Therapeutic Exercises Do Dr Duygu Geler KLC Yeditepe
- Slides: 26
Therapeutic Exercises Doç. Dr. Duygu Geler KÜLCÜ Yeditepe University Medical Faculty Dept. Of Physical Medicine and Rehabilitation
• Therapeutic exercises are prescribed to improve flexibility, increase endurance, aerobic capacity, and strengthening, among other purposes. 2
STRENGTHENING EXERCISES • Are designed to increase the maximal force that a muscle or muscle group can generate Strength is affected by several factors, such as: the type of muscle contraction, speed of contraction, crosssectional size of the muscle, length– tension relationship, and the recruitment of motor units. 3
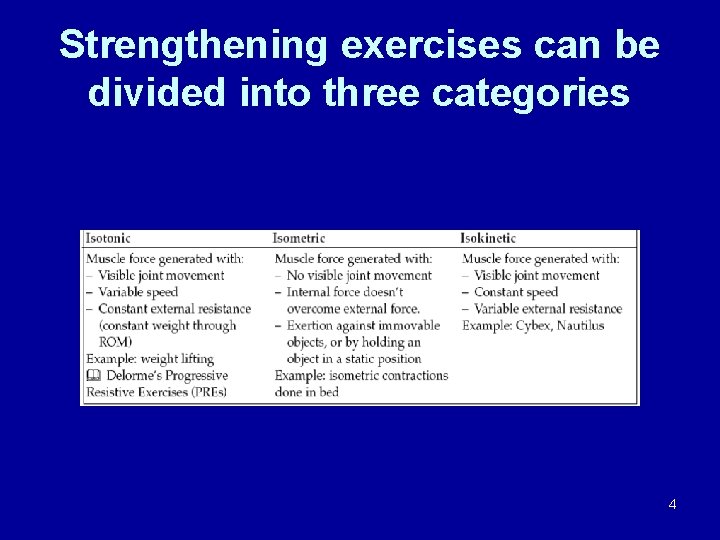
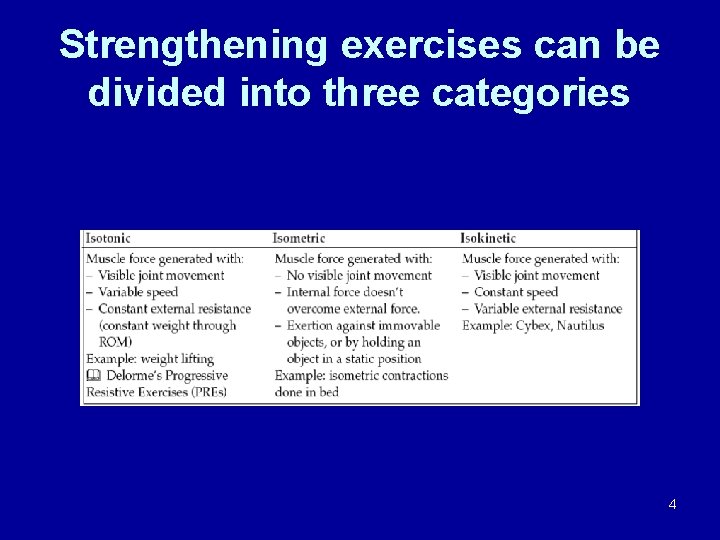
Strengthening exercises can be divided into three categories 4
Delorme exercises • progressive resistive technique—The greatest weight that can be lifted, pulled, or pushed 10 times through full ROM is determined. The patient performs one set of repetitions at 50% of the 10 RM (repetition maximum), a second set of 75% of the 10 RM, and a final set of 10 repetitions of full 10 RM. • Each session consists of the three sets with breaks between sets. The 10 RM is determined each week with progressive advancement as strength increases. 5
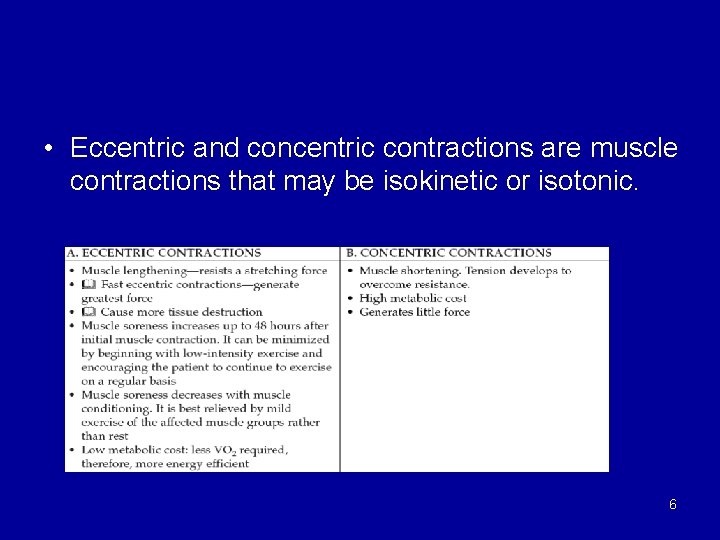
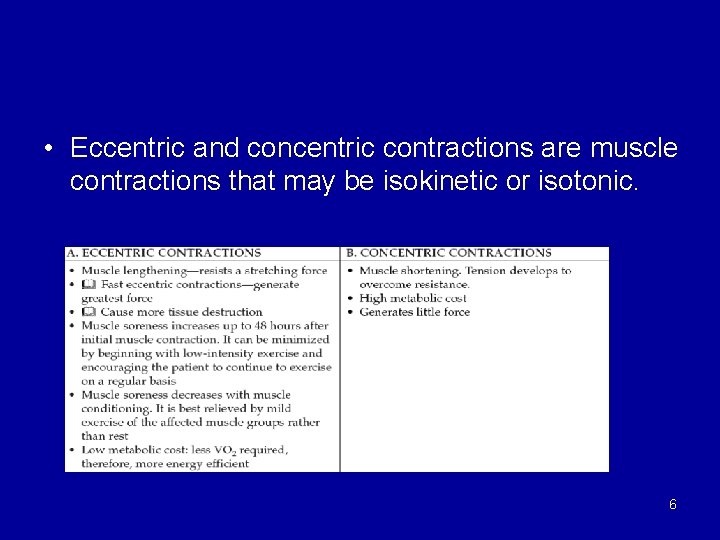
• Eccentric and concentric contractions are muscle contractions that may be isokinetic or isotonic. 6
• Improvement of muscle performance including strength can be increased by the following: – Increasing the amount of weight lifted – Increasing the amount of repetitions or sets – Increasing contraction velocity 7
Conditioning, Total Body Endurance Exercises, or Cardiopulmonary Endurance Exercises • These exercises use large muscle groups, and are continuous and rhythmic, providing low intensity and high repetition, to improve overall cardiopulmonary fitness. • They can be divided into aerobic and anaerobic endurance exercises. 8
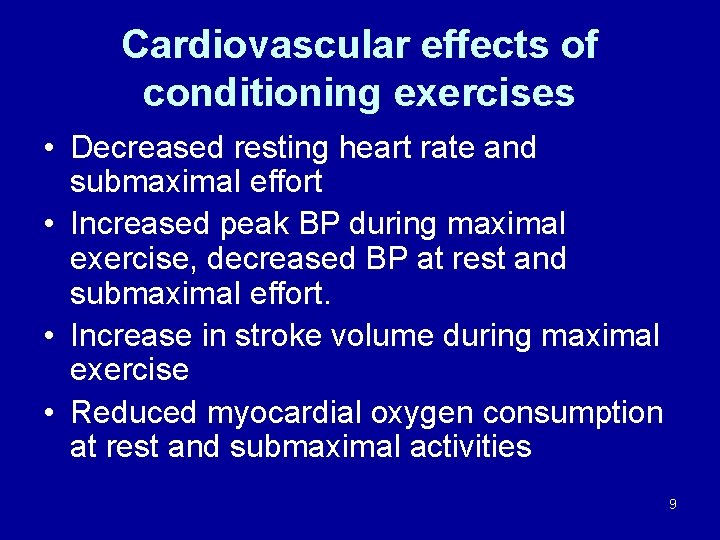
Cardiovascular effects of conditioning exercises • Decreased resting heart rate and submaximal effort • Increased peak BP during maximal exercise, decreased BP at rest and submaximal effort. • Increase in stroke volume during maximal exercise • Reduced myocardial oxygen consumption at rest and submaximal activities 9
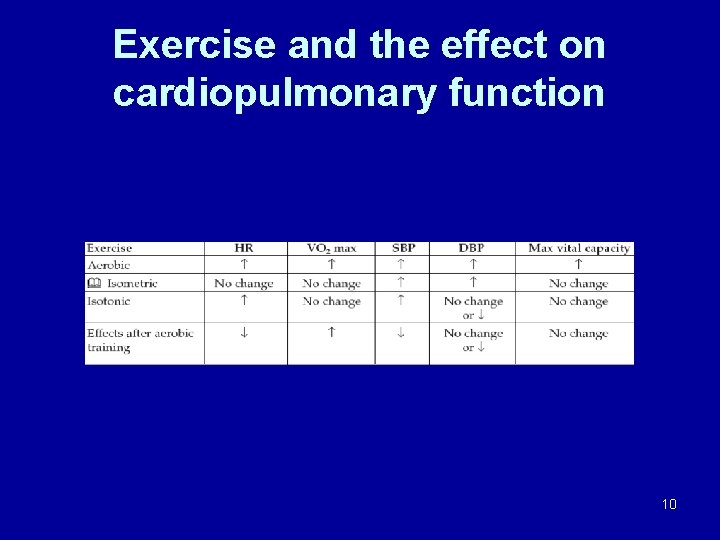
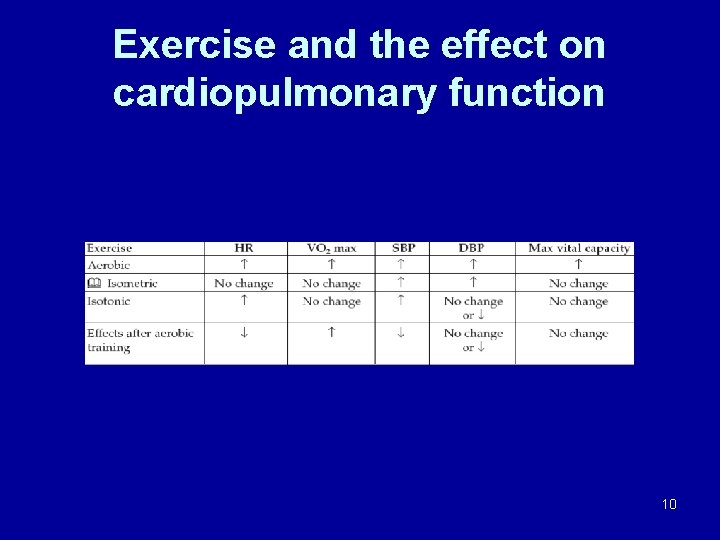
Exercise and the effect on cardiopulmonary function 10
Aerobic endurance exercises • Combination of cardiopulmonary endurance exercise with strengthening • Should consist of a warm-up period, a training period and a cool-down period: • Warm-up 5 to 10 minutes • Training period— 20 to 30 minutes at 40%– 60% (low intensity), 60%– 70% (moderate intensity), or 70%– 85% (heavy intensity) of their VO 2 max • Cool-down period 5 to 10 minutes 11
Guidelines for the quantity and quality of aerobic exercise programs for healthy adults as proposed by the American College of Sports Medicine • Mode—any exercise that uses large muscle groups, continuous and rhythmic in nature. • Examples: running, swimming, walking, stair climbing. – – Frequency— 3– 5 days/week Duration— 20– 60 minutes Intensity— 60%– 90% HR max 50%– 85% of VO 2 max or 50%– 85% of HR reserve max 12
Anaerobic exercises • High-resistance, short-duration exercises at 80% of maximum exertion capacity. • Deplete the glycolytic system, which functions during the first two minutes of exercise. 13
• • • Prevention injuries of locomotor system Increase sportive performance Continue functional capacity Increase pain threshold İncrease not fatty body mass Increase kollagen component of connective tissue • Strengthen tendon and ligaments • Increase thickness of hyalen 14
Mobility exercises: exercises to improve flexibility • Flexibility is defined as the ability to move body joints through their entire range of motion(ROM) • Each joint of the body has a specific ROM • Flexibility exercises maintain mobility within the available ROM • Flexibility exercises should be done at least three times a week, should consist of three to five repetitions once or twice a day 15
TECHNIQUES TO IMPROVE FLEXIBILITY • Can be done through anatomic planes of motion, combined planes of motion (similar to peripheral neuro-facilitation patterns), or through functional teaching activities • Stretching Exercises – Increase ROM by lengthening tendon and muscle beyond the available range – Include static stretching, static stretching with contraction of the antagonist muscle (reciprocal inhibition), static stretching with contraction of the agonist muscle, and ballistic stretching • Ballistic stretching—utilizes repetitive bouncing movements with a rapid stretch. More tension is developed, and more energy is absorbed into the muscle and tendon, which can lead to bone avulsion or muscle–tendon tears. High risk of injury • Static stretch—The joint is moved to the end of the ROM where the position is slowly held for 5 to 60 seconds. Can be done actively or passively. Safe technique • Reciprocal inhibition—The joint is also moved to the end of ROM, and this is followed by a symmetric contraction of the antagonist muscle group for 5 to 30 seconds • Static stretching with contraction of the agonist—The joint is moved to the 16 end of ROM nand followed by an isometric contraction of the agonist muscle for 5 to 30 seconds
EFFECTS OF EXTENDED BEDREST—IMMOBILIZATION AND INACTIVITY • MUSCLE – Strength—immobilization decreases strength by 1. 0% – 1. 5% per day. Strength can decrease as much as 20%– 30 % during only a week to nine days of bedrest. Five weeks of total inactivity costs 50% of the previous muscle strength. A plateau is reached 25%– 40% of original strength. One contraction a day at 50% of maximal strength is enough to prevent this decrease – Restricted activities affect muscle strength and recruitment patterns of muscles distant from specific sites of injury. 17
• BONE AND JOINTS – Lack of gravitational force and muscle pull on bone cause osteopenia. As a result of osteopenia, hypercalcemia develops. Calcium is excreted in the urine and feces starting at 2– 3 days after immobilization, and peaking at 3– 7 weeks. After activity is resumed, calcium levels remain high for 3 weeks, reaching normal values at 5– 6 weeks – Calcium excretion in addition to phosphorus loss causes atrophy and a reduction in fracture threshold of bone – Joints show a decrease in periarticular connective tissue extensibility after inactivity. – Articular cartilage begins to deteriorate due to lack of nutritional support. The hyaline cartilage in synovial joints is not supplied by vascular blood flow. It depends on nutrition from the synovial fluid through loading and unloading of pressure – Ligaments undergo biochemical changes noted as early as two weeks after immobilization. In the case of surgically repaired ligaments, improvement in strength is affected by immobilization. Immobilization causes ligament strength to decrease, compliance to increase, and collagen degradation to increase. 18
GASTROINTESTINAL (GI)—Decreased GI motility leads to constipation GENITOURINARY —Urinary stasis, leading to an increased risk of urolithiasis and urinary tract infections. PULMONARY—Diminished diaphragmatic movement and chest expansion, due to loss of strength of diaphragm and intercostal muscles, leading to impaired secretion clearance. – Reduced cough and bronchial ciliary activity. Patients can develop pneumonia. – Reduction in pulmonary function with decreased tidal volumes, decreased vital capacity. – A-V shunting and regional changes in ventilation-perfusion occur. CARDIAC – Reduction in blood and plasma volumes. – Redistribution of body fluids leads to postural hypotension. Venous blood pooling occurs in the legs. In addition, -adrenergic sympathetic activity is increased. – Cardiovascular efficiency is decreased, increased HR, decreased stroke volume. Heart rate increases approximately 0. 5 beats/minutes/day, leading to immobilization tachycardia and abnormal HR with minimal or submaximal workloads. Stroke volume decrease may reach 15% in 2 weeks of bed rest, as a result of blood volume changes and venous pooling in the lower extremities. There is also a decrease in maximal oxygen extraction (VO 2 max) that can occur as early as 3– 5 days. – Thromboembolism secondary to a decrease in blood volume and increased coagulability. INTEGUMENTARY—skin atrophy and pressure sores develop. 19
Improving Joint Range of Motion • Techniques/exercises-aim to maintain or increase the excursion of a joint – Active assisted – Passive (physiological or accessory) Prevents developing contractures Prevents elasticity of muscle Helps circulation DO NOT APPLY Acute phase of tendon, ligaments and muscle ruptures Unhealing fractures Soon after the surgery of ligament, tendon, nerve, capsule 20
Active ROM Exercises • Involves voluntary movement of a joint through a ROM without assistance 21
Active-assisted ROM Exercises • When additional force (therapist, patient or device) is applied to move the limb/joint through ROM 22
Passive ROM Exercises • When joint ROM is achieved by therapist (or device) alone, without voluntary muscle contraction by the patient. • Long lasting immobilisation • Inflammation, edema • Pain • Splint 23
Open Kinetic Chain Exercises • Exercises where the distal segment is not fixed or in contact with the ground • Used in early stages of rehabilitation 24
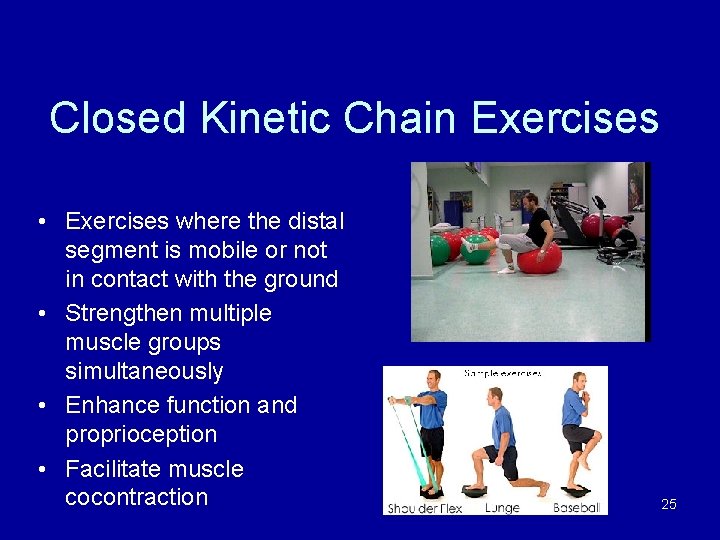
Closed Kinetic Chain Exercises • Exercises where the distal segment is mobile or not in contact with the ground • Strengthen multiple muscle groups simultaneously • Enhance function and proprioception • Facilitate muscle cocontraction 25
Retraining Proprioception/Balance • Balance training – – Progress from NWB—PWB---FWB exercises Eyes open/closed Vary surface to make more difficult Sports/activity specific • Functional retraining – İmportant to retrain function through the rehab process e. g. Walking with crutches to sports specific skills – Specific functional exercises&tasks that aim to return the patient to pre-injury level – May use EMG biofeedback 26
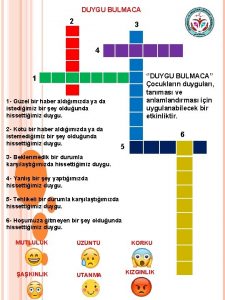
 Temel duygular listesi
Temel duygular listesi Coadsys exam
Coadsys exam Medivia
Medivia Coadsysexam yeditepe
Coadsysexam yeditepe Zoltan geler
Zoltan geler Zoltan geler
Zoltan geler Zoltan geler
Zoltan geler Zoltan geler
Zoltan geler Zoltan geler
Zoltan geler Zoltan geler
Zoltan geler Informatika ffuns
Informatika ffuns Zoltan geler
Zoltan geler Therapeutic photography exercises
Therapeutic photography exercises Principle of therapeutic exercise
Principle of therapeutic exercise Ana duygu nedir
Ana duygu nedir Dolaylı duygu örnekleri
Dolaylı duygu örnekleri Kaygs
Kaygs Duygu altun
Duygu altun Duygu çelik ertuğrul
Duygu çelik ertuğrul Duygular nelerdir
Duygular nelerdir Duygu phillips
Duygu phillips Dilanma
Dilanma Olay düşünce duygu ve hayallerin sözlü ve yazılı
Olay düşünce duygu ve hayallerin sözlü ve yazılı Semra duygu
Semra duygu Duygu çeşitleri
Duygu çeşitleri Duygu bayraktar
Duygu bayraktar Edimsel koşullanma
Edimsel koşullanma