management: § Intravitreal antibiotics are usually helpful, Microbiologically speaking, how is the bacterium P acnes not classified? It is an anaerobic, Gram(+), pleomorphic rod PPV and subtotal capsulectomy Is it part the normal ocular/periocular § of. Use vancomycin 1 mg, microbial eitherflora? in the Yes § unless it follows vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

62 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Which one of these is the #1 cause of chronic endophthalmitis after cataract surgery? Pl acnes Management: § Intravitreal antibiotics are usually helpful, Microbiologically speaking, how is the bacterium P acnes not classified? It is an anaerobic, Gram(+), pleomorphic rod PPV and subtotal capsulectomy Is it part the normal ocular/periocular § of. Use vancomycin 1 mg, microbial eitherflora? in the Yes § unless it follows vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
63 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Which one of these is the #1 cause of chronic endophthalmitis after cataract surgery? Pl acnes Management: § Intravitreal antibiotics are usually helpful, Microbiologically speaking, how is the bacterium P acnes not classified? It is an anaerobic, Gram(+), pleomorphic rod PPV and subtotal capsulectomy Is it part the normal ocular/periocular § of. Use vancomycin 1 mg, microbial eitherflora? in the Yes § unless it follows vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
64 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes By definition, chronic endophthalmitis commences 6+ weeks after surgery. In terms of P acnes… l What is the average amount of time between surgery and presentation? 3 -4 months What is the 2 weeks toantibiotics several yearsare usually not helpful, unless § range? Intravitreal Management: § § it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
65 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes By definition, chronic endophthalmitis commences 6+ weeks after surgery. In terms of P acnes… l What is the average amount of time between surgery and presentation? 3 -4 months What is the 2 weeks toantibiotics several yearsare usually not helpful, unless § range? Intravitreal Management: § § it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
66 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes By definition, chronic endophthalmitis commences 6+ weeks after surgery. In terms of P acnes… l What is the average amount of time between surgery and presentation? 3 -4 months What is the 2 weeks toantibiotics several yearsare usually not helpful, unless § range? Intravitreal Management: § § it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
67 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes By definition, chronic endophthalmitis commences 6+ weeks after surgery. In terms of P acnes… l What is the average amount of time between surgery and presentation? 3 -4 months What is the Two weeks to several years § range? Intravitreal antibiotics are usually not helpful, unless Management: § § it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
68 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Is the inflammation in P acnes chronic post-op endophthalmitis granulomatous, or nongranulomatous? Granulomatous l Management: What is the response to a trial of steroids? § classic Intravitreal antibiotics are usually not helpful, unless it The inflammation will lessen, then recur (or even worsen) when the steroids are stopped § § follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

69 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Is the inflammation in P acnes chronic post-op endophthalmitis granulomatous, or nongranulomatous? Granulomatous l Management: What is the response to a trial of steroids? § classic Intravitreal antibiotics are usually not helpful, unless it The inflammation will lessen, then recur (or even worsen) when the steroids are stopped § § follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
70 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Is the inflammation in P acnes chronic post-op endophthalmitis granulomatous, or nongranulomatous? Granulomatous l Management: What is the response to a trial of steroids? § classic Intravitreal antibiotics are usually not helpful, unless it The inflammation will lessen, then recur (or even worsen) when the steroids are stopped § § follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
71 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P. acnes Is the inflammation in P acnes chronic post-op endophthalmitis granulomatous, or nongranulomatous? Granulomatous l Management: What is the response to a trial of steroids? § classic Intravitreal antibiotics are usually not helpful, unless it The inflammation will lessen, then recur (or even worsen) when the steroids are stopped § § follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange

72 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P. acnes one of the above bugs Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
73 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management: § § § Intravitreal antibiotics are usually not helpful, unless it follows PPV and subtotal capsulectomy Use vancomycin 1 mg, either in the vitreous or in the bag If recurs: Total capsulectomy with IOL removal or exchange
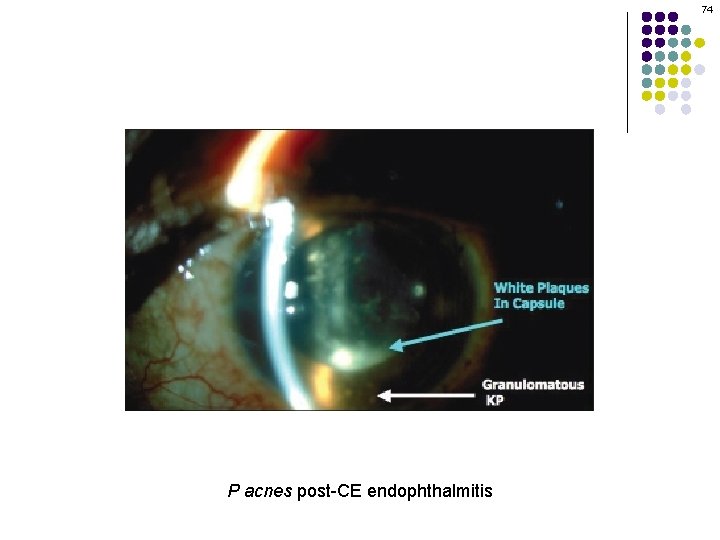
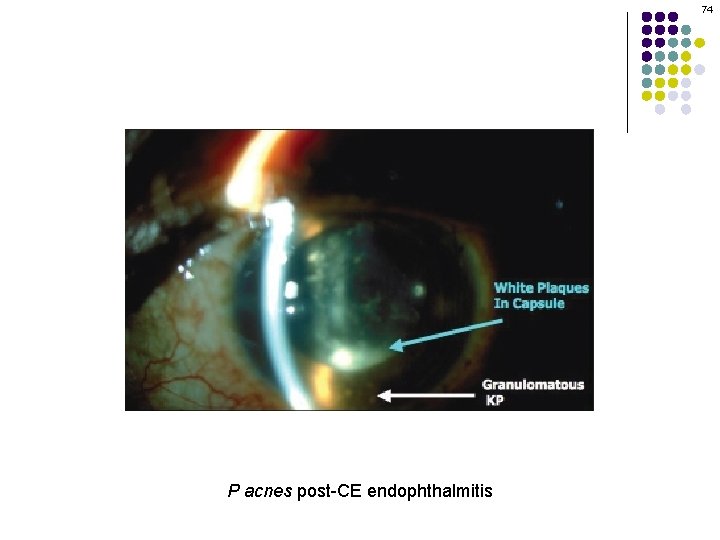
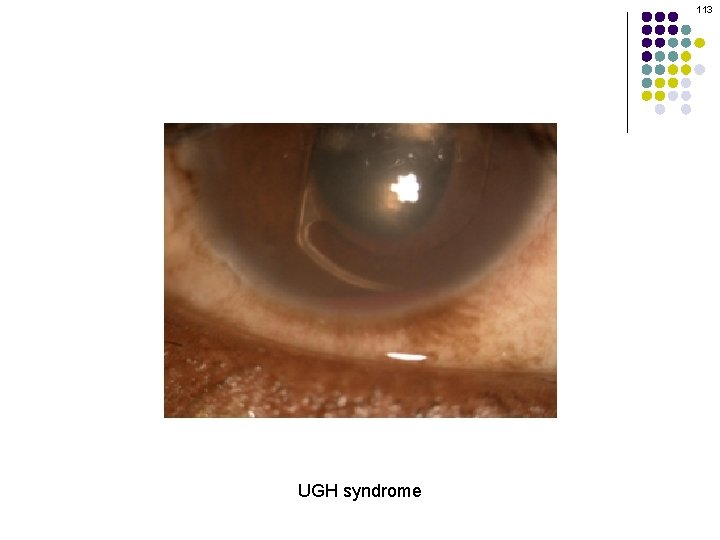
74 P acnes post-CE endophthalmitis
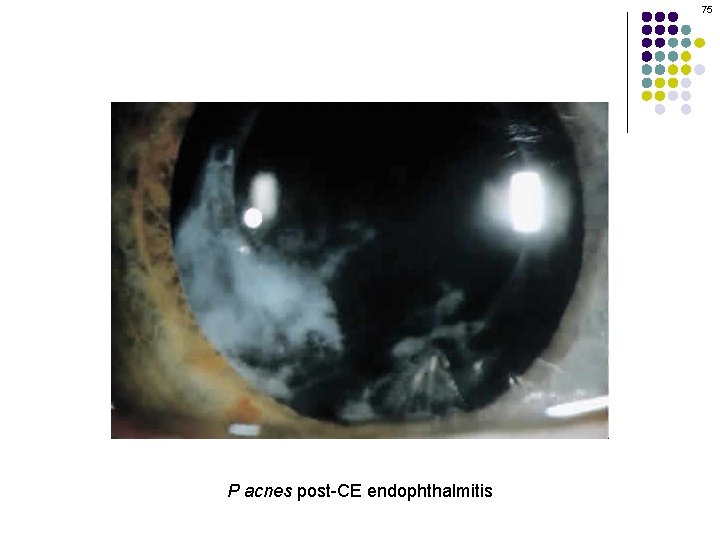
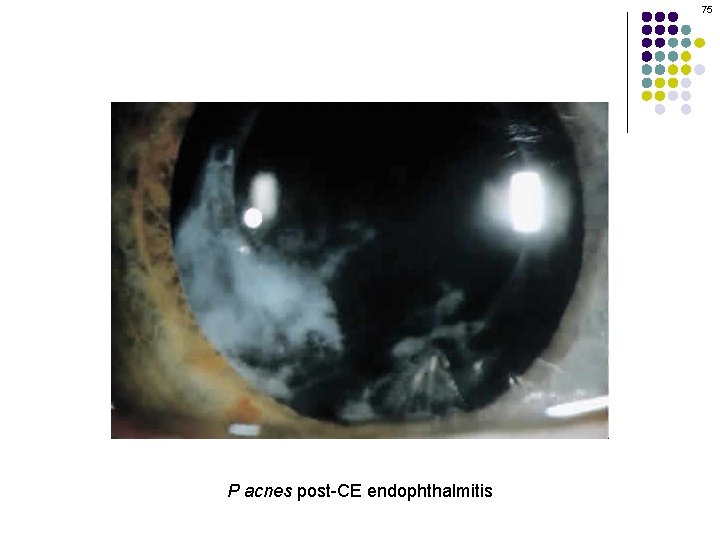
75 P acnes post-CE endophthalmitis
76 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management: How does the fact that P acnes is an anaerobe play a role in its virulence as a cause Intravitreal antibiotics are usually not helpful, unless it follows of §chronic post-op endophthalmitis? The space the IOL andcapsulectomy the bag is relatively anaerobic, thus allowing P acnes PPVbetween and subtotal to flourish, eventually forming a colony large enough to be seen at the slit lamp (ie, the notorious ‘white plaque’) § Use vancomycin 1 mg, either in the vitreous or in the bag § If recurs: Total capsulectomy with IOL removal or exchange
77 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management: How does the fact that P acnes is an anaerobe play a role in its virulence as a cause Intravitreal antibiotics are usually not helpful, unless it follows of §chronic post-op endophthalmitis? The space the IOL andcapsulectomy the bag is relatively anaerobic, thus allowing P acnes PPVbetween and subtotal to flourish, eventually forming a colony large enough to be seen at the slit lamp (ie, the notorious ‘white plaque’) § Use vancomycin 1 mg, either in the vitreous or in the bag § If recurs: Total capsulectomy with IOL removal or exchange
78 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management: How does the fact that P acnes is an anaerobe play a role in its virulence as a cause Intravitreal antibiotics are usually not helpful, unless it follows of §chronic post-op endophthalmitis? The space the IOL andcapsulectomy the bag is relatively anaerobic, thus allowing P acnes PPVbetween and subtotal to flourish, eventually forming a colony large enough to be seen at the slit lamp (ie, the notorious ‘white plaque’) § Use vancomycin 1 mg, either in the vitreous or in the bag § If recurs: Total withand IOL removal or exchange Suppose you (mis)took a P capsulectomy acnes plaque for a PCO, YAG’d it. What would likely result? Seeding of the vitreous with the organism, which would cause the vitritis to worsen
79 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management: How does the fact that P acnes is an anaerobe play a role in its virulence as a cause Intravitreal antibiotics are usually not helpful, unless it follows of §chronic post-op endophthalmitis? The space the IOL andcapsulectomy the bag is relatively anaerobic, thus allowing P acnes PPVbetween and subtotal to flourish, eventually forming a colony large enough to be seen at the slit lamp (ie, the notorious ‘white plaque’) § Use vancomycin 1 mg, either in the vitreous or in the bag § If recurs: Total withand IOL removal or exchange Suppose you (mis)took a P capsulectomy acnes plaque for a PCO, YAG’d it. What would likely result? Seeding of the vitreous with the organism, which would cause the vitritis to worsen

80 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows abb. and capsulectomy--in something-ectomy abx PPV which case, use vancomycin If recurs: IOL removal or exchange
81 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
82 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin surgery If recurs: IOL removal or exchange
83 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
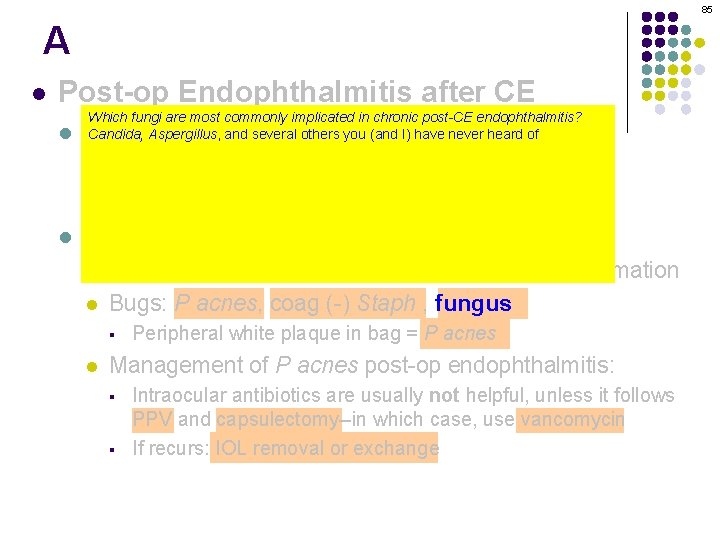
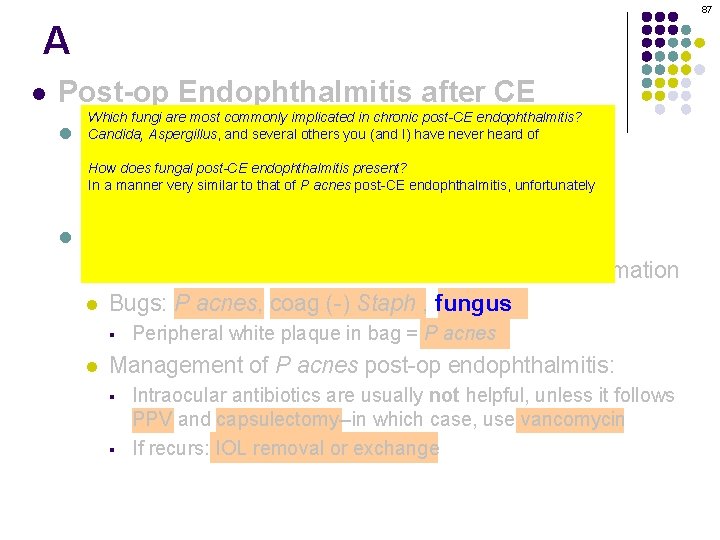
84 Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
85 A l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange

86 Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
87 A l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
88 Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange

89 A/Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange

90 A l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
91 Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
92 A/Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string pearls’ configuration threeof words l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
93 A l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § l Peripheral white plaque in bag = P acnes Management of P acnes post-op endophthalmitis: § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
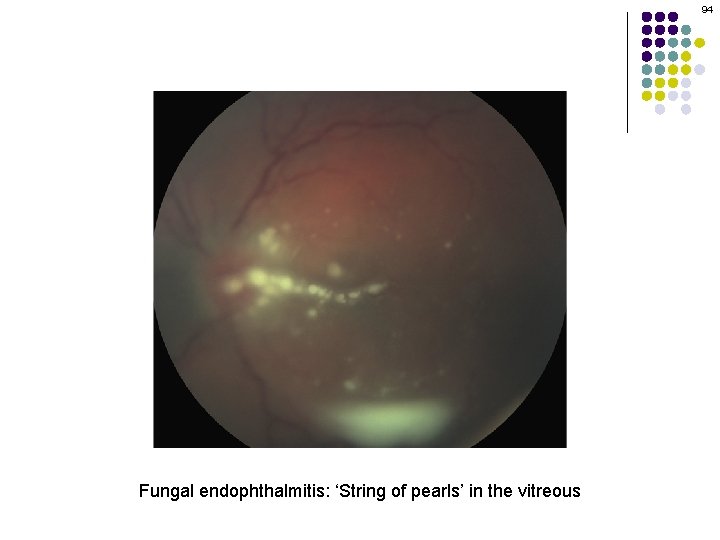
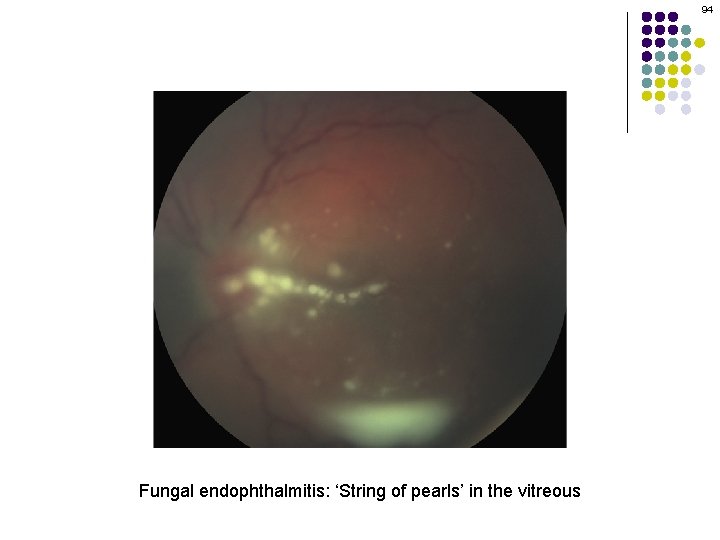
94 Fungal endophthalmitis: ‘String of pearls’ in the vitreous

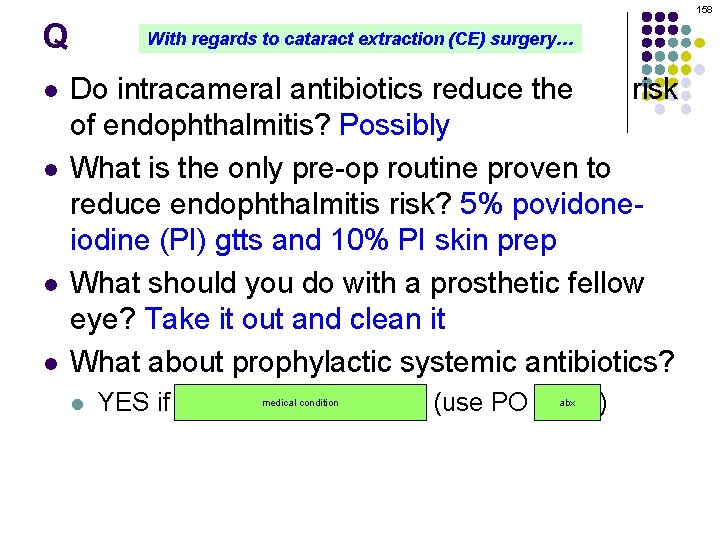
95 Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes How is chronic fungal post-CE endophthalmitis treated? With intravitreal antifungals (usually amphotericin and/or voriconazole). Vitrectomy l may be necessary as well. Management of P acnes post-op endophthalmitis: Intraocular antibiotics are usually not helpful, unless it follows What about systemic antifungals? PPV and capsulectomy--in which case, use vancomycin At this time, it is not clear what role (if any) systemic antifungals can/should play in managing post-op fungal § If recurs: IOLendophthalmitis removal or exchange §
96 A l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes How is chronic fungal post-CE endophthalmitis treated? With intravitreal antifungals (usually amphotericin and/or voriconazole). Vitrectomy l may be necessary as well. Management of P acnes post-op endophthalmitis: Intraocular antibiotics are usually not helpful, unless it follows What about systemic antifungals? PPV and capsulectomy--in which case, use vancomycin At this time, it is not clear what role (if any) systemic antifungals can/should play in managing post-op fungal § If recurs: IOLendophthalmitis removal or exchange §
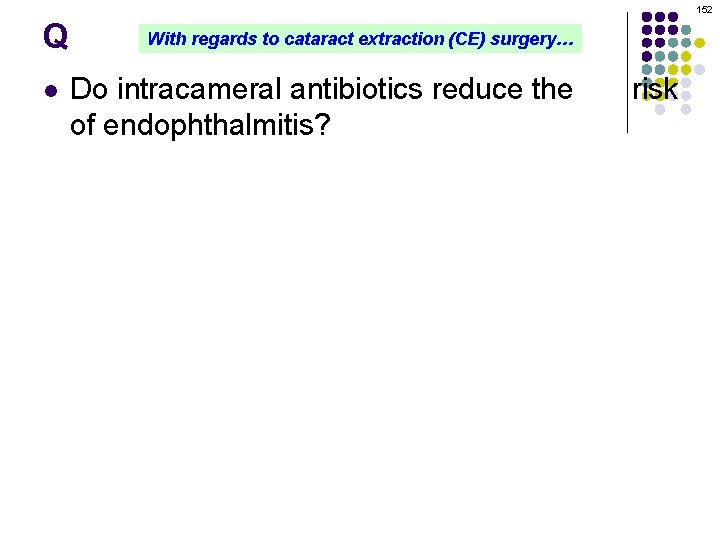
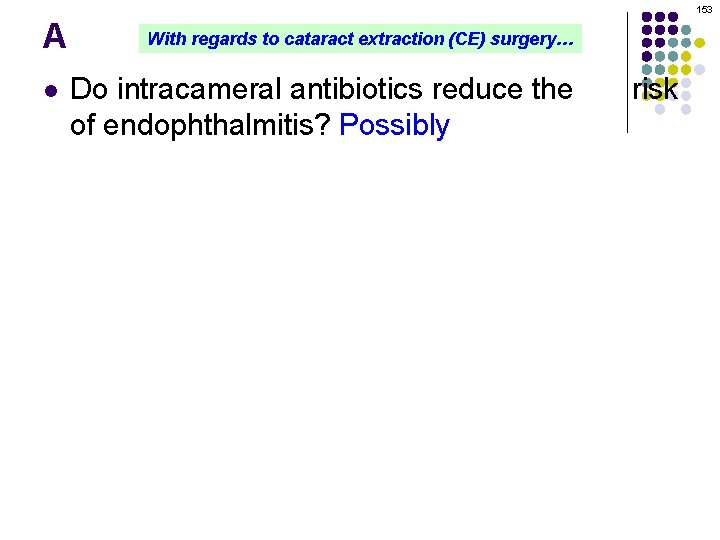
97 Q l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes How is chronic fungal post-CE endophthalmitis treated? With intravitreal antifungals (usually amphotericin and/or voriconazole). Vitrectomy l may be necessary as well. Management of P acnes post-op endophthalmitis: Intraocular antibiotics are usually not helpful, unless it follows What about systemic antifungals? PPV and capsulectomy--in which case, use vancomycin At this time, it is not clear what role (if any) systemic antifungals can/should play in managing post-op fungal § If recurs: IOLendophthalmitis removal or exchange §
98 A l Post-op Endophthalmitis after CE l Which fungi are most commonly implicated in chronic post-CE endophthalmitis? Candida, Aspergillus, and several others you (and I) have never heard of Acute = Within 6 weeks of surgery How does fungal post-CE present? aureus, l Bugs: Coag (-)endophthalmitis Staph, Staph Strep sp In a manner very similar to that of P acnes post-CE endophthalmitis, unfortunately l l Management: Per EVS Are there any clinical findings that are more suggestive of a fungal etiology? Yes. One is found in the anterior segment; the other in the vitreous cavity: --Anterior segment: The presence of corneal infiltrates, iris mass, and/or scleritis --Vitreous: The presence of snowballs, especially in a ‘string of pearls’ configuration l Chronic = More than 6 weeks after surgery l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes How is chronic fungal post-CE endophthalmitis treated? With intravitreal antifungals (usually amphotericin and/or voriconazole). Vitrectomy l may be necessary as well. Management of P acnes post-op endophthalmitis: Intraocular antibiotics are usually not helpful, unless it follows What about systemic antifungals? PPV and capsulectomy--in which case, use vancomycin At this time, it is not clear what role (if any) systemic antifungals can/should play in managing post-op fungal § If recurs: IOLendophthalmitis removal or exchange §
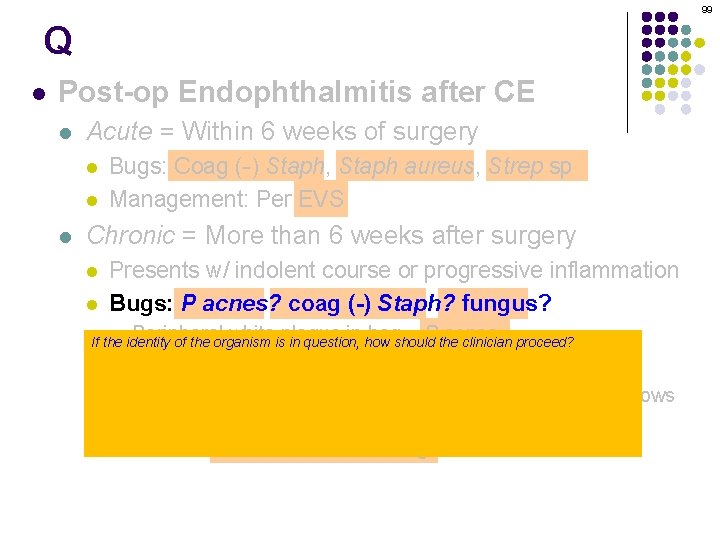
99 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? § Intraocular antibiotics are usually not helpful, unless it follows Stains, definitely. Remember, these pathogens are slow-growing and fastidious; thus, it PPV and capsulectomy--in case, vancomycin could be weeks before they reveal themselveswhich via culturing. Onuse the other hand, staining has the potential to identify the culprit instantly. § If recurs: IOL removal or exchange

100 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? § Intraocular antibiotics are usually not helpful, unless it follows Stains, definitely. Remember, these pathogens are slow-growing and fastidious; thus, it PPV and capsulectomy--in case, vancomycin could be weeks before they reveal themselveswhich via culturing. Onuse the other hand, staining has the potential to identify the culprit instantly. § If recurs: IOL removal or exchange
101 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? threenot culturehelpful, media should be employed? § Intraocular antibiotics are Which usually unless it follows Stains, definitely. Remember, these pathogens are slow-growing and fastidious; thus, it --Aerobic PPV and capsulectomy--in which case, use vancomycin could be weeks before they reveal themselves via culturing. On the other hand, staining --Anaerobic has the potential to identify the culprit instantly. --Fungal § If recurs: IOL removal or exchange

102 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? threenot culturehelpful, media should be employed? § Intraocular antibiotics are Which usually unless it follows Stains, definitely. Remember, these pathogens are slow-growing and fastidious; thus, it --Aerobic PPV and capsulectomy--in which case, use vancomycin could be weeks before they reveal themselves via culturing. On the other hand, staining --Anaerobic has the potential to identify the culprit instantly. --Fungal § If recurs: IOL removal or exchange
103 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? § Intraocular antibiotics are usually not helpful, unless it follows Stains, definitely. Remember, these pathogens are slow-growing fastidious; thus, it Which twoand stains should be used? PPV and capsulectomy--in which case, use vancomycin could be weeks before they reveal themselves via culturing. On the other hand, staining --Gram has the potential to identify the culprit instantly. --Giemsa § If recurs: IOL removal or exchange
104 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? § Intraocular antibiotics are usually not helpful, unless it follows Stains, definitely. Remember, these pathogens are slow-growing fastidious; thus, it Which twoand stains should be used? PPV and capsulectomy--in which case, use vancomycin could be weeks before they reveal themselves via culturing. On the other hand, staining --Gram has the potential to identify the culprit instantly. --Giemsa § If recurs: IOL removal or exchange
105 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? § Intraocular antibiotics are usually not helpful, unless it follows Stains, definitely. Remember, these pathogens are slow-growing and fastidious; thus, it PPV and capsulectomy--in case, vancomycin could be weeks before they reveal themselveswhich via culturing. Onuse the other hand, staining has the potential to identify the culprit instantly. § If recurs: IOL removal or exchange
106 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes? coag (-) Staph? fungus? § identity Peripheral whiteisplaque in how bagshould = P the acnes If the organism in question, clinician proceed? By obtaining aqueous (and vitreous, if PPV is performed) samples for culture and stains l Management of P acnes post-op endophthalmitis: Which is of greater utility--cultures, or stains? § Intraocular antibiotics are usually not helpful, unless it follows Stains, definitely. Remember, these pathogens are slow-growing and fastidious; thus, it PPV and capsulectomy--in case, vancomycin could be weeks before they reveal themselveswhich via culturing. Onuse the other hand, staining has the potential to identify the culprit instantly. § If recurs: IOL removal or exchange

107 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes It is important to bear in mind that certain noninfectious conditions can present in a manner very much like chronic l post-op infectious endophthalmitis. What are some of these conditions? --Retained lens fragments --IOL-related§issues (eg, a square-edged haptic are malpositioned the ciliary sulcus; unless UGH syndrome) Intraocular antibiotics usuallyinnot helpful, it follows --Intraocular lymphoma (ie, masquerade syndrome) Management of P acnes post-op endophthalmitis: § PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
108 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes It is important to bear in mind that certain noninfectious conditions can present in a manner very much like chronic l post-op infectious endophthalmitis. What are some of these conditions? --Retained lens fragments --IOL-related§issues (eg, a square-edged haptic are malpositioned the ciliary sulcus; unless UGH syndrome) Intraocular antibiotics usuallyinnot helpful, it follows --Intraocular lymphoma (ie, masquerade syndrome) Management of P acnes post-op endophthalmitis: § PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
109 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes It is important to bear in mind that certain noninfectious conditions can present in a manner very much like chronic l post-op infectious endophthalmitis. What are some of these conditions? --Retained lens fragments --IOL-related§issues (eg, a square-edged haptic are malpositioned the ciliary sulcus; unless UGH syndrome) Intraocular antibiotics usuallyinnot helpful, it follows --Intraocular lymphoma (ie, masquerade syndrome) Management of P acnes post-op endophthalmitis: PPV and capsulectomy--in which case, use vancomycin What does the UGH in UGH syndrome stand for? § If recurs: IOL removal or exchange Uveitis-glaucoma-hyphema (syndrome) What is UGH syndrome? A constellation of sequelae that can occur when an inappropriately-sized AC IOL chafes the iris and other anterior-segment structures. Advances in IOL manufacturing have made it an uncommon occurrence.
110 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes It is important to bear in mind that certain noninfectious conditions can present in a manner very much like chronic l post-op infectious endophthalmitis. What are some of these conditions? --Retained lens fragments --IOL-related§issues (eg, a square-edged haptic are malpositioned the ciliary sulcus; unless UGH syndrome) Intraocular antibiotics usuallyinnot helpful, it follows --Intraocular lymphoma (ie, masquerade syndrome) Management of P acnes post-op endophthalmitis: PPV and capsulectomy--in which case, use vancomycin What does the UGH in UGH syndrome stand for? § If recurs: IOL removal or exchange Uveitis-glaucoma-hyphema (syndrome) What is UGH syndrome? A constellation of sequelae that can occur when an inappropriately-sized AC IOL chafes the iris and other anterior-segment structures. Advances in IOL manufacturing have made it an uncommon occurrence.

111 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes It is important to bear in mind that certain noninfectious conditions can present in a manner very much like chronic l post-op infectious endophthalmitis. What are some of these conditions? --Retained lens fragments --IOL-related§issues (eg, a square-edged haptic are malpositioned the ciliary sulcus; unless UGH syndrome) Intraocular antibiotics usuallyinnot helpful, it follows --Intraocular lymphoma (ie, masquerade syndrome) Management of P acnes post-op endophthalmitis: PPV and capsulectomy--in which case, use vancomycin What does the UGH in UGH syndrome stand for? § If recurs: IOL removal or exchange Uveitis-glaucoma-hyphema (syndrome) What is UGH syndrome? A constellation of sequelae that can occur when an inappropriately-sized AC IOL chafes the iris and other anterior-segment structures. Advances in IOL manufacturing have made it an uncommon occurrence.
112 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = More than 6 weeks after surgery l l Presents w/ indolent course or progressive inflammation Bugs: P acnes, coag (-) Staph , fungus § Peripheral white plaque in bag = P acnes It is important to bear in mind that certain noninfectious conditions can present in a manner very much like chronic l post-op infectious endophthalmitis. What are some of these conditions? --Retained lens fragments --IOL-related§issues (eg, a square-edged haptic are malpositioned the ciliary sulcus; unless UGH syndrome) Intraocular antibiotics usuallyinnot helpful, it follows --Intraocular lymphoma (ie, masquerade syndrome) Management of P acnes post-op endophthalmitis: PPV and capsulectomy--in which case, use vancomycin What does the UGH in UGH syndrome stand for? § If recurs: IOL removal or exchange Uveitis-glaucoma-hyphema (syndrome) What is UGH syndrome? A constellation of sequelae that can occur when an inappropriately-sized AC IOL chafes the iris and other anterior-segment structures. Advances in IOL manufacturing have made it an uncommon occurrence.
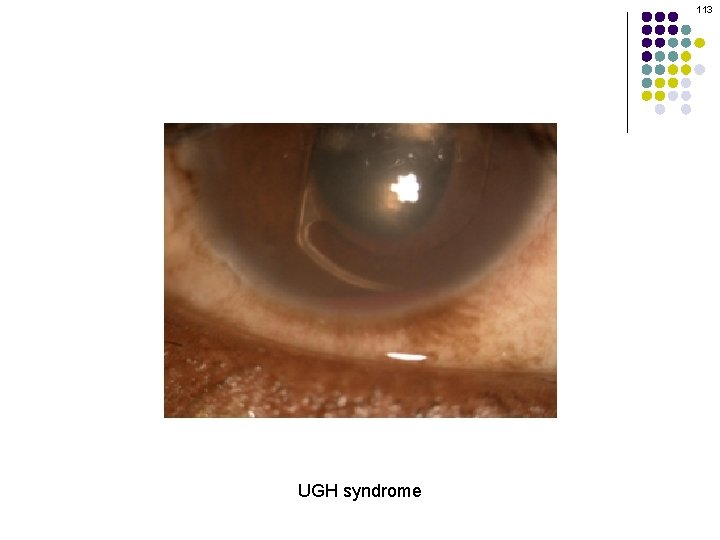
113 UGH syndrome
114 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = main More surgery What are the riskthan factors 6 forweeks post-CE after endophthalmitis? -Presents w/ indolent course or progressive -l-- Bugs: P. acnes, coag (-) Staph , fungus -- § Peripheral white plaque in bag = P. acnes -l-- Management: l § § inflammation Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
115 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = main More surgery What are the riskthan factors 6 forweeks post-CE after endophthalmitis? --Capsular rupture Presents w/ indolent course or progressive --Prolonged surgery time lens fragments l--Retained Bugs: P. acnes, coag (-) Staph , fungus --Clear cornea incision § Peripheral white plaque in bag = P. acnes --Sutureless closure l--Wound Management: leak on post-op day 1 l § § inflammation Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange

116 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = main More surgery What are the riskthan factors 6 forweeks post-CE after endophthalmitis? --Capsular rupture? Presents w/ indolent course or progressive inflammation Which factor presents the largest increase --Prolonged surgery time? in relative risk of post-op endophthalmitis? lens fragments? l--Retained Bugs: P. acnes, coag (-) Staph , fungus Wound leak on POD 1 --one study pegged --Clear cornea incision? increased § Peripheral white plaque in bag its = P. acnesrelative risk at 44! --Sutureless closure? l--Wound Management: leak on post-op day 1? l § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
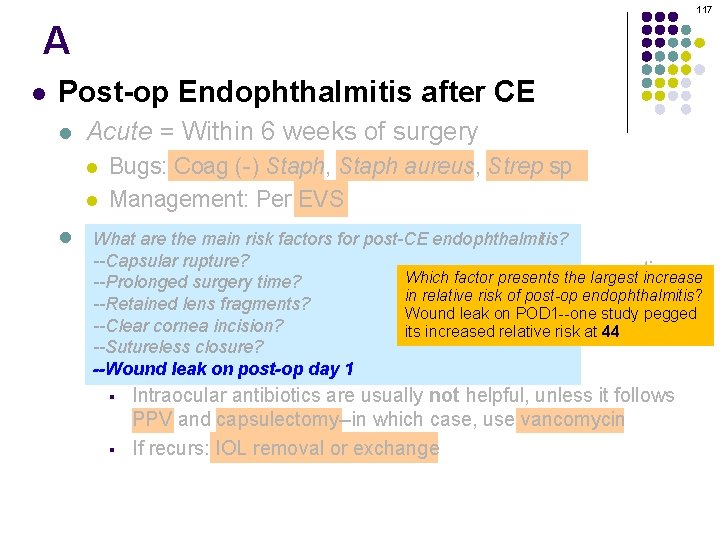
117 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS Chronic = main More surgery What are the riskthan factors 6 forweeks post-CE after endophthalmitis? --Capsular rupture? Presents w/ indolent course or progressive inflammation Which factor presents the largest increase --Prolonged surgery time? in relative risk of post-op endophthalmitis? lens fragments? l--Retained Bugs: P. acnes, coag (-) Staph , fungus Wound leak on POD 1 --one study pegged --Clear cornea incision? increased § Peripheral white plaque in bag its = P. acnesrelative risk at 44 --Sutureless closure? l--Wound Management: leak on post-op day 1 l § § Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
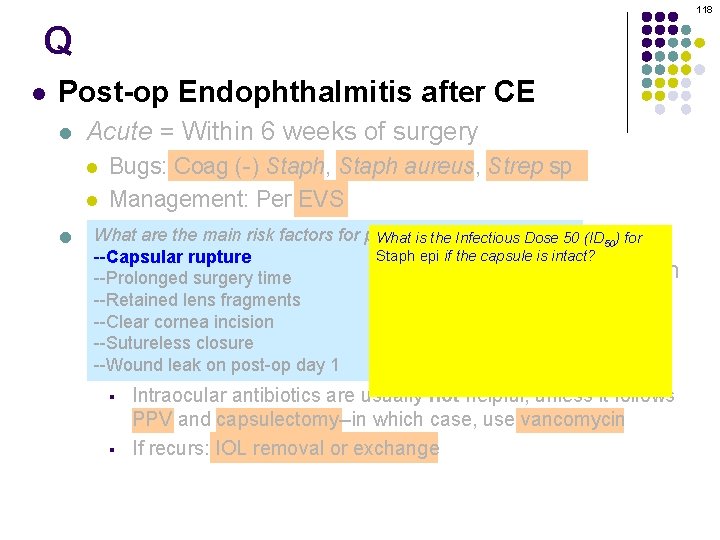
118 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS What are the riskthan factors 6 forweeks post-CE endophthalmitis? What is the Infectious Dose 50 (ID Chronic = main More after surgery 50) for Staph epi if the capsule is intact? --Capsular rupture l--Prolonged Presentssurgery w/ indolent course or one progressive inflammation About million organisms time lens fragments l--Retained Bugs: P. acnes, coag (-) Staph fungus What is , the ID 50 if the capsule is ruptured --Clear cornea incision (ie, if=the Staph epi gets into the vitreous)? § Peripheral white plaque in bag P. acnes --Sutureless closure 10. That’s not a typo--only ten Staph epis need get in the vitreous to produce post-op leak on post-op day 1 l--Wound Management: § § endophthalmitis! Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
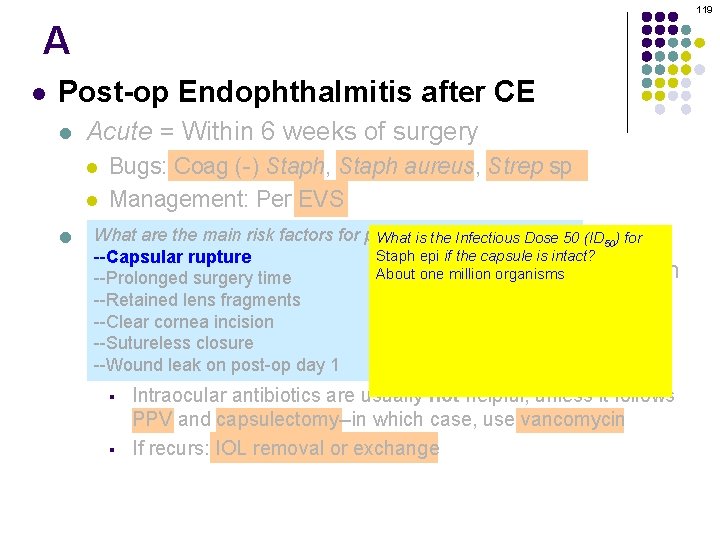
119 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS What are the riskthan factors 6 forweeks post-CE endophthalmitis? What is the Infectious Dose 50 (ID Chronic = main More after surgery 50) for Staph epi if the capsule is intact? --Capsular rupture l--Prolonged Presentssurgery w/ indolent course or one progressive inflammation About million organisms time lens fragments l--Retained Bugs: P. acnes, coag (-) Staph fungus What is , the ID 50 if the capsule is ruptured --Clear cornea incision (ie, if=the Staph epi gets into the vitreous)? § Peripheral white plaque in bag P. acnes --Sutureless closure 10. That’s not a typo--only ten Staph epis need get in the vitreous to produce post-op leak on post-op day 1 l--Wound Management: § § endophthalmitis! Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
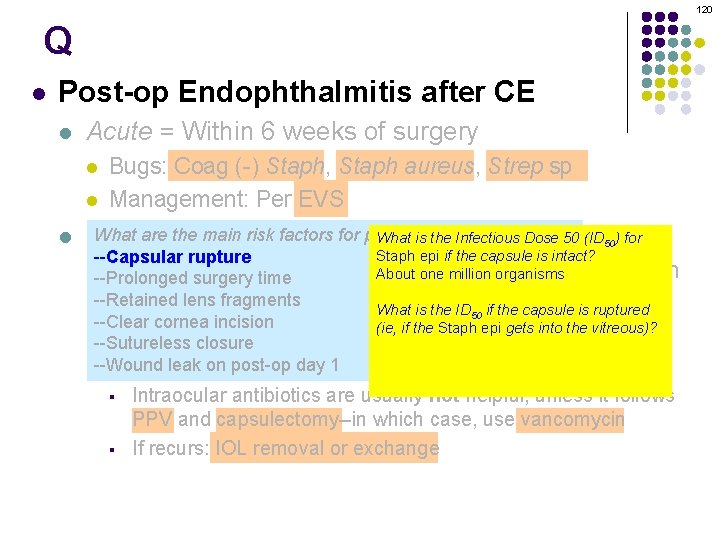
120 Q l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS What are the riskthan factors 6 forweeks post-CE endophthalmitis? What is the Infectious Dose 50 (ID Chronic = main More after surgery 50) for Staph epi if the capsule is intact? --Capsular rupture l--Prolonged Presentssurgery w/ indolent course or one progressive inflammation About million organisms time lens fragments l--Retained Bugs: P. acnes, coag (-) Staph fungus What is , the ID 50 if the capsule is ruptured --Clear cornea incision (ie, if=the Staph epi gets into the vitreous)? § Peripheral white plaque in bag P. acnes --Sutureless closure 10. That’s not a typo--only ten Staph epis need get in the vitreous to produce post-op leak on post-op day 1 l--Wound Management: § § endophthalmitis! Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
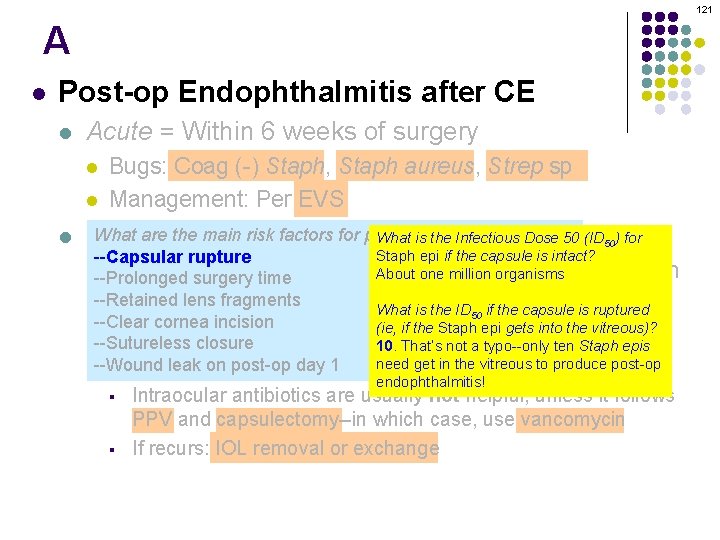
121 A l Post-op Endophthalmitis after CE l Acute = Within 6 weeks of surgery l l l Bugs: Coag (-) Staph, Staph aureus, Strep sp Management: Per EVS What are the riskthan factors 6 forweeks post-CE endophthalmitis? What is the Infectious Dose 50 (ID Chronic = main More after surgery 50) for Staph epi if the capsule is intact? --Capsular rupture l--Prolonged Presentssurgery w/ indolent course or one progressive inflammation About million organisms time lens fragments l--Retained Bugs: P. acnes, coag (-) Staph fungus What is , the ID 50 if the capsule is ruptured --Clear cornea incision (ie, if=the Staph epi gets into the vitreous)? § Peripheral white plaque in bag P. acnes --Sutureless closure 10. That’s not a typo--only ten Staph epis need get in the vitreous to produce post-op leak on post-op day 1 l--Wound Management: § § endophthalmitis! Intraocular antibiotics are usually not helpful, unless it follows PPV and capsulectomy--in which case, use vancomycin If recurs: IOL removal or exchange
122 l Noninfectious endophthalmitis after CE l l l Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent

123 Q l Noninfectious endophthalmitis after CE l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : four words l l l l abb. Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
124 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
125 Q l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : # - #, and unit of time l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent

126 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
127 Q l Noninfectious endophthalmitis after CE l l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : sign (two words) l l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
128 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
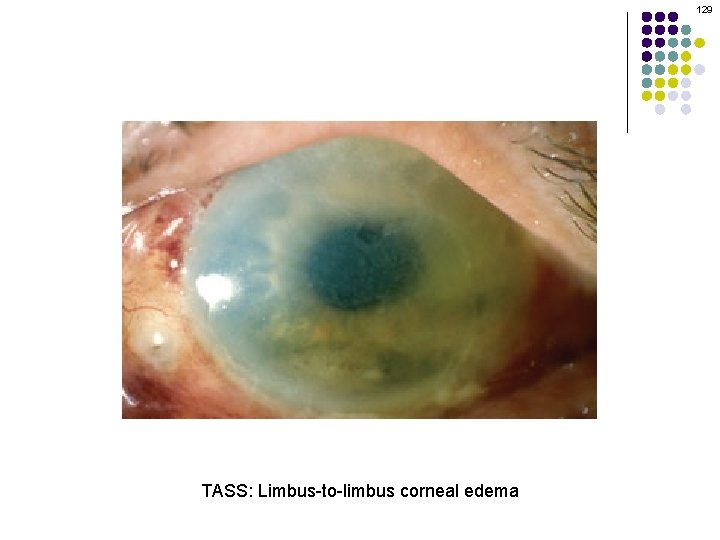
129 TASS: Limbus-to-limbus corneal edema
130 Q l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
131 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
132 Q l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent

133 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent

134 Q l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
135 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
136 Q l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
137 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious endophthalmitis: Markedly worse corneal edema Pathogenesis: Immune reaction to compromised surgical materials; e. g. : l l Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
138 Q l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious How is the diagnosis of TASS made? endophthalmitis: Markedly worse corneal edema It is a diagnosis of exclusion—endophthalmitis in the absence Of positive cultures and stains Pathogenesis: Immune reaction to compromised How is it materials; treated? surgical e. g. : l l Steroids Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent

139 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious How is the diagnosis of TASS made? endophthalmitis: Markedly worse corneal edema It is a diagnosis of exclusion—endophthalmitis in the absence of positive cultures and stains Pathogenesis: Immune reaction to compromised How is it materials; treated? surgical e. g. : l l Steroids Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
140 Q l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious How is the diagnosis of TASS made? endophthalmitis: Markedly worse corneal edema It is a diagnosis of exclusion—endophthalmitis in the absence of positive cultures and stains Pathogenesis: Immune reaction to compromised How is it materials; treated? surgical e. g. : l l Steroids Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
141 A l Noninfectious endophthalmitis after CE l l Noninfectious endophthalmitis is also known as toxic anterior segment syndrome (TASS) Time to presentation: 12 -24 hours after surgery Key difference in presentation from infectious How is the diagnosis of TASS made? endophthalmitis: Markedly worse corneal edema It is a diagnosis of exclusion—endophthalmitis in the absence of positive cultures and stains Pathogenesis: Immune reaction to compromised How is it materials; treated? surgical e. g. : l l Steroids Denatured viscoelastic Preservatives in intracameral solutions IOL issues: sterilization technique; coatings Contamination of equipment with bacterial endotoxins or residual detergent
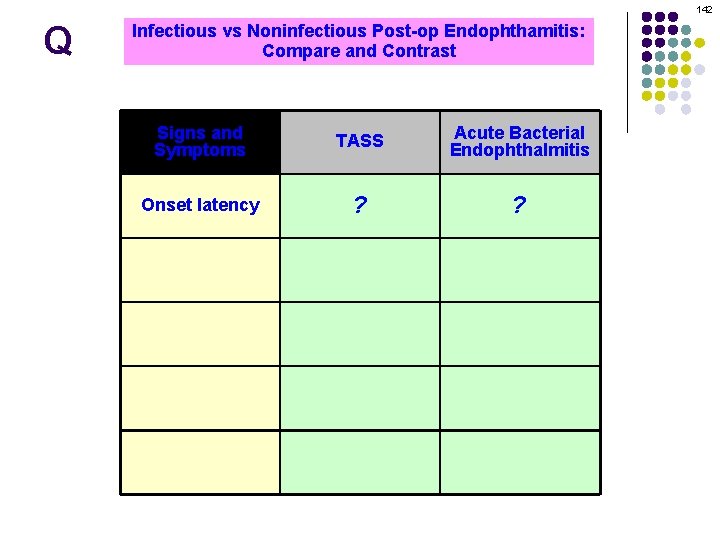
142 Q Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 TASS ? hours Infectious 2 -7? days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present

143 A Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present
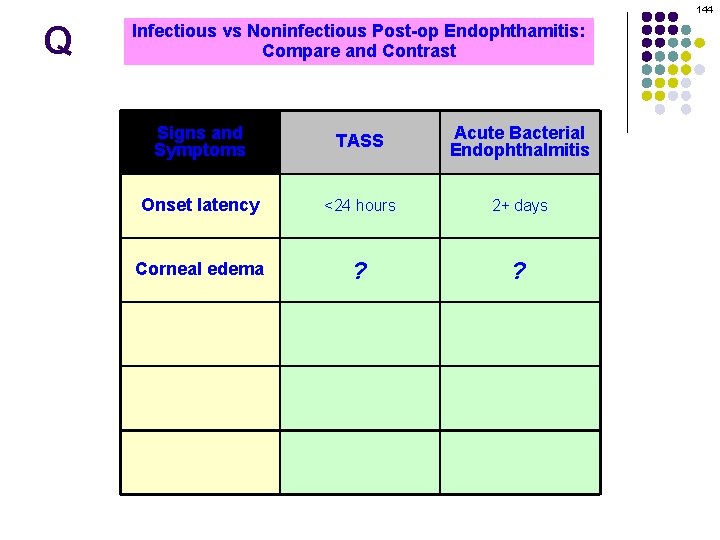
144 Q Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 Profound ? hours 2+ ? days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present
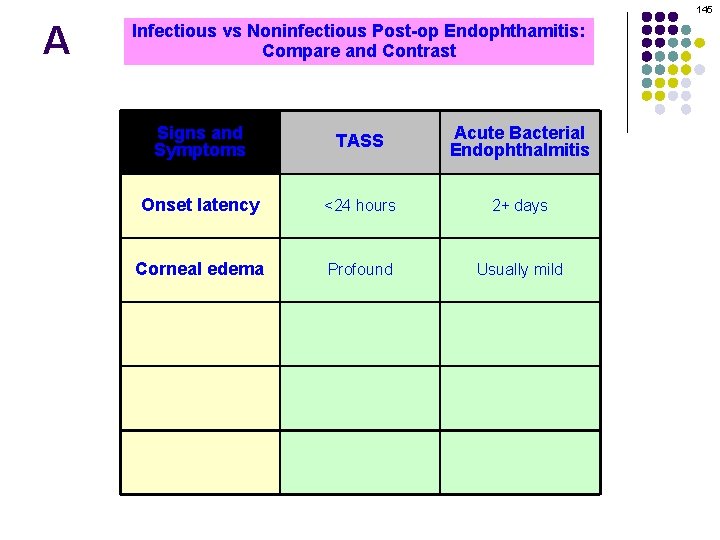
145 A Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present

146 Q Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound ? never Always Usually mild ? present Response to Vitritis steroids Almost Dramatic never Always Equivocal present

147 A Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present
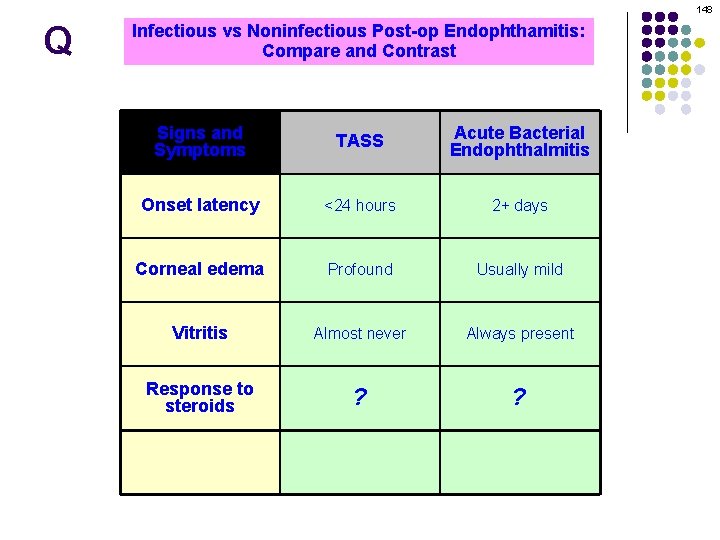
148 Q Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic ? never Always Equivocal ? present
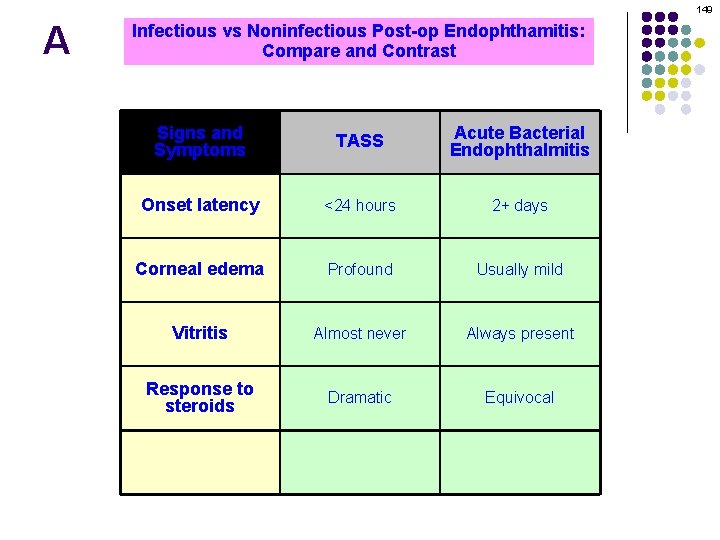
149 A Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present

150 Q Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present Pain ? ?

151 A Infectious vs Noninfectious Post-op Endophthamitis: Compare and Contrast Signs and Symptoms TASS Acute Bacterial Endophthalmitis Signslatency and Onset Symptoms <24 hours TASS Infectious 2+ days Endophthalmitis Onset latency Corneal edema <24 hours Profound 2+ days Usually mild Corneal Vitritis edema Almost Profound never Always Usually present mild Response to Vitritis steroids Almost Dramatic never Always Equivocal present Pain <<Severe
152 Q l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Probably not What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia )
153 A l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia )
154 Q l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia )
155 A l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia )
156 Q l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia )

157 A l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia )
158 Q l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) medical condition abx

159 Q l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia )
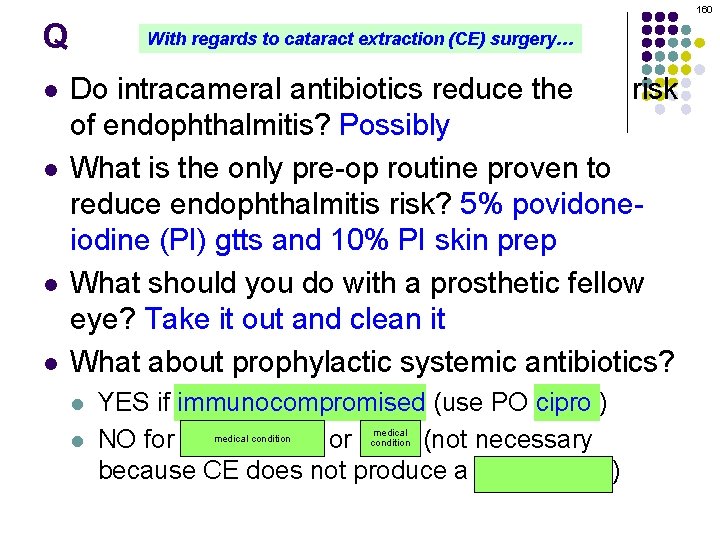
160 Q l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) medical condition
161 A l l With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly What is the only pre-op routine proven to reduce endophthalmitis risk? 5% povidoneiodine (PI) gtts and 10% PI skin prep What should you do with a prosthetic fellow eye? Take it out and clean it What about prophylactic systemic antibiotics? l l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) (MVP = Mitral valve prolapse)

162 Q With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly The efficacy of intracameral antibiotics for endophthalmitis prophylaxis in CE surgery is a complex and l What is the only pre-op routine proven to contentious issue at this time. A recent enormous multicenter prospective study in Europe found that infiltrating cefuroxime into the AC at the end of CE surgery resulted in a five-fold decrease in post-op reduce endophthalmitis risk? 5% povidoneendopthalmitis rates compared to placebo infiltration. iodine (PI) gtts and 10% PI skin prep So case closed then—intracameral cefuroxime is the way to go, right? Not so fast. While cefuroxime was better than placebo, it might not fare any better than the common l What you doantibiotics with (usually a prosthetic fellow American practice ofshould perioperative prophylactic a fourth-generation fluoroquinolone). Take it out and clean So case eye? closed then—perioperative fluoroquinolone is the way it to go, right? Not so fast. The Europeans argue that it is irresponsible to use these agents for prophylaxis, as this will lead l inevitably to resistance (in fact, resistance has alreadysystemic appeared). What about prophylactic antibiotics? l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) So case l closed then—intracameral cefuroxime is the way to go, right? Not so fast. Cefuroxime doesn’t cover Pseudomonas and (especially) MRSA. Additionally, intracameral -appropriate doses of cefuroxime are not available in the US, and Big Pharm is not anxious to provide l them (poor profit margin). Like I said: A complex and contentious issue…
163 A With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly The efficacy of intracameral antibiotics for endophthalmitis prophylaxis in CE surgery is a complex and l What is the only pre-op routine proven to contentious issue at this time. A recent enormous multicenter prospective study in Europe found that infiltrating cefuroxime into the AC at the end of CE surgery resulted in a five-fold decrease in post-op reduce endophthalmitis risk? 5% povidoneendopthalmitis rates compared to placebo infiltration. iodine (PI) gtts and 10% PI skin prep So case closed then—intracameral cefuroxime is the way to go, right? Not so fast. While cefuroxime was better than placebo, it might not fare any better than the common l What you doantibiotics with (usually a prosthetic fellow American practice ofshould perioperative prophylactic a fourth-generation fluoroquinolone). Take it out and clean So case eye? closed then—perioperative fluoroquinolone is the way it to go, right? Not so fast. The Europeans argue that it is irresponsible to use these agents for prophylaxis, as this will lead l inevitably to resistance (in fact, resistance has alreadysystemic appeared). What about prophylactic antibiotics? l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) So case l closed then—intracameral cefuroxime is the way to go, right? Not so fast. Cefuroxime doesn’t cover Pseudomonas and (especially) MRSA. Additionally, intracameral -appropriate doses of cefuroxime are not available in the US, and Big Pharm is not anxious to provide l them (poor profit margin). Like I said: A complex and contentious issue…
164 Q With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly The efficacy of intracameral antibiotics for endophthalmitis prophylaxis in CE surgery is a complex and l What is the only pre-op routine proven to contentious issue at this time. A recent enormous multicenter prospective study in Europe found that infiltrating cefuroxime into the AC at the end of CE surgery resulted in a five-fold decrease in post-op reduce endophthalmitis risk? 5% povidoneendopthalmitis rates compared to placebo infiltration. iodine (PI) gtts and 10% PI skin prep So case closed then—intracameral cefuroxime is the way to go, right? Not so fast. While cefuroxime was better than placebo, it might not fare any better than the common l What you doantibiotics with (usually a prosthetic fellow American practice ofshould perioperative prophylactic a fourth-generation fluoroquinolone). Take it out and clean So case eye? closed then—perioperative fluoroquinolone is the way it to go, right? Not so fast. The Europeans argue that it is irresponsible to use these agents for prophylaxis, as this will lead l inevitably to resistance (in fact, resistance has alreadysystemic appeared). What about prophylactic antibiotics? l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) So case l closed then—intracameral cefuroxime is the way to go, right? Not so fast. Cefuroxime doesn’t cover Pseudomonas and (especially) MRSA. Additionally, intracameral -appropriate doses of cefuroxime are not available in the US, and Big Pharm is not anxious to provide l them (poor profit margin). Like I said: A complex and contentious issue…
165 A With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly The efficacy of intracameral antibiotics for endophthalmitis prophylaxis in CE surgery is a complex and l What is the only pre-op routine proven to contentious issue at this time. A recent enormous multicenter prospective study in Europe found that infiltrating cefuroxime into the AC at the end of CE surgery resulted in a five-fold decrease in post-op reduce endophthalmitis risk? 5% povidoneendopthalmitis rates compared to placebo infiltration. iodine (PI) gtts and 10% PI skin prep So case closed then—intracameral cefuroxime is the way to go, right? Not so fast. While cefuroxime was better than placebo, it might not fare any better than the common l What you doantibiotics with (usually a prosthetic fellow American practice ofshould perioperative prophylactic a fourth-generation fluoroquinolone). Take it out and clean So case eye? closed then—perioperative fluoroquinolone is the way it to go, right? Not so fast. The Europeans argue that it is irresponsible to use these agents for prophylaxis, as this will lead l inevitably to resistance (in fact, resistance has alreadysystemic appeared). What about prophylactic antibiotics? l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) So case l closed then—intracameral cefuroxime is the way to go, right? Not so fast. Cefuroxime doesn’t cover Pseudomonas and (especially) MRSA. Additionally, intracameral -appropriate doses of cefuroxime are not available in the US, and Big Pharm is not anxious to provide l them (poor profit margin). Like I said: A complex and contentious issue…
166 Q With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly The efficacy of intracameral antibiotics for endophthalmitis prophylaxis in CE surgery is a complex and l What is the only pre-op routine proven to contentious issue at this time. A recent enormous multicenter prospective study in Europe found that infiltrating cefuroxime into the AC at the end of CE surgery resulted in a five-fold decrease in post-op reduce endophthalmitis risk? 5% povidoneendopthalmitis rates compared to placebo infiltration. iodine (PI) gtts and 10% PI skin prep So case closed then—intracameral cefuroxime is the way to go, right? Not so fast. While cefuroxime was better than placebo, it might not fare any better than the common l What you doantibiotics with (usually a prosthetic fellow American practice ofshould perioperative prophylactic a fourth-generation fluoroquinolone). Take it out and clean So case eye? closed then—perioperative fluoroquinolone is the way it to go, right? Not so fast. The Europeans argue that it is irresponsible to use these agents for prophylaxis, as this will lead l inevitably to resistance (in fact, resistance has alreadysystemic appeared). What about prophylactic antibiotics? l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) So case l closed then—intracameral cefuroxime is the way to go, right? Not so fast. Cefuroxime doesn’t cover Pseudomonas and (especially) MRSA. Additionally, intracameral -appropriate doses of cefuroxime are not available in the US, and Big Pharm is not anxious to provide l them (poor profit margin). Like I said: A complex and contentious issue…
167 A With regards to cataract extraction (CE) surgery… Do intracameral antibiotics reduce the risk of endophthalmitis? Possibly The efficacy of intracameral antibiotics for endophthalmitis prophylaxis in CE surgery is a complex and l What is the only pre-op routine proven to contentious issue at this time. A recent enormous multicenter prospective study in Europe found that infiltrating cefuroxime into the AC at the end of CE surgery resulted in a five-fold decrease in post-op reduce endophthalmitis risk? 5% povidoneendopthalmitis rates compared to placebo infiltration. iodine (PI) gtts and 10% PI skin prep So case closed then—intracameral cefuroxime is the way to go, right? Not so fast. While cefuroxime was better than placebo, it might not fare any better than the common l What you doantibiotics with (usually a prosthetic fellow American practice ofshould perioperative prophylactic a fourth-generation fluoroquinolone). Take it out and clean So case eye? closed then—perioperative fluoroquinolone is the way it to go, right? Not so fast. The Europeans argue that it is irresponsible to use these agents for prophylaxis, as this will lead l inevitably to resistance (in fact, resistance has alreadysystemic appeared). What about prophylactic antibiotics? l YES if immunocompromised (use PO cipro ) NO for heart valves or MVP (not necessary because CE does not produce a bacteremia ) So case l closed then—intracameral cefuroxime is the way to go, right? Not so fast. Cefuroxime doesn’t cover Pseudomonas and (especially) MRSA. Additionally, intracameral -appropriate doses of cefuroxime are not available in the US, and Big Pharm is not anxious to provide l them (poor profit margin). Like I said: A complex and contentious issue…