Treat with confidence Trusted answers from the American
- Slides: 32
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Care of Infants with Bronchopulmonary Dysplasia Jatinder Bhatia, MD, FAAP Professor and Chief, Division of Neonatology Vice Chair, Clinical Research Department of Pediatrics Medical College of Georgia Regents University Augusta, GA
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Disclaimer § Statements and opinions expressed are those of the author and not necessarily those of the American Academy of Pediatrics. § Mead Johnson sponsors programs such as this to give healthcare professionals access to scientific and educational information provided by experts. The presenter has complete and independent control over the planning and content of the presentation, and is not receiving any compensation from Mead Johnson for this presentation. The presenter’s comments and opinions are not necessarily those of Mead Johnson. In the event that the presentation contains statements about uses of drugs that are not within the drugs' approved indications, Mead Johnson does not promote the use of any drug for indications outside the FDAapproved product label.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Learning Objectives § § § Define bronchopulmonary dysplasia (BPD). List the risk factors for BPD. Identify current strategies to prevent BPD. Describe current management of BPD. Discuss implications for the practicing pediatrician.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Definition § Originally defined by Northway – Clinical, radiological, and pathologic changes – Prolonged mechanical ventilation – High inspiratory oxygen levels – Subsequently, BPD defined by clinical characteristics present at 1 month in association with radiological changes Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy in hyaline membrane disease: bronchopulmonary dysplasia. N Engl J Med. 1967; 276(7): 357– 368.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Births in the United States § § Number of births: 3, 932, 181 Birth rate: 12. 4 per 1000 population Percent born low birthweight: 8% Percent born preterm (<37 weeks gestation): 11. 4% Martin JA, Hamilton BE, Osterman MJK, et al. Births: final data for 2013. Natl Vital Stat Rep. 2015; 64(1): 1– 65.
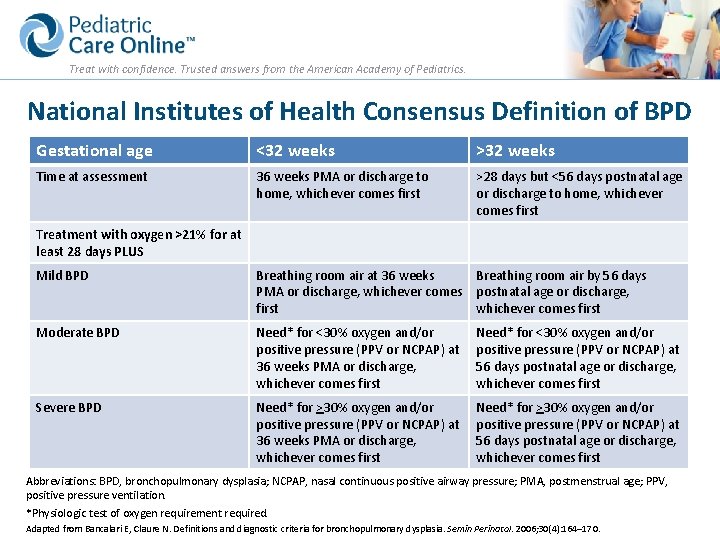
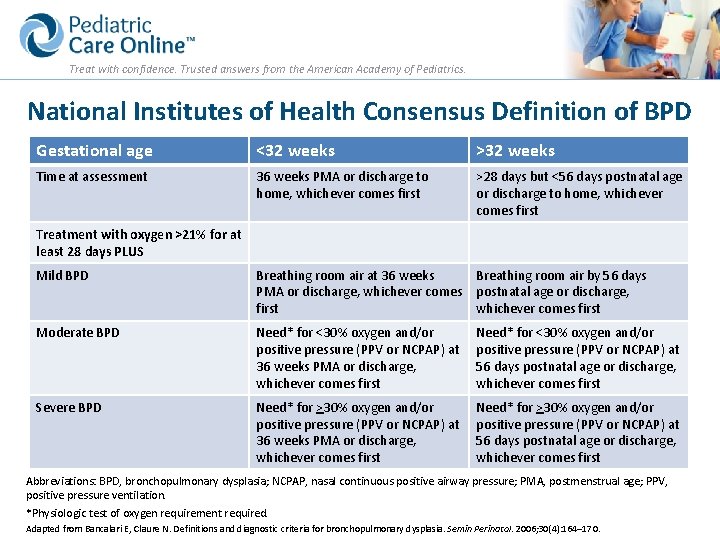
Treat with confidence. Trusted answers from the American Academy of Pediatrics. National Institutes of Health Consensus Definition of BPD Gestational age <32 weeks >32 weeks Time at assessment 36 weeks PMA or discharge to home, whichever comes first >28 days but <56 days postnatal age or discharge to home, whichever comes first Treatment with oxygen >21% for at least 28 days PLUS Mild BPD Breathing room air at 36 weeks Breathing room air by 56 days PMA or discharge, whichever comes postnatal age or discharge, first whichever comes first Moderate BPD Need* for <30% oxygen and/or positive pressure (PPV or NCPAP) at 36 weeks PMA or discharge, whichever comes first Need* for <30% oxygen and/or positive pressure (PPV or NCPAP) at 56 days postnatal age or discharge, whichever comes first Severe BPD Need* for >30% oxygen and/or positive pressure (PPV or NCPAP) at 36 weeks PMA or discharge, whichever comes first Need* for >30% oxygen and/or positive pressure (PPV or NCPAP) at 56 days postnatal age or discharge, whichever comes first Abbreviations: BPD, bronchopulmonary dysplasia; NCPAP, nasal continuous positive airway pressure; PMA, postmenstrual age; PPV, positive pressure ventilation. *Physiologic test of oxygen requirement required. Adapted from Bancalari E, Claure N. Definitions and diagnostic criteria for bronchopulmonary dysplasia. Semin Perinatol. 2006; 30(4): 164– 170.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Physiologic Test for Diagnosis of BPD § Infants receiving <30% O 2 or >30% O 2 with oxygen saturations >96% – O 2 progressively weaned to 21% (room air) – No BPD if saturations remain >90% in room air for 30 minutes – Reduces the incidence of the diagnosis of BPD Walsh MC, Yao Q, Gettner P, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004; 114(5): 1305– 1311.
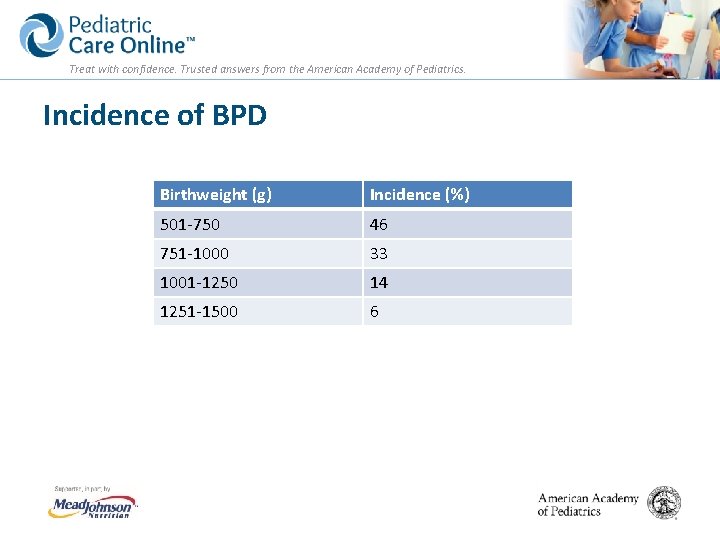
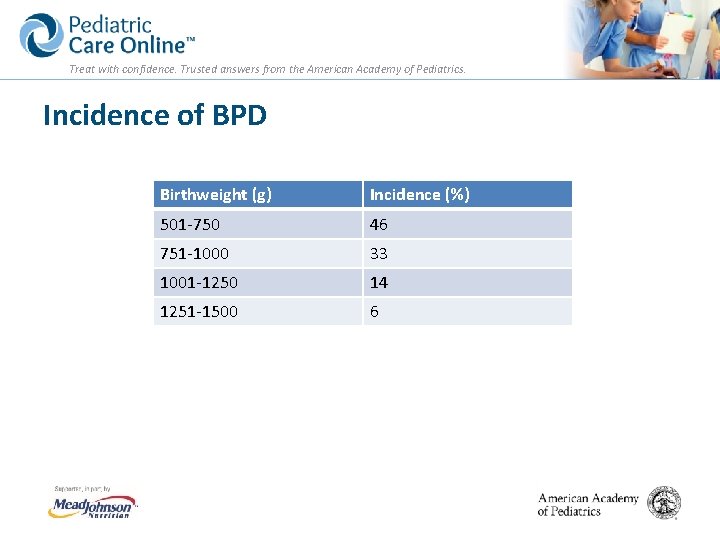
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Incidence of BPD Birthweight (g) Incidence (%) 501 -750 46 751 -1000 33 1001 -1250 14 1251 -1500 6
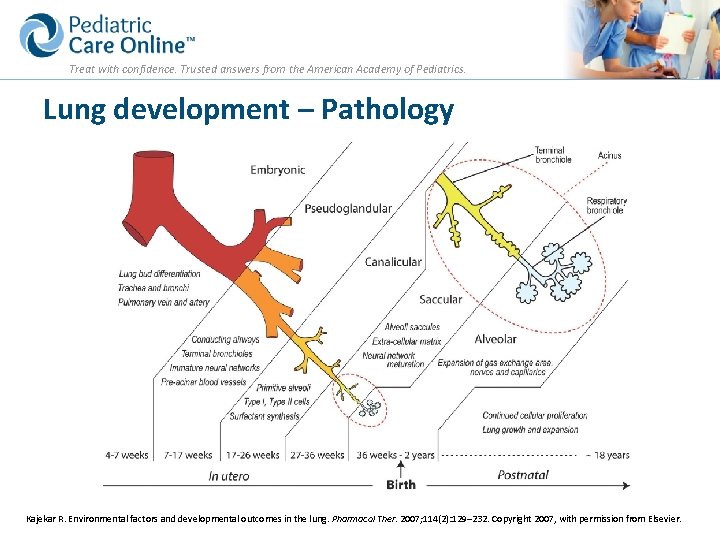
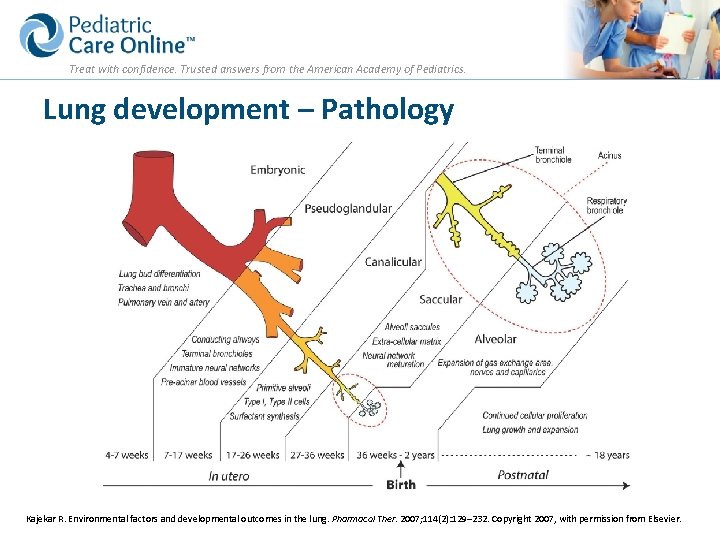
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Lung development – Pathology Kajekar R. Environmental factors and developmental outcomes in the lung. Pharmacol Ther. 2007; 114(2): 129– 232. Copyright 2007, with permission from Elsevier.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Risk Factors for BPD § § Genetic predisposition, male gender, Caucasian Peripartum infection Mechanical ventilation Fluid management – Excessive fluids in the first few days § Patent ductus arteriosus (PDA) – Left to right symptomatic PDA
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Role of Mechanical Ventilation § Major role – Barotrauma, volutrauma – Use of excessive inflation pressures – Not allowing permissive hypercapnea (as long as p. H is satisfactory) – Even a small number of inflations (for example, bagging) and use of high oxygen concentrations soon after birth can affect surfactant deficient lungs: implications for delivery room management
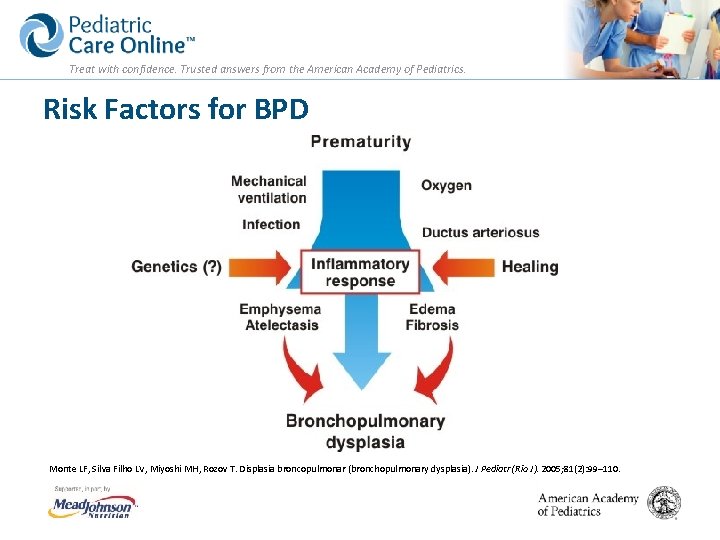
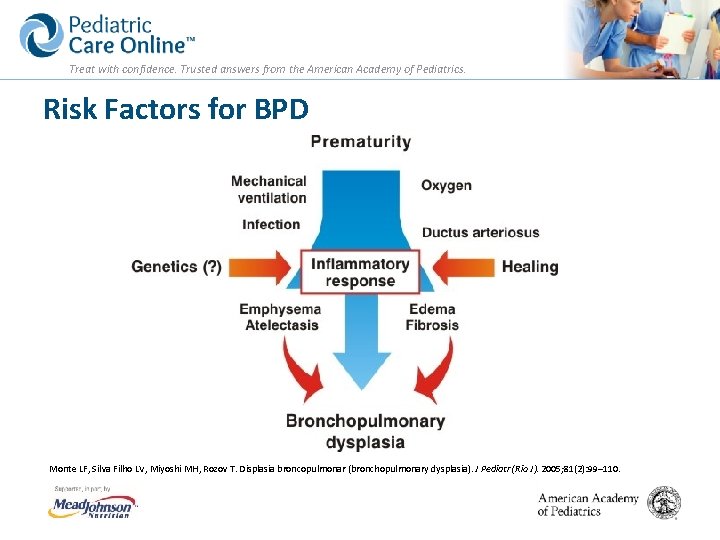
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Risk Factors for BPD Monte LF, Silva Filho LV, Miyoshi MH, Rozov T. Displasia broncopulmonar (bronchopulmonary dysplasia). J Pediatr (Rio J). 2005; 81(2): 99– 110.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Other Factors § Oxygen toxicity (use current targeted oxygen saturations) § Nutrient deficiencies – Vitamin A § Immature antioxidant systems – Superoxide dismutase – Glutathione peroxidase § Infections, inflammation – Sepsis: bacterial and fungal
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Symptoms of BPD § § § Rapid, shallow breathing Continued need for oxygen or ventilatory support Peripheral cyanosis Intercostal retractions Use of accessory muscles of respiration
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Other Issues § § § Trouble feeding Increased work of breathing Delayed growth Development of pulmonary hypertension Cor pulmonale
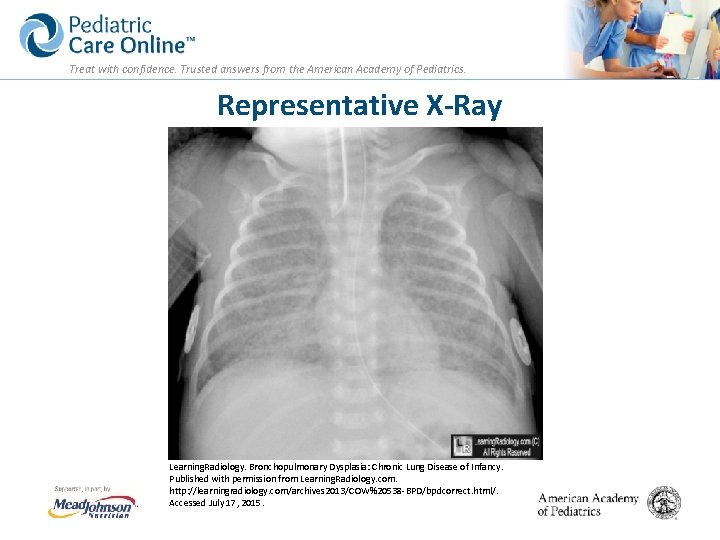
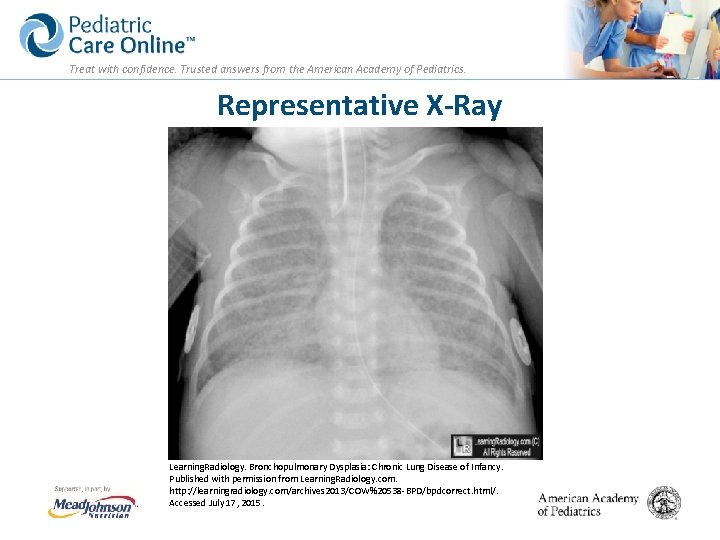
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Representative X-Ray Learning. Radiology. Bronchopulmonary Dysplasia: Chronic Lung Disease of Infancy. Published with permission from Learning. Radiology. com. http: //learningradiology. com/archives 2013/COW%20538 -BPD/bpdcorrect. html/. Accessed July 17, 2015.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Diagnosis § Premature infants, especially those <30 weeks, and still requiring oxygen therapy at original due date § Mild, moderate, or severe § Chest x-ray findings: infiltrates/atelectasis § Blood gas: low O 2, high p. CO 2, low (initially) and later normal p. H with compensation
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Treatment Goals § Prenatal steroids to reduce respiratory distress syndrome § Reduce lung injury by minimizing ventilatory support § Appropriate oxygen saturation targets § Appropriate nutrition to promote growth and prevent extra uterine growth failure/restriction § Aggressive treatment of infections
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Treatment Goals: Drugs that Prevent BPD § Vitamin A: Intramuscular vitamin A* (5000 IU, IM, 3 x week, over 4 weeks) § Relative risk of death or BPD at 36 weeks PMA: 0. 91, 95% CI 0. 83, 1. 00 § Relative risk of reducing death or O 2 requirement at 1 month of age: 0. 93, 95% CI 0. 88, 0. 99 § Oxygen requirement at 36 weeks, 0. 87, 95% CI 0. 77 -0. 99 § Meta-analysis confirmed the reduction of BPD with vitamin A *Would be considered a therapeutic dose. Tyson JE, Wright LL, Oh W, et al. Vitamin A supplementation for extremely-low-birth-weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med. 1999; 340(25): 1962– 1968; and Darlow BA, Graham PJ. Vitamin A supplementation to prevent mortality and short- and long-term morbidity in very low birthweight infants. Cochrane Database Syst Rev. 2011; 10: CD 000501.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Treatment Goals § Caffeine citrate – Caffeine for apnea trial: 2006 infants treated for apnea with primary outcome of death, cerebral palsy, cognitive delay, deafness, or blindness at 18 -21 months corrected age – Secondary analysis: BPD, retinopathy of prematurity, and necrotizing enterocolitis – Infants treated with caffeine had lower risk of BPD than placebo: relative risk 0. 63, 95% CI 0. 52, 0. 73 – Caffeine citrate use in premature infants resulted in a significant reduction in BPD with few side effects. Schmidt B, Roberts RS, Davis P, et al. Caffeine therapy for apnea of prematurity. N Engl J Med. 2006; 354(20): 2112– 2121; and Picone S, Bedetta M, Paolillo P. Caffeine citrate: when and for how long. A literature review. J Matern Fetal Neonatal Med. 2012; 25(S 3): 11– 14.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Treatment Goals: Other Drugs § Late steroids: may have a role § Inositol § Azithromycin/Clarithromycin (eradication of Ureaplasma urealyticum) reduced BPD: does not have FDA-labeled instructions § Inhaled nitric oxide § Other Ballard HO, Shook LA, Bernard P, et al. Use of azithromycin for the prevention of bronchopulmonary dysplasia in preterm infants: a randomized, doubleblind, placebo controlled trial. Pediatr Pulmonol. 2011; 46(2): 111– 118; Beam KS, Aliaga S, Ahlfeld SK, Cohen-Wolkowiez M, Smith PB, Laughon MM. A systematic review of randomized controlled trials for the prevention of bronchopulmonary dysplasia in infants. J Perinatol. 2014; 34(9): 705– 710; Hallman M, Bry K, Hoppu K, Loppi M, Pohjavuori M. Inositol supplementation in premature infants with respiratory distress syndrome. New Engl J Med. 1992; 326(19): 1233– 1239; Ozdemir R, Erdeve O, Dizdar EA, et al. Clarithromycin in preventing bronchopulmonary dysplasia in Ureaplasma urealyticum– positive preterm infants. Pediatrics. 2011; 128(6): e 1496–e 1501; and Doyle LW, Ehrenkranz RA, Halliday HL. Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database Syst Rev. 2014; 5: CD 001145.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Nutrition and Other § Total energy needs may be increased: need to provide energy and protein to satisfy growth requirements § Fluid restriction often required, necessitating calorically dense feedings § Diuretics: electrolyte imbalance; little evidence that they improve outcome Adams JM, Stark A. Management of bronchopulmonary dysplasia, Up. To. Date. June 2015; Gianni ML, Roggero P, Colnaghi MR, et al. The role of nutrition in promoting growth in pre-term infants with bronchopulmonary dysplasia: a prospective non-randomised interventional cohort study. BMC Pediatr. 2014; 14: 235; and Lai NM, Rajadurai SV, Tan K. Increased energy intake for preterm infants with (or developing) bronchopulmonary dysplasia/chronic lung disease. Cochrane Database Syst Rev. 2006; 3: CD 005093.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Prevention § Vitamin A – Involved in regulation of lung development and repair – Prophylactic vitamin A decreases incidence of BPD – Need to treat ~14 -15 infants to have 1 infant survive without BPD § Caffeine – Reduces BPD; mechanism not known
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Prevention § Corticosteroids – High-dose prolonged therapy with dexamethasone used to be standard therapy for BPD. – Increase in adverse neurodevelopment – AAP policy statement recommends limited use under “exceptional clinical circumstances. ”a – When given after 14 days of life, corticosteroids may have short- and long-term benefits that need to be confirmed in larger trials. a Watterberg KL and American Academy of Pediatrics Committee on Fetus and Newborn. Postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia. Pediatrics. 2010; 126(4): 800– 808.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. BPD and the Pediatrician § Abnormal lung function through school age and beyond § More respiratory symptoms, asthma treatment § Pulmonary and systemic hypertension, cor pulmonale
Treat with confidence. Trusted answers from the American Academy of Pediatrics. BPD and the Pediatrician § Poor neurodevelopmental outcome – Language delays – Fine and gross motor impairment § Other – – Feeding difficulty Gastroesophageal reflux Increased energy expenditure Growth failure
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Outpatient Management § Home oxygen to maintain saturations >90%* § Home mechanical ventilation* § Nutritional support – Appropriate fortification of breastmilk – Appropriate formulas § Routine immunizations, including against influenza § Respiratory syncytial virus prophylaxis by AAP criteria § Developmental follow up and intervention* *Use of a multidisciplinary group or consultation suggested.
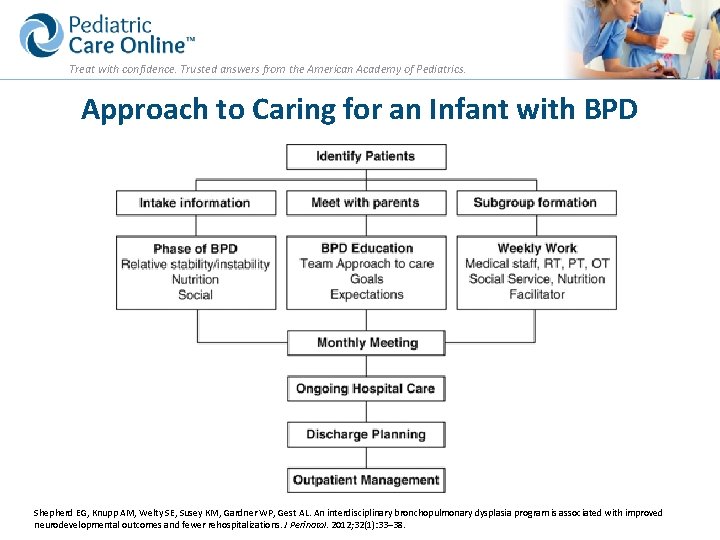
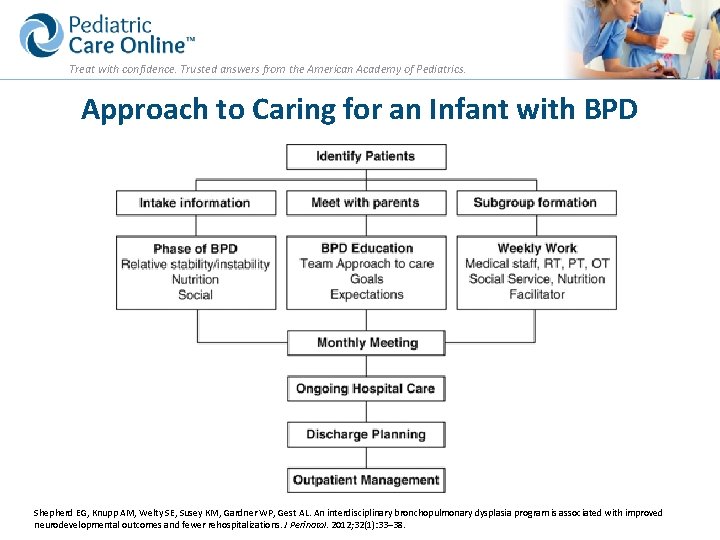
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Approach to Caring for an Infant with BPD Shepherd EG, Knupp AM, Welty SE, Susey KM, Gardner WP, Gest AL. An interdisciplinary bronchopulmonary dysplasia program is associated with improved neurodevelopmental outcomes and fewer rehospitalizations. J Perinatol. 2012; 32(1): 33– 38.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Conclusions § BPD is a known complication in premature infants with initial lung disease. § Incidence increases with decreasing gestational age. § Prenatal steroids reduce the incidence of RDS; effects on incidence of BPD are not shown. § Appropriate resuscitation, judicious use of positive pressure ventilation, and targeted oxygen saturations reduce the incidence of BPD.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Conclusions § Vitamin A has a preventative role. § Early and sustained appropriate nutrition to support growth may reduce BPD. § Caffeine therapy in high-risk infants has been shown to reduce BPD. § Post-natal growth failure is common in infants with BPD. § Post-discharge attention to nutrition can ameliorate the growth failure.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Conclusions § A multidisciplinary team approach, including a nutritionist, cardiology/pulmonary specialists, speech therapist, and developmentalists, is recommended. § Adjunctive therapy should be tailored to individual cases: postnatal steroids, diuretics, and bronchodilators. § Complications, including pulmonary artery and systemic hypertension, should be addressed.
Treat with confidence. Trusted answers from the American Academy of Pediatrics. Visit Pediatric Care Online today for additional information on this and other topics. http: //pediatriccare. solutions. aap. org Pediatric Care Online is a convenient electronic resource for immediate expert help with virtually every pediatric clinical information need with must-have resources that are included in a comprehensive reference library and time-saving clinical tools. Don’t have a subscription to PCO? Then take advantage of a free trial today! Call Mead Johnson Nutrition at 888/363 -2362.
 How do we treat the life the life how we treat
How do we treat the life the life how we treat Treat with confidence
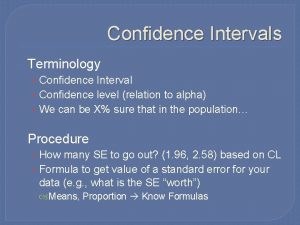
Treat with confidence Confidence interval vs confidence level
Confidence interval vs confidence level Critical value for z score
Critical value for z score The persian empire chapter 4 section 3
The persian empire chapter 4 section 3 Equation for number needed to treat
Equation for number needed to treat Invitation to treat
Invitation to treat Act iv scene ii romeo and juliet
Act iv scene ii romeo and juliet Which seedless plants have been used to treat bee stings?
Which seedless plants have been used to treat bee stings? Number needed to treat calculation
Number needed to treat calculation Offer
Offer Mylantah
Mylantah Calculate number needed to harm
Calculate number needed to harm Nnt formula
Nnt formula Number need to treat
Number need to treat Number needed to treat
Number needed to treat Invitation to treat
Invitation to treat Absolute risk formula
Absolute risk formula Invitation to treat meaning
Invitation to treat meaning Treat everyone with sincerity
Treat everyone with sincerity Summary of act 2 scene 4 romeo and juliet
Summary of act 2 scene 4 romeo and juliet Is byetta used to treat pcos
Is byetta used to treat pcos Treat everyone with sincerity
Treat everyone with sincerity Social facilitation vs social loafing
Social facilitation vs social loafing Mole day treat ideas
Mole day treat ideas How to treat bursitis in the hip
How to treat bursitis in the hip Treat others the way you would like to be
Treat others the way you would like to be Jesuit handbook on lycanthropic culture shock
Jesuit handbook on lycanthropic culture shock Felicia gizycka
Felicia gizycka Treat someone with contempt
Treat someone with contempt Epidydmis
Epidydmis How does aunt alexandra treat calpurnia
How does aunt alexandra treat calpurnia Intention to treat analysis
Intention to treat analysis