The Urinary System Principle Organs Kidneys Ureters Urinary
- Slides: 28
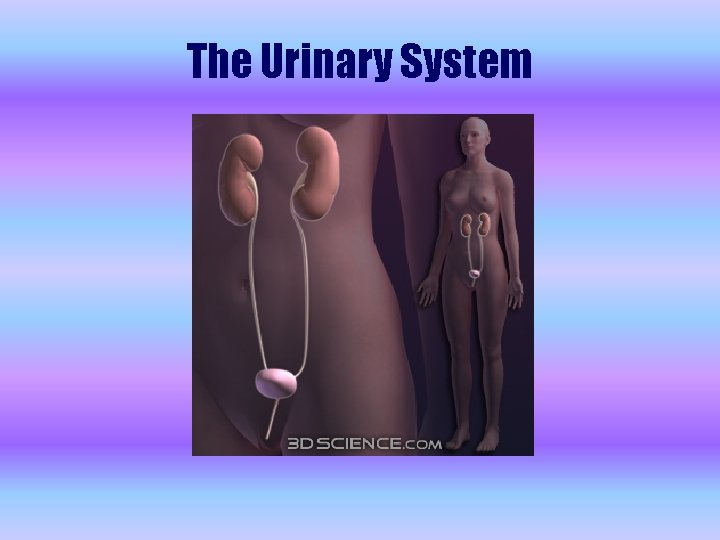
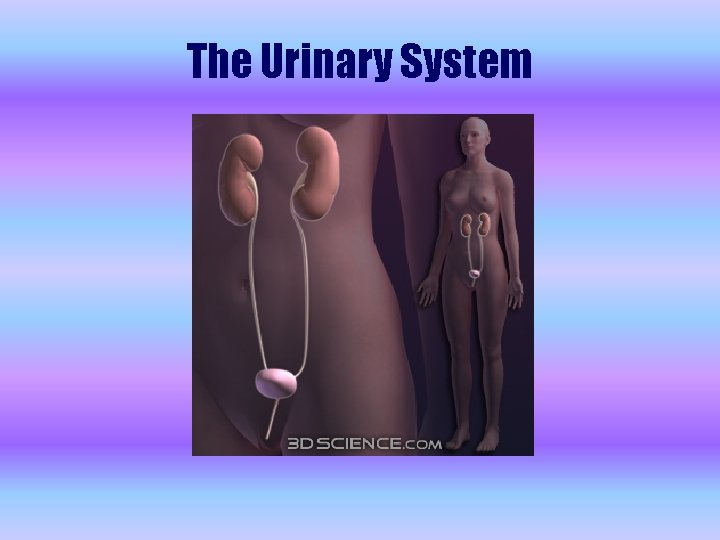
The Urinary System
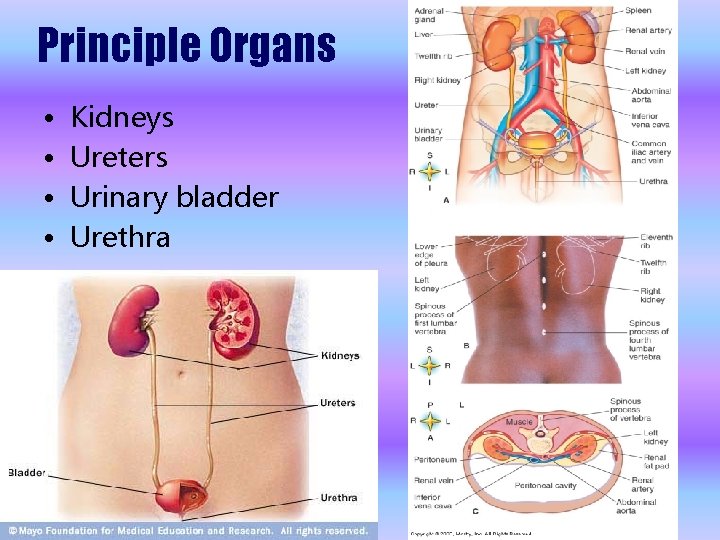
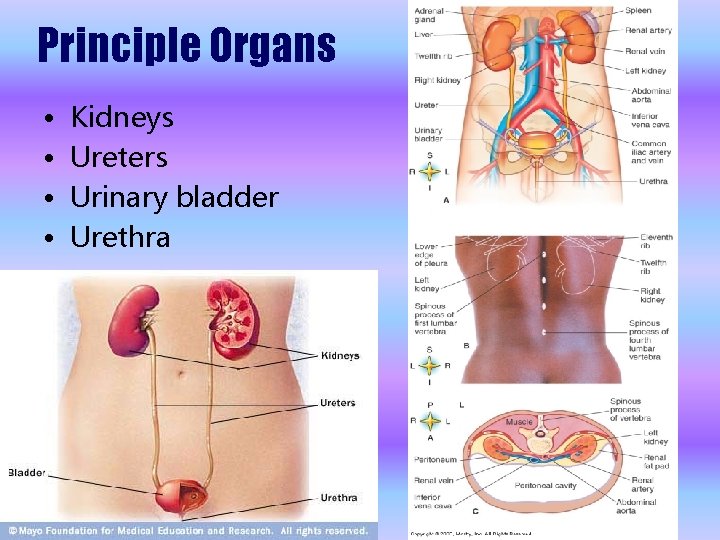
Principle Organs • • Kidneys Ureters Urinary bladder Urethra
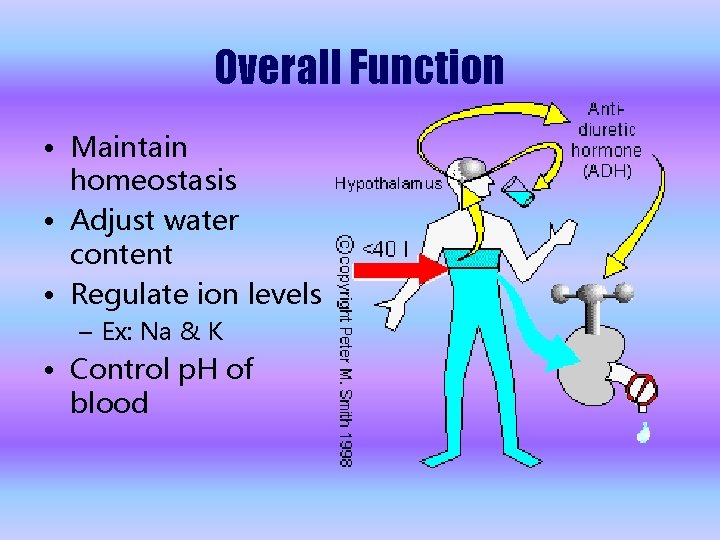
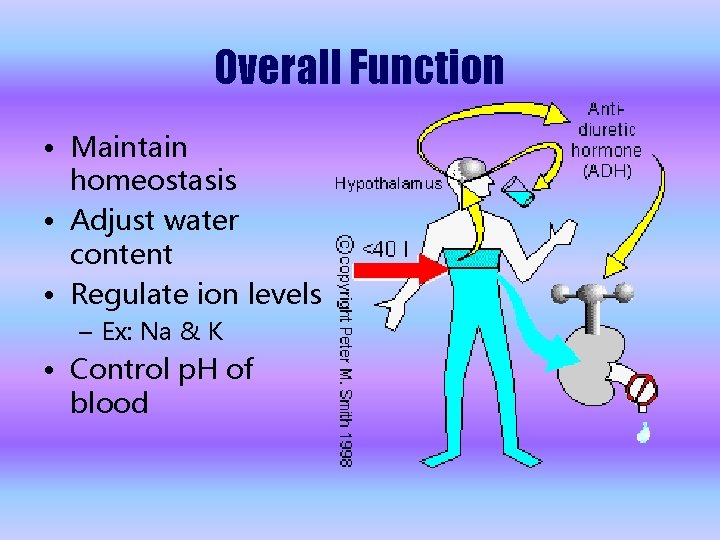
Overall Function • Maintain homeostasis • Adjust water content • Regulate ion levels – Ex: Na & K • Control p. H of blood
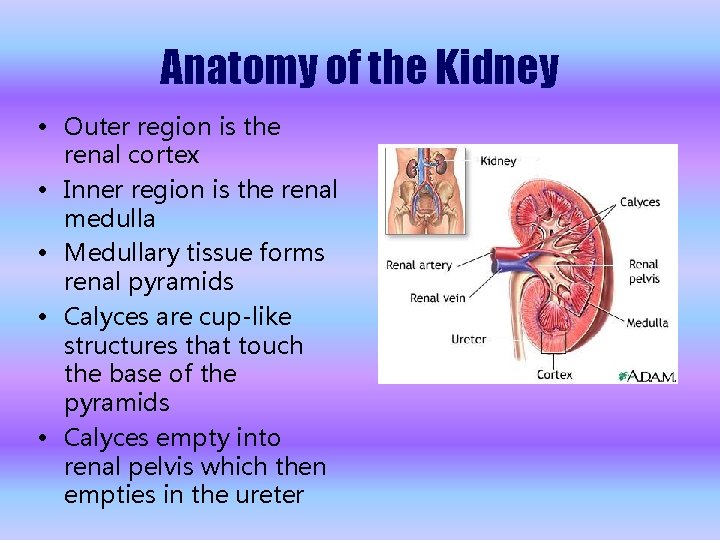
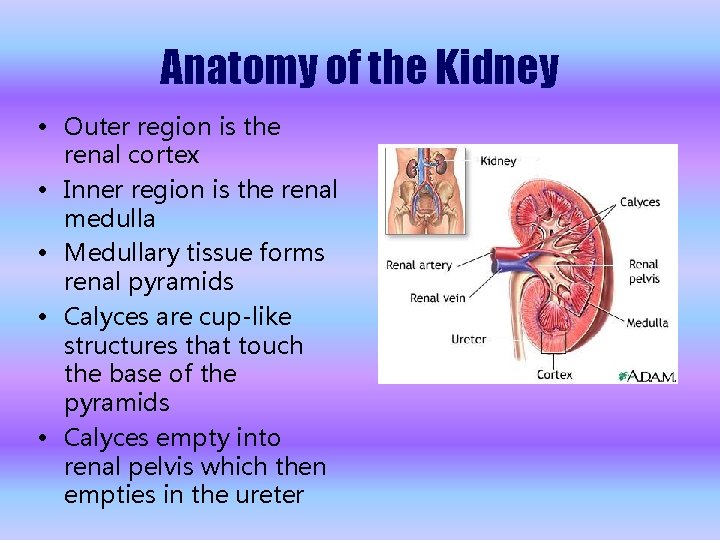
Anatomy of the Kidney • Outer region is the renal cortex • Inner region is the renal medulla • Medullary tissue forms renal pyramids • Calyces are cup-like structures that touch the base of the pyramids • Calyces empty into renal pelvis which then empties in the ureter
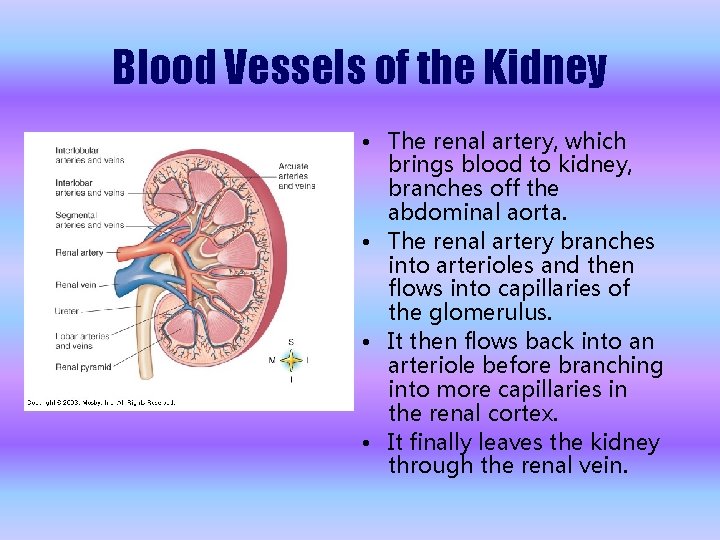
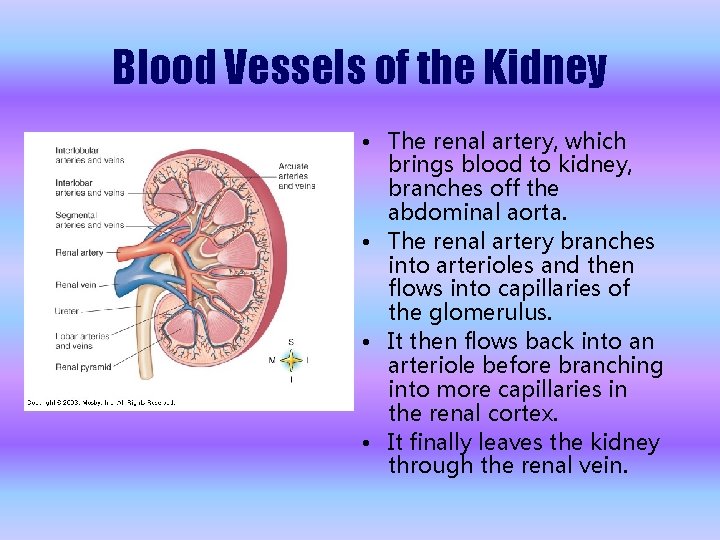
Blood Vessels of the Kidney • The renal artery, which brings blood to kidney, branches off the abdominal aorta. • The renal artery branches into arterioles and then flows into capillaries of the glomerulus. • It then flows back into an arteriole before branching into more capillaries in the renal cortex. • It finally leaves the kidney through the renal vein.
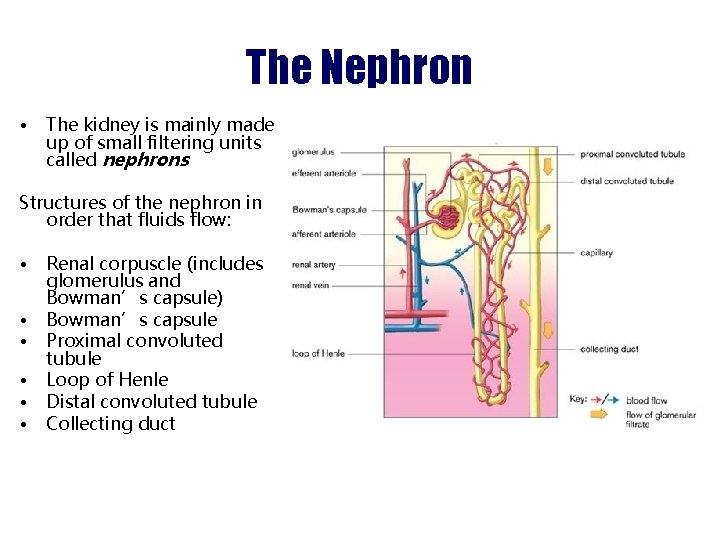
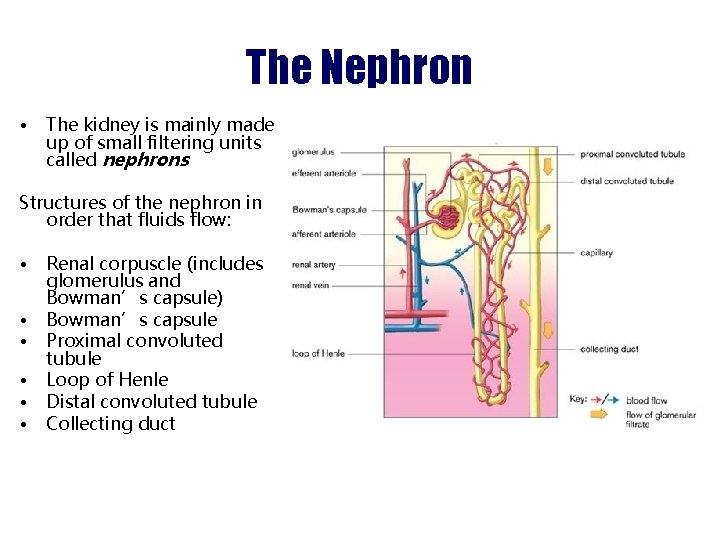
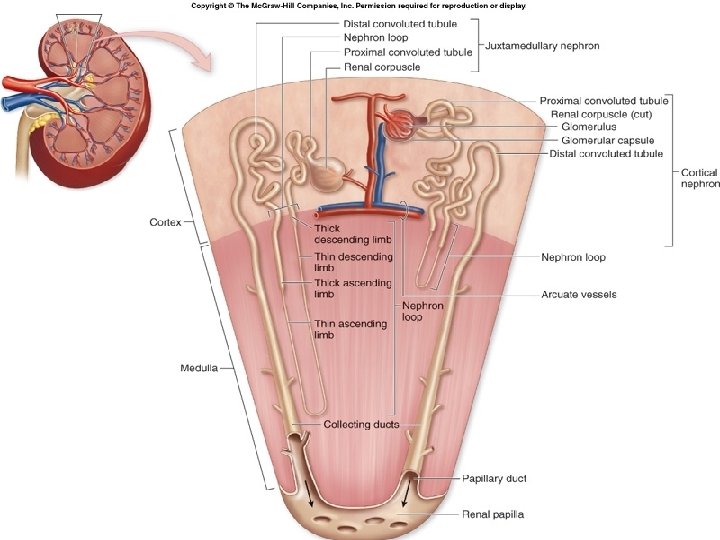
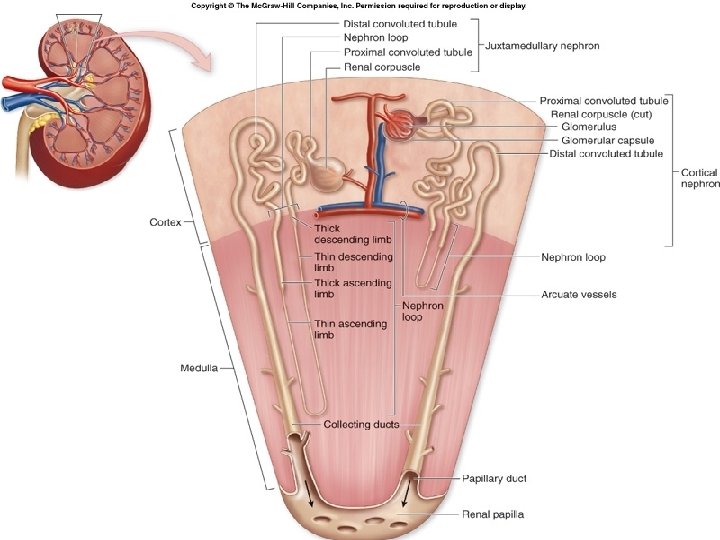
The Nephron • The kidney is mainly made up of small filtering units called nephrons Structures of the nephron in order that fluids flow: • • • Renal corpuscle (includes glomerulus and Bowman’s capsule) Bowman’s capsule Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct
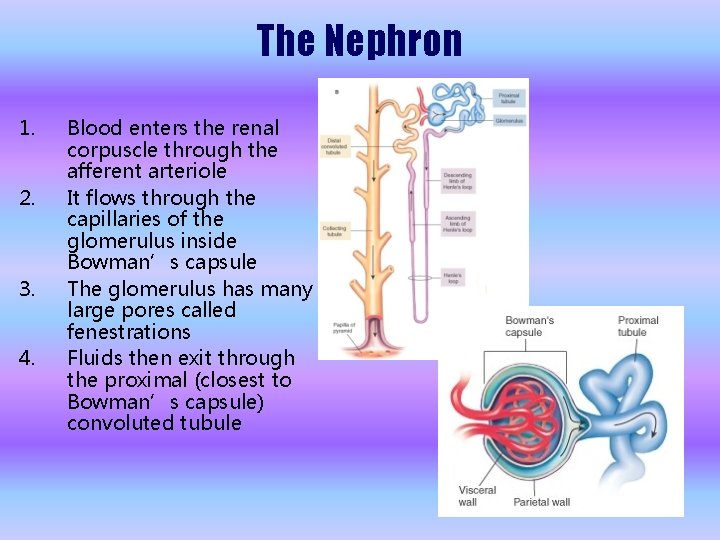
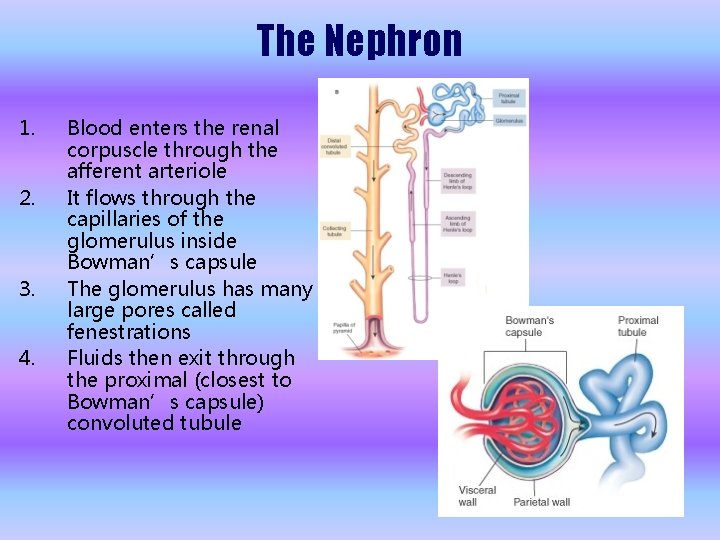
The Nephron 1. 2. 3. 4. Blood enters the renal corpuscle through the afferent arteriole It flows through the capillaries of the glomerulus inside Bowman’s capsule The glomerulus has many large pores called fenestrations Fluids then exit through the proximal (closest to Bowman’s capsule) convoluted tubule
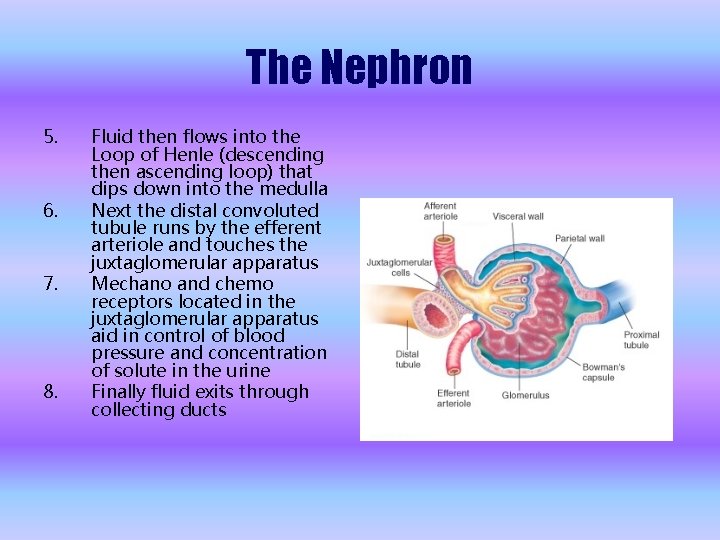
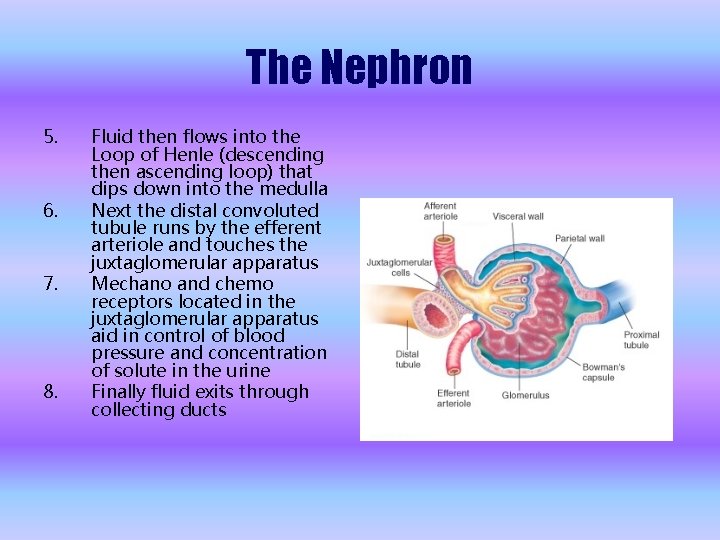
The Nephron 5. 6. 7. 8. Fluid then flows into the Loop of Henle (descending then ascending loop) that dips down into the medulla Next the distal convoluted tubule runs by the efferent arteriole and touches the juxtaglomerular apparatus Mechano and chemo receptors located in the juxtaglomerular apparatus aid in control of blood pressure and concentration of solute in the urine Finally fluid exits through collecting ducts
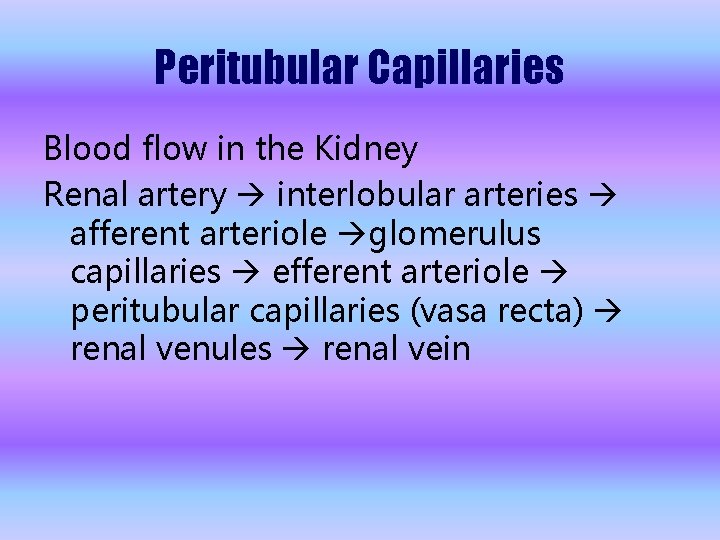
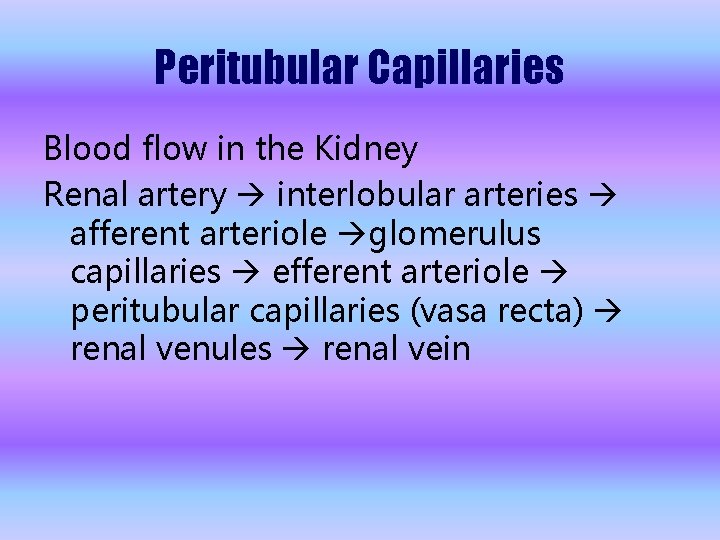
Peritubular Capillaries Blood flow in the Kidney Renal artery interlobular arteries afferent arteriole glomerulus capillaries efferent arteriole peritubular capillaries (vasa recta) renal venules renal vein
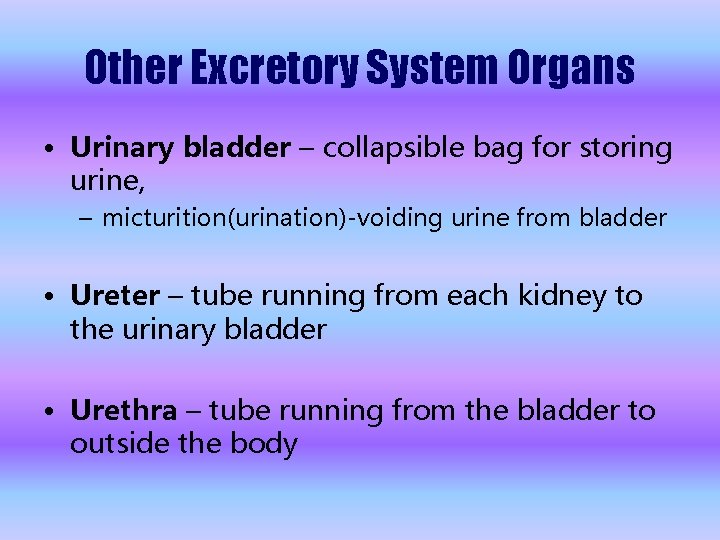
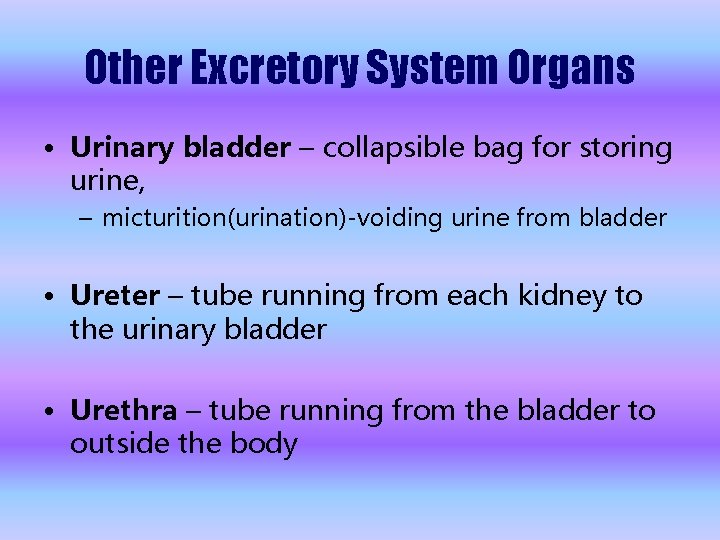
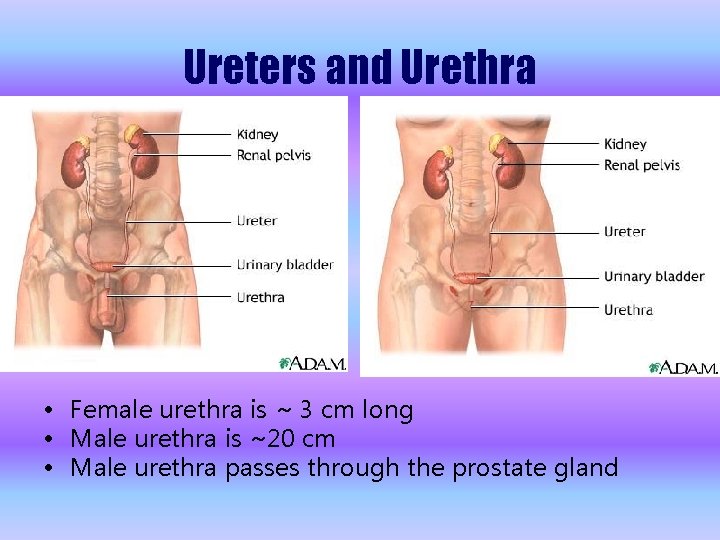
Other Excretory System Organs • Urinary bladder – collapsible bag for storing urine, – micturition(urination)-voiding urine from bladder • Ureter – tube running from each kidney to the urinary bladder • Urethra – tube running from the bladder to outside the body
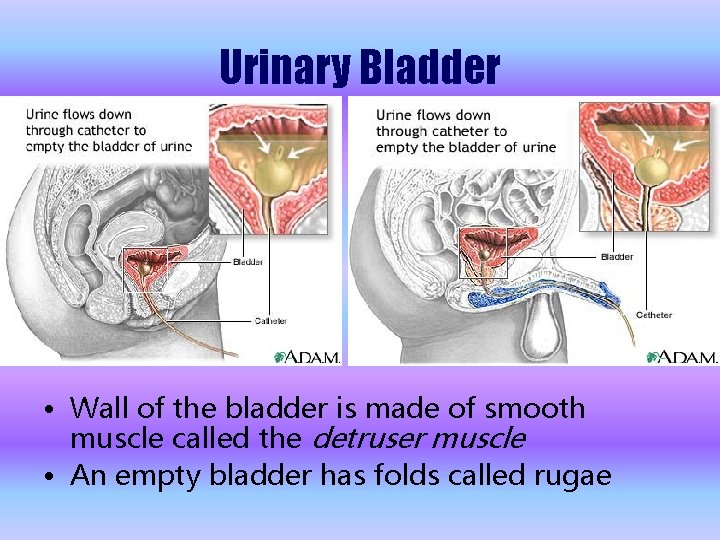
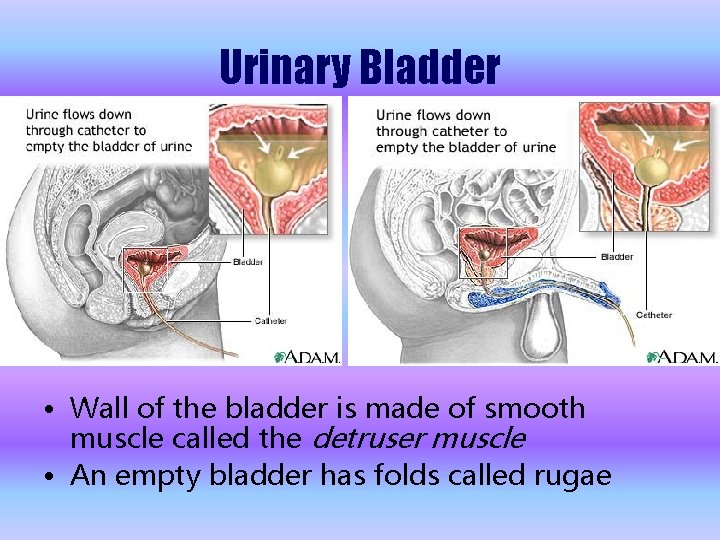
Urinary Bladder • Wall of the bladder is made of smooth muscle called the detruser muscle • An empty bladder has folds called rugae
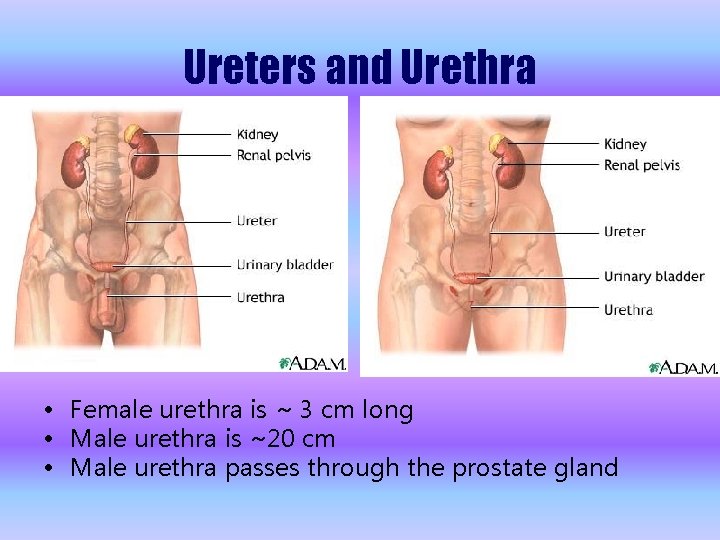
Ureters and Urethra • Female urethra is ~ 3 cm long • Male urethra is ~20 cm • Male urethra passes through the prostate gland
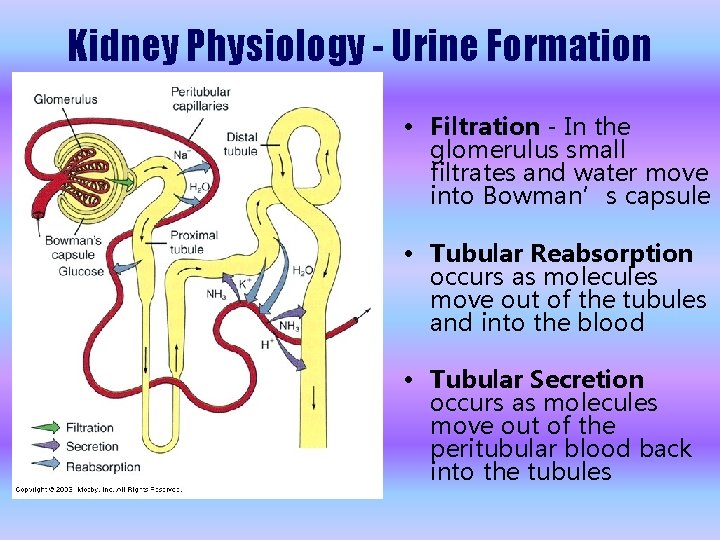
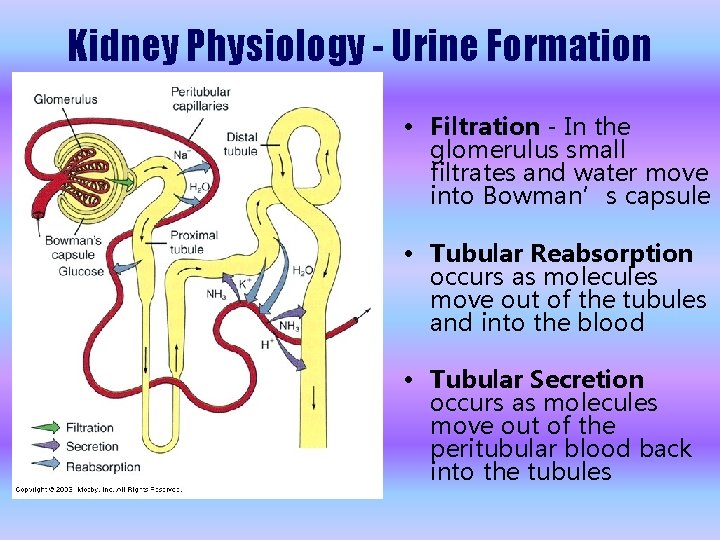
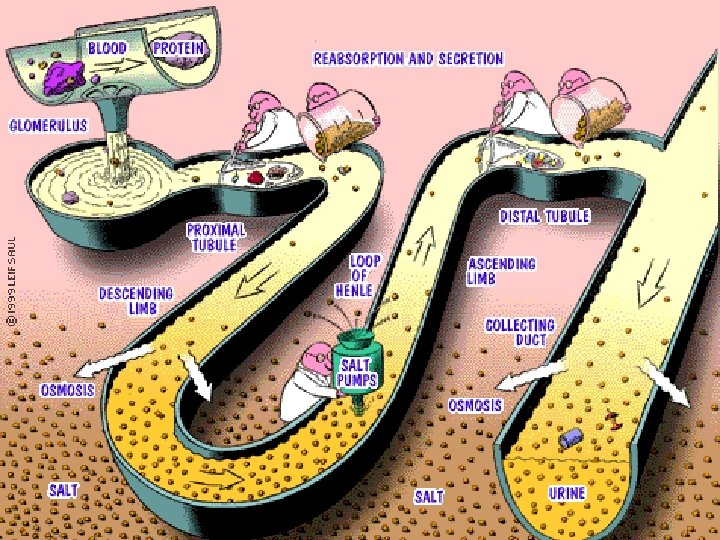
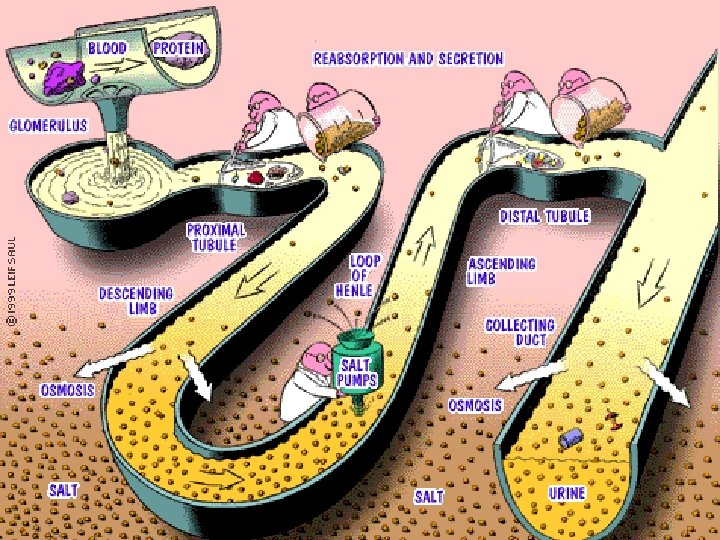
Kidney Physiology - Urine Formation • Filtration - In the glomerulus small filtrates and water move into Bowman’s capsule • Tubular Reabsorption occurs as molecules move out of the tubules and into the blood • Tubular Secretion occurs as molecules move out of the peritubular blood back into the tubules
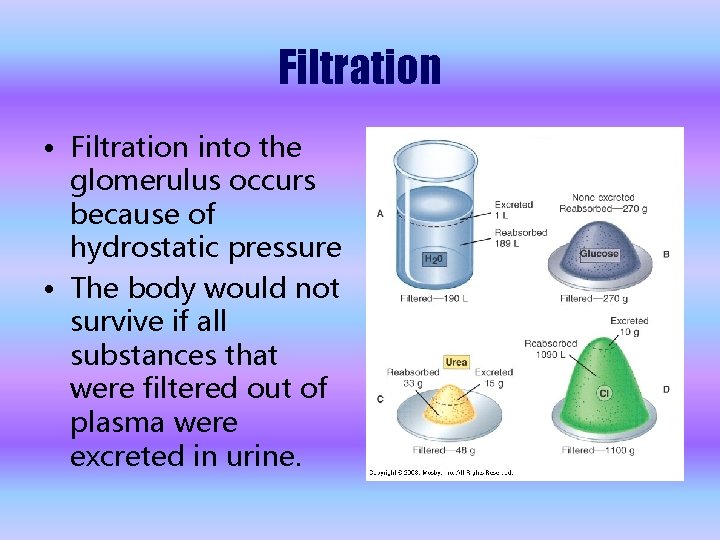
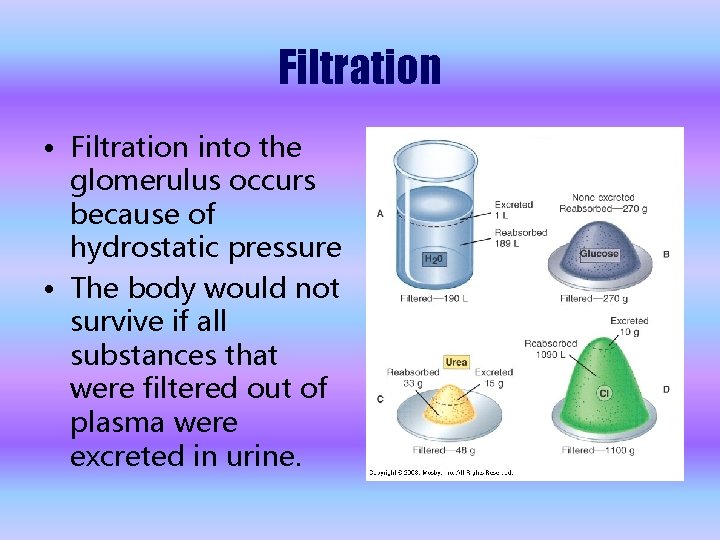
Filtration • Filtration into the glomerulus occurs because of hydrostatic pressure • The body would not survive if all substances that were filtered out of plasma were excreted in urine.
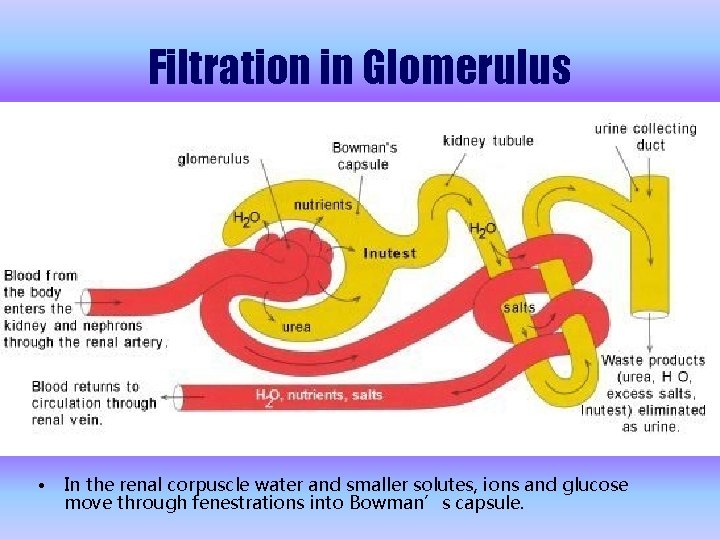
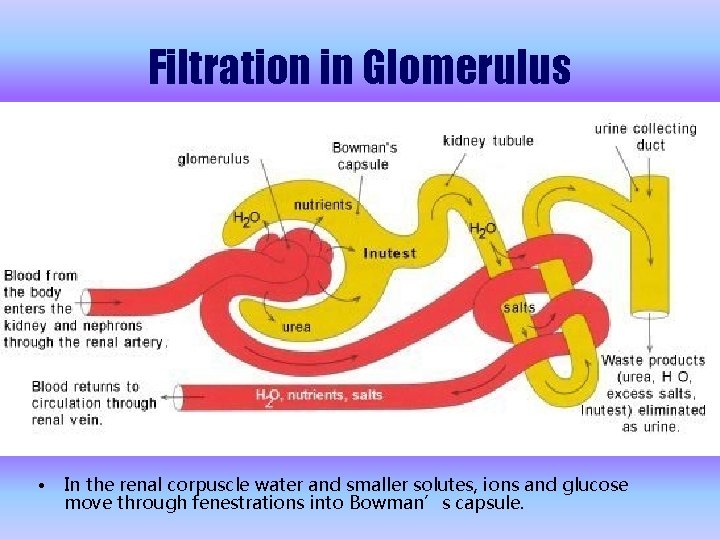
Filtration in Glomerulus • In the renal corpuscle water and smaller solutes, ions and glucose move through fenestrations into Bowman’s capsule.
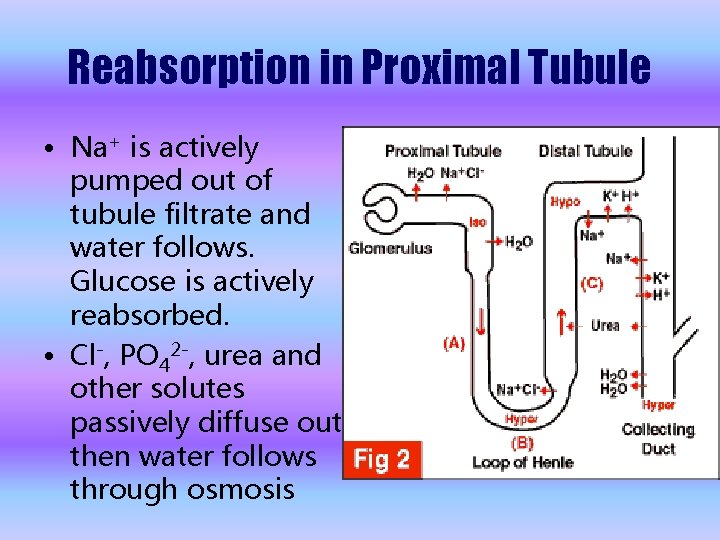
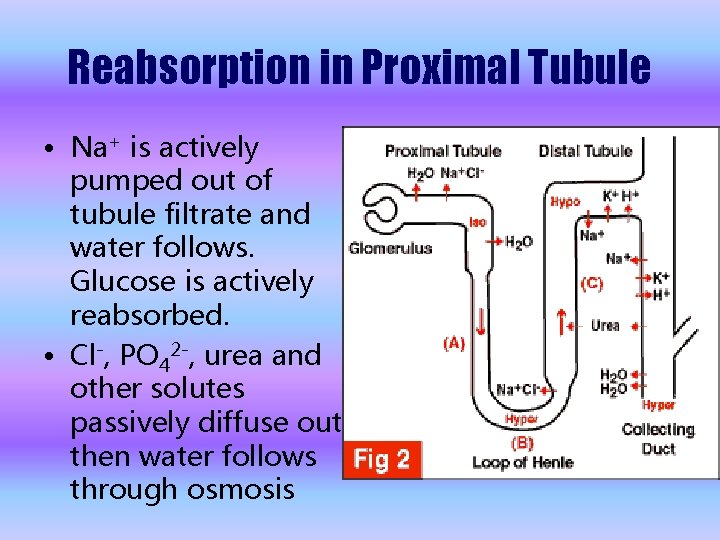
Reabsorption in Proximal Tubule • Na+ is actively pumped out of tubule filtrate and water follows. Glucose is actively reabsorbed. • Cl-, PO 42 -, urea and other solutes passively diffuse out then water follows through osmosis
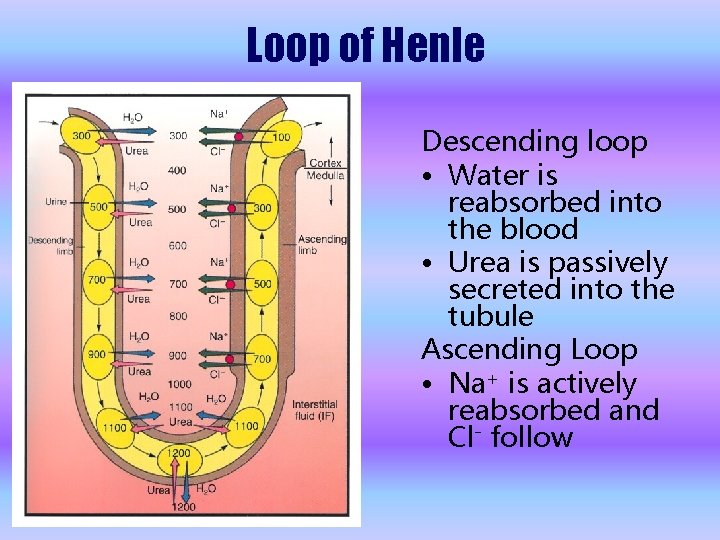
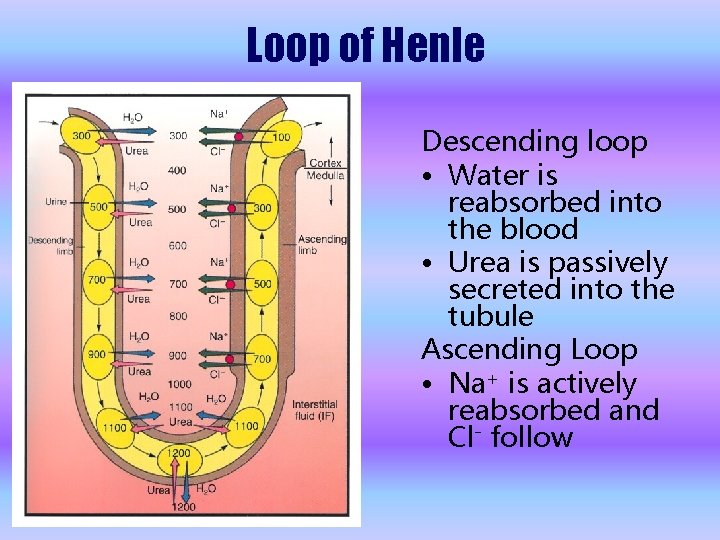
Loop of Henle Descending loop • Water is reabsorbed into the blood • Urea is passively secreted into the tubule Ascending Loop • Na+ is actively reabsorbed and Cl- follow
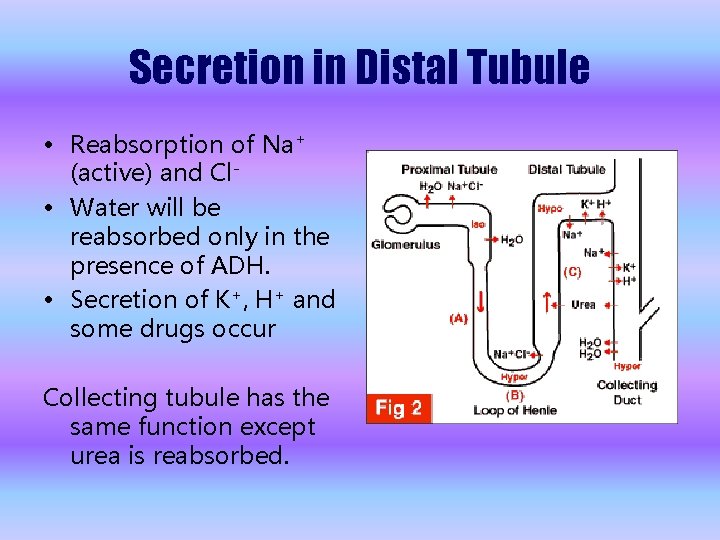
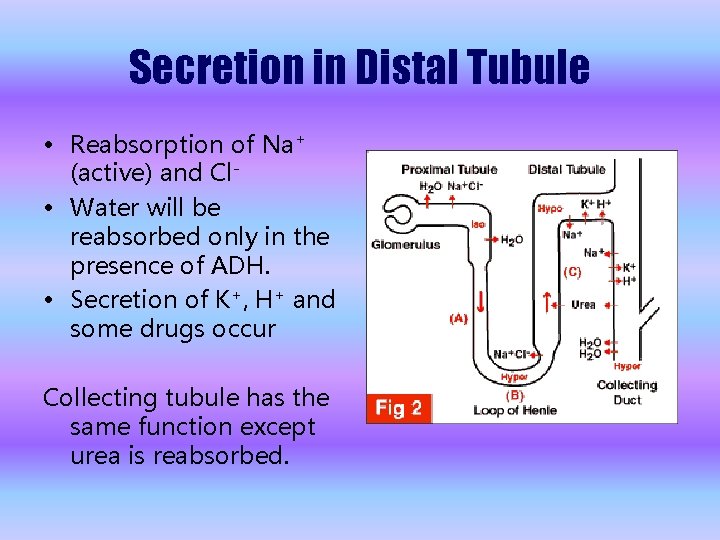
Secretion in Distal Tubule • Reabsorption of Na+ (active) and Cl • Water will be reabsorbed only in the presence of ADH. • Secretion of K+, H+ and some drugs occur Collecting tubule has the same function except urea is reabsorbed.
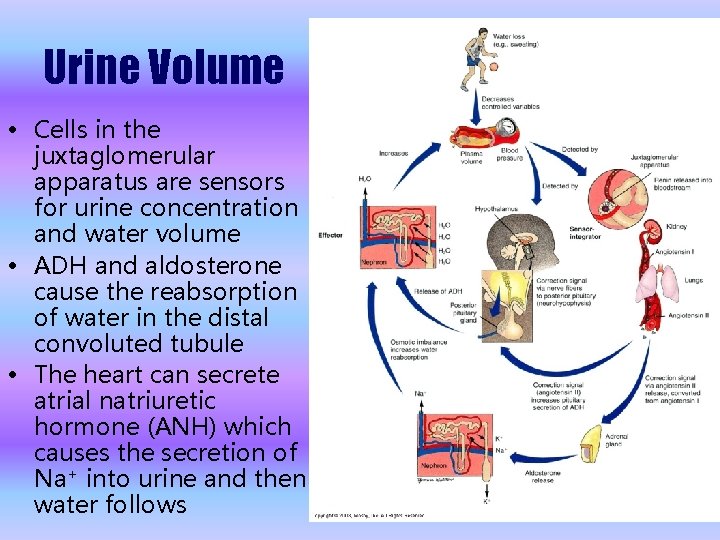
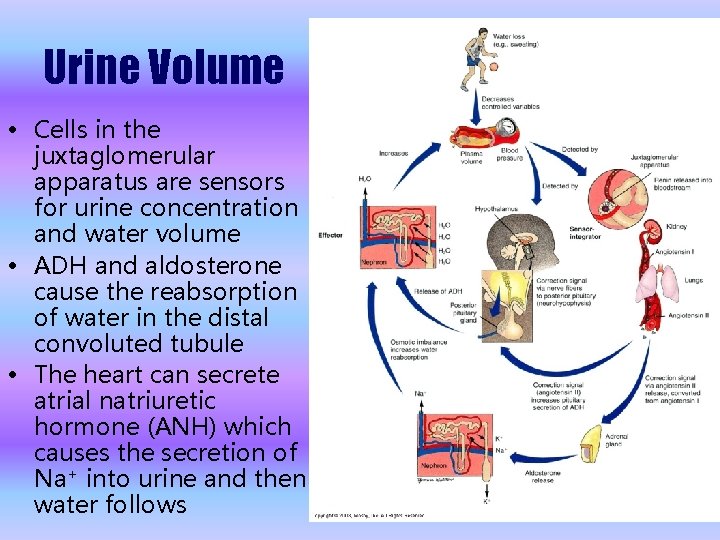
Urine Volume • Cells in the juxtaglomerular apparatus are sensors for urine concentration and water volume • ADH and aldosterone cause the reabsorption of water in the distal convoluted tubule • The heart can secrete atrial natriuretic hormone (ANH) which causes the secretion of Na+ into urine and then water follows
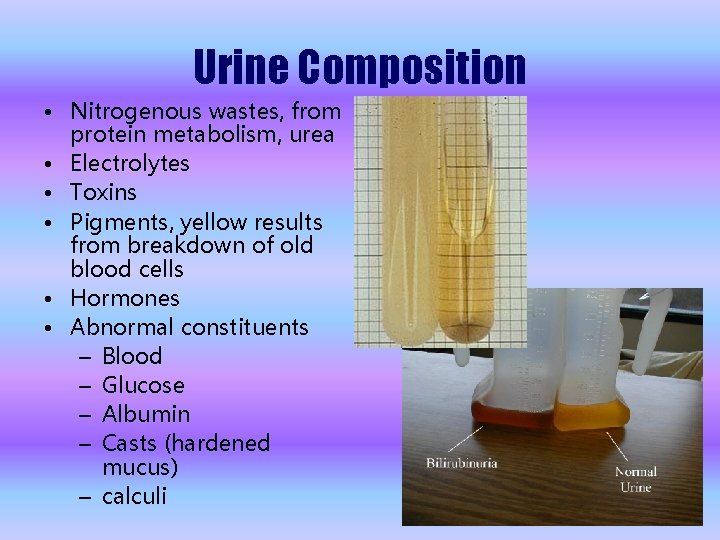
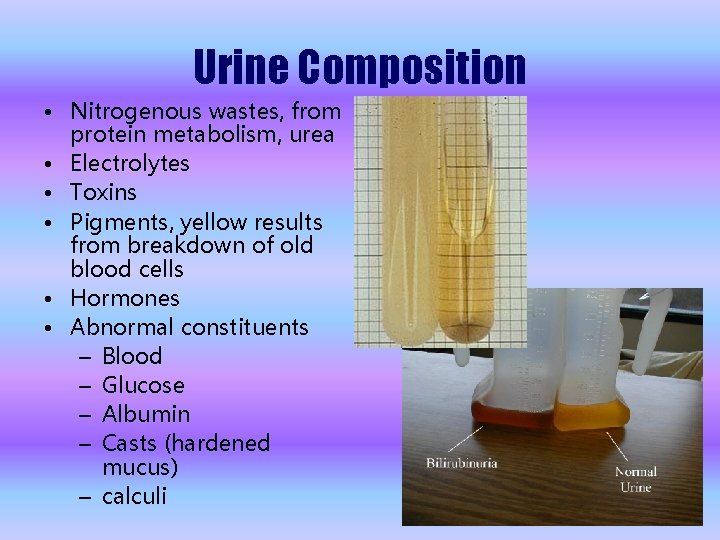
Urine Composition • Nitrogenous wastes, from protein metabolism, urea • Electrolytes • Toxins • Pigments, yellow results from breakdown of old blood cells • Hormones • Abnormal constituents – Blood – Glucose – Albumin – Casts (hardened mucus) – calculi
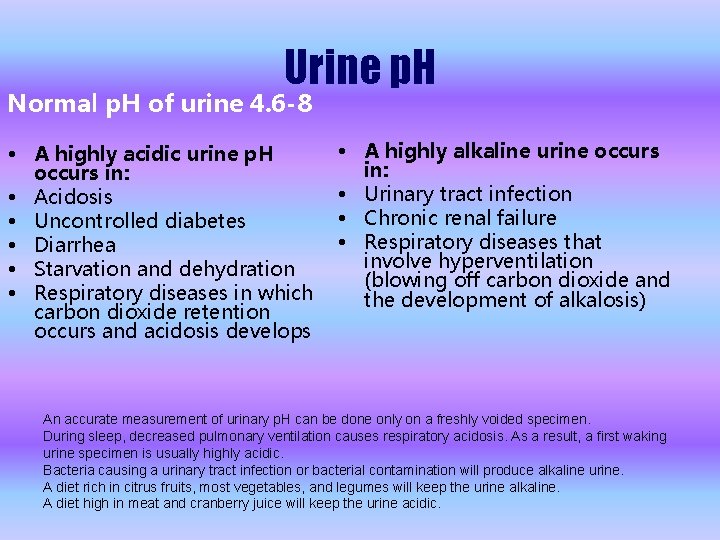
Urine p. H Normal p. H of urine 4. 6 -8 • A highly acidic urine p. H occurs in: • Acidosis • Uncontrolled diabetes • Diarrhea • Starvation and dehydration • Respiratory diseases in which carbon dioxide retention occurs and acidosis develops • A highly alkaline urine occurs in: • Urinary tract infection • Chronic renal failure • Respiratory diseases that involve hyperventilation (blowing off carbon dioxide and the development of alkalosis) An accurate measurement of urinary p. H can be done only on a freshly voided specimen. During sleep, decreased pulmonary ventilation causes respiratory acidosis. As a result, a first waking urine specimen is usually highly acidic. Bacteria causing a urinary tract infection or bacterial contamination will produce alkaline urine. A diet rich in citrus fruits, most vegetables, and legumes will keep the urine alkaline. A diet high in meat and cranberry juice will keep the urine acidic.
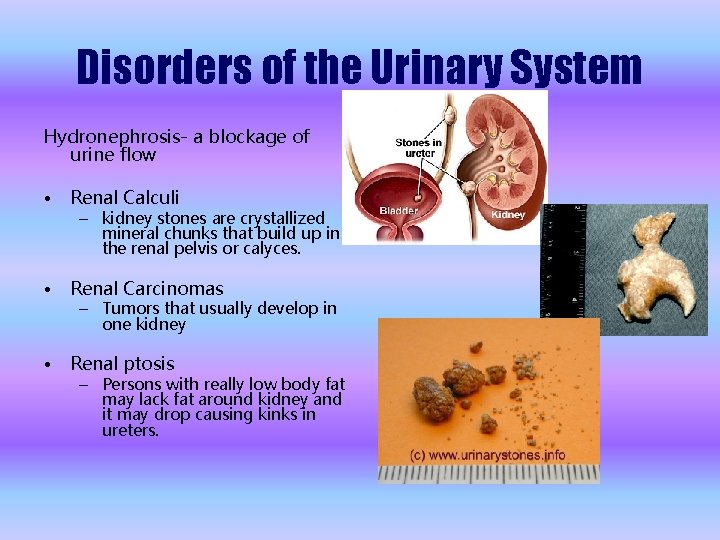
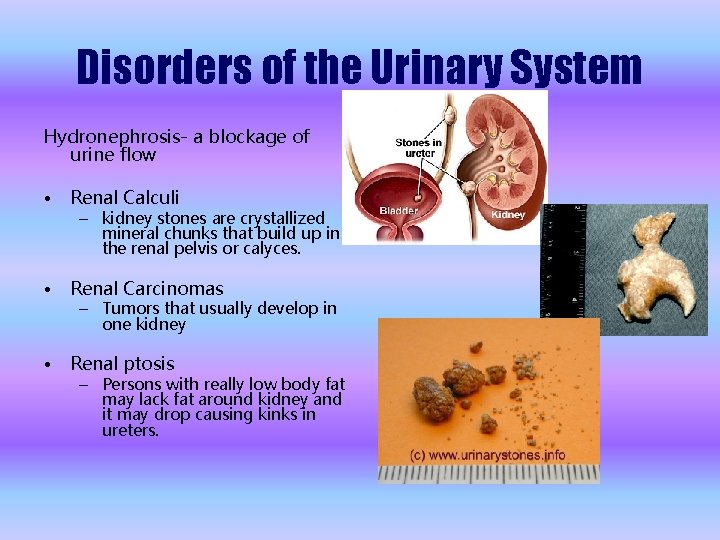
Disorders of the Urinary System Hydronephrosis- a blockage of urine flow • Renal Calculi • Renal Carcinomas • Renal ptosis – kidney stones are crystallized mineral chunks that build up in the renal pelvis or calyces. – Tumors that usually develop in one kidney – Persons with really low body fat may lack fat around kidney and it may drop causing kinks in ureters.
Disorders of the Urinary System Glycosuria- glucose in urine Hematuria- Blood in urine Pyuria- pus in urine Dysuria- painful urination Polyuria- large amounts of urine Oliguria- scant urine Anuria- absence of urine Incontinence- uncontrolled urination
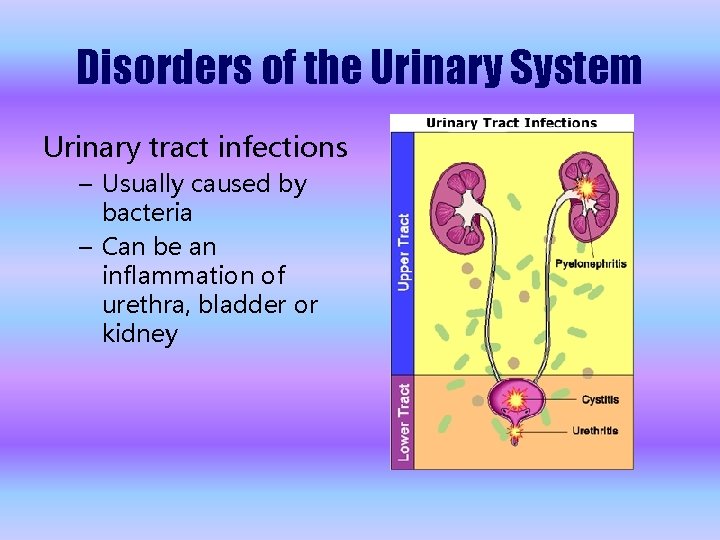
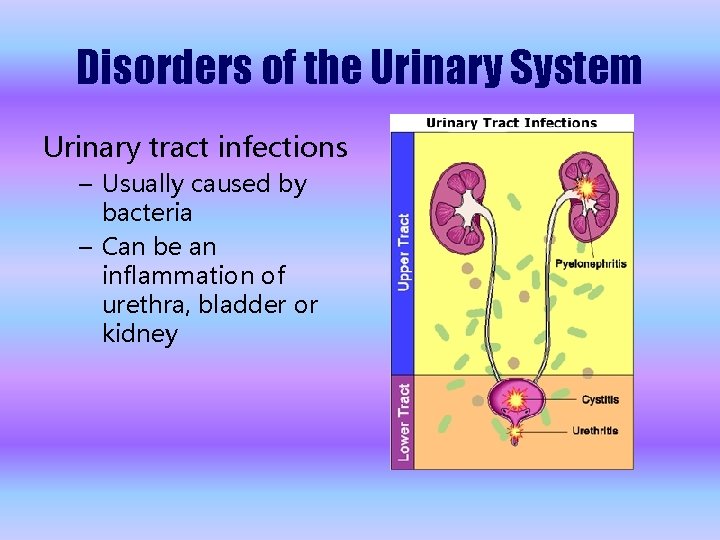
Disorders of the Urinary System Urinary tract infections – Usually caused by bacteria – Can be an inflammation of urethra, bladder or kidney
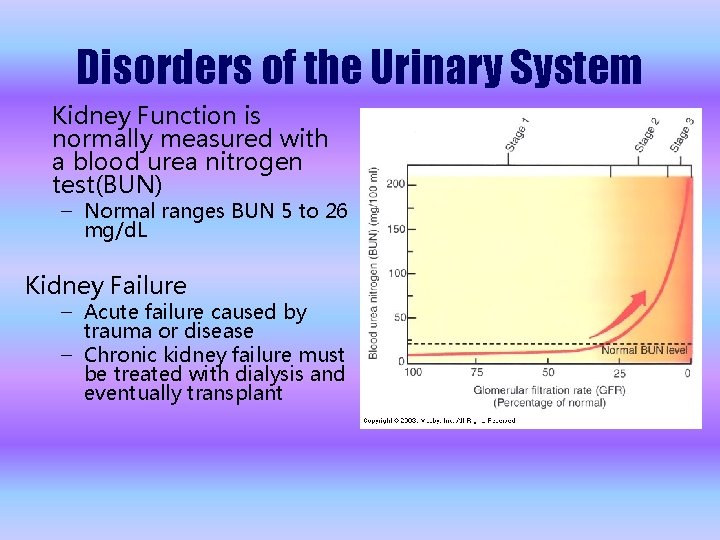
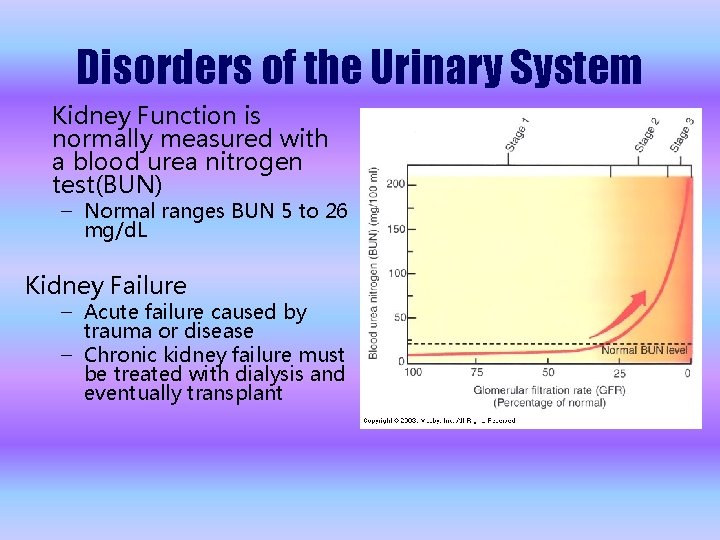
Disorders of the Urinary System Kidney Function is normally measured with a blood urea nitrogen test(BUN) – Normal ranges BUN 5 to 26 mg/d. L Kidney Failure – Acute failure caused by trauma or disease – Chronic kidney failure must be treated with dialysis and eventually transplant
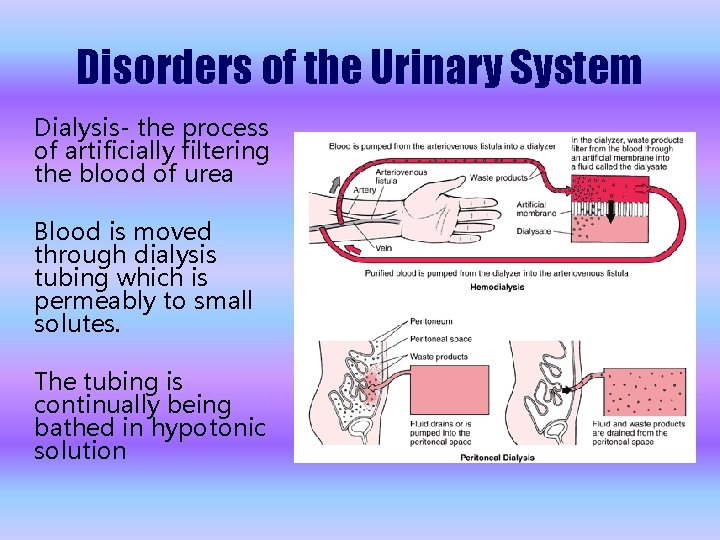
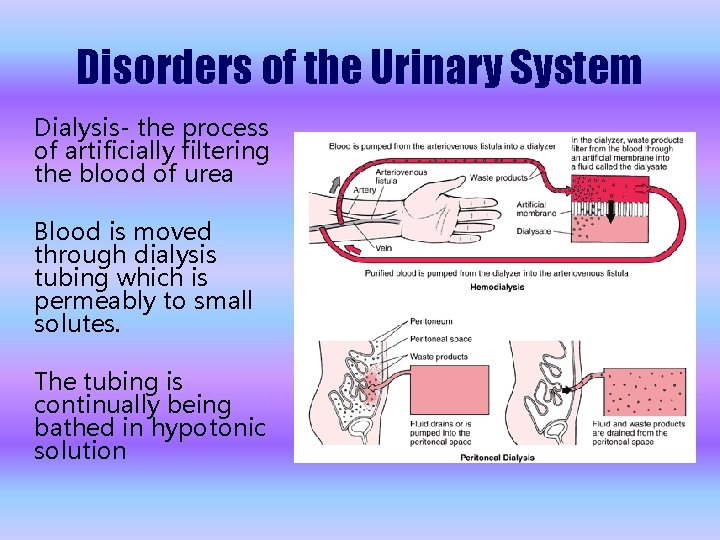
Disorders of the Urinary System Dialysis- the process of artificially filtering the blood of urea Blood is moved through dialysis tubing which is permeably to small solutes. The tubing is continually being bathed in hypotonic solution